Abstract
Objectives.
Mindfulness-based interventions (MBIs) have been widely implemented to improve self-regulation behaviors, often by targeting emotion-related constructs to facilitate change. Yet the degree to which MBIs engage specific measures of emotion-related constructs has not been systematically examined.
Methods.
Using advanced meta-analytic techniques, this review examines construct and measurement engagement in trials of adults that used standardized applications of the two most established MBIs: Mindfulness-Based Stress Reduction (MBSR) and Mindfulness-Based Cognitive Therapy (MBCT), or modified variations of these interventions that met defined criteria.
Results.
Seventy-two studies (N=7,378) were included (MBSR k=47, MBCT k = 21, Modified k=4). MBIs led to significant improvement in emotion-related processing overall, compared to inactive controls (d=0.58; k =36), and in all constructs assessed: depression (d=0.66; k=26), anxiety (d =0.63; k=19), combined mental health (d =0.75; k=7 ) and stress (d =0.44; k=11). Reactions to pain, mood states, emotion regulation, and biological measures lacked sufficient data for analysis. MBIs did not outperform active controls in any analyses. Measurement tool and population-type did not moderate results, but MBI-type did, in that MBCT showed stronger effects than MBSR, although these effects were driven by a small number of studies.
Conclusions.
This review is the first to examine the full scope of emotion-related measures relevant to self-regulation, to determine which measures are most influenced by MBCT/MBSR. Compared to extant reviews, which typically focused on MBI outcomes, this work examined mechanistic processes based on measurement domains and tools. While effect sizes were similar among measurement tools, this review also includes a descriptive evaluation of measures and points of caution, providing guidance to MBI researchers and clinicians for selection of emotion-related measurement tools.
Keywords: mindfulness, affect regulation, emotion, measurement tools
Unhealthy behaviors, such as smoking, overeating, and sedentary lifestyle are prevalent (Hughes et al., 2019) and are major contributors to cardiovascular disease, cancer, and other chronic conditions. Indeed, nearly half of all premature deaths in the U.S. can be attributed to health behaviors and are therefore preventable (Johnson et al., 2014). Despite this knowledge, health behavior change has proven difficult to accomplish and sustain, leading to a re-thinking of behavior change research. The U.S. National Institutes of Health (NIH) Science of Behavior Change (SOBC) initiative calls for applying an experimental medicine, mechanism-focused approach to the field. The overarching aims of this initiative are to identify targets that are mechanisms of change, to identify the most reliable measurement tools, and to identify or create behavioral interventions that can reliably and maximally engage these targets, thereby supporting self-regulation (Nielsen et al., 2018). Self-regulation refers to the process of adaptively managing cognitive, emotional, and self-relevant resources to align mental states and behavior with goals (Magai et al., 2007; Ward et al., 2014; Wing et al., 2008). Changing health behaviors requires self-regulation skills and the ability to effectively cope or manage emotional processes that might be salient to self-regulation behaviors.
Emotion regulation is an individual’s capacity to alter the magnitude and/or duration of an emotional response to stimuli or the presence of emotional states (Gross, 2014; Ochsner & Gross, 2005). Poor emotion regulation impairs the capacity for self-regulation to support health behaviors (DeSteno et al., 2013; Ferrer et al., 2015; Kangas & Gross, 2017; O’Leary et al., 2018) such as those related to diet, exercise, smoking, and medical regimen adherence (Evers et al., 2018). For example, enhanced emotional abilities to cope with stressful situations may increase one’s ability to sustain healthy dietary behaviors under stressful conditions (Smyth & Arigo, 2009). Conversely, psychological distress has been associated with maladaptive health behaviors such as non-adherence to smoking cessation (Cosci et al., 2011) and reduced commitment to sustaining weight loss (Ingels & Zizzi, 2018). In sum, improved emotion regulation has the potential to facilitate self-management of behavior and improve health outcomes. Yet, the mechanisms of self-regulation are still not well understood (Nielsen et al., 2018) and the field is lacking critical data on the interventions that might reliably engage emotion regulation targets as a means to improving self-regulation.
Mindfulness-based interventions (MBIs) may be well-suited to strengthen several aspects of self-regulation, including adaptive forms of emotional expression and regulation (Hölzel et al., 2011; Loucks et al., 2015). There is evidence that MBIs promote health behavior changes, including those related to substance use, smoking, obesity and weight loss (Gawande et al., 2019; Li et al., 2017; Maglione et al., 2017; Rogers et al., 2017; Ruffault et al., 2017). Mindfulness, defined as a non-elaborative state of awareness that arises from attending nonjudgmentally to present moment experience (Kabat-Zinn et al., 2003), may be further operationally defined to include the self-regulation of attention through sustained awareness of mental experience using an accepting, non-evaluative orientation (Hölzel et al., 2011; Vago & Silbersweig, 2012). MBIs have been shown to engage emotion-regulatory psychological processes and neural circuitry, including modulation of amygdala activation (Desbordes et al., 2012; Hölzel et al., 2013; Taren et al., 2015; Taylor et al., 2011), as well as sympathetic nervous system and hypothalamic-adrenal arousal (Carlson et al., 2007; Davidson et al., 2003; Hoge et al., 2018; Ortner et al., 2007; Tang et al., 2007), MBIs have also been shown to change how people respond to stressful situations or negative emotional cues (Brewer et al., 2009; Britton et al., 2010; Britton et al., 2012; Erisman & Roemer, 2010; Garland et al., 2014; Goldin & Gross, 2010; Kuehner et al., 2009).
Despite accumulating evidence that MBIs enhance self-regulation (Gawande et al., 2019; Ostafin et al., 2015; Vohs & Baumeister, 2016), the mechanisms by which this happens is not well understood, and improved understanding will allow us to better target them (Gu et al., 2015; Van Dam et al., 2018). A plethora of MBIs are being developed without systematically building on discoveries of which components of the interventions have the most impact on specific health behaviors and outcomes (Dimidjian & Segal, 2015). Therefore, MBI research would benefit from the experimental medicine, mechanism-focused approach advocated by the SOBC initiative (Nielsen et al., 2018).
The two most established and widespread MBIs are Mindfulness-Based Stress Reduction (MBSR; (Kabat-Zinn, 1982, 2013)) and Mindfulness-Based Cognitive Therapy (MBCT; (Segal et al., 2013; Teasdale et al., 2002)). MBSR, the first mindfulness-based intervention originally designed for chronic medical problems such as pain and stress reduction, is typically comprised of 8 weeks of 2.5-hour sessions with an accompanying allday (~7 hour) retreat later in the course. Subsequent modifications have been made in an effort to better address and accommodate the needs of specific populations. MBCT was adapted from MBSR to target depressive relapse and risk factors for recurrence by integrating elements of cognitive therapy. MBSR and MBCT in particular have been subjected to a large number of methodologically rigorous studies in relation to several conditions related to emotion dysregulation, such as depression, anxiety, and the stress response, as mentioned above. The common elements of these multi-component interventions are formal and informal meditation training, guided practices, investigative inquiry, social support, and didactic components (Crane et al., 2017).
While the clinical efficacy of both MBSR and MBCT for improving emotional symptoms is generally supported in the literature, less is known about their active ingredients or mechanisms of action (Gu et al., 2015). Two different types of self-regulation skills are supported in MBSR and MBCT: (a) cognitive self-regulation, especially the regulation of attention; and, (b) emotion regulation, such as secondary emotional reactivity toward internal and external events (Bishop et al., 2004; Rapgay & Bystrisky, 2009). While both attention and emotion regulation are thought to be key mechanisms of mindfulness, the extent to which these constructs have been measured, and the specific measures used to detect their engagement, have not been subjected to systematic review or meta-analysis (Hennessy et al., 2020).
The present study is part of the NIH Science of Behavior Change initiative to examine the ways in which MBIs impact self-regulation in order to improve health-related outcomes. Following recent proposals on the mechanisms of mindfulness by our group (Hölzel et al., 2011; Loucks et al., 2015) and others (Gallego et al., 2014; Henderson et al., 2012; Jensen et al., 2012; Koszycki et al., 2007; Polusny et al., 2015) the present review is one of a series that will systematically evaluate evidence for the engagement of mechanistic targets by MBIs in three broad self-regulation domains: cognitive processes, emotion regulation, and self-related processes. Of note, in this present review of emotional factors, we will consider anxiety and depression as mechanistic emotion-related constructs, rather than as clinical outcomes. This is based on the rationale that changes in anxiety and depression facilitate changes in selfregulation behaviors. The present work includes a systematic review and a meta-analysis on studies that provided enough information to calculate an effect size. Our primary aims were to determine: (a) the constructs and measures that are most and least represented in the MBSR/MBCT literature; and, (b) which constructs and measures are most engaged by MB SR and MBCT.
METHODS
Established methodologies outlined by the Cochrane Handbook of Systematic Reviews (Higgins et al., 2019) and the Agency for Healthcare Research and Quality’s Methods Guide for Comparative Effectiveness Reviews (AHRQ, 2014) were used to conduct this review. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were followed for the reporting of this systematic review (Liberati et al., 2009; Moher et al., 2010).
Protocol and Registration
On December 9, 2016, a PROSPERO review registration for the protocol for this systematic review was submitted. The review documents were reviewed and confirmation received on the 16th (PROSPERO 2016:CRD42016051765). The posted protocol is available online from www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016051765.
Eligibility Criteria
Titles and abstracts were double-screened by reviewers using the Abstrackr software (Wallace et al., 2012). Included studies were required to have a sample size of at least 10 participants in the mindfulness intervention arm, participants all ≥18 years old, and an outcome or instrument measuring an emotion-related process. Clinical and healthy adult populations, meeting the aforementioned criteria, were included. Only randomized controlled trials with one or more control condition (i.e., active, passive, etc.) were included since this study design is considered to be the gold standard. Active controls could be a range of interventions, including nutrition education, psychoeducation, traditional CBT, and community or online support groups. Passive controls were those in which participants were on a waitlist or treatment-as-usual regimen.
We will use the terms “MBI” and “MBSR/MBCT” interchangeably when discussing included studies. To be considered a standardized intervention of MBSR or MBCT, the intervention content must have been delivered in person, in a group setting, over eight weeks, consistent with the original protocols developed by Teasdale and colleagues (2002) and Rabat-Zinn (1982). The interventions are comprised of weekly classes that are 2.5 hours and with an accompanying all-day (~7 hour) retreat, following the respective manuals for the interventions (Santorelli et al., 2017; Segal et al., 2013). Individual format interventions were excluded because the group process (discussion, inquiry, and dyads) takes up a large proportion of the class content.
In addition to including standardized MBSR and MBCT, we also included modified variations of these interventions that met the following criteria: (a) total class time/session exposure, including retreat, was at least 75% of what is typically prescribed in MBSR or MBCT weekly sessions (i.e., 75% of 20 contact hours=15 hours); (b) full- or half-day retreat; (c) group-based format; and, (d) sample-specific “tailoring” or exercises or psychoeducation that were specific to the targeted condition (e.g., smoking cessation), as long as at least 50% of the original MBSR or MBCT content was included. In the original protocols, a retreat was included as a period of continuous practice intended to strengthen mindfulness skills. A recent meta-analysis (Visted et al., 2015) found significantly larger self-reported mindfulness effect sizes between MBIs that included retreats than in those that excluded them.
Emotion-related processes and emotional states in the included studies were assessed by self-report questionnaires, clinician-administered interviews, or physiological measures of sympathetic hyperarousal and responses to stressful situations or stimuli. Studies with outcomes such as relapse rates and hazard ratios were not applicable to the present research questions. State or trait mindfulness was not included. Although these factors are relevant to emotional processing, we chose to focus on emotional-related constructs. In addition, the content validity of these scales has been questioned (Garland & Gaylord, 2009; Grossman & Van Dam, 2011; Rapgay & Bystrisky, 2009; Visted et al., 2015). For example, although a recent meta-analysis found that from pre- to post-intervention, self-reported mindfulness moderately increased, between group differences in studies with active controls were not significant (Visted et al., 2015).
Information Sources and Search
This systematic review utilized the following four electronic databases: CINAHL, ERIC, PsycINFO, and PubMed (see Appendix for full search terms). To capture the foundational MBI studies, studies published through July 31, 2016, were included with no constraint on the starting date of publications. The AND operator was used to connect terms designed to find mindfulness studies to terms that relate to the domains of self-regulation. The Medical Subject Heading (MeSH) terms of Mindfulness and Meditation were used in addition to the terms related to emotion regulation. Terms were truncated with an asterisk (*) to capture all possible endings for the designated root of the specified word. Filters were used to restrict the retrieved citations to English-only, human-only, and adult-only (age over 18 years old) publications.
We supplemented our review with grey literature searches. Using our already-identified search terms, we searched the Open Grey (http://www.opengrey.eu/) and New York Academy of Medicine Grey Literature Report (http://www.greylit.org/) electronic databases. This search identified six potentially relevant studies. The investigative team identified 10 professional organizations relevant to MBCT and/or MBSR research. As such, the websites of these organizations were searched for non-published reports and where applicable the past 12-month (January 2016 - January 2017) conference proceedings were reviewed. This search identified 29 potentially relevant studies. Conference proceedings authors were contacted to inquire about study details, status, and data availability. Past 12-month monthly reports from the American Mindfulness Research Association (AMRA) were also reviewed, identifying 66 journal articles and 16 ongoing NIH-funded studies. Additional resources searched included: ClincalTrials.gov (17 studies identified); PubMed Similar Articles (22 studies identified); and ISI Web of Science references from reference lists and cited references searches (51 studies identified). Throughout the grey literature process, we compared identified studies with those found during our initial electronic searches and de-duplicated records when appropriate. A senior member of the investigative team examined these results (207 studies total) and assessed their relevance to the present review. Results from 14 studies were not available as data collection was ongoing at the time of this review. Otherwise, studies were excluded because they did not meet inclusion criteria or were not published before August 2016.
