Abstract
Objective
To outline the development of a software solution to improve medication management after hospital discharge, including its design, data sources, intrinsic features, and to evaluate the usability and the perception of use by end-users.
Materials and Methods
Patients were directly involved in the development using a User Center Design (UCD) approach. We conducted usability interviews prior to hospital discharge, before a user started using the application. A technology acceptance questionnaire was administered to evaluate user self-perception after 2 weeks of use.
Results
The following features were developed; pill identification, patient-friendly drug information leaflet, side effect checker, and interaction checker, adherence monitoring and alerts, weekly medication schedule, daily pill reminders, messaging service, and patient medication reviews. The usability interviews show a 98.3% total success rate for all features, severity (on a scale of 1–4) 1.4 (SD 0.79). Regarding the self-perception of use (1–7 agreement scale) the 3 highest-rated domains were: (1) perceived ease of use 5.65 (SD 2.02), (2) output quality 5.44 (SD 1.65), and (3) perceived usefulness 5.29 (SD 2.11).
Discussion
Many medication management apps solutions have been created and most of them have not been properly evaluated. SAM (Smart About Medications) includes the user perspective, integration between a province drug database and the pharmacist workflow in real time. Its features are not limited to maintaining a medication list through manual entry.
Conclusion
We can conclude after evaluation that the application is usable and has been self-perceived as easy to use by end-users. Future studies are required to assess the health benefits associated with its use.
Keywords: medication therapy management, patient empowerment, mobile applications, usability
Lay Summary
A significant proportion of hospitalized patients and emergency department visits related to drug use occur each year in Canada. Adverse drug events and poor adherence to treatment result from prescription or dispensing errors, overdose, lack of knowledge about medications, or communication problems. To address this, at McGill Clinical & Health Informatics research group, we developed a mobile web application called Smart About Medications (SAM), which aims to improve post-hospital discharge medication management. The app provides patients and their caregivers with the updated drug list, pill images, drug information leaflets, a side effect and interaction checker, a weekly schedule, alerts if they do not follow planned therapy, and the ability to connect with pharmacists. This article describes the application, its usability, and user perception.
INTRODUCTION
Background and significance
Effective management of chronic health problems often require the use of prescribed medications. However, achieving the optimal benefits of medications is often compromised by medication nonadherence and adverse drug events (ADEs). ADEs are understood as an injury related to a drug,1 and account for over 1 million emergency department (ED) visits and an approximate 125 000 hospital admissions per year,2 with an annual cost of over $900 million in the United States3 and $36 million in Canada.4 Approximately 2 million patients require hospitalization due to ADEs each year in the United States. In addition, ADEs occur during 1 in 3 hospital stays.2 Thus, reducing ADEs is expected to result in patient safety and quality of care, reducing health care costs, and improving health outcomes.5
Fortunately, many of the factors leading to the occurrence of ADEs are modifiable and largely preventable through reducing use of inappropriate medications, unintended therapy duplication, and prescribing and dispensing errors.6 Additionally, patient adherence to prescribed medication has also been shown to be associated with hospitalizations, mortality, and costs.7–10 Of particular note is the high rate of primary nonadherence to new prescriptions at discharge, which is estimated to be up to 26%.11,12 In our recent study, we showed that 24% of the medication changes made at hospital discharge were not adhered to in the 30 days post-discharge. Among these, 30% percent of dose modifications were filled at the incorrect dose, 27% of newly prescribed medications were not filled, and 12% of discontinued medications were filled.13 Patients who did not adhere to any of their medication changes had a 35% increased risk of experiencing a hospitalization, ED visit, or death in the 30 days post-discharge compared to those who adhered to all changes.14 Nonadherence has also been previously reported in different hospitalized populations. Among patients hospitalized for myocardial infarction, only 74% of patients filled all their discharge prescriptions by 120 days after discharge.11 In an internal medicine cohort, 28% were not adherent to newly prescribed therapy at 7 days after discharge and 24% at 30 days after discharge.12
One of the problems for medication management is that patients are not provided with supportive tools to facilitate the management of their medications upon discharge. In an era of increasingly shorter hospital stays, opportunities for supportive education and counseling during hospitalization are more limited.15 Moreover, patients often do not remember the details of instructions provided during medical visits, particularly when they have multiple health problems and have been prescribed several medications.16 Better methods are needed to empower patients and their caregivers to better manage their medications, particularly following hospital discharge when many changes may be made to their medication regimen.17,18
