Abstract
Bisexual women report more physical and psychological health problems than lesbian women do, which may be attributed to greater sexual minority stress and less social support. However, many studies combine lesbian and bisexual women into a single group. The current study examined if sexual minority stress and social support mediated the association between women’s sexual identity (lesbian or bisexual) and health-related outcomes. A total of 650 U.S. young adult lesbian (n = 227) and bisexual (n = 423) women completed an online survey about sexual minority stress, social support, and physical and mental health problems. Bisexual women reported more physical and mental health problems. A sequential mediation model showed that bisexual women reported greater sexual minority stress than lesbian women, which in turn was associated with less social support, which was associated with more physical and mental health problems. Greater sexual minority stress and lower social support may help explain why bisexual women report more health-related problems than lesbian women. The results of the present study support the importance of examining risk and protective factors for health problems separately for lesbian and bisexual women. Health-related intervention programs that target sexual minority women may need to be tailored differently for lesbian and bisexual women.
Keywords: sexual minority groups, lesbian, bisexual, minority stress, health outcomes, social support
Sexual minority women (SMW) in the United States report higher rates of depression, anxiety, posttraumatic stress disorder, suicidal thoughts, hazardous drinking, and self-injury than heterosexual women (Cochran, Sullivan, & Mays, 2003; Gilman et al., 2001; Hughes, Johnson, Steffen, Wilsnack, & Everett, 2014; Kerr, Santurri, & Peters, 2013). For example, results from the 2012 to 2013 U.S. National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) showed that, compared to heterosexual women, lesbian and bisexual women were nearly twice as likely to be diagnosed with a mood disorder in the past year (Kerridge et al., 2017). Further, compared to heterosexual women, SMW are more likely to be diagnosed with comorbid mental health problems (Cochran et al., 2003). In addition to mental health, rates of physical health problems such as obesity, disability, and gastrointestinal conditions are higher among SMW women than heterosexual women (Bowen, Balsam, & Ender, 2008; Conron, Mimiaga, & Landers, 2010; Dyar et al., 2019; Fredriksen-Goldsen, Kim, & Barkan, 2012). Findings from the U.S. National Health Interview Survey (NHIS) indicate that compared to heterosexual women, SMW were more likely to report multiple chronic health conditions (e.g., asthma, cancer; Gonzales, Przedworski, & Henning-Smith, 2016). However, few studies have examined differences between subgroups of SMW (e.g., lesbian versus bisexual women). Given the elevated rates of mental and physical health problems among SMW, the aim of the current study is to address the critical need to identify risk and protective factors that may contribute to these health disparities separately for lesbian and bisexual women.
Many studies examining health disparities consider lesbian and bisexual women as a single SMW group. However, the U.S. Institute of Medicine (2011) emphasized the need to examine risk factors and health disparities separately among lesbian and bisexual women. Bisexual women report significantly higher rates of anxiety, depression, suicidality, and negative affect compared to lesbian women (Ross et al., 2018; Salway et al., 2019). In addition, results from the NESARC demonstrate that approximately 37% of bisexual women were diagnosed with any mood disorder in the past year, which exceeded rates of both lesbian (25%) and heterosexual (16%) women (Kerridge et al., 2017). Clearly, mental health disparities exist between lesbian and bisexual women.
Although relatively less is known about physical health disparities, important differences between these subgroups of SMW have emerged. For example, based on population data in Washington state, bisexual women reported poorer general health, were less likely to have health insurance coverage, and were more likely to experience financial stress for covering healthcare services compared to lesbian women (Fredriksen-Goldsen, Kim, Barkan, Balsam, & Mincer, 2010). Furthermore, results based on national population data (i.e., the NESARC) show that adult bisexual women reported lower health-related quality of life than heterosexual women (Dyar et al., 2019). Collectively, these results suggest that although SMW in general are more likely than heterosexual women to experience mental and physical health problems, bisexual women may be at the greatest risk.
Sexual Minority Stress
In order to enhance targeted interventions or prevention programs, it is important to identify mechanisms or risk factors specific to SMW that may be associated with negative health outcomes. According to minority stress theory, SMW may experience discrimination as a result of their sexual minority status in society, creating heightened stress and potentially leading to psychological distress (Meyer, 2003). Sexual minority stress has been associated with mental health disorders (e.g., depression and anxiety), suicidal thoughts, and general psychological distress for same-sex attracted men and women as well as self-identified lesbian, gay, and bisexual adults (Bostwick, Boyd, Hughes, West, & McCabe, 2014; Lea, de Wit, & Reynolds, 2014; Lehavot & Simoni, 2011; Lewis, Derlega, Griffin, & Krowinski, 2003; Szymanski, Dunn, & Ikizler, 2014). Additionally, sexual minority stress has been associated with more physical health problems and less engagement in a health-promoting lifestyle among an online sample of sexual minority men and women (Flenar, Tucker, & Williams, 2017). Further, sexual minority adults who experienced sexual minority stress were approximately three times more likely to develop a physical health problem during a one-year period compared to those who did not experience sexual minority stress (Frost, Lehavot, & Meyer, 2015).
Bisexual women may experience more sexual minority stress than lesbian women. Specifically, due to their sexual attractions and potential relationships with both men and women, bisexual women may experience discrimination from both heterosexual and other sexual minority individuals resulting in stress (Dyar, Feinstein, & London, 2015). Sexual minority stressors can be categorized as distal (e.g., experiences of discrimination and stigmatization) or proximal (e.g., internalized negativity about one’s sexual identity, concealment of sexual identity; Meyer, 2003). The current study focuses on proximal stressors. Bisexuality is sometimes perceived as an illegitimate or a temporary sexual orientation (Bostwick & Hequembourg, 2014; Ross, Dobinson, & Eady, 2010; Wandrey et al., 2015) that may create internal stress for bisexual women. That is, bisexual women may be aware of this stigma and perception from others about their sexual identity which may influence their worry or concern that others will judge them for identifying as bisexual. Similarly, bisexual individuals who were more concerned about being accepted were less likely to disclose their sexual identity to family members and others (Mohr, Jackson, & Sheets, 2017). As such, bisexual individuals may conceal their sexual identity for many reasons, one of which could be concerns about reactions from others. As a result of these proximal stressors, bisexual women may develop greater negative attitudes about their sexual identity (i.e., internalized homonegativity) relative to lesbian women (Sarno & Wright, 2013).
Another type of proximal minority stress is identity uncertainty. Bisexual adult men and women reported higher levels of identity uncertainty than gay men and lesbian women (Balsam & Mohr, 2007; Sarno & Wright, 2013). Similarly, among SMW specifically, bisexual women reported higher levels of identity uncertainty than lesbian women (Dyar et al., 2015). Further, among nonmonosexual (i.e., those with attractions toward more than one gender such as bisexual, pansexual, omnisexual, etc.) individuals, greater identity uncertainty was associated with more frequently being assumed to be lesbian/gay (Dyar, Feinstein, Schick, & Davila, 2017). It is important to note that bisexual women may not necessarily be more confused about their sexual identity, but instead they may be mistaken to be a lesbian woman due to the assumption that bisexuality is just a phase or temporary (Ross et al., 2010). As a result of this assumption, bisexual women may question the validity of their identity. Collectively, these findings indicate that bisexual women may experience more proximal stressors than lesbian women.
