ABSTRACT
Peripheral T-cell lymphomas (PTCLs) are a heterogeneous group of aggressive neoplasms. The involvement of ocular structures in haematological neoplasms is rare and usually associated with central nervous system involvement, which may occur as a result of orbital invasion and optic nerve infiltration. In this case report, we describe ocular findings using the novel swept source optical coherence tomography (SS-OCT) in a case of aggressive T-cell lymphoma. SS-OCT has faster scanning speed, deeper tissue penetration due to its longer wavelength laser of 1050 nm and wider scanning areas. In the present case, SS-OCT was helpful in documenting increased retinal nerve fibre layer thickness and prelaminar protrusion associated with visual loss in a patient with an aggressive T-cell lymphoma.
KEYWORDS: CNS lymphoma, optical coherence tomography, optic nerve
The incidence of non-Hodgkin’s lymphoma (NHL) has increased by 0.5% annually.1 Approximately 10% of patients with NHL have central nervous system (CNS) involvement, of whom about 5% may develop optic nerve infiltration. The frequency of CNS involvement in NHL varies according to histological type and subtype aggressiveness.1
Peripheral T-cell lymphomas (PTCLs) are a heterogeneous group of aggressive neoplasms, accounting for less than 15% of NHLs in adults.2 Compared with their B-cell counterparts, PTCLs remain largely unexplored and optimal treatment is still ill-defined due to disease rarity and biological heterogeneity. The involvement of ocular structures in haematological neoplasms is rare and usually associated with CNS involvement, which may occur as a result of malignant infiltration of the optic nerve. Malignant cells disturb the optic nerve circulation and cause nerve swelling.3 Optic nerve head leukaemic infiltration has been reported to occur in only 1.4% of paediatric cases and is an uncommon presentation in adults as well.4
A practical classification system of optic nerve involvement by lymphomatous cells was proposed by Kim et al.1 Optic nerve involvement was classified in the following subtypes, based in the pathophysiology of spread and course of disease: a) primary optic nerve involvement; b) optic nerve involvement with known CNS disease; c) optic nerve involvement with systemic disease; d) optic nerve involvement with primary ocular lymphoma; e) other forms of optic nerve involvement such as optic nerve compression by orbital lymphoma, paraneoplastic optic neuritis, and central retinal artery occlusion by hyperviscosity.
The case reported here is an example of optic nerve involvement due to a known previous CNS malignant infiltration.
Case report
A 19-year-old male patient was diagnosed with PTCL and thymoma seven months prior to his presentation to the neuro-ophthalmology clinic. The diagnosis was based on a positive mediastinal biopsy. He started treatment with the EPOCH regimen (etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin). He developed acute cognitive dysfunction (memory loss, disorientation, and mental confusion) one month after the diagnosis, and a spinal tap was performed. Blast cells were present in the cerebrospinal fluid (CSF). Treatment was changed to the hyper-CVAD regimen (cyclophosphamide, vincristine, doxorubicin, dexamethasone, methotrexate, and cytarabine) with good initial response. He was subsequently treated with further treatment protocols (VCR+Dauno, St Jude R11, and St Jude R15 for refractory disease).
After an episode of neutropenic fever that was treated and he was stabilised, he complained of subacute visual loss and pain in the right eye. On ocular examination, the visual acuity was counting fingers in that eye with a relative afferent pupillary defect, optic disc swelling, and vascular dilation and tortuosity (Figure 1). Swept source optical coherence tomography (SS-OCT) (Triton Plus, Topcon NJ, USA) showed an average circumpapillary retinal nerve fibre layer (cRNFL) thickness of 165 µm (over the 95th percentile) in the right eye, with the most remarkable increased thickness being observed in the nasal and inferior quadrants. A B-scan of the right optic nerve head showed bulging prelaminar tissue compatible with the swelling seen clinically. The ganglion cell-inner plexiform layer (GCL+) showed a reduction in the superior temporal sector (p < .05). The fellow eye had an average cRNFL thickness of 105 µm, but the B-scan of the optic nerve head showed protruded prelaminar tissue. The GCL+ was reduced in the inferior and nasal inferior sectors (p < .05), with zones of reduction at p < .01 in the SuperPixel-200 (Disc:RNFL/Macula:GCL++) (Figure 1).
Figure 1.
