Abstract
Introduction
Anemia remains a major public health problem for children in sub-Saharan Africa (SSA). Iron-rich foods consumption has a determinant role on the anemia status. Hence, this study aimed to determine the prevalence of good consumption of iron-rich foods and its associated factors among children aged 6–23 months in SSA.
Materials and methods
The recent Demographic and Health Survey data sets of thirty-five SSA countries were used. Data were analyzed using STATA/MP version 16.0 and all statistical analyses were done after weighting the data. A generalized linear mixed model using Poisson regression with robust error variance was used to determine factors associated with good consumption of iron-rich food. Association of variables was declared at a p-value of ≤0.05 and adjusted prevalence ratio (aPR) ratio with its 95% confidence interval (CI) was calculated for each variable.
Results
The total weighted samples of 77,001 children aged 6–23 months were included. The prevalence of consumption of iron rich foods was 42.1% (95% CI: 41.78–42.48). Children with age of 12–17 (adjusted prevalence ratio (aPR) = 1.96, 95% CI: 1.89–2.04) and 18–23 months (aPR = 2.05, 95% CI: 1.97–2.14), who took drugs for intestinal parasites (aPR = 1.30, 95% CI: 1.26–1.34), with postnatal check within 2 months (aPR = 1.09, 95% CI: 1.06–1.13), and children from women with ANC visit of 1–3 (aPR = 1.31, 95% CI: 1.24–1.37) and ≥4 (aPR = 1.41, 95% CI: 1.34–1.48) had higher prevalence of good consumption of iron rich foods. Moreover, the prevalence of consumptions of iron rich foods was higher among children from; family with rich (aPR = 1.36, 95%CI: 1.30–1.42) and middle (aPR = 1.14 95% CI: 1.09–1.19) wealth index, and mother with media exposure (aPR = 1.26, 95%CI: 1.22–1.31).
Conclusion
The prevalence of good consumption of iron-rich foods among children aged 6–23 months in SSA countries is low. Child factors, family factors, and community-level factors were significantly associated with consumption of iron rich foods. Strategies to increase the consumption of iron-rich foods during this critical stage of growth and development should be designed in SSA.
Introduction
One in two under-five children suffer from hidden hunger (micronutrient deficiency) [1], and iron deficiency (ID) is the world’s commonest micronutrient deficiency affecting more than 2 billion people in the world, with the highest-burden in African children [2, 3]. This most widespread nutritional deficiency, ID, is the primary cause of iron deficiency anemia (IDA) (hemoglobin levels of < 11g/dl) [4, 5]. Almost half, 47% of under-five children are anemic, which is mainly attributed to ID [6].
The low oxygen-carrying capacity of blood in anemia leads to lack of oxygen supply to the fast-growing children’s brain and negatively affects mental, motor, and cognitive development, which in turn lead to social withdrawal, attention deficit, and impaired school performance of children [7–9]. Iron deficiency in the absence of anemia is even more frequent and has a similar negative impact on mental development which may be irreversible, especially in children less than 2 years, despite adequate therapy [10, 11]. In severe cases, iron deficiency anemia in children is associated with increased mortality [12] and heart failure [13].
According to the 2011 world health organization(WHO) report, anemia affects 60.2% of African children aged 6–59 months, with the highest prevalence in under-five children of sub-Saharan countries, ranging from 74 to 86%, and is primarily due to ID [6]. Iron deficiency in SSA countries is highly prevalent and ranges from 21.7% to 41.9% [14].
The most vulnerable groups to iron deficiency are under-two children who are in high iron demand due to the rapid growth and brain development. As a result, WHO recommends daily iron supplementation for this age group, 6–23 months, in areas where the prevalence of anemia is 40% or greater [15]. Moreover, numerous countries design preventive strategies and conduct interventions like iron supplementation and deworming. However, anemia remains a major public health problem in children in the world, especially in SSA [12].
The possible causes of ID during early childhood are increased iron needs due to rapid growth, inadequate iron intake due to exclusively breastfed without iron supplementation, inadequate dietary iron intake, low availability of dietary sources of iron secondary to low socioeconomic status, and dietary restrictions [16]. Thus, to prevent ID in children older than 6 months, the American Academy of Pediatrics and WHO recommend the introduction and consumption of two servings per day of iron-rich complementary foods, including iron-fortified cereals and pureed meats [17–19]. However, less than half (17–65%) of children consumed iron-rich foods regularly [20]. Iron-rich foods were not commonly consumed among infants in urban areas of China [21]. More than half of infants did not consume the recommended iron-rich food [22] and the consumption of meat, the main iron source, in Africa is the lowest in the world [23]. In French-speaking African countries and Ethiopia, consumption of iron-rich foods ranges from 17–65% [20, 24]. Some of the factors that affect children’s consumption of iron-rich foods include lack of awareness of mothers on iron-rich foods, child age, maternal education, religion, household wealth status, and feeding culture [23–25].
Though iron-rich foods consumption is the main determinant of anemia and a strategy targeted for adequate intake of iron could be achievable and improved [26], there has not been a continent-wide analysis that identified iron-rich foods consumption status and its determinants in children aged 6–23 months in sub-Saharan Africa. Therefore, this study aimed to determine the prevalence of good consumption of iron-rich foods and its associated factors among children aged 6–23 months in sub-Saharan Africa.
The information from this study will help for effective nutritional interventions and assist government and non-governmental organizations, health practitioners, and policymakers to design intervention strategies to improve consumption of iron-rich foods for the most vulnerable group in the most vulnerable sub-regions within SSA.
Materials and methods
Data source
We used the appended most recent nationally representative demographic and health survey (DHS) datasets of 35 sub-Saharan Africa countries. The DHS, collected every five years, is a nationally representative survey that provides population and health indicators at the regional and national levels. DHS surveys are designed to collect data on marriage, fertility, family planning, reproductive health, child health, nutrition, HIV/AIDS, and mortality. Pre-tested and standard DHS questionnaires were used for data collection of the DHS surveys. The questionnaire was conceptualized to the different countries context and the data were collected by trained data collectors [27]. The datasets were obtained from the measure DHS Program at https://www.dhsprogram.com/data/dataset_admin/login_main.cfm.
Those countries with no data on the outcome variable (Sierra Leone and Sudan) were excluded from the analysis. The total weighted samples of 77,001 children aged 6–23 months were included in the study.
Variables of the study
Dependent variable
The dependent variable of this study was children’s (aged 6–23 months) consumption of iron-rich foods, dichotomized as good and poor. According to the DHS, consumption of at least one iron-rich food item among the four food items: meat (beef, pork, lamb, chicken, etc.), egg, organ meat(liver, heart, or other organs), and fish or shellfish at any time in the last 24 hours before the interview was considered as good consumption. On the other hand, no history of iron-rich food consumption in the last 24 hours period preceding the interview was declared as poor consumption [27].
