Summary
Background
Studies vary with respect to the reported effects of day care attendance on childhood asthma.
Objectives
To evaluate the independent and combined effects of day care attendance and respiratory infections on the development of asthma at the age of seven in a prospective birth cohort.
Method
At the age of seven, the study sample included 589 children with complete data of 762 enrolled at birth. Day care hours and number of respiratory infections were reported in follow-up questionnaires through age four. At 7 years of age, asthma was diagnosed in 95 children (16%), based on predefined symptoms criteria confirmed by either asthma FEV1 reversibility after bronchodilator or a positive methacholine test (PC20 = 4 mg/mL). Logistic regression was used to investigate the relationships between asthma at the age of seven, cumulative hours of day care attendance and reported respiratory infections at ages 1–4.
Results
In the univariate analyses, day care attendance at 12 months was associated with an increased risk of asthma [odds ratio (OR) = 1.8, 95% confidence interval (CI) = 1.1–3.0]. Both upper and lower respiratory infections at 12 months also increased the likelihood of asthma [OR = 2.4 (1.4–4.1); OR = 2.3 (1.5–3.7), respectively]. In the final multivariate logistic model, cumulative hours of day care attendance and number of lower respiratory infections at 12 months were associated with asthma [OR = 1.2 (1.1–1.5); OR = 1.4 (1.2–1.7), respectively]. However, a threshold of greater than 37.5 hours per week of day care attendance was associated with a lower risk of asthma [OR = 0.6 (0.4–0.9)].
Conclusion
Depending on duration of attendance, day care during infancy can either increase or reduce risk of asthma at the age of seven.
Keywords: daycare, duration, respiratory infections, childhood, asthma
Introduction
Asthma prevalence has increased in the United States during the last 20 years and is the most common chronic disorder in children [1]. Numerous host and environmental factors have been suspected as playing causative roles [2]. Several hypotheses have been proposed to explain the increasing prevalence of allergic disorders and asthma during childhood [3]. The hygiene hypothesis, for example, proposes that a general decline in the frequency of early infections and reduced exposure to microbial products during infancy may alter the maturation of the immune system favouring Th2-biased allergic responses during infancy and childhood [4]. Altered exposures to environmental microbial flora (e.g. via alterations in the intestinal microbiome) unique to westernized lifestyles have been postulated to account for the increasing prevalence of asthma and other allergic diseases [5]. This theory is bolstered by epidemiological observations that the risk of asthma is reduced among children living with farm animals, thereby enhancing the opportunities for greater exposure to environmental sources of microbial contaminants in early childhood [6]. If this were true, children attending day care with ample opportunities for daily exposure to microbial contaminants from other children may be less likely to develop asthma and other allergic disorders including asthma. However, the results of cross-sectional and longitudinal studies examining the effect of attendance at day care on the development of asthma are conflicting.
In some reports, day care attendance is inversely associated with asthma development [7–10], whereas in other studies, children attending day care in early childhood are at increased risk for childhood asthma [11, 12]. It is known that children attending day care contract more respiratory tract infections than children living at home [13, 14]. In a birth cohort study of children born to atopic parents, Jackson et al. [15] demonstrated that early rhinovirus infections are associated with a greater likelihood of asthma at the age of six. Thus, uncertainty persists as to whether or not early exposure to the day care milieu during infancy and early childhood enhances or reduces the risk of asthma. To address these questions, we hypothesized that early exposure to day care and occurrence of early respiratory infections were likely to independently increase the risk for later development of childhood asthma. Using longitudinal data from the Cincinnati Childhood Allergy and Air Pollution Study (CCAAPS) birth cohort, we investigated the association between duration and timing of day care attendance, reported respiratory infections during the first 4 years of life and the development of asthma objectively confirmed at the age of seven.
Methods
The CCAAPS birth cohort study has been described in our previously published studies. Infants born in the Greater Cincinnati and Northern Kentucky area were identified from birth records and recruited between 2001 and 2003 [16, 17]. The hypothesis of the CCAAPS study was that early life exposure to traffic pollutants increased risk for allergic sensitization and development of allergic rhinitis and asthma during childhood. Parents living either within 400 metres or greater than 1500 m of a major road were invited to a screening visit at one of the clinical study sites. At that initial visit, parents received informed consent, were administered medical and environmental questionnaire, and received skin prick testing to a panel of 15 aeroallergens and two food allergens (egg white, milk). Infants were eligible for participation if one or both parents reported rhinitis, eczema or asthma and exhibited a positive skin prick test (SPT) to at least 1 aeroallergen. The study protocol and informed consent statement were approved by the University of Cincinnati Institutional Review Board. Children enrolled in CCAAPS received annual evaluations at ages 1, 2, 3 and 4 years and follow-up at 7 years.
