Abstract
OBJECTIVES:
To investigate racial differences in elevated C-reactive protein (CRP) and the potential factors contributing to these differences in US older men and women.
DESIGN:
Nationally representative cohort study.
SETTING:
Health and Retirement Study, 2006 to 2014.
PARTICIPANTS:
Noninstitutionalized non-Hispanic black and white older adults living in the United States (n = 13 517).
MEASUREMENTS:
CRP was categorized as elevated (>3.0 mg/L) and nonelevated (≤3.0 mg/L) as the primary outcome. Measures for demographic background, socioeconomic status, psychosocial factors, health behaviors, and physiological health were examined as potential factors contributing to race differences in elevated CRP.
RESULTS:
Median CRP levels (interquartile range) were 1.67 (3.03) mg/L in whites and 2.62 (4.95) mg/L in blacks. Results from random effects logistic regression models showed that blacks had significantly greater odds of elevated CRP than whites (odds ratio = 2.58; 95% confidence interval [CI] = 2.20–3.02). Results also showed that racial difference in elevated CRP varied significantly by sex (predicted probability [PP] [white men] = 0.28 [95% CI = 0.27–0.30]; PP [black men] = 0.38 [95% CI = 0.35–0.41]; PP [white women] = 0.35 [95% CI = 0.34–0.36]; PP [black women] = 0.49 [95% CI = 0.47–0.52]) and remained significant after risk adjustment. In men, the racial differences in elevated CRP were attributable to a combination of socioeconomic (12.3%) and behavioral (16.5%) factors. In women, the racial differences in elevated CRP were primarily attributable to physiological factors (40.0%).
CONCLUSION:
In the US older adult population, blacks were significantly more likely to have elevated CRP than whites; and the factors contributing to these differences varied in men and women.
Keywords: C-reactive protein, Health and Retirement Study, race
C-reactive protein (CRP) is a marker of systemic inflammation that has been associated with a wide range of acute and chronic health conditions, including bacterial and viral infections, diabetes, dementia, cardiovascular disease, and mortality.1–7 According to the American Heart Association (AHA) and the US Centers for Disease Control and Prevention (CDC), elevated concentrations of CRP (>3.0 mg/L) have been linked to increased risks of cardiovascular events, particularly in adults with moderate risks of coronary heart disease.2,6,8,9 Although research has increasingly focused on the clinical utility of CRP in risk prediction and disease management, few studies have considered the characteristics and correlates of elevated CRP in older adults at the national level.
Recent studies have shown that non-Hispanic blacks have disproportionately higher levels of CRP than non-Hispanic whites.10–12 There is also evidence to suggest that race differences in CRP vary by sex—with black women exhibiting the highest levels of CRP and white men exhibiting the lowest levels of CRP.11–16 To our knowledge, however, racial differences in elevated CRP have not been studied in a nationally representative sample of US older men and women. More important, the factors contributing to these differences remain largely unknown. Addressing these gaps in knowledge has potentially important implications for clinical practice and identifying vulnerable segments of the population.
The purpose of this study was to provide a population-level investigation of race differences in elevated CRP among US older adults. Using prospective cohort data from a nationally representative sample of older adults from 2006 to 2014, we examined differences in elevated levels of CRP (>3.0 mg/L) in non-Hispanic whites and blacks older than 50 years. The associations were examined separately in men and women and adjusted for demographic background, socioeconomic status, psychosocial factors, health behaviors, and physiological status to identify potential factors contributing to race differences in CRP.
METHODS
Study Population
The study used data from the nationally representative Health and Retirement Study (HRS), an ongoing prospective study of noninstitutionalized adults older than 50 years residing in the contiguous United States. Sponsored by the National Institute on Aging and the Institute for Social Research at the University of Michigan, the HRS began in 1992 and has followed respondents with biennial interviews through 2016.17 In 2006, the HRS began collecting detailed physiologic measures and blood-spot samples in random half samples, with follow-up measures collected for all subjects every 4 years.18 Additional details on the HRS sampling design, study procedures, and response rates have been documented extensively elsewhere.19 All participants provided informed consent, and the study was approved by the University of Michigan Health Sciences Human Subjects Committee.18
Data for the current study included biennial interviews and biomarker data collected from 2006 to 2014.17 Biomarker data from 2016 were not currently available for analysis. The study was limited to non-Hispanic black or white men and women older than 50 years who provided CRP data. Limited sample sizes for other racial/ethnic groups prohibited their analysis in the current study. The final analytic sample included 13 517 participants (5684 men and 7833 women) who contributed 22 557 observations over the study period.
