Abstract
Patient: Female, 59-year-old
Final Diagnosis: Deep vein thrombosis • pulmonary embolism • thrombosis
Symptoms: Chest pain • shortness of breath
Medication: —
Clinical Procedure: —
Specialty: Hematology • Infectious Diseases • General and Internal Medicine
Objective:
Unusual clinical course
Background:
The COVID-19 pandemic is an ongoing cause of the current global healthcare crisis. Several vaccines were approved for use by emergency vaccination campaigns worldwide. At present, there are very few reports of COVID-19 vaccine-induced immune-thrombotic thrombocytopenia, a variant of heparin-induced thrombocytopenia (HIT), in comparison to the massive number of vaccinated people worldwide.
Case Report:
A 59-year-old woman presented to the Emergency Department with a 3-day history of sudden-onset left leg pain 7 days after receiving her first dose of BNT162b2 mRNA COVID-19 (Pfizer-BioNTech). She was diagnosed with deep vein thrombosis (DVT) and pulmonary embolism (PE) and found to have a positive HIT screen with optical density (OD) of 0.6 via ELISA test. She was hospitalized for 4 days and discharged home with an oral anticoagulant (rivaroxaban).
Conclusions:
This case report describes a possible link between BNT162b2 mRNA COVID-19 (Pfizer-BioNTech) vaccination and thromboembolism. However, further data are needed to support such an association.
Keywords: COVID-19, COVID-19 vaccine, Pulmonary Embolism, Venous Thrombosis
Background
The COVID-19 pandemic continues to be a major healthcare crisis worldwide. Several vaccines have been developed and approved for use by the European Medicines Agency (EMA) and others by the U.S. Food and Drug Administration (FDA) through an Emergency Use Authorization (EUA) [1,2]. While vaccination programs are ongoing in most nations, multiple questions have been raised regarding their safety profiles. EMA reported 222 cases of newly developed thrombosis and thrombocytopenia shortly after vaccination with ChAdOx1 nCoV-19 (AstraZeneca); most of the reported cases were in females under the age of 55 years [3]. Among 54 million recipients of the Pfizer-BioNTech mRNA vaccine, 35 possible cases of central nervous system thrombosis were reported [4] and there was only 1 case of deep vein thrombosis (DVT) among 3010 vaccinated health workers in Italy [5]. Also, there have been a few reports of cerebral venous sinus thrombosis among more than 7 million recipients of the Johnson & Johnson/Janssen vaccine and 5 million recipients of the Moderna mRNA vaccine [4]. The proposed mechanism in vaccination with the ChAdOx1 nCoV-19 vaccine is named vaccine-induced immune-thrombotic thrombocytopenia (VITT), a variant of heparin-induced thrombocytopenia (HIT) [3]. We report extensive thromboembolism in a 59-year-old woman that occurred 7 days after receiving the first dose of the BNT162b2 Pfizer-BioNTech mRNA vaccine.
Case Report
A 59-year-old woman presented to the Emergency Department (ED) at Sultan Qaboos University Hospital (SQUH) with a 3-day history of sudden-onset left leg pain. There was no history of trauma, immobilization, surgical intervention, local injections, fever, weight loss, miscarriages, or skin rash. Her medical background included type 2 diabetes mellitus, osteoarthritis, and COVID-19 pneumonia in September 2020, which required hospitalization in the general ward for 1 week, with no residual complications. Her regular medications were metformin 1000 mg 2 times daily and ethinylestradiol 30 mcg+levonorgestrel 150 mcg, a combined oral contraceptive pill (OCP), with no interruption of therapy for the past 20 years. She received her first dose of BNT162b2 mRNA COVID-19 (Pfizer-BioNTech) 7 days before her current symptom’s onset and approximately 7 months after her diagnosis of COVID-19 pneumonia.
On physical examination she appeared alert and oriented. Her vitals were as follows: temperature 37.1ºC, blood pressure 161/99 mmHg, heart rate 106 bpm, respiratory rate 24 bpm, and oxygen saturation 98% on ambient air. The left leg was swollen and warm with calf tenderness. Chest auscultation revealed bilateral vesicular breath with no added sounds. Other systematic examinations were unremarkable. Laboratory findings are presented in Table 1. Results of a full blood count including platelets count, coagulation profile, and renal parameters were normal. However, D-dimer was markedly high at 24 mg/L FEU. Twelve-lead electrocardiography (ECG) showed sinus tachycardia with no significant ST-segment or T-wave changes. Troponin T and N-terminal pro-B-type natriuretic peptide (ProBNP) were 9 ng/L and 583 pg/mL, respectively. Duplex ultrasonography of the lower limbs showed acute DVT involving the common femoral, superficial femoral, popliteal, posterior tibial, anterior tibial, and deep calf veins of the left lower limb. Due to tachycardia, the patient underwent computed pulmonary tomography angiography (CTPA), which showed saddle thrombus in the bifurcation of the pulmonary trunk and 40 extensive bilateral main pulmonary arteries emboli extending to the lobar segmental and subsegmental branches (Figures 1–3).
