Postpartum depression is related to a variety of adverse health outcomes for mothers and children1–3. Of particular concern, when compared to older mothers, being an adolescent mother is associated with an assortment of risks that precede the pregnancy, such as adverse experiences in childhood, as well as risks that occur together with raising the child, such as experiencing postpartum depression2–5. Children of mothers with postpartum depression are more likely to have a constellation of adverse outcomes including lower infant birth weight, lower child growth, increased risk for childhood obesity, as well as adverse neurodevelopmental and behavioral outcomes 6,7 that may persist into childhood8 and increase the risk for childhood mental health disorders9. Moreover, estimates in low and middle income countries suggest up to 25% of pregnant women experience symptoms of common mental health disorders including depression6. Thus, adolescent mothers in low and middle income countries are particularly vulnerable to pregnancy related complications, as maternal and reproductive health problems are a key cause of disease burden10.
One consistent predictor of postpartum depression is adverse experiences in childhood11. Adolescent mothers living in post-conflict countries, such as Peru, are known to have a high burden of childhood adversity12. For pregnant women in Peru, prior exposure to adverse childhood experiences is associated with an increased risk of poor general health, intimate partner violence, and depressive symptoms occurring during pregnancy13. To date, the majority of research has examined associations of physical, sexual, or psychological abuse experienced in childhood or adulthood intimate partner violence with postpartum depression in Peru6,13–15. While evidence suggests that childhood abuse is one of the strongest predictors of psychopathology such as postpartum depression, other forms of adversities, such as overall household dysfunction, are also important predictors of postpartum depression16. Household dysfunction encompasses events that occurred for others in the child’s household environment including substance use in the household, incarceration of a household member, mental health disorders, and witnessing violence against their mother. Household dysfunction, along with other forms of adverse childhood events, contributes to poor health outcomes in adulthood17, including increased likelihood of an unplanned pregnancy18. Yet, few studies have focused specifically on household dysfunction as related to postpartum depression 16.
Some investigators have examined resilience, or the strengths and resources that enable an individual to overcome the adverse effects of exposure to a risk factor19. Resilience refers to “the process of overcoming the negative effects of risk exposure, coping successfully with traumatic experiences, and avoiding the negative trajectories associated with risks19.” Resilience is not to be confused with positive outcomes or a lack of vulnerability. While some researchers refer to resilience as an outcome, resilience models would operationalize the outcome as “positive adjustment” or a “stable trajectory of mental health despite exposures to risk factors”20. Instead resilience is a set of promotive factors, including assets (i.e., coping skills) or resources (e.g., community organizations), that help an individual evade negative consequences of exposure19. Thus, the present manuscript conceptualizes as a set of promotive factors. In particular, we are interested in asset resilience, which we refer to here as resilience skills. Resilience skills have been conceptualized to include skills such as an individual’s ability to adapt to change, to cope with stress, and to tolerate negative emotions19,21. Resilience are active coping strategies that participants engage in order to minimize the negative consequences of resilience. In this way resilience skills can function as a compensatory (i.e., resilience has a direct effect on outcome), protective (i.e., resilience reduces effect on outcome), or challenge (i.e., resilience and risk factor have curvilinear relationship) promotive factors against negative life events or risk exposure19. Indeed, a substantial body of work has looked at resilience skills that mediate the relationship between risk exposures (e.g., adverse childhood experiences) and mental health22–25.
In the context of the present research, despite the consistent finding that household dysfunction and other adverse childhood experiences are a risk for postpartum depression3, not all young adult mothers with a history of adverse childhood events develop postpartum depression. Prior research has reported that resource resilience in adulthood, such as having social support and a positive maternal-child bond, moderate the relationship between adverse childhood events and symptoms of mental health in pregnant or postpartum period women11. Of note, investigators have reported that resilience skills mediate the relationship between childhood neglect and postpartum mental health symptoms22 including postpartum depression26,27, and risk of suicide28. However, to date, no investigative team has examined the influence of resilience skills on the relation between childhood household dysfunction and postpartum depression within adolescent mothers in Peru. Understanding the role of resilience in postpartum depression may inform future research on interventions to foster resilience skills which aim to reduce the postpartum depression health burden in adolescent mothers and their children.