Measurement
Demographic background included age (in years), geographic region (South or other), and place of residence (urban or rural). Socioeconomic factors included education(less than high school or high school/general education diploma or more), household income (in quartiles: ≤$20 000, $20 001-$40 000, $40 001-$75 000, or >$75 000), and health insurance coverage (uninsured, Medicaid only, or insured). Psychosocial factors included marital status (married or not married); number of depressive symptoms, measured by the eight-item Center for Epidemiologic Studies Depression Scale (range = 0–8)20; level of social support (12 items; range = 0–3, with higher scores indicating more support)21,22; level of financial distress (one item; range = 0–4, with higher scores indicating more distress)21,23;level of everyday discrimination (five items; range = 0–5, with higher scores indicating more discrimination)24; and level of neighborhood disorder (eight items; range = 0–6, with higher scores indicating more disorder).25 Behavioral factors included smoking status (never, past,or current smoker),alcohol consumption(none,moderate, or heavy), and physical inactivity in the past month (yes or no). Physiological factors included overweight or obese body mass index(BMI),calculated as weight in kilograms divided by height in meters squared (25.0–29.9 kg/m2 [overweight] or ≥30.0 kg/m2 [obese]); number of limitations in activities of daily living, defined by reported difficulty in getting bathed, dressed, eating, getting in and out of bed, and walking across a room; current use of cholesterol medication (yes or no); and the diagnosis (yes or no) of multiple health conditions (arthritis, hypertension, diabetes, cancer [excluding skin cancer], chronic lung disease, heart disease [coronary heart disease, angina, congestive heart failure, heart attack, or other heart problems], and stroke). With the exception of sex and race, all measures were included as time-varying covariates.
Outcome Measure
High-sensitivity CRP was ascertained from blood samples collected from respondents using dried blood spots (DBS). Blood samples were collected by trained HRS interviewers and were shipped to the University of Vermont or the University of Washington.18 Samples were assayed at the University of Vermont using the BNII nephelometer (Siemens, Inc) and at the University of Washington using the sandwich enzyme-linked immunosorbent assay. To account for potential differences between DBSs and whole blood tests, the CRP measure provided by HRS adjusted DBS values of CRP to equivalent values using a standard assay with whole blood.26 Frequency distributions of CRP values by race and sex are provided in Supplementary Figure S1 and Figure S2. Based on previous research and recommendations by the AHA and CDC, values of CRP were categorized as elevated (>3.0 mg/L) or nonelevated (≤3.0 mg/L) to denote previously documented levels of risk associated with CRP values. High levels of CRP (>10 mg/L) were retained in the current analyses based on previous research27,28 and because preliminary findings were consistent when high values of CRP were excluded from the analyses. Further details of the HRS and CRP measures have been documented elsewhere.29
Statistical Analysis
Distributions of the study variables were computed for men and women by race. Supplementary distributions were also computed by CRP group (provided in Supplementary Tables S1 and S2). Group comparisons were calculated using t tests and χ2 tests, as appropriate. P values were based on two-tailed tests and considered statistically significant at P < .05. Random effects logistic regression models were used to examine race differences in elevated CRP separately in men and women while accounting for the repeated observations (level 1) within HRS participants (level 2) and adjusting for age, geographic region, and urban/rural residence. Population-averaged models (generalized estimating equations) and logistic regression models with clustering were also assessed during preliminary analyses, and the major findings did not change.
The multivariable analyses were conducted in several steps. First, we examined overall race differences in elevated CRP and tested for differences by sex. Second, a series of sex-specific models were estimated with demographic adjustments and the sequential inclusion of socioeconomic, psychosocial, behavioral, and physiological covariates to examine the potential factors contributing to racial differences in elevated CRP in men and women. Predicted probabilities (PPs) were estimated from the adjusted models to demonstrate the differences in elevated CRP for each population subgroup. Finally, we used Karlson-Holm-Breen(KHB)methods to assess the extent to which the individual and combined covariates contributed to racial differences in elevated CRP (ie, percentage confounding/mediating in the nested nonlinear probability models).30
Missing data among study covariates was minimal (<5%) and omitted from the analyses. Sensitivity analyses using multiple imputation methods produced results that were nearly identical to those presented here. All multivariable models adjusted for clustering on individuals to obtain robust SEs. All analyses were conducted using Stata 15 (StataCorp LP).
RESULTS
Tables 1 and 2 present the distributions of study measures by race in men and women, respectively. Median levels (interquartile range) of CRP were 1.48 (2.66) mg/L in white men, 1.99 (3.86) mg/L in black men, 1.82 (3.27) mg/L in white women, and 3.03 (5.53) mg/L in black women. Elevated CRP (>3.0 mg/L) was most prevalent in black women (50.48%) and least prevalent in white men (28.18%). Compared with whites, black participants were more likely to be younger, live in the South, and possess fewer socioeconomic resources. Black men and women had fewer overall psychosocial resources and more psychosocial risks, less favorable health behaviors, and consistently higher rates of hypertension, diabetes, and stroke.
Table 1.
