Abstract
Background:
Patients with hyperthyroidism have higher risk of atrial fibrillation (AF). However, the risk of thromboembolic event in patients with hyperthyroidism-related AF is controversial.
Objectives:
The aim of the study was to examine the risk of thromboembolic events in AF patients with/without hyperthyroidism.
Methods:
The national retrospective cohort study enrolled AF population was derived from the Taiwan National Health Insurance Research Database. The comparison between the AF patients with clinical hyperthyroidism (HT-AF group) and AF patients without hyperthyroidism (non-thyroid AF group) was made in a propensity score matched cohort and in a real-world setting, of which, the CHA2DS2-VASc level was treated as a stratum variable. The outcomes were ischemic stroke and systemic thromboembolism.
Results:
There were 3,880 patients in HT AF group and 178,711 in non-thyroid AF group. After propensity score analysis, the incidence of thromboembolism event and ischemic stroke were lower in HT AF patients than non-thyroid AF patients (1.6 versus 2.2 events per 100 person-years; HR, 0.73; 95% CI, 0.64–0.82 and 1.4 versus 1.8 events per 100 person-years; HR, 0.74; 95% CI, 0.64–0.84, respectively) in the 4.3 ± 3.2 year follow up period. The differences persistently existed in those receiving anticoagulants or not. In AF patients without anticoagulants, the incidence densities of ischemic stroke/systemic thromboembolism were significantly lower in HT AF group than those in non-thyroid AF group at CHA2DS2-VASc scores ≤ 4 (HR, 0.41; 95% CI, 0.35–0.48, p < 0.001), while the differences disappeared in case of score ≥ 5 (HR, 0.80; 95% CI, 0.63–1.02, p = 0.071).
Conclusion:
Patients with HT AF had lower incidence of thromboembolic events as compared to non-thyroid AF patients. The threshold of CHA2DS2-VASc score for anticoagulation in AF patients with clinical hyperthyroidism should be further evaluated.
Highlights
The incidence of thromboembolic event was different between hyperthyroidism-related atrial fibrillation (HT-AF) and non-thyroid AF patients.
Hyperthyroidism did not confer additional risk of thromboembolic event at CHA2DS2-VASc of ≤ 4.
The benefit of anticoagulation strategy in patients with hyperthyroidism-related AF should be further evaluated, especially at low CHA2DS2-VASc score.
Keywords: hyperthyroidism, atrial fibrillation, thromboembolism, ischemic stroke
Introduction
Atrial fibrillation (AF) is a complication of hyperthyroidism [1,2], and up to 13% of patients with new-onset AF have biochemical evidence of hyperthyroidism [3]. AF occurs in 5% to 15% of patients with hyperthyroidism compared to 1.5% to 2% in the general population [2,4]. However, individuals with hyperthyroidism-related AF differ from those with non-thyroid AF, with higher proportions of women and younger age in the former. In terms of stroke, hyperthyroidism induces hypercoagulable state, endothelial dysfunction, and high inflammation status which contributes to the incidence of thromboembolic events [5,6,7]. In addition, AF is also a well-known risk factor for thromboembolism, and is important to prevent thromboembolism in the management of AF [8]. A few studies have reported that individuals with hyperthyroid AF have a higher risk of stroke than those with non-thyroid AF [5,9,10]. However, there are currently no recommendations focusing on AF patients with clinical hyperthyroidism (HT AF) [8]. In addition, AF related to hyperthyroidism is sometimes considered to be reversible atrial tachyarrhythmia due to the high maintenance rate of sinus rhythm after controlling thyroid hormone [11], and because hypercoagulable and endothelial function can also be improved after correcting hyperthyroidism [6]. Moreover, better adherence to antithyroid drugs was reported to result in a lower risk of stroke in patients with hyperthyroidism in a national cohort study [12].
The CHA2DS2-VASc score is used to predict the risk of stroke/systemic embolism in non-valvular AF patients: Anticoagulation therapy is recommended in patients at CHA2DS2-VASc score ≥ 2 (this treatment can also be considered in case of a CHADS2-VASc of 1) [8]. This study hypothesized that the risk of thromboembolism in patients with new-onset HT AF would be lower than that in non-thyroid AF patients. The Taiwan National Health Insurance Research Database (NHIRD) was utilized–a large national population-based database of medical records–to compare differences in the risk of thromboembolism between HT AF patients and non-thyroid AF patients [13].
Methods
Study cohort
This was a retrospective analysis derived from the NHIRD. A total of 331,484 patients with new-onset AF (International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) code 427.31) were identified from the NHIRD between January 1, 2001 and December 31, 2013. We excluded patients with possible other secondary AF and valvular AF, including those aged <20 years, those whose index diagnosis of AF was during hospitalization for cardiac surgery, and those who were diagnosed with rheumatic valvular heart disease. Those under amiodarone within 1 year before and after a diagnosis of AF were excluded due to the potential effects of this drug on thyroid function. In order to exclude patients with subclinical hyperthyroidism and those with a missing diagnosis of hyperthyroidism, those with a diagnosis of hyperthyroidism but without any prescriptions for anti-hyperthyroidism therapy within 1 year before the index date and the date of diagnosis of hyperthyroidism beyond 1 year before the diagnosis of AF were not accepted. Those with any history of hypothyroidism and those who had received total thyroidectomy within 1 year before and after a diagnosis of AF were excluded. To guarantee receiving adequate anti-hyperthyroidism therapy, those who died or had a thromboembolic event of interest within 180 days after the index date were excluded. The eligible patients were classified into two groups as the HT AF group and those with non-thyroid AF (non-thyroid AF group) (Figure 1). This study was approved by the Institutional Review Board of Chang Gung Memorial Hospital (201700281B1).
Figure 1.