Independent variables
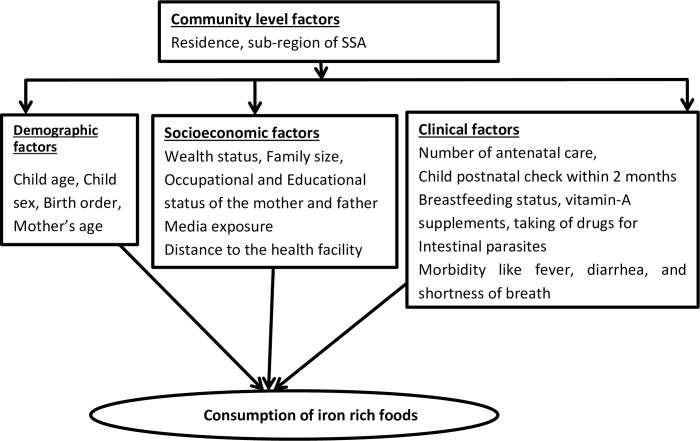
This study included both individual and community-level variables. The individual-level variables were age (6–11, 12–17, and 18–23 months), sex (male or female), breastfeeding status of the child (yes or no), receiving vitamin-A supplements (yes or no), birth order (1, 2–4, and ≥5, mother’s age (<20, 20–34, 35–49 years), any morbidity like fever, diarrhea, and short breath(yes or no), taking of drugs for intestinal parasites (yes or no), educational status of the mother and father (no education, primary, secondary, and higher), occupational status of mother and father (working or not working), number of antenatal care (ANC) (not at all, 1–3, and 4–16), child postnatal check within 2 months (yes or no), family size (≤5 or >5), wealth status (poor, middle, and rich), distance to the health facility (big problem or not a big problem), and media exposure (media exposure was created from the three variables: watching television, listening radio, and reading a newspaper, and labeled as yes if a woman has exposure to either of the three media sources or no if a woman has exposure to none of them). Residence (urban or rural) and region of SSA (East Africa, West Africa, Central Africa, and southern Africa) were the community-level variables (Fig 1).
Fig 1. Conceptual framework for factors associated with consumption of iron rich foods in SSA.
Data analysis procedure
We used STATA version 16.0/MP software for analysis. Before doing any analysis, the data were weighted to ensure the representativeness of the DHS sample and get reliable estimates and standard error [27].
To account for the hierarchical nature of DHS data, since children are within household and household are within the cluster resulting in the correlation of observations which violate the assumption of independence, measures of community variation: Intra-class Correlation Coefficient (ICC); Median Odds Ratio (MOR) and Proportional Change in Variance (PCV) were estimated. We fitted four models: the null-model (without independent variables), model I (only individual-level variables), model II (only community-level variables), and model III (both the individual and community level variables). The smallest deviance value was observed in Model III and hence was the best-fitted model.
Since the outcome variable, good consumption of iron rich foods, is a common problem (42. 1%), a generalized linear mixed model using Poisson regression with robust error variance was employed to identify the associated factors of iron-rich foods consumption among children 6–23 months in SSA. We fitted the bi-variable and multivariable multilevel robust Poisson regression to select variables. So, we choose variables with p-value less than 0.25 in the bi-variable analysis for the multivariable analysis and we considered those clinically important variables. During the bi-variable analysis all the clinically important predictors which were available in the DHS data had p-value less than 0.25. So we have not missed important variables which were reported and assumed as significant predictors of iron rich food consumption. Therefore, we have used stepwise approach than backward elimination and forward variable selection methods considering the clinical significance. Moreover, to choose the variables we have used LLR and pseudo-R2-value to check whether the included variable can cause model improvement. In the multivariable multilevel robust Poisson regression analysis, we used the adjusted prevalence ratio (aPR) with 95% CI and p-value of ≤ 0.05 to declare the statistical significance of the variables.
Ethics consideration
We obtained written consent of downloading and using SSA countries DHS dataset from the International Review Board of Demographic and Health Surveys (DHS) program data archivists after submitting a concept note and description of this study.
Results
Characteristics of the study participants
A total weighted sample of 77,001 children aged 6–23 months was included in this study. More than half (50.7%) of the children were male and 27,077(35.2%) were in the age group of 12–17 months. More than two-thirds of children (68.9%) were rural dwellers. The majorities of mothers were currently working 50,513 (65.6%) and married 53,880 (70.0%). Thirty-four thousand and two hundred twenty-nine (44.5%) of children were from households with poor wealth index. More than half (56.4%) of the children aged 6–23 months lived in a family size of ≥5. Around forty-nine thousand (63.9%) respondents have media exposure and distance of health facility was not a big problem to access medical care for 43,951(57.1%) respondents. Nearly half (47.9%) of children were 2nd to 4th birth order and most (79.3%) children were breastfeeding. The majority (83%) of children received vitamin-A in the first 2-months after delivery. The highest number 28,472 (37%) of children were from West Africa followed by east Africa 25,989 (33.75%) (Table 1).
Table 1. Socio-demographic characteristics of the children aged 6–23 months and respondents, demographic and health survey of sub-Saharan Africa (n = 77,001).
