Abstract
Background
Patient-reported outcomes in atrial fibrillation (AF) are increasingly used to evaluate treatment efficacy and as endpoints in clinical trials. Few studies have related patient-reported outcomes in AF to clinical events and outcomes. We examined the association between patient-reported outcomes and hospitalization risk in individuals with AF receiving care at a regional healthcare system.
Methods and results
We related the AF Effect on QualiTy of Life (AFEQT), a validated measure (range 0–100) with higher scores indicating superior AF-specific patient-reported outcomes, to hospitalization events in a cohort with prevalent AF. We determined incidence rates for hospitalization events (all-cause, cardiac-, or AF-related) across quartiles of AFEQT scores. We used the Andersen-Gill method to account for multiple hospitalization events per individual and compared the risks of hospitalization across AFEQT quartiles in multivariable-adjusted models. In 339 individuals with AF (age 72.3 ± 10.1 years; 43% women) followed for median 2.6 years (range 0–3.4 years), we observed 417 total hospitalization events. We identified increased incidence rates of hospitalization with progressively decreased AFEQT quartile. Relative to those in the highest AFEQT quartile, individuals in the lowest AFEQT quartile had 3-fold greater risk of all-cause hospitalization (95% Confidence Interval [CI] 1.67–6.57, p < 0.001) and 5-fold greater risk of cardiac hospitalization (95% CI 1.66–13.80, p = 0.004).
Conclusions
We identified a progressive association between patient-reported outcomes in AF and risk of hospitalization events. Our results underscore the relevance of patient-reported outcomes to clinical adversity and prognosis in AF.
Keywords: Atrial fibrillation, Patient-reported outcome, Hospitalization
1. Introduction
Atrial fibrillation (AF) is an increasingly prevalent heart rhythm disorder with marked adverse effects on patient-reported outcomes such as quality of life [1]. Patients with AF may have complicated treatments for the condition, insults from other chronic diagnoses, or be directly affected by the tachyarrhythmia and its associated morbidity [2]. Multiple measures have emerged to identify and track patient-reported outcomes in AF [[3], [4], [5]]. Professional society guidelines have emphasized patient-reported measures as metrics to gauge and modify treatment for AF, indicating their importance to AF management [6]. Such measures have likewise been incorporated in clinical trials as secondary outcomes to assess symptoms specific to AF and general physical and psychological health [[7], [8], [9]]. Likewise, patient-reported outcomes have been incorporated into registries to identify factors that influence clinical outcomes in AF [10,11].
We determined to investigate the associations between patient-reported and clinical outcomes. Our rationale was several-fold: first, to date the data describing patient-reported outcomes in AF in relation to clinical adversity remains limited. Second, we appreciated that substantive examination of the association between patient-reported measures and AF may yield insights to enhance and direct patient-centered care, particularly to identify individuals at increased risk of clinical adversity. Third, as patient-reported outcomes are used more frequently as endpoints in clinical trials and studies, how they are affected by AF treatment strategies merits continued exploration.
To conduct our investigation we employed the AF Effect on QualiTy of Life (AFEQT) questionnaire, which has emerged as the most widely used patient-reported measure in AF [12,13]. The AFEQT employs 20 questions in four domains – symptoms, daily activities, treatment concern, and treatment satisfaction – and has been used in clinical trials, including a multicenter, randomized controlled trial of ablation which identified improvement in quality of life as a prominent endpoint [9]. We consequently examined the association between patient-reported outcomes, assessed by the AFEQT, and hospitalization risk in a cohort of individuals with prevalent AF. We hypothesized that individuals with worse measurement of patient-reported outcomes (i.e., lower AFEQT scores) would experience increased risk of hospitalization even after adjustment for AF treatment.
2. Methods
2.1. Cohort selection
We enrolled individuals receiving care at selected ambulatory facilities affiliated with the University of Pittsburgh Medical Center (UPMC) in Pittsburgh, PA, a large, regional healthcare system. We identified individuals with prevalent AF by screening the electronic health record and then making direct contact during clinic visits, by physician or provider referral, or by self-referral. Eligibility criteria included age ≥ 18 years, history of non-valvular AF as documented by the electronic health record, CHA2DS2-VaSc [14] (congestive heart failure, hypertension, age, diabetes, stroke, vascular disease [history of MI, PVD, or aortic atherosclerotic disease], and sex category) score ≥ 2, having been prescribed oral anticoagulation for AF, and English-speaking at a level appropriate to participate in this research protocol. Exclusion criteria included history of ischemic or hemorrhagic stroke, AF secondary to non-cardiac issues, AF within 30 days of any cardiothoracic surgery, and individuals who did not pass a three-item screening instrument prior to informed consent. From 2016 to 2018, we identified 1093 eligible individuals from the electronic health record. Recruitment was conducted primarily as part of regularly scheduled visits and constitutes a convenience sample of the individuals identified as eligible as we have previously described [[15], [16], [17]]. We approached 486 individuals to invite their participation in this study, of whom 339 enrolled. Written informed consent was collected for each participant. The study was approved by the University of Pittsburgh institutional review board.
2.2. Covariates
Age, sex, race, and smoking status were obtained by self-report. Clinical history pertinent to the CHA2DS2-VaSc and body mass index were extracted from the electronic health record. AF treatment including history of electrical or chemical cardioversion, pulmonary vein isolation, and anticoagulant and antiarrhythmic medications (amiodarone, dofetilide, flecainide, lidocaine propafenone, and sotalol) were likewise identified from the electronic record. Social factors obtained from participant self-report included annual household income (<$19,000, $20,000–$49,999, $50,000–$99,999, or >$100,000), and level of education (high school or vocational training, some part of college or an associate degree, bachelor's degree, or any graduate or professional school degree or enrollment).