Measure Selection and Construct Formation
The included measures were selected through a collaborative and iterative process among the doctoral-level authors involved in this project, all of whom are experts in mindfulness-related research. These investigators initially proposed measurement tools and construct terms using their content expertise, then discussed the options and voted among the suggested terms in order to create the final list of terms for each domain of the broader project. The emotion-related process search terms were designed to capture the following domain terms decided upon through deliberation among the co-investigators: emotional/stress reactivity, affect/affect regulation/affectivity, anger, anxiety, avoidance, compassion, coping, decentering, depression, distress tolerance, emotion/emotion identification/emotion regulation, empathy, equanimity, experiential avoidance, exposure, expression, fear/fear extinction, habituation, intention, mood, neuroticism, non-attachment, non-judgment, nonreactivity, pain, positive psychology, reconsolidation, resilience, reperceiving, suppression, and amygdala activity. Upon completion of the search and the data returned, the following terms were retained and rearranged into meaningful constructs for reporting in the present study by the investigative team: (a) anxiety; (b) depression; (c) emotion regulation; (d) mood states (emotion states other than anxiety or depression); (e) comprehensive mental health (measures that assess multiple mental health categories); (f) peripheral biology; (g) reactions to pain/illness; and, (h) stress, coping, and burnout. Full instruments (measures) were inspected in order to categorize the measures in the most meaningful constructs in consideration of the psychometric validation of the instrument.
Data Extraction
Studies meeting all above criteria were extracted, and data were entered and saved in custom-designed forms on the Systematic Review Data Repository (SRDR) online system (http://srdr.ahrq.gov). Before full text articles were extracted, the 17-member review team completed a training using the SRDR. Senior investigators closely supervised the review team through the training and extraction process. To maximize reliability, extraction instructions for each data field of the SRDR form was created and reviewed at weekly meetings. Each study was entered in SRDR by one member of the review team and was assessed for completion and errors by a second Master’s-level reviewer. In assessing inter-rater reliability, 13 pairs of extractors-reviewers were created so that all reviewers were able to edit each extractors’ data entry, including ratings of risk of bias. Mean extractor-reviewer concordance was 94.3% (range=86.4% – 100%) and extractor-reviewer pairs showed high agreement (kappa range=.851 – .990, depending on coding pair).
Data extraction of study level characteristics included demographics, population type, study location, intervention and control group details, and timepoints of data collection. Outcome level details included results for all emotion-related measures. Results from individual studies from intent-to-treat analyses were prioritized in capturing the data; when a study provided both intent-to-treat and completer analyses, the results from the intent-to-treat analysis was extracted.
Assessment of Risk of Bias in Individual Studies
The methodological quality of each study was assessed by reviewers based on predefined criteria using the Cochrane Risk of Bias Tool (Higgins et al., 2019). This tool asks about risk of selection bias, performance bias, detection bias, attrition bias, reporting bias, and other potential biases. Ratings of high-risk or low-risk were assessed for each potential bias; where no information was provided in the study to accurately assess the risk of bias, the recorded response was no data. Risk of bias was assessed independently by study raters and then checked by more senior study staff. Discrepancies were resolved through consultation with the leadership of the investigative team.
Data Synthesis and Analysis
The focus of this review is on group x time effects. Each unique comparison of change over time for the MBI and control condition is reported as a separate contrast. Control groups were coded as inactive or active. Population was coded as non-clinical and clinical, and further coded within each as follows: non-clinical included general and stressed (e.g., caregivers); clinical included depression, anxiety, medical diagnosis, and other/multiple clinical diagnosis. Outcomes were coded according to the eight emotion-related constructs, outlined in the section above. Measures were coded according to measurement scale or type; different versions of similar questionnaires were coded separately (e.g., BDI-I vs. BDI-II), while questionnaires that only differed between full and shortened versions were coded the same (e.g., GAD-2 and GAD-7 were coded as GAD). Non-questionnaire-based assays were collapsed into single measures (e.g., Cortisol slope and Cortisol awakening were coded as Cortisol).
Effect size calculations.
Between-groups effect sizes (d) were standardized mean differences using the post-test means of the two groups (treatment and control) and subtracting the baseline difference between the two groups; d was then corrected for small sample size bias (i.e., Hedges’ d or g). Effect sizes for all outcomes were calculated when studies provided enough information and were coded so that positive ds represent improved outcomes (e.g., improved mood, reduced anxiety) in the treatment group relative to the control group. When studies provided appropriate statistics, follow-up ds were calculated relative to baseline.
Analytic strategies.
We combined effect sizes across studies to provide overall estimates and their 95% confidence intervals (CI) using meta-analysis with robust variance estimation (RVE); this strategy allows for all possible contrasts to be included in the analysis, including follow-up data. RVE controls for the dependence of effect sizes from the same study due to multiple simultaneous measures (Hedges et al., 2010). It was implemented through the robumeta macro in Stata (versionl5; StataCorp (Tanner-Smith & Tipton, 2014)). RVE was performed separately for active and inactive controls, for all outcomes. As a degree of freedom of 4 or more is required for RVE, the following subgroups were also analyzed as data permitted: by construct, by MBI type, and by construct and MBI type together. Rho was set to 0.8 for the correlated effects weight, and sensitivity analyses varied rho from 0-1 to ensure consistent results. Moderator analysis was performed on control group type, and then again within each control type, on measure, MBI type and study population. Heterogeneity for each model is reported using Tau2, which represents between-study variance. Exploratory RVE sub-analyses were performed to investigate interactions of potential moderators.
Inspecting for publication bias across studies, funnel plots and Egger’s tests (Egger et al., 1997) were used to assess the possibility of bias stemming from underrepresentation of small sample size studies with null or negative findings (Johnson & Hennessy, 2019). However, since funnel plots and Egger’s tests include all contrasts without controlling for dependencies of effect sizes as done in RVE, we also include a univariate RVE moderator analysis using standard error as the predictor, to determine if studies with higher standard errors (e.g., smaller studies) routinely have effect sizes that differ in magnitude from studies with greater theoretical precision. All analyses were performed separately by control group type. Lastly, a descriptive analysis of measures was conducted to provide MBI researchers and clinicians with guidance for measurement tool selection. Measures used within the eight emotion-related constructs were summarized and qualitatively discussed.
RESULTS
Study Selection
The initial search returned 8,312 citations identified through searching PubMed and 4,772 citations were returned through searching Cinahl, APA PsycINFO, and ERIC (Figure 1). After deduplication, the number of unique citations identified was 10,802. All 10,802 citations were screened using Abstrackr in order to exclude irrelevant studies based on title and abstracts alone. Using Abstrackr, 8,989 studies were excluded, including 14 studies identified in the grey literature search that did not have available results. This left 1,813 citations for full-text retrieval and full-text screening. Upon assessing the full-text, 1,702 studies were excluded. One hundred eleven studies were identified as being relevant for at least one of the three concurrent systematic reviews. For the presented review, 72 studies were extracted (MBSR k=47, MBCT k=21, Other/Modified k=4), with 7,378 participants reported an outcome in the emotion regulation domain and were included here for qualitative synthesis. Of these having sufficient data, qualitative analysis was performed on 52 studies with a total of 371 effect size estimates.
Figure 1.

PRISMA, flowchart of emotion-related processes systematic review and meta-analysis.
Study and Sample Characteristics
Table 1 provides a summary of the demographic, clinical, and intervention characteristics from the included studies. All included trials were published after the year 2000, ranging from 2005 to 2016. The majority were performed in the United States or Europe (50% and 30.5% respectively). Individual study level details are presented in Supplemental Table 1. The average total sample size was 98 participants per study, with 18341 participants in total, and 10-168 individuals in the MBI arms. For the studies that reported demographic features, the majority of participants were white (90.1%), female (71.6%), and middle-aged (mean age=46.7, SD=9.36).
Table 1.
Demographics of Study Sample and Intervention Characteristics.
| Factor | % or Mean (SD/range) |
|---|---|
| Average sample size | 98.4 (18 to 341) |
| Average age of participants | 46.7 yrs (9.36) |
| % White | 90.1% |
| % Female | 71.6% |
| Location (% of studies) | |
| US | 50% |
| Europe | 30.5% |
| Other | 19.5% |
| Population Diagnosis (% of studies) | |
| Depression | 20.8% |
| Anxiety | 11.1% |
| Stressed (no screening, but expected to be stressed, e.g., caregivers) | 5.6% |
| Medical (e.g., cancer, diabetes) | 37.5% |
| General (no screening) | 18.1% |
| Clinical (other/mixture of psychiatric diagnoses) | 6.9% |
| Type of intervention (% of studies) | |
| MBSR | 65.2% |
| MBCT | 29.1% |
| Modified | 5.5% |
| Includes follow-up data collection | |
| % of studies with short term follow-up (<6 months) | 58.3%; 12.9 wks |
| % of studies with long term follow-up (>=6 months) | 41.6%; 45.5 wks |
| Type of control group (% of studies) | |
| Active | 29.2% |
| Waitlist | 41.7% |
| Treatment as Usual | 25.0% |
| Active and inactive controls | 4.2% |
MBSR outnumbered MBCT by more than 2:1 in the studies meeting our inclusion criteria (Figure 2). Forty-seven studies used MBSR (65.3%), 21 studies used MBCT (29.1%), and 4 studies used modified versions of MBSR/MBCT (5.6%). Regardless of MBI type, most studies used inactive controls; less than one third of all studies (29.2%) used an active control group. Active controls included cognitive behavioral therapy, exercise programs, education and support groups (e.g., Health Enhancement Program), and pharmacotherapy. Most study designs used a waitlist control (41.7%) or treatment as usual (25%) for comparison groups. A small number of studies used both active and inactive control groups (4.2%). Thirty-two percent of studies collected post-intervention data within 10 weeks from baseline, with no additional follow-up data collection. Fifty-eight percent of the studies included additional data collection at a short-term follow-up time (less than 6 months from baseline; mean: 13 weeks), and 42% of the studies included a longer-term follow-up (6 months or greater from baseline; mean: 45.5 weeks). The longest follow-up period was two years (see Supplemental Table 1).
Figure 2.
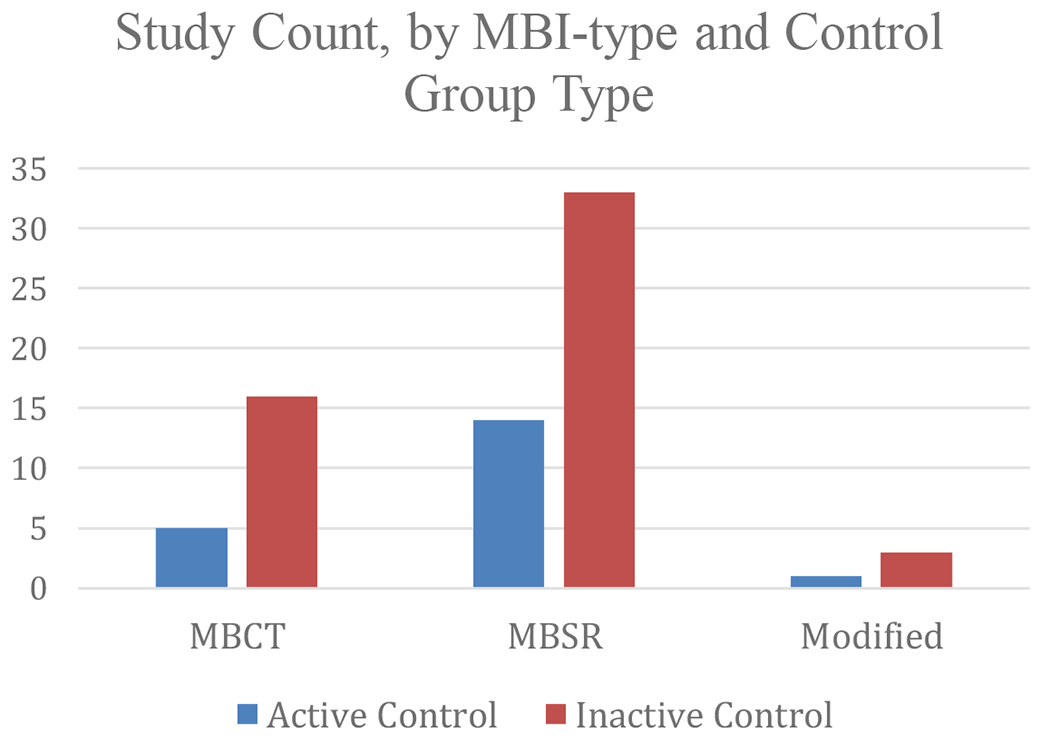
Study count, by mindfulness-based intervention type and control group type.
Clinical samples were most commonly studied (Figure 3; k=55; 76%), but study populations differed by MBI (Supplemental Table 1). Across both types, non-psychiatric medical diagnoses (k=27; 37.5%), depression (k=15, 20.8%), or anxiety (k=8, 11.1%) were the most common clinical groups. Non-clinical samples included general population (18%; k=13) and stressed but otherwise healthy (5.6%, k=4). All but two of the 19 MBCT studies used clinical populations, which were primarily depressed subjects (63%). Thirty-four of the 48 MBSR studies were in clinical populations (70.8%). Depression measures predominated in MBCT studies versus all other constructs more commonly used in MBSR studies. The stress, coping, and burnout construct was only utilized in one study of MBCT, and MBCT studies were notably devoid of biological assays or measures of emotion regulation or reactions to pain/illness.
Figure 3.