Experiencing more minority stress than lesbian women may be associated with greater mental health problems among bisexual women. For example, among a sample of bisexual adult women, those who perceived greater discrimination about their bisexual orientation from both heterosexual and gay/lesbian individuals reported more symptoms of depression (Lambe et al., 2017). In addition, bisexual women report experiencing stigma from lesbian women and gay men because of perceptions regarding sexual irresponsibility (e.g., obsessed with sex due to being bisexual) and hostility (e.g., people not wanting to be their friend because of being bisexual). Bisexual women who reported greater sexual stigma and hostility also reported more depressive symptoms (Dyar, Feinstein, & London, 2014). Thus, compared to lesbian women, bisexual women may experience more sexual minority stress, which could in turn be associated with greater health problems.
Social Support
Because most examinations of SMW’s disparities focus on sexual minority stress and negative health outcomes, it is also important to consider potential protective aspects of SMW’s experiences. For instance, according to the buffering hypothesis, social support may serve as a protective mechanism against negative outcomes when a person experiences stress (Cohen & Wills, 1985). That is, SMW may turn to coping resources such as social support when they experience stressful situations (see Chaudoir, Wang, & Pachankis, 2017). However, sexual minority individuals perceive less social support compared to heterosexual individuals (Jorm et al., 2002; Safren & Pantalone, 2006), suggesting that they may be more susceptible to the negative implications of minority stress. Therefore, it is important to examine whether perceived social support might explain the association (i.e., mediate) between minority stress and negative health outcomes. Although some research has found that there are no differences between bisexual individuals and lesbian women/gay men on social support (Balsam & Mohr, 2007; Jorm et al., 2002).
However, a notable limitation of this literature is that health-related factors, including social support, are typically not examined within SMW subgroups (i.e., comparisons between lesbian and bisexual women), perhaps due to limited sample sizes and a lack of power. Additionally, research indicates that among sexual minority adults, those who experienced more discrimination, concealment of their sexual identity, and internalized homonegativity reported lower social support (Balsam & Mohr, 2007; Friedman & Leaper, 2010; Lehavot & Simoni, 2011). Experiencing greater sexual minority stress may impact how much perceived social support is available to them. Specifically, if SMW experience greater sexual minority stress, they may feel more withdrawn and isolated, which in turn could impact how much social support they seek out and perceive. Because bisexual women may experience more sexual minority stress than lesbian women, they also may report the lowest perceived social support. Thus, one plausible (but untested) explanation for why bisexual women report more health problems when compared to both lesbian and heterosexual women is due to the process of experiencing more sexual minority stress, which then may lower perceived social support.
Limited research exists that examines differences between lesbian and bisexual women on sexual minority stress experiences, social support, and negative health outcomes in a single model. Additionally, another gap in the literature is the specific focus on young SMW. Studies have explored minority stress and health outcomes during adulthood more generally, but less research focuses on young adulthood specifically. Young adulthood may be a particularly important developmental period for SMW because this is when they may acknowledge their sexual minority identity and same-sex attractions and engage in same-sex sexual behaviors (Katz-Wise et al., 2017). Therefore, the current study will test a sequential mediation model to examine if proximal sexual minority stress related to negative identity and social support mediate the association between sexual identity (i.e., lesbian or bisexual) and physical and mental health problems among young adult SMW. We hypothesized that compared to lesbian women, bisexual women will report more sexual minority stress, which in turn will be associated with less social support and which then will be associated with greater physical and psychological health problems.
Method
Participants
Participants were 650 young adult lesbian (n = 227) and bisexual (n = 423) U.S. women who were part of a larger study that examined health behaviors of SMW. Eligibility criteria included self-identifying (a) as exclusively lesbian/gay or bisexual, (b) as cisgender female, and (3) as 18–30 years-old. Demographic information for the sample is displayed in Table 1. For the overall sample, participants were on average 22.69 years old (SD = 3.44). Additionally, the majority of participants were White (n = 463, 71.2%), single (n = 309, 47.5%) or in a relationship/married (n = 316, 48.6%), employed full or part time (n = 334, 51.4%), and completed some college (n = 360, 55.5%).
Table 1.
Demographic Information for Lesbian and Bisexual Women
| Total Sample
(n = 650) |
Lesbian Women
(n = 227, 34.9%) |
Bisexual Women
(n = 423, 65.1%) |
||||
|---|---|---|---|---|---|---|
| M or n | SD or % | M or n | SD or % | M or n | SD or % | |
| Agea | 22.69 | 3.44 | 23.52 | 3.65 | 22.26 | 3.24 |
| Race/ethnicitya | ||||||
| White | 463 | 71.2% | 159 | 71.3% | 304 | 74.1% |
| Black | 82 | 12.6% | 31 | 13.9% | 51 | 12.4% |
| Other | 88 | 13.5% | 33 | 14.8% | 55 | 13.4% |
| Hispanic/Latina (yes)a | 107 | 16.5% | 40 | 17.6% | 67 | 15.8% |
| Relationship status | ||||||
| Single | 309 | 47.5% | 87 | 38.3% | 222 | 52.5% |
| In a relationship/Married | 316 | 48.6% | 134 | 59.0% | 182 | 43.0% |
| Other | 25 | 3.9% | 6 | 2.7% | 19 | 4.5% |
| Employment Status | ||||||
| Employed full/part time | 334 | 51.4% | 136 | 59.9% | 198 | 46.8% |
| Student | 249 | 38.3% | 73 | 32.2% | 176 | 41.6% |
| Unemployed | 67 | 10.3% | 18 | 7.9% | 49 | 11.6% |
| Highest Education Levela | > | |||||
| < High school diploma | 24 | 3.7% | 7 | 3.1% | 17 | 4.0% |
| High school diploma | 89 | 35 | 15.5% | 54 | 12.8% | |
| Some college | 360 | 55.5% | 115 | 50.9% | 245 | 58.0% |
| Bachelor’s degree | 133 | 20.5% | 46 | 20.4% | 87 | 20.6% |
| Master’s/Doctoral degree | 43 | 6.6% | 23 | 10.1% | 20 | 4.6% |
| Income | ||||||
| ≤ $9,999 | 307 | 48.2% | 86 | 38.9% | 221 | 53.2% |
| $10,000 - $19,999 | 139 | 21.8% | 44 | 19.9% | 95 | 22.8% |
| $20,000 - $29,999 | 80 | 12.6% | 32 | 14.5% | 48 | 11.6% |
| $30,000 - $39,999 | 57 | 8.9% | 28 | 12.6% | 29 | 7.0% |
| $40,000 + | 54 | 8.5% | 31 | 14.1% | 23 | 5.4% |
Variable has missing data.
Procedure and Measures
Participants were recruited for a 30-minute online survey through Facebook (n = 579, 89.1%), listservs (n = 14, 2.2%), and other sources (e.g., Craigslist, friends of participants, n = 56, 8.6%). One participant did not report how she learned about the study. Paid Facebook advertisements which stated “Study for [Bisexual or Lesbian] women aged 18–30! Chance to win one of several Amazon.com gift cards!” ran on Facebook and Instagram for a total of 5 days. To optimize recruitment of SMW, profiles of individuals who showed interest in LGBT-related pages and who indicated they were interested in relationships with women were targeted. Participants were offered the opportunity to enter a raffle to win one $50 Amazon gift card, or one of five $25 Amazon gift cards, or one of ten $10 Amazon gift cards for compensation. All procedures were approved by the participating university’s Institutional Review Board. In addition to other measures about health behaviors and experiences, participants completed the following scales in the following order.
