Abstract
Background
There are significant concerns that the COVID‐19 pandemic may have negative effects on substance use and mental health, but most studies to date are cross‐sectional. In a sample of emerging adults, over a two‐week period during the pandemic, the current study examined: (1) changes in drinking‐related outcomes, depression, anxiety, and posttraumatic stress disorder and (2) differences in changes by sex and income loss. The intra‐pandemic measures were compared to pre‐pandemic measures.
Methods
Participants were 473 emerging adults (M age = 23.84; 41.7% male) in an existing longitudinal study on alcohol misuse who were assessed from June 17 to July 1, 2020, during acute public health restrictions in Ontario, Canada. These intra‐pandemic data were matched to participant pre‐pandemic reports, collected an average of 5 months earlier. Assessments included validated measures of drinking, alcohol‐related consequences, and mental health indicators.
Results
Longitudinal analyses revealed significant decreases in heavy drinking and adverse alcohol consequences, with no moderation by sex or income loss, but with substantial heterogeneity in changes. Significant increases in continuous measures of depression and anxiety were present, both of which were moderated by sex. Females reported significantly larger increases in depression and anxiety. Income loss >50% was significantly associated with increases in depression.
Conclusions
During the initial phase of the pandemic, reductions in heavy drinking and alcohol consequences were present in this sample of emerging adults, perhaps due to restrictions on socializing. In contrast, there was an increase in internalizing symptoms , especially in females, highlighting disparities in the mental health impacts of the pandemic.
Keywords: alcohol, anxiety, COVID‐19, depression, emerging adults, sex differences
A longitudinal analysis on the impact of the COVID‐19 pandemic revealed decreases in heavy drinking and adverse alcohol consequences, however there was substantial heterogeneity in changes. Furthermore, the COVID‐19 pandemic had a selective negative effect on depression and anxiety in females and those with major income loss (>50%).

INTRODUCTION
The outbreak of coronavirus disease 2019 (COVID‐19) caused by severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) has posed a major public health concern across the world. In response to the rising number of cases and deaths from COVID‐19, global efforts to mitigate the physical health effects have led to public health interventions such as physical distancing and self‐isolation. Although these measures were important in controlling the spread of the virus, they have led to various negative downstream effects. These include but are not limited to job loss, financial strain, interpersonal strain, food insecurity, and social isolation (Larson et al., 2020; Statistics Canada, 2020e; World Health Organization, 2020). Stressful events are well‐established risk factors for mental health problems and substance abuse (Clay & Parker, 2020; Frasquilho et al., 2016). Early reports suggest that pandemic‐related stress may have further exacerbated mental health and substance use issues (Kujawa et al., 2020). Additionally, the effects of social support and interaction, which often act as buffers against the effects of stress, have also been diminished due to the pandemic (Burke & Weir, 1978; Nabi et al., 2013).
One group that may be particularly sensitive to the effects of the pandemic are emerging adults. Emerging adulthood (aged 18 to 25) is a developmental period characterized by not only positive role transitions into full autonomy (e.g., independent living, workforce entry, marriage), but also high rates of risky behavior, such as heavy episodic drinking (HED; White & Hingson, 2013). Disruptions during emerging adulthood may be particularly challenging, and pandemic‐related stress has cross‐sectionally been associated with the exacerbation of depression, anxiety, and substance use in emerging adults (Czeisler et al., 2020; Hawke et al., 2020; Kujawa et al., 2020; Liu et al., 2020, 2020).
There are also critical sex/gender differences in the impact of the COVID‐19 pandemic. Younger women report greater pandemic‐related distress and anxiety (Brooks et al., 2020; Kujawa et al., 2020; McGinty et al., 2020; Pierce et al., 2020; Statistics Canada, 2020c; Wang et al., 2020). Recent studies among women also found increased reporting of mental health symptoms and alcohol consumption (Rahman et al., 2020; Rodriguez et al., 2020). Because women have been disproportionately affected by both job loss and an uptake in caregiving duties as a result of the pandemic (Adams‐Prassl et al., 2020), they may be more vulnerable to stress. Of note, Kuntsche et al. found that females were more likely to use drinking as a coping mechanism (Kuntsche et al., 2015). In combination, these factors make it important to examine gender differences in alcohol use and mental health outcomes during the pandemic.
Another major impact of COVID‐19 was the loss of income due to pay cuts and layoffs. This has led to significant financial strain and increased levels of depression, especially in women (Jacques‐Avinõ et al., 2020). However, the effect of unemployment (prepandemic) on substance use has been mixed. Some studies show robust associations between unemployment and increased substance use (Lee et al., 2015) and mental health problems (i.e., depression, anxiety; Axelsson & Ejlertsson, 2002; McGee & Thompson, 2015). On the other hand, unemployment has also been shown to decrease the consumption of substances (e.g., alcohol; Ettner, 1997). This may be explained by the decrease in available income to purchase alcohol or other substances. It is also possible that unemployment would lead to decreased work‐related stress, which may lead to decreased substance use as a coping mechanism (Wang et al., 2020). The pandemic adds an additional layer of complexity to the impacts of income loss due to reductions in all social interactions (within and outside of work) and major external stressors, such as fear of infection and uncertainty of the future. Thus, the examination of income loss, mental health, and substance use during the pandemic becomes even more important. Unfortunately, most studies on COVID‐19 impacts have been cross‐sectional, reporting self‐attributions about increases or decreases in behavior. This limits the conclusions that can be drawn, both in terms of accuracy and as far as quantitatively measuring the changes over time.
In contrast, the goal of the current study was to examine changes in drinking and common mental health symptoms longitudinally. Participants in an existing observational longitudinal cohort study of heavy drinking in emerging adulthood received a COVID‐19–specific supplemental assessment during the second phase of the pandemic public health restrictions in Ontario, Canada. Those data were then contrasted with participants’ prepandemic data in terms of drinking, depression, life disruption, anxiety, and posttraumatic stress disorder (PTSD) symptoms. Because pandemic impacts do not fall equally across the population, the study examined two high‐priority moderators, acute economic disruption and biological sex.