Digital technologies, including electronic, mobile, telehealth, and telemedicine modalities, have emerged as increasingly popular and potentially powerful tools in health care to address modifiable health behaviors, empower patients and their caregivers, and enhance patient-centered disease management.19 In addition to providing the opportunity for patients to better communicate with health care providers, these technologies have been shown to improve self-management and adherence to treatment in many conditions, including asthma, chronic obstructive pulmonary disease, hypertension, and diabetes.20–22 In an integrative review conducted in 2017 that examined the types of digital health technologies that targeted medication adherence among patients with chronic conditions, 4 primary strategies were found to have been used to improve adherence: interactive voice recording systems (with or without human interaction), Short Message Service (SMS), telemonitoring and/or tailored care management, and web-based software.19
Patients demand better products to help them satisfy their clinical information needs.23 Many of the issues that prevent adoption and satisfactory use of digital technologies are related to poor design and low usability.24–26 Usable applications must be easy to learn, efficient to use, easy to remember, not prone to errors, and subjectively pleasing to use.27
Objective
In this article, we present a new concept for a web-based solution designed to empower patients and caregivers to better manage their medications in collaboration with their pharmacists. We describe the process of developing the “Smart About Medications” (SAM) platform, its design, data sources, and intrinsic features. We also present results from our assessment of usability and perception of use by end-users.
MATERIALS AND METHODS
Setting
SAM was developed within the McGill Clinical and Health Informatics (MCHI) Research Group, a multidisciplinary team of software developers, researchers, patients, and health professionals, who co-designed and developed the platform consistent with current evidence on optimizing medication self-management and user needs.28 This web-based application was implemented at the McGill University Health Centre (MUHC). The MUHC is a consortium of 5 tertiary hospitals for children and adults, located in Montreal, Quebec, which admits 36 730 patients per year, employs 12 000 nurses and hospital staff, trains over 500 residents, and provides the services of 1587 physicians, pharmacists, and dentists. Patient recruitment was conducted in the internal medicine units of the Montreal General Hospital (MGH) and the Royal Victoria Hospital (RVH) sites of the McGill University Health Centre (MUHC).
Study population
Hospitalized patients were assessed to participate in the study. Patients were eligible if they were over 18 years old, spoke English or French, were covered under the Régie de l’assurance maladie du Québec (RAMQ) prescription drug insurance, planned to be discharged home, had an electronic device (cellphone, tablet, or computer) with internet connection, had an estimated survival prognosis of more than 3 months, and at least one medication prescribed at discharge.
At the hospital, eligible candidates including patients and caregivers were offered to participate in the research project. If accepted, they provided written informed consent before being enrolled in the study, including permission to access patient data from prescription claims (RAMQ). Patients who were cognitively impaired to provide informed consent were enrolled if consent was obtained from a legally authorized representative and if the caregiver administering medications to the patient agreed to use the SAM app on their behalf. Only patients and caregivers who provide written informed consent were given access to the app. Patients cannot designate a new caregiver as a “surrogate” user through the app. The study was granted ethics approval by the MUHC Research Ethics Board.
Data sources
Prescription claims data from the RAMQ, the provincial public health insurer, were used to identify medications dispensed prior to hospital admission and following discharge. These data are available for all Quebec residents who are covered by the public prescription drug insurance plan, which includes those over the age of 65, social assistance recipients, and those whose employers do not provide prescription drug insurance. Medications prescribed to patients at hospital discharge and medication changes made at discharge were identified by reconciling with discharge prescriptions, which were obtained from hospital medical records. Drug-specific information, including patient-friendly monographs, common uses of medications, medication side effects, pill images, and drug-drug interactions were obtained from Vigilance Santé, a drug knowledge database vendor that also develops electronic solutions for community and hospital pharmacies.
Conceptual framework for optimizing medication self-management
The Information-Motivation-Behavioral Skills (IMB) model was used to guide SAM development. IMB is a 3-factor model of behavior change that targets patient adherence,29 and integrates key concepts from classic health behavior models (Theory of Planned Behavior, Self-Determination Theory, and Health Belief Model). In brief, IMB posits that successful behavior change requires individualized interventions to address the informational, motivational, and behavioral skill needs of patients. For medication adherence, this means that individuals must first understand their condition and how prescribed medication(s) help manage symptoms (information), be committed to adhering to recommended therapy (motivation) and have the skills and support that facilitate long-term adherence (behavioral skills).