| Variables | Category | Weighted Frequency | Prevalence |
|---|---|---|---|
| Child age in months | 6–11 | 26,723 | 34.7% |
| 12–17 | 27,077 | 35.2% | |
| 18–23 | 23,201 | 30.1% | |
| Child sex | Male | 39,011 | 50.7% |
| Female | 37,990 | 49.3% | |
| Residence | Urban | 23,989 | 31.2% |
| Rural | 53,013 | 68.9% | |
| Mother’s age in years | < 20 | 11,845 | 15.4% |
| 20–34 | 50,692 | 65.8% | |
| 35–49 | 14,465 | 18.8% | |
| Mother’s educational level | No education | 27,977 | 36.3% |
| Primary | 26,801 | 34.8% | |
| Secondary | 19,452 | 25.3% | |
| Higher | 2,772 | 3.6% | |
| Mother’s occupation | Not working | 26,488 | 34.4% |
| Working | 50,513 | 65.6% | |
| Mother marital status | Married | 53,880 | 70.0% |
| Not married | 23,121 | 30.0% | |
| Father educational level | No education | 32,342 | 42.0% |
| Primary | 20,582 | 26.7% | |
| Secondary | 19,107 | 24.8% | |
| Higher | 4,971 | 6.5% | |
| Father occupation | Not working | 13,260 | 17.2% |
| Working | 63,742 | 83.0% | |
| Wealth index | Poor | 34,229 | 44.5% |
| Middle | 15,602 | 20.3% | |
| Rich | 27,170 | 35.3% | |
| Family size | ≤5 | 33,587 | 43.6% |
| >5 | 43,414 | 56.4% | |
| Media exposure | Yes | 49,172 | 63.9% |
| No | 27,796 | 36.3% | |
| Distance of health facility (getting medical help for self) | Big problem | 33,051 | 42.9% |
| Not a big problem | 43,951 | 57.1% | |
| Number of ANC | No at all | 11,747 | 15.3% |
| 1–3 | 25,018 | 32.5% | |
| 4–6 | 40,236 | 52.3% | |
| Birth order | 1 | 16,957 | 22.0% |
| 2–4 | 36,870 | 47.9% | |
| ≥5 | 23,174 | 30.0% | |
| Child is twin | Yes | 2,322 | 3.0% |
| No | 74,678 | 97.0% | |
| Current breast feeding | Yes | 61,074 | 79.3% |
| No | 15,927 | 20.7% | |
| Received vitamin-A in the first 2-monthes after delivery | Yes | 13,079 | 17.0% |
| No | 63,922 | 83.0% | |
| Child postnatal check within 2 months | Yes | 26,988 | 35.0% |
| No | 50,013 | 65.0% | |
| Had diarrhea recently | Yes | 20,389 | 26.5% |
| No | 56,612 | 73.5% | |
| Fever in the last two weeks | Yes | 21,646 | 28.1% |
| No | 55,355 | 71.9% | |
| Short rapid breath | Yes | 9,339 | 12.3% |
| No | 67,662 | 87.9% | |
| Drugs for intestinal parasites in last 6 months | Yes | 26,209 | 34.0% |
| No | 50,792 | 66.0% | |
| Sub-regions of sub-Saharan Africa countries | East Africa | 25,989 | 33.8% |
| West Africa | 28,472 | 37.0% | |
| Central Africa | 11,352 | 14.7% | |
| Southern Africa | 11,188 | 14.5% |
ANC: Antenatal care.
Random effect analysis
In the null model, the values of Intra Class Correlation (ICC = 1.85%) and Median Odds Ratio (MOR = 1.08) implies the presence of clustering or community level variability of consumption of iron foods. Around 2% of the variation in consumption of iron-rich foods attributed to ICC. In the null model, the presence of heterogeneity of iron-rich food consumption between clusters was indicated by the MOR with a value of 1.08. It indicates that if we randomly select a 6–23 months old child, a child at the cluster with higher consumption of iron-rich foods had around 1.1 higher prevalence of consumption of iron-rich foods than a child at cluster with lower consumption of iron-rich food. Model III had the lowest deviance value (115,708.54) and hence it was selected as the best-fitted model (Table 2).
Table 2. Random effect analysis and model comparison results.
| Parameters | Null model | Model I | Model II | Model III |
|---|---|---|---|---|
| Community-level variance | 0.0062 (0.0038–0 .0104) | 0.0009(0.00007–0.0122) | 0.0041(0.002–0.009) | 0.00019(1.56e-09–25.26) |
| ICC | 1.85% | 0.03% | 0.12% | 0.006% |
| MOR | 1.082 | 1.029 | 1.062 | 1.013 |
| PCV | Ref | 85.484% | 33.87% | 96.94% |
| Deviance(-2LL) | 121,795.72 | 117,424.38 | 120,125.23 | 115,708.54 |
ICC: Intra Class Correlation Coefficient, MOR: Median Odds Ratio, PCV: Proportional Change in Variance.
Consumption of iron-rich foods and associated factors
The magnitude of iron-rich food consumption among children aged 6–23 months in SSA was 42.1% (95% CI: 41.78–42.48). Fish or shellfish was the most (15%) consumed food, while liver, heart, and other organs were the least (4.4%) consumed iron-rich foods (Table 3).
Table 3. Consumption of iron rich foods among children aged 6–23 months, sub-Saharan Africa (n = 77,001).
| Variables | Category | Weighted Frequency | Percent(95%CI) |
|---|---|---|---|
| Iron rich food consumption in the last 24 hours | Good | 32,440 | 42.1(41.78–42.48) |
| Poor | 44,561 | 57.8 (57.52–58.22) | |
| Gave child egg in the last 24 hours | Yes | 10,530 | 13.7 |
| No | 66,471 | 86.3 | |
| Gave child meat (beef, pork, lamb, chicken, etc.) in the last 24 hours | Yes | 12,257 | 15.9 |
| No | 64,745 | 84.1 | |
| Gave child liver, heart, other organs in the last 24 hours | Yes | 3,356 | 4.4 |
| No | 73,645 | 95.6 | |
| Gave child fish or shellfish in the last 24 hours | Yes | 20,117 | 26.1 |
| No | 56,884 | 73.9 |
Both bivariable and multivariable multilevel Poisson regression analyses were employed to identify factors associated with iron-rich foods consumption. In the bivariable analysis, child age, birth order, current breastfeeding status, vitamin A intake, postnatal check within 2 months, fever, short rapid breath, use of drugs for intestinal parasites in last 6 months, maternal and paternal education and occupation, wealth index, family size, media exposure, the distance of health facility, number of ANC visit, residence and region of SSA were the candidate variables for the multilevel multivariable Poisson regression (p<0.25). Whereas, child age, current breastfeeding status, postnatal check within 2 months, use of drugs for intestinal parasites in last 6 months, maternal working status, maternal and paternal education, wealth index, media exposure, number of ANC visit, residence and region of SSA were significantly associated with good consumption of iron-rich foods in the multilevel multivariable Poisson regression (p≤ 0.05).
The prevalence of good consumption of iron among Children aged 12–17 and 18–23 months were 48% (adjusted prevalence ratio (aPR) = 1.48, 95% confidence interval (CI): 1.45–1.53), and 53% (aPR = 1.53, 95%CI: 1.49–1.58) higher, respectively, as compared with a child aged 6–11 months.
