Abstract
Objective
The COVID‐19 pandemic has had considerable economic repercussions for young workers. The current study was undertaken to examine the impact of the pandemic on the employment of young adults with rheumatic disease and on perceptions of work and health.
Methods
Surveys were administered to young adults with rheumatic disease prior to and following the onset of the COVID‐19 pandemic. Surveys asked about employment status and collected information on sociodemographic, disease/health, and work‐context factors. Items also asked about the perceived impact of the COVID‐19 pandemic on work and health. A generalized estimating equation model was fitted to examine the effect of the pandemic on employment.
Results
In total, 133 young adults completed the pre–COVID‐19 pandemic survey (mean age 28.9 years, 82% women). When compared to the pre–COVID‐19 pandemic period, employment decreased from 86% to 71% following the pandemic, but no other changes were identified in sociodemographic, disease/health, or work‐context factors. The time period following the COVID‐19 pandemic was associated with a 72% lower odds of employment compared to the pre‐pandemic period (odds ratio 0.28 [95% confidence interval 0.11–0.71]). Those with a postsecondary education or who reported more mental job demands were more likely to be employed following the onset of the pandemic. Also, a majority of participants reported that the pandemic affected health care (83%), treatment access (54%), working conditions (92%), and occupational health and safety (74%).
Conclusion
The onset of the COVID‐19 pandemic had socioeconomic implications for young people with rheumatic disease. To support economic recovery for individuals with rheumatic disease, strategies to promote employment should be designed that account for the young adult life phase and occupational characteristics.
INTRODUCTION
The COVID‐19 pandemic has had significant economic and health consequences for the working population. In the early spring of 2020, policies and programs were implemented in Canadian provinces that aimed to address the rising community and occupational spread of SARS–CoV‐2 and to minimize cases of COVID‐19, including but not exclusive to the closure of nonessential business, social distancing measures, and changes to health care delivery. Canadian labor force data from the general working population showed a sharp drop in the employment rate (–15.4%) following the start of the pandemic (1). Data also show that youth and young adults were 2 times more likely to report job loss than older age groups (1). While the reopening of the economy was accompanied by an economic rebound, paid work remains lower than pre‐pandemic levels and is susceptible to disruption from additional waves of disease transmission. Of concern, COVID‐19–related employment interruptions have implications for the mental health of young adults (2).
Significance & Innovations.
Using a longitudinal data set, we show a significant reduction in the frequency of young adults with rheumatic disease who were employed after the onset of the COVID‐19 pandemic.
Highlighting occupational inequities in the impact of COVID‐19, participants with a higher education or working in jobs with greater mental demands were less likely to report employment loss.
A majority of participants indicated that the COVID‐19 pandemic affected their health care and medical treatment as well as their working conditions and occupational health and safety.
Preliminary studies show that individuals with autoimmune rheumatic diseases could be at an elevated risk of infection from COVID‐19 when compared to those not living with a rheumatic disease (3). Also, studies of individuals with rheumatic disease reported gaps in the delivery of rheumatology care and treatment and worsening health when compared to pre‐pandemic levels (e.g., greater fatigue, worsening musculoskeletal and cognitive function, and psychological stress) (3, 4). For workers with rheumatic disease, COVID‐19 could pose a specific risk of infection for those in occupational settings that require client‐facing job tasks or where social distancing measures are more challenging (e.g., nursing, teaching, factory work) (5). Workers with rheumatic disease may have experienced changes to their employment attributed to policies aimed at addressing COVID‐19 spread or may have adapted their working situation to address the perceived risk of disease transmission or to cope with psychosocial stressors attributed to the pandemic (4).
Our study focused on young adults with rheumatic disease (ages 18–35 years) who were in the early stages of their working lives. Research conducted prior to the COVID‐19 pandemic indicated that young adults with rheumatic disease face challenges finding and sustaining paid work and are more likely to report barriers to accessing modifications to the work environment to support work and health needs (6, 7). These employment challenges have the potential of being more pronounced during a period of economic disruption and, for young adults, have the potential to impact work experiences across the life course and affect pathways to health (2, 8).