Social support
The Multidimensional Scale of Perceived Social Support (MSPSS; Zimet, Dahlem, Zimet, & Farley, 1988) is a 12-item measure used to examine perceived social support. Participants responded to each item, such as “My friends really try to help me.” to indicate their perceived social support using a 1 (very strongly disagree) to 7 (very strongly agree) response scale. The mean of all items was computed, with higher scores indicating more perceived social support (αbisexual = .89, αlesbian = .88). Validity was established in prior research by demonstrating no association between the MSPSS and social desirability (Dahlem, Zimet, & Walker, 1991) and inverse modest correlations with depression and anxiety (Zimet et al., 1988).
Physical health
The Cohen-Hoberman Inventory of Physical Symptoms (CHIPS; Cohen & Hoberman, 1983) assessed physical health problems in the past 2 weeks. Participants responded to 33 items about how bothered they were by various physical health problems using a scale of 0 (not at all bothered) to 4 (extremely bothered). Two sample items are: “sleep problems” and “weight change.” A total score for physical health problems was created by summing all responses, with higher scores indicating greater physical health problems (αbisexual = .90, αlesbian = .93). Among adults in same-sex relationships, the CHIPS (greater physical health problems) was negatively correlated (r = −.71) with general self-rated physical health (i.e., lower self-rated physical health; Blair & Holmberg, 2008). Sexual minority stress. The Lesbian, Gay, and Bisexual Identity Scale (LGBIS; Mohr & Kendra, 2011) assessed sexual minority stress. The LGBIS contains eight subscales, but similar to prior research (Bregman, Malik, Page, Makynen, & Lindahl, 2013), only five that measure negative identity were selected for the current study: Acceptance Concerns (3 items; αbisexual = .71, αlesbian = .78; a sample item is: “I often wonder whether others judge me for my sexual orientation.”), Concealment Motivation (3 items; αbisexual = .76, αlesbian = .79; a sample item is: “I prefer to keep my same-sex romantic relationships rather private.”), Identity Uncertainty (4 items; αbisexual = .83, αlesbian = .83; a sample item is: “I’m not totally sure what my sexual orientation is.”), Internalized Homonegativity (3 items; αbisexual = .82, αlesbian = .87; a sample item is: “If it were possible, I would choose to be straight.”), and Difficult Process (3 items; αbisexual = .79, αlesbian = .81; a sample item is: “Admitting to myself that I’m an LGB person has been a very slow process.”). Participants indicated how much they agree with each item using a response scale of 1 (disagree strongly) to 6 (agree strongly). The sample item for the Difficult Process subscale reported here was reverse scored. The mean of each subscale was computed, with higher scores indicating greater sexual minority stress. The LGBIS has shown good convergent validity, internal consistency, and test-retest reliability among lesbian/gay and bisexual college students (Mohr & Kendra, 2011).
Mental health
An 18-item version of the Mental Health Inventory (MHI; Veit & Ware, 1983; Weinstein, Berwick, Goldman, Murphy, & Barsky, 1989) was used to examine psychological distress in the past 4 weeks. Participants indicated how often they experienced each symptom (e.g., “Did you feel depressed?” and “Were you able to relax without difficulty?”) in the past 4 weeks using a scale of 1 (all of the time) to 6 (none of the time). Consistent with previous studies (Cokley, McClain, Enciso, & Martinez, 2013; Whittaker & Neville, 2010), 10 items were reverse scored and the mean of all items was computed into a single raw total score. Next, raw scores were transformed into standardized scores that range from 0 to 100 (αbisexual = .94, αlesbian = .94). Scoring of the items was computed so higher scores indicated greater psychological distress. The MHI-18 has shown good discriminant validity between physical and mental health problems (Veit & Ware, 1983).
Analysis Plan
Descriptive information was generated, and bivariate and multivariate analyses were conducted in SPSS. Structural equation modeling (SEM) was conducted using Mplus 7.4 (Muthen & Muthen, 1998–2017) to analyze the hypothesized model. Approximately 14% of the data were missing, and missing data were handled using full information maximum likelihood. In order to model negative identity experiences and create the most parsimonious model, first, we tested the measurement model of sexual minority stress to examine measurement fit statistics of the latent variable. We used recommendations by Hu and Bentler (1999) to examine overall model fit: non-significant Chi-square test of model fit, comparative fit index (CFI) > .95, root mean square error of approximation (RMSEA) < .06, and standardized root mean square residual (SRMR) < .08 would indicate “good” fit. Next, we fit a single, sequential mediation model where the exogenous variable was sexual orientation identity (0 = lesbian, 1 = bisexual), mediator variables were sexual minority stress (latent variable of LGBIS subscales) and social support, and outcome variables were physical health (CHIPS) and mental health (MHI-18) problems.
Demographic variables were explored as potential covariates to determine if they were associated with the mediators and outcome variables of the sequential mediation model. Age was significantly associated with social support (r = .13, p = .001), mental health problems (r = −.17, p < .001), and physical health problems (r = −.13, p = .001). Additionally, race/ethnicity was significantly associated with social support, F(2, 630) = 3.58, p = .028, ηp2 = .010, and mental health problems, F(2, 542) = 3.16, p = .043, ηp2 = .009; relationship status was significantly correlated with social support, F(2, 647) = 14.08, p = .001, ηp2 = .027, and mental health problems, F (2,557) = 7.53, p < .001, ηp2 = .006; and employment was significantly associated with social support, F(2, 631) = 6.39, p = .012, ηp2 = .004, and mental health problems, F(2, 543) = 6.31, p = .012, ηp2 = .010. Therefore, the sequential mediation model controlled for age, race/ethnicity, relationship status, and employment status for relevant outcomes and mediators (i.e., those with significant associations). To test significance of the indirect effects, 95% bias-corrected bootstrapped confidence intervals (CIs) were generated (using 10,000 samples). If the CI did not include 0, the path was determined to be significant at the .05 level.
Results
For descriptive purposes of the sample, ANOVA analyses revealed that lesbian women were significantly older than bisexual women, F(1, 624) = 19.62, p < .001. Additionally, Chi-square analyses revealed that there were differences between lesbian and bisexual women on relationship status, χ2(2) = 15.32, p < .001, ϕ = .15, employment, χ2(2) = 10.29, p = .006, ϕ = .13, and income, χ2(4) = 25.14, p < .001, ϕ = .20. However, there were no differences between lesbian and bisexual women on race/ethnicity, χ2(2) = 0.60, p = .742, Hispanic ethnicity, χ2(1) = 0.40, p = .528, or education, χ2(4) = 9.05, p = .060.
Analyses of Covariance (ANCOVAs) examined differences between lesbian and bisexual women on social support, physical and mental health problems, and the LGBIS subscales. Results are shown in Table 2 and reveal that compared to lesbian women, bisexual women reported significantly more physical health problems, mental health problems, identity uncertainty, and concealment motivation. Correlation analyses were conducted separately for lesbian and bisexual women and showed that physical health problems were significantly associated with mental health problems (lesbian women: r = .40, p < .001; bisexual women: r = .45, p < .001) and social support (lesbian women: r = −.15, p = .029; bisexual women: r = −.19, p < .001) and that mental health problems were significantly associated with social support (lesbian women: r = −.34, p < .001; bisexual women: r = −.37, p < .001).