METHODS
Study design
A supplementary assessment measuring the impact of COVID‐19 was administered to participants from an ongoing longitudinal study on alcohol misuse in emerging adults. The initial cohort of individuals (N = 730) was recruited in 2017 in Hamilton, Ontario, and these individuals were assessed every 8 months. A supplementary COVID‐19 assessment was administered from June 17 to July 1, 2020, during COVID‐19 lockdown. These intra‐COVID assessments were compared to the most recent pre‐COVID assessment, prior to the declaration of the pandemic status of COVID‐19 by the World Health Organization and subsequent declaration of a state of an emergency in Ontario in March 17, 2020. Specifically, participants were required to have a pre‐COVID assessment date ≤243 days from their intra‐COVID assessment completion date (maximum of 8 months pre‐COVID to intra‐COVID). This time frame was to capture participant information that was prior to COVID but relatively proximal, and, although participants had varying durations, this time frame avoided a very wide distribution of pre‐COVID time points. The duration between assessments was, on average, 5 months (IQR: 63 days; see STROBE diagram in Supplemental Material). The current analysis focuses on changes between these two periods of time—prior to the onset of the pandemic and during an acute phase of public health restrictions—to characterize the impact of COVID‐19 on mental health and alcohol use.
Participants
Participants were a voluntary community sample of emerging adults recruited from Hamilton, Ontario. Participants in both studies were recruited using flyers and newspaper, online, and bus ads. Eligibility criteria for participation in the cohort study included HED (≥4/3 standard drinks for males/females; Butt et al., 2011) on at least 2 days in the past month or at least one HED episode and one cannabis use episode per month (i.e., high‐risk substance use; 8% of the sample); aged 19.5 to 23 years; fluency in written English; and no current or past psychosis (i.e., schizophrenia, schizoaffective disorder, or similar conditions). Of the original 730, those still enrolled in the study (N = 708, 52.4% female) were invited to complete an optional supplemental assessment on the impact of the COVID‐19 pandemic. Of these participants, 518 individuals (73% response rate; 58.4% female) completed the COVID‐19 supplemental analysis. A STROBE diagram is provided in Supplemental Material. Those who completed the intra‐COVID survey did not differ from individuals that did not complete the survey on ethnicity and age; a significant difference between biological sex was found (χ2 = 8.94, p < 0.001), with fewer females completing the COVID‐19 survey. Finally, of the 518 intra‐COVID respondents, n = 486 had a pre‐COVID assessment that fell within the window, constituting the final study sample. Participants’ average age was 23.4 at the prepandemic assessment and 23.8 at the intrapandemic assessment. Sample characteristics are reported in Table 1. Contrasts between those who completed the assessment versus those who did not are shown in Supplemental Material; rates of drinking days/week were similar but slightly lower among those who opted out (p = 0.04), but no differences were present for heavy drinking days (HDD)/week (p = 0.94).
TABLE 1.
Descriptive statistics and frequencies of participants (n = 473)
| Characteristic | Mean (SD) or % or median |
|---|---|
| Sex (% female, as assigned at birth) | 58.4% |
| Gender a | |
| cis‐Male | 41.4% |
| cis‐Female | 56.9% |
| Other | 1.69% |
| % White | 70.4% |
| Student status a | 49.05% |
| Age | |
| Pre | 23.42 (±1.22) |
| Intra | 23.84 (±1.29) |
| Median education a | Associates/bachelor's degree |
| Median income | |
| Pre | $45,000 to <$60,000 |
| Intra b | $45,000 to <$60,000 |
| Current living arrangements | |
| Living with family | |
| Pre | 37.0% |
| Intra | 49.0% |
| Living alone | |
| Pre | 9.9% |
| Intra | 10.4% |
| Living with partner (romantic partner) | |
| Pre | 18.6% |
| Intra | 22.7% |
| Living with roommate(s)/group living | |
| Pre | 33.6% |
| Intra | 17.0% |
| Other | |
| Pre | 0.9% |
| Intra | 0.9% |
As per the pre‐COVID assessment.
n = 471.
At each assessment, participants received a gift card ($30 CAD). All assessments were conducted using Research Electronic Data Capture (REDCap) software (Harris et al., 2019), and all aspects of study procedures were reviewed and approved by the Hamilton Research Ethics Board (Protocol #2193). Participants provided electronic informed consent, followed by the assessments.
Assessments
Pandemic impacts
The impact of the pandemic was evaluated through purpose‐built assessments asking participants to report self‐perceived impacts through the following questions: (i) What percentage of your monthly household income (approximately) has been lost as a result of the pandemic? (0% to 100% slider response given); and (ii) visual analogue scales assessing how stressful, sad, irritable, and how much disruption the pandemic induced (from 0 [a scale of little or none] to [100]). To distinguish between none, some, and a large amount of income loss, individuals were categorized into 1 of 3 groups: (1) no monthly income loss, (2) greater than 0%, but less than 50% monthly income loss, and (3) greater than or equal to 50% monthly income loss.
Alcohol and mental health measures
Daily Drinking Questionnaire was used to assess an individual's weekly alcohol consumption (Collins et al., 1985). Participants were asked to estimate the typical number of standard drinks consumed on every day of the week (Monday–Sunday) within the last month. This was then used to calculate average number of drinking days (DD) per week and average number of HDD per week. HDD were defined as days in which more than three drinks for females and more than four drinks for men were consumed (Centre on Substance Use, 2019; NIAA, 2017). Lastly, the Brief Young Adult Alcohol Consequences Questionnaire (B‐YAACQ; Kahler et al., 2008) was used to assess alcohol severity.
Additionally, mental health instruments were administered to evaluate self‐reported clinical symptoms of depression using the Patient Health Questionnaire‐9 (PHQ‐9; Kroenke et al., 2010), anxiety using the Generalized Anxiety Disorder‐7 (GAD‐7; Spitzer et al., 2006), and PTSD using the PTSD Checklist‐5 (PCL‐5; Blevins et al., 2015). The mental health instruments offer two scoring options: a continuous measure and a dichotomous version reflecting a positive or negative screen. Both were used in the analyses. For the dichotomous version, scores of ≥10 on the PHQ‐9, ≥10 on the GAD‐7, and ≥33 on the PCL‐5 were used to indicate clinically significant levels of depression, anxiety, and PTSD, respectively. Extended descriptions of the mental health instruments can be found in the Supplemental Material.
Descriptive measures
Participants completed a comprehensive self‐reported demographic assessment including biological sex, gender, ethnicity, education, income, living arrangements, and other descriptive characteristics.
Quality control
Adequate attention/effort was assessed with five quality control items, which had definitively correct responses (e.g., “For this item, choose response ‘B’.”) and were scattered throughout. For participants to be deemed as having adequate attention/effort, four or more of the five quality control questions were required to be answered correctly.
