Abstract
Background
At the beginning of the COVID-19 pandemic, a cluster outbreak caused by an imported case from Hubei Province was reported in Xi’an City, Shaanxi Province, China. Ten patients from 2 families and 1 hospital were involved in the transmission.
Material/Methods
We conducted an epidemiological investigation to identify the cluster transmission of COVID-19. The demographic, epidemiological, clinical, laboratory, and cluster characteristics were described and analyzed.
Results
From January 27 to February 13, 2020, a total of 10 individuals were confirmed to be infected with SARS-CoV-2 by the nucleic acid testing of nasopharyngeal swabs from 2 families and 1 hospital. Among the confirmed cases, 7 had atypical clinical symptoms and 3 were asymptomatic. The median times from onset to diagnosis and to discharge were 3.5 days (range, 1–5 days) and 19.5 days (range, 16–38 days), respectively. There were 4 patients whose exposure dates were 1, 3, 3, and 2 days earlier than the onset dates of their previous-generation cases, respectively. Four prevention and control measures were effectively used to interrupt the disease transmission.
Conclusions
SARS-CoV-2 can be easily transmitted within families and in hospitals, and asymptomatic patients could act as a source of disease transmission. The results of this outbreak at the early epidemic stage support the recommendation that individuals with confirmed COVID-19 and all their close contacts should be subjected to medical quarantined observation and nucleic acid screening as early as possible, even if they do not have any symptoms. Meanwhile, people in high-risk areas should improve their protective measures.
Keywords: Asymptomatic Infections, Coronavirus Infections, Disease Outbreaks
Background
The fast spread of novel COVID-19 led to a global pandemic [1], and as of February 8, 2021, a total of 105 805 951 confirmed cases and 2 312 278 deaths were reported from 237 countries or regions worldwide [2]. There are several reasons explaining the rapid dissemination of COVID-19. First, SARS-CoV-2, the pathogen causing COVID-19, has high transmissibility and can be transmitted through the respiratory tract, particularly when individuals are in close contact, and other routes [3,4]. Second, there were large numbers of asymptomatic or minimally symptomatic carriers [5], and many studies demonstrated that asymptomatic cases play an important role in the disease transmission. Third, and most importantly, a lack of adoption of effective COVID-19 prevention and control measures made most countries vulnerable to the rapid spread of the disease, which in turn exacerbated further transmission.
There have been many studies on COVID-19, but despite the development of better understanding of the disease, the pandemic has become more serious. Many countries are still struggling to contain COVID-19, particularly the United States, where the cumulative COVID-19 cases and resulting deaths are over 18.82 million and 329 000, respectively [2]. In contrast, China, as the most seriously affected country in the early stage of the COVID-19 epidemic, has brought the disease under control successfully, which might be attributed to aggressive containment measures [6]. China was the first country to report COVID-19 and to recognize the seriousness of the new emerging disease. To slow the spread of the disease during the first stage of this global pandemic, with little knowledge and no effective vaccine or specific drug treatment for COVID-19, a range of nonpharmaceutical interventions were adopted, including prohibiting all travel, locking down cities, wearing masks, and social distancing; these measures were verified to be effective [7–10]. After paying a huge price, China has become the first country in the world to successfully contain the domestic spread of COVID-19. On September 7, the World Health Organization stated that China has brought the disease to a very low level [11] because all cases in the previous 20 days were imported and the people were quarantined right away. Up to February 8, 2021, the confirmed cases and deaths in China were 101 316 and 4 831, respectively [2].
Therefore, the experiences and practices of fighting against COVID-19 could serve as an invaluable reference for other countries or regions to contain the further development of COVID-19. Here, we report a cluster of SARS-CoV-2 infections in the early stage of the epidemic that occurred in Xi’an, Shaanxi Province, which was joint with Hubei Province, to provide more practical evidence for the prevention and control of COVID-19 and to highlight the importance of a swift response to the disease.
Material and Methods
Study Design
On January 27, 2020, a suspected case of COVID-19 in a person with a long history of residence in Xiaogan City (the secondary focus of COVID-19 in Hubei Province) was reported by hospital A in Xi’an City. The hospital immediately collected nasopharyngeal swab samples, which were sent to the local Center for Disease Control and Prevention (CDC) for nucleic acid testing. On January 28, the CDC reported that the case (index patient) was positive for SARS-CoV-2 nucleic acid. Then, 9 other cases were successively identified in the next 16 days, including 4 second-generation patients, 2 third-generation patients, 1 fourth-generation patient, and 2 fifth-generation patients.