User-centered design (UCD)
User-centered design was used through an iterative process in the design and development of SAM to enhance adoption and success.30,31 Feedback was collected through usability assessment interviews during which users interacted for the first time with SAM. Usability assessment was conducted using the think-aloud protocol,32 in which users were asked to perform a set of tasks using the system and to verbalize their thoughts as they completed each task. Each task represents a principal functionality of the app (e.g., messaging, drug information leaflet). Patient feedback collected and audio-recorded was used to fix errors and lead the user-friendly development. In a future qualitative analysis, this audio recording data could also be used. User performance was also observed and registered by a trained research assistant to establish if the user was able to complete the task and to determine the ease/difficulty with which the task was completed, rated in 1-to-4 scale as (1) user can do it perfectly, without any help, (2) user can do it with difficulty but without help, (3) user can do it with difficulty and help, and (4) user cannot do it.
User satisfaction
Following 2 weeks of use of the software, a questionnaire that assesses user perception, satisfaction, and collects feedback on the app’s usability was administered. The questionnaire was developed using the extended versions of the technology acceptance model.33 In this way, users’ impressions, experiences, and perspectives were incorporated into the design and development process to enhance the usability of the product. The response options were given based on a Likert scale from 1 to 7, higher in the scale reflecting better agreement (Supplementary Appendix 1).
RESULTS
Technical specifications
The front end of our solution needed to be friendly and responsive to both desktop and mobile screen sizes. This allows the web application to be accessible by anyone with a device that has a web browser and internet connection, regardless of the device used. Angular 2 was chosen as the framework to develop the front end because of its high level of acceptance among the developer community, its up-to-date use of standard software technologies like Typescript, HTML, and multiple libraries that enhance its capability to provide web application solutions. The back end was developed using JAVA EE, a commonly used framework for enterprise software development. It provides a Rest API for communication with the front end. This Rest API is hosted on a secure McGill server. Oracle SQL was used as the database layer, which can be accessed by researchers for analysis.
Description of functionalities
The main user screen page (Figure 1) lists the drugs prescribed at discharge, which are grouped by therapeutic class (Anatomical Therapeutic Chemical classification—ATC), with patient-friendly labels for each class (e.g. “Heart and/or blood pressure treatment”). Medication names and strengths are displayed as initially prescribed along with the dosage and frequency to be taken. Once a medication is dispensed, the brand name appears below the prescribed name. The following features are also available to the user, grouped by the IMB model: (1) Information: pill identification, patient-friendly drug information leaflet, side effect checker, and interaction checker, (2) Motivation: adherence monitoring and alerts, weekly medication schedule, and daily pill reminders, and (3) Behavioral skills and support: messaging service with the hospital pharmacist and patient medication reviews.
Figure 1.
(a) SAM home screen—desktop view, displaying the medication list; (b) mobile view.
Pill identification
This feature displays an image of the pill next to the generic and brand name, as well as the prescribed dosage of each medication in the list (Figure 1). This aims to ensure that patients take the correct medications at the appropriate dosage and right times.
Drug information leaflet
Patient-friendly monographs are provided to help patients and caregivers understand the common uses, benefits, and side-effects of each medication (Figure 2). Improved drug literacy has the potential to increase the appropriate use of medications by patients.17
Figure 2.

Drug information through patient-friendly monographs.
Adherence monitoring and alerts
This feature uniquely integrates pharmacy claims data from the RAMQ with prescribed medications and uses decision algorithms to generate adherence alerts on (1) prescribed medications that are not filled, (2) discontinued medications that are refilled, and (3) medications that are filled at the wrong dose. Once an alert is generated, users may choose to resolve it by selecting an option from the drop-down menu that explains their situation (e.g. “I did not purchase this medication because I am worried about its side effects”) (Figure 3). This selection generates an alert with the hospital pharmacist, who may reach out to patients through the messaging to discuss their responses.
Figure 3.

Patient alert resolution drop-down menu.