Clinical evaluation
Upper or lower respiratory infections.
Upper respiratory infection (URI) was defined as a positive parental response to the question ‘In the past 12 months, has your child had any of the following: ear infections, sinus infections and respiratory flu’. Lower respiratory infection (LRI) was defined as a positive parental response to the question ‘In the past 12 months, has your child had any of the following: croup, pneumonia, bronchitis and viral infection’ [18]. Both URI and LRI were captured by questionnaire items adapted from the validated International Study of Asthma and Allergies in Childhood (ISAAC) questionnaire [19].
Asthma evaluation at the age of seven.
Asthma symptoms were defined as at least one of the following: (1) a tight or clogged chest or throat in the past 12 months, (2) difficulty in breathing or wheezing after exercise, (3) wheezing or whistling in the chest in the previous 12 months or (4) a previous physician diagnosis of asthma. All children in the study underwent baseline spirometry performed by trained technicians using methods recommended by American Thoracic Society [20]. Those children underwent evaluation for reversibility in FEV1 and methacholine testing (if reversibility was not demonstrated) with one of the following features: (1) there was a parental report of asthma symptoms in the previous 12 months, (2) predicted FEV1 of less than 90% and (3) exhaled nitric oxide level of 20 ppb or greater. Airway reversibility was assessed 15 min after administration of 2.5 mg of nebulized levalbuterol.
Children with less than 12% increase in FEV1 after administration of bronchodilator were tested for bronchial hyperresponsiveness by methacholine challenge testing (MCCT) at a follow-up clinic visit. A modified 4-dose ATS methacholine challenge protocol was used with sequential methacholine concentrations of 0.0625, 0.25, 1 and 4 mg/mL [21]. A positive MCCT result was defined as a 20% or greater decrease in FEV1 after saline diluent challenge in response to 4 mg/mL or less of methacholine.
Children were defined as having asthma if the parent reported asthma symptoms (as previously defined) and the child demonstrated either significant airway reversibility (≥12% increase in FEV1) or a positive MCCT result.
Environmental exposures
Indoor exposures.
Parents were administered a questionnaire gathering information on parental and child health in the previous year and environmental exposures. Environmental tobacco smoke (ETS) was categorically defined as parental report of at least one current smoker residing in the household. House dust samples were collected from a 2 m2 area of floor surface from the infant’s primary living area [22]. Endotoxin concentrations were determined by the limulus amebocyte lysate test (Associates of Cape Cod Inc, Falmouth, MA, USA) in all house dust samples according to methods described by Milton and colleagues [23].
Day care exposure.
History of locations where the child spent 8 or more hours per week (e.g. home, day care, relative’s home) from birth through the age of seven was collected. Information on hours/week that the children that attended a day care was obtained at each clinical visit by asking parents ‘Please list the places where your baby spends his or her time. You should include all babysitters, day care providers or relatives if your baby spends more than 8 hours per week at an address different from his/her home’. Calculation of day care attendance variable did not include day care outside of a ‘day care center’. This ‘day care center’ definition excluded childcare provided at homes of family members, friends or baby sitters. The sizes of day care centres were not accessible.
Outdoor exposure.
Detail of elemental carbon attributable to traffic (ECAT) measurement and home dust mite sample collection has been described previously [24, 25]. Briefly, particulate matter less than 2.5 mm in diameter (PM2.5) was collected at ambient monitoring stations. Elemental carbon concentrations and absorption coefficients were determined [26]. Multivariable UNMIX and chemical mass balance models were then used to determine ECAT at monitoring stations [26]. A land-use regression model was applied to estimate ECAT for locations where a child spent greater than 8 hours per week between ages 6 and 12 months. ECAT exposure was treated as a continuous variable.
Statistical analysis
Univariate analyses were conducted to assess the associations between asthma at the age of seven and day care attendance, and URI, LRI and potential covariates at the age of 12 months included the following: sex, race (African American and non-African American ethnicity), education status (≥high school vs college); parental history of asthma; duration of breastfeeding (<4 and ≥4 months), number of other children living in the home (<2 and ≥2 siblings), presence of 1 or more dogs in the home (yes/no), presence of 1 or more cats in the home (yes/no), ETS exposure (yes/no) and ECAT exposure (≤75% and >75%) with asthma at the age of seven. These predictor variables were analysed as categorical variables and evaluated for association with asthma at the age of seven using the Pearson χ2 test.