Thus, the present study investigated the relationship between childhood household dysfunction and postpartum depression in adolescent mothers in Peru. We hypothesized that there would be a positive relationship between household dysfunction in childhood and postpartum depression. Additionally, we evaluated the extent to which, if at all, resilience skills mediated observed associations15. As discussed above, there are several ways resilience skills may influence outcomes including compensatory (i.e., resilience has a direct effect on outcome), protective (i.e., resilience reduces effect on outcome), or challenge (i.e., resilience and risk factor have curvilinear relationship) promotive factors against negative life events or risk exposure19. In line with prior research which looks at the mediating effect of resilience skills on the relation between other types of childhood neglect and mental health status in adulthood26,27, and consistent with the protective model of resilience, in which the resilience skills may diminish but does not remove the effect of the risk on the outcome in the population19, we hypothesized that the relationship between household dysfunction in childhood and postpartum depression would be mediated by resilience skills.
Methods
Participants and Procedure
The present study was conducted as a part of the Teen Pregnancy Outcomes Maternal and Infant Study (TPROMIS) carried out between November 2016 and September 2018. TPROMIS is an investigation of the risk and protective factors for trauma and mental health among adolescent mothers. Eligible participants (N = 789) were adolescent postpartum mothers, aged 14–18 years old, who gave birth at the Hospital San Bartolomé, Nacional Docente Madre Niño, in Lima, Peru. Following approval from the institutional review boards of the Harvard T. H. Chan School of Public Health in the Office of Human Research Administration, Boston, MA and San Bartolome, Lima, Peru, and completion of written informed consent, participants were interviewed using questionnaires. All interviews were completed in a private setting within a 2–3 days postpartum. Interviews were conducted by a midwife, fluent in Spanish, and trained in research methods. Participants were asked to provide information about sociodemographic characteristics, adverse experiences in childhood, symptoms of depression and anxiety, suicidal ideation, and resilience skills.
Postpartum Depression:
The Patient Health Questionnaire (PHQ-9) is a 9-item scale which screens for depression29 by asking participants to rate the frequency to which they experience depressive symptoms with response options of (0) “not at all,” (1) “several days”, (2) “more than half the days” and (3) “nearly every day.” In the present study, participants responded to items prompting them to recall the frequency they experienced depressive symptoms in the prior 2-weeks, or 14-days. The summary score of PHQ-9 scores can be used as a severity measure and range from 0 to 27. However, a provisional diagnosis of depression can also be assessed via cut off scores. Depression can be defined as score of 10 or greater, which has been supported by several large studies including a meta-analysis of individual participant data30,31. This cut-off for the PHQ-9 has also been validated in Spanish-speaking and pregnant populations32,33. The PHQ-9 was also found to have good reliability among pregnant women in Peru14. Cronbach’s alpha for depression was acceptable at 0.74.
Household Dysfunction in Childhood:
The adverse childhood experiences questionnaire utilized in the present study was adapted from Childhood Physical and Sexual Abuse Questionnaire17. Participants were asked to consider from “the time while you were growing up to now” and identify whether they had experienced the following events: (1) substance abuse in the household (alcohol, or other illicit substances), (2) mental illness (depression or suicide attempt) in the household, (3) incarceration of a household member, and (4) witnessed violence against their mother or step-mother (pushed, grabbed, slapped, or object thrown, being kicked, being bitten, being hit with fist, or being hit with a hard object, being repeatedly hit over at least a few minutes, or being threatened with or hurt by a knife or gun) in the household. The presence of each type of household dysfunction was coded with a binary indicator. Participants were defined as exposed to a category if they responded “yes” to 1 or more of the questions in that category. Cronbach’s alpha for household dysfunction was acceptable at 0.75.
Resilience-
Resilience skills were assessed using the Connor-Davidson Resilience Scale 10-item (CD-RISC-10)34, an abbreviated version of the 25-item CD-RISC21. Participants rate how often they identify with statements of resilience, such as “I am able to adapt to change”, apply to them from (0) “never” to (4) “almost always.” The CD-RISC assesses a respondents ability to: (1) adapt to change, (2) deal with whatever comes their way, (3) try to see the humorous side of problems, (4) bounce back after illness or hardship, (5) achieve goals despite obstacles, (6) believe that coping with stress can strengthen them, (7) stay focused under pressure, (8) not be easily discouraged by failure, (9) think of themselves as a strong person, and (10) handle unpleasant feelings. Resilience skills are calculated by summing participants’ scores that range from 0 to 40. The Spanish language version of CD-RISC-10 has been previously validated35. Our team has recently documented the construct validity and reliability of the CDI-RISC-10 in the present study population (Levey, 2020, personal communication). Cronbach’s alpha for resilience skills was good at 0.8.
Other Covariates:
Participant age was categorized as: 14–15, 16–17, and 18 years. Other sociodemographic variables were categorized as: educational attainment (≤6 years, 7–12 years, and >12 years of completed schooling); participant ethnicity (Mestizo (or mixed race) vs. other); living situation (living with parents, living with partner, or other); access to basics such as foods (hard, not very hard); and planned pregnancy (yes, no).