Weekly medication schedule and daily pill reminders
The weekly medication schedule aims to help patients and caregivers improve medication-taking behaviors by organizing the patient’s medications by day of the week and time of day (morning, afternoon, evening, and bedtime) that they are supposed to be taken (Figure 4). Users have the option to modify the schedule of each medication but receive a warning pop-up if the times they select are inconsistent with the prescribed dosage (e.g., if they schedule a medication to be taken 3 times a day when it has been prescribed to be taken twice a day). Patients and caregivers can also enable SMS text message reminders as further medication scheduling aids.
Figure 4.
Weekly medication schedule.
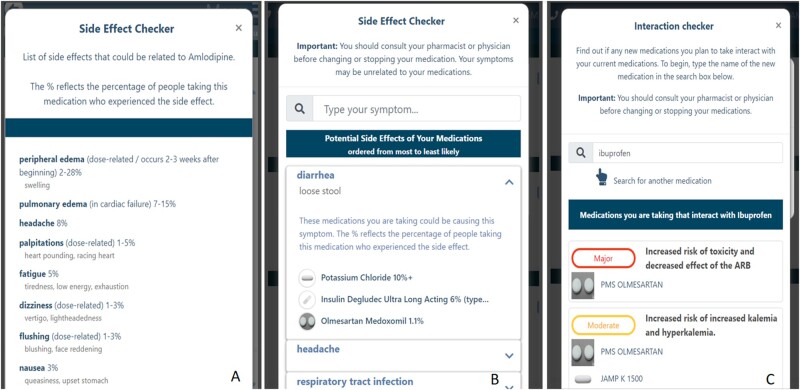
Side effect and drug–drug interaction checker
Two modules of the side effect checker are included in the app. In the first, the side effects associated with a single medication are displayed, along with the frequency of occurrence of each side effect (Figure 5a). In the second, all side effects associated with the patient’s medication profile are listed, along with the medications associated with each side effect (Figure 5b). In this second view, users can also use the search box to determine if a symptom they are experiencing is a possible side effect of one of their medications. Some reading levels across the apps seem complex for the average user, which may significantly reduce the tool’s impact on use and health outcomes. We included under each term a user-friendly synonym if available (eg, “dizziness” = “vertigo”).
Figure 5.
Side effects: (a) of a single drug; (b) of all prescribed and dispensed medications; (c) drug–drug interaction checker.
When several medications are routinely taken, drug–drug interactions become more likely and must be considered whenever the patient adds a new medication to their regimen. For example, over-the-counter medications can interact with other medications the patient is taking and may potentially cause an ADE. This feature allows the user to identify drug-drug interactions between the patient’s current medications and a new medication that the patient intends to start taking (Figure 5c). In this way, the patient can identify possible risks associated with the combination of a new drug with those that are routinely consumed.
Medication reviews by patients
This allows patients to review their medications, describe their experience with a medication (e.g. experienced side effects or benefits), and rank their experience on a scale of 1-to-5 stars. Each patient medication review is anonymized and made visible to other users taking the same drug. Although we must recognize the possibility of introducing a bias to patient behavior based on a review from another user, any patient or caregiver mentioned being concern about reading other users’ comments during usability testing.
Caregiver connect
Because the care and monitoring of medications is a task frequently performed by caregivers, we enabled caregivers to access the system as a user. In the system, the caregiver has a list of patients for whom they provide medication management support. The list of medications and the functionalities are the same as those available to patients. For example, caregivers may send a message to the pharmacist via the messaging system, appropriately identifying the user as the patient’s caregiver.
Communication with pharmacist
This feature allows patients and caregivers to communicate with the hospital pharmacist using a secured messaging service (Figure 6a) to ask any questions they have regarding prescribed medications, therapy changes, and adherence alerts. The pharmacist in turn communicates with the user through the pharmacist dashboard (Figure 6b), a web-based platform which lists all patients under the pharmacist’s care using the app. For each patient, it lists the prescribed and dispensed medications, and displays any nonadherence alerts which have been generated for a patient along with the patient’s resolution of the alert. It also includes a messaging module through which pharmacists can communicate with patients and caregivers. Based on their communication with the patient/caregiver regarding medication concerns, experienced side effects, or nonadherence alerts, hospital pharmacists have the option to (1) recommend a course of action to the patient regarding their medications, (2) consult with the on-duty attending physician regarding a potential change in the patient’s prescription, (3) contact the patient’s community pharmacist to inform them of any dispensing errors or changes made to the patient’s prescription, and (4) contact the patient’s primary care physician, as needed.