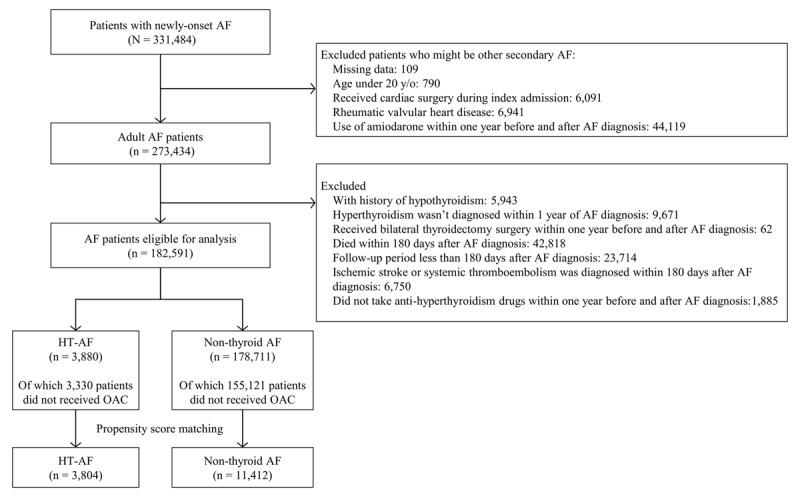
Flowchart of the study.
Comorbidities and outcome definition
Baseline comorbidities including hypertension, diabetes mellitus, chronic kidney disease, dyslipidemia, obstructive lung disease, ischemic heart disease, peripheral artery disease, and stroke were recorded with ICD-9-CM diagnosis codes during the index hospitalization and at least two consecutive clinic visits in the previous year before the index date. The index date was defined as the date when AF was first diagnosed and the observation period ended at the time of death, time of clinical outcome events, or on December 31, 2013. The primary outcome of interest was the occurrence of a thromboembolic event including ischemic stroke and systemic thromboembolism that was defined as the principal diagnosis for the hospitalization. Systemic thromboembolism was defined as the vascular thromboembolic occlusion of an extremity or extracranial vital organ.
Validation of atrial fibrillation, ischemic stroke and systemic thromboembolism in NHIRD
The validation of AF in the NHIRD has been assessed previously, with a positive predictive value (PPV) of 89% [14]. In addition, a previous study with 1,736 consecutive acute ischemic stroke patients validated acute ischemic stroke with a PPV of 88.4% and sensitivity of 97.3% [15]. Furthermore, a validation study for systemic thromboembolism was conducted at the medical center used by this team, and 120 hospitalizations for systemic thromboembolism in AF patients were randomly selected using the same criteria as in this study. After experienced physicians (YSL and VCCW) reviewed the medical records and all imaging results–including vascular duplex, computed tomography angiography, and intervention reports–the PPV of systemic thromboembolism was 86.7%.
Statistics
The baseline characteristics of the HT AF and non-thyroid AF groups were compared using the independent samples t-test for continuous variables and the chi-square test for categorical variables. The risks of mortality and thromboembolic events between the two groups were compared using a Cox proportional hazard model. The Cox models were first conducted in a propensity score-matched cohort, with each patient in the HT AF group being matched to three counterparts in the non-thyroid AF group according to the propensity score calculated based on age, sex, CHA2DS2-VASc components, and non-antithyroid drugs. The matching was processed using a greedy nearest neighbor algorithm with a caliper of 0.2 times of the standard deviation of the logit of propensity score, with random matching order and without replacement. Furthermore, we matched the HT AF patients with non-thyroid AF patients in the cohort with or without oral anticoagulation therapy separately. Cox models were also used in a real-world setting in which the CHA2DS2-VASc score was treated as a stratum variable when comparing the risks of thromboembolic events between the HT AF and non-thyroid AF groups. The study group (HT AF versus non-thyroid AF) was the only explanatory variable in the Cox models. The level of statistical significance was set as 0.05 and no adjustment of multiple testing (multiplicity) was made to avoid low statistical power in this study. Data analysis was conducted using SAS software version 9.4 (SAS Institute, Cary, NC), including the procedures of ‘psmatch’ for propensity score matching and ‘phreg’ for survival analysis.
Results
Baseline characteristics
From January 1, 2001 to December 31, 2013, a total of 331,484 patients with newly diagnosed AF were identified. After applying the exclusion criteria, a total of 182,591 patients were included, of whom 3,880 had HT AF and 178,711 had non-thyroid AF (Figure 1). The baseline characteristics are listed in Table 1. There were higher prevalence rates of nearly all comorbidities in the non-thyroid AF group compared to the HT AF group. In addition, the patients in the HT AF group were younger (Table 1). Similarly, the non-thyroid AF group used more medications, except for beta-blockers.
Table 1.
Real-world baseline characteristics and medications of the patients with atrial fibrillation with and without clinical hyperthyroidism before matching.
| Variables | The whole AF population | AF population without OAC | ||||
|---|---|---|---|---|---|---|
| HT AF (n = 3,880) | Non-HT AF (n = 178,711) | P-value | HT AF (n = 3,330) | Non-HT AF (n = 155,121) | P-value | |
| Age (years, mean, SD) | 60.1 ± 14.8 | 71.9 ± 13.6 | <0.001 | 59.9 ± 14.9 | 72.1 ± 13.7 | <0.001 |
| Sex | <0.001 | <0.001 | ||||
| Male | 1,355 (34.9) | 101,435 (56.8) | 1,139 (34.2) | 87,791 (56.6) | ||
| Comorbidities | ||||||
| Dyslipidemia | 202 (5.2) | 18,422 (10.3) | <0.001 | 165 (5.0) | 15,495 (10.0) | <0.001 |
| Chronic kidney disease | 232 (6.0) | 22,502 (12.6) | <0.001 | 198 (5.9) | 20,145 (13.0) | <0.001 |
| Obstructive pulmonary disease | 379 (9.8) | 35,923 (20.1) | <0.001 | 322 (9.7) | 32,618 (21.0) | <0.001 |
| Ischemic heart disease | 886 (22.8) | 63,793 (35.7) | <0.001 | 753 (22.6) | 55,482 (35.8) | <0.001 |
| Peripheral arterial disease | 57 (1.5) | 4,712 (2.6) | <0.001 | 47 (1.4) | 4,014 (2.6) | <0.001 |
| History of stroke | 223 (5.7) | 26,797 (15.0) | <0.001 | 185 (5.6) | 23,080 (14.9) | <0.001 |
| History of myocardial infarction | 57 (1.5) | 6,778 (3.8) | <0.001 | 48 (1.4) | 5,929 (3.8) | <0.001 |
| Malignancy | 135 (3.5) | 10,549 (5.9) | <0.001 | 120 (3.6) | 9,373 (6.0) | <0.001 |
| Components of CHA2DS 2-VASc | ||||||
| Congestive heart failure | 240 (6.2) | 21,632 (12.1) | <0.001 | 198 (5.9) | 18,741 (12.1) | <0.001 |
| Hypertension | 1,738 (44.8) | 100,341 (56.1) | <0.001 | 1,485 (44.6) | 85,996 (55.4) | <0.001 |
| Age (years) | <0.001 | <0.001 | ||||
| 65–74 | 765 (19.7) | 45,486 (25.5) | 645 (19.4) | 38,488 (24.8) | ||
| ≥75 | 724 (18.7) | 86,584 (48.4) | 610 (18.3) | 76,945 (49.6) | ||
| Diabetes mellitus | 548 (14.1) | 31,986 (17.9) | <0.001 | 466 (14.0) | 27,738 (17.9) | <0.001 |
| Prior stroke or systemic thromboembolism | 252 (6.5) | 29,643 (16.6) | <0.001 | 204 (6.1) | 25,053 (16.2) | <0.001 |
| Vascular disease | 927 (23.9) | 67,315 (37.7) | <0.001 | 787 (23.6) | 58,471 (37.7) | <0.001 |
| Sex: female | 2,525 (65.1) | 77,276 (43.2) | <0.001 | 2,191 (65.8) | 67,330 (43.4) | <0.001 |
| CHA2DS2-VASc score | <0.001 | <0.001 | ||||
| 0 | 532 (13.7) | 12,857 (7.2) | 465 (14.0) | 11,283 (7.3) | ||
| 1 | 1,134 (29.2) | 21,302 (11.9) | 986 (29.6) | 18,249 (11.8) | ||
| 2 | 751 (19.4) | 30,426 (17.0) | 644 (19.3) | 26,297 (17.0) | ||
| 3 | 552 (14.2) | 37,148 (20.8) | 464 (13.9) | 32,311 (20.8) | ||
| 4 | 445 (11.5) | 33,687 (18.8) | 377 (11.3) | 29,383 (18.9) | ||
| 5 | 276 (7.1) | 22,620 (12.7) | 226 (6.8) | 19,696 (12.7) | ||
| 6 | 114 (2.9) | 12,359 (6.9) | 104 (3.1) | 10,690 (6.9) | ||
| 7–9 | 76 (2.0) | 8,312 (4.6) | 64 (2.0) | 7,212 (4.6) | ||
| Total score | 2.2 ± 1.8 | 3.2 ± 1.9 | <0.001 | 2.2 ± 1.8 | 3.2 ± 1.9 | <0.001 |
| Medication | ||||||
| ACEI/ARB | 1,491 (38.4) | 75,769 (42.4) | <0.001 | 1,210 (36.3) | 62,690 (40.4) | <0.001 |
| CCB | 682 (17.6) | 48,664 (27.2) | <0.001 | 605 (18.2) | 42,425 (27.3) | <0.001 |
| β-blocker | 2,809 (72.4) | 61,562 (34.4) | <0.001 | 2,408 (72.3) | 51,644 (33.3) | <0.001 |
| Statin | 197 (5.1) | 19,519 (10.9) | <0.001 | 154 (4.6) | 15,674 (10.1) | <0.001 |
| Biguanides | 382 (9.8) | 18,936 (10.6) | 0.133 | 318 (9.5) | 16,090 (10.4) | 0.123 |
| Sulfonylurea | 392 (10.1) | 20,899 (11.7) | 0.002 | 339 (10.2) | 18,042 (11.6) | 0.010 |
| DPP4i | 76 (2.0) | 2,983 (1.7) | 0.164 | 60 (1.8) | 2,407 (1.6) | 0.249 |
| Insulin | 106 (2.7) | 6,125 (3.4) | 0.018 | 93 (2.8) | 5,384 (3.5) | 0.034 |
| Anticoagulants | 550 (14.2) | 23,590 (13.2) | 0.076 | NA | NA | NA |
| Anti-hyperthyroidism agents | ||||||
| Methimazole | 1,556 (40.1) | 0 (0.0) | NA | 922 (27.7) | 0 (0.0) | NA |
| Carbimazole | 455 (11.7) | 0 (0.0) | NA | 681 (20.5) | 0 (0.0) | NA |
| Propylthiouracil | 814 (21.0) | 0 (0.0) | NA | 374 (11.2) | 0 (0.0) | NA |
| Mixed (switch) | 1,055 (27.2) | 0 (0.0) | NA | 1,353 (40.6) | 0 (0.0) | NA |
ACEI, angiotensin-converting enzyme inhibitors; AF, atrial fibrillation; ARB, angiotensin receptor blockers; CCB, calcium channel blockers; DPP4i, dipeptidyl peptidase 4 inhibitor; HT, hyperthyroidism; OAC, oral anticoagulants; NA, not applicable; SD, standard.
Thromboembolic events between the HT AF and non-thyroid AF groups
Systemic thromboembolism and ischemic stroke were evaluated over a follow-up period of 4.3 ± 3.2 years and analyzed after propensity matching in order to adjust for disparities in baseline characteristics between groups. There were 3,804 patients in the HT AF group and 11,412 patients in the non-thyroid AF group (Supplemental Table S1). In terms of thromboembolic events, the incidence was lower in the HT AF group than in the non-thyroid AF group (1.6 versus 2.2 events per 100 person-years; hazard ratio [HR], 0.73; 95% confidence interval [CI], 0.64–0.82) (Figure 2A). When the incidence of thromboembolic events were assessed separately, the incidence of ischemic stroke was lower in the HT AF group than in the non-thyroid AF group (1.4 versus 1.8 events per 100 person-years; HR, 0.74; 95% CI, 0.64–0.84) (Figure 2B), and the trend was the same in the comparison of systemic thromboembolism (0.3 versus 0.5 events per 100 person-years; HR, 0.71; 95% CI, 0.55–0.93) (Figure 2C).
Figure 2.