Patient-reported outcomes specific to AF were collected with the AFEQT, a validated 20-item instrument scored from 0 to 100, where higher scores indicate a superior outcome over the prior 4 weeks [12]. The AFEQT includes a global score and 4 domain scores (symptoms, daily activities, treatment concerns, and treatment satisfaction). A difference of 5 or more has been identified as a clinically meaningful change in an individual [18].
2.3. .Outcomes ascertainment
Hospitalization events were extracted for each individual by review of the UPMC longitudinal electronic health record, from the date of enrollment to the last date of contact, through March 16, 2020 or date of death as identified by the electronic health record. A hospitalization event was defined as a hospital admission with duration ≥24 h. Each hospitalization event was classified as all-cause, cardiac-related, and/or AF-related upon review of the electronic health record and determination of the primary indicator for hospitalization. Scheduled admissions for elective procedures (such as cardioversion or ablation) were not defined as hospitalization events.
2.4. Statistical analysis
We summarized continuous variables according to their means and standard deviation, and categorial variables as frequencies and percentages. We compared the baseline characteristics according to AFEQT quartile using chi-squared tests for categorical variables and analysis of variance for continuous variables. We then determined the number of hospitalizations events by AFEQT quartile, and calculated incidence rates by incorporating person-years of observation to report differences in hospitalization incidence across quartiles. We graphically represented the number of hospitalizations per patient over time using mean cumulative function of hospitalization curves.
Next, we utilized the Andersen-Gill model to analyze recurrent hospitalizations and calculated hazard ratios by the AFEQT quartile for all-cause, cardiac-, and AF-related hospitalization. The Andersen-Gill model accounts for the correlation of recurrent events within the same individual; in contrast to the standard time-to-first-event analysis of a Cox proportional hazards model, we gain the additional benefit of using all events for each participant rather than censoring at the first end-point [19,20]. We employed multivariable-adjusted models to examine the relation of the AFEQT to hospitalization endpoints. Multivariable models were constructed sequentially to adjust for demographic factors consisting of age, sex, and race (Model 1), then additionally adding clinical factors consisting of body mass index, heart failure, hypertension, diabetes, and vascular disease, and treatment for atrial fibrillation (ablations, cardioversion, antiarrhythmic medications) (Model 2), and finally adding the socioeconomic factors of annual household income and educational attainment (Model 3). All statistical analyses were conducted with SAS version 9.4 (Cary, North Carolina).
3. Results
Baseline characteristics at study enrollment are presented in Table 1. There were 339 participants enrolled in the study with a median 2.6-year length of follow-up (range 0–3.4 years). The average age was 72.3 ± 10.1 years, and 144 (42.5%) were women. Most study participants had an annual household income in the $20,000–49,999 range (n = 100, 29.5%), while education for most participants was at the high school or vocational level (n = 117, 34.5%).
Table 1.
Characteristics of the study cohort (n = 339) by AFEQT quartile.
| Characteristic | All participants |
Quartile 1 (<66.6) |
Quartile 2 (66.6 to < 80.0) |
Quartile 3 (80.0 to 90.0) |
Quartile 4 (>90.0) |
|---|---|---|---|---|---|
| n = 339 | n = 78 | n = 94 | n = 85 | n = 81 | |
| Age, years | 72.3 ± 10.1 | 69.9 ± 9.8 | 72.8 ± 11.1 | 73.2 ± 10.9 | 72.9 ± 7.8 |
| Female sex | 144 (42.5%) | 42 (53.8%) | 39 (41.5%) | 33 (38.8%) | 30 (37.0%) |
| White race | 320 (94.4%) | 72 (92.3%) | 86 (91.5%) | 83 (97.6%) | 78 (96.3%) |
| Body mass index (m/kg2) | 31.2 ± 7.2 | 33.2 ± 8.3 | 31.4 ± 7.5 | 29.1 ± 5.6 | 31.0 ± 6.4 |
| Smoking history | |||||
| Never | 169 (49.9%) | 32 (41.0%) | 49 (52.1%) | 46 (54.1%) | 41 (50.6%) |
| Former | 152 (44.8%) | 37 (47.4%) | 44 (46.8%) | 36 (42.4%) | 35 (43.2%) |
| Current | 18 (5.3%) | 9 (11.5%) | 1 (1.1%) | 3 (3.5%) | 5 (6.2%) |
| Heart failure (any) | 111 (32.7%) | 34 (43.6%) | 40 (42.6%) | 24 (28.2%) | 13 (16.0%) |
| Preserved | 61 (18.0%) | 16 (20.5%) | 28 (29.8%) | 10 (11.8%) | 7 (8.6%) |