Sample Distributions for Men by Race, Health and Retirement Study (2006 to 2014)
| Total | Black | White | P value | |
|---|---|---|---|---|
| Number of observations (participants) | 9341 (5684) | 1125 (809) | 8216 (4875) | |
| CRP, median (IQR), mg/L | 1.55 (2.79) | 1.99 (3.86) | 1.48 (2.66) | <.001 |
| Elevated CRP | 2738 (29.31) | 423 (37.60) | 2315 (28.18) | <.001 |
| Demographic Background | ||||
| Age, mean (SD), y | 68.42 (10.10) | 65.02 (9.48) | 68.89 (10.10) | <.001 |
| Lives in the South | 3588 (38.41) | 649 (57.69) | 2939 (35.77) | <.001 |
| Rural residence | 4925 (52.72) | 406 (36.09) | 4519 (55.00) | <.001 |
| Socioeconomic Factors | ||||
| Less than HS education | 1136 (12.16) | 302 (26.84) | 834 (10.15) | <.001 |
| Household income | ||||
| ≤ $20,000 | 1117 (11.96) | 333 (29.60) | 784 (9.54) | <.001 |
| $20,001–$40,000 | 2228 (23.85) | 257 (22.84) | 1971 (23.99) | .398 |
| $40,001–$75,000 | 2749 (29.43) | 289 (25.69) | 2460 (29.94) | .003 |
| > $75,000 | 3247 (34.76) | 246 (21.87) | 3001 (36.53) | <.001 |
| Health Insurance | ||||
| Insured | 8795 (94.15) | 937 (83.29) | 7858 (95.64) | <.001 |
| Uninsured | 109 (1.17) | 64 (5.69) | 45 (0.55) | |
| Medicaid-only | 437 (4.68) | 124 (11.02) | 313 (3.81) | |
| Psychosocial Factors | ||||
| Not married | 2285 (24.46) | 468 (41.60) | 1817 (22.12) | <.001 |
| Depressive symptoms, mean (SD) | 1.05 (1.66) | 1.51 (1.88) | 0.99 (1.62) | <.001 |
| Social support, mean (SD) | 2.07 (0.52) | 2.09 (0.58) | 2.07 (0.51) | .217 |
| Financial distress, mean (SD) | 0.86 (0.97) | 1.34 (1.05) | 0.80 (0.94) | <.001 |
| Everyday discrimination, mean (SD) | 0.67 (0.77) | 0.86 (0.94) | 0.64 (0.73) | <.001 |
| Neighborhood disorder, mean (SD) | 1.43 (1.34) | 2.21 (1.54) | 1.32 (1.28) | <.001 |
| Behavioral Factors | ||||
| Smoking | ||||
| Never smoked | 3187 (34.12) | 334 (29.69) | 2853 (34.72) | .001 |
| Past smoking | 4970 (53.21) | 536 (47.64) | 4434 (53.97) | <.001 |
| Current smoking | 1184 (12.68) | 255 (22.67) | 929 (11.31) | <.001 |
| Alcohol consumption | ||||
| No consumption | 4888 (52.33) | 687 (61.07) | 4201 (51.13) | <.001 |
| Moderate consumption | 3173 (33.97) | 272 (24.18) | 2901 (35.31) | <.001 |
| Heavy consumption | 1280 (13.70) | 166 (14.76) | 1114 (13.56) | .274 |
| Physical inactivity | 1279 (13.69) | 152 (13.51) | 1127 (13.72) | .850 |
| Physiological Factors | ||||
| Overweight/obese | 7143 (76.47) | 858 (76.27) | 6285 (76.50) | .864 |
| ADL limitations, mean (SD) | 0.21 (0.66) | 0.28 (0.77) | 0.20 (0.64) | <.001 |
| Cholesterol medication use | 4660 (49.89) | 531 (47.20) | 4129 (50.26) | .055 |
| Diagnoses | ||||
| Arthritis | 5120 (54.81) | 560 (49.78) | 4560 (55.50) | <.001 |
| Hypertension | 5598 (59.93) | 815 (72.44) | 4783 (58.22) | <.001 |
| Diabetes | 2182 (23.36) | 356 (31.64) | 1826 (22.22) | <.001 |
| Cancer | 1692 (18.11) | 181 (16.09) | 1511 (18.39) | .060 |
| Pulmonary disease | 939 (10.05) | 88 (7.82) | 851 (10.36) | .008 |
| Heart disease | 2843 (30.44) | 229 (20.36) | 2614 (31.82) | <.001 |
| Stroke | 696 (7.45) | 104 (9.24) | 592 (7.21) | .015 |
Abbreviations: CRP, C-reactive protein; HS, high school; ADL, activities of daily living.
Note. Values reported as weighted percentages, means (standard deviation [SD]), or median (interquartile range [IQR])
Table 2.