The relation between asthma at the age of seven and continuously measured day care (DC) hours was investigated at each age. First, exploratory generalized additive modeling (GAM) was performed assuming a logistic model, in which asthma (the outcome) was modeled as a cubic spline function of continuous DC hours [27, 28]. The significance levels of the linear and nonlinear components of age-specific models were obtained. The overall predictive ability of the models across ages was compared by the deviance statistic. Only for DC hours at 12 months were the linear and nonlinear components of the spline curve significant at the 5% level in the GAM models. The graph at 12 months showed that the slope of the DC curve was approximately linearly increasing up to 1800 hours and then clearly decreased after 1800 hours of cumulative day care center exposure. Data at 12 months were then parameterically modeled as a two-component linear spline function using standard logistic regression. Parameters were estimated on the intervals from 0 to 1800 and >1800. All potential covariates listed in Table 1 were included in an initial multivariate logistic regression model. Variables in the final multiple regression model were chosen by backward stepwise regression and included if the P value was less than 0.05. Odds ratio (OR) and 95% confidence interval (CI) were computed for the final model.
Table 1.
Asthma odds ratio and 95% confidence limits of primary independent variables at the age of 12 months and other covariates. Cell entries are number, % of column total
| Asthma at the age of 7 |
||||
|---|---|---|---|---|
| Primary independent variables | Total N = 589 |
Yes N = 95 |
No N = 494 |
OR (95% CI) |
| Day care attendance (Yes) | 102 (17) | 24 (25) | 78 (16) | 1.8 (1.1–3.0) |
| URI (Yes) | 333 (60) | 68 (76) | 265 (57) | 2.4 (1.4–4.1) |
| LRI (Yes) | 186 (34) | 45 (51) | 141 (31) | 2.3 (1.5–3.7) |
| Other covariates | ||||
| Female | 266 (45) | 37 (39) | 229 (46) | 0.7 (0.5–1.2) |
| Race (African American) | 131 (22) | 35 (37) | 96 (19) | 2.4 (1.5–3.9) |
| Parental asthma (Yes) | 240 (41) | 54 (57) | 186 (38) | 2.2 (1.4–3.4) |
| Breastfeeding ≥ 4 mos | 312 (53) | 37 (39) | 275 (56) | 0.5 (0.3–0.8) |
| Mother education ≤ high school | 147 (25) | 41 (43) | 106 (21) | 2.7 (1.7–4.3) |
| At least one sibling | 381 (66) | 57 (61) | 324 (67) | 0.8 (0.5–1.2) |
| Dog in home | 208 (35) | 25 (26) | 183 (37) | 0.6 (0.4–1.0) |
| Cat in home | 132 (22) | 14 (15) | 118 (24) | 0.5 (0.3–1.0) |
| ECAT>75th %tile | 166 (28) | 33 (35) | 133 (27) | 1.4 (0.9–2.3) |
| Endotoxin>75th %tile | 134 (23) | 26 (27) | 108 (22) | 1.4 (0.8–2.3) |
| ETS | 112 (21) | 24 (25) | 88 (18) | 1.6 (0.9–2.7) |
We also analysed the association between the total number of hours of day care attendance and the total number of respiratory infections using Spearman’s correlation coefficient. Statistical analyses were performed using SAS version 9.3 (SAS Institute, Inc., Cary, NC, USA).
Results
Demographics and exposure characters
A total of 762 children at the age of 12 months were enrolled in this cohort. Of these, 589 children completed both a medical examination and a questionnaire at the age of seven. Asthma was identified in 95 (16%) children according to the aforementioned asthma case definitions. Of these 589 children, 323 were male (55%) and 266 female (45%). Among the 589 subjects, 125 (21%) were African-American, and 464 (79%) were non-African-American.
Univariate analysis of year one predictors of asthma at the age of seven
Univariate analyses of independent variables are presented in Table 1. Children who started attending day care before 12 months had a significant increased risk for asthma at the age of seven compared with children who did not attend day care. Infants who experienced any upper or lower respiratory tract infections during the first year had a significantly greater likelihood of asthma. Race (African American), parental history of asthma (yes) and lower level of education (i.e. high school graduate or less) were also significantly associated with asthma. Breastfeeding duration greater than 4 months was significantly associated with a reduced likelihood of asthma, suggesting a protective effect. Potential covariates that were not predictive of asthma in the univariate analyses included gender, the presence of siblings, cat or dog in the home, indoor exposure to environmental tobacco, high endotoxin level and high ECAT exposure.