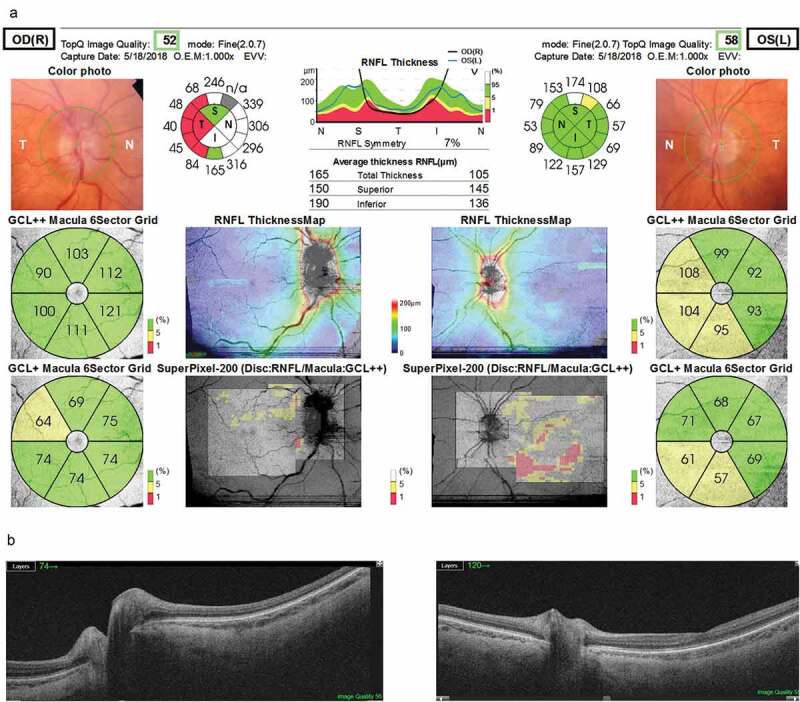
Comprehensive report that includes a colour image of the optic nerve head obtained simultaneously with the OCT scanning. The right eye (upper left) shows optic disc swelling, increased brightness of the retinal nerve fibre layer, and increased vascular tortuosity and dilation. The left eye (upper right) presents mild irregularity of the optic disc borders and pallor. The circumpapillary retinal nerve fibre layer (RNFL) thickness average and sectors and a normative profile graph where the left and right eye thicknesses are plotted (top middle), the sectorial thickness of the ganglion-cell inner plexiform layer (GCL+) as well as the former with the macular RNFL added (GCL++), and an RNFL thickness map and a superpixel panoramic map merging the macular GCL++ map and the disc RNFL map are also depicted. B-scans (from the 12 × 9 mm cube) showing, on the lower left side, greater protrusion of the prelaminar tissue of the right eye compatible with the clinical findings of optic disc swelling
Computed tomography (CT) of the head and orbits showed no apparent lesion. A spinal tap was then performed and this showed 100% blasts in the CSF, despite a normal opening pressure (15 cmCSF). Intrathecal chemotherapy (MADIT – methotrexate, cytarabine, and dexamethasone) and systemic dexamethasone was started. Magnetic resonance imaging (MRI) of the brain and orbits showed infiltration and diffuse swelling of the right optic nerve from the intra-orbital portion to the pre-chiasmatic portion, compatible with neoplastic infiltration (Figure 2). He continued to be treated with the MADIT protocol; however, his visual acuity decreased to no light perception and he died a few weeks later.
Figure 2.
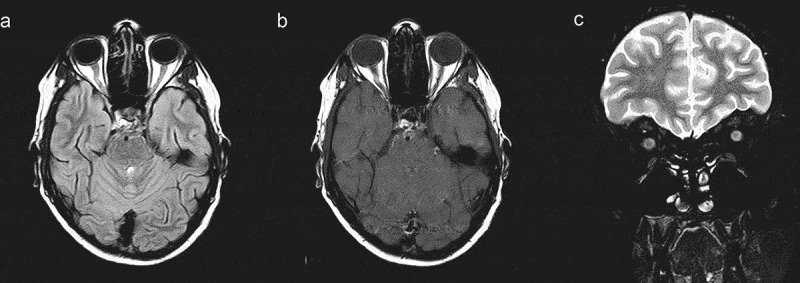
MRI of the brain and orbits. (a) Axial fast fluid attenuated inversion recovery image showing hyperintensity and increased thickness of the right optic nerve. (b) Gadolinium-enhanced axial T1-weighted image showing enhancement of the right optic nerve head. (c) Coronal T2-weighted image showing an increased diameter of the right optic nerve
Discussion
Optic nerve involvement in T-cell lymphomas is rare, with reports of ocular involvement in lymphomas of large cell, small cell, and mixed cell types. In a post-mortem histopathological study of 384 patients with leukaemia, 18% with acute leukaemia and 16% with chronic leukaemia had optic nerve involvement.5,6 The case reported here evidences optic nerve infiltration by malignant cells in a patient with known previous CNS disease infiltration and normal intracranial pressure. This case of PTCL demonstrates optic nerve malignant infiltration has been observed and documented by the novel SS-OCT technology.