Data analyses
For descriptive results of data collected during the pandemic, significant differences in proportions of responses across biological sex were tested using the chi‐square test of independence. To test differences in mean responses between males and females, independent t‐tests were conducted. The core analysis comprised an examination of within‐subjects changes over time (pre‐COVID to intra‐COVID) and interactions between time with two candidate moderators, loss of income (i.e., trichotomized as 0, <50, and 50+% income loss; “Lost Income”), and biological sex (as assigned at birth). Specifically, to analyze changes in alcohol consumption behavior and mental health outcomes from the pre‐COVID to intra‐COVID time period, linear mixed‐effects models (LMMs) and generalized linear mixed‐effects models (GLMMs) were fit by REML using the “lme4” package (Bates et al., 2015). Mixed effects were used to allow for the intraindividual variation to be accounted for as random effects. In addition to fitting basic models to predict the change in outcomes across time, subsequent models were fitted with a trichotomized lost income variable and biological sex separately as fixed effects. Lastly, if significant changes in mental health outcomes were observed, follow‐up analyses examined their relationship with alcohol‐related behaviors. More specifically, these analyses examined interactions between temporal changes (pre‐COVID to intra‐COVID) in alcohol‐related consequences with clinically relevant changes in mental health symptomology (clinically relevant increase or no clinically relevant increase; Kroenke, 2012; Toussaint et al., 2020). LMMs were conducted to analyze changes in continuous outcomes, while GLMMs were used to analyze the changes in dichotomous outcomes. Significance of the fixed effects in both the LMMs and GLMMs was determined by conducting Wald test with Kenward–Roger degrees of freedom using the “car” package, to produce type II analysis‐of‐variance tables for each fitted model, which is appropriate for factorial independent variables. Relevant post hoc tests on the fitted models were carried out using the “emmeans” package to obtain the calculated mean response for each group and to determine whether the change in mean response from pre‐COVID to intra‐COVID time point was significantly different. In the case of significant interactions for both biological sex and lost income with time, models were first estimated including the 3‐way fixed interaction effect, and then, the estimated marginal means at each time point for every level of lost income were contrasted for males and females. All analyses were conducted using R version 4.0.3 (R Core Team, 2020). Significance level was set at α ≤ 0.01 to adjust for multiple comparisons.
RESULTS
Quality control and participants’ characteristics
Of the 486 participants, seven participants had inadequate attention/effort and a further five had completed only a partial survey resulting in no quality control questions being answered. One additional participant was removed for having only partial data in the COVID‐19 assessment. This left a total of n = 473 participants for the pre‐COVID and intra‐COVID analysis (91.3% of participants who were administered the COVID assessment). Out of the 473 participants, 58.4% were female, and the majority identified as White (70.3%). See Table 1 for sample descriptive statistics.
Cross‐sectional impacts of COVID‐19 on life disruption
Figure 1 displays pandemic‐induced disruption to daily life and emotional impact, in general and based on biological sex. Participants reported high disruption and moderate negative affect. There were no significant differences between biological sexes on disruption to daily life (t = −1.38, p = 0.17), but females reported significantly greater feelings of irritability (t = −3.84, p = 1.44E−04), sadness (t = −5.86, p = 1.02E−08), and stress (t = −6.34, p = 6.28E−10) due to the pandemic.
FIGURE 1.
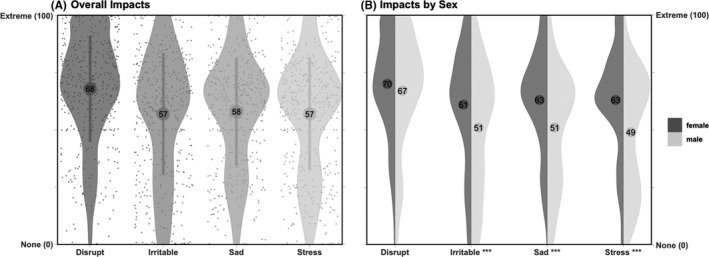
Violin plots of ratings of the psychosocial impact of COVID‐19 with respect to disruption, irritability, sadness, and stress. Mean (±1 SD) ratings are provided in circles for the overall sample (Panel A) and for males and females (Panel B). Visual analogue scales range from 0 (“None or little”) to 100 (“Extreme”). ***p < 0.001
Approximately, 60% of participants reported monthly income loss due to the pandemic. More specifically, 37.6% of individuals reported greater than 0% but less than 50% monthly income loss and 22.4% reported greater than 50% loss in monthly income. Differences in lost income by biological sex were not statistically significant (χ2 = 1.47, p = 0.48). Furthermore, prepandemic, there were no significant differences in employment status (full‐time, part‐time, and unemployed) by biological sex, but the reported household income of males was significantly higher than females (t = −2.72, p = 6.88E−03). Using medians to clarify categories, median male household income was “At least $60,000 but less than $75,000,” while females median household income was “At least $45,000 but less than $60,000.”
COVID‐19 impacts on drinking
Linear mixed effects assessed changes in alcohol consumption and alcohol‐related problems (pre‐COVID to intra‐COVID) in general and based on biological sex and income loss (Table 2; Figure 2). LMMs revealed no significant main effects or interactions for DD, but there was a significant decrease in HDD and in the odds of endorsing ≥1 HDD per week from pre‐COVID to intra‐COVID (OR: 0.32, p < 0.001). With regard to alcohol‐related consequences, LMMs revealed a significant main effect of Time, which suggested a significant decrease in alcohol‐related problems pre‐COVID to intra‐COVID. Interactions between changes in drinking and either income loss or sex were not significant. Individual changes in drinking are shown in the plots in Figure 3.
TABLE 2.
Changes in alcohol consumption and alcohol problems from prepandemic to intrapandemic with interactions with loss of income and sex
| Time | Time × lost income | Time × sex | ||||
|---|---|---|---|---|---|---|
| F/(χ2) | p | F/(χ2) | p | F/(χ2) | p | |
| Drinking days/week | 0.63 | 0.43 | 1.48 | 0.23 | 0.39 | 0.53 |
| HDD/week | 6.48 | 0.01 | 1.79 | 0.17 | 0.08 | 0.78 |
| HDD+ a | 25.36 | 4.76E−07 | 1.56 | 0.46 | 0.01 | 0.92 |
| B‐YAACQ | 67.81 | 1.79E−15 | 0.38 | 0.69 | 5.32 | 0.02 |
Significant effects are in boldface.
Abbreviations: B‐YAACQ, Brief Young Adult Alcohol Consequences Questionnaire; HDD+, any heavy drinking days.
Denotes dichotomous outcome (any HDDs).