Sample Distributions for Women by Race, Health and Retirement Study (2006 to 2014)
| Total | Black | White | P value | |
|---|---|---|---|---|
| Number of observations (participants) | 13216 (7833) | 2072 (1416) | 11144 (6417) | |
| CRP, median (IQR), mg/L | 1.97 (3.59) | 3.03 (5.53) | 1.82 (3.27) | <.001 |
| Elevated CRP | 4848 (36.68) | 1046 (50.48) | 3802 (34.12) | <.001 |
| Demographic Background | ||||
| Age, mean (SD), y | 67.67 (10.64) | 63.70 (9.57) | 68.41 (10.66) | <.001 |
| Lives in the South | 5280 (39.95) | 1198 (57.82) | 4082 (36.63) | <.001 |
| Rural residence | 7011 (53.05) | 722 (34.85) | 6289 (56.43) | <.001 |
| Socioeconomic Factors | ||||
| Less than HS education | 1510 (11.43) | 429 (20.70) | 1081 (9.70) | <.001 |
| Household income | ||||
| ≤ $20,000 | 2826 (21.38) | 840 (40.54) | 1986 (17.82) | <.001 |
| $20,001–$40,000 | 3594 (27.19) | 547 (26.40) | 3047 (27.34) | .376 |
| $40,001–$75,000 | 3354 (25.38) | 410 (19.79) | 2944 (26.42) | <.001 |
| > $75,000 | 3442 (26.04) | 275 (13.27) | 3167 (28.42) | <.001 |
| Health Insurance | ||||
| Insured | 12224 (92.49) | 1637 (79.01) | 10587 (95.00) | <.001 |
| Uninsured | 307 (2.32) | 175 (8.45) | 132 (1.18) | |
| Medicaid-only | 685 (5.18) | 260 (12.55) | 425 (3.81) | |
| Psychosocial Factors | ||||
| Not married | 5836 (44.16) | 1311 (63.27) | 4525 (40.60) | <.001 |
| Depressive symptoms, mean (SD) | 1.37 (1.92) | 1.80 (2.14) | 1.29 (1.86) | <.001 |
| Social support, mean (SD) | 2.20 (0.52) | 2.19 (0.55) | 2.20 (0.51) | .259 |
| Financial distress, mean (SD) | 0.98 (1.03) | 1.48 (1.08) | 0.89 (0.99) | <.001 |
| Everyday discrimination, mean (SD) | 0.56 (0.71) | 0.73 (0.85) | 0.53 (0.67) | <.001 |
| Neighborhood disorder, mean (SD) | 1.48 (1.36) | 2.31 (1.55) | 1.33 (1.26) | <.001 |
| Behavioral Factors | ||||
| Smoking | ||||
| Never smoked | 6783 (51.32) | 978 (47.20) | 5805 (52.09) | <.001 |
| Past smoking | 4801 (36.33) | 689 (33.25) | 4112 (36.90) | .002 |
| Current smoking | 1632 (12.35) | 405 (19.55) | 1227 (11.01) | <.001 |
| Alcohol consumption | ||||
| No consumption | 8781 (66.44) | 1565 (75.53) | 7216 (64.75) | <.001 |
| Moderate consumption | 3865 (29.24) | 392 (18.92) | 3473 (31.16) | <.001 |
| Heavy consumption | 570 (4.31) | 115 (5.55) | 455 (4.08) | .003 |
| Physical inactivity | 2630 (19.90) | 503 (24.28) | 2127 (19.09) | <.001 |
| Physiological Factors | ||||
| Overweight/obese | 8945 (67.68) | 1739 (83.93) | 7206 (64.66) | <.001 |
| ADL limitations, mean (SD) | 0.22 (0.69) | 0.37 (0.93) | 0.19 (0.63) | <.001 |
| Cholesterol medication use | 5271 (39.88) | 804 (38.80) | 4467 (40.08) | .274 |
| Diagnoses | ||||
| Arthritis | 8790 (66.51) | 1354 (65.35) | 7436 (66.73) | .222 |
| Hypertension | 7802 (59.03) | 1562 (75.39) | 6240 (55.99) | <.001 |
| Diabetes | 2469 (18.68) | 619 (29.87) | 1850 (16.60) | <.001 |
| Cancer | 1984 (15.01) | 199 (9.60) | 1785 (16.02) | <.001 |
| Pulmonary disease | 1504 (11.38) | 207 (9.99) | 1297 (11.64) | .030 |
| Heart disease | 2907 (22.00) | 453 (21.86) | 2454 (22.02) | .863 |
| Stroke | 699 (5.29) | 133 (6.42) | 566 (5.08) | .012 |
Abbreviations: CRP, C-reactive protein; HS, high school; ADL, activities of daily living.
Note. Values reported as weighted percentages, means (standard deviation [SD]), or median (interquartile range [IQR])
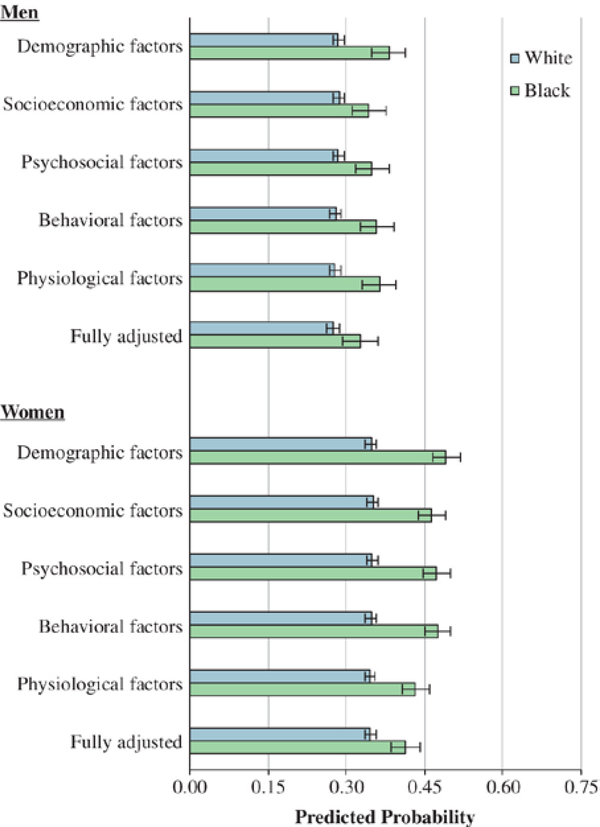
Results from random effects logistic regression models (Table 3) showed that blacks had significantly greater odds of elevated CRP than whites (odds ratio [OR] = 2.58; 95% confidence interval [CI] = 2.20–3.02) after adjustment for age, sex, region, and urban/rural residence. Results also demonstrated that the association between race and elevated CRP differed significantly in men and women (OR for race * sex interaction = 1.55; 95% CI = 1.13–2.12). PPs from the covariate-adjusted models are summarized in Figure 1 (with model estimates provided in Supplementary Tables S3 and S4). In demographic-adjusted models, results showed that blacks had significantly higher PPs of elevated CRP than whites (PP [white men] = 0.28 [95% CI = 0.27–0.30] vs PP [black men] = 0.38 [95% CI = 0.35–0.41]; and PP [white women] = 0.35 [95% CI = 0.34–0.36] vs PP [black women] = 0.49 [95% CI = 0.47–0.52]). The inclusion of covariates attenuated the magnitude of race differences in elevated CRP; however, the associations remained significant in the fully adjusted models for both men and women (PP [white men] = 0.27 [95% CI = 0.26–0.29] vs PP [black men] = 0.33 [95% CI = 0.29–0.36]; and PP [white women] = 0.35 [95% CI = 0.34–0.36] vs PP [black women] = 0.41 [95% CI = 0.39–0.44]).