| Reduced | 44 (13.0%) | 17 (21.8%) | 10 (10.6%) | 11 (12.9%) | 6 (7.4%) |
| Not specified | 6 (1.8%) | 1 (1.3%) | 2 (2.1%) | 3 (3.5%) | 0 (0.0%) |
| Hypertension | 243 (71.7%) | 57 (73.1%) | 71 (75.5%) | 56 (65.9%) | 59 (72.8%) |
| Diabetes | 82 (24.2%) | 21 (26.9%) | 22 (23.4%) | 21 (24.7%) | 18 (22.2%) |
| Vascular disease | 82 (24.2%) | 23 (29.5%) | 17 (18.1%) | 20 (23.5%) | 21 (25.9%) |
| Education | |||||
| High school/vocational | 117 (34.5%) | 30 (38.5%) | 39 (41.5%) | 26 (30.6%) | 21 (25.9%) |
| Some college | 67 (19.8%) | 12 (15.4%) | 22 (23.4%) | 15 (17.6%) | 18 (22.2%) |
| Bachelor's | 79 (23.3%) | 26 (33.3%) | 12 (12.8%) | 21 (24.7%) | 20 (24.7%) |
| Graduate | 76 (22.4%) | 10 (12.8%) | 21 (22.3%) | 23 (27.1%) | 22 (27.2%) |
| Income | |||||
| <$19,999 | 35 (10.3%) | 15 (19.2%) | 9 (9.6%) | 5 (5.9%) | 6 (7.4%) |
| $20,000-49,999 | 100 (29.5%) | 25 (32.1%) | 33 (35.1%) | 23 (27.1%) | 18 (22.2%) |
| $50,000-99,999 | 97 (28.6%) | 20 (25.6%) | 29 (30.9%) | 25 (29.4%) | 23 (28.4%) |
| >$100,000 | 64 (18.9%) | 10 (12.8%) | 8 (8.5%) | 22 (25.9%) | 24 (29.6%) |
| Refused/no answer | 43 (12.7%) | 8 (10.3%) | 15 (16.0%) | 10 (11.8%) | 10 (12.3%) |
| AFEQT | 76.4 ± 17.6 | 50.4 ± 12.6 | 73.3 ± 4.0 | 85.8 ± 2.8 | 94.8 ± 2.6 |
Continuous measures expressed as mean ± standard deviation, and categories by their distribution and percentages. AFEQT indicates Atrial Fibrillation Effect on QualiTy of Life.
The AFEQT quartiles were: 0 to <66.6 (Quartile 1); 66.6 to <80.0 (Quartile 2); 80.0 to 90.0 (Quartile 3); and >90.0 to 100.0 (Quartile 4). There were no significant differences in age, sex, or race/ethnicity across AFEQT quartiles. While a greater proportion of participants with heart failure belonged to the higher AFEQT quartiles, the distributions of hypertension, diabetes, and vascular disease were consistent across quartiles. Of the 339 individuals enrolled in the study, there was a cumulative total of 417 hospitalizations, among which 175 were categorized as cardiac-related (42.0%) and 64 (15.3%) as related to AF. The frequency of all-cause hospitalization ranged from one (n = 54 individuals) to 15 (n = 1); cardiac hospitalization from one (n = 42) to 9 (n = 1); and AF hospitalization from one (n = 24) to 6 (n = 1).
Table 2 presents the number of events and incidence rates for all-cause and cardiac-related hospitalization by AFEQT quartile. We noted an overall increase in the incidence of both categories of hospitalization with progressive decrease in AFEQT quartile. The hospitalization incidence rate per patient-year for individuals in the lowest AFEQT quartile was approximately 4-fold that of those in the highest AFEQT quartile (Quartile 1, 0.72; Quartile 4, 0.19). The incidence rate of cardiac-related hospitalization for individuals in the lowest AFEQT quartile was 8-fold that of those in the highest AFEQT quartile (Quartile 1, 0.40; Quartile 4, 0.05). Supplemental Table 1 presents the number of events and incidence rates for AF-related hospitalization stratified by AFEQT quartile. The incidence rate of AF-related hospitalization for those in the lowest AFEQT quartile was 10-fold that of those in the highest AFEQT quartile (Quartile 1, 0.10; Quartile 4, 0.01).
Table 2.
Incidence of hospitalization events in study cohort by AFEQT quartile.
| Hospitalization events | Person-time at risk (yrs) | Incidence ratea | |
|---|---|---|---|
| All-cause hospitalization | |||
| Quartile 1 (n = 78) | 142 | 198.6 | 0.72 |
| Quartile 2 (n = 94) | 148 | 244.9 | 0.60 |
| Quartile 3 (n = 85) | 89 | 219.7 | 0.41 |
| Quartile 4 (n = 81) | 38 | 204.5 | 0.19 |
| Cardiac-related hospitalization | |||
| Quartile 1 (n = 78) | 79 | 198.6 | 0.40 |
| Quartile 2 (n = 94) | 54 | 244.9 | 0.22 |
| Quartile 3 (n = 85) | 31 | 219.7 | 0.14 |
| Quartile 4 (n = 81) | 11 | 204.5 | 0.05 |
Incidence rate reported as number of hospitalizations per patient-year. AFEQT indicates Atrial Fibrillation Effect on QualiTy of Life.
Fig. 1A presents the graded associations between AFEQT quartile and all-cause hospitalization events over follow-up. Likewise, Fig. 1B presents the association between AFEQT and cardiac-related hospitalizations, also stratified by AFEQT quartile. Supplementary Fig. 1 presents AF-related hospitalization events by AFEQT quartile. The figures consistently demonstrate the strong, prospective associations between lower AFEQT scores and increasing frequency of hospitalization events.
Fig. 1.