Reported respiratory infections and asthma at age 7
Table 2 shows analyses evaluating respiratory infections at different ages and likelihood of asthma at the age of seven. In this study, the number of children who experienced a URI was 333 (60%) at 12 months, 288 (54%) at 24 months, 261 (50%) at 36 months and 216 (39%) 48 months. In the first 2 years of life, the frequency of children with any report of a URI was positively and significantly associated with asthma at the age of seven. The latter association was not significant after 24 months. The highest frequency of any reported LRI was in the first 12 months (34%) compared with 24, 36 and 48 months (22–24%). At the age of 12 and 36 months, LRI was significantly associated with asthma at the age of seven. No significant associations were detected between total day care hours and number of respiratory infections at any age (data not shown).
Table 2.
Unadjusted OR and 95% CI measuring associations between asthma at the age of seven and infections (Yes/No) for 589 subjects
| Age (Month) | URI (Yes) N (% of total) |
Asthma Number of subjects (% URI) |
OR (95% CI) | |
| Yes | No | |||
| (A) Upper respiratory infections (URI) | ||||
| 12 | 333 (60%) | 68 (76%) | 265 (57%) | 2.4 (1.4–4.1) |
| 24 | 288 (54%) | 56 (66%) | 232 (50%) | 1.8 (1.1–3.0) |
| 36 | 261 (50%) | 50 (59%) | 211 (48%) | 1.5 (0.9–2.5) |
| 48 | 216 (39%) | 37 (42%) | 179 (38%) | 1.2 (0.7–1.8) |
| Age (Month) | LRI (Yes) N (% of total) |
Asthma Number of subjects (% LRI) |
OR (95% CI) | |
| Yes | No | |||
| (B) Lower respiratory infections (LRI) | ||||
| 12 | 186 (34%) | 45 (51%) | 141 (31%) | 2.3 (1.5–3.7) |
| 24 | 120 (22%) | 22 (26%) | 98 (22%) | 1.2 (0.7–2.1) |
| 36 | 126 (24%) | 33 (39%) | 93 (21%) | 2.4 (1.4–3.9) |
| 48 | 126 (23%) | 23 (26%) | 103 (22%) | 1.2 (0.7–2.1) |
Upper respiratory infection defined as ear infection, sinus infection, and respiratory flu. Lower respiratory conditions defined as croup, bronchitis, pneumonia, and viral infection.
Day care attendance
The association between asthma and day care attendance at different ages is presented in Table 3. Of the 589 children, day care attendance was reported in 52 (9%) at 6 months, 102 (17%) subjects at 12 months, 128 (22%) subjects at 24 months, 143 (24%) at 36 months and 138(23%) at 48 months. Analysis of the ages of day care attendance revealed that children entering day care before 6 or 12 months had a significantly greater likelihood of developing asthma at the age of seven [OR (95% CI), 3.1 (1.7–5.8), 1.8 (1.1–3.0), respectively]. Although, this trend continued with increasing age, there was no significant association between day care attendance at 24, 36 and 48 months and asthma at the age of seven.
Table 3.