FIGURE 2.
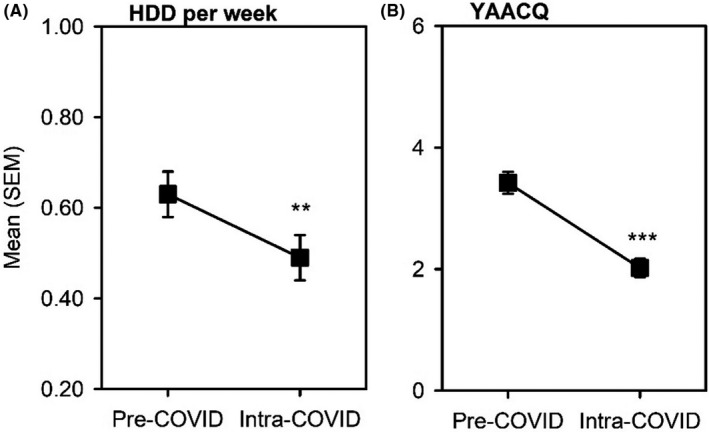
Changes in heavy drinking days (Panel A) and Brief Young Adult Alcohol Consequences Questionnaire (Panel B) from pre‐COVID to intra‐COVID, **p ≤ 0.01, ***p ≤ 0.001
FIGURE 3.
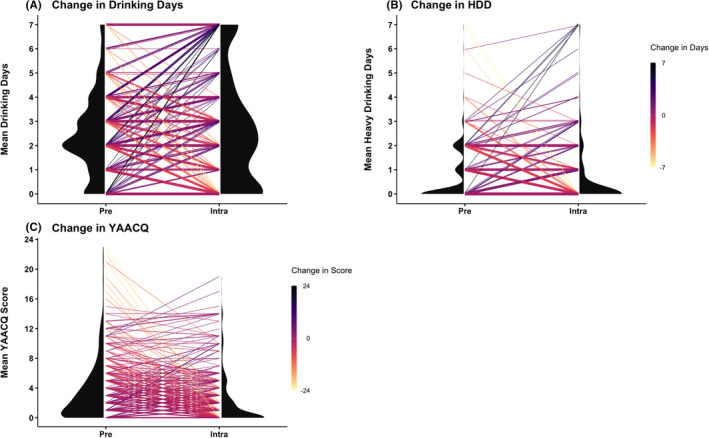
Corset plots of individual drinking changes in drinking days (Panel A), heavy drinking days (Panel B), and Brief Young Adult Alcohol Consequences Questionnaire (Panel C)
COVID‐19 impacts on mental health symptoms
Changes in mental health outcomes (pre‐COVID to intra‐COVID) and interactions with biological sex and income loss are shown in Table 3 and Figure 4. There were significant increases in depression and anxiety symptoms over time; however, PTSD symptoms remained unchanged. With regard to depression, LMMs revealed a significant main effect of Time and significant Time × Lost Income and Time × Sex interactions, but not a 3‐way interaction of Lost Income ×Sex × Time. Post hoc tests examining Sex × Time interaction revealed that females reported a significant increase in depression scores during the lockdown. There were no significant changes in depression scores for males. Post hoc tests examining Lost Income × Time interaction revealed that those reporting ≥50% income loss showed a significant increase in depression scores during the COVID‐19 lockdown. With respect to exceeding the clinical screening cutoff on the PHQ‐9, GLMMs revealed a significant Time × Sex interaction. Post hoc tests revealed a significant increase (188%) in the odds of meeting or exceeding the screening threshold for depression (OR: 2.88, p = 3.00E−04; pre‐COVID: 25.7%; intra‐COVID: 36.9%) in females pre‐COVID to intra‐COVID. No significant changes in odds of meeting a clinical threshold were found for males (OR = 0.55, p = 0.08; pre‐COVID: 23.4%, intra‐COVID: 19.8%). Overall, the threshold for individuals meeting a clinical cutoff for PHQ‐9 changed from 25.6% pre‐COVID to 29.6% intra‐COVID.
TABLE 3.
Changes in mental health from prepandemic to intrapandemic with interactions with loss of income and sex
| Time | Time × lost income | Time × sex | ||||
|---|---|---|---|---|---|---|
| F/(χ2) | p | F/(χ2) | p | F/(χ2) | p | |
| PHQ‐9 score | 12.78 | 3.87E−04 | 5.24 | 5.61E−03 | 11.69 | 6.84E−04 |
| PHQ‐9 threshold a | 3.50 | .06 | 4.30 | 0.12 | 13.05 | 3.03E−04 |
| GAD‐7 score | 10.29 | 1.43 E−03 | 1.37 | 0.25 | 6.71 | 9.88E−03 |
| GAD‐7 threshold a | 3.36 | .07 | 1.84 | 0.40 | 1.78 | 0.18 |
| PCL‐5 score | 0.20 | .66 | 1.24 | 0.29 | 0.43 | 0.51 |
| PCL‐5 threshold a | 0.60 | .44 | 6.32 | 0.04 | 0.12 | 0.74 |
Significant effects are in boldface.
Abbreviations: PHQ‐9, Patient Health Questionnaire‐9; GAD‐7, Generalized Anxiety Disorder Questionnaire‐7; PCL‐5, Posttraumatic Stress Disorder Checklist‐5.
Denotes dichotomous outcome (screens positive or negative).
FIGURE 4.