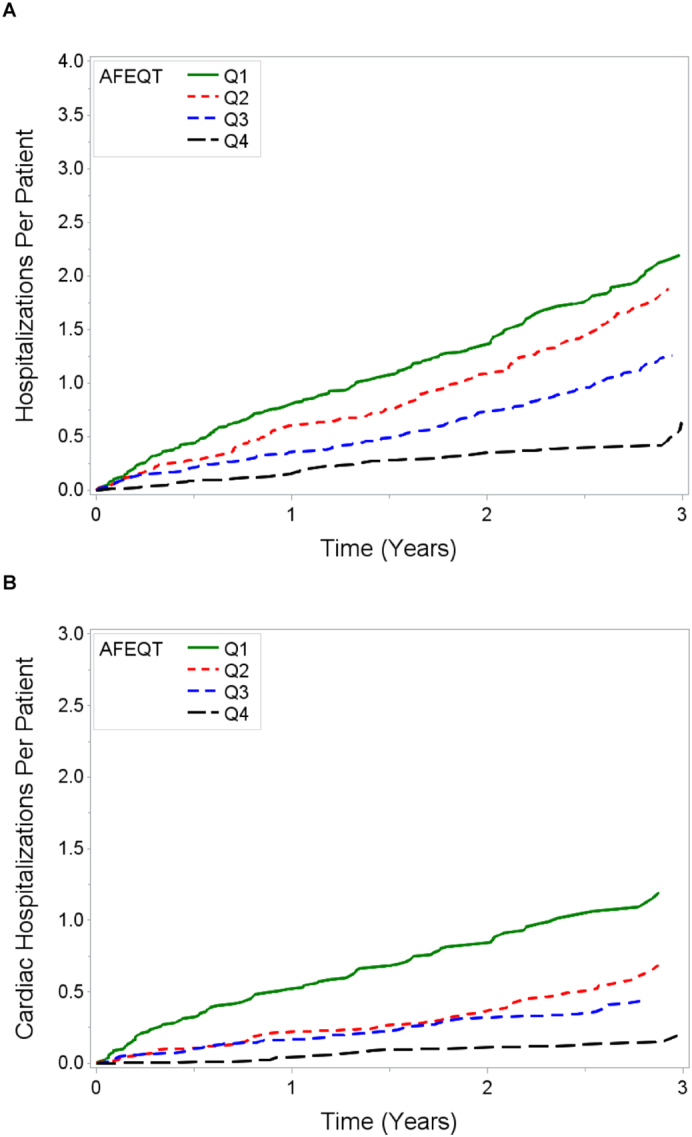
A and B. Mean cumulative function of (A) all-cause and (B) cardiac-related hospitalization after study enrollment according to AFEQT quartile scores. AFEQT indicates Atrial Fibrillation Effect on QualiTy of life, and categorization into quartiles, labeled as Q1-Q4 in the figure, is as defined by the text.
Table 3 presents the associations between health-related quality of life as measured by the AFEQT and risk of all-cause and cardiac-related hospitalization in multivariable-adjusted models. With the highest AFEQT quartile serving as the referent, the risk of hospitalization in both categories progressively increased across lower AFEQT quartiles. Individuals in the lowest AFEQT quartile had approximately 3-fold the risk of overall hospitalization as individuals in the highest AFEQT quartile after adjustment for demographic, clinical, and socioeconomic factors (95% CI 1.67–6.57, p < 0.001). For cardiac hospitalization, the progressive increase in risk with decrease in AFEQT quartile was more pronounced. Individuals in the lowest AFEQT quartile had nearly five-fold the risk of cardiac hospitalization as individuals in the highest AFEQT quartile (CI 1.66–13.80, p = 0.004). Supplemental Table 2 presents the associations between the AFEQT and risk of AF hospitalization. The progressive increase in risk with decrease in AFEQT quartile was most pronounced with AF hospitalization. Individuals in the lowest AFEQT quartile had approximately 16 times the risk of AF hospitalization as individuals in the highest AFEQT quartile (CI 2.00–133.10, p = 0.009).
Table 3.
Risks of all-cause and cardiac-related hospitalization according to AFEQT quartile.
| Model 1 |
Model 2 |
Model 3 |
||||
|---|---|---|---|---|---|---|
| HR (95% CI) | P-value | HR (95% CI) | P-value | HR (95% CI) | P-value | |
| All-cause hospitalization | ||||||
| Quartile 1 | 4.22 (2.39, 7.44) | <0.001 | 3.56 (1.80, 7.02) | <0.001 | 3.32 (1.67, 6.57) | <0.001 |
| Quartile 2 | 3.14 (1.70, 5.72) | <0.001 | 2.95 (1.48, 5.89) | 0.002 | 2.75 (1.41, 5.37) | 0.003 |
| Quartile 3 | 2.15 (1.20, 3.83) | 0.009 | 1.75 (0.85, 3.58) | 0.12 | 1.69 (0.83, 3.43) | 0.15 |
| Quartile 4 (referent) | – | – | – | |||
| Cardiac-related hospitalization | ||||||
| Quartile 1 | 7.41 (3.17, 17.20) | <0.001 | 5.43 (1.94, 15.10) | 0.001 | 4.79 (1.66, 13.80) | 0.004 |
| Quartile 2 | 3.88 (1.60, 9.29) | 0.002 | 3.30 (1.22, 8.85) | 0.018 | 3.28 (1.21, 8.83) | 0.019 |
| Quartile 3 | 2.71 (1.12, 6.51) | 0.026 | 2.23 (0.78, 6.37) | 0.13 | 2.05 (0.70, 5.99) | 0.19 |
| Quartile 4 (referent) | – | – | – | |||
Model 1 adjusted for age, sex, and race.
Model 2 adjusted for Model 1 covariates, body mass index, heart failure, hypertension, diabetes, vascular disease, and treatment for atrial fibrillation (ablations, cardioversion, antiarrhythmic medications).