Table 3.
Adjusted Odds Ratios for Elevated CRP by Race and Sex, Health and Retirement Study (2006 to 2014)
| Model 1 |
Model 2 |
|||||
|---|---|---|---|---|---|---|
| Coefficient (SE) | OR (95% CI) | P value | Coefficient (SE) | OR (95% CI) | P value | |
| Black | 0.95 (0.08) | 2.58 (2.20–3.02) | <.001 | 0.67 (0.13) | 1.95 (1.51–2.52) | <.001 |
| Female | 0.53 (0.06) | 1.70 (1.51–1.90) | <.001 | 0.46 (0.06) | 1.58 (1.40–1.79) | <.001 |
| Black x Female | 0.44 (0.16) | 1.55 (1.13–2.12) | .006 | |||
Abbreviations: CRP, C-reactive protein; SE, standard error; OR, odds ratio; CI, confidence interval.
Note. Models adjusted for age, region, and urban/rural residence.
Figure 1.
Predicted probabilities of elevated C-reactive protein by race in US men and women, Health and Retirement Study (2006–2014). Note. All models adjusted for age, region, and urban/rural residence. Socioeconomic factors included education, household income, and health insurance. Psychosocial factors included marital status, depressive symptoms, social support, financial distress, everyday discrimination, and neighborhood disorder. Behavioral factors included smoking status, alcohol consumption, and physical inactivity. Physiological factors included overweight/obesity, activity of daily living limitations, arthritis, hypertension, diabetes, cancer, chronic lung disease, heart disease, and stroke.
The KHB decomposition of direct and indirect effects (Table 4) showed that the racial differences in elevated CRP among men were attributable to a combination of socioeconomic (12.3%), and behavioral (16.5%) factors. Specifically, low income (16.3%) and current smoking (13.4%) were the major factors contributing to racial differences in CRP among older men in the study. In women, the racial differences in elevated CRP were primarily attributable to physiological factors (40.0%)—with overweight/obesity (24.6%) being the most prominent confounding factor.
Table 4.
Percentage of Association Between Race and Elevated CRP Attributable to Study Covariates in Men and Women, Health and Retirement Study (2006 to 2014)
| Men | Women | |
|---|---|---|
| Socioeconomic Factors | 12.26% | 10.14% |
| Less than H.S. education | 3.26% | 1.74% |
| H.H. income ≤ $20,000 | 15.39% | 8.17% |
| H.H. income $20,001–$40,000 | 2.02% | 0.63% |
| H.H. income $40,001–$75,000 | −1.11% | −1.30% |
| Uninsured | −1.08% | 1.59% |
| Medicaid-only coverage | −6.22% | −0.69% |
| Psychosocial Factors | 9.40% | −1.20% |
| Not married | 0.02% | −4.17% |
| Depressive symptoms | 6.10% | −1.10% |
| Social support | 0.40% | −0.02% |
| Financial distress | 0.67% | 2.76% |
| Everyday discrimination | −0.24% | 0.59% |
| Neighborhood disorder | 2.45% | 0.74% |
| Behavioral Factors | 16.49% | 8.18% |
| Past smoking | −2.39% | −0.83% |
| Current smoking | 13.44% | 1.96% |
| No alcohol consumption | 4.45% | 4.17% |
| Heavy alcohol consumption | −0.50% | −0.01% |
| Physical inactivity | 1.49% | 2.89% |
| Physiological Factors | 9.50% | 39.98% |
| Overweight/obese | −1.46% | 24.62% |
| ADL limitations | 3.62% | 4.00% |
| Cholesterol medication use | −0.47% | −1.57% |
| Arthritis | −0.12% | 0.43% |
| Hypertension | 9.33% | 10.35% |
| Diabetes | 0.07% | 3.23% |
| Cancer | 0.33% | −0.32% |
| Pulmonary disease | −1.33% | −0.78% |
| Heart disease | −1.61% | 0.29% |
| Stroke | 1.14% | −0.27% |
| Total | 47.65% | 57.10% |
Abbreviations: CRP, C-reactive protein; H.S., high school; H.H., household; ADL, activities of daily living.