Children who were currently breastfeeding had a 14% (aPR = 1.14, 95%CI: 1.12–1.17) higher prevalence of good consumption of iron-rich foods compared to their counterparts. Child postnatal check within 2 months increased the likelihood of good consumption of iron-rich foods by 4% (aPR = 1.04, 95% CI: 1.01–1.06). Good consumption of iron-rich foods among 6–23 months aged children who took drugs for intestinal parasites in the last 6 months was 13% (aPR = 1.30, 95% CI: 1.11–1.15) higher as compared to those who didn’t take. Compared to children from women with no ANC visit, children from women with ANC visit of 1–3 and ≥4 had 17% (aPR = 1.17, 95% CI: 1.13–1.21), and 21% (aPR = 1.21, 95% CI: 1.17–1.25) higher consumption of iron-rich foods. Children from mothers with the educational level of primary, secondary and higher education had 14% (aPR = 1.14, 95% CI: 1.10–1.17), 18% (aPR = 1.18, 95% CI: 1.14–1.22), and 24%(aPR: 1.24, 95% CI: 1.17–1.30) higher prevalence of consumption of iron-rich foods, respectively, than children from non-educated mothers. The prevalence of good consumption of iron-rich foods among children from currently working mothers was 10% (aPR = 1.10, 95% CI: 1.08–1.13) higher than those of children from not currently working mothers. Primary, secondary, and higher educational level of the father was associated with 9% (aPR = 1.09, 95% CI: 1.06–1.12), 13% (aPR = 1.13, 95% CI: 1.10–1.17), and 15% (aPR = 1.15, 95% CI: 1.10–1.20) higher prevalence of children’s good consumption of iron-rich foods, respectively, than that of children from non-educated fathers. Children from a family with rich and middle wealth index had 6% (aPR = 1.06, 95%CI: 1.03–1.09), and 14% (aPR = 1.14 95% CI: 1.10–1.18) higher prevalence of good consumption of iron-rich foods than children from a family with poor wealth index.
Children from the urban area had 14% (aPR = 1.14, 95% CI: 1.11–1.18) higher prevalence of consuming iron-rich foods than a child from a rural area. Children from a woman with Media exposure had 15% (aPR = 1.26, 95%CI: 1.12–1.17) higher prevalence of consumption of iron-rich foods as compared to children from a woman with no media exposure. Children from West Africa, Central Africa, and Southern Africa countries had 31% (aPR = 1.31, 95% CI: 1.26–1.35), 48% (aPR = 1.48, 95% CI: 1.42–1.53), and 52% (aPR = 1.52, 95% CI: 1.46–1.57) higher prevalence of good consumption of iron-rich foods, respectively, than children from east Africa countries (Table 4).
Table 4. Multilevel Poisson regression analyses of good consumption of iron in sub-Saharan Africa (n = 77,001).
| Variables | Good consumption | Prevalence Ratio (95% Confidence Interval) | |||
|---|---|---|---|---|---|
| Yes | No | uPR | aPR | ||
| N (%) | N (%) | ||||
| Child age in months | 6–11 | 8,090(24.94) | 18,633(41.81) | 1 | 1 |
| 12–17 | 12,624(38.91) | 14,453(32.43) | 1.53(1.49–1.56) | 1.48(1.45–1.53)* | |
| 18–23 | 11,726(36.15) | 11,476(25.75) | 1.66(1.63–1.70) | 1.53(1.49–1.58)* | |
| Child sex | Male | 16,482 (50.81) | 15,958(49.19) | 1.00(0.98–1.02) | |
| Female | 22,529 (50.56) | 22,032(49.44) | 1 | ||
| Residence | Urban | 13,319(41.06) | 10,670 (23.94) | 1.44(1.41–1.48) | 1.14(1.11–1.18)* |
| Rural | 19,121(58.94) | 33,892(76.06) | 1 | 1 | |
| Mother’s age in years | < 20 | 4,668(14.39) | 7,176(16.10) | 1 | 1 |
| 20–34 | 21,744(67.03) | 28,948(64.96) | 1.07(1.05–1.09) | 1.05(0.99–1.05) | |
| 35–49 | 6,028(18.58) | 8,437(18.93) | 1.05(1.0–1.07) | 1.03(0.98–1.087) | |
| Mother’s educational level | No education | 9,138(28.17) | 18,839(42.28) | 1 | 1 |
| Primary | 10,956 (33.77) | 15,845(35.56) | 1.25(1.22–1.28) | 1.14(1.10–1.17)* | |
| Secondary | 10,567(32.58) | 8,884(19.94) | 1.65(1.60–1.69) | 1.18(1.14–1.22)* | |
| Higher | 1,779(5.48) | 993(2.23) | 1.90(1.83–1.98) | 1.24(1.17–1.30)* | |
| Mother’s Occupation | Not working | 10,662(32.87) | 15,826(35.51) | 1 | 1 |
| Working | 21,778(67.13) | 28,736(64.49) | 1.07(1.05–1.09) | 1.10(1.08–1.13)* | |
| Father Educational level | No education | 11,753(36.23) | 20,589(46.20) | 1 | 1 |
| Primary | 7,878 (24.28) | 12,704(28.51) | 1.07(1.05–1.10) | 1.09(1.06–1.12)* | |
| Secondary | 9,883(30.46) | 9,224(20.70) | 1.42(1.39–1.45) | 1.13(1.10–1.17)* | |
| Higher | 2,927(9.02) | 2,045(4.59) | 1.57(1.52–1.62) | 1.15(1.10–1.20)* | |
| Father Occupation | Not working | 5,968 (18.40) | 7,292(16.36) | 1 | 1 |
| Working | 26,472(81.60) | 37,270(83.64) | 0.93(0.91–0.94) | 0.94(0.92–0 .97) | |
| Wealth Index | Poor | 11,866(36.58) | 22,363 (50.18) | 1 | 1 |
| Middle | 6,420(19.79) | 9,182(20.61) | 1.21(1.18–1.24) | 1.06(1.03–1.09)* | |
| Rich | 14,154(43.63) | 13,016(29.2) | 1.47(1.43–1.50) | 1.14(1.10–1.18)* | |
| Family Size | ≤5 | 14,498(44.69) | 19,088 (42.84) | 1.03(1.02–1.05) | 0.98(0.96–1.00) |
| >5 | 17,941(55.31) | 25,473(57.16) | 1 | 1 | |
| Media Exposure | Yes | 23,244(71.68) | 25,928(58.21) | 1.41(1.38–1.43) | 1.15(1.12–1.17)* |
| No | 9,186(28.32) | 18,611(41.79) | 1 | 1 | |
| Distance of health facility (getting medical help for self) | Big problem | 12,784(39.41) | 20,266(45.48) | 1 | 1 |
| Not a big problem | 19,656(60.59) | 24,295(54.52) | 1.17(1.15–1.19) | 1.01(0.99–1.04) | |
| Birth order | 1 | 7,615 (23.47) | 9,342(20.97) | 1 | 1 |
| 2–4 | 16,035(49.43) | 20,835(46.76) | 0.96(0.96–0 .99) | 0.95(0.95–1.00) | |
| ≥5 | 8,790(27.10) | 14,384(32.28) | 0.87(0.85–0.89) | 0.97(0.93–1.00) | |
| Child is Twin | Yes | 997(3.07) | 1,326(2.97) | 0.99(0.93–1.05) | |
| No | 31,442(96.93) | 43,236(97.03) | 1 | ||
| Number of ANC | No at all | 3,830(11.81) | 7,917(17.77) | 1 | 1 |
| 1–3 | 9,542(29.41) | 15,476(34.73) | 1.18(1.15–1.22) | 1.17(1.13–1.21)* | |
| ≥4 | 19,068(58.78) | 21,168(47.50) | 1.45(1.40–1.49) | 1.21(1.17–1.25)* | |
| Current Breast Feeding | Yes | 23,074(71.13) | 37,999(85.27 | 1 | 1 |
| No | 9,365(28.87) | 6,562(14.73) | 1.54(1.51–1.57) | 1.14(1.12–1.17)* | |
| Received vitamin-A in the first 2-monthes after delivery | Yes | 6,056(18.67) | 7,023(15.76) | 1.11(1.09–1.14) | 1.00(0.98–1.03) |
| No | 26,384(81.33) | 37,538(84.24) | 1 | 1 | |
| Child postnatal check within 2 months | Yes | 12,641(38.97) | 14,347(32.20) | 1.17(1.15–1.19) | 1.04(1.01–1.06)* |
| No | 19,799(61.03) | 30,215(67.80) | 1 | ||
| Had diarrhea recently | Yes | 8,592(26.48) | 11,798(26.47) | 1 | |