Statistical Analysis:
We first examined the frequency distribution of demographic variables and childhood household dysfunction. Comparisons of categorical variables were made between those who experienced household dysfunction, and those who did not using Chi-squared tests. Then, student’s t tests evaluated mean differences. Logistic regression was used to calculate odds ratios (ORs) and 95 percent confidence intervals (95% CI) to assess the relation of exposure factors that were consistent with household dysfunction and postpartum depression. In addition, exploratory mediation analysis was conducted to assess if the relation between childhood household dysfunction and postpartum depression could be partially explained through the indirect effects of resilience skills). Mediation analysis tested whether the relation between childhood household dysfunction and postpartum depression could be explained through the pathway of resilience skills, or both. Resilience is a hypothesized mediator of adverse experiences in childhood (i.e., household dysfunction) and mental disorders (i.e.., postpartum depression)22–25,36. We conducted the mediation analysis in line with other epidemiological studies that have sought to understand mechanistic pathways37. The mediation analysis was accomplished by fitting two regression models, a log-linear regression for resilience skills (the mediator) and a log-linear regression model for postpartum depression, adjusting for confounders. The mediation analysis decomposes the total effect of household dysfunction on postpartum depression into two components: the OR of a natural direct effect (NDE) and an OR of a natural indirect effect (NIE). The NDE is interpreted as the effect of household dysfunction on postpartum depression if the mediator (resilience skills) was set to what it would have been without household dysfunction as a child38. The NIE is interpreted as the effect on postpartum depression when household dysfunction is present after setting resilience skills (mediator) to what it would have been with versus without household dysfunction as a child. All analyses were performed with Stata 39.
Results:
Table 1 summarizes the sociodemographic and mental health characteristics of the study sample. Mean age of the participants was approximately 17 years (M = 17.1, SD = 1.1); nearly half of the participants living with the father of the infant (45.12%), and the overwhelming majority of participants completed at least seven years of education (93.71%). Roughly 73% of the participants reported difficulty paying for basics such as food items. The prevalence of postpartum depression was 10%. About 20% of the participants reported a childhood history of substance use in the household, 6% reported a childhood history of incarceration of a household member, about 10% reported a childhood history of mental illness in the household, and about 16% reported a childhood history of witnessing violence committed against their mother. The association between the history of childhood household dysfunction and postpartum depression is presented in Table 2. Compared with those who did not report childhood dysfunction, those who reported experiencing any childhood household dysfunction had increased odds of postpartum depression (aOR = 3.0; 95% CI: 1.88–4.82). After adjusting for potential confounders including age, race, and difficulty paying for basics, those who had childhood experience with substance abuse in the household (aOR = 2.79; 95% CI 1.63–4.7), incarceration of a household member (aOR = 2.94; 95% CI 1.37–5.91), mental illness in the household (aOR = 3.18; 95% CI 1.59–6.02), or witnessing violence committed against their mother (aOR = 1.91; 95% CI 1.09–3.26) had increased odds of postpartum depression compared with those who reported no household dysfunction in childhood. Given prior findings which focus on the robust influence of childhood physical and sexual abuse on adult health outcomes16, we further adjusted for childhood physical or sexual abuse. The magnitude of associations remained virtually identical for any childhood household dysfunction (aOR = 3.16, 95% CI 1.96–5.14), substance abuse in the household (aOR = 2.91, 95% CI 1.69–4.93), incarceration of a household member (aOR = 2.63, 95% CI 1.21–5.36), mental illness in the household (aOR = 3.17, 95% CI 1.58–6.04), and witnessing violence committed against their mother (aOR = 2.05, 95% CI 1.15–3.55). Additionally, we looked at the cumulative risk of reporting childhood household dysfunction. Those who reported one type of dysfunction (aOR = 3.04, 95% CI 1.70, 5.35), two types of dysfunction (aOR = 1.65 95% CI 0.56, 3.90), and three or more types of dysfunction (aOR = 6.10, 95% CI 2.67, 13.3) all had a higher risk of postpartum depression than those who reported no childhood household dysfunction. Logistic regression assessing the cumulative effect of reported childhood dysfunctions found a positive relationship between number of childhood household dysfunctions reported and postpartum depression (B = 0.53, p < 0.001).
Table 1.