Figure 6.
(a) Messaging service; (b) pharmacist dashboard.
User characteristics
All consented patients and caregivers users were invited for a usability assessment while at the hospital prior to using the app, and a user satisfaction questionnaire 2 weeks after discharge. Among the participants, 31 performed the usability test and 12 completed the satisfaction questionnaire. The mean age of patients was 54.4 years old, 56.5% were female and most spoke English as their preferred language. The mean age for caregivers was 55 years old. All baseline characteristics can be found in Table 1.
Table 1.
Baseline user characteristics
| Characteristic | Patients | Caregivers |
|---|---|---|
| Sample (N) | 23 | 8 |
| Age, years (mean) | 54.4 (SD 18.8) | 55 (SD 10.9) |
| Sex | ||
| Female | 13 (56.5%) | 7 (87.5%) |
| Male | 10 (43.5%) | 1 (12.5%) |
| Hospital | ||
| RVH | 15 (65.2%) | 5 (62.5%) |
| MGH | 8 (34.8%) | 3 (37.5%) |
| Language | ||
| English | 18 (78.3%) | 7 (87.5%) |
| French | 5 (21.7%) | 1 (12.5%) |
Usability assessment and user performance
During the assessment, the tasks centered around the patient’s ability and the ease of use of each feature of the app. As the side effect and interaction checkers were developed later in the design and development cycle, there was a smaller number of usability tests completed for these features. Overall, most patients were able to complete each task, most of them without any help. Results can be found in Table 2. The exception was the task of completing a medication review, where only 3 patients (9.7%) did not complete the task. Patients struggled with this task, they are not normally asked to evaluate their experience with a medication, and they were not sure what comments were expected.
Table 2.
Usability and user performance
| Task to perform | Tests (N) | Severity level 1a | Severity level 2a | Severity level 3a | Severity level 4a | Severity scale, mean (SD) | Success-error rate (%) |
|---|---|---|---|---|---|---|---|
| Login | 29 | 27 | 0 | 2 | 0 | 1.14 (SD 0.51) | 100% |
| Search for more information | 31 | 26 | 0 | 5 | 0 | 1.32 (SD 0.74) | 100% |
| Send a message | 31 | 23 | 5 | 3 | 0 | 1.35 (SD 0.65) | 100% |
| Adding a medication review | 31 | 19 | 2 | 7 | 3 | 1.81 (SD 1.09) | 90.3% |
| Side effects information | 23 | 21 | 1 | 1 | 0 | 1.13 (SD 0.45) | 100% |
| Side effects checker | 21 | 12 | 3 | 6 | 0 | 1.71 (SD 0.88) | 100% |
| Interaction checker | 6 | 5 | 1 | 0 | 0 | 1.17 (SD 0.37) | 100% |
| Overall | 172 | 133 | 12 | 24 | 3 | 1.4 (SD 0.79) | 98.3% |
Severity scale rated in 4 levels as (1) the user can do it perfectly, without any help, (2) the user can do it with difficulty but without help, (3) the user can do it with difficulty and help, and (4) the user cannot do it.
User satisfaction by end-users
After 2 weeks of using SAM, a self-assessment web questionnaire was completed by 12 of 31 patients who were discharged home regarding their perceptions and satisfaction on a 1-to-7 agreement scale. On average, patient’s perception on SAM was positive. The highest ratings were for perceived ease of use (mean: 5.65), output quality (mean: 5.44) and usefulness (mean: 5.29), while the lowest ratings were in relevance (mean: 4.86), and subjective norm (mean: 3.81), understood as the belief that their social circle will approve and support a particular behavior, results can be found in Table 3.
Table 3.