| No | 23,848(73.52) | 32,764(73.53) | 1.00(0.99–1.03) | ||
| Fever in the last two weeks | Yes | 8,936(27.55) | 12,710(28.52) | 1 | 1 |
| No | 23,503(72.45) | 31,852(71.48) | 1.03(1.01–1.04) | 0.99(0.97–1.02) | |
| Short rapid breath | Yes | 3,790(11.68) | 5,549(12.45) | 1 | 1 |
| No | 28,650(88.32) | 39,012(87.55) | 1.04(1.01–1.07) | 1.00(0.97–1.04) | |
| Drugs for intestinal parasites in last 6 months | Yes | 13,301(41.00) | 12,909(28.97) | 1.36(1.33–1.39) | 1.13(1.11–1.15)* |
| No | 19,139(59.00) | 31,653(71.03) | 1 | 1 | |
| Sub-Region of sub-Saharan Africa | East Africa | 8,628(26.60) | 17,361 (38.96) | 1 | 1 |
| West Africa | 11,931(36.78) | 16,541(37.12) | 1.22(1.19–1.25) | 1.31(1.26–1.35)* | |
| Central Africa | 5,768(17.78) | 5,583(12.53) | 1.49(1.44–1.53) | 1.48(1.42–1.53)* | |
| Southern Africa | 6,113(18.84) | 5,075(11.39) | 1.56(1.51–1.62) | 1.52(1.46–1.57)* | |
*p ≤ 0.05, uPR: Unadjusted Prevalence Ratio, aPR: Adjusted Prevalence Ratio, CI: Confidence Interval.
Discussion
Iron-rich foods consumption has a significant role in blood iron level and anemia status. However, there is no evidence of the consumption of iron-rich food status and its associated factors in SSA. Hence, this study determined the weighted prevalence of good consumption of iron-rich foods and its associated factors among children aged 6–23 months in SSA.
The weighted prevalence of good consumption of iron-rich foods among children aged 6–23 months in SSA was 42.1%, which is lower than the result of studies conducted in Australia (82.6%) [28], Ireland (90%) [29], Mexico (63.1%) [30], East Asia and the Pacific (62.5%) [31], China (51%) [21], and Bangladesh (50%) [32]. The lower prevalence of good consumption of iron-rich foods in SSA might be due to household’s food insecurity and poor economic status of SSA countries, the poorest in the world, which makes iron-rich foods or animal source foods unaffordable [33] while such foods are greatly accessible in high-income counties [23, 34]. Children 6–23 months in most regions of SSA consumed no animal source food, iron-rich foods [31], instead tubers and cereals are the most common food [35] and consumption of meat in Africa is the lowest in the world, influenced by economic, cultural, and religious factors [36].
In light of this low prevalence of consumption of iron-rich foods among children aged 6–23 months in SSA, it is imperative for nutrition programs to emphasize and improve consumption of iron rich foods, animal source foods, and other alternative foods rich in iron (vegetables and fruits) in SSA young children.
However, the prevalence of good consumption of iron-rich foods in the present study is higher than the prevalence reported in Zambia (33.1%) [37], Ethiopia (21.4%) [24], and Madagascar (19.6%) [38]. This divergent result could be due to a difference in socioeconomic status, beliefs, norms, and cultural practice of children feeding. In Ethiopia, animal source foods are consumed mostly only during holidays as they are considered luxurious foods instead of basic daily requirements. Moreover, animal and animal source foods rich in iron are used mainly for the market purpose [39]. In the case of Zambia, most (70%) of energy source is maize with low consumption of iron rich foods [33].
Individual and community-level variables were found to be associated with the consumption of iron rich foods. Children aged 12–23 months had higher prevalence of good consumption of iron-rich foods than children aged from 6–11 months. This is in line with studies elsewhere [31, 35, 40–42]. This lower consumption of iron-rich food in 6–12 months children as compared to older children might be due to the mother’s perceptions that children before the age of 1 year should not consume animal-source foods [43]. Moreover, older children have regular consumption of foods prepared for the family with a greater content of iron [44]. Therefore, there is a need for national strategies to enhance the consumption of iron-rich foods in infants.
As this study demonstrated, the use of drugs for intestinal parasites in the last 6 months for children aged 6–23 months was associated with higher prevalence of good consumption of iron-rich foods than those who didn’t use. This finding is in agreement with the study in Uganda [45]. This might be because women who use drugs for intestinal parasites for their children will have similar motivation and commitment to give iron-rich foods for their children and an opportunity to interact with health care providers, and hence get counseling on appropriate child nutrition. Moreover, taking drugs for intestinal parasites might increase children’s food intake, thereby increases the consumption of iron-rich foods [46].
Children from mothers and fathers with educational status of primary or higher had higher prevalence of good consumption of iron-rich foods than children whose parents were non-educated. This finding is in agreement with other studies [41, 47–51]. The higher odds of good consumption of iron-rich foods in children from educated parents might be due to better exposure to media, understanding of and more access to information about children’s feeding practices and consumption of iron-rich foods [51]. Moreover, higher education is also related to higher income that in turn allows them to afford more iron-rich foods, like meat.
In the present study children with a postnatal check (PNC) within 2 months had higher prevalence of good consumption of iron-rich foods which is in line with another study [35]. In agreement with the previous studies [41, 42, 52], in this study, children from mothers with ANC visits had higher prevalence of good consumption of iron-rich foods than their counterparts. The possible justification for the higher odds of good consumption of iron-rich foods among children with a postnatal check within 2 months and from the mothers with ANC visit might be because, during the ANC and PNC visits, mothers will have an opportunity to learn about healthy child nutrition and appropriate feeding practice and get motivated to nourish their children iron-rich foods [35]. Therefore it is imperative to promote community-based nutritional education, and offer universal ANC and PNC for mothers in SSA countries to improve consumption of iron-rich foods consumption.