Unadjusted OR and 95% CI measuring associations between asthma at the age of seven and day care attendance (Yes/No)
| Age (month) | Day care attendance N (% of 589) |
Asthma Number of subjects (% daycare) |
OR (95% CI) | |
|---|---|---|---|---|
| Yes (N = 95) | No (N = 494) | |||
| 6 | 52 (9%) | 18 (19%) | 34 (7%) | 3.1 (1.7–5.8) |
| 12 | 102 (17%) | 24 (25%) | 78 (16%) | 1.8 (1.1–3.0) |
| 24 | 128 (22%) | 24 (25%) | 104 (21%) | 1.3 (0.7–2.1) |
| 36 | 143 (24%) | 27 (28%) | 116 (23%) | 1.3 (0.8–2.1) |
| 48 | 138 (23%) | 23 (24%) | 115 (23%) | 1.0 (0.6–1.7) |
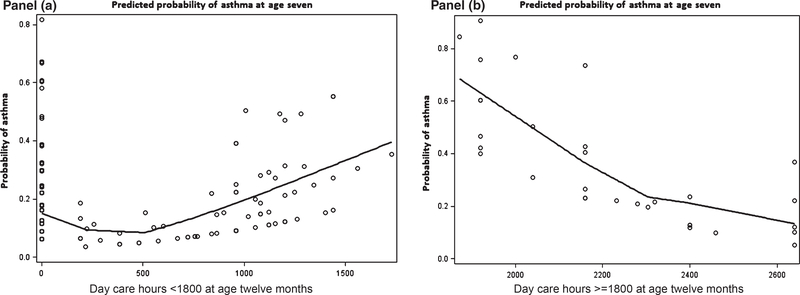
A linear spline model not adjusted for covariates was used to visualize the relationship between day care hours and asthma at the age of seven. Day care hour attendance ranged from 192 hours to 2640 hours at the age of 12 months. As shown in Fig. 1, during the first 12 months of life, total duration of day care attendance increased the probability of asthma at the age of seven if total cumulative day care hours were below 1800 hours (Panel a). Interestingly, the likelihood of asthma decreased when day care attendance exceeded 1800 total hours (Panel b). Of 102 children attending day care, cumulative duration less than 1800 hours was found in 68 (67%) children. Based on this observation, 2 day care continuous variables (i.e. <1800 and ≥1800 hours) were included in the final multivariate model.
Fig. 1.
Linear spline models (unadjusted) on two-interval day care hours (<1800, ≥1800) of age 12 months and asthma prediction at the age of seven.
Multivariate model of predictors of asthma at the age of seven
The final multivariate logistic regression analysis (Table 4) included the following predictor variables: parental asthma, lower maternal education, total number of LRIs at 12 months and total number of day care hours at 12 months. After adjusting for the aforementioned environmental exposures and host characteristics, significant predictors of asthma at 7 years of age in the final model included parental asthma, low maternal education, number of lower respiratory infections and total hours of day care attendance by the age of 12 months. Consistent with the spline curve, cumulative duration of day care attendance of less than 1800 hours was associated with asthma at the age of seven [OR, 1.2 (1.1–1.5), P < 0.01], whereas day care duration exceeding 1800 hours was associated with a reduced likelihood of asthma at the age of seven [OR, 0.6 (0.4–0.9), P < 0.05]. The number of LRIs (but not URIs) remained significantly associated with asthma in the multivariate model.
Table 4.
Adjusted OR and 95% CI measuring the effects of day care attendance and LRI, at 12 months on asthma at age 7
| Primary variables and covariates | OR (95% CI) |
|---|---|
| Parental asthma (Yes) | 2.0 (1.1–3.6) |
| Mother education (≤high school) | 3.4 (2.1–6.0) |
| LRI (+1) | 1.4 (1.2–1.8) |
| Day care hours | |
| <1800 hours (+100) | 1.2 (1.1–1.5) |
| ≥1800 hours (+100) | 0.6 (0.4–0.9) |
OR are expressed as a + 1 unit increase in LRI and +100 hours increase in day care attendance.
Discussion
This study demonstrated significant associations between early day care attendance during infancy and development of childhood asthma confirmed at the age of seven. Both age of day care attendance and cumulative duration of day care exposure were significant determinants of asthma risk at the age of seven. Interestingly, we found a bidirectional relationship between early day care attendance during infancy and likelihood of asthma. In other words, day care attendance during the first year was significantly associated with an increased likelihood of asthma at the age of seven if cumulative day care attendance was less than 1800 hours reported in 67% of infants attending day care, and conversely, duration of day care attendance exceeding 1800 hours was associated with reduced risk of asthma. To our knowledge, this is the first study to show that day care attendance can increase or decrease the likelihood of childhood asthma depending on the total duration of attendance during the first year of life.
Previous studies examining possible associations between day care attendance and asthma are conflicting. There are four published cross-sectional studies that reporting that day care attendance increases the risk of asthma at ages ranging from 6 to 14 years [11, 12, 14, 29]. Conversely, two population-based birth cohort studies suggested that day care attendance in the first year of life was associated with reduced likelihood of development of asthma at ages ranging from 5 to 11 years [7, 30]. Two other population-based cohort studies showed no association between day care attendance before 12 months and asthma at the age of eight or 11 [31, 32]. It is noteworthy that another birth cohort study of children selected on the basis of parental atopy (comparable to this study) found that day care attendance in early life was associated with a decreased risk of asthma at the age of six [33], but only among children without a maternal history of asthma. No association between day care attendance and the development of asthma at the age of six was reported in another high-risk asthma cohort [34]. These aforementioned studies, however, are difficult to compare with our study because day care attendance was not quantified and asthma outcomes were not objectively defined.