Using longitudinal survey data, we sought to determine changes to employment in a sample of young adults with rheumatic disease in the period following the implementation of policies and programs to address COVID‐19 spread (i.e., post COVID‐19 pandemic onset) when compared to the period prior to the COVID‐19 pandemic. Secondly, we examined the sociodemographic, disease/health, and work‐context factors related to employment following the onset of the COVID‐19 pandemic. Cross‐sectional data collected after the onset of the pandemic examined a third objective: to describe the impact of COVID‐19 on perceptions of work and health.
MATERIALS AND METHODS
In a cohort of Canadian young adults with rheumatic disease, a survey was administered at 2 time points separated by 9 months: prior to policies and programs being widely applied to address the spread of COVID‐19 (December 1, 2019 to March 31, 2020); and after restrictions related to the COVID‐19 pandemic being widely applied (last survey completed December 12, 2020). The study included individuals between the ages of 18–35 years with a self‐reported diagnosis of rheumatic disease from a doctor (e.g., juvenile arthritis, systemic lupus erythematosus, rheumatoid arthritis) and having held paid employment (in the past year) or looking for work. Past studies note challenges of recruiting young adults with rheumatic disease to participate in surveys (9). Accordingly, we used 3 purposive recruitment approaches to maximize engagement. First, participants were recruited from specialty clinics in 3 Canadian provinces (British Columbia, Ontario, and Quebec). Eligible participants recruited through clinics were provided with a study invitation that included a link to the survey. Second, eligible participants were identified and recruited through an existing panel of Canadians maintained by a research firm that is nationally representative according to region and income (9). Third, community‐based recruitment was conducted through 3 patient‐led organizations of individuals with rheumatic disease that shared study advertisements through their listservs or social media accounts. All interested eligible potential participants were provided with detailed study information; informed consent was obtained, and eligibility was confirmed. A 30‐minute online English‐ or French‐language survey was administered to participants at each time point. University of Toronto’s Research Ethics Board approved study procedures (REB number 36588).
Survey
The survey was informed by previous qualitative research (7). Items and measures were selected according to past studies of people with rheumatic disease in which validity, reliability, and associations with employment were established (6, 10).
Employment status as outcome
At each time point, respondents were asked about their current employment status. Respondents were classified as employed or not employed (i.e., student, short‐term leave, furloughed or temporarily laid off, on long‐term leave, unemployed but looking for work, unemployed, and not looking for work).
Covariates
Participant details were collected at each time point, including age (years), sex/gender, educational attainment, and marital status. Information on diagnosis of rheumatic disease, age at disease onset, and self‐rated health (1 = poor, 5 = excellent) was obtained. Self‐reported pain, fatigue, and disease activity were measured using 11‐point scales (0 = no pain/fatigue/disease activity, 10 = worst possible pain/fatigue/disease activity) (11). The 10‐item Center for Epidemiological Studies Depression Scale (CESD‐10) was used to measure frequency of current depressive symptoms (e.g., depressed mood and feelings of guilt) using a 5‐point ordinal scale (0 = rarely/none of them time, 4 = all of the time) (12). A CESD‐10 score ≥10 indicated depression. Participants completed the 12‐item Workplace Activity Limitation Scale (WALS) to measure difficulties with workplace acts and tasks (i.e., problems with lower mobility, upper mobility, and concentration) (0 = no difficulty/not applicable to job, 3 = unable to do). Items were summed to produce a score ranging from 0 to 36 (10).
Participants were asked about whether they held part‐time (<30 hours/week) or full‐time employment (≥30 hours/week) or held a permanent or temporary contract, their job tenure (years), and the job sector worked (trades/transportation, sales/services, professional services, health care/social services, technology). Participants were asked about the physical activity requirements of their workplace and mental job demands (1 = not at all, 5 = a great deal). Additionally, participants were asked about their perceptions of job control, job stress, and organizational support (1 = not at all, 5 = a great deal).