Data Collection and Analysis
The data of patients were obtained from the epidemiological investigation during the COVID-19 outbreak in Xi’an City. A confirmed case was defined as an individual with positive respiratory swabs and clinical symptoms [12]. The date of onset of asymptomatic cases was defined as the date of collection of positive swab specimens, while the date of diagnosis was determined as the date of a positive test [13]. Using a unified questionnaire from the Third Edition of Novel Coronavirus Prevention and Control Protocol [14], the investigators had face-to-face interviews with the people with confirmed COVID-19 or had face-to-face or telephone interviews with their families and other informed persons (including medical staff) to obtain details on demographic characteristics, clinical symptoms, treatment history, and activity patterns (including history of travel, residence, exposure, and close contacts for 14 days prior to quarantine). Two investigators (HZ and ZJC) cross-checked the acquired data to make sure the information was correct. The demographic, epidemiological, clinical, and cluster characteristics of the 10 patients were described and analyzed.
Laboratory Testing
The nasopharyngeal swabs obtained from the patients were tested by real-time reverse-transcription polymerase chain reaction (RT-PCR) assay for SARS-CoV-2 or a genetic sequence that matches SARS-CoV-2, using from detection reagents from Shanghai Bojie Medical Technology Co., Ltd. and Shanghai Jienuo Biotechnology Co., Ltd.
Ethics Statement
This study was approved by the Institutional Review Board of the Xi’an City Center for Disease Control and Prevention (XA20200504). We obtained written consent from all the patients, and all the description and analysis were anonymized to protect the individuals’ privacy.
Results
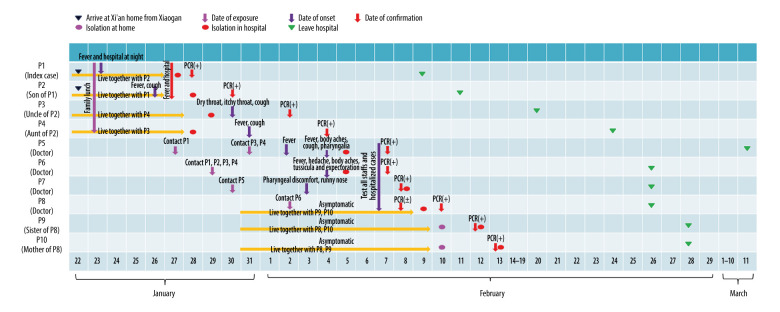
Ten individuals were confirmed as having SARS-CoV-2 infection, affecting 2 families and a public general hospital. We numbered the cases from 1 to 10 according to the order of illness onset (Figure 1).
Figure 1.
Timelines of progression in the clinical course in 10 patients with confirmed COVID-19.
Patient 1, the index case, was a 45-year-old woman living in Xiaogan City, Hubei Province. On January 22, she drove from Xiaogan to Xi’an with her husband and son. The next day, she developed a fever of 38.5°C and went to hospital A. She underwent a computed tomography (CT) examination, and the result was normal. From January 24 to 26, she had no fever during the day but had fevers up to 38.4°C at night. On January 27, she went to hospital A for re-examination, and she was questioned by the traffic police because the car license showed that the car was from Hubei Province. She was sent to hospital A and SARS-COV-2 infection was confirmed by a positive nucleic acid detection result on January 28. There were 6 close contacts related with her. Patient 2 was thought to be the second generation of this outbreak, along with patients 3, 4, and 5; patients 3 and 4 were family members of the index case and patient 5 was a doctor. Patients 6 and 7 were infected by the family member and the doctor, respectively. Patient 6 transmitted the disease to patient 8, who then spread it to family members, patients 9 and 10. Other detail information is shown in Table 1.
Table 1.