Sociodemographic and mental health characteristics of the study population (N=789)
| Characteristics | All Participants (N=789) | |
|---|---|---|
| n | % | |
| Age (years) | ||
| ≤15 | 91 | 11.7 |
| 16–17 | 309 | 39.7 |
| 18 | 379 | 48.7 |
| Education (years) | ||
| ≤6 | 27 | 3.5 |
| 7–12 | 730 | 93.7 |
| >12 | 22 | 2.8 |
| Mestizo ethnicity | 537 | 68.1 |
| Live with | ||
| Parents | 212 | 27.3 |
| Father of your baby | 351 | 45.1 |
| Other | 215 | 27.6 |
| Difficulty paying for basics | ||
| Very hard/hard/somewhat hard | 539 | 73.2 |
| Not very hard | 197 | 26.8 |
| Planned Pregnancy | 130 | 16.5 |
| C-section Delivery | 191 | 24.2 |
| Childhood history of substance use in household | ||
| Alcohol | 121 | 15.3 |
| Other illicit substances | 47 | 6 |
| Both alcohol and other illicit substances | 30 | 3.8 |
| Childhood history of incarceration of a household member | 52 | 6.6 |
| Childhood history of mental illness in household | ||
| Depression or other mental illness | 36 | 4.6 |
| Suicide attempt | 41 | 5.2 |
| Both mental illness and suicide attempt | 14 | 1.8 |
| Childhood history of witnessing violence against their mother | ||
| Pushed, grabbed, slapped, object thrown at | 143 | 18.1 |
| Kicked, bitten, hit with fist, hit with hard object | 96 | 12.2 |
| Hit repeatedly over at least a few minutes | 89 | 11.3 |
| Threatened with, or hurt by, knife or gun | 9 | 1.1 |
| Depressive disorders (PHQ-9≥10) | 81 | 10.3 |
| Mean | SD | |
| Age (years) | 17.06 | 1.12 |
| Resilience (CD-RISC) | 34.5 | 5.3 |
Abbreviations: PHQ-9, The Patient Health Questionnaire 9-item, CD-RISC, Connor-Davidson Resilience Scale 10-item
Table 2.
Association between childhood household dysfunction and postpartum depression (N = 789)*
| No Depression | Depression | |||||
|---|---|---|---|---|---|---|
| Household Dysfunction | N | % | N | % | Unadjusted OR (CI 95%) | Adjusted OR (CI 95%) |
| Number of household dysfunctions reported | ||||||
| No dysfunction | 500 | 63.37 | 36 | 4.56 | Reference | Reference |
| Any dysfunction | 208 | 26.36 | 45 | 5.7 | 3.00 (1.89, 4.82) | 3.00 (1.88, 4.82) |
| Number of household dysfunction | ||||||
| 1 | 125 | 15.84 | 26 | 3.29 | 2.96 (1.71, 5.10) | 3.04 (1.70, 5.35) |
| 2 | 54 | 6.84 | 7 | 0.89 | 1.85 (0.72, 4.14) | 1.65 (0.56, 3.90) |
| ≥ 3 | 29 | 3.68 | 12 | 1.52 | 5.9 (2.70, 12.4) | 6.10 (2.67, 13.3) |
| *p-value for trend | B=0.53, p<0.001 | B=0.53, p<0.001 | ||||
| Type of household dysfunction | ||||||
| Substance use | 111 | 13.94 | 27 | 3.42 | 2.69 (1.61, 4.42) | 2.79 (1.63, 4.7) |
| Mental illness | 47 | 5.96 | 16 | 1.03 | 3.46 (1.81, 6.34) | 3.18 (1.59, 6.02) |
| Incarceration | 40 | 5.07 | 12 | 1.52 | 2.94 (1.42, 5.72) | 2.94 (1.37, 5.91) |
| Violence against mother | 125 | 15.84 | 23 | 2.92 | 1.85 (1.08, 3.08) | 1.91 (1.09, 3.26) |
Note: Analysis adjusted for maternal age (years), race (Mestizo vs. Other), difficulty paying for basics
Logistic regression
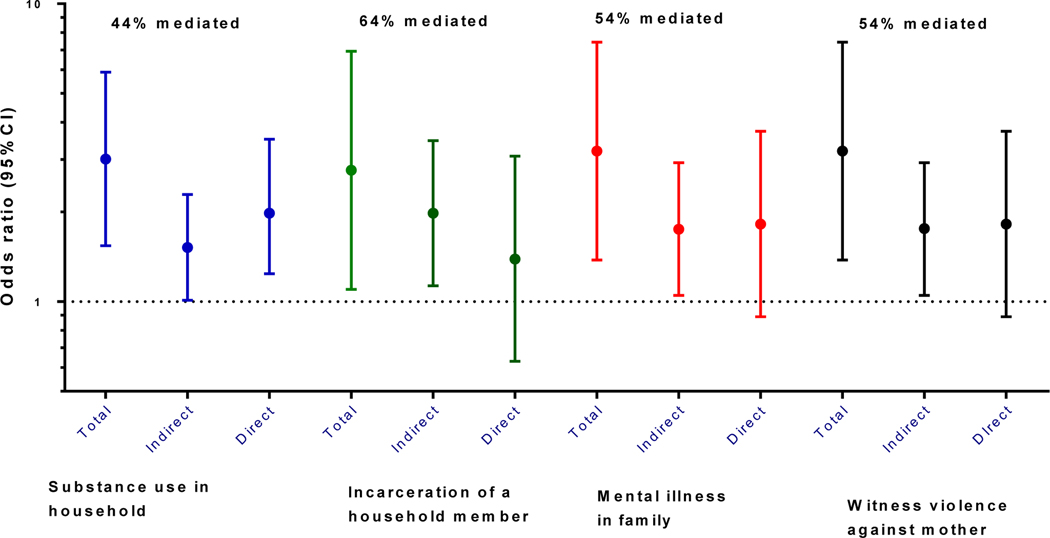
Since resilience skills may be on the causal pathway between household dysfunction in childhood and postpartum depression, we explored the extent to which resilience skills (as measured using CD-RISC) are a mediator of the association of childhood household dysfunction with sleep postpartum depression (Figure 1). From these analyses, we found that resilience skills accounted for 44% of the indirect effect of the relation between substance use in household and postpartum depression (Figure 1). Similarly, resilience skills accounted for 64% of the indirect effect of between the incarceration of a household member and postpartum depression, 54% of the indirect effect of between mental illness in the household and postpartum depression, and 54% of the indirect effect of between witnessing violence committed against their mother in household and postpartum depression (Figure 1).