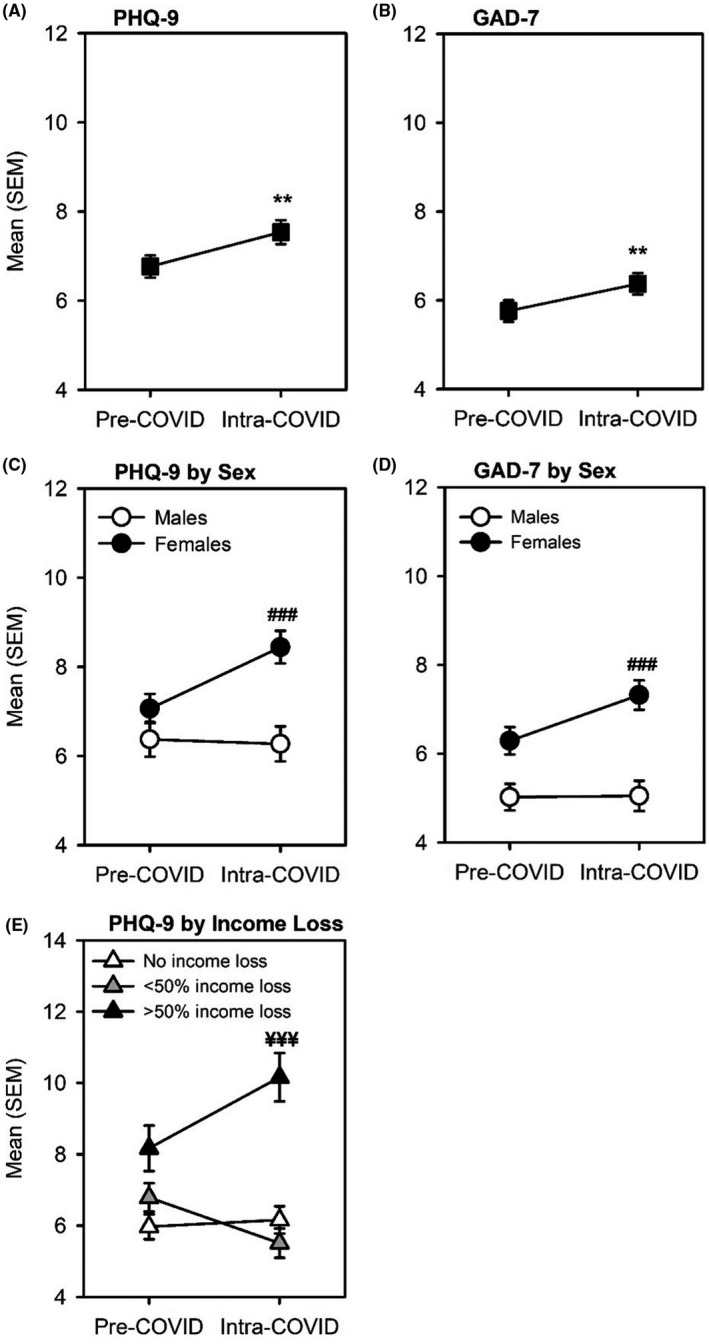
Changes in overall mental health outcomes (Panels A–B), interaction with sex (Panels C–D), and interactions with income (Panel E). **p < 0.01 and represents significant changes from pre‐COVID; ### p < 0.001 and represents significant changes in females from pre‐COVID to intra‐COVID; ¥¥¥ p < 0.001 and represents significant change in individuals reporting >50% income loss from pre‐COVID to intra‐COVID
For anxiety, LMMs revealed a significant main effect of Time and a significant interaction of Time × Sex. Overall, there was a significant increase in anxiety scores from pre‐COVID to intra‐COVID. Post hoc tests examining Time × Sex interaction revealed that females reported significant increases in anxiety pre‐COVID to intra‐COVID. There were no significant changes in anxiety scores for males. With respect to clinical diagnosis of anxiety, GLMMs revealed no significant main effect or interactions, suggesting the increases were within the subclinical range.
To explore whether increases in depression and anxiety were associated with changes in drinking, GLMMs assessed changes in alcohol‐related behaviors based on whether individuals exhibited a clinically significant change over time. Overall, the results suggested that changes in depression and anxiety were independent from drinking. The one exception was with respect to depression, where GLMMs revealed a significant Time × Clinically Significant Change interaction for B‐YAACQ. Post hoc tests revealed larger decreases in alcohol‐related problems in those individuals that did not report a clinically significant change in depression scores. No interactions were observed for depression for HDD or DD, and no interactions were observed for anxiety in relation to B‐YAACQ, HDD, or DD. These results are reported in the Supplemental Material.
DISCUSSION
The current study longitudinally examined the impacts of the COVID‐19 pandemic on heavy drinking in emerging adults. The primary aim was to extend cross‐sectional studies by longitudinally examining the impact of the COVID‐19 pandemic on drinking and other aspects of mental health, in general and whether this differed by sex and income loss, and second the effect of the pandemic on various psychosocial and experiential variables. As context, in terms of general self‐reported impacts of the pandemic, participants reported a robust negative impact across various experiential domains. More specifically, greater perceived life disruption, stress, sadness, and irritability were reported as consequences of the pandemic. This effect was exacerbated in females, who reported greater feelings of irritability, sadness, and stress than their male counterparts. Consistently, the Canadian government reported that women were among the harder hit groups during the pandemic with respect to mental health (Statistics Canada, 2020a). In terms of income loss, a large proportion (60%) of individuals reported some loss of income due to the COVID‐19 pandemic, including approximately one in five reporting a loss of ≥50% of their income. These effects in income loss were not sex‐specific, but females reported a lower median household income than males. Therefore, despite comparable proportion of income loss, females may have had less discretionary income.
In longitudinal analyses, there was a general decrease in heavy drinking, a 68% decrease in odds of endorsing any weekly heavy drinking episodes, and a decrease in alcohol‐related problems in emerging adults. No changes in the number of DD per week were observed. These effects were not moderated by biological sex or income loss. On its face, this is surprising given widespread anecdotal reports of increases in drinking and, for example, increases in household expenditures on alcohol from prepandemic to intrapandemic (Statistics Canada, 2021). However, among young people, studies have also reported decreases in alcohol consumption (Glowacz & Schmits, 2020; White et al., 2020). There are several explanations for this general decrease in younger individuals (Pollard et al., 2020). First, risky alcohol consumption and related harms often occur in bars and nightclubs (Hughes et al., 2010) and subsequently their closure during the pandemic decreases the opportunity to engage in risky alcohol‐associated behavior. Furthermore, peer influences can be strong predictors of alcohol misuse (Beck et al., 2013; Dumas et al., 2020; Read et al., 2005; Washburn et al., 2014). And so, the decrease in the proportion of individuals living with roommates or in group living arrangements during the pandemic (see Table 1) in combination with mandated physical distancing measures may lead to reductions in problem drinking as a result of decreased in‐person social interactions. From a public health standpoint, this would not be considered an adverse impact of the pandemic and illustrates its multifarious effects. Of note, a closer examination of HDD and adverse drinking‐related consequences (Figure 3) revealed considerable heterogeneity in the direction of actual self‐reported changes in HDD and alcohol‐related consequences. The heterogeneity may also explain why some researchers report decreases in alcohol consumption (White et al., 2020), while others report increases in emerging adults (Lechner et al., 2020; Rodriguez et al., 2020). Nonetheless, the results suggest complex effects of the pandemic on drinking‐related outcomes in emerging adults.