Self-perception satisfaction by patient end-users (12 responses)
| Domain | Mean (SD) |
|---|---|
| Behavioral intention | 5.17 (SD 2.12) |
| Perceived usefulness | 5.29 (SD 2.11) |
| Subjective norm | 3.81 (SD 1.74) |
| Relevance | 4.86 (SD 1.78) |
| Output quality | 5.44 (SD 1.65) |
| Result demonstrability | 5.06 (SD 1.82) |
| Perceived ease of use | 5.65 (SD 2.02) |
| Computer self-efficacy | 5.60 (SD 2.00) |
| Perceived enjoyment | 5.24 (SD 1.97) |
DISCUSSION
This article describes the process of developing the SAM platform, its design, data sources, and intrinsic features. Currently, many medication management app solutions have been created. However, the features of most of these applications are limited to maintaining a medication list through manual entry, pill reminders, and refill requests,34,35 and most of them have not been evaluated.35,36 By integrating our system with the provincial health insurance database and allowing patients direct access to their pharmacist, our innovative patient-centered approach aims to help and empower patients and caregivers in the medication management process, highlighting the 3 best self-perceived domains of SAM: perceived ease of use, output quality, and perceived usefulness. Based on the general concept of self-efficacy, defined as one’s confidence about his or her abilities to perform a computer-related task successfully,37 it was not included as an assessment domain of SAM, since this characteristic depends on the user ability more than an intrinsic software attribute.
As a limitation, we must recognize the small number of participants this project had. For user testing is already described in the literature the low number of users needed to have proper feedback and make usability evaluations. Testing the system with at least 5 users is enough to elaborate a usability evaluation.38 Nevertheless, we had a low-rate response of the usability assessment after 2 weeks of use (37.9%). The total number of responses (12 users) may not have sufficient power to make a definitive evaluation of user’s perspective. Further analysis, including more patients could solve this limitation, giving more accurate and generalizable results.
Regardless of the article’s focus on the patient and caregiver perception and experience, we must recognize the potential impact on the pharmacist’s work, including the extra work for the patient follow-up by messages after discharge and alert resolution. However, due to the low number of users, only a few patients have been followed by a pharmacist at the same time. Nevertheless, we must consider this point when escalating the project to a bigger number of users to avoid professional exhaustion and burnout.
The COVID-19 pandemic is a new situation for patients, health professionals, researchers, and policymakers to establish methods of managing care remotely.39 Public measures such as physical distancing and stay-at-home orders have changed patients’ needs, requiring urgent action to transform and adapt health care delivery,40 where the strategic approach using information technology has had a massive acceleration since the pandemic began.41 High-risk populations, such as patients with several chronic conditions and complex drug regimens, will face the difficult choice between iatrogenic exposure to COVID-19 during a clinical visit and postponing health care services.42 This situation is a call for health information technologies to fill the gap and help patients when managing medication at home. Also, we emphasize the importance of new tools, like the one described in this manuscript, to create a link between the pharmacist team and patients, bring a better follow-up of patients regardless the physical distance.
In this project, we faced and successfully integrated SAM with provincial prescription claims insurance data, a major added value of SAM that allowed alerts to be generated for errors in dispensing and unfilled prescriptions. While SAM has only been tested in the post-discharge patient context, in future we will test its value in enhancing medication management in the community by integrating SAM with an integrated drug management system (MOXXI).43 This application, developed previously by our research group, will enable community based primary care physicians and pharmacists to co-manage chronic and episodic drug therapy.
CONCLUSION
We described several features regarding medication management and evaluated the usability and the perception of use. We can conclude that the application is usable. Also, ease of use, output quality, and usefulness were the outstanding qualities in the evaluation by real-life end-users. More studies are needed to assess the health-related benefits associated with its use.
FUNDING
The funding sources for the work is made by the Ministry of Economics, Science, and Innovation (MÉSI) under the funding opportunity of the Health and Social Services Innovation Support Fund (FSISSS).
AUTHOR CONTRIBUTIONS
Each author has participated in the work to take public responsibility for appropriate portions of the content. Authorship credit was based on (1) substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data for the work; (2) drafting the article or revising it critically for important intellectual content; and (3) final approval of the version to be published. All conditions were met.
ETHICS APPROVAL
This study was authorized by the Research Ethics Board (REB) of the McGill University Health Centre (MUHC). Study number 2019-4597.
SUPPLEMENTARY MATERIAL
Supplementary material is available at Journal of the American Medical Informatics Association online.
Supplementary Material
ACKNOWLEDGMENTS
We thank all the teamwork that collaborated on this work, particularly all the pharmacy teams at the MUHC. This study was possible by support provided by the RAMQ and the McGill Clinical Health Informatics Research Group (MCHI).
CONFLICT OF INTEREST STATEMENT
None declared.
DATA AVAILABILITY
Conversation recordings and transcripts cannot be shared publicly for the privacy and confidentiality of study participants.