Figure 1.
Total, indirect and direct effect of resilience onto relation between childhood household dysfunction and postpartum depression. Model adjusted for age, education, ethnicity, living situation, difficulty accessing basics, and planned pregnancy (N = 789).
Discussion
The present study extends the literature by documenting increases in the odds for postpartum depression among adolescent mothers with a history of childhood household dysfunction. This finding was also true for the subtypes of childhood household dysfunction including substance use in the household, mental illness in the household, incarceration of a household member, and witnessing violence against their mother, which were all associated with higher odds of postpartum depression. Additionally, the number of childhood household dysfunctions reported was associated with increased risk for postpartum depression. Our findings are largely consistent with prior studies documenting associations between household dysfunction and adverse health outcomes16,40.
While other studies have looked at the influence of resilience skills on household dysfunction and other forms of adverse experiences in childhood22,26–28, to our knowledge, this is the first study investigating resilience skills as a mediator of the relationship between childhood household dysfunction and postpartum depression in adolescent women in Peru. We found that the relationship between childhood household dysfunction and postpartum depression in adolescent mothers in Peru was partially mediated by resilience skills. The mediating effect of resilience is reminiscent of the Albee hypothesis, which postulated an equation in which “psychopathology risk” could be estimated by an “individual’s stress level” + “their particular organic factors” divided by “their coping skills” + “their self-esteem and social support”41. A more recent version of this is the mind body medicine equation, which to estimates “vulnerability to stress-related non-communicable diseases” by diving an individual’s stress level (“genetic vulnerability” + “adverse childhood experiences) by their resilience factors (“genetic endowment” + “positive psychology” + “healthy lifestyle)42.
The influence of resilience skills on the relationship between childhood household dysfunction and postpartum depression may have some preventative and clinical implications. Prior research has shown potential for postpartum home interventions, which target household dysfunction directly by increasing the quality of home environments43. Our findings suggest that influencing household dysfunction may also decrease postpartum depression in adolescent mothers. Thus, home based interventions that both aim to prevent childhood household dysfunction and provide strategies for developing resilience skills to cope with household dysfunction may also provide multiple avenues of prevention for and treatment of the intergenerational effects of postpartum depression3,7. Future work should investigate the clinical utility of developing resilience skills, like coping with adverse events or tolerating negative emotions, alongside other maternal health interventions as a way to diminish the injurious effects of household dysfunction on postpartum depression for adolescent mothers.