Perceptions of COVID‐19 impact
Descriptive items were developed that asked about the perceived impact of the COVID‐19 pandemic on work and health and were measured after the onset of the pandemic. Two questions asked about the extent to which the COVID‐10 pandemic interrupted access to health care providers and medical treatment (1 = not at all, 5 = a great deal). Also, 2 questions asked about the extent to which the COVID‐19 pandemic affected workplace health and safety and working conditions (1 = not at all, 5 = a great deal).
Statistical analysis
Descriptive statistics (i.e., percentages, means) were used to examine variable distributions. Chi‐square tests and t‐tests were conducted to compare employment status and sociodemographic, health/disease, and work‐context factors using observations collected for each participant prior to the COVID‐19 pandemic and after the onset of the pandemic. Univariable logistic regression models were conducted to examine the individual relationship between each study variable collected prior to the COVID‐19 pandemic and the odds of employment following the onset of the pandemic. We fitted a multivariable generalized estimating equation (GEE) model to examine change in employment status in the time period after the onset of the COVID‐19 pandemic when compared to the period prior to the pandemic. Our model also enabled the examination of relationships between study variables and employment after the onset of the COVID‐19 pandemic. The GEE model was fitted with a logit link and exchangeable correlation structure to account for the relationship between observations within participants over time. Analyses were conducted using SAS, version 9.30 (13).
RESULTS
Overall, 133 young adults with rheumatic disease completed the survey prior to the COVID‐19 pandemic. Of those, 83% completed the survey after the onset of the COVID‐19 pandemic. No significant difference was identified between participants who completed both surveys and those lost to follow‐up. A majority of participants were women (82%) and had a postsecondary education (87%). Less than one‐half of participants indicated being married/living as if married (43%), and 15% reported having primary childcare responsibilities. Approximately 28% reported having juvenile arthritis, and 36% reported having rheumatoid arthritis; 70% indicated a diagnosis of a pediatric disease. Prior to the COVID‐19 pandemic, participants indicated moderate‐to‐low mean pain (mean ± SD 4.3 ± 2.4), fatigue (mean ± SD 5.8 ± 2.6), and disease activity scores (mean ± SD 3.8 ± 2.5). Also, prior to the COVID‐19 pandemic, approximately two‐thirds of participants reported good, very good, or excellent health (62%); 63% indicated depressive symptoms. Participants indicated moderate limitations to workplace activity prior to the pandemic (mean ± SD 9.9 ± 5.9) (Table 1).
Table 1.
Sociodemographic, disease/health, and work‐context factors reported by young adults with rheumatic disease prior to and after the onset of the COVID‐19 pandemic*
| Characteristic |
Prior to COVID‐19 pandemic (n = 133) |
After onset of COVID‐19 pandemic (n = 110) |
P |