Model 3 adjusted for Model 2 covariates, annual household income, and educational attainment.
AFEQT indicates Atrial Fibrillation Effect on QualiTy of Life; HR, hazard ratio; CI, confidential interval.
4. Discussion
In a moderate-sized cohort of individuals with AF, we identified significant and consistent associations between validated, AF-specific patient-reported outcomes and adverse clinical events, specifically hospitalization. We noted a graded increase in risk of hospitalization as patient-reported outcomes declined. Our results underscore the importance of patient-reported outcomes as informative measures of health risk and clinical adversity in individuals with AF.
Our study is particularly relevant as patient-reported outcomes are increasingly used in clinical trials as primary endpoints. For example, the AFEQT was used in a multicenter randomized trial of over 2000 patients comparing catheter ablation and antiarrhythmic drug therapy in AF [9]. The AFEQT has also been used to investigate the merits of earlier cardioversion to maintain sinus rhythm in recent-onset AF [21]. Our results are consistent with a prior study, which showed that lower quality of life, a central patient-reported outcome in AF, was associated with higher hospitalization risk [22]. In contrast to being conducted in a large-sized, multi-center registry, our study was conducted in a single regional healthcare system, in which we expect individuals would have decreased heterogeneity in the evaluation and management of AF. In addition, AF treatment history and relevant medications, which may influence patient-reported outcomes, are accounted for in our multivariable-adjusted analyses. In sum, our study extends our understanding of the relation of patient-reported to clinical outcomes in AF.
We consider that our findings have important implications for patient care. The delivery of patient-centered care is essential to improving outcomes in cardiovascular disease. A higher level of patient engagement in decision-making and symptom management has been associated with better clinical outcomes in AF [23]. Implementation of patient-centered care may reduce length of hospital stay, enhance physical functioning, and increase self-efficacy in cardiovascular disease [24,25]. In our study, we established that patient-centered outcomes are associated with clinical outcomes in AF, even after consideration of demographic, socioeconomic, AF treatment history, and comorbid factors included in our multivariable adjustment. Measuring patient-reported outcomes in AF patients may identify individuals at increased hospitalization risk and thereby facilitate strategic interventions to prevent clinical adversity.
Strengths of our study include the use of a moderate-sized cohort within a single-center regional healthcare system, use of a disease-specific instrument that measures patient-reported outcomes with domains pertinent to the patient experience of AF, and inclusion of cardiac and AF-specific endpoints. Our study has several limitations. First, although the use of a moderate-sized, regional-based cohort enhanced the validity of our results, our cohort's generalizability is limited. Second, our analysis may not account for health care delivery factors that may affect the associations between patient-reported outcomes and the risk of hospitalization that we identified here. For example, it is possible that patients received attention and services not accounted for by this analysis. Third, we are unable to exclude the presence of additional covariates which may have confounded our analyses. Finally, although we identified an association between patient-reported outcomes and hospitalization, we did not account for a broad array of measures such as psychological function, functional status, and general health perceptions that may be relevant [26,27]. Future research is needed to identify the causal mechanisms that may explain the complicated mechanisms by which patient-reported outcomes may mediate hospitalization risk as observed in our study.
5. Conclusion
In conclusion, we identified a significant association between disease-specific patient-reported outcomes and hospitalization risk in a moderate-sized cohort of individuals with prevalent AF. Our findings extend our understanding of the relevance of patient-reported outcomes to clinical adversity in AF. Our study specifically validates the importance of assessing patient-reported outcomes to improve and focus care.
CRediT authorship contribution statement
Yimin Chen: Conceptualization, Methodology, Validation, Investigation, Writing- Original draft preparation, Visualization. Tarryn Tertulien: Writing- Reviewing and Editing. Andrew D. Althouse: Conceptualization, Methodology, Software, Formal analysis, Data curation, Visualization. Amber Johnson: Writing- Reviewing and Editing. Brittany Gisi: Writing- Reviewing and Editing. Jared W. Magnani: Conceptualization, Methodology, Investigation, Writing- Review & Editing, Supervision, Project administration, Funding acquisition.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
None.
Sources of funding
This work was supported by NIH/National Heart, Lung, and Blood Institute grants R33HL144669 and R01HL143010.
Disclosures
Dr. Magnani is supported by NIH/National Heart, Lung, and Blood Institute grants as specified in the sources of funding. Dr. Magnani has full access to all data in the study and takes responsibility for its integrity and the data analysis. There are no other disclosures.
Footnotes
Subject term list: Atrial fibrillation, Quality and Outcomes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ahjo.2021.100007.