A few limitations should be considered when interpreting these study findings. First, care should be taken in interpreting the relationship between childhood household dysfunction and postpartum depression as the data were collected in a cross-sectional interview. Second, our results may not be generalizable to all adolescent mothers in Peru. As the participants were recruited from just one of the main hospitals in Lima, and with only 35% of Peruvian adolescents living in Lima44, the experiences of these young women in may not represent the experiences of teen mothers throughout the country. Additionally, up to 65% of adolescents in Lima live in low-income human settlements where they are unlikely to have access to health care44. In these environments, the experience of family tension, poverty, challenging transitions, racism, and violence may be even more amplified45. Thus, it is important to consider the effect of resilience skills based on the relevant challenges faced by adolescent mothers dependent on each particular social environmental context. Finally, there are limitations to self-report measures of resilience. Resilience theorists argue that the best measures of resilience are context, population, risk, and outcome dependent19. While our selected measure includes many resilience skills (e.g., coping with adverse events), there may be other skills specific to being an adolescent mother in Peru not measured by the scale used here. It is important to note that resilience is not a static trait, but a contextual set of skills which are dependent on variables such as environment, population, and outcome measured19.
Conclusions
In summary, childhood household dysfunction is positively related to postpartum depression in adolescent mothers in Peru. We found that resilience skills partially mediated this relation between childhood household dysfunction and postpartum depression. This is the first study, to our knowledge, to assess resilience skills as a mediator of the relation between childhood household dysfunction and postpartum depression in adolescent mothers in Peru. Future research should investigate the potential clinical implications of teaching resilience skills as a strategy to reduce the harmful effects of household dysfunction on postpartum depression in adolescent mothers in low- and middle-income countries.
Implication and Contribution.
The experience in childhood of substance use in the household and mental illness in the household are related to postpartum depression in adolescent mothers in Peru. Resilience partially mediated the relationship between the experience in childhood of substance use, mental illness, incarceration, and witnessing violence against your mother in the household and postpartum depression. Further work should investigate factors favoring resilience and other potential buffers of the deleterious mental health effects of adverse childhood events.
Sources of Funding and Acknowledgments:
This research was supported by funding from the National Institute of Health’s National Center on Minority Health and Health Disparities (T37MD001449) and National Institute of Mental Health (1t32MH116140–01, 5T32MH116140–02)
Footnotes
Disclosure of Potential Conflict: All authors have no potential conflict, perceived or otherwise to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Letourneau NL, Tramonte L, Willms JD. Maternal Depression, Family Functioning and Children’s Longitudinal Development. J Pediatr Nurs. 2013;28(3):223–234. doi: 10.1016/j.pedn.2012.07.014 [DOI] [PubMed] [Google Scholar]
- 2.Grace SL, Evindar A, Stewart DE. The effect of postpartum depression on child cognitive development and behavior: A review and critical analysis of the literature. Arch Womens Ment Health. 2003;6(4):263–274. doi: 10.1007/s00737-003-0024-6 [DOI] [PubMed] [Google Scholar]
- 3.Choi KW, Houts R, Arseneault L, Pariante C, Sikkema KJ, Moffitt TE. Maternal depression in the intergenerational transmission of childhood maltreatment and its sequelae: Testing postpartum effects in a longitudinal birth cohort. Dev Psychopathol. 2019;31(1):143–156. doi: 10.1017/S0954579418000032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clin Child Fam Psychol Rev. 2011;14(1):1–27. doi: 10.1007/s10567-010-0080-1 [DOI] [PubMed] [Google Scholar]
- 5.Baudry C, Tarabulsy GM, Atkinson L, Pearson J, St-pierre A. Intervention with Adolescent Mother-Child Dyads and Cognitive Development in Early Childhood: a Meta-Analysis. Prev Sci N Y. 2017;18(1):116–130. doi: 10.1007/s11121-016-0731-7 [DOI] [PubMed] [Google Scholar]