|---|---|---|---|
| Employment status | |||
| Employed | 114 (85.7) | 78 (70.9) | 0.01 |
| Not employed | 19 (14.3) | 32 (29.1) | |
| Sociodemographic factors | |||
| Age, mean ± SD years | 28.7 ± 4.9 | 29.6 ± 4.8 | 0.17 |
| Sex/gender | 0.97 | ||
| Women | 109 (82.0) | 91 (82.7) | |
| Men | 23 (17.3) | 18 (16.4) | |
| Non‐binary | 1 (0.75) | 1 (0.91) | |
| Educational attainment | |||
| Less than postsecondary education | 17 (12.8) | 14 (12.7) | |
| Postsecondary education or more | 116 (87.2) | 96 (87.3) | |
| Married/living as if married | 57 (42.9) | 50 (45.5) | 0.68 |
| Primary childcare responsibilities | 19 (14.9) | 17 (15.5) | 0.92 |
| Disease/health factors | |||
| Rheumatic disease diagnosis | 0.61 | ||
| Juvenile arthritis | 37 (27.8) | 33 (30.0) | |
| Lupus | 16 (12.0) | 16 (16.4) | |
| Rheumatoid arthritis | 48 (36.1) | 32 (29.1) | |
| Other rheumatic disease diagnosis | 32 (24.1) | 27 (24.6) | |
| Pediatric disease onset, age <18 years | 90 (69.0) | 76 (69.7) | 0.86 |
| Pain score, mean ± SD (range 0–10) | 4.3 ± 2.4 | 4.30 ± 2.6 | 0.96 |
| Fatigue score, mean ± SD (range 0–10) | 5.8 ± 2.6 | 5.31 ± 2.6 | 0.14 |
| Disease activity score, mean ± SD (range 0–10) | 3.8 ± 2.5 | 3.6 ± 2.5 | 0.53 |
| Flare severity | 0.29 | ||
| No flares | 28 (21.1) | 31 (28.2) | |
| 1–2 flares | 66 (49.6) | 51 (46.4) | |
| ≥3 flares | 36 (27.1) | 27 (24.5) | |
| Do not know | 3 (2.3) | 1 (0.9) | |
| Self‐rated health | 0.86 | ||
| Poor | 14 (10.5) | 6 (5.5) | |
| Fair | 37 (27.8) | 35 (31.8) | |
| Good | 48 (36.1) | 45 (40.9) | |
| Very good | 30 (22.6) | 18 (16.4) | |
| Excellent | 4 (3.0) | 6 (5.45) | |
| Depression | |||
| Depressed, CESD‐10 score ≥10 | 84 (63.2) | 67 (60.9) | 0.72 |
| Not depressed, CESD‐10 score <10 | 49 (37.8) | 43 (39.1) | |
| Workplace activity limitations mean ± SD (WALS score range 0–36) | 9.9 ± 5.9 | 9.5 ± 6.3 | 0.57 |
| Work‐context factors† | |||
| Employment type | 0.24 | ||
| Full‐time work hours, ≥30 hours/week | 87 (76.3) | 65 (83.3) | |
| Part‐time work hours, <30 hours/week | 27 (23.7) | 13 (16.7) | |
| Employment contract | 0.92 | ||
| Permanent contract | 84 (73.7) | 58 (74.4) | |
| Temporary contract | 30 (26.3) | 52 (25.6) | |
| Job tenure, mean ± SD years | 3.4 ± 3.4 | 3.9 ± 3.8 | 0.29 |
| Job control, mean ± SD (range 1–5) | 2.9 ± 1.2 | 2.9 ± 1.2 | 0.74 |
| Workplace physical activity requirement, mean ± SD (range 1–5) | 3.0 ± 1.4 | 2.7 ± 1.5 | 0.13 |
| Perceived mental job demands, mean ± SD (range 1–5) | 3.8 ± 1.1 | 3.7 ± 1.2 | 0.58 |
| Perceived job stress, mean ± SD (range 1–5) | 3.1 ± 0.9 | 3.1 ± 1.1 | 0.72 |
| Perceived organizational support, mean ± SD (range 1–5) | 3.2 ± 1.3 | 3.3 ± 1.3 | 0.31 |
| Job sector | 0.48 | ||
| Trades/transportation | 29 (21.8) | 20 (25.6) | |
| Sales/services | 12 (9.02) | 3 (3.9) | |
| Professional services/technology | 15 (11.3) | 14 (17.9) | |
| Health care/social services | 57 (42.9) | 41 (52.6) |
Values are the number (%) unless indicated otherwise. CESD‐10 = 10‐item Center for Epidemiological Studies Depression Scale; WALS = Workplace Activity Limitations Scale.
Percentage calculated for those reporting paid employment.