Information of the confirmed cases of COVID-19 in the cluster.
| Frist-generation | Second-generation | Third-generation | Fourth-generation | Fifth-generation | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Sex | Female | Male | Male | Female | Female | Male | Male | Female | Female | Female |
| Age | 45 | 14 | 54 | 53 | 44 | 47 | 54 | 53 | 55 | 83 |
| Exposure cause | Living history of Xiaogan | Living history of Xiaogan | Have lunch with 1,2 | Have lunch with 1,2 | Accept 1,3,4 | Accept 1,2,3,4 | Contact 5 | Contact 6 | Family of 8 | Family of 8 |
| Date of exposure | Before Jan 22 | Before Jan 25 | Jan 23 | Jan 23 | Jan 27 and 31 | Jan 29 | Jan 30 | Feb 2 | Feb 2–8 | Feb 2–8 |
| Date of onset | Jan 23 | Jan 26 | Jan 30 | Jan 31 | Feb 2 | Feb 4 | Feb 3 | Feb 9 | Feb 10 | Feb 12 |
| Date of quarantine | Jan 27 | Jan 28 | Jan 29 | Jan 28 | Feb 5 | Feb 5 | Feb 8 | Feb 9 | Feb 10 | Feb 10 |
| Date of confirm | Jan 28 | Jan 30 | Feb 2 | Feb 4 | Feb 7 | Feb 7 | Feb 8 | Feb 10 | Feb 12 | Feb 13 |
| Date of discharge | Feb 9 | Feb 11 | Feb 20 | Feb 24 | Mar 11 | Feb 26 | Feb 26 | Feb 26 | Feb 28 | Feb 28 |
| Exposure time (longest/shortest) (d) | −/1 | −/4 | 7 | 8 | 6/2 | 6 | 4 | 7 | 8/2 | 8/2 |
| Interval between onset and confirm (d) | 5 | 4 | 3 | 4 | 5 | 3 | 5 | 1 | 2 | 1 |
| Interval between onset and discharge (d) | 17 | 16 | 21 | 24 | 38 | 22 | 23 | 17 | 18 | 16 |
− Indicates that the exposure time of patients 1–2 cannot be accurately estimated due to the long-term residence in the epidemic area.
In the cluster, only 2 cases (patients 1 and 2) had an exposure history from traveling in an epidemic area of Hubei Province, while other cases had no exposure history in Hubei and no history of contacting other suspected sources (Table 1). Six cases were familial transmission, and 4 cases were nosocomial infection. The median times from onset to diagnosis and to discharge were 3.5 days (range, 1.0–5.0 days) and 19.5 days (range, 16.0–38.0 days), respectively. The median incubation period of COVID-19 was 4.0 days (range, 1.0–8.0 days), according to the shortest exposure time of patients 1 to 10. The day when patients 3 and 4 had a meal with patients 1 and 2 was 1 and 3 days earlier than the onset of the later 2, respectively, the day patient 7 contacted patient 5 was 3 days earlier than the onset for patient 5, and the exposure day of patient 8 was 2 days earlier than the onset for patient 6. The exposure time of the next generation was 3 days earlier than the onset of previous generation (Figure 1). At the time of admission, mycoplasma pneumoniae, chlamydia infection, and influenza A and B virus infection were excluded for all cases.
Of the 10 confirmed cases, 7 cases had varying degrees of clinical symptoms (Table 2) and 3 cases were asymptomatic. Fever and cough were the most common symptoms, reported in 5 (71%) and 5 (71%) individuals, respectively, and 1 adult was diagnosed as having severe pneumonia. The results of chest CT presented varying degrees of ground-glass pulmonary lesions upon admission for all patients, except patient 2, a teenager.
Table 2.
Clinical findings and laboratory test results of COVID-19 confirmed cases upon admission.
| Patient | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Clinical findings | Fever | Fever, cough | Dry throat, pharyngeal itching, expectoration | Fever, cough | Fever, muscular stiffness, pharyngalgia, cough | Fever, headache, muscular stiffness, white sputum | Throat discomfort, runny nose | No symptom | No symptom | No symptom |
| WBC (1×109/L) | 4.5 | 5.8 | 4.0 | 2.5* | 6.1 | 3.4* | 3.81* | 3.24* | 3.82 | 4.10 |
| NEU (1×109/L) | 2.6 | 2.3 | 3.5 | 1.8 | 4.1 | 2.1 | 2.06 | 2.28 | 2.02 | 2.53 |
| NEU% | 57.4 | 39.5* | 78.9 | 69.9 | 76.7# | 62.3 | 53.9 | 70.4# | 52.7 | 62.00 |
| LYM (1×109/L) | 1.6 | 3 | 0.5* | 0.6* | 0.8* | 0.8* | 1.41 | 0.64* | 1.43 | 1.20 |
| LYM% | 36.1 | 51.2# | 10.7* | 22.8 | 12.1* | 22.4 | 37.3 | 19.7* | 37.5 | 29.20 |
| CRP (mg/L) | 10.23# | <5.0 | 25.88# | <10.0 | <10.0 | 28.9# | <10.0 | <10.0 | <10.0 | <10.0 |
| hs-CRP (mg/L) | >10# | <0.5 | >10# | 4.85# | 4.64# | >10# | 0.53 | 4.89# | 1.56 | 4.20# |
| Chest CT | Multiple patchy and ground glass shadows in both lungs | Normal | Ground glass shadows in the both lungs, especially lower lobe of the left lung | Pleural hypertrophy and scattered ground glass shadows in both lungs | Multiple patchy ground glass shadows in the lower lobe of the right lung and the left lung | Nodules in the right upper lobe and the left lower lobe of the lung, and hyperdense shadow in the middle lobe of the right lung | Hyperdense shadows with blurred borders in the left lung near the subpleural nodules | Multiple stripe and patchy ground glass shadows with blurred borders in the left lower lobe of the lung | Flocculent and speckled hyperdense shadows in the upper lobe of the left lung and the middle and lower lobes of the right lung | Multiple flocculent hyperdense shadows with blurred borders in both lungs |
Indicates a reduced result compared to normal results,
indicates an increase result compared to normal results.