Table 2.
Comparisons of Lesbian and Bisexual Women on Study Variables
| Lesbian Women
(n = 227) |
Bisexual Women
(n = 423) |
Group Comparisons |
|||||
|---|---|---|---|---|---|---|---|
| adj. M | SE | adj. M | SE | F (df) | p | ηp2 | |
| Physical Health Problems | 33.26 | 1.50 | 37.67 | 1.08 | 5.63 (1, 623) | .018 | .009 |
| Mental Health Problems | 43.41 | 1.36 | 51.16 | 1.02 | 20.42 (1, 520) | <.001 | .038 |
| Social Support | 5.38 | 0.07 | 5.22 | 0.05 | 3.31 (1, 603) | .070 | .005 |
| LGBIS subscales | |||||||
| Difficult Process | 3.06 | 0.09 | 3.05 | 0.07 | 0.003 (1, 629) | .960 | .000 |
| Internalized Homonegativity | 1.70 | 0.07 | 1.66 | 0.05 | 0.25 (1, 622) | .621 | .000 |
| Identity Uncertainty | 1.47 | 0.07 | 2.06 | 0.05 | 52.62 (1, 621) | <.001 | .078 |
| Concealment Motivation | 2.53 | 0.08 | 3.15 | 0.06 | 39.71 (1, 629) | <.001 | .059 |
| Acceptance Concerns | 0.46 (1, 605) | .499 | .001 | ||||
Note. LGBIS = Lesbian, Gay, and Bisexual Identity Scale. ANCOVA models for physical health problems, mental health problems, and social support control for relevant covariates mentioned in the Analysis Plan section. For the LGBIS subscales, age was controlled for in the internalized homonegativity, identity uncertainty, and acceptance concerns model; race/ethnicity was controlled for in the difficult process and acceptance concerns model; relationship status was controlled for in the internalized homonegativity, identity uncertainty, and concealment motivation models; and employment was controlled for in the difficult process and identity uncertainty models.
Measurement Model of Sexual Minority Stress
A single latent variable for sexual minority stress was created using the LGBIS subscales associated with negative identity: Acceptance Concerns, Concealment Motivation, Identity Uncertainty, Internalized Homonegativity, and Difficult Process. A confirmatory factor analysis (CFA) was conducted to examine the appropriateness of using each observed LGBIS subscale score as an indicator for the latent variable of sexual minority stress. The measurement model for sexual minority stress showed good model fit, χ2(5) = 12.14, p = .033 (CFI = .98; RMSEA = .05, p = .504; and SRMR = .02). Standardized factor loadings of observed subscale scores on the sexual minority stress latent variable were: Acceptance Concerns = 0.61, Concealment Motivation = 0.55, Identity Uncertainty = 0.46, Internalized Homonegativity = 0.49, and Difficult Process = 0.63.
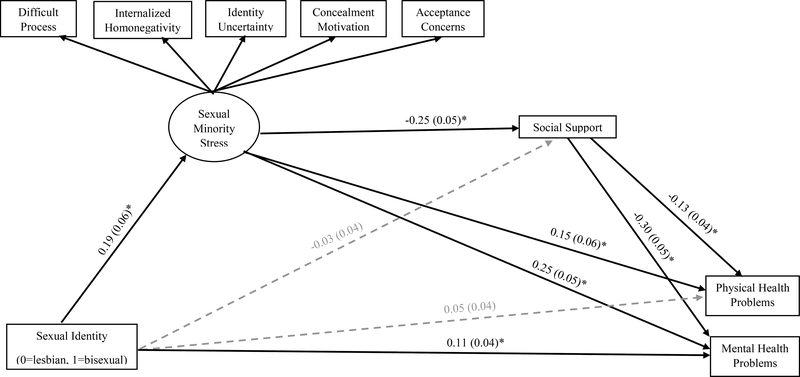
Sequential Mediation Model
After fitting the measurement model, structural paths were added to test the model that sexual minority stress and social support would mediate the association between sexual identity with physical and mental health problems. Direct and indirect pathways are shown in Table 3 and Figure 1. There was a significant indirect association (indirect effect not shown in the table) between sexual identity and physical health problems (indirect effect: β = 0.01; B = 0.28, unstandardized 95% CI [0.08, 0.72]) and mental health problems (indirect effect: β = 0.01; B = 0.57, unstandardized 95% CI [0.21, 1.19]) through sexual minority stress and social support. Consistent with our hypothesis, bisexual women reported greater sexual minority stress than lesbian women, sexual minority stress was associated with lower social support, and lower social support was associated with more physical and mental health problems. There was not a significant direct effect of sexual identity on physical health problems after controlling for covariates, and the indirect effects through sexual minority stress and social support also were not significant. However, sexual identity had a significant direct association with mental health problems, indicating that bisexual women reported greater mental health problems, even after controlling for covariates and indirect effects through sexual minority stress and social support.
Table 3.
Summary of Path Coefficients of Sexual Minority Stress and Social Support as Mediators between the Association of Sexual Identity and Physical and Mental Health
| β | B | 95% CI for B | |
|---|---|---|---|
| Path a1 | |||
| Sexual Identity → SMS | 0.19* | 0.29 | [0.12, 0.44] |
| Path d | |||
| SMS → Social Support | −0.25* | −0.37 | [−0.54, −0.22] |
| Path b2 | |||
| Social Support → Physical Health Problems | −0.13* | −2.59 | [−4.35, −0.87] |
| Social Support → Mental Health Problems | −0.30* | −5.34 | [−6.95, −3.65] |
| Path c’ | |||
| Sexual Identity → Physical Health Problems | 0.05 | 2.51 | [−1.50, 6.10] |
| Sexual Identity → Mental Health Problems | 0.11* | 4.35 | [1.22, 7.46] |
| Path a2 | |||
| Sexual Identity → Social Support | −0.03 | −0.07 | [−0.25, 0.11] |
| Path b1 | |||
| SMS → Physical Health Problems | 0.15* | 4.53 | [1.05, 8.50] |
| SMS → Mental Health Problems | 0.25* | 6.53 | [3.85, 9.30] |
Note. SMS = sexual minority stress latent variable. Sexual identity: 0 = lesbian, 1 = bisexual. Model controlled for age, race/ethnicity, relationship status, and employment status.
p < .05.
Figure 1.
Sequential mediation model results of sexual minority stress and social support mediating the association between sexual identity and physical and mental health. Standardized beta coefficients reported, with standard errors in parentheses. Paths reaching statistical significance are indicated with solid black lines; non-significant paths are indicated with dashed grey lines. *p < .05.
Discussion
Minority stress theory suggests that SMW may have more health problems due to stressors related to their sexual identity (Meyer, 2003). The current study examined differences in health-related outcomes among lesbian and bisexual women and explored if sexual minority stress related to negative identity experiences and social support mediated the association between sexual identity (i.e., lesbian or bisexual) and physical and mental health problems. Our test of a sequential mediation model offers information regarding potential underlying mechanisms of the association between sexual identity and health outcomes. Consistent with our predictions, bisexual women reported more sexual minority stress than lesbian women, which was in turn associated with lower social support, which then was associated with more physical and mental health problems.