Of note, 86% of participants held paid employment prior to the COVID‐19 pandemic. An examination of information on work‐context factors collected prior to the COVID‐19 pandemic showed that 76% of participants worked full‐time hours, 74% held a permanent job, and just under one‐half worked in the health care/social services job sector (43%). Participants reported moderate mean job control (mean ± SD 2.9 ± 1.2), mental job demands (mean ± SD 3.8 ± 1.1), job stress (mean ± SD 3.1 ± 0.9), organizational support (mean ± SD 3.2 ± 1.3), and requirements of workplace physical activity (mean ± SD 3.0 ± 1.4).
Significantly fewer participants were employed after the onset of the COVID‐19 pandemic (71%) (P < 0.01). Additionally, after the onset of the pandemic, participants did not report significant differences to sociodemographic, disease/health, or work‐context factors (Table 1).
When adjusting for study covariates, the time period after the onset of the COVID‐19 pandemic was associated with a 72% lower odds of employment when compared to the time period prior to the pandemic (odds ratio [OR] 0.28 [95% confidence interval (95% CI) 0.11–0.71]) (Table 2). Having a postsecondary education prior to the COVID‐19 pandemic was associated with a greater odds of employment following the onset of the pandemic when compared to those not holding a postsecondary education (OR 7.2 [95% CI 1.76–26.62]). Those reporting that their job required greater mental demands prior to the COVID‐19 pandemic were more likely to report employment after the onset of the COVID‐19 pandemic (OR 1.56 [95% CI 1.08–2.25]). Also, the multivariable model indicated an association between being a woman and a lower likelihood of employment when compared to men (OR 0.26 [95% CI 0.11–0.71]). Pediatric onset of rheumatic disease was associated with a greater likelihood of being employed when compared to those with adult‐onset rheumatic disease (OR 2.68 [95% CI 1.12–6.43]).
Table 2.
Univariable model and multivariable generalized estimating equation (GEE) model examining the effect of the COVID‐19 pandemic on the employment of young adults with rheumatic disease*
|
Univariable OR (95% CI)† |
Multivariable OR (95% CI)‡ |
|
|---|---|---|
| Time period | ||
| Prior to COVID‐19 pandemic | – | |
| Following onset COVID‐19 pandemic | 0.28 (0.11–0.71)§ | |
| Sociodemographic¶ | ||
| Age, years | 1.11 (1.01–1.21)§ | 1.08 (0.99–1.17) |
| Sex/gender | ||
| Women | 0.91 (0.30–2.81) | 0.26 (0.11–0.71)§ |
| Men | – | – |
| Education | ||
| Less than postsecondary education | – | – |
| Postsecondary education or more | 3.94 (1.24–12.52)§ | 7.2 (1.93–26.62)§ |
| Marital status | ||
| Married/living as if married | 1.83 (0.77–4.40) | 2.5 (0.99–6.42) |
| Not married or living as if married | – | – |
| Childcare responsibilities | ||
| Primary childcare responsibilities | 0.29 (0.06–1.47) | 0.35 (0.07–1.82) |
| No childcare responsibilities/not primary caregiver | – | – |
| Disease/health factors¶ | ||
| Disease onset | ||
| Pediatric disease onset, age <18 years | 1.3 (0.53–3.11) | 2.68 (1.12–6.43)§ |
| Adult onset, age >18 years | – | – |
| Self‐rated health | ||
| Poor/fair | – | – |
| Good/very good/excellent | 2.67 (1.13–6.27)§ | 1.79 (0.60–5.38) |
| Pain score (range 0–10) | 0.75 (0.62–0.91) | 1.08 (0.80–1.46) |
| Fatigue score (range 0–10) | 0.84 (0.70–0.99) | 0.93 (0.67–1.28) |
| Disease activity score (range 0–10) | 0.78 (0.65–0.94)§ | 0.96 (0.68–1.37) |
| Depression | ||
| Depressed, CESD‐10 score ≥10 | 0.93 (0.87–0.99)§ | 0.46 (0.15–1.37) |
| Not depressed, CESD‐10 score <10 | – | – |
| Workplace activity limitations (WALS score range 0–36) | 0.91 (0.85–0.98)§ | 1.01 (0.92–1.11) |
| Work‐context factors¶ | ||
| Job control (range 1–5) | 1.11 (0.77–1.61) | 1.38 (0.95–2.00) |
| Organizational support (range 1–5) | 1.37 (0.95–1.98) | 0.91 (0.61–1.35) |
| Physical activity (range 1–5) | 0.62 (0.45–0.87)§ | 1.19 (0.82–1.73) |
| Mentally demanding job (range 1–5) | 1.41 (0.94–2.12)§ | 1.56 (1.08–2.25)§ |
95% CI = 95% confidence interval; CESD‐10 = 10‐item Center for Epidemiological Studies Depression Scale; OR = odds ratio; WALS = Workplace Activity Limitations Scale.