With respect to other mental health outcomes, there was evidence of modest increases in depression (+0.8) and anxiety (+0.6) symptoms during the COVID‐19 pandemic. These effects were moderated by sex and income loss. Specifically, females reported significant increases in depression and anxiety, an effect not observed in males. Furthermore, considering the clinical significance (i.e., positive screening of depression), females showed a 188% increase in odds of meeting the clinical depression threshold pre‐COVID to intra‐COVID. Again, similar effects were not observed in males. Overall, results are consistent with studies reporting higher levels of emotional distress in young adults stemming from the pandemic (Bäuerle et al., 2020; Dawel et al., 2020; Huang & Zhao, 2020; Lechner et al., 2020; Pierce et al., 2020). It is possible that females experienced worsened mental health symptoms due to both increased predisposition and higher exposure to psychosocial stressors (e.g., increased loneliness, decreases in perceived social support, and higher intolerance to uncertainty; Cao et al., 2020; Lee et al., 2020; Li & Wang, 2020; Seco Ferreira et al., 2020). However, sex effects have been mixed. While some studies show higher pandemic‐induced anxiety and depression in females (Dawel et al., 2020; Solomou & Constantinidou, 2020), others report no sex differences (Huang & Zhao, 2020). The current study also revealed an effect of income loss on depression scores. Those reporting ≥50% income loss reported significant increases in their depression scores. This makes sense as financial instability is associated with greater distress (Akkaya‐Kalayci et al., 2020; Olesen et al., 2013).
Notably, follow‐up analyses also examined temporal changes in alcohol‐related behavior in individuals with and without a clinically relevant increase in depression and anxiety scores, finding that the changes in drinking and the other mental health were largely independent. No differences in alcohol‐related behaviors were found in those with clinically relevant increases in depression or anxiety. Conversely, changes in drinking were not associated with changes in depression or anxiety. The exception was that those without clinically significant increases in depression showed significantly greater decreases in alcohol‐related problems from pre‐COVID to intra‐COVID, but the effect size was modest and the interaction did not substantively change the relationship. These results are surprising, as previous studies have reported increases in drinking in those reporting increases in mental health symptomology (Rodriguez et al., 2020), but may also be consistent with drinking being predominantly related to recreation and socializing in emerging adults, rather than negative affect regulation.
This study must be considered in the context of its strengths and limitations. The longitudinal design of this study allows mental health and alcohol consumption behaviors to be compared from before to during the COVID‐19 lockdown. Furthermore, the use of emerging adults, comparisons of sex differences, and examination of acute economic disruption further characterize the impact of COVID‐19 in important subpopulations. There also exist several methodological considerations. For example, the prepandemic assessment varied in terms of time frame, albeit within a structured window. Much of the sample identified as White, which limits the generalizability of the results, especially since ethnic minorities and other high‐risk groups (e.g., LGBTQ2S + individuals) have been disproportionately impacted by the pandemic with respect to financial burden and health concerns (Statistics Canada, 2020b, 2020d, 2020f). Furthermore, information was not collected regarding exposure to pandemic‐related loss/trauma or COVID‐19 status, which may have effects on mental health and substance use. Lastly, this was a volunteer‐based sample of emerging adults endorsing heavy drinking at certain thresholds at the time of recruitment, thus limiting generalizability to the general population in this age‐group. This latter consideration is mitigated, however, by the very high rates of drinking among emerging adults (CDC, 2020; Centre on Substance Use, 2019).
Overall, the current set of results suggests multifarious impacts of the COVID‐19 pandemic on heavy drinking in emerging adults. High‐risk drinking and alcohol‐related problems decreased across the sample and did so irrespective of sex and economic impact. Perhaps most saliently, the impact on other mental health indicators was not equally distributed across the population. The COVID‐19 pandemic had a selective negative effect on depression and anxiety in females and those with major income loss. Taken together, these results suggest that clinical service providers should attend closely to subpopulation status when considering the pandemic's mental health impacts.
CONFLICT OF INTEREST
James MacKillop is a principal in BEAM Diagnostics, Inc., but no BEAM products were used in the study reported. No other authors have declarations.
Supporting information
Supinfo S1
REFERENCES
- Adams‐Prassl, A. , Boneva, T. , Golin, M. & Rauh, C. (2020) Inequality in the impact of the coronavirus shock: evidence from real time surveys. Journal of Public Economics, 189, 104245. [Google Scholar]
- Akkaya‐Kalayci, T. , Kothgassner, O.D. , Wenzel, T. , Goreis, A. , Chen, A. , Ceri, V. et al. (2020) The impact of the COVID‐19 pandemic on mental health and psychological well‐being of young people living in Austria and Turkey: a multicenter study. International Journal of Environmental Research and Public Health, 17(23), 9111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Axelsson, L. & Ejlertsson, G. (2002) Self‐reported health, self‐esteem and social support among young unemployed people: a population‐based study. International Journal of Social Welfare, 11(2), 111–119. [Google Scholar]
- Bates, D. , Mächler, M. , Bolker, B.M. & Walker, S.C. (2015) Fitting linear mixed‐effects models using lme4. Journal of Statistical Software, 67(1), 1–48. [Google Scholar]
- Bäuerle, A. , Steinbach, J. , Schweda, A. , Beckord, J. , Hetkamp, M. , Weismüller, B. et al. (2020) Mental Health Burden of the COVID‐19 Outbreak in Germany: predictors of mental health impairment. Journal of Primary Care & Community Health, 11, 215013272095368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck, K.H. , Caldeira, K.M. , Vincent, K.B. & Arria, A.M. (2013) Social contexts of drinking and subsequent alcohol use disorder among college students. The American Journal of Drug and Alcohol Abuse, 39(1), 38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blevins, C.A. , Weathers, F.W. , Davis, M.T. , Witte, T.K. & Domino, J.L. (2015) The posttraumatic stress disorder checklist for DSM‐5 (PCL‐5): development and initial psychometric evaluation. Journal of Traumatic Stress, 28(6), 489–498. [DOI] [PubMed] [Google Scholar]