These findings add to the literature in several important ways. Consistent with previous research (Bostwick et al., 2010; Dyar et al., 2019; Fredriksen-Goldsen et al., 2010; Hughes et al., 2014; Kerr et al., 2013; Kerridge et al., 2017), our findings revealed that bisexual women reported more mental and physical health problems than lesbian women. To elucidate why bisexual women may experience more negative health-related outcomes, we also examined differences on proximal minority stressors related to negative identity. When examining the individual sexual minority stress subscales, two scales were significantly different for lesbian and bisexual women. Compared to lesbian women, bisexual women reported greater identity uncertainty and concealment motivation. Bisexual women report feeling as though heterosexual and gay/lesbian individuals perceive them as being “confused” or bisexuality as a “temporary phase” (Bostwick & Hequembourg, 2014; Ross et al., 2010; Wandrey et al., 2015). Therefore, bisexual women may question the validity or attempt to hide their sexual identity to avoid stigma due to these negative assumptions.
However, it is important to note that this assumption that a bisexual identity is a “phase” is contradictory to research showing that bisexuality is stable across time (Diamond, 2008). Although there were no differences on the difficult process, internalized homonegativity, and acceptance concern subscales, to capture multiple forms of negative identity experiences, the present study created a single latent variable of sexual minority stress. Results revealed that compared to lesbian women, bisexual women reported greater sexual minority stress (i.e., higher scores on the negative identity variable). Thus, the negative identity experiences that bisexual women experience may be one factor that increases their risk for negative health outcomes such as mental and physical health problems.
Findings from the current study support minority stress theory (Meyer, 2003), which may be one reason why bisexual women report greater health problems than lesbian women. Specifically, bisexual women reported more sexual minority stressors related to negative identity experiences which were associated with greater mental health problems. As we stated previously, the internal processes of the minority stressors that bisexual women experience may contribute to greater psychological distress. Expanding upon prior findings, results from the current study showed that greater sexual minority stress was associated with more physical health problems. It could be that bisexual women are more apprehensive than lesbian women about seeking medical attention due to previous negative experiences related to their sexual identity from medical professionals. Prior research has shown that physicians hold the greatest negative attitudes toward bisexual individuals, relative to transgender, lesbian, and gay individuals (Jabson, Mitchell, & Doty, 2016). Therefore, even if unintentional, those in the medical field may treat bisexual patients differently than other heterosexual or sexual/gender minority patients which may impact the internal processes of bisexual individuals. Furthermore, bias about female patients may be particularly problematic. Medical research has historically focused on illnesses from a male perspective and negative stereotypes of female patients have been found to influence treatment and diagnosis (see Verdonk, Benschop, de Haes, & Largo-Janssen, 2009 for a review). Taken together, bisexual women may be the most likely to have previously had a negative experience with a medical professional related to both their sexual identity and sex/gender. Because of these previous experiences, bisexual women may be reluctant to seek treatment which could exacerbate their physical health problems.
In the current study, sexual minority stress was also negatively associated with social support. Past research suggests the most common form of coping with sexual minority stress among bisexual and non-monosexual adults is seeking social support from friends, family, partners, and other LGBTQ community affiliations (Doan Van, Mereish, Woulfe, & Katz-Wise, 2019). Thus, those SMW who experience more sexual minority stress may be more reluctant to seek social support from these individuals due to internal processes and fear of their reactions. Further, bisexual women who experience more sexual minority stress may have the lowest perceived social support. Qualitative research has documented that young bisexual women are more open to seeking social support from other bisexual men and women than other sexual minority individuals (e.g., lesbian women, gay men; Wandrey et al., 2015). However, seeking social support from other bisexual individuals would require having an established social network of bisexual peers which may be challenging if those who identity as bisexual report more negative identity stressors which may impact disclosing their sexual identity. Additionally, developing social support networks of young bisexual women may be the most challenging because women are older than men when they first disclose their nonheterosexual identity (Martos, Nezhad, & Meyer, 2015). Negative perceptions about bisexuality may deter bisexual women from turning to either heterosexual men and women or other sexual minority individuals for support because they do not want to experience discrimination or stigma. Taken together, bisexual women who experience more sexual minority stress may have fewer networks of social support than lesbian women which in turn is associated with negative health outcomes such as physical and mental health problems.
Limitations and Future Research Directions
Several limitations should be noted. First, ours was a cross-sectional study and therefore causal pathways between the study variables cannot be confirmed. For example, we posit that bisexual women may have lower social support because they experience more minority stress, but it is also possible that they experience more stress because they have less social support or that both are lower because of an unmeasured third variable. Second, young adult women between the ages of 18 to 30 were recruited online for the current study. Therefore, how results may generalize to other groups of lesbian and bisexual women is unknown.
Third, only participants who self-identified as lesbian or bisexual were included in the current study. A self-report measure was used to examine sexual identity; however, some studies use measures of sexual attraction and sexual behavior (Bostwick et al., 2010; Johns, Zimmerman, & Bauermeister, 2013). Due to the growing number of young adult women who identify as other non-monosexual identities (e.g., queer, pansexual; Morandini, Blaszczynski, & Dar-Nimrod, 2017), future research should consider examining a range of sexual identities to determine differences on sexual minority stress experiences and health outcomes. Similarly, only cisgender women were included in the current study. Although beyond the scope of our study, future research should also examine the experiences of transgender women. It is important to include samples of all women to inform future research.
Fourth, bisexual-specific stressors were not examined. Measuring bisexual-specific stressors (e.g., Brewster & Moradi, 2010) would provide further information to enhance prevention and intervention programs to reduce health problems among bisexual women. Fifth, geographic location was not examined. Sexual minority individuals may have different experiences (e.g., minority stressors) based on their location. Similarly, examining experiences and health outcomes of sexual minority women outside of the U.S. is also important. Thus, future research should examine how geographic region and country may impact minority stress, perceived social support, and health outcomes.
Although we assessed proximal sexual minority stressors, consideration of institutional policies that promote discrimination (i.e., structural stigma; Hatzenbuehler, 2014) are important to identify to further understanding and reduce health disparities. Specifically, physical health problems also may be attributed to structural discrimination or anticipated discrimination from healthcare providers. For example, among bisexual and other non-monosexual adults, acknowledging the inability to find a job to cover the cost of medical treatment and prior stigma from healthcare workers were perceived to be a direct contributors to poor physical health (Doan Van et al., 2019). Although not explicitly examined in the current study, it is possible that bisexual women may experience more sexual minority stress which in turn could lead to greater reluctance to seek medical treatment and consequently exacerbate physical health problems.
Finally, our results highlight the importance of studying distinct subgroups (e.g., lesbian or bisexual) within the SMW population (e.g., Institute of Medicine, 2011). However, it should be noted that prior research has consistently documented increased health risks among lesbian and bisexual women compared to heterosexual women (Gonzales et al., 2016; Kerr et al., 2013). Therefore, results of our study should not undermine the fact that compared to heterosexual women, all SMW likely face unique forms of stressors and discrimination (i.e., sexual minority stress) that may have negative health implications. Although beyond the scope of our study, future studies should incorporate a comparison group of heterosexual women to further document the specific mechanisms associated with health disparities of bisexual and lesbian women.