Univariable logistic regression model examining the relationship between study variables and employment after the onset of the COVID‐19 pandemic. Due to limitations of sample size, the participant who was non‐binary was not included in the model and should be examined in further analyses.
GEE model examined the relationship between study variables and employment following the application of policies and programs to address the spread of COVID‐19. Due to limitations of sample size, the participant who was non‐binary was not included in the model and should be examined in further analyses.
Significant.
Measured prior to the onset of policies and programs to address the spread of COVID‐19.
More than 80% of participants indicated that the COVID‐19 pandemic affected access to health care, of which just under one‐half reported quite a bit/a great deal of impact. Also, 44% of participants reported that the COVID‐19 pandemic affected access to medical treatment. More than 90% of participants indicated that the COVID‐19 pandemic affected working conditions, of which one‐half indicated quite a bit/a great deal of impact. Close to three‐fourths of participants indicated that the COVID‐19 pandemic affected their perceptions of occupational health and safety (74%) (Figure 1).
Figure 1.
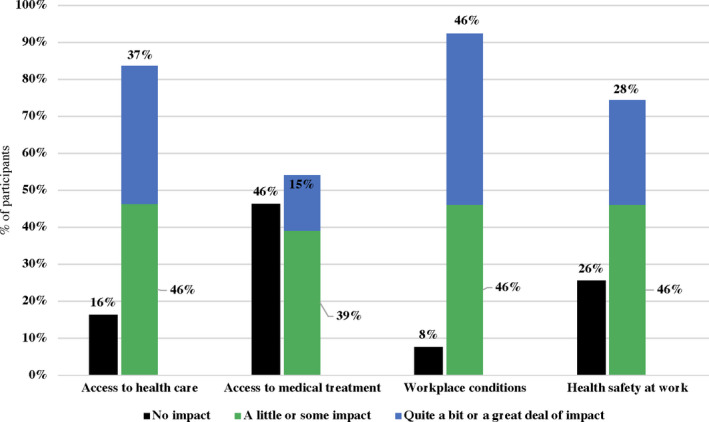
Perceived impact of the COVID‐19 pandemic on work and health as indicated in data from young people with rheumatic disease collected after the onset of the pandemic.
DISCUSSION
Young adults with rheumatic disease are a labor market group with vulnerability to the economic impact of the COVID‐19 pandemic. Utilizing a longitudinal survey of a purposively recruited sample of Canadian young adults with rheumatic disease, we showed a significant decline in employment following the onset of the COVID‐19 pandemic when compared to pre‐pandemic levels. For the young adults in our study, having a less established employment history, a more recently diagnosed condition, or working in entry‐level positions could mean that they were particularly susceptible to labor market shocks (7). Scholarship on the social determinants of health indicate that paid work provides pathways to promoting long‐term health and quality of life (8). Disruption to employment because of COVID‐19 at the early career phase could have significant implications for employment and health outcomes (2). Supporting employment engagement represents a strategy to assist young people with rheumatic disease in recovering from the effects of the COVID‐19 pandemic and to promote health.