Appendix A. Supplementary data
Supplementary material
References
- 1.Dorian P., Jung W., Newman D., Paquette M., Wood K., Ayers G.M., Camm J., Akhtar M., Luderitz B. The impairment of health-related quality of life in patients with intermittent atrial fibrillation: implications for the assessment of investigational therapy. J. Am. Coll. Cardiol. 2000 doi: 10.1016/S0735-1097(00)00886-X. [DOI] [PubMed] [Google Scholar]
- 2.Randolph T.C., Simon D.J.N., Thomas L., Allen L.A., Fonarow G.C., Gersh B.J., Kowey P.R., Reiffel J.A., Naccarelli G.V., Chan P.S., Spertus J.A., Peterson E.D., Piccini J.P. Patient factors associated with quality of life in atrial fibrillation. Am. Heart J. 2016 doi: 10.1016/j.ahj.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Badia X., Arribas F., Ormaetxe J.M., Peinado R., de los Terreros M.S. Development of a questionnaire to measure health-related quality of life (HRQoL) in patients with atrial fibrillation (AF-QoL) Health Qual. Life Outcomes. 2007 doi: 10.1186/1477-7525-5-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dorian P., Paquette M., Newman D., Green M., Connolly S.J., Talajic M., Roy D. Quality of life improves with treatment in the Canadian trial of atrial fibrillation. Am. Heart J. 2002 doi: 10.1067/mhj.2002.122518. [DOI] [PubMed] [Google Scholar]
- 5.Wokhlu A., Monahan K.H., Hodge D.O., Asirvatham S.J., Friedman P.A., Munger T.M., Bradley D.J., Bluhm C.M., Haroldson J.M., Packer D.L. Long-term quality of life after ablation of atrial fibrillation. The impact of recurrence, symptom relief, and placebo effect. J Am Coll Cardiol. 2010 doi: 10.1016/j.jacc.2010.01.040. [DOI] [PubMed] [Google Scholar]
- 6.January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, Conti JB, Ellinor PT, Ezekowitz MD, Field ME, Murray KT, Sacco RL, Stevenson WG, Tchou PJ, Tracy CM, Yancy CW. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation. J Am Coll Cardiol. 2014. doi: 10.1016/j.jacc.2014.03.022. [DOI] [PubMed]
- 7.Mont L., Bisbal F., Hernández-Madrid A., Pérez-Castellano N., Viñolas X., Arenal A., Arribas F., Fernández-Lozano I., Bodegas A., Cobos A., Matía R., Pérez-Villacastín J., Guerra J.M., Ávila P., López-Gil M., Castro V., Arana J.I., Brugada J. Catheter ablation vs. antiarrhythmic drug treatment of persistent atrial fibrillation: a multicentre, randomized, controlled trial (SARA study) Eur. Heart J. 2014 doi: 10.1093/eurheartj/eht457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Groenveld HF, Crijns HJGM, Van Den Berg MP, Van Sonderen E, Alings AM, Tijssen JGP, Hillege HL, Tuininga YS, Van Veldhuisen DJ, Ranchor A V., Van Gelder IC. The effect of rate control on quality of life in patients with permanent atrial fibrillation: data from the race II (Rate Control Efficacy In Permanent Atrial Fibrillation II) study. J Am Coll Cardiol. 2011. doi: 10.1016/j.jacc.2011.06.055. [DOI] [PubMed]
- 9.Mark D.B., Anstrom K.J., Sheng S., Piccini J.P., Baloch K.N., Monahan K.H., Daniels M.R., Bahnson T.D., Poole J.E., Rosenberg Y., Lee K.L., Packer D.L. Effect of catheter ablation vs medical therapy on quality of life among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA - Journal of the American Medical Association. 2019 doi: 10.1001/jama.2019.0692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bai Y., Bai R., Wu J.H., Zhang T., Liu N., Shi X.B., Liu X.Y., Liu X.H., Du X., Dong J.Z., Ma C.S. Differences in quality of life between atrial fibrillation patients with low stroke risk treated with and without catheter ablat. J. Am. Heart Assoc. 2015 doi: 10.1161/JAHA.115.002130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cherian T.S., Shrader P., Fonarow G.C., Allen L.A., Piccini J.P., Peterson E.D., Thomas L., Kowey P.R., Gersh B.J., Mahaffey K.W. Effect of atrial fibrillation on mortality, stroke risk, and quality-of-life scores in patients with heart failure (from the outcomes registry for better informed treatment of atrial fibrillation [ORBIT-AF]) Am. J. Cardiol. 2017 doi: 10.1016/j.amjcard.2017.02.050. [DOI] [PubMed] [Google Scholar]
- 12.Spertus J., Dorian P., Bubien R., Lewis S., Godejohn D., Reynolds M.R., Lakkireddy D.R., Wimmer A.P., Bhandari A., Burk C. Development and validation of the atrial fibrillation effect on QualiTy-of-life (AFEQT) questionnaire in patients with atrial fibrillation. Circ Arrhythmia Electrophysiol. 2011 doi: 10.1161/CIRCEP.110.958033. [DOI] [PubMed] [Google Scholar]