In this study, our asthma definition required objective confirmation with demonstration of ≥12% bronchodilator reversibility in FEV1 or a positive methacholine challenge test (PC20 ≤ 4 mg/mL) as defined by ATS guidelines [21], whereas the aforementioned studies defined asthma exclusively based on parental reporting. Moreover, we ascertained the duration of day care attendance, which has not been performed in previous studies. Our finding of a relationship between cumulative duration of day care attendance and development of asthma is novel. If confirmed, this finding could guide future recommendations to parents regarding the risks and/or benefits of day care attendance in the first year of life.
The mechanisms to explain why duration of day care attendance less than l hours increased the risk for asthma and why day care attendance greater than 1800 hours could reduce the likelihood of asthma are not clear. It is noteworthy that the association between day care attendance and asthma persisted in the multivariate model along with other significant covariates including parental asthma, maternal education and LRIs. We found no associations between multiple siblings, pet ownership, endotoxin level at home and the development of asthma at the age of seven. Thus, the exposure-dependent effect of day care attendance cannot otherwise be explained by other early environmental exposures, which have been previously associated with decreased risk of childhood asthma [7, 35, 36]. Lu et al. [37] reported that day care attendance is associated with increased incidence of gastrointestinal infections. However, in the largest birth cohort study to date investigating the gut microbiome during infancy, Bisgaard et al. [38] found that reduced microbiota diversity was not associated with asthma at the age of six; the effect of day care attendance was not examined. Therefore, future large prospective studies investigating the impact of the day care attendance on the gut and respiratory microbiome and subsequent risk of childhood asthma are warranted.
Our results also indicated that the number of LRIs at 12 months was positively associated with the development of asthma at the age of seven. This is in line with several studies that reported lower respiratory infections increase the risk of asthma at ages ranging from 6 to 10 years [32, 33, 39]. Although our study did not collect airway specimens, we suspect that most episodes of LRIs during infancy were likely associated with respiratory syncytial viral or rhinovirus [40]. Lower respiratory infections caused by human rhinovirus during infancy have been recognized to be a strong predictor of school-age asthma [34, 41].
Our findings in the multivariate model demonstrate strong and significant relationships between childhood asthma, parental history of asthma and lower maternal education and are similar to previous studies indicating that infants of parents with asthma or lower education were more likely to develop asthma later in life [42, 43].
Several limitations need to be considered in this study. First, the data regarding day care attendance were obtained retrospectively, but at each annual clinical exam. Secondly, we were not able to obtain information on the size of each day care center. Thirdly, we assessed the presence of respiratory infections in early life based on parental reporting, which is subject to recall bias. In some cases, this may have led to some misclassification, but this type of misclassification is most likely non-differential, which can make associations weaker but not change their direction [44]. Finally, the children enrolled in the CCAAPS cohort are high-risk children (i.e. born to at least one atopic parent), and these results may not be generalizable to children born to non-atopic parents.
In conclusion, our study is the first to report that both the timing and duration of day care attendance in a high-risk cohort might influence the risk of asthma. Cumulative hours of day care attendance in the first year of life less than 1800 hours were found to increase the risk of asthma in the majority of children. In contrast, cumulative hours of day care attendance in the first year of life exceeding 1800 hours reduced the likelihood of asthma at the age of seven. Lower respiratory infections in the first year of life, parental history of asthma and lower maternal education were also identified as risk factors for the development of childhood asthma.
Footnotes
Conflict of Interests
The authors declare no conflict of interest.