WBC – white blood cell; NEU (%) – neutrophils (%); LYM (%) – lymphocytes (%); CRP – C-reactive protein; hs-CRP – hypersensitive-C-reactive-protein; CT – chest computerized tomography.
Discussion
There were 10 patients confirmed in the cluster transmission of COVID-19 in the early stage of the epidemic from January 27 to February 13, 2020. The median incubation period was 4.0 days, which was consistent with previous studies [15–17]. The median time from onset to confirmation was 3.5 days, which was much shorter than in a previous study [18] and could be attributable to the definition of exposure time in this study.
Patient 1 had a long history of living in the focus of COVID-19 and was regarded as the index case of this outbreak. Patient 2 also lived in Xiaogan, but he was a student at a middle school, where he spent much of his time and had relatively smaller chance of contact with other sources of infection. No cases were found in the school. It was difficult to define the infectious source for patient 2, and the first apparent indication of human-to-human transmission in this cluster was detected with confirmed infection of patient 3. Upon patient 1 having a clinically diagnosed suspected case on the evening of 27 January, Xi’an CDC immediately conducted medical observation and nucleic acid testing for all close contacts, then confirmed patients 2–4. Due to the lack of emergency experience and inadequate protection in the early stage, 2 doctors working in hospital A (patients 5 and 6) were infected, most likely through contact with patients 1, 3, or 4. Patient 5 was regarded as the second-generation because she had been in close contact with patient 1 for up to an hour, while patient 6 had not. Furthermore, with the swift response in contact tracing and quarantine of close contacts, patients 7–10 were detected, ensuring no further onward transmission.
Many studies have shown that COVID-19 cases were highly contagious at the pre-incubation period [19–21]; however, the above results suggest that the exposure time of the next generation was earlier than 1–3 days after the onset of disease in the previous generation of patients (Table 1). This finding could indicate that COVID-19 cases had high infectivity for at least 3 days at the end of the incubation period [22,23]. The sixth edition of COVID-19 Prevention and Control Plan suggested that a person is infectious in the last 2 days of incubation of COVID-19 [24] and the current guideline, namely the seventh edition does not mention relevant information [25]. Our findings demonstrate that it might be earlier than we know.
Although patients 5 and 6 wore surgical masks when they were in contact with outpatients in the hospital, they were infected as well, indicating that only adopting primary protections such as surgical masks cannot prevent the transmission of COVID-19. Thus, wearing adequately protective equipment, such as N95 respirators, medical masks, eye protection, gowns, and gloves at the same time, should be strengthened in high-risk areas such as hospitals. Patient 8 was infected in the hospital and then transmitted the virus to family members during the incubation period, strengthening the evidence that asymptomatic cases play important roles in the transmission of COVID-19. Zou et al [26] found that the viral load of symptomatic and asymptomatic patients was similar. It has been reported that asymptomatic infected persons might represent a key node for epidemic prevention and control, and close contacts should be restricted as confirmed cases [27]. Du et al [28] suggested that 12.6% of transmission was presymptomatic. High infectivity and a high proportion of asymptomatic individuals (30%) among cases exacerbated the difficulty of preventing the dissemination of the disease, highlighting that more rigorous measures should be taken to control and prevent the transmission of COVID-19 [29].
To identify all suspected cases and control the transmission of COVID-19 in hospital A and other communities, medical officers adopted rigorous strategies and measures to block the further spread of COVID-19. The effective measures included the following. First, the Fever Clinic and Emergency Department of hospital A were shut down immediately, and terminal disinfection of the hospital was conducted. Medical service of the whole hospital was suspended, with patients with mild disease being transferred out of the hospital for home isolation and patients with severe disease remaining isolated in the hospital. Second, the nucleic acid screening was immediately conducted for all hospital staff and inpatients. People with positive results were hospitalized for isolation and treatment, while those with negative results were quarantined at home. Third, the CDC conducted comprehensive free nucleic acid screening for patients and their escort personnel who visited the hospital since January 23 and warned them to stay at home for 14 days of isolation. Meanwhile, the close contacts of the cases whose screening results were positive underwent nucleic acid screening and quarantined for 14 days. Fourth, at the expiration of the isolation period, the Xi’an CDC conducted nucleic acid screening for all the above-mentioned people again to ensure that there were no new infections. As of March 12, all close contacts associated with the outbreak had exceeded twice the longest incubation periods and the last case was discharged from the hospital. No new infections occurred, and the outbreak was considered to have subsided. Recent reports suggested that SARS-CoV-2 has mutated to increase its infectivity and a patient who had recovered was re-infected [30,31], which indicates that the effectiveness of the vaccine is questionable and strict control measures remain the effective means of preventing further development of the disease. Our study can serve as a valuable reference for controlling the transmission of COVID-19.
Conclusions
The cluster transmission of COVID-19 in the current study showed that COVID-19 can be easily transmitted within families and in hospitals, due to close contact and the lack of efficient protections. At the end of the incubation period (at least 3 days before onset), a patient can be highly contagious, and asymptomatic patients can also be a source of infection within clusters. It is recommended that people with confirmed cases should be quarantined and treated as quickly as possible, and that all their close contacts should be subjected to medical quarantined observation and nucleic acid screening to prevent the risk of further spread.
Acknowledgments
We thank all medical staff and health practitioners who have contributed to the fight against COVID-19.
Footnotes
Conflict of interest
None.
Source of support: This work was supported by the Health Research Fund Project of Xi’an (J201802036) and the National Natural Science Fund of China (81803289). The funding agencies had no role in the study design, data collection and analysis, or preparation of the manuscript
References
- 1.World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19. 2020. Mar 11, https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020.
- 2.World Health Organization. WHO coronavirus (COVID-19) dashboard. https://covid19.who.int/
- 3.Li Q, Guan X, Wu P, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yang HY, Duan GC. [Analysis on the epidemic factors for COVID-19]. Zhonghua Yu Fang Yi Xue Za Zhi. 2020;54(6):608–13. doi: 10.3760/cma.j.cn112150-20200227-00196. [in Chinese] [DOI] [PubMed] [Google Scholar]
- 5.Li R, Pei S, Chen B, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2) Science. 2020;368(6490):489–93. doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tian H, Liu Y, Li Y, et al. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368(6491):638–42. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lai S, Ruktanonchai NW, Zhou L, et al. Effect of non-pharmaceutical interventions to contain COVID-19 in China. Nature. 2020;585(7825):410–13. doi: 10.1038/s41586-020-2293-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsiang S, Allen D, Annan-Phan S, et al. The effect of large-scale anti-contagion policies on the COVID-19 pandemic. Nature. 2020;584(7820):262–67. doi: 10.1038/s41586-020-2404-8. [DOI] [PubMed] [Google Scholar]
- 9.Ng V, Fazil A, Waddell LA, et al. Projected effects of nonpharmaceutical public health interventions to prevent resurgence of SARS-CoV-2 transmission in Canada. CMAJ. 2020;192(37):E1053–64. doi: 10.1503/cmaj.200990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chinazzi M, Davis JT, Ajelli M, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (COVID-19) outbreak. Science. 2020;368(6489):395–400. doi: 10.1126/science.aba9757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization. Virtual press conference. 2020. Sep 7, https://www.who.int/docs/default-source/coronaviruse/transcripts/covid-19-virtual-press-conference---7-september-corrects-name.pdf.
- 12.National Health Commission, PRC. COVID-19 Diagnosis and Treatment Protocol (Trial version 4) [EB/OL] 2020. Jan 27, http://www.nhc.gov.cn/xcs/zhengcwj/202001/4294563ed35b43209b31739bd0785e67.shtml.