REFERENCES
- 1. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err is Human: Building a Safer Health System. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 2. U.S. Department of Health and Human Services ooDPaHP. National Action Plan for Adverse Drug Event Prevention. Washington, DC: Author; 2014. [Google Scholar]
- 3. Slight SP, Seger DL, Franz C, et al. The national cost of adverse drug events resulting from inappropriate medication-related alert overrides in the United States. J Am Med Inform Assoc 2018; 25 (9): 1183–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wu C, Bell CM, Wodchis WP.. Incidence and economic burden of adverse drug reactions among elderly patients in Ontario emergency departments: a retrospective study. Drug Saf 2012; 35 (9): 769–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. U.S. Department of Health and Human Services ooDPaHP. Adverse Drug Events Washington, D.C. 2020. https://health.gov/our-work/health-care-quality/adverse-drug-events Accessed November 29, 2020.
- 6. Bartlett G, Blais R, Tamblyn R, et al. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ 2008; 178 (12): 1555–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Modi A, Siris ES, Tang J, et al. Cost and consequences of noncompliance with osteoporosis treatment among women initiating therapy. Curr Med Res Opin 2015; 31 (4): 757–65. [DOI] [PubMed] [Google Scholar]
- 8. Cutler RL, Fernandez-Llimos F, Frommer M, et al. Economic impact of medication non-adherence by disease groups: a systematic review. BMJ Open 2018; 8 (1): e016982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sokol MC, McGuigan KA, Verbrugge RR, et al. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care 2005; 43 (6): 521–30. [DOI] [PubMed] [Google Scholar]
- 10. Simpson SH, Eurich DT, Majumdar SR, et al. A meta-analysis of the association between adherence to drug therapy and mortality. BMJ 2006; 333 (7557): 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jackevicius CA, Li P, Tu JV.. Prevalence, predictors, and outcomes of primary nonadherence after acute myocardial infarction. Circulation 2008; 117 (8): 1028–36. [DOI] [PubMed] [Google Scholar]
- 12. Fallis BA, Dhalla IA, Klemensberg J, et al. Primary medication non-adherence after discharge from a general internal medicine service. PLos One 2013; 8: e61735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Weir DL, Motulsky A, Abrahamowicz M, et al. Challenges at care transitions: failure to follow medication changes made at hospital discharge. Am J Med 2019; 132 (10): 1216–24.e5. [DOI] [PubMed] [Google Scholar]
- 14. Weir DL, Motulsky A, Abrahamowicz M, et al. Failure to follow medication changes made at hospital discharge is associated with adverse events in 30 days. Health Serv Res 2020; 55 (4): 512–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sawan MJ, Wennekers D, Sakiris M, et al. Interventions at hospital discharge to guide caregivers in medication management for people living with dementia: a systematic review. J Gen Intern Med 2021; 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Duerden M, Avery T, Payne R.. Polypharmacy and Medicines Optimisation. Making it Safe and Sound. London: The King’s Fund; 2013. [Google Scholar]
- 17. Dayer L, Heldenbrand S, Anderson P, et al. Smartphone medication adherence apps: potential benefits to patients and providers. J Am Pharm Assoc 2013; 53 (2): 172–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Heldenbrand S, Martin BC, Gubbins PO, et al. Assessment of medication adherence app features, functionality, and health literacy level and the creation of a searchable Web-based adherence app resource for health care professionals and patients. J Am Pharm Assoc (2003) 2016; 56 (3): 293–302. [DOI] [PubMed] [Google Scholar]
- 19. Conway CM, Kelechi TJ.. Digital health for medication adherence in adult diabetes or hypertension: an integrative review. JMIR Diabetes 2017; 2 (2): e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Patel N, Jones P, Adamson V, et al. Chronic obstructive pulmonary disease patients' experiences of an enhanced self-management model of care. Qual Health Res 2016; 26 (4): 568–77. [DOI] [PubMed] [Google Scholar]
- 21. Morrison D, Mair FS, Chaudhuri R, et al. Details of development of the resource for adults with asthma in the RAISIN (randomized trial of an asthma internet self-management intervention) study. BMC Med Inform Decis Mak 2015; 15: 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wakefield BJ, Holman JE, Ray A, et al. Effectiveness of home telehealth in comorbid diabetes and hypertension: a randomized, controlled trial. Telemed J E Health 2011; 17 (4): 254–61. [DOI] [PubMed] [Google Scholar]