- 13.Kotecha D., Ahmed A., Calvert M., Lencioni M., Terwee C.B., Lane D.A. Patient-reported outcomes for quality of life assessment in atrial fibrillation: a systematic review of measurement properties. PLoS One. 2016 doi: 10.1371/journal.pone.0165790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lip GYH, Nieuwlaat R, Pisters R, Lane DA, Crijns HJGM, Andresen D, Camm AJ, Davies W, Capucci A, Olsson B, Aliot E, Cobbe S, Le Heuzey JY, Santini M, Vardas P, Manini M, Bramley C, Laforest V, Taylor C, Del Gaiso S, Huber K, De Backer G, Sirakova V, Cerbak R, Thayssen P, Lehto S, Blanc JJ, Delahaye F, Kobulia B, Zeymer U, Cokkinos D, Karlocai K, Graham I, Shelley E, Behar S, Maggioni A, Gonçalves L, Grabauskiene V, Asmussen I, Deckers J, Stepinska J, Mareev V, Vasiljevic Z, Riecansky I, Kenda MF, Alonso A, Lopez-Sendon JL, Rosengren A, Buser P, Okay T, Sychov O, Fox K, Schofield P, Simoons M, Wood D, Battler A, Boersma E, Fox K, Komajda M, McGregor K, Mulder B, Priori S, Ryde'n L, Vahanian A, Wijns W, Sanofi-Aventis, Grigoryan S V., Apetyan I, Aroyan S, Azarapetyan L, Anvari A, Gottsauner-Wolf M, Pfaffenberger S, Aydinkoc K, Kalla K, Penka M, Drexel H, Langer P, Pierard LA, Legrand V, Blommaert D, Schroeder E, Mancini I, Geelen P, Brugada P, De Zutter M, Vrints C, Vercammen M, Morissens M, Borisov B, Petrov VA, Marinova M, Assen A, Goudev R, Peychev Y, Stoyanovsky V, Stoynev E, Kranjcevic S, Moutiris J, Ioannides M, Evequoz D, Spacilova J, Novak M, Eisenberger M, Mullerova J, Kautzner J, Riedlbauchova L, Petru` J, Taborsky M, Cappelen H, Sharaf YA, Ibrahim BSS, Tammam K, Saad A, Elghawaby H, Sherif HZ, Farouk H, Mielke A, Breithardt G, Engelen M, Kirchhof P, Zimmermann P, Aviles FF, Rubio J, Malpartida F, Corona M, Sanchez LT, Miguel J, Herrera L, Quesada A, Garcia AJM, Gonzalez CS, Juango MSA, Berjon-Reyero J, Alegret JM, Fernandez JMC, Carrascosa C, Romero RAF, Lara MG, Sendon JLL, de Diego JJG, Martin LS, Irurita M, Guttierez NH, Rubio JRS, Antorrena I, Paves AB, Salvador A, Orriach MD, Garcia AA, Epelde F, Martinez VB, Sanchez AB, Galvez CP, Rivero RF, Madrid AH, Baron-Esquivias G, Peinado R, Guindal JAG, Vera TR, Fernandez EL, Gayan R, Garcia J, Bodegas A, Lopez JT, Florez JM, Cabezas CL, de Castroviejo EVR, Bellido JM, Ruiz ME, Savolainen K, Nieminen M, Toivonen L, Syvanne M, Pietila M, Galley D, Beltra C, Gay A, Daubert JC, Lecocq G, Poulain C, Cleland JGFC, Shelton R, Choudhury A, Abuladze G, Jashi I, Tsiavou A, Giamouzis G, Dagres N, Kostopoulou A, Tsoutsanis D, Stefanadis C, Latsios G, Vogiatzis I, Gotsis A, Bozia P, Karakiriou M, Koulouris S, Parissis J, Kostakis G, Kouris N, Kontogianni D, Athanasios K, Douras A, Tsanakis T, Marketou M, Patsourakos N, Czopf L, Halmosi R, Pre'da I, Csoti E, Badics A, Strasberg B, Freedberg NA, Katz A, Zalzstein E, Grosbard A, Goldhammer E, Nahir M, Epstein M, Vider I, Luria D, Mandelzweig L, Aloisi B, Cavallaro A, Antonielli E, Doronzo B, Pancaldo D, Mazzola C, Buontempi L, Calvi V, Giuffrida G, Figlia A, Ippolito F, Gelmini GP, Gaibazzi N, Ziacchi V, De Tommasi F, Lombardi F, Fiorentini C, Terranova P, Maiolino P, Albunni M, Pinna-Pintor P, Fumagalli S, Masotti G, Boncinelli L, Rossi D, Santoro GM, Fioranelli M, Naccarella F, Maranga SS, Lepera G, Bresciani B, Seragnoli E, Forti MC, Cortina V, Baciarello G, Cicconetti P, Lax A, Vitali F, Igidbashian D, Scarpino L, Terrazzino S, Tavazzi L, Cantu F, Pentimalli F, Novo S, Coppola G, Zingarini G, Ambrozio G, Moruzzi P, Callegari S, Saccomanno G, Russo P, Carbonieri E, Paino A, Zanetta M, Barducci E, Cemin R, Rauhe W, Pitscheider W, Meloni M, Marchi SM, Di Gennaro M, Calcagno S, Squaratti P, Quartili F, Bertocchi P, De Martini M, Mantovani G, Komorovsky R, Desideri A, Celegon L, Tarantini L, Catania G, Lucci D, Bianchini F, Puodziukynas A, Kavoliuniene A, Barauskiene V, Aidietis A, Barysiene J, Vysniauskas V, Zukauskiene I, Kazakeviciene N, Georgievska-Ismail L, Poposka L, Vataman E, Grosu AA, op Reimer WS, de Swart E, Lenzen M, Jansen C, Brons R, Tebbe H, van Hoogenhuyze DCA, Veerhoek MJ, Kamps M, Haan D, van Rijn N, Bootsma A, Baur L, van den A, Fransen H, Eurlings L, Meeder J, De Boer MJ, Winter J, Broers H, Werter C, Bijl M, Versluis S, Milkowska M, Wozakowska-Kaplon B, Janion M, Lepska L, Swiatecka G, Kokowicz P, Cybulski J, Gorecki A, Szulc M, Rekosz J, Manczak R, Wnuk-Wojnar AM, Trusz-Gluza M, Rybicka-Musialik A, Myszor J, Szpajer M, Cymerman K, Sadowski J, Sniezek-Maciejewska M, Ciesla-Dul M, Gorkiewicz-Kot I, Grodzicki T, Rewiuk K, Kubik L, Lewit J, de Sousa JMFR, Ferreira R, Freitas A, Morais JCA, Pires R, Gomes MJV, Gago P, Candeias RAC, Nunes L, Sa JVM, Ventura M, de Oliveira M, Alves LB, Bostaca I, Olariu CT, Dan GA, Dan A, Podoleanu C, Frigy A, Georgescu GIM, Arsenescu C, Statescu C, Sascau R, Dimitrascu DL, Rancea R, Shubik Y V., Duplyakov D, Shalak M, Danielyan M, Galyavich A, Zakirova V, Hatala R, Kaliska G, Kmec J, Zupan I, Tasiè J, Vokac D, Edvardsson N, Poci D, Gamra H, Denguir H, Sepetoglu A, Arat-Ozkan A, Orynchak M, Paliy E, Vakalyuk I, Malidze D, Prog R, Yabluchansky MI, Makienko NV, Potpara T, Knezevic S, Randjelovic M. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the Euro Heart Survey on atrial fibrillation. Chest. 2010. doi: 10.1378/chest.09-1584. [DOI] [PubMed]