Wealth index was the other factor that significantly associated with good consumption of iron-rich foods. In line with this study, studies elsewhere revealed the association of high wealth index with good consumption of iron-rich foods [31, 35, 41, 53–55]. This is obviously due to the high economic status resulting in better access to financial resources and information to afford iron-rich foods. It is revealed that a lack of financial resources is a barrier to access nutritious foods [35, 56]. Therefore, especially for low income households, it is imperative to give attention to other less expensive and easily affordable iron rich foods like vegetables and fruits.
Children from mothers with media exposure had higher prevalence of good consumption of iron-rich foods than the children whose mothers haven’t media exposure. It is in agreement with other studies [38, 57–59]. The association between mass media exposure and good consumption of iron-rich foods might be because of exposure to mass media, a great source of information for the society, has been found highly important in improving the knowledge and practices of mothers on infant and young child feeding by increasing caregivers access to health message on appropriate feeding practice of their children [60, 61].
The strength of this study, the first study to assess consumption of iron-rich foods among children aged 6–23 months at SSA level, includes; it uses large representative sample for children aged 6–23 months from the latest DHS data of SSA countries, and hence it is generalizable. This study assessed the association between individual, and community level variables and consumption of iron-rich foods using a multilevel Poisson regression model that accounts for the correlated nature of DHS data to get reliable estimates. However, the following limitations should be considered. First, this study couldn’t show casual associations because the data source is a cross-sectional survey. Second, there might be a recall bias as data was collected from the mother or the caregiver by interview. Third, since we have used secondary data, DHS data, consumption of plant-based iron rich foods and iron-fortified foods were not considered, which might have underestimated the prevalence of consumption of iron rich foods in our study. Moreover, their bioavailability was not assessed. Though the iron rich foods are consumed, their bioavailability is affected by concomitant dietary compositions that are either Fe absorption enhancers (ascorbic acid) or inhibitors (tea polyphnols). However, DHS didn’t consider them. Lastly, quantities of iron-rich foods consumed or adequacy of iron intake, according to WHO recommended daily allowance of iron, was not determined.
Conclusion
The prevalence of good consumption of iron-rich foods among children aged 6–23 months in SSA countries is low. Child factors: age, current breastfeeding status, drugs use for intestinal parasites in last 6 months; family factors; maternal and paternal education, maternal occupation, postnatal check within 2 months wealth index, media exposure, number of ANC visit; and community level factors: residence and sub-region of SSA were significantly associated with consumption of iron-rich foods. Strategies to increase consumption of iron-rich foods during this critical stage, the first two years of life, of growth and development should be designed by considering these modifiable factors for children in SSA. Moreover, strategies that allow the improvements of consumption of iron rich foods from other sources, instead of thinking only animal source foods, should be designed. We strongly recommend the forthcoming researchers to consider and investigate plant-based iron rich foods and bioavailability of iron rich foods using a primary data.
Acknowledgments
We would like to express our thanks to the MEASURE DHS Program for providing the dataset for this study.
List of abbreviations
- ANC
Antenatal Care
- ID
Iron deficiency
- IDA
Iron Deficiency Anemia
- PNC
Postnatal Check
- SSA
sub-Saharan Africa
- WHO
World Health Organization
Data Availability
All relevant data are within the paper.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.UNICEF. The State of The World’s Children 2019-Growing Well in a Changing World. 2019.
- 2.Kassebaum NJ, Jasrasaria R, Naghavi M, Wulf SK, Johns N, Lozano R, et al. A systematic analysis of global anemia burden from 1990 to 2010. Blood. 2014;123(5):615–24. doi: 10.1182/blood-2013-06-508325 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vos T, Abajobir AA, Abate KH, Abbafati C, Abbas KM, Abd-Allah F, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. 2017;390(10100):1211–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bateman RM, Sharpe MD, Jagger JE, Ellis CG, Solé-Violán J, López-Rodríguez M, et al. 36th International Symposium on Intensive Care and Emergency Medicine: Brussels, Belgium. 15–18 March 2016. Critical care (London, England). 2016;20(Suppl 2):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.WHO. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. World Health Organization, 2011. [Google Scholar]
- 6.WHO. The global prevalence of anaemia in 2011. Geneva: World Health Organization. 2015. [Google Scholar]
- 7.Ai Y, Zhao SR, Zhou G, Ma X, Liu J. Hemoglobin status associated with performance IQ but not verbal IQ in Chinese preschool children. Pediatrics international: official journal of the Japan Pediatric Society. 2012;54(5):669–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCann JC, Ames BN. An overview of evidence for a causal relation between iron deficiency during development and deficits in cognitive or behavioral function. The American journal of clinical nutrition. 2007;85(4):931–45. doi: 10.1093/ajcn/85.4.931 [DOI] [PubMed] [Google Scholar]
- 9.Beard JL, Connor JR. Iron status and neural functioning. Annual review of nutrition. 2003;23:41–58. doi: 10.1146/annurev.nutr.23.020102.075739 [DOI] [PubMed] [Google Scholar]
- 10.Radlowski EC, Johnson RW. Perinatal iron deficiency and neurocognitive development. Frontiers in human neuroscience. 2013;7:585. doi: 10.3389/fnhum.2013.00585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lozoff B, Beard J, Connor J, Felt B, Georgieff M, Schallert T. Long-lasting neural and behavioral effects of iron deficiency in infancy. Nutrition reviews. 2006;64(suppl_2):S34–S43. doi: 10.1301/nr.2006.may.s34-s43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scott SP, Chen-Edinboro LP, Caulfield LE, Murray-Kolb LE. The impact of anemia on child mortality: an updated review. Nutrients. 2014;6(12):5915–32. doi: 10.3390/nu6125915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adekanmbi AF, Ogunlesi TA, Olowu AO, Fetuga MB. Current trends in the prevalence and aetiology of childhood congestive cardiac failure in Sagamu. Journal of tropical pediatrics. 2007;53(2):103–6. doi: 10.1093/tropej/fml064 [DOI] [PubMed] [Google Scholar]
- 14.Muriuki JM, Mentzer AJ, Webb EL, Morovat A, Kimita W, Ndungu FM, et al. Estimating the burden of iron deficiency among African children. 2020;18(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.WHO. Daily iron supplementation in children 6–23 months of age 2016 [updated 25 November 2016; cited 2020 12 December]. Available from: https://www.who.int/elena/titles/iron_supplementation_children/en/.