References
- 1.Eder W, Ege MJ, von Mutius E. The asthma epidemic. New Engl J Med 2006; 355:2226–35. [DOI] [PubMed] [Google Scholar]
- 2.von Mutius E. Environmental factors influencing the development and progression of pediatric asthma. J Allergy Clin Immunol 2002; 109: S525–32. [DOI] [PubMed] [Google Scholar]
- 3.Schaub B, Lauener R, von Mutius E. The many faces of the hygiene hypothesis. J Allergy Clin Immunol 2006; 117:969–77; quiz 78. [DOI] [PubMed] [Google Scholar]
- 4.Strachan DP. Hay fever, hygiene, and household size. BMJ 1989; 299:1259–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.von Mutius E. Infection: friend or foe in the development of atopy and asthma? The epidemiological evidence. Eur Respir J 2001; 18:872–81. [DOI] [PubMed] [Google Scholar]
- 6.von Mutius E, Radon K. Living on a farm: impact on asthma induction and clinical course. Immunol Allergy Clin North Am 2008; 28:631–47, ix-x. [DOI] [PubMed] [Google Scholar]
- 7.Ball TM, Castro-Rodriguez JA, Griffith KA, Holberg CJ, Martinez FD, Wright AL. Siblings, day-care attendance, and the risk of asthma and wheezing during childhood. New Engl J Med 2000; 343:538–43. [DOI] [PubMed] [Google Scholar]
- 8.Infante-Rivard C, Amre D, Gautrin D, Malo JL. Family size, day-care attendance, and breastfeeding in relation to the incidence of childhood asthma. Am J Epidemiol 2001; 153:653–8. [DOI] [PubMed] [Google Scholar]
- 9.Kramer U, Heinrich J, Wjst M, Wichmann HE. Age of entry to day nursery and allergy in later childhood. Lancet 1999; 353:450–4. [DOI] [PubMed] [Google Scholar]
- 10.Celedon JC, Litonjua AA, Ryan L, Weiss ST, Gold DR. Day care attendance, respiratory tract illnesses, wheezing, asthma, and total serum IgE level in early childhood. Arch Pediatr Adolesc Med 2002; 156:241–5. [DOI] [PubMed] [Google Scholar]
- 11.Sun Y, Sundell J. Early daycare attendance increase the risk for respiratory infections and asthma of children. J Asthma 2011; 48:790–6. [DOI] [PubMed] [Google Scholar]
- 12.Hagerhed-Engman L, Bornehag CG, Sundell J, Aberg N. Day-care attendance and increased risk for respiratory and allergic symptoms in preschool age. Allergy 2006; 61:447–53. [DOI] [PubMed] [Google Scholar]
- 13.Marbury MC, Maldonado G, Waller L. Lower respiratory illness, recurrent wheezing, and day care attendance. Am J Respir Crit Care Med 1997; 155:156–61. [DOI] [PubMed] [Google Scholar]
- 14.Nafstad P, Hagen JA, Oie L, Magnus P, Jaakkola JJ. Day care centers and respiratory health. Pediatrics 1999; 103:753–8. [DOI] [PubMed] [Google Scholar]
- 15.Jackson DJ, Johnston SL. The role of viruses in acute exacerbations of asthma. J Allergy Clin Immunol 2010; 125:1178–87; quiz 88–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ryan PH, LeMasters G, Biagini J et al. Is it traffic type, volume, or distance? Wheezing in infants living near truck and bus traffic. J Allergy Clin Immunol 2005; 116:279–84. [DOI] [PubMed] [Google Scholar]
- 17.LeMasters GK, Wilson K, Levin L et al. High prevalence of aeroallergen sensitization among infants of atopic parents. J Pediatr 2006; 149:505–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Biagini JM, LeMasters GK, Ryan PH et al. Environmental risk factors of rhinitis in early infancy. Pediatr Allergy Immunol 2006; 17:278–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asher MI, Keil U, Anderson HR et al. International Study of Asthma and Allergies in Childhood (ISAAC): rationale and methods. Eur Respir J 1995; 8:483–91. [DOI] [PubMed] [Google Scholar]
- 20.Miller MR, Crapo R, Hankinson J et al. General considerations for lung function testing. Eur Respir J 2005; 26:153–61. [DOI] [PubMed] [Google Scholar]
- 21.Crapo RO, Casaburi R, Coates AL et al. Guidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med 2000; 161:309–29. [DOI] [PubMed] [Google Scholar]
- 22.Campo P, Kalra HK, Levin L et al. Influence of dog ownership and high endotoxin on wheezing and atopy during infancy. J Allergy Clin Immunol 2006; 118:1271–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Milton DK, Johnson DK, Park JH. Environmental endotoxin measurement: interference and sources of variation in the Limulus assay of house dust. Am Ind Hyg Assoc J 1997; 58:861–7. [DOI] [PubMed] [Google Scholar]