- Brooks, S.K. , Webster, R.K. , Smith, L.E. , Woodland, L. , Wessely, S. , Greenberg, N. & et al. (2020). The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet, 395 10227, 912–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burke, R.J. & Weir, T. (1978) Benefits to adolescents of informal helping relationships with their parents and peers. Psychological Reports, 42(3_suppl), 1175–1184. [Google Scholar]
- Butt, P. , Beirness, D. , Gliksman, L. , Paradis, C. & Stockwell, T. (2011) Alcohol and health in Canada: a summary of evidence and guidelines for low risk drinking. Ottawa, ON: Canadian Centre on Substance Abuse. [Google Scholar]
- Cao, W. , Fang, Z. , Hou, G. , Han, M. , Xu, X. , Dong, J. et al. (2020) The psychological impact of the COVID‐19 epidemic on college students in China. Psychiatry Research, 287, 112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC . (2020). Underage drinking. CDC. https://www.cdc.gov/alcohol/fact‐sheets/underage‐drinking.htm [Google Scholar]
- Centre on Substance Use . (2019). Alcohol (Canadian Drug Summary). https://www.ccsa.ca/alcohol‐canadian‐drug‐summary [Google Scholar]
- Clay, J.M. & Parker, M.O. (2020) Alcohol use and misuse during the COVID‐19 pandemic: a potential public health crisis?. The Lancet, 5(5), e259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins, R.L. , Parks, G.A. & Marlatt, G.A. (1985) Social determinants of alcohol consumption: the effects of social interaction and model status on the self‐administration of alcohol. Journal of Consulting and Clinical Psychology, 53(2), 189–200. [DOI] [PubMed] [Google Scholar]
- Czeisler, M.É. , Lane, R.I. , Petrosky, E. , Wiley, J.F. , Christensen, A. , Njai, R. et al. (2020) Mental health, substance use, and suicidal ideation during the COVID‐19 Pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report, 69(32), 1049–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawel, A. , Shou, Y. , Smithson, M. , Cherbuin, N. , Banfield, M. , Calear, A.L. et al. (2020) The effect of COVID‐19 on mental health and wellbeing in a representative sample of Australian adults. Frontiers in Psychiatry, 11, 579985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumas, T.M. , Ellis, W. & Litt, D.M. (2020) What does adolescent substance use look like during the COVID‐19 pandemic? Examining changes in frequency, social contexts, and pandemic‐related predictors. Journal of Adolescent Health, 67(3), 354–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettner, S.L. (1997) Measuring the human cost of a weak economy: Does unemployment lead to alcohol abuse? Social Science and Medicine, 44(2), 251–260. [DOI] [PubMed] [Google Scholar]
- Frasquilho, D. , Matos, M.G. , Salonna, F. , Guerreiro, D. , Storti, C.C. , Gaspar, T. et al. (2016). Mental health outcomes in times of economic recession: A systematic literature review Health behavior, health promotion and society. In BMC Public Health, 16(1), 1–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glowacz, F. & Schmits, E. (2020) Psychological distress during the COVID‐19 lockdown: the young adults most at risk. Psychiatry Research, 293, 113486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris, P.A. , Taylor, R. , Minor, B.L. , Elliott, V. , Fernandez, M. , O’Neal, L. et al. (2019) The REDCap consortium: building an international community of software platform partners. Journal of Biomedical Informatics, 95, 103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawke, L.D. , Barbic, S.P. , Voineskos, A. , Szatmari, P. , Cleverley, K. , Hayes, E. et al. (2020) Impacts of COVID‐19 on youth mental health, substance use, and well‐being: a rapid survey of clinical and community samples: Répercussions de la COVID‐19 sur la santé mentale, l’utilisation de substances et le bien‐être des adolescents : un sondage rapide d’échantillons cliniques et communautaires. Canadian Journal of Psychiatry, 65(10), 701–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang, Y. & Zhao, N. (2020) Generalized anxiety disorder, depressive symptoms and sleep quality during COVID‐19 outbreak in China: a web‐based cross‐sectional survey. Psychiatry Research, 288, 112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes, K. , Furness, L. , Jones, L. & Bellis, M.A. (2010). Reducing harm in drinking environments: evidence and practice in Europe. Liverpool: Centre for Public Health. [Google Scholar]
- Jacques‐Avinõ, C. , López‐Jiménez, T. , Medina‐Perucha, L. , De Bont, J. , Goncąlves, A.Q. , Duarte‐Salles, T. et al. (2020) Gender‐based approach on the social impact and mental health in Spain during COVID‐19 lockdown: a cross‐sectional study. British Medical Journal Open, 10(11), e044617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler, C.W. , Hustad, J. , Barnett, N.P. , Strong, D.R. & Borsari, B. (2008) Validation of the 30‐day version of the brief young adult alcohol consequences questionnaire for use in longitudinal studies. Journal of Studies on Alcohol and Drugs, 69(4), 611–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K. (2012) Enhancing the clinical utility of depression screening. Canadian Medical Association Journal, 184(3), 281–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K. , Spitzer, R.L. , Williams, J.B.W. & Löwe, B. (2010). The Patient Health Questionnaire Somatic, Anxiety,... [Gen Hosp Psychiatry. 2010 Jul‐Aug]—PubMed result. General Hospital Psychiatry, 32(4), 345–359. [DOI] [PubMed] [Google Scholar]
- Kujawa, A. , Green, H. , Compas, B.E. , Dickey, L. & Pegg, S. (2020) Exposure to COVID‐19 pandemic stress: associations with depression and anxiety in emerging adults in the United States. Depression and Anxiety, 37(12), 1280–1288. [DOI] [PubMed] [Google Scholar]
- Kuntsche, E. , Wicki, M. , Windlin, B. , Roberts, C. , Gabhainn, S.N. , Van Der Sluijs, W. et al. (2015) Drinking motives mediate cultural differences but not gender differences in adolescent alcohol use. Journal of Adolescent Health, 56(3), 323–329. [DOI] [PubMed] [Google Scholar]