- 16.Ziegler EE. Consumption of cow’s milk as a cause of iron deficiency in infants and toddlers. Nutrition reviews. 2011;69(suppl_1):S37–S42. doi: 10.1111/j.1753-4887.2011.00431.x [DOI] [PubMed] [Google Scholar]
- 17.Siega-Riz AM, Deming DM, Reidy KC, Fox MK, Condon E, Briefel RR. Food consumption patterns of infants and toddlers: where are we now? Journal of the American Dietetic Association. 2010;110(12):S38–S51. doi: 10.1016/j.jada.2010.09.001 [DOI] [PubMed] [Google Scholar]
- 18.Wagner C, Greer F. American Academy of Pediatrics Committee on Nutrition Prevention of rickets and vitamin D deficiency in infants, children, and adolescents. Pediatrics. 2008;122(5):1142–52. doi: 10.1542/peds.2008-1862 [DOI] [PubMed] [Google Scholar]
- 19.Jones AD, Ickes SB, Smith LE, Mbuya MN, Chasekwa B, Heidkamp RA, et al. W orld H ealth O rganization infant and young child feeding indicators and their associations with child anthropometry: a synthesis of recent findings. Maternal & child nutrition. 2014;10(1):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Diouf S, Folquet M, Mbofung K, Ndiaye O, Brou K, Dupont C, et al. Prevalence and determinants of anemia in young children in French-speaking Africa. Role of iron deficiency. Archives de pediatrie: organe officiel de la Societe francaise de pediatrie. 2015;22(11):1188–97. doi: 10.1016/j.arcped.2015.08.015 [DOI] [PubMed] [Google Scholar]
- 21.Yu P, Denney L, Zheng Y, Vinyes-Parés G, Reidy KC, Eldridge AL, et al. Food groups consumed by infants and toddlers in urban areas of China. Food & nutrition research. 2016;60(1):30289. doi: 10.3402/fnr.v60.30289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dee DL, Sharma AJ, Cogswell ME, Grummer-Strawn LM, Fein SB, Scanlon KS. Sources of supplemental iron among breastfed infants during the first year of life. Pediatrics. 2008;122(Supplement 2):S98–S104. doi: 10.1542/peds.2008-1315m [DOI] [PubMed] [Google Scholar]
- 23.Milford AB, Le Mouël C, Bodirsky BL, Rolinski S. Drivers of meat consumption. Appetite. 2019;141:104313. doi: 10.1016/j.appet.2019.06.005 [DOI] [PubMed] [Google Scholar]
- 24.Tiruneh SA, Ayele BA, Yitbarek GY, Asnakew DT, Engidaw MT, Gebremariam AD. Spatial distribution of iron rich foods consumption and its associated factors among children aged 6–23 months in Ethiopia: spatial and multilevel analysis of 2016 Ethiopian demographic and health survey. Nutrition Journal. 2020;19(1):1–13. doi: 10.1186/s12937-019-0518-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Berhanu Z, Alemu T, Argaw D. Predictors of inappropriate complementary feeding practice among children aged 6 to 23 months in Wonago District, South Ethiopia, 2017; case control study. BMC pediatrics. 2019;19(1):146. doi: 10.1186/s12887-019-1523-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kehoe L, Walton J, McNulty B, Nugent A, Flynn A. Dietary strategies for achieving adequate vitamin D and iron intakes in young children in Ireland. Journal of Human Nutrition and Dietetics. 2017;30(4):405–16. doi: 10.1111/jhn.12449 [DOI] [PubMed] [Google Scholar]
- 27.Croft TN, Marshall AM, Allen CK, Arnold F, Assaf S, Balian S. Guide to DHS statistics. Rockville, Maryland, USA: ICF. 2018. [Google Scholar]
- 28.Scott JA, Gee G, Devenish G, Ha D, Do L. Determinants and sources of iron intakes of Australian toddlers: findings from the SMILE cohort study. International journal of environmental research and public health. 2019;16(2):181. doi: 10.3390/ijerph16020181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.McCarthy EK, Ní Chaoimh C, Hourihane JOB, Kenny LC, Irvine AD, Murray DM, et al. Iron intakes and status of 2‐year‐old children in the Cork BASELINE Birth Cohort Study. Maternal & child nutrition. 2017;13(3):e12320. doi: 10.1111/mcn.12320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vdl Cruz-Góngora, Villalpando S, Shamah-Levy T. Prevalence of anemia and consumption of iron-rich food groups in Mexican children and adolescents: Ensanut MC 2016. Salud publica de Mexico. 2018;60:291–300. doi: 10.21149/8824 [DOI] [PubMed] [Google Scholar]
- 31.White JM, Bégin F, Kumapley R, Murray C, Krasevec J. Complementary feeding practices: Current global and regional estimates. Maternal & child nutrition. 2017;13:e12505. doi: 10.1111/mcn.12505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kabir I, Khanam M, Agho KE, Mihrshahi S, Dibley MJ, Roy SK. Determinants of inappropriate complementary feeding practices in infant and young children in Bangladesh: secondary data analysis of Demographic Health Survey 2007. Maternal & child nutrition. 2012;8:11–27. doi: 10.1111/j.1740-8709.2011.00379.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith LC, Alderman H, Aduayom D. Food insecurity in sub-Saharan Africa: new estimates from household expenditure surveys: Intl Food Policy Res Inst; 2006. [Google Scholar]
- 34.Ritchie H, Roser M. Meat and dairy production. Our World in Data. 2017. [Google Scholar]
- 35.Gewa CA, Leslie TF. Distribution and determinants of young child feeding practices in the East African region: demographic health survey data analysis from 2008–2011. Journal of Health, Population and Nutrition. 2015;34(1):6. doi: 10.1186/s41043-015-0008-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arimond M, Ruel MT. Dietary diversity is associated with child nutritional status: evidence from 11 demographic and health surveys. The Journal of nutrition. 2004;134(10):2579–85. doi: 10.1093/jn/134.10.2579 [DOI] [PubMed] [Google Scholar]
- 37.Marinda PA, Genschick S, Khayeka-Wandabwa C, Kiwanuka-Lubinda R, Thilsted SH. Dietary diversity determinants and contribution of fish to maternal and under-five nutritional status in Zambia. PloS one. 2018;13(9):e0204009. doi: 10.1371/journal.pone.0204009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rakotomanana H, Gates GE, Hildebrand D, Stoecker BJ. Situation and determinants of the infant and young child feeding (IYCF) indicators in Madagascar: analysis of the 2009 Demographic and Health Survey. BMC public health. 2017;17(1):812. doi: 10.1186/s12889-017-4835-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Haileselassie M, Redae G, Berhe G, Henry CJ, Nickerson MT, Tyler B, et al. Why are animal source foods rarely consumed by 6–23 months old children in rural communities of Northern Ethiopia? A qualitative study. PloS one. 2020;15(1):e0225707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rodríguez-Ramírez S, Munoz-Espinosa A, Rivera JA, González-Castell D, González de Cosío T. Mexican children under 2 years of age consume food groups high in energy and low in micronutrients. The Journal of nutrition. 2016;146(9):1916S–23S. doi: 10.3945/jn.115.220145 [DOI] [PubMed] [Google Scholar]