Note. Models also adjusted for age, region, and urban/rural residence.
DISCUSSION
In this large nationally representative investigation of race differences in elevated CRP among US older adults, we found that black older adults were significantly more likely to have elevated levels of CRP than white older adults. Furthermore, we found that the racial differences in elevated CRP were greater in women than in men and that the associations remained after accounting for a wide range of demographic, socioeconomic, psychosocial, behavioral, and physiological factors. However, we also found that the major factors contributing to the racial differences in CRP varied for men and women.
For men, we found that a combination of socioeconomic and behavioral factors was most attributable to race differences in elevated CRP. In terms of socioeconomic factors, the results showed that low income was the principal factor contributing to elevated CRP in black older men relative to white older men. Interestingly, our findings further suggest that the effect of low income was independent of increased levels of financial distress or inadequate access to important health resources (ie, medical insurance)—which were also included in our analyses. In terms of behavioral factors, we found evidence consistent with prior research showing that current smoking plays an important role in the elevated levels of CRP observed in black older adults.14,31 With more than twice the rate of smoking in blacks compared with whites (22.7% vs 11.3%, respectively), it is possible that older black men may resort to unhealthy behaviors, such as smoking, to cope with their greater exposure to stress.32 Taken together, we encourage additional studies to further examine why socioeconomic and behavioral factors may be contributing to racial differences in CRP among older men.
For women, our study showed that physiological factors (40.0%) had the greatest influence on the relationship between race and elevated CRP. In particular, we found that overweight/obesity was the key factor contributing to this association. These findings support existing research that has suggested a complex interplay among BMI and levels of CRP.33 Moreover, prior studies have shown that disproportionate levels of BMI play a role in the racial variations in CRP among women but not among men.11,12,14 The findings from the present study parallel prior evidence that sex differences in CRP are partly due to higher BMI and because adipose tissue is a mediator of inflammation.11–13,34 Finally, although we also found that socioeconomic factors contributed to race differences in elevated CRP among women, these associations were somewhat less pronounced than what has been previously demonstrated in overall levels of CRP.14
Overall, our study showed that a wide array of socioeconomic, psychosocial, behavioral, and physiological factors accounted for approximately half of the racial variation in elevated CRP in US older men and women. We encourage additional studies to consider other potential factors that may contribute to racial differences in elevated CRP. For example, we suspect that more comprehensive assessments of other factors—such as diet, sleep, acute/chronic stress, segregation, and other neighborhood-related factors—may be important avenues for future research. In addition, it is notable that diagnosed heart disease did not explain racial variations in CRP among men and women It is possible that the self-reported measure of heart disease used in this study did not optimally capture participants’ history of cardiovascular disease.We again encourage future studies to further explore these associations.
Major strengths of this study included the nationally representative sample of older adults, repeated measures of high-sensitivity CRP and multiple covariates over an extended period (8 years), and the direct decomposition of factors contributing to race differences in elevated CRP. Prior studies, particularly among older adults, rarely include longitudinal data; and few have considered clinically meaningful measures of CRP. Most studies have examined continuous measures of CRP (often log transformed) that limit the practical and actionable understanding of the associations to inform their translation to clinical practice. Moreover, this study was unique in that we directly quantified the extent to which a wide array of socioeconomic, psychosocial, behavioral, and physiological factors contributed to racial differences in elevated CRP in men and women.
Despite the strengths of this study, we acknowledge several limitations. First, we remain guarded in the interpretation of the associations from this observational study and caution against causal inference. Although we included longitudinal data to account for individual-level changes in CRP levels and related covariates, our primary objective was to document overall differences in elevated CRP rather than evaluate changes in CRP over time. Second, we recognize that additional unmeasured factors may have played a role in the associations between race and elevated CRP in men and women. For example, the HRS did not provide information on the presence of acute infections, use of anti-inflammatory medications, hormone replacement therapy, neighborhood and environmental conditions, or other salient race-related stressors (eg, segregation) that may have contributed to differences in elevated CRP. Relatedly, our study included self-reported indicators of key measures (eg, disease diagnoses); and we cannot rule out issues of recall or other forms of measurement bias. Finally, the HRS is limited to noninstitutionalized older adults and the findings may not be representative of all US older adults. Likewise, selective mortality—particularly among blacks—also may have influenced the findings.35
CONCLUSION
In a nationally representative sample of US older adults, we found that blacks were significantly more likely to have elevated levels of CRP than whites; and that the major factors contributing to these differences varied in men and women. These findings provided new evidence of racial differences in a clinically relevant measure of inflammation that could potentially be used to identify patients at risk of adverse outcomes. From a population health perspective, our findings may help clinicians to better identify patient groups with elevated CRP, as well as identify key factors for potentially targeted interventions to reduce these risks.
Supplementary Material
Supplementary Table S1: Sample distributions by C-reactive protein in men, Health and Retirement Study (2006-2014).
Supplementary Table S2: Sample distributions by C-reactive protein in women, Health and Retirement Study (2006-2014).
Supplementary Table S3: Adjusted odds ratios (95% confidence intervals) of elevated CRP in men, Health and Retirement Study (2006-2014).
Supplementary Table S4: Adjusted odds ratios (95% confidence intervals) of elevated CRP in women, Health and Retirement Study (2006-2014).