Practice Implications
The sequence of more minority stress and less social support may confer enhanced risk for negative health outcomes among bisexual women. Consequently, focusing on more effective coping skills for minority stress and enhancing social support networks and interactions may result in positive health outcomes. Cognitive-behavioral therapy focused on affirming GB identities and reducing sexual minority stress processes was linked to improved health outcomes for young adult gay and bisexual men (i.e., reduced depressive symptoms, fewer alcohol-related problems, less risky sex; Pachankis, Hatzenbuehler, Rendina, Safren, & Parsons, 2015). A recent online intervention by Israel and colleagues (2019) guided bisexual individuals through several modules that included evaluating and challenging negative stereotypes about bisexual people, identifying negative messages to which they have been exposed as well as increasing self-efficacy by explaining how they rejected these messages, and focusing on positive aspects of bisexuality. Results of their study revealed that internalized stressors specific to bisexual individuals were reduced following the intervention.
In addition to enhancing coping skills (e.g., increased self-efficacy), online interventions may have the potential to facilitate a “safe” environment due to their potential of anonymity where bisexual women can process and discuss bisexual-specific sexual minority stressors. As such, creating an online community may provide an outlet for bisexual women to discuss experiences and coping strategies while also providing them with a sense of increased social support of a bisexual community. Because heterosexual individuals as well as lesbians and gay men may have negative attitudes about bisexual individuals (Friedman et al., 2014), developing interventions that reduce stigma from these groups is also important. For example, as outlined by Dyar, Lytle, London, and Levy (2015), the lesbian and gay community may provide a unique contribution of support to bisexual individuals due to their shared minority status. These efforts toward reducing sexual minority stress and increasing social support could decrease health disparities among SMW in general and among bisexual women specifically.
The development of policies to reduce stigma and discrimination experiences of SMW in general and bisexual women specifically may help reduce sexual minority stress. For instance, among SMW, expectation of stigma by others, discrimination, and depressive symptoms were lower after Illinois signed and enacted a law legalizing and protecting civil unions (Everett, Hatzenbuehler, & Hughes, 2016). SMW were also more likely to disclose their sexual identity and reported higher satisfaction with their healthcare providers if they lived in states that had nondiscrimination policies (Baldwin, Dodge, Schick, Sander, & Fortenberry, 2017). Although our study focused on proximal stressors, legislation that protects SMW may also target distal stressors such as structural discrimination and stigma, and these policies show promising effects on mental and physical health outcomes.
It is also important to interpret and understand results of our study in terms of the intersecting identities as sexual minority individuals and as women. Specifically, social support may be a particularly important variable to combat negative outcomes for women. For instance, among a sample of women (sexual identity not reported), on days when they experienced more stress, those with more social support reported less physical health problems than women with lower social support (Stein & Smith, 2015). Further, among heterosexual couples, women, compared to men, provide more effective social support when their partner is stressed (Bodenmann et al., 2015). Perhaps because lesbian women are often in relationships with women, they receive more effective forms of social support when they experience sexual minority stressors. However, social support during stressful experiences may be particularly limited for bisexual women in relationships with men. These results highlight the importance to develop intervention programs that focus on enhancing skills for those who may provide social support to SMW.
Conclusions
Consistent with the U.S. Institute of Medicine’s (2011) recommendations to examine subgroups of SMW, there were marked differences in our study between lesbian and bisexual women regarding health outcomes and social support. Further, our results support Meyer’s (2003) sexual minority stress model and the importance of protective factors, indicating that sexual minority stress and social support may be important mechanisms to consider when explaining greater health disparities for bisexual women. Findings highlight the central role that sexual minority stress plays when considering the health and potential coping strategies of SMW. Overall, our results add to the literature by identifying health disparities within the SMW population and emphasizing the salient role of sexual minority stress and social support on the health of both lesbian and bisexual women.
Acknowledgements
Research reported in this publication was supported by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) of the National Institutes of Health under award number R15AA020424 to Robin Lewis (PI). The content of this article is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health (NIH), the funding agency.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Contributor Information
Sarah J. Ehlke, Department of Psychology, Old Dominion University, Norfolk, VA.
Abby L. Braitman, Department of Psychology, Old Dominion University, Virginia Consortium Program in Clinical Psychology, Norfolk, VA.
Charlotte A. Dawson, Department of Psychology, Old Dominion University, Virginia Consortium Program in Clinical Psychology, Norfolk, VA.
Kristin E. Heron, Department of Psychology, Old Dominion University, Virginia Consortium Program in Clinical Psychology, Norfolk, VA.
Robin J. Lewis, Department of Psychology, Old Dominion University, Virginia Consortium Program in Clinical Psychology, Norfolk, VA.
References
- Baldwin AM, Dodge B, Schick V, Sanders SA, & Fortenberry JD (2017). Sexual minority women’s satisfaction with health care providers and state-level structural support: Investigating the impact of lesbian, gay, bisexual, and transgender nondiscrimination legislation. Women’s Health Issues, 27, 271–278. 10.1016/j.whi.2017.01.004 [DOI] [PubMed] [Google Scholar]
- Balsam KF, & Mohr JJ (2007). Adaptation to sexual orientation stigma: a comparison of bisexual and lesbian/gay adults. Journal of Counseling Psychology, 54, 306–319. 10.1037/0022-0167.54.3.306 [DOI] [Google Scholar]
- Blair KL, & Holmberg D (2008). Perceived social network support and well-being in same-sex versus mixed-sex romantic relationships. Journal of Social and Personal Relationships, 25, 769–791. 10.1177/0265407508096695 [DOI] [Google Scholar]
- Bodenmann G, Meuwly N, Germann J, Nussbeck FW, Heinrichs M, & Bradbury TN (2015). Effects of stress on the social support provided by men and women in intimate relationships. Psychological Science, 26, 1584–1594. 10.1177/0956797615594616 [DOI] [PubMed] [Google Scholar]
- Bostwick WB, Boyd CJ, Hughes TL, & McCabe SE (2010). Dimensions of sexual orientation and the prevalence of mood and anxiety disorders in the United States. American Journal of Public Health, 100, 468–475. 10.2105/ajph.2008.152942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick WB, Boyd CJ, Hughes TL, West BT, & McCabe SE (2014). Discrimination and mental health among lesbian, gay, and bisexual adults in the United States. American Journal of Orthopsychiatry, 84, 35–45. 10.1037/h0098851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostwick W, & Hequembourg A (2014). ‘Just a little hint’: Bisexual-specific microaggressions and their connection to epistemic injustices. Culture, Health & Sexuality, 16, 488–503. 10.1080/13691058.2014.889754 [DOI] [PubMed] [Google Scholar]