- 24.Ryan PH, Bernstein DI, Lockey J et al. Exposure to traffic-related particles and endotoxin during infancy is associated with wheezing at age 3 years. Am J Respir Crit Care Med 2009; 180:1068–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ryan PH, Lemasters GK, Biswas P et al. A comparison of proximity and land use regression traffic exposure models and wheezing in infants. Environ Health Perspect 2007; 115:278–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hu S, McDonald R, Martuzevicius D et al. UNMIX modeling of ambient PM (2.5) near an interstate highway in Cincinnati, OH, USA. Atmos Environ 2006; 40:378–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hastie T, Tibshirani R. Generalized additive models. 1st edn. London; New York: Chapman and Hall, 1990. [Google Scholar]
- 28.Reponen T, Lockey J, Bernstein DI et al. Infant origins of childhood asthma associated with specific molds. J Allergy Clin Immunol 2012; 130:639–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Salam MT, Li YF, Langholz B, Gilliland FD, Children’s Health Study. Early-life environmental risk factors for asthma: findings from the Children’s Health Study. Environ Health Perspect 2004; 112:760–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nicolaou NC, Simpson A, Lowe LA, Murray CS, Woodcock A, Custovic A. Day-care attendance, position in sibship, and early childhood wheezing: a population-based birth cohort study. J Allergy Clin Immunol 2008; 122:500–6 e5. [DOI] [PubMed] [Google Scholar]
- 31.Caudri D, Wijga A, Scholtens S et al. Early daycare is associated with an increase in airway symptoms in early childhood but is no protection against asthma or atopy at 8 years. Am J Respir Crit Care Med 2009; 180:491–8. [DOI] [PubMed] [Google Scholar]
- 32.Nafstad P, Brunekreef B, Skrondal A, Nystad W. Early respiratory infections, asthma, and allergy: 10-year follow-up of the Oslo Birth Cohort. Pediatrics 2005; 116:e255–62. [DOI] [PubMed] [Google Scholar]
- 33.Celedon JC, Wright RJ, Litonjua AA et al. Day care attendance in early life, maternal history of asthma, and asthma at the age of 6 years. Am J Respir Crit Care Med 2003; 167:1239–43. [DOI] [PubMed] [Google Scholar]
- 34.Jackson DJ, Gangnon RE, Evans MD et al. Wheezing rhinovirus illnesses in early life predict asthma development in high-risk children. Am J Respir Crit Care Med 2008; 178:667–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Braun-Fahrlander C, Riedler J, Herz U et al. , Allergy, Endotoxin Study T. Environmental exposure to endotoxin and its relation to asthma in school-age children. New Engl J Med 2002; 347:869–77. [DOI] [PubMed] [Google Scholar]
- 36.Perzanowski MS, Ronmark E, Platts-Mills TA, Lundback B. Effect of cat and dog ownership on sensitization and development of asthma among preteenage children. Am J Respir Crit Care Med 2002; 166:696–702. [DOI] [PubMed] [Google Scholar]
- 37.Lu N, Samuels ME, Shi L, Baker SL, Glover SH, Sanders JM. Child day care risks of common infectious diseases revisited. Child Care Health Dev 2004; 30:361–8. [DOI] [PubMed] [Google Scholar]
- 38.Bisgaard H, Li N, Bonnelykke K et al. Reduced diversity of the intestinal microbiota during infancy is associated with increased risk of allergic disease at school age. J Allergy Clin Immunol 2011; 128:646–52 e1–5. [DOI] [PubMed] [Google Scholar]
- 39.Thomson JA, Widjaja C, Darmaputra AA et al. Early childhood infections and immunisation and the development of allergic disease in particular asthma in a high-risk cohort: a prospective study of allergy-prone children from birth to six years. Pediatr Allergy Immunol 2010; 21:1076–85. [DOI] [PubMed] [Google Scholar]
- 40.Darville T, Yamauchi T. Respiratory syncytial virus. Pediatr Rev 1998; 19:55–61. [DOI] [PubMed] [Google Scholar]
- 41.Guilbert TW, Singh AM, Danov Z et al. Decreased lung function after preschool wheezing rhinovirus illnesses in children at risk to develop asthma. J Allergy Clin Immunol 2011; 128:532–8 e1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Castro-Rodriguez JA. The Asthma Predictive Index: a very useful tool for predicting asthma in young children. J Allergy Clin Immunol 2010; 126:212–6. [DOI] [PubMed] [Google Scholar]
- 43.Ruijsbroek A, Wijga AH, Kerkhof M, Koppelman GH, Smit HA, Droomers M. The development of socio-economic health differences in childhood: results of the Dutch longitudinal PIAMA birth cohort. BMC Public Health 2011; 11:225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jurek AM, Greenland S, Maldonado G, Church TR. Proper interpretation of non-differential misclassification effects: expectations vs observations. Int J Epidemiol 2005; 34:680–7. [DOI] [PubMed] [Google Scholar]