Supplementary Figure S1: Frequency distribution of C-reactive protein levels by race in US men, Health and Retirement Study (2006-2014).
Supplementary Figure S2: Frequency distribution of C-reactive protein levels by race in US women, Health and Retirement Study (2006-2014).
ACKNOWLEDGMENTS
Financial Disclosure: This study was funded in part by the National Institute on Aging Training Grant (T32-AG000029) for Dr Farmer.
Sponsor’s Role: The National Institute on Aging (NIA) had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. The views expressed in this article are those of the authors and do not necessarily reflect those of Duke University or the NIA.
Footnotes
Conflict of Interest: None declared.
SUPPORTING INFORMATION
Additional Supporting Information may be found in the online version of this article.
REFERENCES
- 1.Andreeva E, Melbye H. Usefulness of C-reactive protein testing in acute cough/respiratory tract infection: an open cluster-randomized clinical trial with C-reactive protein testing in the intervention group. BMC Fam Pract. 2014;15(1):80. 10.1186/1471-2296-15-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pearson TA, Mensah GA, Alexander RW, et al. Markers of inflammation and cardiovascular disease application to clinical and public health practice a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2006; 107(3):499–511. 10.1161/01.CIR.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 3.Ryu J-A, Yang JH, Lee D, et al. Clinical usefulness of procalcitonin and C-reactive protein as outcome predictors in critically ill patients with severe sepsis and septic shock. PLoS One. 2015;10(9):e0138150. 10.1371/journal.pone.0138150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kuo H-K, Yen C-J, Chang C-H, Kuo C-K, Chen J-H, Sorond F. Relation of C-reactive protein to stroke, cognitive disorders, and depression in the general population: systematic review and meta-analysis. Lancet Neurol. 2005; 4(6):371–380. 10.1016/S1474-4422(05)70099-5. [DOI] [PubMed] [Google Scholar]
- 5.Kaptoge S, Di Angelantonio E, Lowe G, et al. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet. 2010;375(9709):132–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Buckley DI, Fu R, Freeman M, Rogers K, Helfand M. Clinical guidelines C-reactive protein as a risk factor for coronary heart disease. Ann Intern Med. 2009;151(7):483–495. [DOI] [PubMed] [Google Scholar]
- 7.Straczek C, Ducimetiere P, Barberger-Gateau P, et al. Higher level of systemic C-reactive protein is independently predictive of coronary heart disease in older community-dwelling adults: the three-city study. J Am Geriatr Soc. 2010;58(1):129–135. 10.1111/j.1532-5415.2009.02625.x. [DOI] [PubMed] [Google Scholar]
- 8.Parrinello CM, Lutsey PL, Ballantyne CM, Folsom AR, Pankow JS, Selvin E Six-year change in high-sensitivity C-reactive protein and risk of diabetes, cardiovascular disease, and mortality background single measurements of elevated high-sensitivity C-reactive protein (hs-CRP) are associated with increased. Am Heart J. 2015;170(2):380–389. 10.1016/j.ahj.2015.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mani P, Puri R, Schwartz GG, et al. Association of initial and serial C-reactive protein levels with adverse cardiovascular events and death after acute coronary syndrome: a secondary analysis of the VISTA-16 trial. JAMA Cardiol. 2019;4:314–320. 10.1001/jamacardio.2019.0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nazmi A, Victora CG. Socioeconomic and racial/ethnic differentials of C-reactive protein levels: a systematic review of population-based studies. BMC Public Health. 2007;7:212. 10.1186/1471-2458-7-212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khera A, Mcguire DK, Murphy SA, et al. Race and gender differences in C-reactive protein levels. J Am Coll Cardiol. 2005;46(3):464–469. 10.1016/j.jacc.2005.04.051. [DOI] [PubMed] [Google Scholar]
- 12.Kelley-Hedgepeth A, Lloyd-Jones DM, Colvin A, et al. Ethnic differences in C-reactive protein concentrations. Clin Chem. 2008;54(6):1027–1037. [DOI] [PubMed] [Google Scholar]
- 13.Albert MA, Glynn RJ, Buring J, Ridker PM. C-reactive protein levels among women of various ethnic groups living in the United States (from the Women’s Health Study). Am J Cardiol. 2004;93(10):1238–1242. [DOI] [PubMed] [Google Scholar]
- 14.Herd P, Karraker A, Friedman E. The social patterns of a biological risk factor for disease: race, gender, socioeconomic position, and C-reactive protein. J Gerontol B Psychol Sci Soc Sci. 2012;67 B(4):503–513. 10.1093/geronb/gbs048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cushman M, Mcclure LA, Howard VJ, Jenny NS, Lakoski SG, Howard G.Implications of increased C-reactive protein for cardiovascular risk stratification in black and white men and women in the US. Clin Chem. 2009;55(9): 1627–1636. 10.1373/clinchem.2008.122093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gruenewald TL, Cohen S, Matthews KA, Tracy R, Seeman TE. Association of socioeconomic status with inflammation markers in black and white men and women in the Coronary Artery Risk Development in Young Adults (CARDIA) study. Soc Sci Med. 2009;69:451–459. 10.1016/jsocscimed.2009.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Juster TF, Suzman R. An overview of the Health and Retirement Study.J Hum Resour. 1995;30(Special Issue):S7–S56. https://www.jstor.org/stable/pdf/146277.pdf. Accessed December 18, 2018. [Google Scholar]
- 18.Crimmins E, Kim JK, Kim JK, Weir D. Documentation of Blood-Based Biomarkers in the 2014 Health and Retirement Study. Ann Arbor, MI: Survey Research Center, University of Michigan; 2017. [Google Scholar]
- 19.Health and Retirement Study. A Longitudinal Study of Health, Retirement,and Aging. Sponsored by the National Institute on Aging. http://hrsonline.isr.umich.edu/. Accessed January 29, 2019. [Google Scholar]
- 20.Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Measur. 1977;1(3):385–401. 10.1177/014662167700100306. [DOI] [Google Scholar]
- 21.Smith J, Ryan L, Fisher GG, Sonnega A, Weir D. Psychosocial and Lifestyle Questionnaire 2006–2016 Documentation Report Core Section LB. 2017. https://hrs.isr.umich.edu/sites/default/files/biblio/HRS2006-2016SAQDocumentation_07.06.17_0.pdf. Accessed January 4, 2019.
- 22.Walen HR, Lachman ME. Social support and strain from partner, family,and friends: costs and benefits for men and women in adulthood. J Soc Pers Relat. 2000;17(1):5–30. 10.1177/0265407500171001. [DOI] [Google Scholar]
- 23.Campbell A, Converse PE, Rodgers WL. The Quality of American Life: Perceptions, Evaluations, and Satisfactions. NY, New York: Russell Sage Foundation; 1976. [Google Scholar]
- 24.Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997;2(3):335–351. 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 25.Cagney KA, Glass TA, Skarupsk KA, Barnes LL, Schwartz BS, Mendes de Leon CF. Neighborhood-level cohesion and disorder: measurement and validation in two older adult urban populations. J Gerontol B Psychol Sci Soc Sci. 2009;64B(3):415–424. 10.1093/geronb/gbn041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Crimmins E, Faul J, Kim JK, et al. HRS Documentation Report Documentation of Biomarkers in the 2006 and 2008 Health and Retirement Study. 2013. http://hrsonline.isr.umich.edu/modules/meta/2010/core/qnaire/online/2010PhysicalMeasuresBio. Accessed January 4, 2019.
- 27.Alley DE, Seeman TE, Ki Kim J, Karlamangla A, Hu P, Crimmins EM.Socioeconomic status and C-reactive protein levels in the US population: NHANES IV. Brain Behav Immun. 2006;20(5):498–504. 10.1016/j.bbi.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 28.Hamer M, Chida Y, Stamatakis E. Association of very highly elevated C-reactive protein concentration with cardiovascular events and all-cause mortality. Clin Chem. 2010;56(1):132–135. http://clinchem.aaccjnls.org/content/clinchem/56/1/132.full.pdf. [DOI] [PubMed] [Google Scholar]
- 29.Crimmins EM, Finch CE. Infection, inflammation, height, and longevity. Proc Natl Acad Sci U S A. 2006;103(2):498–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bernt Karlson K, Holm A, Breen R. Comparing regression coefficients between same-sample nested models using logit and probit: a new method. Sociol Methodol. 2012;42:286–313. 10.1177/0081175012444861. [DOI] [Google Scholar]
- 31.Ho JY, Elo IT. The contribution of smoking to black-white differences inU.S. mortality. Demography. 2012;50:545–568. 10.1007/s13524-012-0159-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brondolo E, Monge A, Agosta J, et al. Perceived ethnic discrimination and cigarette smoking: examining the moderating effects of race/ethnicity and gender in a sample of black and Latino urban adults. J Behav Med. 2015;38 (4):689–700. 10.1007/s10865-015-9645-2. [DOI] [PubMed] [Google Scholar]
- 33.Kraus VB, Luta G, Renner JB, Dragomir AD, Jordan JM. Interpretation of serum C-reactive protein (CRP) levels for cardiovascular disease risk is complicated by race, pulmonary disease, body mass index, and osteoarthritis. Osteoarthr Cartil. 2007;15:966–971. 10.1016/j.joca.2007.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Albert MA, Ridker PM. C-reactive protein as a risk predictor: do race/ethnicity and gender make a difference? Circulation. 2006;114(5):67–75. 10.1161/CIRCULATIONAHA.106.613570. [DOI] [PubMed] [Google Scholar]
- 35.Stewart QT. The shape of inequality: racial disparities in age-specific mortality. Biodemography Soc Biol. 2010;54(2):152–182. 10.1080/19485565.2008.9989140. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Table S1: Sample distributions by C-reactive protein in men, Health and Retirement Study (2006-2014).
Supplementary Table S2: Sample distributions by C-reactive protein in women, Health and Retirement Study (2006-2014).
Supplementary Table S3: Adjusted odds ratios (95% confidence intervals) of elevated CRP in men, Health and Retirement Study (2006-2014).
Supplementary Table S4: Adjusted odds ratios (95% confidence intervals) of elevated CRP in women, Health and Retirement Study (2006-2014).
Supplementary Figure S1: Frequency distribution of C-reactive protein levels by race in US men, Health and Retirement Study (2006-2014).
Supplementary Figure S2: Frequency distribution of C-reactive protein levels by race in US women, Health and Retirement Study (2006-2014).