- 13.National Health Commission, PRC. Notice of the General Office of the National Health Commission on Issuing the New Coronavirus Pneumonia Prevention and Control Plan. Fifth Edition. 2020. Feb 21, http://www.nhc.gov.cn/jkj/s3577/202002/a5d6f7b8c48c451c87dba14889b30147.shtml.
- 14.National Health Commission, PRC. Notice of the General Office of the National Health Commission on Printing and Distributing the Pneumonia Prevention and Control Plan for Novel Coronavirus Infection. Third Edition. 2020. Jan 28, [cited 2020 April 6[. http://www.nhc.gov.cn/xcs/zhengcwj/202001/470b128513fe46f086d79667db9f76a5.shtml.
- 15.Pung R, Chiew CJ, Young BE, et al. Investigation of three clusters of COVID-19 in Singapore: Implications for surveillance and response measures. Lancet. 2020;395(10229):1039–46. doi: 10.1016/S0140-6736(20)30528-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: Estimation and application. Ann Intern Med. 2020;172(9):577–82. doi: 10.7326/M20-0504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jin X, Lian JS, Hu JH, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69(6):1002–9. doi: 10.1136/gutjnl-2020-320926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tian S, Hu N, Lou J, et al. Characteristics of COVID-19 infection in Beijing. J Infect. 2020;80(4):401–6. doi: 10.1016/j.jinf.2020.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gao Y, Shi C, Chen Y, et al. A cluster of the Corona Virus Disease 2019 caused by incubation period transmission in Wuxi, China. J Infect. 2020;80(6):666–70. doi: 10.1016/j.jinf.2020.03.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang L, Zhang X, Zhang X, et al. Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16–23 years outside Wuhan and characteristics of young patients with COVID-19: A prospective contact-tracing study. J Infect. 2020;80(6):e1–e13. doi: 10.1016/j.jinf.2020.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Li P, Fu JB, Li KF, et al. Transmission of COVID-19 in the terminal stage of incubation period: A familial cluster. Int J Infect Dis. 2020;96:452–53. doi: 10.1016/j.ijid.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Qian G, Yang N, Ma AHY, et al. A COVID-19 Transmission within a family cluster by presymptomatic infectors in China. Clin Infect Dis. 2020;71(15):861–62. doi: 10.1093/cid/ciaa316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wei WE, Li Z, Chiew CJ, et al. Presymptomatic transmission of SARS-CoV-2 – Singapore, January 23–March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(14):411–15. doi: 10.15585/mmwr.mm6914e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Health Commission, Notice of the General Office of the National Health Commission on Issuing the New Coronavirus Pneumonia Prevention and Control Plan. Sixth Edition. 2020. Mar 7, http://www.nhc.gov.cn/xcs/zhengcwj/202003/4856d5b0458141fa9f376853224d41d7.shtml.
- 25.National Health Commission, PRC. Notice on Issuing the New Coronavirus Pneumonia Prevention and Control Plan. Seventh Edition. 2020. Sep 15, http://www.nhc.gov.cn/cms-search/xxgk/getManuscriptXxgk.htm?id=318683cbfaee4191aee29cd774b19d8d.
- 26.Zou L, Ruan F, Huang M, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382(12):1177–79. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465–69. doi: 10.1038/s41586-020-2196-x. [DOI] [PubMed] [Google Scholar]
- 28.Du Z, Xu X, Wu Y, et al. Serial interval of COVID-19 among publicly reported confirmed cases. Emerg Infect Dis. 2020;26(6):1341–43. doi: 10.3201/eid2606.200357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lu S, Lin J, Zhang Z, et al. Alert for non-respiratory symptoms of Coronavirus Disease 2019 (COVID-19) patients in epidemic period: A case report of familial cluster with three asymptomatic COVID-19 patients. J Med Virol. 2021;93(1):518–21. doi: 10.1002/jmv.25776. [DOI] [PubMed] [Google Scholar]
- 30.Korber B, Fischer WM, Gnanakaran S, et al. Tracking changes in SARS-CoV-2 spike: Evidence that D614G increases infectivity of the COVID-19 virus. Cell. 2020;182(4):812–27.e19. doi: 10.1016/j.cell.2020.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.To KK, Hung IF, Ip JD, et al. COVID-19 re-infection by a phylogenetically distinct SARS-coronavirus-2 strain confirmed by whole genome sequencing. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1275. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]