- Bowen DJ, Balsam KF, & Ender SR (2008). A review of obesity issues in sexual minority women. Obesity, 16, 221–228. 10.1038/oby.2007.34 [DOI] [PubMed] [Google Scholar]
- Bregman HR, Malik NM, Page MJ, Makynen E, & Lindahl KM (2013). Identity profiles in lesbian, gay, and bisexual youth: The role of family influences. Journal of Youth and Adolescence, 42, 417–430. 10.1007/s10964-012-9798-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewster ME, & Moradi B (2010). Perceived experiences of anti-bisexual prejudice: Instrument development and evaluation. Journal of Counseling Psychology, 57, 451–468. 10.1037/a0021116 [DOI] [PubMed] [Google Scholar]
- Chaudoir SR, Wang K, & Pachankis JE (2017). What reduces sexual minority stress? A review of the intervention “toolkit.” Journal of Social Issues, 73, 586–617. 10.1111/josi.12233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cochran SD, Sullivan JG, & Mays VM (2003). Prevalence of mental disorders, psychological distress, and mental health services use among lesbian, gay, and bisexual adults in the United States. Journal of Consulting and Clinical Psychology, 71, 53–61. 10.1037/0022-006x.71.1.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, & Hoberman HM (1983). Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology, 13, 99–125. 10.1111/j.1559-1816.1983.tb02325.x [DOI] [Google Scholar]
- Cohen S, & Wills TA (1985). Stress, social support, and the buffering hypothesis. Psychological Bulletin, 98, 310–357. 10.1037/0033-2909.98.2.310 [DOI] [PubMed] [Google Scholar]
- Cokley K, McClain S, Enciso A, & Martinez M (2013). An examination of the impact of minority status stress and impostor feelings on the mental health of diverse ethnic minority college students. Journal of Multicultural Counseling and Development, 41, 82–95. 10.1002/j.2161-1912.2013.00029.x [DOI] [Google Scholar]
- Conron KJ, Mimiaga MJ, & Landers SJ (2010). A population-based study of sexual orientation identity and gender differences in adult health. American Journal of Public Health, 100, 1953–1960. 10.2105/ajph.2009.174169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dahlem NW, Zimet GD, & Walker RR (1991). The multidimensional scale of perceived social support: A confirmation study. Journal of Clinical Psychology, 47, 756–761. [DOI] [PubMed] [Google Scholar]
- Diamond LM (2008). Female bisexuality from adolescence to adulthood: results from a 10-year longitudinal study. Developmental Psychology, 44, 5–14. 10.1037/0012-1649.44.1.5 [DOI] [PubMed] [Google Scholar]
- Doan Van EE, Mereish EH, Woulfe JM, & Katz-Wise SL (2019). Perceived discrimination, coping mechanisms, and effects on health in bisexual and other non-monosexual adults. Archives of Sexual Behavior, 48, 159–174. 10.1007/s10508-018-1254-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyar C, Feinstein BA, & London B (2014). Dimensions of sexual identity and minority stress among bisexual women: The role of partner gender. Psychology of Sexual Orientation and Gender Diversity, 1, 441–451. 10.1037/sgd0000063 [DOI] [Google Scholar]
- Dyar C, Feinstein BA, & London B (2015). Mediators of differences between lesbians and bisexual women in sexual identity and minority stress. Psychology of Sexual Orientation and Gender Diversity, 2, 43–51. 10.1037/sgd0000090 [DOI] [Google Scholar]
- Dyar C, Feinstein BA, Schick V, & Davila J (2017). Minority stress, sexual identity uncertainty, and partner gender decision making among nonmonosexual individuals. Psychology of Sexual Orientation and Gender Diversity, 4, 87–104. 10.1037/sgd0000213 [DOI] [Google Scholar]
- Dyar C, Lytle A, London B, & Levy SR (2015). Application of bisexuality research to the development of a set of guidelines for intervention efforts to reduce binegativity. Translational Issues in Psychological Science, 1, 352–362. 10.1037/tps0000045 [DOI] [Google Scholar]
- Dyar C, Taggart TC, Rodriguez-Seijas C, Thompson RG, Elliott JC, Hasin DS, Eaton NR (2019). Physical health disparities across dimensions of sexual orientation, race/ethnicity, and sex: Evidence for increased risk among bisexual adults. Archives of Sexual Behavior, 48, 225–242. 10.1007/s10508-018-1169-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everett BG, Hatzenbuehler ML, & Hughes TL (2016). The impact of civil union legislation on minority stress, depression, and hazardous drinking in a diverse sample of sexual-minority women: A quasi-natural experiment. Social Science & Medicine, 169, 180–190. 10.1016/j.socscimed.2016.09.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flenar DJ, Tucker CM, & Williams JL (2017). Sexual minority stress, coping, and physical health indicators. Journal of Clinical Psychology in Medical Settings, 24, 223–233. 10.1037/sgd0000066 [DOI] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Kim HJ, & Barkan SE (2012). Disability among lesbian, gay, and bisexual adults: Disparities in prevalence and risk. American Journal of Public Health, 102, e16–e21. 10.2105/AJPH.2011.300379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fredriksen-Goldsen KI, Kim HJ, Barkan SE, Balsam KF, & Mincer SL (2010). Disparities in health-related quality of life: A comparison of lesbians and bisexual women. American Journal of Public Health, 100, 2255–2261. 10.2105/AJPH.2009.177329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman MR, Dodge B, Schick V, Herbenick D, Hubach RD, Bowling J, … Reece M (2014). From bias to bisexual health disparities: Attitudes toward bisexual men and women in the United States. LGBT Health, 1, 309–318. 10.1089/lgbt.2014.0005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman C, & Leaper C (2010). Sexual-minority college women’s experiences with discrimination: Relations with identity and collective action. Psychology of Women Quarterly, 34, 152–164. 10.1111/j.1471-6402.2010.01558.x [DOI] [Google Scholar]
- Frost DM, Lehavot K, & Meyer IH (2015). Minority stress and physical health among sexual minority individuals. Journal of Behavioral Medicine, 38, 1–8. 10.1007/s10865-013-9523-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman SE, Cochran SD, Mays VM, Hughes M, Ostrow D, & Kessler RC (2001). Risk of psychiatric disorders among individuals reporting same-sex sexual partners in the National Comorbidity Survey. American Journal of Public Health, 91, 933–939. 10.2105/ajph.91.6.933 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzales G, Przedworski J, & Henning-Smith C (2016). Comparison of health and health risk factors between lesbian, gay, and bisexual adults and heterosexual adults in the United States: Results from the National Health Interview Survey. JAMA Internal Medicine, 176, 1344–1351. 10.1001/jamainternmed.2016.3432 [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML (2014). Structural stigma and the health of lesbian, gay, and bisexual populations. Current Directions in Psychological Science, 23, 127–132. 10.1177/0963721414523775 [DOI] [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hughes TL, Johnson TP, Steffen AD, Wilsnack SC, & Everett B (2014). Lifetime victimization, hazardous drinking, and depression among heterosexual and sexual minority women. LGBT Health, 1, 192–203. 10.1089/lgbt.2014.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. (2011). The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Israel T, Choi AY, Goodman JA, Matsuno E, Lin Y-J, Kary KG, … Merrill CRS (2019). Reducing internalized binegativity: Development and efficacy of an online intervention. Psychology of Sexual Orientation and Gender Diversity, 6, 149–159. 10.1037/sgd0000314 [DOI] [Google Scholar]