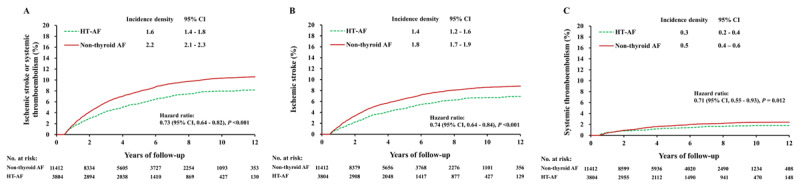
Cumulative event rates of ischemic stroke or systemic thromboembolism (A), ischemic stroke (B), and systemic thromboembolism (C) in AF patients with clinical hyperthyroidism and non-thyroid AF patients in a propensity score-matched cohort. AF: atrial fibrillation.
Regarding the mortality, the incidence of mortality was lower in the HT AF patients than that in the non-thyroid AF patients. (3.7 versus 10.2 events per 100 person-years; HR, 0.36; 95% confidence interval [CI], 0.34–0.39) and similar results can be observed after propensity score matching (3.7 versus 5.0 events per 100 person-years; HR, 0.74; 95% CI, 0.68–0.80) (Supplemental Figure S1).
Thromboembolic events in subgroups with/without anticoagulation therapy
The thromboembolic events in the patients with and without prescriptions for anticoagulants were analyzed after propensity matching and the baseline characteristics are listed in Supplemental Table S1. In the patients without anticoagulation therapy, the incidence of thromboembolic event was still significantly lower in the HT AF group than in the non-thyroid AF group (1.5 versus 2.1 events per 100 person-years; HR, 0.72; 95% CI, 0.62–0.82) (Figure 3A). The trend was similar in the comparisons of ischemic stroke and systemic thromboembolic events (Figure 3B, 3C). In the patients with anticoagulation therapy, the incidence of thromboembolic event was also significantly lower in the HT AF group than in the non-thyroid AF group (2.6 versus 3.6 events per 100 person-years; HR, 0.72; 95% CI, 0.55–0.95) (Figure 4A). The difference existed in terms of systemic thromboembolism and it has a trend in terms of ischemic stroke (Figure 4B, 4C).
Figure 3.
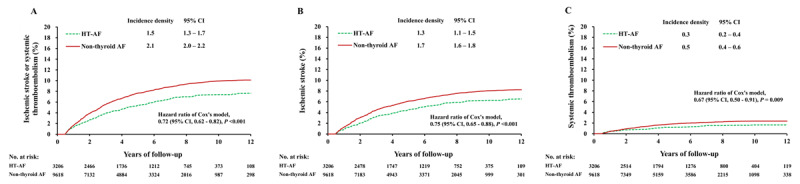
Cumulative event rates of ischemic stroke or systemic thromboembolism (A), ischemic stroke (B), and systemic thromboembolism (C) in AF patients with clinical hyperthyroidism and non-thyroid AF patients who were not prescribed with anticoagulants after propensity score matching. AF: atrial fibrillation.
Figure 4.
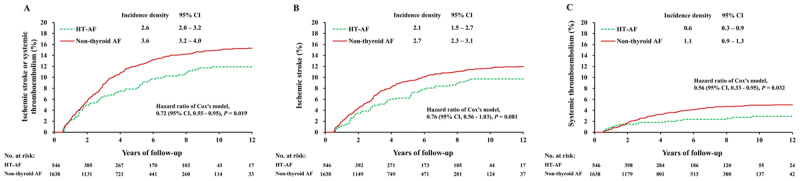
Cumulative event rates of ischemic stroke or systemic thromboembolism (A), ischemic stroke (B), and systemic thromboembolism (C) in AF patients with clinical hyperthyroidism and non-hyperthyroidism AF patients who were prescribed with anticoagulants after propensity score matching. AF: atrial fibrillation.
In addition, the incidence of thromboembolic events was analyzed in HT patients receiving different antithyroid drugs (including methimazole, carbimazole, and propylthiouracil) by excluding those who used two or more antithyroid drugs during the observation period. The risks of ischemic stroke among those receiving methimazole, carbimazole, or propylthiouracil were not significantly different, neither in the whole cohort nor in those stratified according to the use of anticoagulants (Supplemental Figure S2).
Thromboembolic events according to CHA2DS2-VASc score in patients without anticoagulant therapy
As shown in Table 1, the distribution of CHA2DS2-VASc scores differed in the two groups. The incidence density (ID) of thromboembolic event (Figure 5A) and ischemic stroke (Figure 5B) were significantly lower in the HT AF group than in the non-thyroid AF group with CHA2DS2-VASc scores of 1–4, but there was no significant difference in those with a CHA2DS2-VASc score ≥ 5 (Table 2). However, the incidence of systemic thromboembolism in the non-thyroid AF group was significantly higher than that in the HT AF group in both those with a CHA2DS2-VASc score ≤ 4 and ≥ 5 (Figure 5C) (Table 2). Importantly, those with HT-AF with a CHA2DS2-VASc score of 1 had very low rates of thromboembolic events, ischemic stroke, and systemic thromboembolism (ID: 0.6 events, 0.5 and 0.11 per 100 person-years, respectively), compared to the non-thyroid AF patients with a score of 0 (ID: 1.7 events, 1.4 and 0.35 per 100 person-years, respectively) (Figures 5A–5C). In terms of mortality, the incidence of mortality was higher in non-thyroid AF group than that in HT AF group in any level of CHA2DS2-VASc. (Supplemental Table S2)
Figure 5.
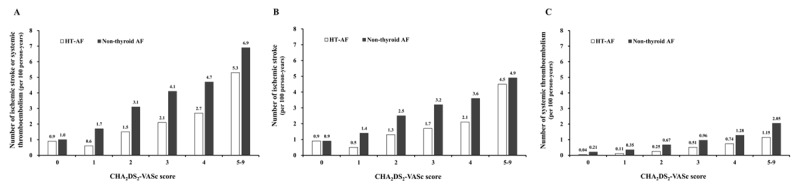
Incidence densities of ischemic stroke or systemic thromboembolism (A), ischemic stroke (B), and systemic thromboembolism (C) in AF patients with clinical hyperthyroidism and non-thyroid AF patients in a real-world setting according to CHA2DS2-VASc score. AF: atrial fibrillation.
Table 2.
Detailed information of Ischemic Stroke/Systemic Thromboembolism, Ischemic Stroke and Systemic Thromboembolism in AF patients with and without clinical hyperthyroidism who did not prescribe any anticoagulation therapy.
| Ischemic stroke/ Systemic thromboembolism | ||||||||
|---|---|---|---|---|---|---|---|---|
| CHA2DS2-VASc | HT AF | Non-HT AF | HT AF vs. Non-HT AF | |||||
| Numbers | Event (%) | ID (95% CI) § | Numbers | Event (%) | ID (95% CI) § | HR (95% CI) | P-value | |
| 0 | 465 | 21 (4.5) | 0.9 (0.5–1.3) | 11283 | 583 (5.2) | 1.0 (0.9–1.1) | 0.82 (0.53–1.27) | 0.376 |
| 1 | 986 | 32 (3.3) | 0.6 (0.4–0.8) | 18249 | 1462 (8.0) | 1.7 (1.6–1.8) | 0.36 (0.25–0.51) | <0.001 |
| 2 | 644 | 45 (7.0) | 1.5 (1.1–1.9) | 26297 | 3083 (11.7) | 3.1 (3.0–3.2) | 0.49 (0.36–0.65) | <0.001 |
| 3 | 464 | 43 (9.3) | 2.1 (1.5–2.7) | 32311 | 4512 (14.0) | 4.1 (4.0–4.2) | 0.52 (0.39–0.71) | <0.001 |
| 4 | 377 | 39 (10.3) | 2.7 (1.8–3.6) | 29383 | 4311 (14.7) | 4.7 (4.6–4.8) | 0.58 (0.42–0.80) | <0.001 |
| 5–9 | 394 | 67 (17.0) | 5.3 (4.0–6.6) | 37598 | 6800 (18.1) | 6.9 (6.7–7.1) | 0.80 (0.63–1.02) | 0.071 |
| Stratified | ||||||||
| 0–4 | 2936 | 180 (6.1) | 1.3 (1.1–1.5) | 117523 | 13951 (11.9) | 3.1 (3.0–3.2) | 0.41 (0.35–0.48) | <0.001 |
| 5–9 | 394 | 67 (17.0) | 5.3 (4.0–6.6) | 37598 | 6430 (17.1) | 6.9 (6.7–7.1) | 0.80 (0.63–1.02) | 0.071 |
| Total | 3330 | 247 (7.4) | 1.6 (1.4–1.8) | 155121 | 20381 (13.1) | 3.9 (3.8–4.0) | 0.44 (0.38–0.49) | <0.001 |
| Ischemic Stroke | ||||||||
| 0 | 465 | 21 (4.5) | 0.9 (0.5–1.3) | 11283 | 487 (4.3) | 0.9 (0.8–1.0) | 0.99 (0.64–1.53) | 0.954 |
| 1 | 986 | 28 (2.8) | 0.5 (0.3–0.7) | 18249 | 1226 (6.7) | 1.4 (1.3–1.5) | 0.37 (0.26–0.54) | <0.001 |
| 2 | 644 | 39 (6.1) | 1.3 (0.9–1.7) | 26297 | 2551 (9.7) | 2.5 (2.4–2.6) | 0.51 (0.37–0.70) | <0.001 |
| 3 | 464 | 35 (7.5) | 1.7 (1.1–2.3) | 32311 | 3627 (11.2) | 3.2 (3.1–3.3) | 0.53 (0.38–0.74) | <0.001 |
| 4 | 377 | 31 (8.2) | 2.1 (1.3–2.9) | 29383 | 3316 (11.3) | 3.6 (3.5–3.7) | 0.60 (0.42–0.86) | 0.005 |
| 5–9 | 394 | 57 (14.5) | 4.5 (3.3–5.7) | 37598 | 4747 (12.6) | 4.9 (4.8–5.0) | 0.93 (0.72–1.21) | 0.600 |
| Stratified | ||||||||
| 0–4 | 2936 | 154 (5.3) | 1.1 (0.9–1.3) | 117523 | 11207 (9.5) | 2.5 (2.5–2.5) | 0.44 (0.38–0.52) | <0.001 |
| 5–9 | 394 | 57 (14.5) | 4.5 (3.3–5.7) | 37598 | 4747 (12.6) | 4.9 (4.8–5.0) | 0.93 (0.72–1.21) | 0.600 |
| Total | 3330 | 211 (6.3) | 1.4 (1.2–1.6) | 155121 | 15954 (10.3) | 2.9 (2.9–2.9) | 0.48 (0.42–0.55) | <0.001 |
| Systemic Thromboembolism | ||||||||
| 0 | 465 | 1 (0.2) | 0.04 (–0.04–0.12) | 11283 | 123 (1.1) | 0.21 (0.17–0.25) | 0.19 (0.03–1.33) | 0.093 |
| 1 | 986 | 6 (0.6) | 0.11 (0.02–0.20) | 18249 | 313 (1.7) | 0.35 (0.31–0.39) | 0.32 (0.14–0.72) | 0.006 |
| 2 | 644 | 8 (1.2) | 0.25 (0.07–0.43) | 26297 | 721 (2.7) | 0.67 (0.62–0.72) | 0.38 (0.19–0.76) | 0.006 |
| 3 | 464 | 11 (2.4) | 0.51 (0.21–0.81) | 32311 | 1139 (3.5) | 0.96 (0.90–1.02) | 0.54 (0.30–0.98) | 0.042 |
| 4 | 377 | 11 (2.9) | 0.74 (0.30–1.18) | 29383 | 1254 (4.3) | 1.28 (1.21–1.35) | 0.58 (0.32–1.05) | 0.074 |
| 5–9 | 394 | 16 (4.1) | 1.15 (0.59–1.71) | 37598 | 2123 (5.7) | 2.05 (1.96–2.14) | 0.58 (0.36–0.95) | 0.030 |
| Stratified | ||||||||
| 0–4 | 2936 | 37 (1.3) | 0.25 (0.17–0.33) | 117523 | 3550 (3.0) | 0.75 (0.73–0.77) | 0.34 (0.25–0.47) | <0.001 |
| 5–9 | 394 | 16 (4.1) | 1.15 (0.59–1.71) | 37598 | 2123 (5.7) | 2.05 (1.96–2.14) | 0.58 (0.36–0.95) | 0.030 |
| Total | 3330 | 53 (1.6) | 0.33 (0.24–0.42) | 155121 | 5673 (3.7) | 0.99 (0.96–1.02) | 0.35 (0.26–0.45) | <0.001 |
AF, atrial fibrillation; HT, hyperthyroidism; ID, incidence density; CI, confidence interval; HR, hazard ratio.
§ Incidence density: Number of events per 100 person-years.
Discussion
This is the first large cohort study to evaluate the incidence of thromboembolism in patients with AF according to thyroid status using propensity score-matched analysis to compensate for baseline disparities. Results showed that the incidence rates of ischemic stroke and systemic thromboembolism were lower in the patients with HT AF than in those with non-thyroid AF, whether or not they were receiving anticoagulants. In addition, antithyroid medication did not alter the incidence of thromboembolism. In terms of ischemic stroke and thromboembolic event risk stratification, according to CHA2DS2-VASc score, the incidence rates in the HT AF group were significantly lower in those with a CHA2DS2-VASc score of ≤ 4 but comparable to those with a CHA2DS2-VASc score ≥ 5 in the non-thyroid AF group.
Atrial fibrillation in patients with clinical hyperthyroidism is often considered as reversible, with a high sinus rhythm maintenance rate after the restoration of thyroid function compared to those with non-hyperthyroid AF [11,16,17]. Thyroid hormone increases automaticity and enhances triggered activity of the cardiomyocytes of pulmonary veins, and this may increase the arrhythmogenic activity of pulmonary veins and thus induce the occurrence of AF [18]. This hinted at a lower burden of AF in patients with hyperthyroidism when the thyroid is in a euthyroid status [11]. In terms of burden of AF, it was reported to have high correlation with thromboembolic event from patients with cardiac implanted electronic devices implantation [19]. On the other hand, it was documented that long-term risk of ischemic stroke was lower in patients with AF occurring with stress than those with a history of AF from study enrolled patients admitted for sepsis [20]. This explained why the long-term risk of thromboembolism was significantly lower in HT AF group than non-thyroid AF group in this study though some studies showed higher thromboembolic event at the initial phase in hyperthyroidism patients with thyrotoxic AF [10].
One small prospective single center study reported a higher incidence of ischemic stroke in hyperthyroidism patients who presented with new-onset AF than in those without AF after 1 year of follow-up, after matching for age and gender [10]. However, another observational study that included AF patients did not find that hyperthyroidism was an independent risk factor for stroke or systemic thromboembolism in a 10-year follow-up period [21]. Moreover, another observational AF cohort study enrolled 642 hyperthyroid AF patients, and found that the patients with hyperthyroidism AF had a lower risk of stroke compared to their non-thyroid counterparts with the same CHA2DS2-VASc score [22]. Taken together, these studies suggest that hyperthyroidism may be a risk factor contributing to thromboembolism, but that AF plays a key role in thromboembolism, including ischemic stroke, in long-term follow up. However, these studies had some limitations, including a small sample size favoring heterogeneous conclusions and no adjustments for several comorbidities, even different baseline comorbidities between them. In addition, hyperthyroidism patients who present with AF should be treated, but this was not considered in these studies. To fill these gaps and to reduce confounding bias as far as possible, this study enrolled a large nationwide cohort. Based on reimbursements of the Taiwan National Health Insurance program, antithyroid therapy should be prescribed based on the clinical presentation and disease relevance. Therefore, around 5~6% of the AF patients had concomitant hyperthyroidism–or had a history of–and around 1% of those with new-onset AF also had a clinical diagnosis of hyperthyroidism in our study. This prevalence is similar to previous reports, in which 5~15% of patients with AF had hyperthyroidism, but fewer than 1% had new-onset AF caused by hyperthyroidism [2]. Of note, the presence of hyperthyroidism did not confer an additional risk of thromboembolic events compared with non-thyroid AF in the patients with a CHA2DS2-VASc score ≤ 4 in this study which was compatible to those with a CHA2DS2-VASc score ≥ 5. In addition, while the major drugs used to treat hyperthyroidism, including methimazole, carbimazole, and propylthiouracil are metabolized through the liver, none of the previous reports mentioned the impact of these drugs on thromboembolism, except for hepatoxicity [23,24]. As anticoagulants are mainly metabolized in the liver, a subgroup analysis was performed of those receiving different antithyroid therapies in those with/without anticoagulation therapy which found that the incidence of thromboembolic events may be not influenced by antithyroid therapies.
Furthermore, more than 80% of the AF patients did not receive anticoagulation therapy in the enrolled population, which allowed assessment of the “natural” incidence of thromboembolism. According to previous reports on the prevalence of the underuse of anticoagulation therapy in Asia, including Taiwan, only around 20~25% of AF patients receive anticoagulation therapy [25,26]. In terms of anticoagulation therapy in patients with hyperthyroidism-related AF in Asia, the prevalence varies from 6% in China [5] to around 20% in Hong Kong [22]. Further studies should be conducted in HT AF patients with anticoagulants.
The results of this study have two clinical implications: First, it provides strong evidence that the incidence of thromboembolic events differs between hyperthyroidism-related AF patients and non-thyroid AF patients, regardless of whether or not they receive anticoagulants. In addition, it was found that different antithyroid drugs did not influence the incidence of thromboembolic events in HT AF patients. Second, current guidelines mandate the use of anticoagulants in patients with a CHA2DS2-VASc score ≥ 2 and also suggest their use in patients with a CHA2DS2-VASc score of 1, but do not mention whether thyroid function should alter the strategy of preventing thromboembolic events in AF patients However, the incidence of thromboembolic events, including ischemic stroke, was lower than 1% in the HT AF patients with a CHA2DS2-VASc score £ 1 in this study. Several clinical trials have reported that direct oral anticoagulants should be considered when the annual incidence of stroke is ≥ 0.9% [27]. Therefore, the strategy of anticoagulation therapy for AF patients with clinical hyperthyroidism should be reconsidered and investigated further, especially in those with a CHA2DS2-VASc score of 1.