- 41.Baek Y, Chitekwe S. Sociodemographic factors associated with inadequate food group consumption and dietary diversity among infants and young children in Nepal. PloS one. 2019;14(3):e0213610. doi: 10.1371/journal.pone.0213610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Na M, Aguayo VM, Arimond M, Dahal P, Lamichhane B, Pokharel R, et al. Trends and predictors of appropriate complementary feeding practices in Nepal: An analysis of national household survey data collected between 2001 and 2014. Maternal & Child Nutrition. 2018;14:e12564. doi: 10.1111/mcn.12564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Locks LM, Pandey PR, Osei AK, Spiro DS, Adhikari DP, Haselow NJ, et al. Using formative research to design a context‐specific behaviour change strategy to improve infant and young child feeding practices and nutrition in N epal. Maternal & Child Nutrition. 2015;11(4):882–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Carvalho AGC, Lira PICd, Barros MdFA, Aléssio MLM, Lima MdC, Carbonneau MA, et al. Diagnosis of iron deficiency anemia in children of Northeast Brazil. Revista de saude publica. 2010;44(3):513–9. doi: 10.1590/s0034-89102010000300015 [DOI] [PubMed] [Google Scholar]
- 45.Mokori A, Schonfeldt H, Hendriks SL. Child factors associated with complementary feeding practices in Uganda. South African Journal of Clinical Nutrition. 2017;30(1):7–14. [Google Scholar]
- 46.Sungkar S, Ridwan AS, Kusumowidagdo G. The effect of deworming using triple-dose albendazole on nutritional status of children in Perobatang village, Southwest Sumba, Indonesia. Journal of parasitology research. 2017;2017. doi: 10.1155/2017/5476739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mamiro PS, Kolsteren P, Roberfroid D, Tatala S, Opsomer AS, Van Camp JH. Feeding practices and factors contributing to wasting, stunting, and iron-deficiency anaemia among 3-23-month old children in Kilosa district, rural Tanzania. Journal of Health, Population and Nutrition. 2005:222–30. [PubMed] [Google Scholar]
- 48.Ickes S, Baguma C, Brahe CA, Myhre JA, Adair L, Bentley M, et al. Maternal participation in a nutrition education program in Uganda is associated with improved infant and young child feeding practices and feeding knowledge: a post-program comparison study. BMC nutrition. 2017;3(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Senarath U, Agho KE, Akram DeS, Godakandage SS, Hazir T, Jayawickrama H, et al. Comparisons of complementary feeding indicators and associated factors in children aged 6–23 months across five South Asian countries. Maternal & child nutrition. 2012;8:89–106. doi: 10.1111/j.1740-8709.2011.00370.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Worwood M. Indicators of the iron status of populations: ferritin. Assessing the iron status of populations: report of a joint World Health Organization/Centers for Disease Control and Prevention technical consultation on the assessment of iron status at the population level. 2007;2:35–74. [Google Scholar]
- 51.Solomon D, Aderaw Z, Tegegne TK. Minimum dietary diversity and associated factors among children aged 6–23 months in Addis Ababa, Ethiopia. International journal for equity in health. 2017;16(1):181. doi: 10.1186/s12939-017-0680-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Mya KS, Kyaw AT, Tun T. Feeding practices and nutritional status of children age 6–23 months in Myanmar: A secondary analysis of the 2015–16 Demographic and Health Survey. PloS one. 2019;14(1):e0209044. doi: 10.1371/journal.pone.0209044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sánchez-Pimienta TG, López-Olmedo N, Rodríguez-Ramírez S, García-Guerra A, Rivera JA, Carriquiry AL, et al. High prevalence of inadequate calcium and iron intakes by Mexican population groups as assessed by 24-hour recalls. The Journal of nutrition. 2016;146(9):1874S–80S. doi: 10.3945/jn.115.227074 [DOI] [PubMed] [Google Scholar]
- 54.Venegas-Aviles Y, Rodríguez-Ramírez S, Monterrubio-Flores E, García-Guerra A. Sociodemographic factors associated with low intake of bioavailable iron in preschoolers: National Health and Nutrition Survey 2012, Mexico. Nutrition journal. 2020;19(1):1–10. doi: 10.1186/s12937-019-0518-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mayen A-L, Marques-Vidal P, Paccaud F, Bovet P, Stringhini S. Socioeconomic determinants of dietary patterns in low-and middle-income countries: a systematic review. The American journal of clinical nutrition. 2014;100(6):1520–31. doi: 10.3945/ajcn.114.089029 [DOI] [PubMed] [Google Scholar]
- 56.Victor R, Baines SK, Agho KE, Dibley MJ. Factors associated with inappropriate complementary feeding practices among children aged 6–23 months in T anzania. Maternal & child nutrition. 2014;10(4):545–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kim SS, Nguyen PH, Tran LM, Alayon S, Menon P, Frongillo EA. Different Combinations of Behavior Change Interventions and Frequencies of Interpersonal Contacts Are Associated with Infant and Young Child Feeding Practices in Bangladesh, Ethiopia, and Vietnam. Current developments in nutrition. 2020;4(2):nzz140. doi: 10.1093/cdn/nzz140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Graziose MM, Downs SM, O’Brien Q, Fanzo J. Systematic review of the design, implementation and effectiveness of mass media and nutrition education interventions for infant and young child feeding. Public health nutrition. 2018;21(2):273–87. doi: 10.1017/S1368980017002786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kim SS, Nguyen PH, Yohannes Y, Abebe Y, Tharaney M, Drummond E, et al. Behavior Change Interventions Delivered through Interpersonal Communication, Agricultural Activities, Community Mobilization, and Mass Media Increase Complementary Feeding Practices and Reduce Child Stunting in Ethiopia. The Journal of nutrition. 2019;149(8):1470–81. doi: 10.1093/jn/nxz087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Mashreky SR, Rahman F, Rahman A, Talab A, Rahman Z. Role of mass media in increasing knowledge and practices of mothers on IYCF: findings from a community trial in rural Bangladesh. South East Asia Journal of Public Health. 2015;5(1):18–24. [Google Scholar]
- 61.Menon P, Nguyen PH, Saha KK, Khaled A, Sanghvi T, Baker J, et al. Combining intensive counseling by frontline workers with a nationwide mass media campaign has large differential impacts on complementary feeding practices but not on child growth: results of a cluster-randomized program evaluation in Bangladesh. The Journal of nutrition. 2016;146(10):2075–84. doi: 10.3945/jn.116.232314 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper.