Abstract
Purpose
To investigate the combined role of irrational beliefs, anxiety and depression in the 10-year incidence of type 2 diabetes, and the underlying effect of biochemical, and socio-behavioural factors.
Methods
Within the context of the ATTICA cohort study (2002–2012), 853 participants without evidence of CVD [453 men (45 ± 13 years) and 400 women (44 ± 18 years)] underwent psychological evaluation through the Irrational Beliefs Inventory (IBI) (range 0–88), the Zung Self-Rating-Depression-Scale (ZDRS) and the State-Trait-Anxiety-Inventory (STAI). Diagnosis of diabetes at follow-up examination was based on the criteria of the American Diabetes Association (ADA).
Results
Mean IBI score was 53 ± 10 in men and 51 ± 11 in women (p = 0.68). Participants with high irrational beliefs who also had anxiety symptoms had a 93% excess risk of developing diabetes during the 10-year follow-up (Hazard Ratio 1.93; 95%CI 1.34, 2.78) as compared to those without anxiety. Moreover, diabetes risk was 73% higher among individuals with high levels of irrational beliefs and depression as compared to those where depression was absent (1.73; 1.21, 2.46). Lower education status, family history of diabetes, hypercholesterolemia, high BMI, as well as tumor necrosis factor and total antioxidant capacity were revealed as mediating risk factors related to the tested associations.
Conclusion
Irrational beliefs among apparently healthy adults trigger depression and anxiety symptomatology, and through the increased inflammation and oxidative stress profile, were associated with increased diabetes risk. This observation moves psychological research a step forward in supporting and guiding primary prevention of mental health and metabolic conditions.
Keywords: Irrational beliefs, Anxiety, Depression, Type 2 diabetes incidence, Inflammation, Oxidative stress
Introduction
Type 2 diabetes mellitus (T2DM) is a severe and chronic disease that affects quality of life and significantly contributes to morbidity and mortality [1–3]. According to the International Diabetes Federation (IDF), 1 in 11 adults aged 20–79 had diabetes in 2015 and by 2040 the number of individuals with T2DM is expected to rise to 642 million, worldwide [4, 5]. Diabetes is a demanding and expensive health condition without definitive treatment, making primary care the cornerstone of the global response to the disease prevention [6, 7].
During the past years, data from epidemiological studies underlined the crucial role of psychological disorders, such as depression, stress and anxiety, on several chronic illnesses. However, what triggers such disorders in relation to the development of cardio-metabolic diseases is still a matter of investigation. According to Albert Ellis’s rational-emotive behavioral therapy (REBT), irrational beliefs are negative, subjective and extremely unrealistic cognitive constructs (i.e., perfectionism, catastrophizing, frustration intolerance, self-, other- and life-downing) that may generate negative and dysfunctional emotions (like anxiety, depression, anger, etc.) and behavioural consequences (e.g., poor dietary or other lifestyle choices) under stressful circumstances [8–12]. The current literature suggests that psychological disorders are not direct causes of T2DM, but can cause fluctuations on glucose metabolism, increase body weight and, thus, lead to T2DM. Moreover, several studies have indicated that emotional disturbances can increase the risk of T2DM through unhealthy lifestyle behaviours, such as eating habits, physical inactivity, smoking and alcohol overconsumption [13, 14]. However, the exact pathways by which psychological disorders play a role in the development of T2DM are not well studied and understood. It is known that increased concentrations of pro-inflammatory cytokines contribute to the pathogenesis of T2DM [15, 16]. Cytokines also trigger the production of acute-phase reactants such as C-reactive protein [16]. The early stages of diabetes (prediabetes) are also characterized by an increased synthesis of pro-inflammatory cytokines and acute-phase proteins that show a gradual increase as the disease progresses [16]. Alongside, increased cytokine serum concentrations activate the hypothalamic–pituitary–adrenal (HPA) axis and increase oxidative stress in the brain [17, 18]. Moreover, the etiology of insulin resistance, dyslipidemia, β-cell dysfunction, impaired glucose tolerance and the subsequent development of T2DM has now been associated with increased oxidative stress [18, 19].
Although the association of anxiety and depression in T2DM risk has been proposed in previous studies, several bio-psychosocial mechanisms remain unclear regarding this association. To the best of our knowledge, no previous study has assessed the synergistic role of irrational beliefs, as a pre-cursor of neurotic/depressive symptomatology in the development of T2DM, by exploring the potential mediating effect of inflammation and oxidative stress. Therefore, the present study aimed to evaluate the combined role of irrational beliefs and specific mental health conditions, anxiety and depression, in the 10-year incidence of T2DM, taking into consideration a variety of inflammatory and oxidation markers, as well socio-behavioural factors. The research hypothesis was that irrational beliefs trigger emotions through certain inflammatory and oxidative stress pathways, leading to increased risk of diabetes.
Methods
Design
The ATTICA study is a population-based, prospective survey that was carried out in the province of Attica, in Greece. Briefly, 3042 adults (18–89 years old, 49% men, 73% participation rate) without any clinical evidence of cardiovascular, other atherosclerotic diseases, or chronic viral infections, agreed to give blood samples for biochemical and genetic analyses, in addition to the requested socio-demographic, lifestyle and medical information, including the psychological evaluation.
Setting
The study was conducted in the greater metropolitan Athens area (including 78% urban and 22% rural regions) during 2001–2002. The participants’ examination was performed using face-to-face interviews, in the individuals' home or workplace, by trained personnel (cardiologists, general practitioners, dieticians and nurses, as well as psychiatrists/psychologists). Two follow-up examinations (2006 and 2012) were also performed.
Sample
Of the initially enrolled 3042 participants, a subsample of 853 participants [453 men (45 ± 13 years), 400 women (44 ± 18 years)] agreed to participate in the psychological evaluation and form the working sample of this study. This subsample is representative of the total study’s sample since there were no differences in sex and age distribution between the studied sample and the overall study’s population (all p-values > 0.4).
Baseline measurements
Socio-demographic and lifestyle measurements
The sociodemographic and lifestyle characteristics assessed included age, sex, educational level attained and mean annual income during the past three years, dietary habits and level of adherence to the Mediterranean diet, physical activity status, and smoking habits. Socio-economic status (SES) was also classified into three groups (tertiles; low, medium and high) according to the SES categorization already used, taking into account education level and mean annual income of the preceding three years [20].
Current smokers were classified as individuals who smoked at least one cigarette per day during the previous year, former smokers were defined as those who had stopped smoking more than 1 year previously, and the rest were classified as never smokers.
Dietary habits were assessed using a validated semi-quantitative food-frequency questionnaire (FFQ), the EPIC-Greek questionnaire that was provided by the Unit of Nutrition of Athens University Medical School, and according to which participants recalled and reported average weekly or daily intake of food items during the past year [21]. Moreover, a specific diet score, i.e., the MedDietScore, was calculated based on the reported dietary habits and assessed adherence to the Mediterranean diet for each participant [22].
The short form of the International Physical Activity Questionnaire (IPAQ) was used to assess physical activity status. IPAQ was used as an index of weekly energy expenditure using frequency (times per week), duration (in minutes per time) and intensity of sports or other habits related to physical activity (in expended calories per time) [23]. Participants who did not report any physical activities were defined as sedentary, while the rest were classified as physically active.
Biochemical and clinical evaluation
Blood samples were collected from the antecubital vein between 8 to 10 am, in a sitting position after 12 h of fasting and alcohol abstinence. Blood glucose levels (mg/dL) were measured with a Beckman Glucose Analyzer (Beckman Instruments, Fullerton, CA, USA). Serum insulin concentrations were assayed using radioimmunoassay (RIA100, Pharmacia Co., Erlangen, Germany). Participants with baseline blood glucose levels > 125 mg/dl or reported previously diagnosed with T2DM or use of anti-diabetic medication (n = 210), were excluded from the present analysis, because according to the American Diabetes Association they are considered as having T2DM [24].
Obesity was defined as Body Mass Index (BMI) greater than 29.9 kg/m2, according to WHO criteria [25]. Waist (in cm) and hip (in cm) circumferences were also measured; and waist-to-hip (WH) and waist-to-height (WHt) ratios were calculated. An abnormal WH ratio was considered > 0.8 for women and > 1 for men, whereas an abnormal WHt ratio was > 0.5 for both sexes. Regarding other clinical characteristics, arterial blood pressure (3 recordings) was measured at the end of the physical examination with the subject in a sitting position and being at least 30 min at rest. Participants whose average blood pressure levels were ≥ 140/90 mmHg or were under antihypertensive medication were classified as being hypertensive. Hypercholesterolemia was defined as total cholesterol levels > 200 mg/dL or the use of lipids lowering agents. The intra and inter-assay coefficients of variation of cholesterol levels did not exceed 9%. The metabolic syndrome was defined according to ATP III criteria [26]. Furthermore, inflammatory markers (that is, C-reactive protein (CRP), serum amyloid-A (SAA), human tumor necrosis factor-alpha (TNF-α), fibrinogen, interleukin-6 (IL-6)) and oxidative stress markers (serum total antioxidant capacity (TAC) and plasma oxidized LDL-cholesterol (ox-LDL)) were also measured in our institution’s laboratory following established procedures, by a BNII Dade Behring automatic nephelometry.
Psychological evaluation
Irrational beliefs were assessed at baseline using the Irrational Beliefs Inventory (IBI), a brief self-report measure based on the work of Ellis [27]. The inventory consists of 11 statements, each reflecting one irrational belief, including, worrying, rigidity, need for approval, problem avoidance, and emotional irresponsibility [28]. Each item is followed by a 9-point bipolar scale ranging from disagree to agree. The scales are summed to yield a total score ranging from 0 to 88 (the higher score the greater severity of irrational beliefs). The IBI was developed as an instrument to assess the association between endorsement of irrational beliefs and various aspects of maladaptive emotion and behaviour that have been developed within Ellis's theoretical and applied model that views irrational beliefs as maladaptive [27]. For this study, the IBI score was also divided into 3 categories with the 1st tertile corresponding to the lowest IBI scores (< 48, i.e., less irrational beliefs/thoughts), the 2nd to the moderate IBI scores (48–56) and the 3rd to the highest IBI scores (> 56, i.e., frequent irrational beliefs/thoughts). Depressive symptomatology was assessed using the validated Greek translation of the Zung Self-Rating Depression Scale (ZDRS). The time window was the preceding 4-week period before the administration. The ZDRS total score range is 20–80; with higher values indicating more severe depression symptoms [29]. Based on the validated ZDRS cut-off score for the Greek population, we applied a cut-off score of 45 to dichotomize the study cohort to participants with and without clinically relevant depressive symptomatology [30]. Anxiety levels were assessed using the validated Greek translation of the State Anxiety subscale of the Spielberger State-Trait Anxiety Inventory (STAI) [31]. The total score of the 20-item STAI ranges from 20 to 80 with higher score values being indicative of more severe anxiety symptoms [29]. In the context of this study, the STAI score was used as a continuous variable, since cut-off scores for the adult Greek population require further validation [31].
10-year follow-up examination
The 10-year follow-up was performed during 2011–2012. Of the initially enrolled 3,042 participants at baseline, 2,583 participated at follow-up examination (85% participation rate; of those lost to follow-up, n = 224 could not be traced due to missing contact information and n = 235 denied participating). After also excluding participants diagnosed with T2DM at baseline (n = 210), and those who did not attend the psychological examination (n = 1,528), the working sample consisted of n = 845 participants. Diagnosis of T2DM at follow-up examination was based on the criteria of the American Diabetes Association mentioned above [24]. No differences in the baseline characteristics of the participants (age, sex, years of education, family history of diabetes, physical activity status, hypercholesterolemia, BMI, abnormal waist-to-hip and waist-to-height ratios and energy intake) were observed between those for whom information about their 10-year status was available compared to those that it was not (all p-values > 0.05). However, some differences were found regarding prevalence of hypertension (lost vs. participated to follow-up: 30% vs. 26%, p = 0.036), smoking habits (58% vs. 54%, p = 0.028), as well as fasting glucose levels (88 ± 12 vs. 80 ± 13 mg/dL, p = 0.005) and fasting insulin levels (12 ± 3.0 vs. 13 ± 3.4 μU/mL, p = 0.014).
Study size, power analysis
Power analysis showed that the number of participants in the working dataset was adequate to evaluate two-sided differences between subgroups of the study and the investigated parameters greater than 20%, achieving statistical power > 0.80 at < 0.05 probability level (p-value).
Statistical methods
Incidence (and the corresponding 95% confidence interval) of diabetes was calculated as the ratio of new cases to the number of people participated, free of diabetes at baseline, who participated in the follow-up. Continuous variables are presented as mean values ± standard deviation and categorical variables as frequencies. Associations between categorical variables were tested using the chi-squared test. Comparisons of mean values of normally distributed variables between those who developed diabetes and those who did not were performed using a Student’s t-test, after controlling for equality of variances using Levene’s test. For continuous variables that were not normally distributed (i.e., years of school education) the Mann–Whitney non-parametric test was applied to evaluate the differences in the distributions of the skewed variables. Continuous variables were tested for normality through P-P plots. Associations between normally distributed variables and IBI tertiles were evaluated through a one-way analysis of variance, while for the non-normally-distributed variables, the Kruskal–Wallis test was used. Associations between categorical variables and IBI tertiles were tested with chi-squared tests. Since the exact time to event (i.e., development of diabetes) was not known, the relative risk of developing the disease during the 10-year follow-up period was estimated using the odds ratios (OR) and their corresponding 95% confidence intervals (CIs) through logistic regression analysis. Interactions between sex and other covariates were tested in all steps, and when significant, they remained in the final model. Hosmer–Lemeshow test was applied to evaluate the models’ goodness-of-fit. The –2loglikelihood ratio of the initial vs. the final model was also calculated to evaluate models’ performance. All known confounders were included in the models, after testing for collinearity. Sobel’s test was used to evaluate a potential mediation effect of a covariate entered in the model. Path analysis using Structural Equation Modeling (SEM), was also performed in order to explore the paths by which IBI score affects T2DM risk. Specifically, two SEM were estimated in order to examine the theoretical research model, i.e., the direct or the mediating effect of IBI on CVD risk, through the effect of socio-demographic, biochemical and clinical factors. Results of path analysis are presented as regression coefficients; compact lines represent a direct effect, whereas dotted lines an indirect effect. STATA software, version 16 (TStat S.r.l. 67,039 Sulmona AQ, Italy) was used for all statistical analyses.
Results
Baseline characteristics and irrational beliefs
Mean IBI score was 53±10 for men and 51±11 for women (p = 0.68); mean STAI score was 40±11 for men and 40±12 for women (p = 0.79) and mean ZDRS score was 37±7 for men and 33±7 for women (p < 0.001). To explore the profile of participants according to their classification on the IBI scale an exploratory analysis was performed. As it can be seen in Table 1, people in the highest tertile were, older, more likely to be smokers, married, less educated, as they reported fewer school years and, they had lower annual income (p < 0.001). Also, those with a high level of irrational beliefs had higher BMI and prevalence of obesity (p < 0.001), medical history of hypercholesterolemia, (p = 0.004) and family history of diabetes (p = 0.05). No associations between irrational beliefs status of the participants and sex, sedentary lifestyle and history of hypertension were observed (all p-values > 0.10) (Table 1).
Table 1.
Baseline sociodemographic, lifestyle and clinical characteristics of the ATTICA study participants, according to IBI tertiles (n = 845)
| Overall sample | IBI tertiles | ||||
|---|---|---|---|---|---|
| 1st (Low) |
2nd (Moderate) |
3rd (High) |
p | ||
| Age, years | 39 ± 11 | 40 ± 10 | 41 ± 10 | 47 ± 8 | 0.001 |
| Male sex, % | 52 | 47 | 52 | 55 | 0.17 |
| Years of school | 13 ± 3 | 14 ± 2.5 | 13 ± 3 | 11 ± 3 | < 0.001 |
| Current smoking, % | 41 | 36 | 47 | 47 | < 0.001 |
| Sedentary life, % | 54 | 51 | 59 | 52 | 0.12 |
| Obesity, % | 48 | 47 | 54 | 55 | < 0.001 |
| Body Mass Index (kg/m2) | 25 ± 4 | 25 ± 4 | 26 ± 4 | 27 ± 4 | < 0.001 |
| MedDietScore (0–55) | 27.5 ± 8 | 27 ± 9 | 25.6 ± 7 | 27 ± 9 | < 0.001 |
| Family history of diabetes, %yes | 25 | 22 | 30 | 27 | 0.05 |
| Hypertension, %yes | 24 | 23 | 26 | 23 | 0.28 |
| Hypercholesterolemia, %yes | 31 | 27 | 33 | 34 | 0.004 |
| C-reactive protein (mg/L) | 2 ± 2.8 | 2.1 ± 2.8 | 2.1 ± 2.5 | 1.7 ± 3.7 | 0.002 |
| Interleukin 6 (IL-6) (pg/ml) | 1.3 ± 0.3 | 1.4 ± 0.3 | 1.3 ± 0.3 | 1.1 ± 0.4 | < 0.001 |
| TNF-alpha (pg/ml) | 6.1 ± 3 | 6.6 ± 2.4 | 6.3 ± 3.4 | 5 ± 2.6 | 0.13 |
| Total antioxidant capacity (μmol/L) | 237 ± 40 | 250 ± 55 | 233 ± 29 | 229 ± 38 | < 0.001 |
| Oxidised LDL—C (mg/dl) | 63 ± 33 | 72 ± 36 | 60 ± 31 | 54 ± 30 | 0.10 |
| Fibrinogen (mg/dl) | 304 ± 72 | 313 ± 72 | 308 ± 78 | 275 ± 52 | 0.55 |
| ZDRS (0–80) a | 35 ± 7 | 33 ± 6 | 36 ± 7 | 38 ± 6 | < 0.001 |
| STAI (0–80) b | 40 ± 12 | 35 ± 10 | 41 ± 11 | 45 ± 12 | < 0.001 |
Data are presented as mean ± standard deviation (SD) (i.e., mean (SD)). P-values were obtained using One-way analysis of variance for independent samples for the normally distributed variables, Kruskal–Wallis Test for the rest quantitative variables and chi squared test for categorical variables;
a Zung self-rating Depression Scale; b Spielberger State-Trait anxiety Inventory
10-year incidence of T2DM
During 2002–2012, the age-adjusted 10-year incidence of diabetes was n = 191 cases (12.9%, 95%CI: 10.4, 15.4), or 12.900 / 100.000 participants; of them, n = 97 (incidence: 13.4%, 95%CI: 10.8%, 16.0%) were men and n = 94 (incidence: 12.4%, 95%CI: 10.1%, 14.7%) were women (p for sex differences = 0.89); the men-to-women incidence ratio was approximately 1-to-1, across all age groups.
Then, the analysis was focused on those who developed diabetes during the past 10-years. It was revealed that participants who developed T2DM had 11.8% higher baseline IBI score as compared to those who did not develop (i.e., 57 vs. 51/80) (Table 2). Moreover, people who developed T2DM, were older, reported lower adherence to the Mediterranean diet at the baseline evaluation and had lower education level (all p-values < 0.05). Regarding anthropometric characteristics, participants who developed diabetes had higher BMI and waist circumference values, as well as abnormal WH and WHt ratios (all p-values < 0.001); additionally, they were more likely to be predisposed to diabetes due to family status, they had a medical history of hypertension and hypercholesterolemia, as well as higher fasting glucose, insulin, and triglycerides levels (all p-values < 0.001), increased levels of C-reactive protein (p = 0.009), TNF-alpha (p = 0.08) and fibrinogen (p < 0.001) at baseline (Table 2).
Table 2.
Baseline characteristics of the ATTICA study’s participants according to the 10-year diabetes incidence (n = 845)
| Status at 10-year follow – up | |||
|---|---|---|---|
| Socio-demographic characteristics | Without diabetes | With diabetes | p |
| Age, years | 44 ± 13 | 53 ± 11 | < 0.001 |
| Male sex, % | 49 | 51 | 0.57 |
| Education status, %Low | 6 | 18.5 | < 0.001 |
| Lifestyle characteristics | |||
| Current smokers, % | 54 | 52 | 0.62 |
| Physically active, % | 43 | 38 | 0.25 |
| MedDietScore (0–55) | 28 ± 8 | 24 ± 10 | 0.01 |
| Medical history and biomarkers | |||
| Fasting glucose, mg/dL | 88 ± 12 | 95 ± 14 | < 0.001 |
| Insulin levels (μU/ml) | 12 ± 1.2 | 12.6 ± 1.6 | < 0.001 |
| Triglycerides (mg/dl) | 91 ± 55 | 120 ± 32 | < 0.001 |
| Hypertension, % | 27 | 46 | < 0.001 |
| Hypercholesterolemia, % | 37 | 56 | < 0.001 |
| Family history of diabetes, % | 20 | 36 | < 0.001 |
| Body mass index, kg/m2 | 26 ± 4 | 29 ± 5 | < 0.001 |
| Waist circumference, cm | 88 ± 14 | 98 ± 16 | < 0.001 |
| Abnormal WHR ratio, % | 34 | 59 | < 0.001 |
| C-reactive protein (mg/L) | 2 ± 2.8 | 2.5 ± 2 | 0.009 |
| Interleukin 6 (IL-6) (pg/ml) | 1.3 ± 0.3 | 1.5 ± 0.2 | < 0.001 |
| TNF-alpha (pg/ml) | 6 ± 3 | 6.8 ± 1.5 | 0.08 |
| Total antioxidant capacity (μmol/L) | 238 ± 42 | 229 ± 14 | 0.84 |
| Oxidized LDL—C (mg/dl) | 63 ± 34 | 68 ± 32 | 0.78 |
| Fibrinogen (mg/dl) | 304 ± 73 | 309 ± 60 | 0.001 |
| Mental health conditions | |||
| IBI (22 – 88) | 51 ± 11 | 57 ± 9 | 0.001 |
| ZDRS (0–80) | 35 ± 7 | 38 ± 10 | 0.68 |
| STAI (0–80) | 39 ± 12 | 44 ± 8 | < 0.001 |
Participants who developed T2DM during the 10-year follow-up had an 11.8% higher IBI score at baseline examination as compared to those who did not develop (i.e., 57 vs. 51/80, p < 0.001). Moreover, the 10-year incidence of T2DM was 5% among those in the lowest IBI tertile, as compared to 7.8% among those in the middle and 7.5% among those in the highest tertile (p for trend < 0.001). Further analysis revealed that participants with high IBI score (i.e., above median value, 52) had a 12% higher risk of developing diabetes during the 10-year follow-up compared to those with IBI score below the median (OR, 95%CI, 1.12; 1.03, 1.28), after adjusting for age, sex, medical history of hypertension, hypercholesterolemia, BMI, MedDietScore, smoking habits, physical activity status and family history of diabetes.
Irrational beliefs, depression and anxiety in relation to diabetes incidence
A highly significant interaction was observed between IBI and STAI, as well as IBI and ZDRS on the risk of developing T2DM (p’s < 0.001). Thus, to evaluate the main goal of this study, i.e., the role of irrational beliefs in relation to anxiety and depression on the 10-year risk of T2DM, a latent variable (high-IBI-high/low-STAI) was created classifying participants with a high IBI score (i.e., above median value, 52, which is 50% of the participants) and high STAI score (> 40, median) in one group, and those with high IBI score but low STAI score into another. Similarly, a latent variable (high-IBI-high/low-ZDRS) was created classifying participants with high IBI and high ZDRS (> 34, median) into one group and those with high IBI and low ZDRS into the other. It was observed that the 66% of participants who had a high IBI score (i.e., above the median value, 52) also had a high STAI score (> 40, median) (68% men vs. 64% women, p = 0.08). Similarly, the 65% of individuals with a high IBI score also had a high ZDRS score (> 34, median) (68% men vs. 62% women, p = 0.01).
Unadjusted data analysis revealed that participants with high irrational beliefs, who also had anxiety symptoms, had a 93% higher risk of developing T2DM during the 10-year follow-up as compared to those with high levels of irrational beliefs but without anxiety symptomatology (OR, 95%CI, 1.93; 1.34, 2.78); i.e., an excess 81% risk as compared to the irrational beliefs effect alone, as reported above. Similarly, participants with a high irrational belief score who also reported depression symptoms, showed a 73% higher T2DM risk, compared to those who did not have depression symptoms (OR, 95%CI, 1.73; 1.21, 2.46) i.e., 61% excess risk as compared to the irrational beliefs effect alone.
To further explore the associations between participants’ characteristics and the 10-year incidence of diabetes in people who succumbed to anxiety and depression symptomatology because of irrational beliefs, we conducted additional analyses (Table 3). The 10-year incidence of T2DM was 15.1% among those who were classified as high-IBI-high-STAI, 6.4% among those who were high-IBI-low-STAI (p < 0.001), as well as 15.2% among those who were classified as high-IBI-high-ZDRS, and 6.8% among those who were high-IBI-low-ZDRS (p < 0.001). Moreover, participants who had anxiety and depression in addition to the irrational beliefs were mostly women (p = 0.08 and p = 0.01, respectively), older, less educated, less physically active and smokers compared to the participants with high irrational beliefs but without serious anxiety and depressive symptomatology (all p-values < 0.001). They also had a higher BMI, waist circumference and abnormal WHR ratio, as well as high triglyceride and hypertension levels (all p-values < 0.05). Regarding biochemical markers, high-IBI-high-STAI or high-IBI-high-ZDRS participants had higher levels of CRP, ox-LDL and fibrinogen as compared to those with high irrational beliefs but without serious symptoms of anxiety and depression (all p-values < 0.05) (Table 3).
Table 3.
Characteristics of participants with high IBI score (≥ 52), who also had anxiety symptoms (i.e., STAI > 40) or depression (ZDRS > 34) (n = 845)
| Baseline characteristics | Irrational beliefs & anxiety | Irrational beliefs & depression | ||||
|---|---|---|---|---|---|---|
| Participants with high-IBI-low-STAI |
Participants with high-IBI-high-STAI | p | Participants with high-IBI-low-ZDRS | Participants with high-IBI-high-ZDRS | p | |
| Age, years | 40 ± 10 | 45 ± 13 | < 0.001 | 42 ± 11 | 44 ± 13 | < 0.001 |
| Male sex, % | 52.2 | 47.4 | 0.08 | 53.4 | 46.8 | 0.01 |
| Years of school | 16 ± 4 | 10 ± 2.7 | < 0.001 | 15 ± 1 | 10 ± 3 | < 0.001 |
| Lifestyle | ||||||
| Current smokers, % | 35.8 | 43.3 | 0.006 | 35 | 43.8 | 0.001 |
| Physically active, % | 46.8 | 39.6 | 0.009 | 48 | 39 | 0.001 |
| MedDietScore (0–55) | 28 ± 6 | 23 ± 7 | < 0.001 | 27 ± 6 | 23 ± 7 | < 0.001 |
| Medical history | ||||||
| Fasting glucose, mg/dL | 89 ± 12 | 90 ± 12 | 0.78 | 90 ± 12 | 89 ± 12 | 0.23 |
| Insulin levels (μU/ml) | 12.5 ± 1.6 | 13 ± 4 | 0.001 | 12.8 ± 2.5 | 12.9 ± 4 | 0.57 |
| Triglycerides (mg/dl) | 106 ± 63 | 118 ± 85 | 0.004 | 106 ± 64 | 117 ± 84 | 0.01 |
| Hypertension, % | 24.4 | 32.7 | 0.002 | 26 | 32 | 0.02 |
| Hypercholesterolemia, % | 35.8 | 40.3 | 0.10 | 36 | 40 | 0.11 |
| Family history of diabetes, % | 24.6 | 21 | 0.13 | 23 | 21.7 | 0.55 |
| Body mass index, kg/m2 | 25 ± 4 | 27 ± 4 | < 0.001 | 25.2 ± 4 | 26.7 ± 4 | < 0.001 |
| Waist circumference, cm | 87 ± 15 | 90 ± 14 | < 0.001 | 87.6 ± 15 | 90 ± 14 | 0.004 |
| Abnormal WHR ratio | 28.8 | 41.3 | < 0.001 | 29.7 | 40.6 | < 0.001 |
| C-reactive protein (mg/L) | 1.6 ± 2.2 | 1.9 ± 2.4 | 0.005 | 1.6 ± 2.2 | 2 ± 2.5 | 0.008 |
| Interleukin 6 (IL-6) (pg/ml) | 1.3 ± 0.5 | 1.4 ± 0.4 | 0.007 | 1.4 ± 0.5 | 1.4 ± 0.5 | 0.14 |
| TNF-alpha (pg/ml) | 5.9 ± 4 | 6.4 ± 4.5 | 0.06 | 6 ± 4 | 6.3 ± 4.5 | 0.28 |
| Total antioxidant capacity (μmol/L) | 249 ± 53 | 226 ± 34 | < 0.001 | 242 ± 51 | 228 ± 35 | 0.01 |
| Oxidised LDL—C (mg/dl) | 57 ± 26 | 63 ± 28 | 0.003 | 58 ± 25 | 63 ± 29 | 0.01 |
| Fibrinogen (mg/dl) | 295 ± 62 | 313 ± 69 | < 0.001 | 299 ± 62 | 310 ± 70 | 0.006 |
As already reported, crude analysis revealed a positive association between high-IBI-high-STAI score and risk of developing T2DM during the 10-year follow-up. However, residual confounding may exist, especially when several associations between high-IBI-high-STAI score or high-IBI-high-ZDRS score and age, social, behavioural and biochemical factors were already observed. After adjustment for sex, age, educational and smoking status, participants with high-IBI-high-STAI had a 4.11 times higher likelihood of diabetes as compared to those with high-IBI-low-STAI (95%CI 1.13, 14.97) (Table 4, Model 2). It is notable that when educational status, mainly, and smoking habits, were taken into account in Model 2 the effect of high-IBI-high-STAI on 10-year T2DM incidence substantially increased as compared to the previous Model 1 (Table 4) (Sobel’s test for mediation p-value = 0.01). The association between high-IBI-high-STAI remained significant even when adjusting for BMI, physical activity (Model 3, Table 4); and MedDietScore (Model 4, Table 4), but lost its significance when medical history, and, particularly, family history of diabetes were entered in Model 5 (suggesting a strong mediation effect of the genetic predisposition) (Sobel’s test p-value p < 0.001).
Table 4.
Results from nested, multi-adjusted models that evaluated the association between irrational beliefs and anxiety with the 10-year incidence of diabetes (results are presented as Hazard Ratios and 95% confidence intervals)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| IBI & STAI | |||||
|
High-IBI-high-STAI vs High-IBI-low-STAI |
1.93* (1.34, 2.78) |
4.11* (1.13, 14.97) |
4.18* (1.04, 16.75) |
4.06* (1.05, 16.44) |
3.49 (0.67, 18.12) |
| Education status (medium vs. low tertile) |
0.53* (0.35, 0.79) |
0.57 * (0.38, 0.85) |
0.57* (0.38, 0.86) |
0.68 (0.43, 1.07) |
|
| Current smoking (Y/N) |
0.93 (0.66, 1.31) |
0.94 (0.66, 1.33) |
0.94 (0.66, 1.33) |
1.01 (0.68, 1.49) |
|
| Body Mass Index (per 1 kg/m2) |
1.15* (1.10, 1.19) |
1.15* (1.11, 1.20) |
1.15* (1.10, 1.20) |
||
| Physical activity (Y/N) |
0.92 (0.65, 1.29) |
0.92 (0.65, 1.29) |
0.90 (0.61, 1.33) |
||
| MedDietScore (per 1 unit) |
1.01 (0.98, 1.04) |
1.01 (0.97, 1.04) |
|||
| Hypertension (Y/N) |
1.34 (0.91, 1.96) |
||||
| Hypercholesterolemia (Y/N) |
1.68* (1.16, 2.43) |
All models are age and sex adjusted
*p-values < 0.05
Regarding irrational beliefs and depression, after adjustment for sex and age, depression-related-to-irrational beliefs were significantly associated with the 10-year incidence of diabetes (Model 1, Table 5). Specifically, participants with high IBI and high ZDRS score had a 1.51 times higher likelihood of developing T2DM during the 10-year follow-up as compared to participants who had high irrational beliefs but low levels of depression (95%CI 1.05, 2.18). Similar to the previous analyses, the later association remained significant even when adjusting for education, and smoking status, and slightly lost its significance when BMI, physical activity status, and Mediterranean diet adherence were taken into account (Models 2 and 3, Table 5). The impact of irrational beliefs and depression became insignificant when participants’ medical history, as well as family history of diabetes were entered in Model 5 (Sobel’s test p-value p = 0.03).
Table 5.
Results from nested, multi-adjusted models that evaluated the association between irrational beliefs and depression with the 10-year incidence of diabetes (results are presented as Hazard Ratios and 95% confidence intervals)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| IBI & ZDRS | |||||
|
High-IBI-high-ZDS vs High-IBI-low-ZDS |
1.51* (1.05, 2.18) |
2.16* (1.06, 4.41) |
1.85 (0.87, 3.94) |
1.87 (0.88, 3.97) |
1.69 (0.69, 4.12) |
| Education status (medium vs. low tertile) |
0.58* (0.38, 0.87) |
0.61* (0.40, 0.92) |
0.61* (0.40, 0.93) |
0.71 (0.45, 1.13) |
|
| Current smoking (Y/N) |
0.93 (0.66, 1.31) |
0.95 (0.67, 1.34) |
0.95 (0.67, 1.35) |
1.02 (0.69, 1.51) |
|
| Body Mass Index (per 1 kg/m2) |
1.15* (1.10, 1.19) |
1.15* (1.11, 1.20) |
1.15* (1.10, 1.20 |
||
| Physical activity (Y/N) |
0.93 (0.66, 1.32) |
0.93 (0.66, 1.31) |
0.92 (0.62, 1.35) |
||
| MedDietScore (per 1 unit) |
1.01 (0.98, 1.04) |
1.01 (0.98, 1.04) |
|||
| Hypertension (Y/N) |
1.32 (0.90, 1.93) |
||||
| Hypercholesterolemia (Y/N) |
1.64* (1.13, 2.37) |
||||
| Family history of diabetes (Y/N) |
2.41* (1.61, 3.60) |
All models are age and sex adjusted
*p-values < 0.05
Biochemical markers in relation to irrational beliefs – diabetes association
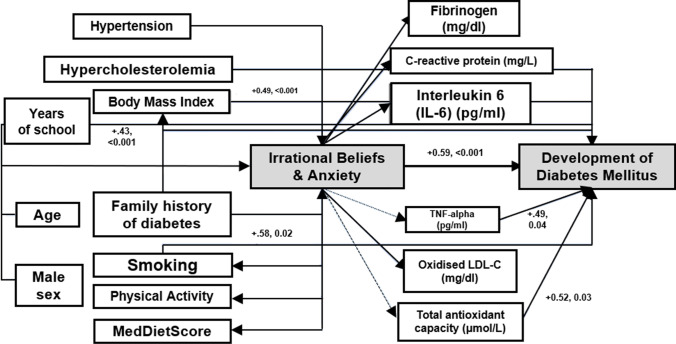
To further explore the potential mediating effect of inflammatory and oxidative stress markers on the associations between irrational beliefs, anxiety, depression and T2DM risk, we evaluated additional nested models by introducing each of the investigating biomarkers in the final Model 5 reported in Tables 4 and 5. It was observed that when TNF-α and total antioxidant capacity were entered in Model 5 (Table 4) that evaluated anxiety-related-to-irrational beliefs, a significant mediation occurred in the effect on the 10-year incidence of T2DM (OR 3.10, 95%CI 0.60, 15.94, Sobel’s test p-value p < 0.001 and OR 14.72, 95%CI 1.06, 203, Sobel’s test p-value p < 0.001, respectively). Figure 1 illustrates a path-model, that highlights the direct and indirect effect of high-IBI-high-STAI on the risk of developing T2DM (data represent beta-coefficients and p-values derived from the logistic regression models).
Fig. 1.
A path-model, that illustrates the direct and indirect effect of increased irrational beliefs and anxiety symptoms on the risk of developing diabetes (data presented as beta-coefficients and p-values and derived from the logistic regression models)
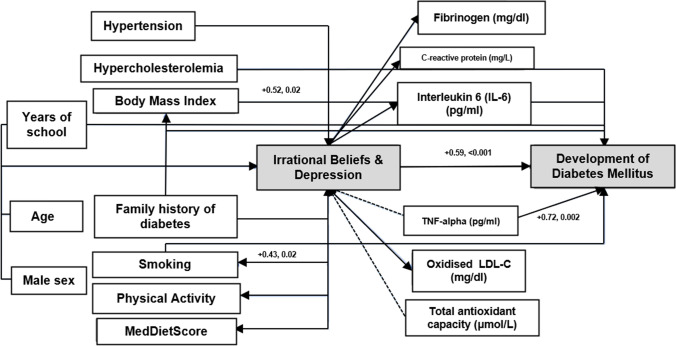
It was also observed that when TNF-α was entered in Model 5 (Table 5), a significant mediation occurred in the effect of depression related to irrational beliefs on the 10-year incidence of diabetes (OR 2.27, 95%CI 0.91, 5.68, Sobel’s test p-value p = 0.03). Figure 2 illustrates a path-model that demonstrates a direct and indirect effect of high-IBI-high-ZDRS on the risk of developing T2DM (data represent beta-coefficients and p-values derived from the logistic regression models).
Fig. 2.
A path-model, that illustrates the direct and indirect effect of increased irrational beliefs and depressive symptoms on the risk of developing diabetes (data presented as beta-coefficients and p-values and derived from the logistic regression models)
Discussion
In the present work, we evaluated the synergistic role of irrational beliefs, anxiety and depression over a 10-year incidence of T2DM. It was revealed that people who exhibit higher levels of irrational beliefs experience a higher 10-year risk of developing T2DM. Moreover, individuals who experience irrational beliefs synergistically with anxiety or depression experience excess risk of T2DM, which seems to be mediated by inflammation and oxidation markers levels. Despite the limitations of this work due to its observational (and not experimental) nature, it conveys important public health messages, since it strongly suggests, for the first time in the literature, the synergistic role of irrational beliefs, anxiety and depression in the development of T2DM and the underlying effect of particular inflammatory and oxidative stress markers, as well as socio-behavioural factors, like education level and dietary habits.
The inverse association between educational or socioeconomic status and T2DM has been reported in several studies. Although the causal mechanism between education and diabetes is unclear, limited education may contribute to diabetes development through complex processes including mediating risk factors, such as psychological attributes (stress, anxiety, depression, personality traits, unsuccessful coping strategies, etc.), lifestyle behaviours (smoking, physical inactivity, malnutrition, obesity, etc.), biochemical and clinical complications, as well as access and quality of healthcare services and information [32, 33]. Education level appears to assist individuals to generalize information into practical behaviours in order to prevent or manage chronic diseases more effectively and promote healthy behaviours (health literacy) [34, 35]. In contrast, low SES populations are subject to high levels of chronic stress that are likely to increase the risk of generalized anxiety, depression, unhealthy behaviours and coping strategies, even diabetes due to financial pressure, job insecurity, stigma and low income [33]. In accordance, the present study revealed that educational status was lower among individuals in the highest tertile of irrational beliefs, in participants with high levels of irrational beliefs and anxiety or depression symptoms and those who developed diabetes mellitus over a 10-year follow-up period. Moreover, educational status was a mediating factor in the relationship between participants who were classified as high-IBI-high-anxiety or -depression and a 10-year diabetes risk. Low educational status may coexist with irrational beliefs among individuals who have less opportunities to understand public health messages resulting in negative emotional problems, such as chronic stress, anxiety, depression and behavioural reactions (poor eating habits, heavy smoking and physical inactivity). This finding was consistent with previous studies showing a strong association between irrational beliefs and socioeconomically disadvantaged classes, as well as low socioeconomic status with adverse health outcomes, such as diabetes mellitus [36–38]. Actually, chronic stress associated with socioeconomic distress, can simultaneously affect lifestyle factors that can adversely influence inflammatory activity and oxidative stress [32]. In addition, chronic inflammation is considered a mediator of the association between socioeconomic adversity and type 2 diabetes association [34].
The relationship between anxiety and depression with inflammation and oxidative stress has been investigated in several studies, although the direction of this relationship remains unclear. The pathophysiology of depression is related to the inflammatory process due to microglial activation, increased cytokine release and oxidative stress [39, 40]. Additionally, psychological stress, and particularly emotional states of anxiety, fear and insecurity, affect hemostatic functions and trigger coagulation and fibrinolysis systems [41]. Elevated plasma homocysteine and interleukin-6 have also been associated with psychological stress, indicating another potential mechanism between anxiety and diabetes [41].
Although researchers examining psychological constructs are familiar with the perspective of psychological modulation of cellular immunity [12], little is known about the role of irrational beliefs in cytokines and oxidative stress and whether together they can predict T2DM. It is possible that irrational beliefs may not merely be a causal factor of emotional disturbances such as anxiety and depression, but also of biochemical reactions and clinical complications as in type 2 diabetes [12]. Such a hypothesis is generally supported by studies providing evidence that irrational beliefs increase the likelihood of experiencing negative feelings and physiological changes that predispose individuals to poor physical health [12]. The self-efficacy theory developed by Bandura (1977) and the maladaptive perfectionism construct may provide additional insight into the biopsychosocial aspects of the disease process. Self-efficacy is described as the belief in one’s capacity to act in such a way as to manage prospective situations [42]. People generally avoid health behaviours and activities when they do not feel confident to handle them [42]. Thus, these negative beliefs-expectations affect the thought cycle and emotions. Studies have shown that the perceived inefficacy transforms activities into stressors, resulting in the initiation of biochemical processes involving hormonal secretions, increased catecholamine secretion and weaknesses in the immune system [42]. Maladaptive perfectionism is considered an irrational, self-defeating belief combining excessively high personal performance standards and extremely critical self-evaluation, associated with a decline in preventive health behaviours, psychological distress, biochemical reactions e.g., high cortisol response and physical problems possibly via stress reactivity and health-risk behaviours [43–45].
Previous studies have shown that people who experience dysfunctional thoughts have higher plasma levels of C-reactive protein, interleukin-6, TNF-α and white blood cells than those with lower dysfunctional thinking [12]. Our findings are consistent with the aforementioned literature. Specifically, we found that participants with high irrational beliefs who also had anxiety or depression had augmented fibrinogen, CRP, TNF-α and LDL-C levels. Moreover, TNF-α and total antioxidant capacity showed to be strong mediating factors of the relationship between high-IBI-high-STAI or -ZDRS with type 2 diabetes incidence.
Bringing it all together, the combined impact of irrational beliefs system, anxiety and depression as well as certain socio-economic, and lifestyle indicators may promote an inflammatory state, oxidative stress and insulin resistance [12]. Behavioural factors like diet, physical activity and smoking are also linked to biochemical consequences. Eating habits away from a typical Mediterranean diet and high in saturated fat, for example, can promote both acute upregulation of pro-inflammatory biomarkers, such as IL-6 and sustained low-grade systemic inflammation and raised BMI, visceral fat mass and hypercholesterolemia [12, 46]. People with a sedentary lifestyle have higher concentrations of circulating pro-inflammatory mediators [12]. Smoking is also linked to insulin resistance, low-grade inflammation and increased oxidative stress [41]. Mechanisms involved include the abnormal activity of the sympathetic nervous system and secretion of catecholamines resulting in high cortisol levels and contributing to hyperglycemia as well as the hypothalamic–pituitary–adrenal axis activation which results in changes in inflammation [12]. Inflammation affects insulin receptor signaling, increases β-cell apoptosis and inflammatory markers and is associated with oxidative stress and future diabetes risk [46]. Even though our findings do not result in the mediating effect of specific lifestyle factors such as diet, smoking and physical inactivity in the tested relationships, they are associated with irrational beliefs and type 2 diabetes independently and potentially through the mediating effect of BMI.
Limitations
We are aware that our research has some limitations. Calculation of person-time and incidence rates were not feasible to be performed because the exact date of diabetes development was not available. The date of its diagnosis was included instead. As for diabetes determinants, relative risks were estimated by odds ratios through multiple logistic regression analysis, which may overestimate the actual relative risk. However, it is known that for low-prevalence diseases, the odds ratio is an accurate estimate of the relative risk. Another issue is that associations with disease incidence were based entirely on baseline information, but many lifestyle factors such as physical activity, and smoking status may have changed during the 10-year follow-up period. The working sample is likely to be a limitation of the current work although no differences were observed regarding age, sex distribution and SES level between those in the psychological evaluation and the remaining ATTICA study participants. The few significant, but meaningless differences observed regarding the baseline characteristics between those who participated in the 10-year follow-up and those who agreed to participate in the psychological evaluation may be considered a reporting bias. Finally, we did not control for genetic causal factors apart from family history of diabetes.
Conclusion
We consider our work the first step towards enhancing our understanding of how irrational beliefs synergistically with mental health problems can predict T2DM, through biochemical, social, and behavioural mechanisms. Our approach may be useful for guiding clinicians to detect high-risk individuals and target maladaptive thoughts in order to guide primary prevention before the potential onset of mental health problems that along with biochemical abnormalities could contribute to diabetes development. We may even suggest the implementation of intervention programs aimed at modifying irrational beliefs and lifestyle behaviours that undermine health. However, the findings need to be interpreted with caution as further observational and experimental studies are needed.
Acknowledgments
The authors would like to thank the ATTICA study group of investigators: Yannis Skoumas, Natassa Katinioti, Labros Papadimitriou, Constantina Masoura, Spiros Vellas, Yannis Lentzas, Manolis Kambaxis, Konstadina Palliou, Vassiliki Metaxa, Agathi Ntzouvani, Dimitris Mpougatsas, Nikolaos Skourlis, Christina Papanikolaou, Georgia-Maria Kouli, Aimilia Christou, Adella Zana, Maria Ntertimani, Aikaterini Kalogeropoulou, Evangelia Pitaraki, Alexandros Laskaris, Mihail Hatzigeorgiou and Athanasios Grekas for their assistance in the initial physical examination and follow-up evaluation, Efi Tsetsekou for her assistance in psychological evaluations, as well as the laboratory team: Carmen Vassiliadou and George Dedoussis (genetic analysis), Marina Toutouza-Giotsa, Constadina Tselika and Sia Poulopoulou (biochemical analysis) and Maria Toutouza for the database management.
Appendix
Funding
The ATTICA study was supported by research grants from the Hellenic Cardiology Society [HCS2002] and the Hellenic Atherosclerosis Society [HAS2003].
Data availability
The data that support the findings of this study are available from the ATTICA study but restrictions apply to the availability of these data, which were used under license for the current study, and so are not yet publicly available. Data are however available from the authors upon reasonable request and with permission of the ATTICA project.
Declarations
Ethics approval
The study was approved by the Institutional Ethics (#017/1.5.2001) committee and all participants were informed about the aims and procedures and agreed to participate providing written consent.
Conflicts of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Orozco-Beltrán D, Sánchez E, Garrido A, et al. Trends in mortality from diabetes mellitus in Spain: 1998–2013. Revista Española de Cardiología (English Edition) 2017;70(6):433–443. doi: 10.1016/j.rec.2016.09.022. [DOI] [PubMed] [Google Scholar]
- 2.Ramtahal R, Khan C, Maharaj-Khan K, et al. Prevalence of self-reported sleep duration and sleep habits in type 2 diabetes patients in South Trinidad. JEGH. 2015;5(S1):S35. doi: 10.1016/j.jegh.2015.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.İlhan N, Telli S, Temel B, Aştı T. Health literacy and diabetes self-care in individuals with type 2 diabetes in Turkey. Prim Care Diabetes. 2021;15(1):74–79. doi: 10.1016/j.pcd.2020.06.009. [DOI] [PubMed] [Google Scholar]
- 4.International Diabetes Federation. IDF Diabetes Atlas — 7th Edition. DiabetesAtlashttp://www.diabetesatlas.org/ (2015). [PubMed]
- 5.Makrilakis K, Kalpourtzi N, Ioannidis I, et al. Prevalence of diabetes and pre-diabetes in Greece. Results of the First National Survey of Morbidity and Risk Factors (EMENO) study. Diabetes Research and Clinical Practice. 2021 Feb;172:108646. [DOI] [PubMed]
- 6.Koloverou E, Panagiotakos DB, Pitsavos C, et al. 10-year incidence of diabetes and associated risk factors in Greece: the ATTICA study (2002–2012) Review of Diabetic Studies. 2014;11(2):181–189. doi: 10.1900/RDS.2014.11.181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. The Lancet. 2017;389(10085):2239–2251. doi: 10.1016/S0140-6736(17)30058-2. [DOI] [PubMed] [Google Scholar]
- 8.Dryden W, Bond FW. Reason and emotion in psychotherapy: Albert Ellis. Br J Psychiatry. 1994;165(1):131–135. doi: 10.1192/bjp.165.1.131. [DOI] [PubMed] [Google Scholar]
- 9.Hyland P, Boduszek D. Resolving a difference between cognitive therapy and rational emotive behaviour therapy: towards the development of an integrated CBT model of psychopathology. Ment Health Rev J. 2012;17(2):104–116. doi: 10.1108/13619321211270425. [DOI] [Google Scholar]
- 10.Buschmann T, Horn RA, Blankenship VR, et al. The Relationship Between Automatic Thoughts and Irrational Beliefs Predicting Anxiety and Depression. J Rat-Emo Cognitive-Behav Ther. 2018;36(2):137–162. doi: 10.1007/s10942-017-0278-y. [DOI] [Google Scholar]
- 11.Esmaeilinasab M, Ebrahimi M, Mokarrar MH, Rahmati L, Mahjouri MY, et al. Type II diabetes and personality; a study to explore other psychosomatic aspects of diabetes. J Diabetes Metab Disord. 2016;15(1):1–5. doi: 10.1186/s40200-016-0281-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Papageorgiou C, Panagiotakos DB, Pitsavos C, et al. Association between plasma inflammatory markers and irrational beliefs; the ATTICA epidemiological study. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30(8):1496–1503. doi: 10.1016/j.pnpbp.2006.05.018. [DOI] [PubMed] [Google Scholar]
- 13.Pouwer F, Kupper N, Adriaanse MC. Does emotional stress cause type 2 diabetes mellitus? A review from the European Depression in Diabetes (EDID) Research Consortium. Discov Med. 2010;9(45):112–118. [PubMed] [Google Scholar]
- 14.Bonnet F, Irving K, Terra J-L, et al. Anxiety and depression are associated with unhealthy lifestyle in patients at risk of cardiovascular disease. Atherosclerosis. 2005;178(2):339–344. doi: 10.1016/j.atherosclerosis.2004.08.035. [DOI] [PubMed] [Google Scholar]
- 15.Vogelzangs N, Kritchevsky SB, Beekman ATF, et al. Depressive Symptoms and Change in Abdominal Obesity in Older Persons. Arch Gen Psychiatry. 2008;65(12):1386. doi: 10.1001/archpsyc.65.12.1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Badawi. Type 2 diabetes mellitus and inflammation: Prospects for biomarkers of risk and nutritional intervention. DMSOTT. 2010 May;173. [DOI] [PMC free article] [PubMed]
- 17.Hoyo-Becerra C, Schlaak JF, Hermann DM. Insights from interferon-α-related depression for the pathogenesis of depression associated with inflammation. Brain Behav Immun. 2014;42:222–231. doi: 10.1016/j.bbi.2014.06.200. [DOI] [PubMed] [Google Scholar]
- 18.Henriksen EJ, Diamond-Stanic MK, Marchionne EM. Oxidative stress and the etiology of insulin resistance and type 2 diabetes. Free Radical Biol Med. 2011;51(5):993–999. doi: 10.1016/j.freeradbiomed.2010.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tangvarasittichai S. Oxidative stress, insulin resistance, dyslipidemia and type 2 diabetes mellitus. WJD. 2015;6(3):456. doi: 10.4239/wjd.v6.i3.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vlismas K, et al. Socio-economic status, dietary habits and health-related outcomes in various parts of the world: a review. Cent Eur J Public Health. 2009;17(2):55–63. doi: 10.21101/cejph.a3475. [DOI] [PubMed] [Google Scholar]
- 21.Panagiotakos DB, Pitsavos C, Stefanadis C. Dietary patterns: A Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr Metab Cardiovasc Dis. 2006;16(8):559–568. doi: 10.1016/j.numecd.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 22.Panagiotakos D. Dietary patterns: A Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr Metab Cardiov Dis 2006. [DOI] [PubMed]
- 23.Papathanasiou G, Georgoudis G, Papandreou M, et al. Reliability measures of the short International Physical Activity Questionnaire (IPAQ) in Greek young adults. Hellenic J Cardiol. 2009;50(4):283–294. [PubMed] [Google Scholar]
- 24.American Diabetes Association Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 1997;20(7):1183–1197. doi: 10.2337/diacare.20.7.1183. [DOI] [PubMed] [Google Scholar]
- 25.Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser, 2000. 894: p. i-xii, 1–253. [PubMed]
- 26.Grundy SM, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 27.Alden L, Safran J. Irrational beliefs and non-assertive behavior. Cognit Ther Res. 1978;2:357–364. doi: 10.1007/BF01172652. [DOI] [Google Scholar]
- 28.Bridges KR, Sanderman R. The irrational beliefs inventory: Cross cultural comparisons between American and Dutch samples. J Rational-Emot Cognitive-Behav Ther. 2002;20(1):65–71. doi: 10.1023/A:1015133004916. [DOI] [Google Scholar]
- 29.Kyrou I, Kollia N, Panagiotakos D, et al. Association of depression and anxiety status with 10-year cardiovascular disease incidence among apparently healthy Greek adults: The ATTICA Study. Eur J Prev Cardiolog. 2017;24(2):145–152. doi: 10.1177/2047487316670918. [DOI] [PubMed] [Google Scholar]
- 30.Fountoulakis KN, lacovides A, Samolis S, et al. Reliability, validity and psychometric properties of the Greek translation of the Zung Depression Rating Scale. BMC Psychiatry. 2001;1:6. [DOI] [PMC free article] [PubMed]
- 31.Fountoulakis KN, Papadopoulou M, Kleanthous S, et al. Reliability and psychometric properties of the Greek translation of the State-Trait Anxiety Inventory Form Y: preliminary data. Ann Gen Psychiatry. 2006;31(5):2. doi: 10.1186/1744-859X-5-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stringhini S, Batty GD, Bovet P, et al. Association of Lifecourse Socioeconomic Status with Chronic Inflammation and Type 2 Diabetes Risk: The Whitehall II Prospective Cohort Study. Ma RCW, editor. PLoS Med. 2013 Jul 2;10(7):e1001479. [DOI] [PMC free article] [PubMed]
- 33.Houle J, Lauzier-Jobin F, Beaulieu M-D, et al. Socioeconomic status and glycemic control in adult patients with type 2 diabetes: a mediation analysis. BMJ Open Diab Res Care. 2016;4(1):e000184. doi: 10.1136/bmjdrc-2015-000184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee TC, Glynn RJ, Peña JM, et al. Socioeconomic Status and Incident Type 2 Diabetes Mellitus: Data from the Women’s Health Study. Herder C, editor. PLoS ONE. 2011 Dec 14;6(12): e27670. [DOI] [PMC free article] [PubMed]
- 35.Dizaji MB, Taghdisi MH, Solhi M, Hoseini SM, Shafieyan Z, et al. Effects of educational intervention based on PRECEDE model on self care behaviors and control in patients with type 2 diabetes in 2012. J Diabetes Metab Disord. 2014;13(1):1–6. doi: 10.1186/2251-6581-13-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kollia N, Panagiotakos DB, Georgousopoulou E, et al. Exploring the association between low socioeconomic status and cardiovascular disease risk in healthy Greeks, in the years of financial crisis (2002–2012): The ATTICA study. Int J Cardiol. 2016;223:758–763. doi: 10.1016/j.ijcard.2016.08.294. [DOI] [PubMed] [Google Scholar]
- 37.Kastorini CM, Lykou A, Yannakoulia M, et al. The influence of a school-based intervention programme regarding adherence to a healthy diet in children and adolescents from disadvantaged areas in Greece: The DIATROFI study. J Epidemiol Community Health. 2016;70(7):671–677. doi: 10.1136/jech-2015-205680. [DOI] [PubMed] [Google Scholar]
- 38.Notara V, Panagiotakos DB, Kogias Y, et al. & GREECS Study Investigators. The Impact of Educational Status on 10-Year (2004–2014) Cardiovascular Disease Prognosis and All-cause Mortality Among Acute Coronary Syndrome Patients in the Greek Acute Coronary Syndrome (GREECS) Longitudinal Study. Journal of Preventive Medicine and Public Health. 2016; 49(4), 220–229. [DOI] [PMC free article] [PubMed]
- 39.Réus GZ, Carlessi AS, Silva RH, et al. Relationship of Oxidative Stress as a Link between Diabetes Mellitus and Major Depressive Disorder. Oxid Med Cell Longev. 2019;3(2019):1–6. doi: 10.1155/2019/8637970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Querstret D, Cropley M. Assessing treatments used to reduce rumination and/or worry: A systematic review. Clin Psychol Rev. 2013;33(8):996–1009. doi: 10.1016/j.cpr.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 41.Pitsavos C, Panagiotakos DB, Papageorgiou C, et al. Anxiety in relation to inflammation and coagulation markers, among healthy adults: The ATTICA Study. Atherosclerosis. 2006;185(2):320–326. doi: 10.1016/j.atherosclerosis.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 42.Karademas EC. Self-efficacy, social support and well-being. Personality Individ Differ. 2006;40(6):1281–1290. doi: 10.1016/j.paid.2005.10.019. [DOI] [Google Scholar]
- 43.Ellis A. The role of irrational beliefs in perfectionism. In: Flett GL, Hewitt PL, editors. Perfectionism: Theory, research, and treatment [Internet]. Washington: American Psychological Association; 2002 [cited 2021 Feb 1]. p. 217–29.
- 44.Williams CJ, Cropley M. The relationship between perfectionism and engagement in preventive health behaviours: The mediating role of self-concealment. J Health Psychol. 2014;19(10):1211–1221. doi: 10.1177/1359105313488971. [DOI] [PubMed] [Google Scholar]
- 45.Richardson CME, Rice KG, Devine DP. Perfectionism, emotion regulation, and the cortisol stress response. J Couns Psychol. 2014;61(1):110–118. doi: 10.1037/a0034446. [DOI] [PubMed] [Google Scholar]
- 46.Fedoce AG, Ferreira F, Bota RG, et al. The role of oxidative stress in anxiety disorder: cause or consequence? Free Radical Res. 2018;52(7):737–750. doi: 10.1080/10715762.2018.1475733. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the ATTICA study but restrictions apply to the availability of these data, which were used under license for the current study, and so are not yet publicly available. Data are however available from the authors upon reasonable request and with permission of the ATTICA project.