There are several limitations to this study. First, it could not be clearly confirmed that hyperthyroidism was the direct cause of AF as it was not possible to access the primary medical records of all patients. This study tried to increase the likelihood that AF in our patients was related to hyperthyroidism by enrolling patients with new-onset AF and a diagnosis of hyperthyroidism around the same time as the diagnosis of AF. This study also excluded patients under amiodarone therapy within 1 year before enrollment. Second, this study was unable to differentiate different types of AF because this information is not available in the NHIRD. However, the incidence of ischemic stroke is considered to be lower in paroxysmal AF patients than in those with sustained AF [28], and the different types of AF should not change the anticoagulation strategy [8]. In addition, Wong et al. reported that hyperthyroid AF patients who had a restored sinus rhythm had a lower incidence of stroke than those with persistent AF [29]. In this study, information on sinus rhythm restoration was lacking. Third, as laboratory data are not available in the NHIRD, thyroid function could not be assessed, and so subclinical hyperthyroidism or the severity of hyperthyroidism could not be clearly classified. Although the level of thyroxine may affect the restoration of sinus rhythm [30] and influence endothelial function and coagulation status [6], two strategies were used to minimize these limitations. The first strategy was to include antithyroid drugs as one of the selection criteria in the HT AF group to increase the likelihood of a correct diagnosis of hyperthyroidism, and the second was to count the number of clinical events after 6 months of antithyroid therapy under the assumption that a euthyroid status had been achieved.
Conclusion
In this study, the patients with hyperthyroidism-associated AF had a lower risk of thromboembolic events, including ischemic stroke, than those with non-thyroid AF, especially in those with a CHA2DS2-VASc score of ≤4. Findings suggested the use of anticoagulants might be reconsidered in patients with HT-related AF, especially at low CHA2DS2-VASc score. Further large database analyses are required to confirm these findings.
Additional File
The additional file for this article can be found as follows:
Tables S1 & S2 and Figures S1 & S2.
Acknowledgements
We would like to thank Alfred Hsing-Fen Lin and Zoe Ya-Jhu Syu for the statistical assistance during the completion of this manuscript
Contributor Information
Victor Aboyans, Email: vaboyans@live.fr.
Mien-Cheng Chen, Email: chenmien@ms76.hinet.net.
Competing Interests
The authors have no competing interests to declare.
Author Contributions
YS Lin, HY Tsai, V Aboyans and MC Chen contributed to study concept and design; HY Tsia, CY Lin and VCC Wu contributed to acquisition of data; VCC Wu, TH Chen and TY Yang contributed to analysis and interpretation of data; YS Lin, HY Tsia and CY Lin drafted the manuscript; YS Lin, V Aboyans and MC Chen critically revised the manuscript for important intellectual content. All authors reviewed the manuscript and completed final approval.
Victor Aboyans and Mien-Cheng Chen contributed equally as joint senior authors.
References
- 1.Bielecka-Dabrowa A, Mikhailidis DP, Rysz J, Banach M. The mechanisms of atrial fibrillation in hyperthyroidism. Thyroid Res. 2009; 2(1): 4. DOI: 10.1186/1756-6614-2-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klein I, Ojamaa K. Thyroid hormone and the cardiovascular system. N Engl J Med. 2001; 344(7): 501–9. DOI: 10.1056/NEJM200102153440707 [DOI] [PubMed] [Google Scholar]
- 3.Forfar JC, Miller HC, Toft AD. Occult thyrotoxicosis: A correctable cause of “idiopathic” atrial fibrillation. Am J Cardiol. 1979; 44(1): 9–12. DOI: 10.1016/0002-9149(79)90243-1 [DOI] [PubMed] [Google Scholar]
- 4.Sawin CT, Geller A, Wolf PA, et al. Low serum thyrotropin concentrations as a risk factor for atrial fibrillation in older persons. N Engl J Med. 1994; 331(19): 1249–52. DOI: 10.1056/NEJM199411103311901 [DOI] [PubMed] [Google Scholar]
- 5.Chen Q, Yan Y, Zhang L, Cheng K, Liu Y, Zhu W. Effect of hyperthyroidism on the hypercoagulable state and thromboembolic events in patients with atrial fibrillation. Cardiology. 2014; 127(3): 176–82. DOI: 10.1159/000356954 [DOI] [PubMed] [Google Scholar]
- 6.Burggraaf J, Lalezari S, Emeis JJ, et al. Endothelial function in patients with hyperthyroidism before and after treatment with propranolol and thiamazol. Thyroid. 2001; 11(2): 153–60. DOI: 10.1089/105072501300042820 [DOI] [PubMed] [Google Scholar]
- 7.Sato Y, Sato Y, Kakisako S, Honda Y, Kaji M. Cerebral embolism and hyperthyroidism. The Kurume Med J. 1989; 36(1): 23–7. DOI: 10.2739/kurumemedj.36.23 [DOI] [PubMed] [Google Scholar]
- 8.Kirchhof P, Benussi S, Kotecha D, et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS: The Task Force for the management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESCEndorsed by the European Stroke Organisation (ESO). Eur Heart J. 2016; 37(38): 2893–2962. DOI: 10.1093/eurheartj/ehw210 [DOI] [PubMed] [Google Scholar]
- 9.Poulin MF, Doukky R. Hyperthyroid atrial fibrillation: Does it matter for stroke risk? Cardiology. 2014; 128(1): 51–3. DOI: 10.1159/000357613 [DOI] [PubMed] [Google Scholar]
- 10.Siu CW, Pong V, Zhang X, et al. Risk of ischemic stroke after new-onset atrial fibrillation in patients with hyperthyroidism. Heart Rhythm. 2009; 6(2): 169–73. DOI: 10.1016/j.hrthm.2008.10.023 [DOI] [PubMed] [Google Scholar]