- 6.Gelaye B, Rondon M, Araya R, Williams MA. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry. 2016;3(10):973–982. doi: 10.1016/S2215-0366(16)30284-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McDonnell CG, Valentino K. Intergenerational Effects of Childhood Trauma: Evaluating Pathways Among Maternal ACEs, Perinatal Depressive Symptoms, and Infant Outcomes. Child Maltreat. 2016;21(4):317–326. doi: 10.1177/1077559516659556 [DOI] [PubMed] [Google Scholar]
- 8.Bennett IM, Schott W, Krutikova S, Behrman JR. Maternal mental health, and child growth and development, in four low-income and middle-income countries. J Epidemiol Community Health. 2016;70(2):168–173. doi: 10.1136/jech-2014-205311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Patel V, Flisher AJ, Nikapota A, Malhotra S. Promoting child and adolescent mental health in low and middle income countries. J Child Psychol Psychiatry. 2008;49(3):313–334. doi: 10.1111/j.1469-7610.2007.01824.x [DOI] [PubMed] [Google Scholar]
- 10.The Global Burden of Disease Child and Adolescent Health Collaboration, Kassebaum N, Kyu HH, et al. Child and Adolescent Health From 1990 to 2015: Findings From the Global Burden of Diseases, Injuries, and Risk Factors 2015 Study. JAMA Pediatr. 2017;171(6):573. doi: 10.1001/jamapediatrics.2017.0250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alvarez-Segura M, Garcia-Esteve L, Torres A, et al. Are women with a history of abuse more vulnerable to perinatal depressive symptoms? A systematic review. Arch Womens Ment Health. 2014;17(5):343–357. doi: 10.1007/s00737-014-0440-9 [DOI] [PubMed] [Google Scholar]
- 12.INEI, Instituto Nacional de Estadistica e Informatica. Perú: Indicadores de violencia familiar y sexual, 2009–2018. Published 2018. Accessed May 29, 2019. https://www.inei.gob.pe/media/MenuRecursivo/publicaciones_digitales/Est/Lib1584/libro.pdf [Google Scholar]
- 13.Barrios YV, Gelaye B, Zhong Q, et al. Association of Childhood Physical and Sexual Abuse with Intimate Partner Violence, Poor General Health and Depressive Symptoms among Pregnant Women. Elhai JD, ed. PLOS ONE. 2015;10(1):e0116609. doi: 10.1371/journal.pone.0116609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.ZHONG Q-Y WELLS A, RONDON MB, et al. Childhood Abuse and Suicidal Ideation in a Cohort of Pregnant Peruvian Women. Am J Obstet Gynecol. 2016;215(4):501.e1–501.e8. doi: 10.1016/j.ajog.2016.04.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Intimate Partner Violence and Risk for Depression Among Postpartum Women in Lima, Peru - ProQuest. Accessed May 29, 2019. https://search.proquest.com/openview/3eec975573efcf4f2c6c5bb3ab36791b/1?pq-origsite=gscholar&cbl=45619 [DOI] [PubMed]
- 16.Wilson LM, Reid AJ, Midmer DK, Biringer A, Carroll JC, Stewart DE. Antenatal psychosocial risk factors associated with adverse postpartum family outcomes. CMAJ Can Med Assoc J. 1996;154(6):785–799. [PMC free article] [PubMed] [Google Scholar]
- 17.Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults: The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14(4):245–258. doi: 10.1016/S0749-3797(98)00017-8 [DOI] [PubMed] [Google Scholar]
- 18.Dietz PM, Spitz AM, Anda RF, et al. Unintended Pregnancy Among Adult Women Exposed to Abuse or Household Dysfunction During Their Childhood. 282(14):1359–1364. doi: 10.1001/jama.282.14.1359 [DOI] [PubMed] [Google Scholar]
- 19.Fergus S, Zimmerman MA. ADOLESCENT RESILIENCE: A Framework for Understanding Healthy Development in the Face of Risk. Annu Rev Public Health. 2005;26(1):399–419. doi: 10.1146/annurev.publhealth.26.021304.144357 [DOI] [PubMed] [Google Scholar]
- 20.Bonanno GA. Loss, Trauma, and Human Resilience: Have We Underestimated the Human Capacity to Thrive After Extremely Aversive Events? Am Psychol. 2004;59(1):20–28. doi: 10.1037/0003-066X.59.1.20 [DOI] [PubMed] [Google Scholar]
- 21.Connor KM, Davidson JRT. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC). Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- 22.Lee SW, Bae GY, Rim H-D, et al. Mediating Effect of Resilience on the Association between Emotional Neglect and Depressive Symptoms. Psychiatry Investig. 2018;15(1):62–69. doi: 10.4306/pi.2018.15.1.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Catabay CJ, Stockman JK, Campbell JC, Tsuyuki K. Perceived stress and mental health: The mediating roles of social support and resilience among black women exposed to sexual violence. J Affect Disord. 2019;259:143–149. doi: 10.1016/j.jad.2019.08.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Charbonneau D. Model of mindfulness and mental health outcomes: Need fulfillment and resilience as mediators = Modèle de résultats de la pleine conscience et de la santé mentale: besoin de réalisation et de résilience en tant que médiateurs. Can J Behav Sci Rev Can Sci Comport. 2019;51(4):239–247. doi: 10.1037/cbs0000137 [DOI] [Google Scholar]