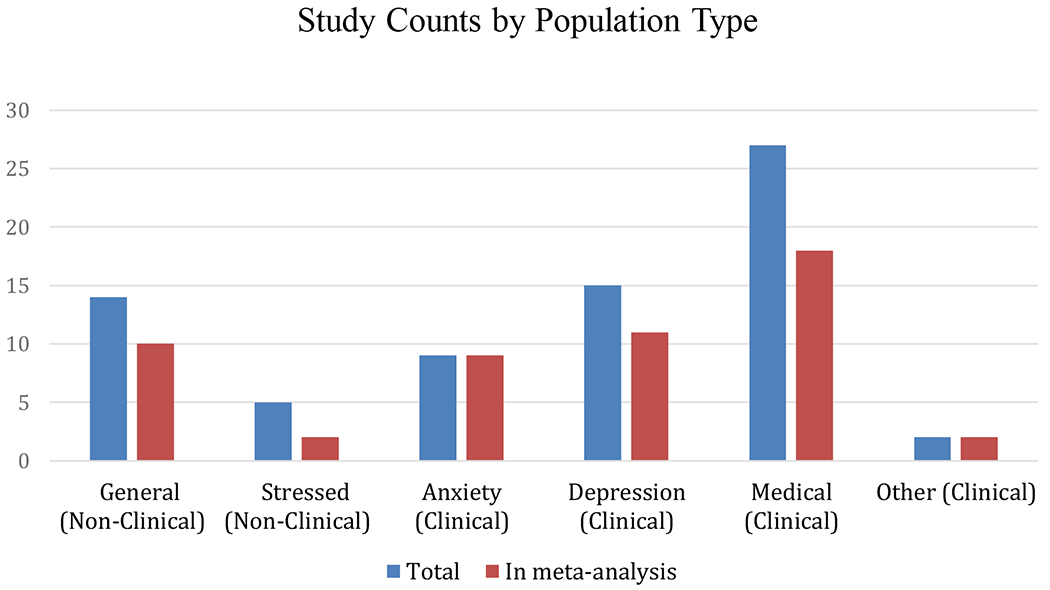
Study count, by study population type.
Risk of Bias
Risk of bias across studies is presented in Figure 4. Blinding of patients, assessors, and group allocation were the primary risk of bias concerns. A majority described an adequate method of randomization generation, such as through computer programs. For the studies that did not describe their randomization methodology, it was generally stated that participants were randomized with no further information.
Figure 4.

Risk of Bias of included studies.
Allocation was properly concealed in a majority of studies. However, participants were blinded to group allocation in very few studies. Forty-five (60%) of the studies reported that they were unable to properly blind participants due to the nature of MBIs and the controls used. Blinding of outcome assessors was adequately described in a majority of the studies.
Fourteen (19%) of the included studies had attrition bias or incomplete outcome data due to the amount, nature, or handling of incomplete data. Nine studies (12%) displayed evidence of selective outcome reporting bias; the remaining 66 studies did not. Forty-six (61%) of the included studies used intention-to-treat analysis.
Potential Reporting Bias and Non-reporting
Funnel plot and Egger’s test for studies with inactive controls showed potential for publication bias, favoring studies with positive outcomes (Supplemental Figure 1). In contrast, this trend was not significant for studies with active controls (Supplemental Figure 2). Using moderator analysis of standard error to look for small study bias led to similar findings: smaller studies with inactive controls showed a non-significant trend for larger effects (Table 3), a trend that was not apparent in studies with active controls. Between-group comparative data were not reported in 11.9% of all contrasts. Thus, effect sizes could not be calculated in these instances. Non-reporting was nearly twice as likely to occur in trials with active controls.
Table 3.
Moderator analysis for mindfulness-based interventions on emotion-related processing.
| Effect Modifier | K (N ds) | b | 95% CI | df | p-value | Tau2 |
|---|---|---|---|---|---|---|
| Control Group type | 52 (371) | −0.54 | (−0.76, −0.31) | 35 | <.0001 | 0.20 |
| MBI vs Inactive Control | ||||||
| Measure | 36 (229) | 0.004 | (−0.01, 0.01) | 24 | 0.6387 | 0.23 |
| MBI Type | 36 (229) | −0.44 | (−0.82, −0.06) | 15 | 0.0249 | 0.23 |
| Population | 36 (229) | 0.02 | (−0.07, 0.11) | 12 | 0.6654 | 0.23 |
| Standard Error (publication bias) | 36 (229) | 2.35 | (−0.13, 4.83) | 17 | 0.0618 | 0.19 |
| MBI vs Active Control | ||||||
| Measure | 20 (142) | 0.00 | (−0.42, 0.64) | 15 | 0.4776 | 0.26 |
| MBI Type | 20 (142) | 0.10 | (−0.42, 0.64) | 9 | 0.6486 | 0.26 |
| Population | 20 (142) | −0.01 | (−0.14, 0.13) | 10 | 0.9180 | 0.26 |
| Standard Error (publication bias) | 20 (142) | −0.56 | (−3.02, 1.90) | 8 | 0.6130 | 0.21 |
Note. Effects in boldface reach statistical significance. CI, Confidence interval; b, beta coefficient, ; df, degrees of freedom; k, Number of studies; RVE, Robust variance estimation;
Robust Variance Estimator (RVE) and Moderator Analysis
RVE analysis (Table 2) shows MBIs led to significant improvement in emotion-related processing overall, compared to inactive controls (d=0.58; k= 36), but not compared to active controls (d=0.05; k=20). Within the emotion-related constructs that had sufficient data to perform RVE, MBIs outperformed inactive controls for depression (d=0.66; k=26), anxiety (d=0.63; k=19), combined mental health (d=0.75; k=7 ) and stress (d=0.44; k=11). MBIs did not outperform active controls in any emotion-related categories (depression d=0.16, k=17; anxiety d=0.03, k=14; combined mental health d=0.11, k=7). The following emotion-related categories did not have sufficient data for RVE: peripheral biology, reactions to pain/illness, emotion regulation, and mood states.
Table 2.
Estimated Pooled Effects, Using Robust Variance Estimation, of Mindfulness-based Interventions on Emotion-Related Outcomes.
| RVE Results | k (N ds) | ES (d) | 95% CI | df | p-value | Tau2 |
|---|---|---|---|---|---|---|
| MBI vs Inactive Control | ||||||
| All outcomes | 36 (229) | 0.58 | (0.41, 0.75) | 34 | <.0001 | 0.23 |
| By Construct | ||||||
| Depression | 26 (63) | 0.66 | (0.43, 0.89) | 24 | <.0001 | 0.27 |
| Anxiety | 19 (51) | 0.63 | (0.33, 0.92) | 17 | 0.0003 | 0.23 |
| Stress | 11 (27) | 0.44 | (0.20, 0.68) | 9 | 0.0023 | 0.09 |
| Mood | 11 (47) | 0.28 | (0.15, 0.41) | 9 | 0.0009 | 0.05 |
| Combined Mental Health | 7 (14) | 0.75 | (0.12, 1.38) | 6 | 0.0278 | 0.36 |
| By MBI Type | ||||||
| MBCT | 12 (61) | 0.85 | (0.50, 1.20) | 11 | 0.0003 | 0.25 |
| MBSR | 23 (163) | 0.47 | (0.29, 0.66) | 22 | <.0001 | 0.24 |
| By Construct & MBI type | ||||||
| Anxiety | ||||||
| MBCT | 6 (14) | 1.06 | (0.12, 2.01) | 5 | 0.0300 | 0.52 |
| MBSR | 13 (37) | 0.43 | (0.18, 0.69) | 11 | 0.0030 | 0.11 |
| Depression | ||||||
| MBCT | 11 (29) | 0.72 | (0.38, 1.06) | 10 | 0.0009 | 0.17 |
| MBSR | 15 (34) | 0.62 | (0.29, 0.95) | 14 | 0.0012 | 0.34 |
| MBI vs Active Control | ||||||
| All outcomes | 20 (142) | 0.05 | (−0.10, 0.20) | 19 | 0.4900 | 0.2 |
| By Construct | ||||||
| Depression | 17 (53) | 0.16 | (−0.10, 0.41) | 16 | 0.2045 | 0.28 |
| Anxiety | 14 (50) | 0.03 | (−0.12, 0.18) | 12 | 0.7040 | 0.05 |
| Combined Mental Health | 7 (19) | 0.11 | (−0.37, 0.59) | 6 | 0.6025 | 0.18 |
Note. Effects in boldface reach statistical significance. CI, Confidence interval; d, Effect size (standardized mean difference, where positive values imply improvement); df, degrees of freedom; k, Number of studies; RVE, Robust variance estimation.
The following factors were assessed in moderator analysis: control group type, MBI type, population, and measure (Table 3). Control group type was a significant moderator across studies (p<0.001); therefore, all subsequent analyses were conducted separately for active vs. inactive control groups. MBI type was a significant moderator for studies with inactive controls (p<0.02); subgroup analysis (Table 2) explored this finding further by showing MBCT (d=0.85) outperformed MBSR (d=0.47). Additional subgroup analysis showed this performance difference was most apparent in the anxiety construct (d=1.06 for MBCT; d=0.43 for MBSR); however, it is important to note that MBCT was only used in 6 studies with anxiety measures, with high between-study variance (Tau2=0.52). For depression, results for the two MBI types were similar, with MBCT (d=0.72) showing only a slightly higher effect size than MBSR (d=0.62), in studies with inactive controls.
Population-type and measure were not significant moderators. Population-type was tested both as a dichotomized variable (e.g., clinical, non-clinical; b=−0.03, p= 0.92) and as a continuous variable (e.g., depression, anxiety, etc.; b=0.02, p= 0.67). To look at the moderating effect of population in interaction with MBI type, we performed an exploratory RVE sub-analysis (Table 4). In studies comparing MBIs to inactive controls, 70% of MBSR studies used clinical populations, with medium effect size (d=0.54; k=16); 83% of MBCT studies used clinical populations, also with medium effect size (d =0.66; k =10). The 30% of MBSR studies that used non-clinical populations showed small effects (d =0.31; k =7). There were only two MBCT studies that used non-clinical populations; affects appeared high (d =1.91; k =2), but should be interpreted with caution due to the low sample size. For studies comparing MBIs to active controls, data was lacking to test significant effects for all MBI-type and population combinations except MBSR studies with clinical samples, which had no effect (d=0.06; k =11). To determine if type of measurement tool impacted outcome within a specific construct, univariate moderator analysis was performed within each construct that contained sufficient data; measurement tool was not a significant moderator within any construct (Supplemental Table 2).
Table 4.
Exploratory sub-analysis to evaluate pooled effect estimates by control-type, MBI-type, and population-type (clinical versus non-clinical).
| RVE Exploratory Sub-Analysis | k (N ds) | ES (d) | 95% CI | df | p-value | Tau2 |
|---|---|---|---|---|---|---|
| MBI vs Inactive Control | ||||||
| MBSR | ||||||
| Clinical | 16 (119) | 0.54 | (0.27, 0.81) | 15 | 0.0007 | 0.27 |
| Non-clinical | 7 (44) | 0.31 | (0.13, 0.48) | 5 | 0.0060 | 0.04 |
| MBCT | ||||||
| Clinical | 10 (52) | 0.66 | (0.43, 0.90) | 8 | 0.0002 | 0.10 |
| Non-clinical | 2 (9) | 1.91 | (−1.73, 5.57) | 1 | * | 0.36 |
| MBI vs Active Control | ||||||
| MBSR | ||||||
| Clinical | 11 (87) | 0.06 | (−0.11, 0.24) | 10 | 0.4460 | 0.19 |
| Non-clinical | 3 (17) | 0.14 | (−0.93, 1.20) | 2 | * | 0.88 |
| MBCT | ||||||
| Clinical | 5 (36) | 0.00 | (−0.49, 0.50) | 4 | * | 0.38 |
| Non-clinical | 1 (2) | -- | -- | -- | -- | -- |
Note. Effects in boldface reach statistical significance.
df is less than 4, which makes p-value untrustworthy (Tanner-Smith and Tipton, 2014).
CI, Confidence interval; d, Effect size (standardized mean difference, where positive values imply improvement; df, degrees of freedom; k, Number of studies; RVE, Robust variance estimation;
Descriptive Analysis of Measurement Tools
Table 5 summarizes the usage frequency of various measurement tools for emotion-related processing, separated into eight emotion-related constructs, also separated by study design (active versus inactive control). Number of measurement tools used per construct varied as follows: anxiety=19, depression=17, mood states=8, comprehensive mental health=7, stress/coping/burnout=7, biological measures=6, emotion regulation=3, reactions to pain/illness=2 measurement tools. Figure 5 shows the number of studies assessing each construct, in total, and in the meta-analysis. To provide guidance on the use of measures within each of the eight emotion-related constructs, a summary of measurement usage in the included studies is provided, followed by a brief review of highlighted measures.