Optic nerve head infiltration can be considered a sign of extramedullary relapse that precedes the haematological relapse by months before it is apparent. A complete ophthalmological examination can sometimes prompt changes in the therapeutic regimen that may have an impact on prognosis. Optical coherence tomography (OCT) is currently considered an essential imaging tool for a comprehensive ophthalmological evaluation.7 SS-OCT, used in the present case, is a novel iteration with faster scanning speed, deeper tissue penetration due to its longer wavelength laser of 1050 nm, and wider scanning areas.8 These features allow a myriad of biomarkers, both quantitative and qualitative, to be appreciated and potentially followed-up longitudinally. These advantages, compared with earlier generations of OCT systems, will certainly increase its usefulness in the field of Neuro-ophthalmology. In the present case, SS-OCT was helpful in documenting increased RNFL thickness and prelaminar protrusion associated with acute visual loss in a patient with an aggressive T-cell lymphoma. These findings prompted immediate neuroimaging and a spinal tap test, which helped to guide the haematology team in treatment decisions.
The optic nerve passes through a small-diameter bony space, the optic canal, and some authors argue that the invasion of leukaemic cells creates a mechanical barrier that blocks CSF flow at this level. Thus, cytotoxic drugs are unable to reach the affected nerve segments. Neuroimaging documentation of optic nerve involvement is critical to confirm both the fundus and OCT findings and to prompt further management. It is also important to note that the differential diagnosis of ocular symptoms in leukaemia/lymphoma should include leukaemic retinopathy, hyperviscosity and vascular occlusion and bleeding, retinal neovascularisation, and involvement of central visual pathways.9
The present case underlines the importance of a high level of suspicion to rule out optic nerve malignant infiltration.10,11 Complete neuro-ophthalmological examination and neuroimaging are required. Notwithstanding, ancillary examinations such as OCT could be clinically useful. OCT is able to show micrometric structures objectively. Ocular complaints with optic nerve and retinal findings documented with OCT could detect disease recurrence and lead to treatments to preserve vision. SS-OCT is the latest generation of this technology, featuring wider evaluation areas, deeper penetration, and faster scanning speed. This technology can potentially enhance the early detection of suspected CNS involvement in haematological neoplasms.
Declaration of interest statement
The authors have no conflicts of interest regarding this report.
References
- 1.Kim JL, Mendoza PR, Rashid A, et al. Optic nerve lymphoma: report of two cases and review of the literature. Surv Ophthalmol. 2015;60(2):153–165. doi: 10.1016/j.survophthal.2014.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rodriguez-Abreu D, Filho VB, Zucca E.. Peripheral T-cell lymphomas, unspecified (or not otherwise specified): a review. Hematol Oncol. 2008;26:8–20. [DOI] [PubMed] [Google Scholar]
- 3.Camera A, Piccirillo G, Cennamo G, et al. Optic nerve involvement in acute lymphoblastic leukemia. Leuk Lymphoma. 1993;11(1–2):153–155. [DOI] [PubMed] [Google Scholar]
- 4.Mayo GL, Carter JE, McKinnon SJ. Bilateral optic disk edema and blindness as initial presentation of acute lymphocytic leukemia. Am J Ophthalmol. 2002;134:141–142. [DOI] [PubMed] [Google Scholar]
- 5.Schocket LS, Massaro-Giordano M, Volpe NJ, Galetta SL. Bilateral optic nerve infiltration in central nervous system leukemia. Am J Ophthalmol. 2003;135:94–96. [DOI] [PubMed] [Google Scholar]
- 6.Kincaid MC, Green WR. Ocular and orbital involvement in leukemia. Surv Ophthalmol. 1983;27:211–232. [DOI] [PubMed] [Google Scholar]
- 7.Chan NCY, Chan CKM. The role of optical coherence tomography in the acute management of neuro-ophthalmic diseases. Asia Pac J Ophthalmol (Phila). 2018;7:265–270. [DOI] [PubMed] [Google Scholar]
- 8.Potsaid B, Baumann B, Huang D, et al. Ultrahigh speed 1050nm swept source/Fourier domain OCT retinal and anterior segment imaging at 100,000 to 400,000 axial scans per second. Opt Express. 2010;18(19):20029–20048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mateo J, Abarzuza R, Núñez E, Cristóbal JA. [Bilateral optic nerve infiltration in acute lymphoblastic leukemia in remission]. Arch Soc Esp Oftalmol. 2007;82:167–170. [DOI] [PubMed] [Google Scholar]
- 10.Birnbaum FA, Meekins LC, Srinivasan A, Murchison AP. A lot of nerve. Surv Ophthalmol. 2020;65:272–277. [DOI] [PubMed] [Google Scholar]
- 11.Alqurashi L, Alqahtani A. Ocular infiltration as the only relapse sign of atypical lymphoma under chemotherapy: a case report. Cureus. 2019;11:e4049. [DOI] [PMC free article] [PubMed] [Google Scholar]