- Jabson JM, Mitchell JW, & Doty SB (2016). Associations between non-discrimination and training policies and physicians’ attitudes and knowledge about sexual and gender minority patients: a comparison of physicians from two hospitals. BMC Public Health, 16, 256–266. 10.1186/s12889-016-2927-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johns MM, Zimmerman M, & Bauermeister JA (2013). Sexual attraction, sexual identity, and psychosocial wellbeing in a national sample of young women during emerging adulthood. Journal of Youth and Adolescence, 42, 82–95. 10.1007/s10964-012-9795-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm AF, Korten AE, Rodgers B, Jacomb PA, & Christensen H (2002). Sexual orientation and mental health: results from a community survey of young and middle–aged adults. The British Journal of Psychiatry, 180, 423–427. 10.1192/bjp.180.5.423 [DOI] [PubMed] [Google Scholar]
- Katz-Wise SL, Rosario M, Calzo JP, Scherer EA, Sarda V, & Austin SB (2017). Associations of timing of sexual orientation developmental milestones and other sexual minority stressors with internalizing mental health symptoms among sexual minority young adults. Archives of Sexual Behavior, 46, 1441–1452. 10.1080/00224499.2016.1170757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr DL, Santurri L, & Peters P (2013). A comparison of lesbian, bisexual, and heterosexual college undergraduate women on selected mental health issues. Journal of American College Health, 61, 185–194. 10.1080/07448481.2013.787619 [DOI] [PubMed] [Google Scholar]
- Kerridge BT, Pickering RP, Saha TD, Ruan WJ, Chou SP, Zhang H, … Hasin DS (2017). Prevalence, sociodemographic correlates and DSM-5 substance use disorders and other psychiatric disorders among sexual minorities in the United States. Drug and Alcohol Dependence, 170, 82–92. 10.1016/j.drugalcdep.2016.10.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambe J, Cerezo A, & O’Shaughnessy T (2017). Minority stress, community involvement, and mental health among bisexual women. Psychology of Sexual Orientation and Gender Diversity, 4, 218–226. 10.1037/sgd0000222 [DOI] [Google Scholar]
- Lea T, de Wit J, & Reynolds R (2014). Minority stress in lesbian, gay, and bisexual young adults in Australia: Associations with psychological distress, suicidality, and substance use. Archives of Sexual Behavior, 43, 1571–1578. 10.1007/s10508-014-0266-6 [DOI] [PubMed] [Google Scholar]
- Lehavot K, & Simoni JM (2011). The impact of minority stress on mental health and substance use among sexual minority women. Journal of Consulting and Clinical Psychology, 79, 159–170. 10.1037/a0022839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis RJ, Derlega VJ, Griffin JL, & Krowinski AC (2003). Stressors for gay men and lesbians: Life stress, gay-related stress, stigma consciousness, and depressive symptoms. Journal of Social and Clinical Psychology, 22, 716–729. 10.1521/jscp.22.6.716.22932 [DOI] [Google Scholar]
- Martos AJ, Nezhad S, & Meyer IH (2015). Variations in sexual identity milestones among lesbians, gay men, and bisexuals. Sexuality Research and Social Policy, 12, 24–33. 10.1007/s13178-014-0167-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. 10.1037/0033-2909.129.5.674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohr JJ, Jackson SD, & Sheets RL (2017). Sexual orientation self-presentation among bisexual-identified women and men: Patterns and predictors. Archives of Sexual Behavior, 46, 1465–1479. 10.1007/s10508-016-0808-1 [DOI] [PubMed] [Google Scholar]
- Mohr JJ, & Kendra MS (2011). Revision and extension of a multidimensional measure of sexual minority identity: The Lesbian, Gay, and Bisexual Identity Scale. Journal of Counseling Psychology, 58, 234–245. 10.1037/a0022858 [DOI] [PubMed] [Google Scholar]
- Morandini JS, Blaszczynski A, & Dar-Nimrod I (2017). Who adopts queer and pansexual sexual identities? The Journal of Sex Research, 54, 911–922. 10.1080/00224499.2016.1249332 [DOI] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998–2017). Mplus user’s guide (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Pachankis JE, Hatzenbuehler ML, Rendina HJ, Safren SA, & Parsons JT (2015). LGB-affirmative cognitive-behavioral therapy for young adult gay and bisexual men: A randomized controlled trial of a transdiagnostic minority stress approach. Journal of Consulting and Clinical Psychology, 83, 875–889. 10.1037/ccp0000037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross LE, Dobinson C, & Eady A (2010). Perceived determinants of mental health for bisexual people: A qualitative examination. American Journal of Public Health, 100, 496–502. 10.2105/AJPH.2008.156307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross LE, Salway T, Tarasoff LA, MacKay JM, Hawkins BW, & Fehr CP (2018). Prevalence of depression and anxiety among bisexual people compared to gay, lesbian, and heterosexual individuals: A systematic review and meta-analysis. The Journal of Sex Research, 55, 435–456. 10.1080/00224499.2017.1387755 [DOI] [PubMed] [Google Scholar]
- Safren SA, & Pantalone DW (2006). Social anxiety and barriers to resilience among lesbian, gay, and bisexual adolescents. In Omoto AM & Kurtzman HS (Eds.), Contemporary perspectives on lesbian, gay, and bisexual psychology. Sexual orientation and mental health: Examining identity and development in lesbian, gay, and bisexual people (pp. 55–71). Washington, DC: American Psychological Association. 10.1037/11261-003 [DOI] [Google Scholar]
- Salway T, Ross LE, Fehr CP, Burley J, Asadi S, Hawkins B, & Tarasoff LA (2019). A systematic review and meta-analysis of disparities in the prevalence of suicide ideation and attempt among bisexual populations. Archives of Sexual Behavior, 48, 89–111. 10.1007/s10508-018-1150-6 [DOI] [PubMed] [Google Scholar]
- Sarno E, & Wright AJ (2013). Homonegative microaggressions and identity in bisexual men and women. Journal of Bisexuality, 13, 63–81. 10.1080/15299716.2013.756677 [DOI] [Google Scholar]
- Stein ER, & Smith BW (2015). Social support attenuates the harmful effects of stress in healthy adult women. Social Science & Medicine, 146, 129–136. 10.1016/j.socscimed.2015.10.038 [DOI] [PubMed] [Google Scholar]
- Szymanski DM, Dunn TL, & Ikizler AS (2014). Multiple minority stressors and psychological distress among sexual minority women: The roles of rumination and maladaptive coping. Psychology of Sexual Orientation and Gender Diversity, 1, 412–421. 10.1037/sgd0000066 [DOI] [Google Scholar]
- Veit CT, & Ware JE (1983). The structure of psychological distress and well-being in general populations. Journal of Consulting and Clinical Psychology, 51, 730–742. 10.1037//0022-006x.51.5.730 [DOI] [PubMed] [Google Scholar]
- Verdonk P, Benschop YW, De Haes HC, & Lagro-Janssen TL (2009). From gender bias to gender awareness in medical education. Advances in Health Sciences Education, 14, 135–152. 10.1007/s10459-008-9100-z [DOI] [PubMed] [Google Scholar]
- Wandrey RL, Mosack KE, & Moore EM (2015). Coming out to family and friends as bisexually identified young adult women: A discussion of homophobia, biphobia, and heteronormativity. Journal of Bisexuality, 15, 204–229. 10.1080/15299716.2015.1018657 [DOI] [Google Scholar]
- Weinstein M, Berwick D, Goldman P, Murphy J, & Barsky A (1989). A comparison of three psychiatric screening tests using receiver operating characteristic analysis. Medical Care, 27, 593–607. 10.1097/00005650-198906000-00003 [DOI] [PubMed] [Google Scholar]
- Whittaker VA, & Neville HA (2010). Examining the relation between racial identity attitude clusters and psychological health outcomes in African American college students. Journal of Black Psychology, 36, 383–409. 10.1177/0095798409353757 [DOI] [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, & Farley GK (1988). The multidimensional scale of perceived social support. Journal of Personality Assessment, 52, 30–41. 10.1037/t02380-000 [DOI] [PubMed] [Google Scholar]