Table 5:
Measurement tools for emotion-related processing and frequency of use in mindfulness-based studies
| Assay/Measure | Inactive Control K | Active Control K | Total K | Assay/Measure | Inactive Control K | Active Control K | Total K |
|---|---|---|---|---|---|---|---|
| Emotion Regulation Measures | Depression | ||||||
| ACS | 1 | 0 | 1 | ATQ-N | 1 | 0 | 1 |
| CEC | 1 | 1 | 1 | BADS | 1 | 0 | 1 |
| DERS | 2 | 0 | 2 | BDI | 11 | 1 | 11 |
| Biological Measures | BDI-II | 6 | 8 | 14 | |||
| Breathing rate | 1 | 0 | 1 | BDI-18: Depression | 0 | 1 | 1 |
| Capsaicin induced flare size | 0 | 1 | 1 | BSS | 1 | 0 | 1 |
| Cortisol (salivary or serum; diurnal or provoked) | 3 | 4 | 6 | CES-D | 6 | 4 | 10 |
| Heart rate (resting, anticipation, response, recovery) | 2 | 0 | 2 | DASS | 1 | 0 | 1 |
| IL-8 | 0 | 1 | 1 | DASS-21: Depression | 1 | 0 | 1 |
| TNF-alpha | 0 | 1 | 1 | HADS-D | 1 | 0 | 1 |
| Anxiety | HAM-D | 7 | 4 | 11 | |||
| ASI | 1 | 0 | 1 | IDS | 1 | 0 | 1 |
| BAI | 4 | 5 | 8 | PGWBI: Depression | 0 | 1 | 1 |
| BSI | 0 | 1 | 1 | PHQ-9 | 5 | 2 | 6 |
| CAPS-5 | 1 | 0 | 1 | POMS: Depression | 1 | 1 | 2 |
| DASS-21: Anxiety | 1 | 0 | 1 | QIDS | 1 | 0 | 1 |
| GAD-2 MBSR-CBT | 1 | 2 | 2 | SCL-90R: Depression | 4 | 3 | 6 |
| HADS-A | 2 | 0 | 2 | Mood States | |||
| HAM-A | 1 | 1 | 2 | BRUMS: Anger | 1 | 0 | 1 |
| LSAS | 0 | 2 | 2 | ESM: Positive Affect | 1 | 0 | 1 |
| PCL-C | 1 | 0 | 1 | GDS: Relationship Distress | 1 | 0 | 1 |
| PGWBI: Anxiety | 0 | 1 | 1 | PANAS: Negative | 1 | 0 | 1 |
| PSWQ | 5 | 2 | 7 | PANAS: Positive | 5 | 0 | 5 |
| SCL-90R-anxiety | 3 | 3 | 6 | POMS | 2 | 1 | 3 |
| SIAS-S | 0 | 2 | 2 | STAXI-II | 1 | 0 | 1 |
| STAI - state anxiety1 | 7 | 4 | 11 | Reactions to Pain/Illness | |||
| STAI-trait anxiety | 4 | 0 | 4 | CPAQ | 2 | 0 | 2 |
| STICSA | 1 | 0 | 1 | CSQ: Catastrophic Think | 1 | 0 | 1 |
| VSI | 0 | 1 | 1 | Stress, Coping, and Burnout | |||
| Comprehensive Mental Health | C-SOSI | 0 | 1 | 1 | |||
| BSI | 1 | 0 | 1 | DASS-21: Stress | 1 | 0 | 1 |
| BSI-18: General Severity (psychological distress) | 1 | 1 | 2 | MBI | 3 | 0 | 3 |
| CGI | 0 | 2 | 2 | PSI | 1 | 1 | 2 |
| DASS-21 | 1 | 0 | 1 | PSQ-R | 1 | 0 | 1 |
| EPQR-S: Neuroticism | 1 | 0 | 1 | PSS | 10 | 4 | 13 |
| PGWBI: Global | 0 | 1 | 1 | Wheaton Chronic Stress Inventory | 1 | 0 | 1 |
| PWB | 1 | 0 | 1 | ||||
| SCL-90-R | 5 | 4 | 8 | ||||
Abbreviations: ACS = Attentional Control Scale; ASI = Anxiety Sensitivity Index; ATQ-N = Automatic Thoughts Questionnaire Negative; BADS = Behavioral Activation for Depression Scale; BAI = Beck Anxiety Inventory; BDI = Beck Depression Inventory; BDI-II = Beck Depression Inventory II; BDI-18 = Beck Depression Inventory 18-item; BRUMS = Brunel Mood Scale; BSI = Brief Symptom Inventory; BSI-18 Brief Symptom Inventory 18-item; BSS = Beck Scale for Suicide Ideation; CAPS-5 = Clinician-Administered PTSD Scale; CEC = Courtauld Emotional Control Scale; CES-D = Center for Epidemiologic Studies Depression Scale; CGI = Clinical Global Impression; CPAQ = Chronic Pain Acceptance Questionnaire; C-SOSI = Calgary Symptoms of Stress Inventory; CSQ = Coping Strategies Questionnaire; DASS-21 = Depression, Anxiety, and Stress Scale 21-item; DERS = Difficulties in Emotion Regulation Scale; EPQR-S = Eysenck Personality Questionnaire Revised Short; ESM = Experience Sampling Method; GAD-2 = Generalized Anxiety Disorder 2-item; GDS = Global Distress Scale; HADS-A = Hospital Anxiety and Depression Scale Anxiety; HADS-D = Hospital Anxiety and Depression Scale Depression; HAM-A = Hamilton Rating Scale Anxiety; HAM-D = Hamilton Rating Scale Depression; IDS = Inventory of Depressive Symptomatology; IL-8 = Interleukin-8; LSAS = Liebowitz Social Anxiety Scale; MBI = Maslach Burnout Inventory; PANAS = Positive and Negative Affect Scale; PCL-C = PTSD Checklist Civilian; PGWBI = Psychological General Well-Being Index; PHQ-9 = Patient Health Questionnaire 9-item; POMS = Profile of Mood States; PSI = Parenting Stress Index; PSQ-R = Perceived Stress Questionnaire Revised; PSS = Perceived Stress Scale; PSWQ = Penn State Worry Questionnaire; PWB = Psychological Wellbeing Scale; QIDS = Quick Inventory of Depressive Symptomatology; SCL-90-R = Symptom Checklist-90-Revised; SIAS-S = Social Interaction Anxiety Scale Straightforward; SPS = Social Phobia Scale; STAI = State-Trait Anxiety Scale; STAXI-II = State Trait Anger Expression Inventory II; STICSA = State-Trait Inventory for Cognitive and Somatic Anxiety; TNF-alpha = Tumour Necrosis Factor alpha; VSI = Visceral Sensitivity Index; Wheaton Chronic Stress Inventory.
Figure 5.
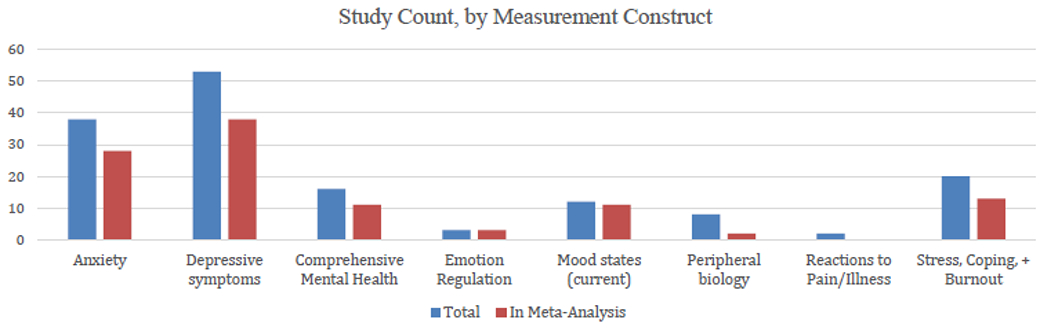
Study count, by measurement contruct.
Anxiety
Of the 19 tools used to measure anxiety, State-Trait Anxiety Scale (STAI) was used most frequently (k= 11), followed by the Beck Anxiety Inventory (BAI, k=8), and Penn State Worry Questionnaire (PSWQ, k=7). The STAI has been shown to have internal consistency and discriminant validity (Barnes et al., 2002) and has been translated into at least 48 languages (Julian, 2011). STAI-State (“STAI-Y1”) is the “state” half of the STAI, and is comprised of 20 statements about current anxiety symptoms. Interestingly, given that an emotional ‘state’ changes over time, the STAI-State can be used to measure reactions to laboratory stress provocation. Two of the included studies reported STAI scores during the Trier Social Stress Test (Kirschbaum et al., 1993), a task in which the participant has to give an impromptu speech in front of an audience; in both cases, participants in the MBI arm had a greater drop in STAI-state than the control group (Britton et al., 2012; Hoge et al., 2013). The BAI is a self-report scale in which the subject is asked to rate how much s/he is bothered by list of anxiety symptoms in the last week (such as “unable to relax” or “fear of the worst happening”) (Beck et al., 1988), and the PSWQ (Meyer et al., 1990) was developed for use in populations with generalized anxiety disorder, and includes questions about the excessiveness or intensity of worry and the tendency for the worrying to be generalized.
In selecting an anxiety measure for use in MBI studies, perhaps the most important determination is the study population: some instruments for anxiety symptoms were designed for and validated in populations with abnormal anxiety levels (i.e. patients with anxiety disorders). Using some measures in a general population (with presumably much lower levels of anxiety) may create a floor effect, in which changes over time cannot be detected because they are already so low. The BAI and PSWQ, for example, were both designed to be used in clinical populations.
Depression
The most common measures of depression were Beck Depression Inventory (BDI, k=11;BDI-II k=14), the Center for Epidemiologic Studies Depression Scale (CES-D, k=10), and Hamilton Rating Scale Depression (HAM-D, k=11). The BDI-I, introduced in 1961, assesses intensity of depression symptoms in the last week (Beck et al., 1961). The BDI-II published in 1996 was designed to have a better balance of symptoms: in the earlier BDI-I (consistent with Beck’s cognitive theory of depression) there was a strong emphasis on cognitive/affective items (18 out of 21) with only 3 assessing somatic-vegetative questions, whereas with the BDI-II, they are more balanced (10 and 11 items, respectively) which is thought to apply more closely to the depression criteria in the American Psychiatric Association’s Diagnostic and Statistical Manual of Mental Disorders (Dozois et al., 1998; Wang & Gorenstein, 2013). The HAM-D is a widely used clinician-rated scale done in a semi-structured interview format, in which a trained clinician assesses the severity of depression symptoms (Hamilton, 1960). Originally developed in 1960 for a hospitalized patient population, it has undergone several revisions and a considerable amount of psychometric study.
Similar to issues described above with anxiety symptoms, some depression scales were designed for a clinical population (such as people with current major depression) and may not be useful in mostly healthy populations such as college students where changes during an MBI may not be detectable. Another consideration is whether to use a self-report, survey-type questionnaire, or a measure meant to be used by a trained mental health clinician (“clinician-administered” scales). It is possible that clinician-rated instruments perform better (potentially less prone to bias) than self-report ones, as has been found in other trials of depression treatments (Cuijpers et al., 2010).
Emotion Regulation
Four studies assessed emotion regulation, using three different measures: The Difficulties in Emotion Regulation Scale (DERS) (Gratz & Roemer, 2004), the Affective Control Scale (ACS) (Berg et al., 1998), and the Courtauld Emotional Control Scale (CEC) (Watson & Greer, 1983). Each tool examines different aspects of the overarching construct of emotion regulation. The most commonly used measure was the DERS (60% of contrasts), which assesses dimensions of one’s self-reported ability to cope with negative emotions. Conversely, the ACS assesses fear of experiencing (particularly intense) positive and negative emotions, with no assessment of coping ability. The CEC is the only measurement tool in this review to assess engagement in specific strategies to cope with negative emotions. Specifically, the CEC is a self-reported assessment of suppressing the expression of anger, anxiety, and depressed mood.
Assessment of self-reported ability to cope with different consequences of negative emotion (as with the DERS) is important, given that poor or ineffective emotion regulation can deplete resources for self-regulation of health behaviors, or can lead to reliance on unhealthy, but hedonically rewarding, behaviors as an emotion regulatory strategy (DeSteno et al., 2013; Ferrer et al., 2015; Ferrer & Mendes, 2018; Kangas & Gross, 2017). Individuals differ in their ability to recognize and accurately understand their emotional experience (e.g., (Lievens & Chan, 2017; Wright et al., 2018)). Moreover, given that one goal of MBIs is to improve interoceptive awareness, it is possible that individuals in MBI conditions might be able to more accurately reflect on their emotions and related reactions, compared to control conditions (Gawande et al., 2019). Differences on these scales might reflect such increased awareness, as opposed to any actual differences in emotion regulatory ability. As such, it is important for future MBI studies to assess tendency to engage in particular regulatory strategies (such as expressive suppression, as assessed by the ACS) to obtain a more comprehensive picture of any differences.
It is noteworthy that none of the studies covered in this review used the most commonly employed measure of emotion regulation: the Emotion Regulation Questionnaire (ERQ; (Gross & John, 2003)). The ERQ assesses two emotion regulation strategies: suppression, which has been shown to be ineffective and can actually impede self-regulation and health behaviors (Ferrer et al., 2017; Hofmann et al., 2007); and cognitive reappraisal, which has been linked to better self-regulation of health behaviors (Evers et al., 2010; Taut et al., 2012). MBIs might facilitate greater capacity for and reliance on cognitive reappraisal, and less reliance on suppression, given their focus on nonjudgmental acceptance of negative states (Garland et al., 2011). Future MBI trials targeting self-regulation of health behaviors should consider including assessments of cognitive reappraisal and suppression (Gross & John, 2003).
Comprehensive Mental Health
Eight different measurement tools were used to assess comprehensive mental health, a broad construct covering a range of emotional and psychological experiences and symptoms. The Symptom Checklist-90-Revised (SCL-90-R; (Derogatis, 1994)) was most frequent, appearing in 8 studies, although it should be noted that some studies only reported SCL-90-R subscale results (e.g., anxiety and depression subscales; see anxiety and depression sections for discussion of those data). Additionally, Brief Symptom Inventory-18 (Derogatis, 2000) was used in some studies; the B SI-18 is a shortened version of the SCL-90-R. Other measures were the Clinical Global Impression - Severity (CGI-S; (Guy, 1976)), a single item; the Depression Anxiety Stress Scale (DASS; (Lovibond & Lovibond, 1995)); the Psychological General Well-Being Index (PGWI; (Dupuy, 1984)); the Psychological Well-Being Scale (PWBS; (Ryff, 1989)); and the Neuroticism subscale of the Eysenck Personality Questionnaire (Eysenck et al., 1985).
Comprehensive mental health measures might be most useful in studies of non-clinical populations. They provide overall “snapshots” of mental health and well-being, but arguably lack sensitivity to detect symptom- or diagnosis-specific changes that could result from intervention. The most commonly used tool, the SCL-90-R, is quite lengthy with 90 items. However, it does facilitate a broad assessment of nine domains, including anxiety, depression, and psychoticism, which might be useful in a heterogeneous sample.
Mood States and Emotion
Of the seven general measures of mood states and emotions, the Positive and Negative Affect Schedule (PANAS; (Watson et al., 1988)) was the most prevalent, followed by the Profile of Mood States (POMS; (McNair et al., 1971)). Other measures of mood included the Global Mood Scale (GMS; (Harper et al., 1998)); feelings of entrapment and escape motivation, measured by the Entrapment Scale (EE; (Gilbert & Allan, 1998)); and, pleasantness experienced in daily activities was measured using an experience sampling method (ESM); relationship distress was measured through a Global Distress Scale (GDS; (Snyder, 1997)). This category of measures has a variety of uses. For instance, the PANAS can be used to measure state or trait affect. Overall, these scales are likely to be more useful as secondary outcome or mediational measures, rather than primary outcome assessments.