Descriptive findings highlighted the work and health implications of the COVID‐19 pandemic. Participants reported that the pandemic affected health care access and medical treatment as well as working conditions and occupational health and safety. This was not, however, reflected by self‐reported disease severity or other health factors that did not differ between pre‐ and post–COVID‐19 periods. The loss of employment identified in our sample could be attributed to labor market policies that addressed occupational spread of COVID‐19, which may have affected participants who were at an early career stage, rather than being related to changes to health. Additional research is required to elaborate on the ways in which the COVID‐19 pandemic affected employment of young adults with rheumatic disease, as well as short‐ and longer term labor market outcomes.
Study findings could reflect occupational inequities in the impact of COVID‐19. Participants reporting greater educational attainment or those working in jobs with greater mental demands were more likely to be employed following the onset of the COVID‐19 pandemic. It may be that educational attainment and mental demands are proxies for those employed in higher skilled jobs that may be performed from home or where there is opportunity to modify work (14). Aligning with labor force data, our study of young adults with rheumatic disease found an association between being a women and not working after the onset of the COVID‐19 pandemic (1, 15). These preliminary findings may be explained by differences in workplace experiences (e.g., occupation) and roles outside of work (e.g., childcare responsibilities) for female participants that could have contributed to a greater socioeconomic burden of the pandemic (16). Research in a larger sample is required to further examine differences in sex and gender in the impact on employment among young adults with rheumatic disease. Findings pointing to the importance of contextual and personal factors should be considered in the design of policies and programs that support participation in paid work during the COVID‐19 pandemic and during periods of economic recovery.
We determined changes in employment resulting from the COVID‐19 pandemic that were attributed to the longitudinal design of the study. Our study timeframe was, however, limited, and we were not able to ascertain whether the removal or reapplication of policies addressing additional waves of COVID‐19 resulted in employment fluctuations or if other forces may be driving change in paid work. Also, we focused mainly on employment status but did not examine changes in work hours or productivity that could also have been affected by the COVID‐19 pandemic. Sample characteristics mirror past studies of young adults with rheumatic disease (17). Participants were purposively recruited, and there may be limitations related to the small sample size and generalizability of findings. Nonetheless, these data provide important preliminary insight into the work and health implications of the COVID‐19 pandemic for a vulnerable subgroup of workers.
In conclusion, the COVID‐19 pandemic contributed to a significant decrease in the employment of young adults with rheumatic disease. Of concern, for those at the early career phase, the effect of the pandemic on employment could extend across the course of life and have significant implications for work and health. Employment interventions should be considered for young adults with rheumatic disease to support recovery from the COVID‐19 pandemic.
AUTHOR CONTRIBUTIONS
All authors were involved in drafting the article or revising it critically for important intellectual content, and all authors approved the final version to be submitted for publication. Dr. Jetha had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Study conception and design
Jetha, Tucker, Gignac.
Acquisition of data
Jetha, Tucker, Gignac.
Analysis and interpretation of data
Jetha, Chen.
ACKNOWLEDGMENTS
The authors thank Ms Julie Bowring for her assistance with data collection and manuscript preparation, and Drs. Louise Perlin and Elizabeth M. Hazel for their recruitment support.
Supported by Arthritis Society, Canada (Young Investigator Operating grant 17‐0095 to Dr. Jetha).
No potential conflicts of interest relevant to this article were reported.
References
- 1. Statistics Canada . Labour force survey. August 2020. URL: https://www150.statcan.gc.ca/n1/daily‐quotidien/200904/dq200904a‐eng.htm.