- Larson, N. , Slaughter‐Acey, J. , Alexander, T. , Berge, J. , Harnack, L. & Neumark‐Sztainer, D. (2021) Emerging adults’ intersecting experiences of food insecurity, unsafe neighbourhoods and discrimination during the coronavirus disease 2019 (COVID‐19) outbreak. Public Health Nutrition, 24(3), 519–530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lechner, W.V. , Laurene, K.R. , Patel, S. , Anderson, M. , Grega, C. & Kenne, D.R. (2020) Changes in alcohol use as a function of psychological distress and social support following COVID‐19 related University closings. Addictive Behaviors, 110, 106527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, C.M. , Cadigan, J.M. & Rhew, I.C. (2020) Increases in loneliness among young adults during the COVID‐19 pandemic and association with increases in mental health problems. Journal of Adolescent Health, 67(5), 714–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee, J.O. , Hill, K.G. , Hartigan, L.A. , Boden, J.M. , Guttmannova, K. , Kosterman, R. et al. (2015) Unemployment and substance use problems among young adults: does childhood low socioeconomic status exacerbate the effect? Social Science and Medicine, 143, 36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, L.Z. & Wang, S. (2020) Prevalence and predictors of general psychiatric disorders and loneliness during COVID‐19 in the United Kingdom. Psychiatry Research, 291, 113267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, C.H. , Stevens, C. , Conrad, R.C. & Hahm, H.C. (2020) Evidence for elevated psychiatric distress, poor sleep, and quality of life concerns during the COVID‐19 pandemic among U.S. young adults with suspected and reported psychiatric diagnoses. Psychiatry Research, 292, 113345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu, C.H. , Zhang, E. , Wong, G.T.F. , Hyun, S. , & Hahm, H. (2020) Factors associated with depression, anxiety, and PTSD symptomatology during the COVID‐19 pandemic: clinical implications for U.S. young adult mental health. Psychiatry Research, 290, 113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGee, R.E. & Thompson, N.J. (2015) Unemployment and depression among emerging adults in 12 states, behavioral risk factor surveillance system, 2010. Preventing Chronic Disease, 12(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty, E.E. , Presskreischer, R. , Han, H. & Barry, C.L. (2020) Psychological distress and loneliness reported by US Adults in 2018 and April 2020. JAMA, 324(1), 93–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabi, R.L. , Prestin, A. & So, J. (2013) Facebook friends with (health) benefits? Exploring social network site use and perceptions of social support, stress, and well‐being. Cyberpsychology, Behavior, and Social Networking, 16(10), 721–727. [DOI] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism, & National Institute on Alcohol Abuse and Alcoholism (NIAA) . (2017). Drinking levels defined. [Google Scholar]
- Olesen, S.C. , Butterworth, P. , Leach, L.S. , Kelaher, M. & Pirkis, J. (2013) Mental health affects future employment as job loss affects mental health: findings from a longitudinal population study. BMC Psychiatry, 13(1), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce, M. , Hope, H. , Ford, T. , Hatch, S. , Hotopf, M. , John, A. et al. (2020) Mental health before and during the COVID‐19 pandemic: a longitudinal probability sample survey of the UK population. The Lancet Psychiatry, 7(10), 883–892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard, M.S. , Tucker, J.S. & Green, H.D. (2020) Changes in adult alcohol use and consequences during the COVID‐19 Pandemic in the US. JAMA Network Open, 3(9), e2022942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team (2020) R: A language and environment for statistical computing [Computer software manual]. Vienna: Austria. Retrieved from https://www.R‐project.org. [Google Scholar]
- Rahman, M.A. , Hoque, N. , Alif, S.M. , Salehin, M. , Islam, S.M.S. , Banik, B. et al. (2020) Factors associated with psychological distress, fear and coping strategies during the COVID‐19 pandemic in Australia. Globalization and Health, 16(1), 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read, J.P. , Wood, M.D. & Capone, C. (2005) A prospective investigation of relations between social influences and alcohol involvement during the transition into college. Journal of Studies on Alcohol, 66(1), 23–34. [DOI] [PubMed] [Google Scholar]
- Rodriguez, L.M. , Litt, D.M. & Stewart, S.H. (2020) Drinking to cope with the pandemic: the unique associations of COVID‐19‐related perceived threat and psychological distress to drinking behaviors in American men and women. Addictive Behaviors, 110, 106532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seco Ferreira, D.C. , Lisboa Oliveira, W. , Costa Delabrida, Z.N. , Faro, A. & Cerqueira‐Santos, E. (2020) Intolerance of uncertainty and mental health in Brazil during the Covid‐19 pandemic. Suma Psicológica, 27(1), 62–69. [Google Scholar]
- Solomou, I. & Constantinidou, F. (2020) Prevalence and predictors of anxiety and depression symptoms during the COVID‐19 pandemic and compliance with precautionary measures: age and sex matter. International Journal of Environmental Research and Public Health, 17(14), 4924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer, R.L. , Kroenke, K. , Williams, J.B.W. & Löwe, B. (2006) A brief measure for assessing generalized anxiety disorder: the GAD‐7. Archives of Internal Medicine, 166(10), 1092–1097. [DOI] [PubMed] [Google Scholar]
- Statistics Canada . (2020a). COVID‐19 in Canada: a six‐month update on social and economic impacts. [Google Scholar]
- Statistics Canada . (2020b). Economic impact of COVID‐19 among visible minority groups. [Google Scholar]
- Statistics Canada . (2020c). Gender differences in mental health during the COVID‐19 pandemic. [Google Scholar]
- Statistics Canada . (2020d). Impacts of COVID‐19 on immigrants and people designated as visible minorities. [Google Scholar]
- Statistics Canada . (2020e). The Daily — Payroll employment, earnings and hours, and job vacancies, October 2020. [Google Scholar]
- Statistics Canada . (2020f). Vulnerabilities related to COVID‐19 among LGBTQ2+ Canadians. [Google Scholar]
- Statistics Canada . (2021). Add/Remove data—Detailed household final consumption expenditure, Canada, quarterly. [Google Scholar]
- Toussaint, A. , Hüsing, P. , Gumz, A. , Wingenfeld, K. , Härter, M. , Schramm, E. et al. (2020) Sensitivity to change and minimal clinically important difference of the 7‐item Generalized Anxiety Disorder Questionnaire (GAD‐7). Journal of Affective Disorders, 265, 395–401. [DOI] [PubMed] [Google Scholar]
- Wang, C. , Pan, R. , Wan, X. , Tan, Y. , Xu, L. , Ho, C.S. & et al. (2020) Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. International Journal of Environmental Research and Public Health, 17(5), 1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washburn, I.J. , Capaldi, D.M. , Kim, H.K. & Feingold, A. (2014) Alcohol and marijuana use in early adulthood for at‐risk men: Time‐varying associations with peer and partner substance use. Drug and Alcohol Dependence, 140, 112–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White, A. & Hingson, R. (2013) The burden of alcohol use: excessive alcohol consumption and related consequences among college students. PsycNET Alcohol Research, 35(3), 201–218. [PMC free article] [PubMed] [Google Scholar]
- White, H.R. , Stevens, A.K. , Hayes, K. & Jackson, K.M. (2020) Changes in alcohol consumption among college students due to COVID‐19: effects of campus closure and residential change. Journal of Studies on Alcohol and Drugs, 81(6), 725–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization . (2020). Impact of COVID‐19 on people’s livelihoods, their health and our food systems. https://www.who.int/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supinfo S1