Stress, Coping, and Burnout
Of the seven measures that were used to assess stress, coping, and burnout, the Perceived Stress Scale (PSS; (Cohen et al., 1983; Cohen & Williamson, 1988)) was used most (k=13). The PSS is the most widely used instrument for measuring subjects’ appraisal of how overwhelming they experience the stress in their lives to be as a function of available coping resources. Items are scored on a 5-point Likert scale.
Measures of perceived stress are designed to assess the degree to which events in one’s life are appraised as stressful, an approach based on the tradition of research on psychological stress that emphasizes one’s subjective evaluation of the imbalance between environmental demands and one’s ability to cope with these demands (Koolhaas et al., 2011; Lazarus & Folkman, 1984). Perceived stress has been associated with unhealthy behaviors (Ng & Jeffery, 2003; O’Connor et al., 2008), poor medical regimen adherence (Cosci et al., 2011; Elfhag & Rossner, 2005) including medication adherence (Tabibian et al., 2015), cardiovascular disease and mortality (Robinson et al., 2004; Stansfeld et al., 2002), and poor outcomes in studies of health behavior interventions (Evers et al., 2006; Mansyur et al., 2013). The most commonly used measure for this construct, the PSS, is also the most widely used instrument for assessing the relationship between stress and health. The original instrument was shortened after factor analysis indicated that 10 items comprised a single factor, although later factor analytic studies have found that both versions are comprised of two factors.
Interestingly, while most of the questions on the PSS ask the respondent about how they “felt” about stressors (e.g. “In the past week, how often have you felt nervous or stressed”), three of the items unique to the 14-item version ask how often the respondent “acted” in response to the stressors. Specifically, these three items ask: “how often have you dealt successfully with hassles,” “..found yourself thinking about things you had to accomplish,” and, “…have you been able to control your time”. Thus, the two versions differ in that PSS-10 primarily assesses emotional responses while the 14-item version also assesses respondents’ actions in response to the stressors. MBIs emphasize that acknowledging the presence of difficult emotions triggered by stress leads to a more adaptive response than trying to change or regulate emotions (Dahl et al., 2015; Kabat-Zinn, 2003; Teasdale et al., 2002). The PSS-14 may more effectively measure the impact of mindfulness on a key aspect of self-regulation, viz., the ability to respond more effectively to negative emotions related to stress, as opposed to experiencing less negative emotion. This is an important distinction, and therefore we recommend using the PSS-14 in future studies, as well as recommend the development of a new scale that specifically addresses responding to stress rather than feeling stress.
Another consideration for researchers is the overlap between what is measured by the PSS and emotion-related symptoms measured by other measures. Cohen pointed to this overlap in his original paper describing the PSS (Cohen et al., 1983), and he suggested that the perception of stress may be influenced by symptoms of depression. Subsequent research has confirmed overlap with both depression and anxiety symptomatology (Pariante, 2003; Suls & Bunde, 2005). Thus, for clinical populations in particular, intervention research that focuses on MBI’s impact on perceived stress as a purported mechanism of change should also include measures of depression and anxiety and examine the unique variance attributable to each.
Reaction to Pain/Illness
Two different questionnaires were used to assess reaction to pain or illness. Two studies used the Chronic Pain Acceptance Questionnaire (CPAQ; (McCracken et al., 2004)), while one study used the Coping Strategies Questionnaire (CSQ; (Rosenstiel & Keefe, 1983)). Like the PSS 14, the “engagement in activity despite pain” subscale of the CPAQ assess the respondent’s actions (e.g. “There are many activities I do when I feel pain”), rather than emotional responses to their pain. The CSQ includes a 6-item subscale tapping dimensions of helplessness and pessimism in the context of pain.
Pain acceptance has been defined as acknowledging that one has pain, giving up unproductive attempts to control pain, acting as if pain does not necessarily imply disability, and being able to commit one’s efforts toward living a satisfying life despite pain (Hayes et al., 2012; McCracken et al., 2004). Acceptance of chronic pain as measured by the CPAQ has been found to be inversely correlated with depression, physical and psychosocial disability, pain-related anxiety, and pain intensity, and also positively correlated with increased daily activity and improved work status (Deyo et al., 1993). Another study found that chronic pain patients who reported being able to live a satisfying life despite pain also reported greater confidence in their coping ability, less depression, and less pain behavior (Jacob et al., 1993). Typically, MBI studies with chronic pain patients find little or no change in the pain intensity, yet these programs are still considered valuable by patients, presumably due to the increase in pain acceptance which leads to decreases in disability and increases in the ability to engage in pleasurable activities that might have been avoided due to fear of pain. Notably, the original mindfulness program developed by Kabat-Zinn was designed specifically for chronic pain patients, with the goal of teaching them how to respond rather than react to pain (Kabat-Zinn, 2013). Pain is an inevitable and natural part of life. How one responds to pain is idiosyncratic, influenced by past experience, and can be modified. One important goal of MBIs is to recognize maladaptive habitual responses such as pain avoidance, evaluate the veracity and utility of such responses, and then modify them to be more adaptive.
Although not used in any included studies, a relevant measurement option would be to examine pain catastrophizing in future MBI trials. Pain catastrophizing refers to a set of exaggerated and ruminating negative cognitions and emotions during actual or perceived painful stimulation (Leung, 2012). The Pain Catastrophizing Scale (PCS; (Sullivan, 2009)) has become the “reference standard psychometric tool for pain catastrophizing” (Leung, 2012) with more than 5000 citations since publication in 1995. PCS scores correlate with other health measures, including pain intensity, pain-related disability, and psychological distress (Severeijns et al., 2001). In theory, pain catastrophizing would decrease with improved mindfulness skills.
Peripheral Biology
Six peripheral biological measures related to emotional factors were assessed across the included studies, the most common of which was cortisol (six studies). Some studies assessed cortisol at a single time point, while others used a slope or curve composed of several time points, which is more consistent with expert consensus guidelines for using cortisol to measure stress (Ryan et al., 2016; Stalder et al., 2016). Other biological measures included respiration and heart rate (e.g., resting, during a stress task), systemic inflammatory markers (e.g., IL-8, TNF-alpha), and local inflammatory response assessed by capsaicin induced flare size.
As mentioned above, single time point measures of cortisol (in saliva or blood) are extremely problematic and should be avoided given high variability owing to diurnal cycle, effects of food, exercise and smoking, ultradian rhythms, menstrual cycle, medication use, and transient infection. A much preferred method would be to use the cortisol awakening response (Fries et al., 2009), or even better, a laboratory stress that brings cortisol levels above daily cycling levels and is therefore more robust and consistent for measurement, such as the Trier Social Stress Test (Kirschbaum et al., 1993) or the Cold Pressor Task (Santa Ana et al., 2006).
Type of measure: self-report vs. objective
The vast majority of studies (85.7%) relied on subjective self-report measures and questionnaires, in contrast to objective measures including clinician-rated scales, and behavioral or peripheral biological assays. The few studies (5.6%) which used trained clinician-rated measures (HAMD, HAMA (which includes SIGH-A), CAPS, LSAS, and CGI), were done in populations with a psychiatric disorder.
DISCUSSION
This review is the first to examine the full scope of emotion-related measures relevant to self-regulation, to determine which measures are most influenced by MBCT/MBSR. The review includes 72 studies, with a total of 7,378 participants. Seventy-two separate measurement tools were used across eight different constructs of emotion regulation, most frequently anxiety and depression. The most commonly used measurement tools were STAI-State for anxiety, cortisol for peripheral biology, PSS for stress, SCL-90-R for comprehensive mental health, and Ham-D, BDI, and BDI-II for depression.
The risk of bias overall was low and was primarily driven by a lack of participant blinding and concealment information not being reported. However, nearly 12% of contrasts were not reported, suggesting that results not favoring MBCT/MBSR may be less likely to be reported. Furthermore, there were indications of publication bias in studies using inactive controls. Using advanced meta-analytic techniques that handle internally correlated effect estimates to allow inclusion of all contrasts, results showed that compared to inactive controls, MBIs showed similar, medium effects across multiple constructs: depression, anxiety, and combined mental health outcomes. Effects were small for stress and mood. More studies are required to evaluate the effects of MBIs on emotion regulation, reaction to pain/illness, and peripheral biology.
As expected, control group type largely influenced effect size estimates; MBIs did not show significant differences from active controls, in any analyses. Note that previous metaanalyses have also found that effect sizes for MBIs were significantly greater for anxiety and depression when compared to non-specific active control conditions (e.g. psychoeducational or support groups, relaxation training), but were not significantly different compared with evidence-based behavioral treatments (Goldberg et al., 2019; Khoury et al., 2013). Another large meta-analysis also found that effects of MBIs were significantly greater for anxiety and depression when compared with inactive controls, but not for active control conditions (Goyal et al., 2014). The failure to include active control conditions has been repeatedly emphasized as a significant weakness in mindfulness research (Baer, 2003; Bishop, 2002; Davidson & Kaszniak, 2015; Goldberg et al., 2017) and the need for such controls is obvious. Use of waitlist controls in particular has been discouraged, as both lack of patient blinding and increased rates of nocebo effects in waitlist conditions leads to “inflated effects sizes for the experimental treatment (p. 259),” (Holmes et al., 2018). Because 40% of the studies in this review used waitlist controls, it is likely that effect sizes from these studies may be an overestimate. In treatment development work, it is not uncommon to explore initial effects of a novel intervention as compared to usual care (i.e., “treatment-as-usual). This can be an important foundational step to determine if a novel intervention, like an MBI, might have an added benefit over and above existing treatment. However, as MBI research continues to progress, more comparisons with active controls will be beneficial. Moreover, intention-to-treat analyses and longer follow-up periods will increase the rigor of future MBI RCT research.
Measurement tool did not influence results overall, nor within any construct. This suggests that one measurement tool did not consistently outperform any other within each construct. It is important to note, however, that many measurement tools were only used in a single study and these studies were not designed to compare the different measurement tools. Additionally, population type did not influence results, whether dichotomized as clinical versus non-clinical, or separated into various population types. Results showed stronger effects for MBSR trials in clinical compared to non-clinical populations. For MBCT, the majority of studies were performed in clinical populations, precluding comparison of population type within MBCT.
MBI type was a significant moderator, in studies with inactive controls; MBCT showed large effects while MBSR had small effects overall. This difference was mainly driven by anxiety outcomes, whereas MBCT showed large effects but high between-study variance. For depression, both MBI types had medium effect sizes. Attempting to untangle the influence of MBI type and population, further exploratory analysis showed MBSR and MBCT both had medium effects in clinical populations, but MBCT had large effects in the two studies with non-clinical populations, whereas MBSR had small effects in non-clinical populations. Thus, while MBCT appeared to outperform MBSR in several sub-analyses, these effects were driven by a small number of studies and should be interpreted with caution.
It is possible that several places where MBSR and MBCT deviate may contribute to MBCT’s larger effect sizes on emotion-related constructs. MBCT requires higher levels of clinical training for teachers, and has a published session x session manual and adherence and fidelity guidelines. During the second half of the program, MBCT provides depression-specific psychoeducation, with class and homework practice in applying mindfulness skills to working with difficult emotions, while MBSR focuses on a range of topics, including stress, habits (diet, media) and interpersonal communication (Crane et al., 2013; Crane et al., 2012; Santorelli et al., 2017; Segal et al., 2002). Because MBCT had a higher percentage of clinical samples, it is possible that higher baseline severity could lead to larger effect sizes for MBCT. However, type of sample (clinical vs. nonclinical) was not a significant predictor of effect size. Thus, direct, head-to-head comparisons of MBSR and MBCT in the same study are needed to examine their relative effectiveness for engaging emotion-related constructs, especially for anxiety and depression.
Need for more objective measures
As outlined above, few studies in this literature include measures of emotional processes that do not rely on self-report. Subjective experience of emotion, as assessed by self-report measures of depression and anxiety, may be a consequential outcome itself influencing behavior change; more objective assessments can contribute greater precision towards identifying intervention targets and mechanisms of change. Given the relative lack of correspondence between self-reported emotions and physiological assessments (Cacioppo et al., 2000; Lindquist et al., 2012), including such assessments would provide information about mechanisms underlying behavior change above and beyond what could be provided by selfreport. Relatedly, because emotion categories assessed in self-reported scales may not correspond with physiological processes involved in affective states, self-reported assessments may not capture important mechanisms that contribute to self-regulation of health behaviors (Barrett, 2006a, 2006b). As such, future MBI trials should include physiological assessments such as facial activity, or behavioral manifestations of emotion (e.g., reactions to a stressor, reaction time, decision-making) and nervous system activity (Coan, 2010; Coan & Allen, 2007; Quigley et al., 2014), in addition to self-reports to improve detection of emotional differentiation (Barrett et al., 2001; Ottenstein & Lischetzke, In Press).
Limitations
Our goal was to strike a balance between inclusion of MBSR and MBCT trials which made slight modifications to the standard curriculum for specific populations, and maximizing generalizability to standard MBSR/MBCT interventions. The decision to not require strict adherence to the curriculum in terms of classroom and retreat time, and inclusion of nonstandard content, resulted from the finding that our initial search excluded many relevant studies. By expanding our inclusion criteria, we may have introduced more variability into our results. Nevertheless, a number of studies that may have produced relevant findings for MBI engagement of emotion-related constructs were excluded because they did not meet the inclusion criteria. By restricting the inclusion criteria to studies published in English, our review does not account for findings in non-English publications. Regarding racial diversity, the majority of participants in the studies were white (90.1%), which limits the generalizability of findings. In addition, methodological features of the interventions that may significantly impact outcomes, such as treatment fidelity, teacher training and effectiveness, and participant adherence, were beyond the scope of this review. These important considerations were the focus of a recent systematic review which found only modest evidence for improvement in the methodological rigor of MBI research in recent years (Goldberg et al., 2017).