- 15.Gisi B., Althouse A.D., Mathier A.S., Pusateri A., Rollman B.L., LaRosa A., Magnani J.W. The unmeasured burden: contribution of depression and psychological stress to patient-reported outcomes in atrial fibrillation. Int. J. Cardiol. 2020 doi: 10.1016/j.ijcard.2019.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guhl E., Althouse A., Sharbaugh M., Pusateri A.M., Paasche-Orlow M., Magnani J.W. Association of income and health-related quality of life in atrial fibrillation. Open Hear. 2019 doi: 10.1136/openhrt-2018-000974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.LaRosa A.R., Pusateri A.M., Althouse A.D., Mathier A.S., Essien U.R., Magnani J.W. Mind the gap: deficits in fundamental disease-specific knowledge in atrial fibrillation. Int. J. Cardiol. 2019 doi: 10.1016/j.ijcard.2019.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Holmes D.N., Piccini J.P., Allen L.A., Fonarow G.C., Gersh B.J., Kowey P.R., O’Brien E.C., Reiffel J.A., Naccarelli G.V., Ezekowitz M.D., Chan P.S., Singer D.E., Spertus J.A., Peterson E.D., Thomas L. Defining clinically important difference in the atrial fibrillation effect on quality-of-life score. Circ Cardiovasc Qual Outcomes. 2019 doi: 10.1161/CIRCOUTCOMES.118.005358. [DOI] [PubMed] [Google Scholar]
- 19.Amorim L.D.A.F., Cai J. Modelling recurrent events: a tutorial for analysis in epidemiology. Int. J. Epidemiol. 2015 doi: 10.1093/ije/dyu222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Andersen P.K., Gill R.D. Cox’s regression model for counting processes: a large sample study. Ann. Stat. 1982 doi: 10.1214/aos/1176345976. [DOI] [Google Scholar]
- 21.Pluymaekers N.A.H.A., Dudink E.A.M.P., Luermans J.G.L.M., Meeder J.G., Lenderink T., Widdershoven J., Bucx J.J.J., Rienstra M., Kamp O., Van Opstal J.M., Alings M., Oomen A., Kirchhof C.J., Van Dijk V.F., Ramanna H., Liem A., Dekker L.R., Essers B.A.B., Tijssen J.G.P., Van Gelder I.C., Crijns H.J.G.M. Early or delayed cardioversion in recent-onset atrial fibrillation. N Engl J Med. 2019 doi: 10.1056/nejmoa1900353. [DOI] [PubMed] [Google Scholar]
- 22.Freeman J.V., Simon D.N., Go A.S., Spertus J., Fonarow G.C., Gersh B.J., Hylek E.M., Kowey P.R., Mahaffey K.W., Thomas L.E., Chang P., Peterson E.D., Piccini J.P. quality of life, and patient outcomes: results from the outcomes registry for better informed treatment of atrial fibrillation (ORBIT-AF). Circ Cardiovasc Qual Outcomes. 2015. Association between atrial fibrillation symptoms. [DOI] [PubMed] [Google Scholar]
- 23.McCabe P.J., Stuart-Mullen L.G., McLeod C.J., Byrne T.O., Schmidt M.M., Branda M.E., Griffin J.M. Patient activation for self-management is associated with health status in patients with atrial fibrillation. Patient Prefer Adherence. 2018 doi: 10.2147/PPA.S172970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ekman I., Wolf A., Olsson L.E., Taft C., Dudas K., Schaufelberger M., Swedberg K. Effects of person-centred care in patients with chronic heart failure: the PCC-HF study. Eur. Heart J. 2012 doi: 10.1093/eurheartj/ehr306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fors A., Swedberg K., Ulin K., Wolf A., Ekman I. Effects of person-centred care after an event of acute coronary syndrome: two-year follow-up of a randomised controlled trial. Int. J. Cardiol. 2017 doi: 10.1016/j.ijcard.2017.08.069. [DOI] [PubMed] [Google Scholar]
- 26.Walters T.E., Wick K., Tan G., Mearns M., Joseph S.A., Morton J.B., Sanders P., Bryant C., Kistler P.M., Kalman J.M. Symptom severity and quality of life in patients with atrial fibrillation: psychological function outweighs clinical predictors. Int. J. Cardiol. 2019 doi: 10.1016/j.ijcard.2018.10.101. [DOI] [PubMed] [Google Scholar]
- 27.Ferrans C.E., Zerwic J.J., Wilbur J.E., Larson J.L. Conceptual model of health-related quality of life. J. Nurs. Scholarsh. 2005 doi: 10.1111/j.1547-5069.2005.00058.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material