- 25.Fritz J, de Graaff AM, Caisley H, van Harmelen A-L, Wilkinson PO. A Systematic Review of Amenable Resilience Factors That Moderate and/or Mediate the Relationship Between Childhood Adversity and Mental Health in Young People. Front Psychiatry. 2018;9. doi: 10.3389/fpsyt.2018.00230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wingo AP, Wrenn G, Pelletier T, Gutman AR, Bradley B, Ressler KJ. Moderating effects of resilience on depression in individuals with a history of childhood abuse or trauma exposure. J Affect Disord. 2010;126(3):411–414. doi: 10.1016/j.jad.2010.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schulz A, Becker M, Van der Auwera S, et al. The impact of childhood trauma on depression: Does resilience matter? Population-based results from the Study of Health in Pomerania. J Psychosom Res. 2014;77(2):97–103. doi: 10.1016/j.jpsychores.2014.06.008 [DOI] [PubMed] [Google Scholar]
- 28.Roy A, Carli V, Sarchiapone M. Resilience mitigates the suicide risk associated with childhood trauma. J Affect Disord. 2011;133(3):591–594. doi: 10.1016/j.jad.2011.05.006 [DOI] [PubMed] [Google Scholar]
- 29.Kroenke K, Spitzer RL, Williams JBW. The PHQ-9. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Levis B, Benedetti A, Thombs BD. Accuracy of Patient Health Questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. Published online 2019:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ Can Med Assoc J. 2012;184(3):E191–E196. doi: 10.1503/cmaj.110829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhong Q-Y, Gelaye B, Rondon MB, et al. Using the Patient Health Questionnaire (PHQ-9) and the Edinburgh Postnatal Depression Scale (EPDS) to assess suicidal ideation among pregnant women in Lima, Peru. Arch Womens Ment Health. 2015;18(6):783–792. doi: 10.1007/s00737-014-0481-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Calderón M, Gálvez-Buccollini JA, Cueva G, Ordoñez C, Bromley C, Fiestas F. Validación de la versión peruana del PHQ-9 para el diagnóstico de depresión. Rev Peru Med Exp Salud Pública. 2012;29:578–579. doi: 10.1590/S1726-46342012000400027 [DOI] [PubMed] [Google Scholar]
- 34.Campbell-Sills L, Stein MB. Psychometric analysis and refinement of the connor–davidson resilience scale (CD-RISC): Validation of a 10-item measure of resilience. J Trauma Stress. 2007;20(6):1019–1028. doi: 10.1002/jts.20271 [DOI] [PubMed] [Google Scholar]
- 35.Notario-Pacheco B, Solera-Martínez M, Serrano-Parra MD, Bartolomé-Gutiérrez R, García-Campayo J, Martínez-Vizcaíno V. Reliability and validity of the Spanish version of the 10-item Connor-Davidson Resilience Scale (10-item CD-RISC) in young adults. Health Qual Life Outcomes. 2011;9(1):63. doi: 10.1186/1477-7525-9-63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sanchez SE, Pineda O, Chaves DZ, et al. Childhood physical and sexual abuse experiences associated with post-traumatic stress disorder among pregnant women. Ann Epidemiol. 2017;27(11):716–723.e1. doi: 10.1016/j.annepidem.2017.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Explanation in Causal Inference: Methods for Mediation and Interaction. Oxford University Press; 2015. [DOI] [PubMed] [Google Scholar]
- 38.Odds ratios for mediation analysis for a dichotomous outcome. - PubMed - NCBI. Accessed July 22, 2019. https://www-ncbi-nlm-nihgov.offcampus.lib.washington.edu/pubmed/21036955
- 39.StataCorp. Stat Statistical Software: Release 16. StataCorp LLC; 2019. [Google Scholar]
- 40.Gelaye B, Kajeepeta S, Zhong Q-Y, et al. Childhood abuse is associated with stress-related sleep disturbance and poor sleep quality in pregnancy. Sleep Med. 2015;16(10):1274–1280. doi: 10.1016/j.sleep.2015.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Albee GW. Preventing psychopathology and promoting human potential. Am Psychol. 1982;37:043–1050. [DOI] [PubMed] [Google Scholar]
- 42.Fricchione GL. Compassion and Healing in Medicine and Society. On the Nature and Uses of Attachment Solutions for Separation Challenges. Johns Hopkins University Press [Google Scholar]
- 43.Shaw E, Levitt C, Wong S, Kaczorowski J. Systematic Review of the Literature on Postpartum Care: Effectiveness of Postpartum Support to Improve Maternal Parenting, Mental Health, Quality of Life, and Physical Health. Birth. 2006;33(3):210–220. doi: 10.1111/j.1523-536X.2006.00106.x [DOI] [PubMed] [Google Scholar]
- 44.CPI (Compañía peruana de estudios de mercados y opinión pública). Peru: Población 2017. Mark Rep. Published online 2017. [Google Scholar]
- 45.Bayer AM, Gilman RH, Tsui AO, Hindin MJ. What is adolescence?: Adolescents narrate their lives in Lima, Peru. J Adolesc. 2010;33(4):509–520. doi: 10.1016/j.adolescence.2010.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]