The dataset used for this review includes studies published through 2016, which provide a foundational perspective, representing the first 10 years of MBI research. Initial MBSR/MBCT studies were more likely to be conducted by original developers or by teachers trained with the original methodology. Thus, while an update of this review will be warranted, the current review provides novel information about the engagement of emotion-related mechanisms, especially for depression and anxiety. Future reviews will hopefully shed more light on constructs that were under-represented in our review, particularly pain, peripheral biology, and emotion regulation.
One aim of this review was to use advanced analytic techniques to determine if certain measurement tools are more likely to be engaged than others in MBSR/MBCT interventions. While the results from our meta-analysis and moderator analysis suggest tool selection does not impact effect sizes, there were numerous measurement tools that were used in only one or two studies, thus limiting power and our ability to compare tools within emotion-related constructs. As more data accumulate, advanced synthesis techniques (e.g., network metaanalysis) may well reveal that certain tools provide more consistent engagement than others within specific emotion-related constructs. Nevertheless, the current review provides an important contribution to guide measurement tool selection for emotion-related constructs, by reviewing the most commonly used tools and highlighting important considerations, which has not been done before. By optimizing measurement selection to align with hypothesized engagement of targets, research and clinical care has the potential to become more precise and personalized.
Supplementary Material
Acknowledgements
We thank Blair T. Johnson and Emily A. Hennessy for their methodological advice. We also would like to thank Ana Alejandre-Lara for her work on the figures and manuscript preparation.
Funding
This work was supported by the National Institutes of Health (NIH) Science of Behavior Change Common Fund Program through an award administered by the National Center for Complementary and Integrative Health (grant UH2AT009145). W.B.B. received funding from NIH grant K23AT006328-01A1. The views presented here are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Conflict of interest
E.B.L. is Director of the Mindfulness Center at Brown Ciniversity. The Mindfulness Center, a non-profit entity, has an Education Unit that provides mindfulness-based program delivery to the general public for fees. However, E.B.L.’s salary is not tied to quantity or content of programs offered through the Mindfulness Center. W.B.B. is a MBSR and MBCT teacher and has received financial compensation for this role. W.B.B. receives payments for providing trainings and education in scientific literacy, meditation safety, and trauma-informed mindfulness. W.B.B. is nominally affiliated with the Mindfulness Center at Brown University which generates income by offering mindfulness classes to the public; W.B.B. does not receive any financial compensation from the Mindfulness Center. The other authors have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
*Denotes study included in the systematic review and meta-analyses.
- AHRQ. (2014). Methods guide for effectiveness and comparative effectiveness reviews. Agency for Healthcare Research and Quality. www.effectivehealthcare.ahrq.gov [PubMed] [Google Scholar]
- Baer RA (2003). Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology-Science and Practice, 10(2), 125–143. 10.1093/clipsy/bpg015 [DOI] [Google Scholar]
- Bames LLB, Harp D, & Jung WS (2002). Reliability generalization of scores on the Spielberger state-trait anxiety inventory. Educational and Psychological Measurement, 62(4), 603–618. 10.1177/001316402128775049 [DOI] [Google Scholar]
- Barrett LF (2006a). Are emotions natural kinds? Perspectives on Psychological Science, 7(1), 28–58. 10.1111/j.1745-6916.2006.00003.x [DOI] [PubMed] [Google Scholar]
- Barrett LF (2006b). Solving the emotion paradox: Categorization and the experience of emotion. Personality and Social Psychology Review, 70(1), 20–46. 10.1207/s15327957pspr1001_2 [DOI] [PubMed] [Google Scholar]
- Barrett LF, Gross J, Christensen TC, & Benvenuto M (2001). Knowing what you’re feeling and knowing what to do about it: Mapping the relation between emotion differentiation and emotion regulation. Cognition & Emotion, 75(6), 713–724. 10.1080/02699930143000239 [DOI] [Google Scholar]
- Beck AT, Brown G, Epstein N, & Steer RA (1988). An inventory for measuring clinical anxiety - Psychometric properties. Journal of Consulting and Clinical Psychology, 56(6), 893–897. 10.1037//0022-006x.56.6.893 [DOI] [PubMed] [Google Scholar]
- Beck AT, Erbaugh J, Ward CH, Mock J, & Mendelsohn M (1961). An inventory for measuring depression. Archives of General Psychiatry, 4(6), 561–571. [DOI] [PubMed] [Google Scholar]
- Berg CZ, Shapiro N, Chambless DL, & Ahrens AH (1998). Are emotions frightening? II: an analogue study of fear of emotion, interpersonal conflict, and panic onset. Behaviour Research and Therapy, 56(1), 3–15. 10.1016/S0005-7967(97)10027-4 [DOI] [PubMed] [Google Scholar]
- Bishop SR (2002). What do we really know about mindfulness-based stress reduction? Psychosomatic Medicine, 64(1), 71–83. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Segal ZV, Abbey S, Speca M, Velting D, & Devins G (2004). Mindfulness: A proposed operational definition. Clinical Psychology-Science and Practice, 11(3), 230–241. 10.1093/clipsy/bph077 [DOI] [Google Scholar]
- Brewer JA, Sinha R, Chen JA, Michalsen RN, Babuscio TA, Nich C, Grier A, Bergquist KL, Reis DL, Potenza MN, Carroll KM, & Rounsaville BJ (2009). Mindfulness training and stress reactivity in substance abuse: results from a randomized, controlled stage I pilot study. Substance Abuse, 30(4), 306–317. 10.1080/08897070903250241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton WB, Bootzin RR, Cousins JC, Hasler BP, Peck T, & Shapiro SL (2010). The contribution of mindfulness practice to a multicomponent behavioral sleep intervention following substance abuse treatment in adolescents: a treatment-development study. Substance Abuse, 31(2), 86–97. 10.1080/08897071003641297 [DOI] [PubMed] [Google Scholar]
- *Britton WB, Shahar B, Szepsenwol O, & Jacobs WJ (2012). Mindfulness-based cognitive therapy improves emotional reactivity to social stress: results from a randomized controlled trial. Behavior Therapy, 43(2), 365–380. 10.1016/j.beth.2011.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Berntson GG, Larsen JT, Poehlmann KM, & Ito TA (2000). The psychophysiology of emotion. Handbook of emotions, 2, 173–191. [Google Scholar]
- Carlson LE, Speca M, Faris P, & Patel KD (2007). One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behavior and Immunity, 21(8), 1038–1049. 10.1016/j.bbi.2007.04.002 [DOI] [PubMed] [Google Scholar]
- Coan JA (2010). Emergent ghosts of the emotion machine. Emotion Review, 2(3), 274–285. 10.1177/1754073910361978 [DOI] [Google Scholar]
- Coan JA, & Allen JJ (Eds.). (2007). Handbook of emotion elicitation and assessment. Oxford University Press. [Google Scholar]
- Cohen S, Kamarck T, & Mermelstein R (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Cohen S, & Williamson G (1988). Perceived stress in a probability sample of the United States. In Spacapan S & Oskamp S (Eds.), The Social Psychology of Health (pp. 31–67). Sage Publications, Inc. [Google Scholar]
- Cosci F, Pistelli F, Lazzarini N, & Carrozzi L (2011). Nicotine dependence and psychological distress: outcomes and clinical implications in smoking cessation. Psychological Research and Behavior Management, 4, 119–128. 10.2147/PRBM.S14243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane RS, Brewer J, Feldman C, Kabat-Zinn J, Santorelli S, Williams JM, & Kuyken W (2017). What defines mindfulness-based programs? The warp and the weft. Psychological Medicine, 47(6), 990–999. 10.1017/S0033291716003317 [DOI] [PubMed] [Google Scholar]
- Crane RS, Eames C, Kuyken W, Hastings RP, Williams JM, Bartley T, Evans A, Silverton S, Soulsby JG, & Surawy C (2013). Development and validation of the mindfulness-based interventions - teaching assessment criteria (MBI:TAC). Assessment, 20(6), 681–688. 10.1177/1073191113490790 [DOI] [PubMed] [Google Scholar]
- Crane RS, Kuyken W, Williams JM, Hastings RP, Cooper L, & Fennell MJ (2012). Competence in teaching mindfulness-based courses: Concepts, development and assessment. Mindfulness, 2(1), 76–84. 10.1007/s12671-011-0073-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P, Li JA, Hofmann SG, & Andersson G (2010). Self-reported versus clinician-rated symptoms of depression as outcome measures in psychotherapy research on depression: A meta-analysis. Clinincal Psychology Review, 30(6), 768–778. 10.1016/j.cpr.2010.06.001 [DOI] [PubMed] [Google Scholar]
- Dahl CJ, Lutz A, & Davidson RJ (2015). Reconstructing and deconstructing the self: cognitive mechanisms in meditation practice. Trends in Cognitive Sciences, 19(9), 515–523. 10.1016/j.tics.2015.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson RJ, Kabat-Zinn J, Schumacher J, Rosenkranz M, Muller D, Santorelli SF, Urbanowski F, Harrington A, Bonus K, & Sheridan JF (2003). Alterations in brain and immune function produced by mindfulness meditation. Psychosomatic Medicine, 65(4), 564–570. 10.1097/01.PSY.0000077505.67574.E3 [DOI] [PubMed] [Google Scholar]
- Davidson RJ, & Kaszniak AW (2015). Conceptual and methodological issues in research on mindfulness and meditation. The America Psychologist, 70(7), 581–592. 10.1037/a0039512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR (1994). SCL-90-R administration, scoring and procedures manual (3rd ed.). NSC Peason, Inc. [Google Scholar]
- Derogatis LR (2000). BSI-18: Administration, Scoring, and Procedures Manual National Computer Systems. [Google Scholar]
- Desbordes G, Negi LT, Pace TW, Wallace BA, Raison CL, & Schwartz EL (2012). Effects of mindful-attention and compassion meditation training on amygdala response to emotional stimuli in an ordinary, non-meditative state. Frontiers in Human Neuroscience, 6, 292. 10.3389/fnhum.2012.00292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeSteno D, Gross JJ, & Kubzansky L (2013). Affective science and health: The importance of emotion and emotion regulation. Health Psychology, 32(5), 474–486. 10.1037/a0030259 [DOI] [PubMed] [Google Scholar]
- Deyo RA, Ciol MA, Cherkin DC, Loeser JD, & Bigos SJ (1993). Lumbar Spinal-fusion - a Cohort study of complications, reoperations, and resource use in the medicare population. Spine, 75(11), 1463–1470. [PubMed] [Google Scholar]
- Dimidjian S, & Segal ZV (2015). Prospects for a clinical science of mindfulness-based intervention. The America Psychologist, 70(7), 593–620. 10.1037/a0039589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dozois DJA, Dobson KS, & Ahnberg JL (1998). A psychometric evaluation of the Beck Depression Inventory - II. Psychological Assessment, 70(2), 83–89. [Google Scholar]
- Dupuy H (1984). The Psychological General Well Being Index (PGWBI). In Wenger N, Mattson M, Furburg C, & Elinson J (Eds.), Assessment of Quality of Life in Clinical Trials of Cardiovascular Therapies (pp. 170–183). Le Jacq Publishing. [DOI] [PubMed] [Google Scholar]
- Egger M, Smith GD, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. Bmj-British Medical Journal, 375(7109), 629–634. 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elfhag K, & Rossner S (2005). Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obesity Reviews, 5(1), 67–85. 10.1111/j.1467-789X.2005.00170.x [DOI] [PubMed] [Google Scholar]
- Erisman SM, & Roemer L (2010). A preliminary investigation of the effects of experimentally induced mindfulness on emotional responding to film clips. Emotion, 10(1), 72–82. 10.1037/a0017162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evers C, Dingemans A, Junghans AF, & Boeve A (2018). Feeling bad or feeling good, does emotion affect your consumption of food? A meta-analysis of the experimental evidence. Neuroscience and Biobehavioral Reviews, 92, 195–208. 10.1016/j.neubiorev.2018.05.028 [DOI] [PubMed] [Google Scholar]
- Evers C, Marijn Stok F, & de Ridder DT (2010). Feeding your feelings: emotion regulation strategies and emotional eating. Personality and Social Psychology Bulletin, 36(6), 792–804. 10.1177/0146167210371383 [DOI] [PubMed] [Google Scholar]
- Evers KE, Prochaska JO, Johnson JL, Mauriello LA, Padula JA, & Prochaska JM (2006). A randomized clinical trial of a population- and transtheoretical model-based stress-management intervention. Health Psychology, 25(4), 521–529. 10.1037/0278-6133.25.4.521 [DOI] [PubMed] [Google Scholar]
- Eysenck SBG, Eysenck HJ, & Barrett P (1985). A revised version of the Psychoticism Scale. Personality and Individual Differences, 6(1), 21–29. 10.1016/0191-8869(85)90026-1 [DOI] [Google Scholar]
- Ferrer RA, Green PA, & Barrett LF (2015). Affective science perspectives on cancer control: Strategically crafting a mutually beneficial research agenda. Perspectives on Psychological Science, 10(3), 328–345. 10.1177/1745691615576755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrer RA, Green PA, Oh AY, Hennessy E, & Dwyer LA (2017). Emotion suppression, emotional eating, and eating behavior among parent-adolescent dyads. Emotion, 17(7), 1052–1065. 10.1037/emo0000295 [DOI] [PubMed] [Google Scholar]