- 2. Ganson KT, Tsai AC, Weiser SD, Benabou SE, Nagata JM. Job insecurity and symptoms of anxiety and depression among US young adults during COVID‐19. J Adolesc Health 2021;68:53–6. [DOI] [PubMed] [Google Scholar]
- 3. Zhong J, Shen G, Yang H, Huang A, Chen X, Dong L, et al. COVID‐19 in patients with rheumatic disease in Hubei province, China: a multicentre retrospective observational study. Lancet 2020;2:e557–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Mancuso CA, Duculan R, Jannat‐Khah D, Barbhaiya M, Bass AR, Mehta B. Rheumatic disease‐related symptoms during the height of the COVID‐19 pandemic. HSS J 2020:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lan FY, Wei CF, Hsu YT, Christiani DC, Kales SN. Work‐related COVID‐19 transmission in six Asian countries/areas: a follow‐up study. PloS One 2020;15:e0233588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Jetha A, Badley E, Beaton D, Fortin PR, Shiff NJ, Rosenberg AM, et al. Transitioning to employment with a rheumatic disease: the role of independence, overprotection, and social support. J Rheumatol 2014;41:2386–94. [DOI] [PubMed] [Google Scholar]
- 7. Jetha A, Bowring J, Tucker S, Connelly CE, Martin Ginis KA, Proulx L, et al. Transitions that matter: life course differences in the employment of adults with arthritis. Disabil Rehabil 2018;40:3127–35. [DOI] [PubMed] [Google Scholar]
- 8. Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, et al. Adolescence and the social determinants of health. Lancet 2012;379:1641–52. [DOI] [PubMed] [Google Scholar]
- 9. Jetha A, Tucker L, Bowring J, Backman CL, Proulx L, Kristman V, et al. Casting a wide net: comparing strategies for recruiting 18–35‐year‐olds with rheumatic disease as study participants. Arthritis Rheumatol 2019;71 Suppl 10. URL: https://acrabstracts.org/abstract/casting‐a‐wide‐net‐comparing‐strategies‐for‐recruiting‐18‐35‐year‐olds‐with‐rheumatic‐disease‐as‐study‐participants/. [Google Scholar]
- 10. Gignac MA, Cao X, Tang K, Beaton DE. Examination of arthritis‐related work place activity limitations and intermittent disability over four‐and‐a‐half years and its relationship to job modifications and outcomes. Arthritis Care Res (Hoboken) 2011;63:953–62. [DOI] [PubMed] [Google Scholar]
- 11. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS pain), Numeric Rating Scale for Pain (NRS pain), McGill Pain Questionnaire (MPQ), Short‐Form McGill Pain Questionnaire (SF‐MPQ), Chronic Pain Grade Scale (CPGS), Short Form‐36 Bodily Pain Scale (SF‐36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken) 2011;63 Suppl 11:S240–52. [DOI] [PubMed] [Google Scholar]
- 12. Bradley KL, Bagnell AL, Brannen CL. Factorial validity of the Center for Epidemiological Studies Depression 10 in adolescents. Issues Ment Health Nurs 2010;31:408–12. [DOI] [PubMed] [Google Scholar]
- 13. SAS software: release 9.3. Cary (NC): SAS Institute; 2015. [Google Scholar]
- 14. Cazes S, Hijzen A, Saint‐Martin A. Measuring and assessing job quality: the OECD Job Quality Framework. OECD Social, Employment and Migration Working Papers, No. 174. OECD Publishing, Paris. 2015. URL: https://www.oecd‐ilibrary.org/social‐issues‐migration‐health/measuring‐and‐assessing‐job‐quality_5jrp02kjw1mr‐en. [Google Scholar]
- 15. Madgavkar A, White O, Krishnan M, Mahajan D, Azcue X. COVID‐19 and gender equality: countering the regressive effects. McKinsey Global Institute. 2020. URL: com/featured-insights/future‐of‐work/covid‐19‐and‐gender‐equalitycountering‐the‐regressive‐effects. [Google Scholar]
- 16. Quinn MM, Smith PM. Gender, work, and health. Oxford: Oxford University Press; 2018. [Google Scholar]
- 17. Jetha A, Badley E, Beaton D, Fortin PR, Shiff NJ, Gignac MA. Unpacking early work experiences of young adults with rheumatic disease: an examination of absenteeism, job disruptions, and productivity loss. Arthritis Care Res (Hoboken) 2015;67:1246–54. [DOI] [PubMed] [Google Scholar]