- 11.Nakazawa HK, Handa S, Nakamura Y, et al. High maintenance rate of sinus rhythm after cardioversion in post-thyrotoxic chronic atrial fibrillation. Int J Cardiol. 1987; 16(1): 47–55. DOI: 10.1016/0167-5273(87)90269-5 [DOI] [PubMed] [Google Scholar]
- 12.Tsai MS, Chuang PY, Huang CH, et al. Better adherence to antithyroid drug is associated with decreased risk of stroke in hyperthyroidism patients. Int J Clin Pract. 2015; 69(12): 1473–85. DOI: 10.1111/ijcp.12724 [DOI] [PubMed] [Google Scholar]
- 13.Lin LY, Warren-Gash C, Smeeth L, Chen PC. Data resource profile: The National Health Insurance Research Database (NHIRD). Epidemiol Health. 2018; 40: e2018062. DOI: 10.4178/epih.e2018062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chang CH, Lee YC, Tsai CT, et al. Continuation of statin therapy and a decreased risk of atrial fibrillation/flutter in patients with and without chronic kidney disease. Atherosclerosis. 2014; 232(1): 224–30. DOI: 10.1016/j.atherosclerosis.2013.11.036 [DOI] [PubMed] [Google Scholar]
- 15.Hsieh CY, Chen CH, Li CY, Lai ML. Validating the diagnosis of acute ischemic stroke in a National Health Insurance claims database. J Formos Me Assoc. 2015; 114(3): 254–9. DOI: 10.1016/j.jfma.2013.09.009 [DOI] [PubMed] [Google Scholar]
- 16.Siu CW, Jim MH, Zhang X, et al. Comparison of atrial fibrillation recurrence rates after successful electrical cardioversion in patients with hyperthyroidism-induced versus non-hyperthyroidism-induced persistent atrial fibrillation. Am J Cardiol. 2009; 103(4): 540–3. DOI: 10.1016/j.amjcard.2008.10.019 [DOI] [PubMed] [Google Scholar]
- 17.Nakazawa H, Lythall DA, Noh J, et al. Is there a place for the late cardioversion of atrial fibrillation? A long-term follow-up study of patients with post-thyrotoxic atrial fibrillation. Eur Heart J. 2000; 21(4): 327–33. DOI: 10.1053/euhj.1999.1956 [DOI] [PubMed] [Google Scholar]
- 18.Chen YC, Chen SA, Chen YJ, Chang MS, Chan P, Lin CI. Effects of thyroid hormone on the arrhythmogenic activity of pulmonary vein cardiomyocytes. J Am Col Cardiol. 2002; 39(2): 366–72. DOI: 10.1016/S0735-1097(01)01731-4 [DOI] [PubMed] [Google Scholar]
- 19.Boriani G, Glotzer TV, Santini M, et al. Device-detected atrial fibrillation and risk for stroke: An analysis of > 10,000 patients from the SOS AF project (Stroke preventiOn Strategies based on Atrial Fibrillation information from implanted devices). Eur Heart J. 2014; 35(8): 508–16. DOI: 10.1093/eurheartj/eht491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walkey AJ, Hammill BG, Curtis LH, Benjamin EJ. Long-term outcomes following development of new-onset atrial fibrillation during sepsis. Chest. 2014; 146(5): 1187–95. DOI: 10.1378/chest.14-0003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bruere H, Fauchier L, Bernard Brunet A, et al. History of thyroid disorders in relation to clinical outcomes in atrial fibrillation. Am J Med. 2015; 128(1): 30–7. DOI: 10.1016/j.amjmed.2014.07.014 [DOI] [PubMed] [Google Scholar]
- 22.Chan PH, Hai J, Yeung CY, et al. Benefit of anticoagulation therapy in hyperthyroidism-related atrial fibrillation. Clinical cardiology. 2015; 38(8): 476–82. DOI: 10.1002/clc.22427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang MT, Lee WJ, Huang TY, Chu CL, Hsieh CH. Antithyroid drug-related hepatotoxicity in hyperthyroidism patients: A population-based cohort study. Br J Clin Pharmacol. 2014; 78(3): 619–29. DOI: 10.1111/bcp.12336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Akmal A, Kung J. Propylthiouracil, and methimazole, and carbimazole-related hepatotoxicity. Expert Opin Drug Saf. 2014; 13(10): 1397–406. DOI: 10.1517/14740338.2014.953796 [DOI] [PubMed] [Google Scholar]
- 25.Gamra H, Murin J, Chiang CE, et al. Use of antithrombotics in atrial fibrillation in Africa, Europe, Asia and South America: Insights from the International RealiseAF Survey. Arch Cardiovasc Dises. 2014; 107(2): 77–87. DOI: 10.1016/j.acvd.2014.01.001 [DOI] [PubMed] [Google Scholar]
- 26.Hsieh FI, Lien LM, Chen ST, et al. Get With the Guidelines-Stroke performance indicators: Surveillance of stroke care in the Taiwan Stroke Registry: Get With the Guidelines-Stroke in Taiwan. Circulation. 2010; 122(11): 1116–23. DOI: 10.1161/CIRCULATIONAHA.110.936526 [DOI] [PubMed] [Google Scholar]
- 27.Eckman MH, Singer DE, Rosand J, Greenberg SM. Moving the tipping point: The decision to anticoagulate patients with atrial fibrillation. Circ Cardiovasc Qual Outcomes. 2011; 4(1): 14–21. DOI: 10.1161/CIRCOUTCOMES.110.958108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hohnloser SH, Pajitnev D, Pogue J, et al. Incidence of stroke in paroxysmal versus sustained atrial fibrillation in patients taking oral anticoagulation or combined antiplatelet therapy: an ACTIVE W Substudy. J Am Col Cardiol. 2007; 50(21): 2156–61. DOI: 10.1016/j.jacc.2007.07.076 [DOI] [PubMed] [Google Scholar]
- 29.Wong CL, Tam HV, Fok CV, Lam PE, Fung LM. Thyrotoxic atrial fibrillation: Factors associated with persistence and risk of ischemic stroke. J Thyroid Res. 2017; 2017: 4259183. DOI: 10.1155/2017/4259183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Baumgartner C, da Costa BR, Collet TH, et al. Thyroid Function Within the Normal Range, Subclinical Hypothyroidism, and the Risk of Atrial Fibrillation. Circulation. 2017; 136(22): 2100–16. DOI: 10.1161/CIRCULATIONAHA.117.028753 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1 & S2 and Figures S1 & S2.