- Ferrer RA, & Mendes WB (2018). Emotion, health decision making, and health behaviour. Psychology & Health, 22(1), 1–16. 10.1080/08870446.2017.1385787 [DOI] [PubMed] [Google Scholar]
- Fries E, Dettenborn L, & Kirschbaum C (2009). The cortisol awakening response (CAR): Facts and future directions. International Journal of Psychophysiology, 72(1), 67–73. 10.1016/j.ijpsycho.2008.03.014 [DOI] [PubMed] [Google Scholar]
- Gallego J, Aguilar-Parra JM, Cangas AJ, Langer AI, & Manas I (2014). Effect of a mindfulness program on stress, anxiety and depression in university students. Spanish Journal of Psychology, 17, E109. 10.1017/sjp.2014.102 [DOI] [PubMed] [Google Scholar]
- Garland EL, & Gaylord S (2009). Envisioning a future contemplative science of mindfulness: Fruitful methods and new content for the next wave of research. Complementary Health Practice Review, 14(1), 3–9. 10.1177/1533210109333718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garland EL, Gaylord SA, & Fredrickson BL (2011). Positive reappraisal mediates the stress-reductive effects of mindfulness: An upward spiral process. Mindfulness, 2(1), 59–67. 10.1007/s12671-011-0043-8 [DOI] [Google Scholar]
- Garland EL, Thomas E, & Howard MO (2014). Mindfulness-oriented recovery enhancement ameliorates the impact of pain on self-reported psychological and physical function among opioid-using chronic pain patients. Journal of Pain Symptom Management, 48(6), 1091–1099. 10.1016/j.jpainsymman.2014.03.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gawande R, To MN, Pine E, Griswold T, Creedon TB, Brunel A, Lozada A, Loucks EB, & Schuman-Olivier Z (2019). Mindfulness training enhances self-regulation and facilitates health behavior change for primary care patients: a randomized controlled trial. Journal of General Internal Medicine, 34(2), 293–302. 10.1007/s11606-018-4739-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert P, & Allan S (1998). The role of defeat and entrapment (arrested flight) in depression: an exploration of an evolutionary view. Psycholocial Medicine, 28(3), 585–598. 10.1017/S0033291798006710 [DOI] [PubMed] [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Davidson RJ, Kearney DJ, & Simpson TL (2019). Mindfulness-based cognitive therapy for the treatment of current depressive symptoms: a meta-analysis. Cognitive Behaviour Therapy, 48(6), 445–462. 10.1080/16506073.2018.1556330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Simpson TL, Kearney DJ, & Davidson RJ (2017). Is mindfulness research methodology improving over time? A systematic review. PLoS One, 12(10), e0187298. 10.1371/journal.pone.0187298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldin PR, & Gross JJ (2010). Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion, 10(1), 83–91. 10.1037/a0018441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal M, Singh S, Sibinga EM, Gould NF, Rowland-Seymour A, Sharma R, Berger Z, Sleicher D, Maron DD, Shihab HM, Ranasinghe PD, Linn S, Saha S, Bass EB, & Haythornthwaite JA (2014). Meditation programs for psychological stress and well being: a systematic review and meta-analysis. JAMA Internal Medicine, 174(3), 357–368. 10.1001/jamainternmed.2013.13018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. 10.1023/B:Joba.0000007455.08539.94 [DOI] [Google Scholar]
- Gross JJ (2014). Emotion regulation: Conceptual and empirical foundations. In Gross JJ (Ed.), Handbook of emotion regulation (pp. 3–20). The Guilford Press. [Google Scholar]
- Gross JJ, & John OP (2003). Individual differences in two emotion regulation processes: Implications for affect, relationships, and well-being. Journal of Personality and Social Psychology, 85(2), 348–362. 10.1037/0022-3514.85.2.348 [DOI] [PubMed] [Google Scholar]
- Grossman P, & Van Dam NT (2011). Mindfulness, by any other name…: trials and tribulations of sati in western psychology and science. Contemporary Buddhism, 12(1), 219–239. 10.1080/14639947.2011.564841 [DOI] [Google Scholar]
- Gu J, Strauss C, Bond R, & Cavanagh K (2015). How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clinical Psychology Review, 37, 1–12. 10.1016/j.cpr.2015.01.006 [DOI] [PubMed] [Google Scholar]
- Guy W (1976). Clinical global impression. In Guy W (Ed.), CDEU assessment manual for psychopharmacology (pp. 218–221). National Institute of Mental Health. [Google Scholar]
- Hamilton M (1960). A rating scale for depression. Journal of Neurology Neurosurgery and Psychiatry, 23(1), 56–62. 10.1136/jnnp.23.1.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harper A, Power M, & Grp W (1998). Development of the World Health Organization WHOQOL-BREF quality of life assessment. Psychological Medicine, 28(3), 551–558. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl KD, & Wilson KG (2012). Acceptance and commitment therapy: The process and practice of mindful change (2nd edition). Guilford. [Google Scholar]
- Hedges LV, Tipton E, & Johnson MC (2010). Robust variance estimation in meta-regression with dependent effect size estimates. Research Synthesis Methods, 7(1), 39–65. 10.1002/jrsm.5 [DOI] [PubMed] [Google Scholar]
- *Henderson VP, Clemow L, Massion AO, Hurley TG, Druker S, & Hebert JR (2012). The effects of mindfulness-based stress reduction on psychosocial outcomes and quality of life in early-stage breast cancer patients: a randomized trial. Breast Cancer Research and Treatment, 737(1), 99–109. 10.1007/s10549-011-1738-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hennessy EA, Johnson BT, Acabchuk RL, McCloskey K, & Stewart-James J (2020). Self regulation mechanisms in health behavior change: a systematic meta-review of meta-analyses, 2006–2017. Health Psychology Review, 74(1), 6–42. 10.1080/17437199.2019.1679654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, & Welch VA (2019). Cochrane Handbook for Systematic Reviews of Interventions version 6.0 (updated August 2079). Available from www.training.cochrane.org/handbook. (6.0 ed.). Cochrane. https://training.cochrane.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann W, Rauch W, & Gawronski B (2007). And deplete us not into temptation: Automatic attitudes, dietary restraint, and self-regulatory resources as determinants of eating behavior. Journal of Experimental Social Psychology, 43(3), 497–504. 10.1016/j.jesp.2006.05.004 [DOI] [Google Scholar]
- *Hoge EA, Bui E, Marques L, Metcalf CA, Morris LK, Robinaugh DJ, Worthington JJ, Pollack MH, & Simon NM (2013). Randomized controlled trial of mindfulness meditation for generalized anxiety disorder: effects on anxiety and stress reactivity. Journal of Clinical Psychiatry, 74(8), 786–792. 10.4088/JCP.12m08083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge EA, Bui E, Palitz SA, Schwarz NR, Owens ME, Johnston JM, Pollack MH, & Simon NM (2018). The effect of mindfulness meditation training on biological acute stress responses in generalized anxiety disorder. Psychiatry Research, 262, 328–332. 10.1016/j.psychres.2017.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes EA, Ghaderi A, Harmer CJ, Ramchandani PG, Cuijpers P, Morrison AP, Roiser JP, Bockting CLH, O’Connor RC, Shafran R, Moulds ML, & Craske MG (2018). The Lancet Psychiatry Commission on psychological treatments research in tomorrow’s science. Lancet Psychiatry, 5(3), 237–286. 10.1016/S2215-0366(17)30513-8 [DOI] [PubMed] [Google Scholar]
- Holzel BK, Hoge EA, Greve DN, Gard T, Creswell JD, Brown KW, Barrett LF, Schwartz C, Vaitl D, & Lazar SW (2013). Neural mechanisms of symptom improvements in generalized anxiety disorder following mindfulness training. Neuroimage Clinical, 2, 448–458. 10.1016/j.nicl.2013.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel BK, Lazar SW, Gard T, Schuman-Olivier Z, Vago DR, & Ott U (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science, 6(6), 537–559. 10.1177/1745691611419671 [DOI] [PubMed] [Google Scholar]
- Hughes MC, Baker TA, Kim H, & Valdes EG (2019). Health behaviors and related disparities of insured adults with a health care provider in the United States, 2015-2016. Preventive Medicine, 120, 42–49. 10.1016/j.ypmed.2019.01.004 [DOI] [PubMed] [Google Scholar]
- Ingels JS, & Zizzi S (2018). A qualitative analysis of the role of emotions in different patterns of long-term weight loss. Psychology & Health, 55(8), 1014–1027. 10.1080/08870446.2018.1453511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacob MC, Kems RD, Rosenberg R, & Haythomthwaite J (1993). Chronic Pain - Intrusion and accommodation. Behaviour Research and Therapy, 31(5), 519–527. [DOI] [PubMed] [Google Scholar]
- Jensen CG, Vangkilde S, Frokjaer V, & Hasselbalch SG (2012). Mindfulness training affects attention—or is it attentional effort? Journal of Experimental Psychology General 777(1), 106–123. 10.1037/a0024931 [DOI] [PubMed] [Google Scholar]
- Johnson BT, & Hennessy EA (2019). Systematic reviews and meta-analyses in the health sciences: Best practice methods for research syntheses. Social Science & Medicine, 233, 237–251. 10.1016/j.socscimed.2019.05.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson NB, Hayes LD, Brown K, Hoo EC, & Ethier KA (2014). CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors—United States, 2005–2013. MMWR, Suppl 63, 3–27. [PubMed] [Google Scholar]
- Julian LJ (2011). Measures of anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care Research (Hoboken), 63 Suppl 11, S467–472. 10.1002/acr.20561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. General Hospital Psychiatry, 7(1), 33–47. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J (2003). Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology-Science and Practice, 10(2), 144–156. 10.1093/clipsy/bpg016 [DOI] [Google Scholar]
- Kabat-Zinn J (2013). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Bantam. [Google Scholar]
- Kabat-Zinn J, Wheeler E, Light T, Skillings A, Scharf MJ, Cropey TG, Hosmer D, & Bamhard JD (2003). Part II: Influence of a mindfulness meditation-based stress reduction intervention on rates of skin clearing in patients with moderate to severe psoriasis undergoing phototherapy (UVB) and photochemo-therapy (PUVA). Constructivism in the Human Sciences, 8(2), 85–106. [Google Scholar]
- Kangas M, & Gross JJ (2017). The Affect Regulation in Cancer framework: Understanding affective responding across the cancer trajectory. Journal of Health Psychology, 25(1), 7–25. 10.1177/1359105317748468 [DOI] [PubMed] [Google Scholar]
- Khoury B, Lecomte T, Fortin G, Masse M, Therien P, Bouchard V, Chapleau MA, Paquin K, & Hofmann SG (2013). Mindfulness-based therapy: a comprehensive meta-analysis. Clinical Psychology Review, 88(6), 763–771. 10.1016/j.cpr.2013.05.005 [DOI] [PubMed] [Google Scholar]
- Kirschbaum C, Pirke KM, & Hellhammer DH (1993). The Trier Social Stress Test - a Tool for Investigating Psychobiological Stress Responses in a Laboratory Setting. Neuropsychobiology, 28(1-2), 76–81. 10.1159/000119004 [DOI] [PubMed] [Google Scholar]
- Koolhaas JM, Bartolomucci A, Buwalda B, de Boer SF, Flugge G, Korte SM, Meerlo P, Murison R, Olivier B, Palanza P, Richter-Levin G, Sgoifo A, Steimer T, Stiedl O, van Dijk G, Wohr M, & Fuchs E (2011). Stress revisited: A critical evaluation of the stress concept. Neuroscience and Biobehavioral Reviews, 38(5), 1291–1301. 10.1016/j.neubiorev.2011.02.003 [DOI] [PubMed] [Google Scholar]
- *Koszycki D, Benger M, Shlik J, & Bradwejn J (2007). Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behaviour Research and Therapy, 48(10), 2518–2526. 10.1016/j.brat.2007.04.011 [DOI] [PubMed] [Google Scholar]
- Kuehner C, Huffziger S, & Liebsch K (2009). Rumination, distraction and mindful self-focus: effects on mood, dysfunctional attitudes and cortisol stress response. Psychological Medicine, 39(2), 219–228. 10.1017/s0033291708003553 [DOI] [PubMed] [Google Scholar]
- Lazarus RS, & Folkman S (1984). Stress, Appraisal, and Coping. Springer. [Google Scholar]
- Leung L (2012). Pain catastrophizing: an updated review. Indian Journal of Psychological Medicine, 34(3), 204–217. 10.4103/0253-7176.106012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W, Howard MO, Garland EL, McGovern P, & Lazar M (2017). Mindfulness treatment for substance misuse: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 75, 62–96. 10.1016/j.jsat.2017.01.008 [DOI] [PubMed] [Google Scholar]
- Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JPA, Clarke M, Devereaux PJ, Kleijnen J, & Moher D (2009). The PRISMA Statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Plos Medicine, 6(7). 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lievens F, & Chan D (2017). Practical intelligence, emotional intelligence, and social intelligence. In InFarr JL & Tippins NT (Eds.) Handbook of employee selection (pp. 342–364). Routledge. [Google Scholar]
- Lindquist KA, Wager TD, Kober H, Bliss-Moreau E, & Barrett LF (2012). The brain basis of emotion: A meta-analytic review. Behavioral and Brain Sciences, 35(3), 121–143. 10.1017/S0140525x11000446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loucks EB, Schuman-Olivier Z, Britton WB, Fresco DM, Desbordes G, Brewer JA, & Fulwiler C (2015). Mindfulness and cardiovascular disease risk: State of the evidence, plausible mechanisms, and theoretical framework. Current Cardiology Report, 17(12), 112. 10.1007/s11886-015-0668-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states - Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 55(3), 335–343. 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- Magai C, Consedine N, Neugut AI, & Hershman DL (2007). Common psychosocial factors underlying breast cancer screening and breast cancer treatment adherence: A conceptual review and synthesis. Journal of Womens Health, 16(1), 11–23. 10.1089/jwh.2006.0024 [DOI] [PubMed] [Google Scholar]