- 23. Friedberg MW, Chen MW, Van Busum KR, et al. Factors Affecting Physician Professional Satisfaction and Their Implications for Patient Care, Health Systems, and Health Policy. RAND Health, AMA; 2013; pp. 33–46. [PMC free article] [PubMed] [Google Scholar]
- 24. Zahabi M, Kaber D, Swangnetr M.. Usability and safety in electronic medical records interface design: a review of recent literature and guideline formulation. Hum Factors 2015; 57 (5): 805–34. [DOI] [PubMed] [Google Scholar]
- 25. LeRouge C, Wickramasinghe N.. A review of usercentered design for diabetes-related consumer health informatics technologies. J Diabetes Sci Technol 2013; 77 (44): 1039–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hermawati S, Lawson G.. Managing obesity through mobile phone applications: a state of the art review rom a user-centred design perspective. Pers Ubiquit Comput 2014; 18 (8): 2003–23. [Google Scholar]
- 27. Nielsen J. Usability Engineering. Boston: Academic; 1993. [Google Scholar]
- 28. Habib B, Márquez FS, Buckeridge DL, et al. Evaluation of a mobile application to enhance medication management following hospital discharge: study protocol for a pilot randomized controlled trial. Stud Health Technol Inform 2019;264:1929–30. [DOI] [PubMed] [Google Scholar]
- 29. DiMatteo MR, Haskard-Zolnierek KB, Martin LR.. Improving patient adherence: a three-factor model to guide practice. Health Psychol Rev 2012; 6 (1): 74–91. [Google Scholar]
- 30. Norman DA, Draper SW, eds. User Centered System Design. Hillsdale, NJ: Erlbaum; 1986. [Google Scholar]
- 31. Schleyer TK, Thyvalikakath TP, Hong J. What is user-centered design? J Am Dent Assoc. 2007; 138 (8): 1081–2. [DOI] [PubMed] [Google Scholar]
- 32. Charters E. The use of think-aloud methods in qualitative research: an introduction to think-aloud methods. Brock Educ J 2003; 12 (2): 68–82. [Google Scholar]
- 33. Venkatesh V, Bala H.. Technology acceptance model 3 and a research agenda on interventions. Decision Sci 2008; 39 (2): 273–315. [Google Scholar]
- 34. Santo K, Richtering SS, Chalmers J, et al. Mobile phone apps to improve medication adherence: a systematic stepwise process to identify high-quality apps. JMIR mHealth uHealth 2016; 4 (4): e132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Ahmed I, Ahmad NS, Ali S, et al. Medication adherence apps: review and content analysis. JMIR Mhealth Uhealth 2018; 6 (3): e62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Lancaster K, Abuzour A, Khaira M, et al. The use and effects of electronic health tools for patient self-monitoring and reporting of outcomes following medication use: systematic review. J Med Internet Res 2018; 20 (12): e294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Compeau DR, Higgins CA.. Computer self-efficacy: development of a measure and initial test. MIS Q 1995a; 19 (2): 189–211. [Google Scholar]
- 38. Nielsen J, Landauer TK.. A mathematical model of the finding of usability problems. In: Proceedings of the INTERACT'93 and CHI'93 conference on Human factors in computing systems. 1993.
- 39. Adalja AA, Toner E, Inglesby TV.. Priorities for the US health community responding to COVID-19. JAMA 2020; 323 (14): 1343–4. [DOI] [PubMed] [Google Scholar]
- 40. Ronquillo JG, Lester WT, Zuckerman DM.. Using informatics to guide public health policy during the COVID-19 pandemic in the USA. Journal of Public Health 2020; 42 (4): 660–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Boulos MN, Geraghty EM.. Geographical tracking and mapping of coronavirus disease COVID-19/severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) epidemic and associated events around the world: how 21st century GIS technologies are supporting the global fight against outbreaks and epidemics. Int J Health Geogr 2020; 19 (1): 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Keesara S, Jonas A, Schulman K.. Covid-19 and health care’s digital revolution. N Engl J Med 2020; 4382 (23): e82. [DOI] [PubMed] [Google Scholar]
- 43. Tamblyn R, et al. Using novel Canadian resources to improve medication reconciliation at discharge: study protocol for a randomized controlled trial. Trials 2012; 13 (1): 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Conversation recordings and transcripts cannot be shared publicly for the privacy and confidentiality of study participants.