- Maglione MA, Maher AR, Ewing B, Colaiaco B, Newberry S, Kandrack R, Shanman RM, Sorbero ME, & Hempel S (2017). Efficacy of mindfulness meditation for smoking cessation: A systematic review and meta-analysis. Addictive Behaviors, 69, 27–34. 10.1016/j.addbeh.2017.01.022 [DOI] [PubMed] [Google Scholar]
- Mansyur CL, Pavlik VN, Hyman DJ, Taylor WC, & Goodrick GK (2013). Self-efficacy and barriers to multiple behavior change in low-income African Americans with hypertension. Journal of Behavioral Medicine, 56(1), 75–85. 10.1007/s10865-012-9403-7 [DOI] [PubMed] [Google Scholar]
- McCracken LM, Vowles KE, & Eccleston C (2004). Acceptance of chronic pain: component analysis and a revised assessment method. Pain, 107(1-2), 159–166. 10.1016/j.pain.2003.10.012 [DOI] [PubMed] [Google Scholar]
- McNair DA, Lorr M, & Droppelman LF (1971). Profile of Mood States. Educational and Industrial Testing Service. [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, & Borkovec TD (1990). Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy, 28(6), 487–495. 10.1016/0005-7967(90)90135-6 [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG, & Grp P (2010). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. International Journal of Surgery, 8(5), 336–341. 10.1016/j.ijsu.2010.02.007 [DOI] [PubMed] [Google Scholar]
- Ng DM, & Jeffery RW (2003). Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychology, 22(6), 638–642. 10.1037/0278-6133.33.6.638 [DOI] [PubMed] [Google Scholar]
- Nielsen L, Riddle M, King JW, Aklin WM, Chen W, Clark D, Collier E, Czajkowski S, Esposito L, Ferrer R, Green P, Hunter C, Kehl K, King R, Onken L, Simmons JM, Stoeckel L, Stoney C, Tully L, & Weber W (2018). The NIH Science of Behavior Change Program: Transforming the science through a focus on mechanisms of change. Behaviour Research and Therapy, 101, 3–11. 10.1016/j.brat.2017.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor DB, Jones F, Conner M, McMillan B, & Ferguson E (2008). Effects of daily hassles and eating style on eating behavior. Health Psychology, 27(1), S20–S31. 10.1037/0278-6133.27.1(Suppl.).S20 [DOI] [PubMed] [Google Scholar]
- O’Leary D, Suri G, & Gross JJ (2018). Reducing behavioural risk factors for cancer: An affect regulation perspective. Psychological Health, 33(1), 17–39. 10.1080/08870446.2017.1314480 [DOI] [PubMed] [Google Scholar]
- Ochsner KN, & Gross JJ (2005). The cognitive control of emotion. Trends in Cognitive Sciences, 9(5), 242–249. 10.1016/j.tics.2005.03.010 [DOI] [PubMed] [Google Scholar]
- Ortner CNM, Kilner SJ, & Zelazo PD (2007). Mindfulness meditation and reduced emotional interference on a cognitive task. Motivation and Emotion, 31(4), 271–283. 10.1007/s11031-007-9076-7 [DOI] [Google Scholar]
- Ostafin BD, Robinson MD, & Meier BP (Eds.). (2015). Handbook of Mindfulness and Self Regulation. Springer. [Google Scholar]
- Ottenstein C, & Lischetzke T (In Press). Development of a novel method of emotion differentiation that uses open-ended descriptions of momentary affective states. Assessment. 10.1177/1073191119839138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pariante CM (2003). Depression, stress and the adrenal axis. Journal of Neuroendocrinology, 15(8), 811–812. 10.1046/j.1365-2826.2003.01058.x [DOI] [PubMed] [Google Scholar]
- *Polusny MA, Erbes CR, Thuras P, Moran A, Lamberty GJ, Collins RC, Rodman JL, & Lim KO (2015). Mindfulness-based stress reduction for Posttraumatic Stress Disorder among veterans: A randomized clinical trial. Jama, 314(5), 456–465. 10.1001/jama.2015.8361 [DOI] [PubMed] [Google Scholar]
- Quigley KS, Lindquist KA, & Barrett LF (2014). Inducing and measuring emotion and affect: Tips, tricks, and secrets. In Reis HT & Judd CM (Eds.). Handbook of research methods in social and personality psychology (pp. 220–252). Cambridge University Press. [Google Scholar]
- Rapgay L, & Bystrisky A (2009). Classical mindfulness: an introduction to its theory and practice for clinical application. Annals of the New York Academy of Science, 1172, 148–162. 10.1111/j.1749-6632.2009.04405.x [DOI] [PubMed] [Google Scholar]
- Robinson KL, McBeth J, & MacFarlane GJ (2004). Psychological distress and premature mortality in the general population: A prospective study. Annals of Epidemiology, 14(7), 467–472. 10.1016/j.annepidem.2003.11.007 [DOI] [PubMed] [Google Scholar]
- Rogers JM, Ferrari M, Mosely K, Lang CP, & Brennan L (2017). Mindfulness-based interventions for adults who are overweight or obese: a meta-analysis of physical and psychological health outcomes. Obesity Reviews, 15(1), 51–67. 10.1111/obr.12461 [DOI] [PubMed] [Google Scholar]
- Rosenstiel AK, & Keefe FJ (1983). The use of coping strategies in chronic low-back-pain patients - Relationship to patient characteristics and current adjustment. Pain, 17(1), 33–44. [DOI] [PubMed] [Google Scholar]
- Ruffault A, Czernichow S, Hagger MS, Ferrand M, Erichot N, Carette C, Boujut E, & Flahault C (2017). The effects of mindfulness training on weight-loss and health-related behaviours in adults with overweight and obesity: A systematic review and meta-analysis. Obesity Research and Clinical Practice, 11(5S1), 90–111. 10.1016/j.orcp.2016.09.002 [DOI] [PubMed] [Google Scholar]
- Ryan R, Booth S, Spathis A, Mollart S, & Clow A (2016). Use of salivary diurnal cortisol as an outcome measure in randomised controlled trials: a systematic review. Annals of Behavioral Medicine, 50(2), 210–236. 10.1007/s12160-015-9753-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryff CD (1989). Happiness is everything, or is it - Explorations on the meaning of psychological well-being. Journal of Personality and Social Psychology, 57(6), 1069–1081. 10.1037/0022-3514.57.6.1069 [DOI] [Google Scholar]
- Santa Ana EJ, Saladin ME, Back SE, Waldrop AE, Spratt EG, McRae AL, LaRowe SD, Timmerman MA, Upadhyaya H, & Brady KT (2006). PTSD and the HPA axis: Differences in response to the cold pressor task among individuals with child vs. adult trauma. Psychoneuroendocrinology, 31(4), 501–509. 10.1016/j.psyneuen.2005.11.009 [DOI] [PubMed] [Google Scholar]
- Santorelli S, Meleo-Meyer F, Koerbel L, Kabat-Zinn J, Blacker M, Herbette G, & Fulwiler C (2017). Mindfulness-Based Stress Reduction (MBSR) Authorized Curriculum Guide (Santorelli SF, Kabat-Zinn J, Blacker M, Meleo-Meye r. F., & Koerbel LS, Eds.). http://www.umassmed.edu/cfm/training/mbsr-curriculum [Google Scholar]
- Segal ZV, Teasdale JD, Williams JM, & Gemar MC (2002). The mindfulness-based cognitive therapy adherence scale: Inter-rater reliability, adherence to protocol and treatment distinctiveness. Clinical Psychology & Psychotherapy, 9(2), 131–138. 10.1002/cpp.320 [DOI] [Google Scholar]
- Segal ZV, Williams JM, & Teasdale JD (2013). Mindfulness-based cognitive therapy for depression (2nd ed.). Guilford Press. [Google Scholar]
- Severeijns R, Vlaeyen JWS, van den Hout MA, & Weber WEJ (2001). Pain catastrophizing predicts pain intensity, disability, and psychological distress independent of the level of physical impairment. Clinical Journal of Pain, 17(2), 165–172. [DOI] [PubMed] [Google Scholar]
- Smyth JM, & Arigo D (2009). Recent evidence supports emotion-regulation interventions for improving health in at-risk and clinical populations. Current Opinion in Psychiatry, 22(2), 205–210. 10.1097/YCO.0b013e3283252d6d [DOI] [PubMed] [Google Scholar]
- Snyder DK (1997). Manual for the Marital Satisfaction Inventory-Revised. Western Psychological Services. [Google Scholar]
- Stalder T, Kirschbaum C, Kudielka BM, Adam EK, Pruessner JC, Wust S, Dockray S, Smyth N, Evans P, Hellhammer DH, Miller R, Wetherell MA, Lupien SJ, & Clow A (2016). Assessment of the cortisol awakening response: Expert consensus guidelines. Psychoneuroendocrinology, 63, 414–432. 10.1016/j.psyneuen.2015.10.010 [DOI] [PubMed] [Google Scholar]
- Stansfeld SA, Fuhrer R, Shipley MJ, & Marmot MG (2002). Psychological distress as a risk factor for coronary heart disease in the Whitehall II Study. International Journal of Epidemiology, 31(1), 248–255. 10.1093/ije/31.1.248 [DOI] [PubMed] [Google Scholar]
- Sullivan MJL (2009). The Pain Catastrophizing Scale: User Manual (Vol. 5). McGill University. [Google Scholar]
- Suls J, & Bunde J (2005). Anger, anxiety, and depression as risk factors for cardiovascular disease: The problems and implications of overlapping affective dispositions. Psychological Bulletin, 131(2), 260–300. 10.1037/0033-2909.131.2.260 [DOI] [PubMed] [Google Scholar]
- Tabibian A, Tabibian JH, Beckman LJ, Raffals LL, Papadakis KA, & Kane SV (2015). Predictors of health-related quality of life and adherence in Crohn’s disease and Ulcerative Colitis: Implications for clinical management. Digestive Diseases and Sciences, 60(5), 1366–1374. 10.1007/s10620-014-3471-1 [DOI] [PubMed] [Google Scholar]
- Tang YY, Ma Y, Wang J, Fan Y, Feng S, Lu Q, Yu Q, Sui D, Rothbart MK, Fan M, & Posner MI (2007). Short-term meditation training improves attention and self-regulation. Proceedings of the National Academdy of Science U S A, 104(43), 17152–17156. 10.1073/pnas.0707678104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner-Smith EE, & Tipton E (2014). Robust variance estimation with dependent effect sizes: practical considerations including a software tutorial in Stata and SPSS. Research Synthesis Methods, 5(1), 13–30. 10.1002/jrsm.1091 [DOI] [PubMed] [Google Scholar]
- Taren AA, Gianaros PJ, Greco CM, Lindsay EK, Fairgrieve A, Brown KW, Rosen RK, Ferris JL, Julson E, Marsland AL, Bursley JK, Ramsburg J, & Creswell JD (2015). Mindfulness meditation training alters stress-related amygdala resting state functional connectivity: a randomized controlled trial. Social Cognitive Affective Neuroscience, 10(12), 1758–1768. 10.1093/scan/nsv066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taut D, Renner B, & Baban A (2012). Reappraise the Situation but Express Your Emotions: Impact of Emotion Regulation Strategies on ad libitum Food Intake. Frontiers in Psychology, 3, 359. 10.3389/fpsyg.2012.00359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor VA, Grant J, Daneault V, Scavone G, Breton E, Roffe-Vidal S, Courtemanche J, Lavarenne AS, & Beauregard M (2011). Impact of mindfulness on the neural responses to emotional pictures in experienced and beginner meditators. Neuroimage, 57(4), 1524–1533. 10.1016/j.neuroimage.2011.06.001 [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Moore RG, Hayhurst H, Pope M, Williams S, & Segal ZV (2002). Metacognitive awareness and prevention of relapse in depression: empirical evidence. Journal of Consulting and Clinical Psychology, 70(2), 275–287. [DOI] [PubMed] [Google Scholar]
- Vago DR, & Silbersweig DA (2012). Self-awareness, self-regulation, and self-transcendence (S-ART): a framework for understanding the neurobiological mechanisms of mindfulness. Frontiers in Human Neuroscience, 6, 296. 10.3389/fnhum.2012.00296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Dam NT, van Vugt MK, Vago DR, Schmalzl L, Saron CD, Olendzki A, Meissner T, Lazar SW, Kerr CE, Gorchov J, Fox KCR, Field BA, Britton WB, Brefczynski-Lewis JA, & Meyer DE (2018). Mind the hype: A critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspectives on Psychological Science, 13(1), 36–61. 10.1177/1745691617709589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visted E, Vollestad J, Nielsen MB, & Nielsen GH (2015). The impact of group-based mindfulness training on self-reported mindfulness: a systematic review and meta-analysis. Mindfulness, 6(3), 501–522. 10.1007/s12671-014-0283-5 [DOI] [Google Scholar]
- Vohs KD, & Baumeister RF (Eds.). (2016). Handbook of Self-Regulation: Research, Theory, and Applications (3rd ed.). Guilford Press. [Google Scholar]
- Wallace BC, Small K, Brodley CE, Lau J, & Trikalinos TA (2012). Deploying an interactive machine learning system in an evidence-based practice center: abstrackr. Proceedings of the 2nd ACM SIGHIT International Health Informatics Symposium, [Google Scholar]
- Wang YP, & Gorenstein C (2013). Psychometric properties of the Beck Depression Inventory-II: a comprehensive review. Revista Brasileira De Psiquiatria, 35(4), 416–431. 10.1590/1516-4446-2012-1048 [DOI] [PubMed] [Google Scholar]
- Ward BW, Schiller JS, & Goodman RA (2014). Multiple chronic conditions among US adults: A 2012 update. Preventing Chronic Disease, 11. 10.5888/pcd11.130389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Clark LA, & Tellegen A (1988). Development and validation of brief measures of positive and negative affect - the PANAS scales. Journal of Personality and Social Psychology, 54(6), 1063–1070. 10.1037//0022-3514.54.6.1063 [DOI] [PubMed] [Google Scholar]
- Watson M, & Greer S (1983). Development of a Questionnaire Measure of Emotional Control. Journal of Psychosomatic Research, 27(4), 299–305. 10.1016/0022-3999(83)90052-1 [DOI] [PubMed] [Google Scholar]
- Wing RR, Papandonatos G, Fava JL, Gorin AA, Phelan S, McCaffery J, & Tate DF (2008). Maintaining Large Weight Losses: The Role of Behavioral and Psychological Factors. Journal of Consulting and Clinical Psychology, 76(6), 1015–1021. 10.1037/a0014159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright R, Riedel R, Sechrest L, Lane RD, & Smith R (2018). Sex differences in emotion recognition ability: The mediating role of trait emotional awareness. Motivation and Emotion, 42(1), 149–160. 10.1007/s11031-017-9648-0 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