Table 1.
Summary of laboratory tests results.
| Test | Result | Normal range |
|---|---|---|
| Hb (g/L) | 15 | 11–14.5 |
| Haematocrit (L/L) | 0.45 | 0.34–0.43 |
| Platelet count (109 /L) | 182 | 150–450 |
| White cell count (109 /L) | 6.1 | 2.4–9.5 |
| PT (sec) | 10.8 | 9.8–12 |
| APTT (sec) | 27.3 | 25–36.4 |
| Fibrinogen (g/l) | 6.1 | 1.7–3.6 |
| D-dimer (mg/L FEU) | 24 | 0.2–0.7 |
| CRP (mg/L) | 77 | 0–5 |
| Troponin T (ng/L) | 9 | <14 |
| ProBNP (pg/ml) | 583 | 20–285 |
| eGFR (ml/min/1.73 m2) | >90 | >90 |
| HIT (optical density) | 0.617 | <0.4 |
APTT – activated partial thromboplastin time; CRP – C reactive protein; Hb – haemoglobin; HIT – heparin induced thrombocytopenia; eGFR – estimated gomeurlar filtration rate; PT – prothrombin time; ProBNP – N-terminal pro B-type natriuretic peptide.
Figure 1.
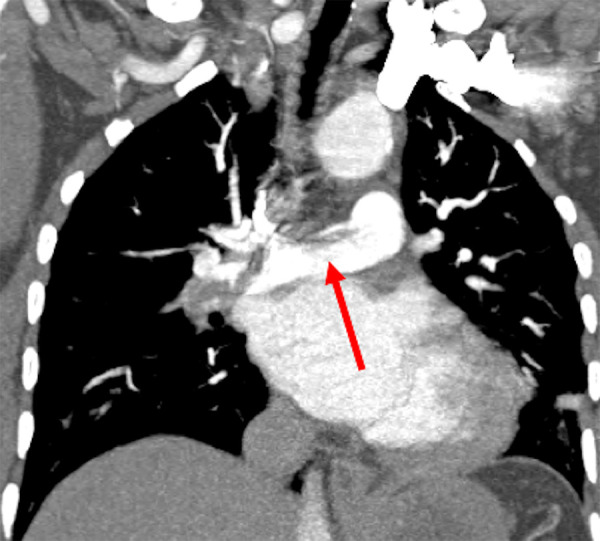
Coronal section CTPA demonstrating a linear branching filling defect in the pulmonary trunk bifurcation in keeping with saddle thrombus.
Figure 2.
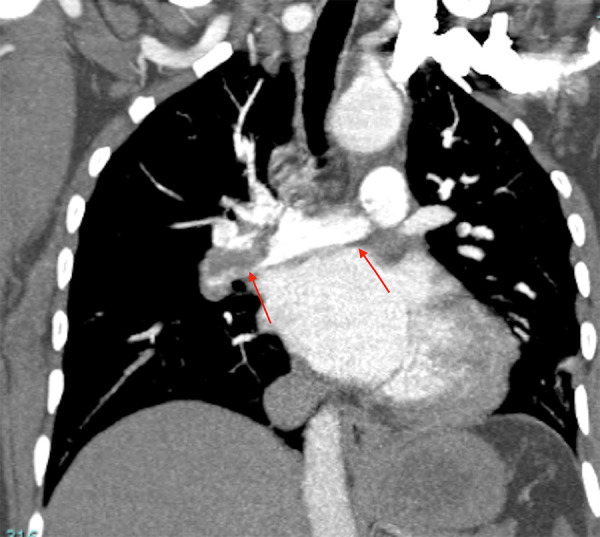
Coronal section CTPA illustrates extensive pulmonary emboli in the right main pulmonary artery and left main pulmonary artery.
Figure 3.

Coronal section CTPA shows extensive pulmonary emboli in segmental and subsegmental branches in both lower lobes.
The pulmonary embolism (PE) severity index was 59, with the absence of right ventricular (RV) strain, elevated ProBNP, and negative troponin. Therefore, she was managed initially with enoxaparin 1 mg/kg 2 times daily, and she remained hemo-dynamically stable after the initiation of anticoagulation, with a temperature of 37.0ºC, blood pressure 130/70 mmHg, heart rate 90 bpm, respiratory rate 19 bpm, and oxygen saturation 97% on ambient air. In view of the close time interval between the COVID-19 vaccine and the onset of her symptoms, a blood sample for HIT ELISA was collected on the 2nd day of admission and was reported positive on the 4th day (Table 1). Given the positive HIT test, enoxaparin was ceased, and the patient was started on rivaroxaban 15 mg twice daily for 21 days, followed by rivaroxaban 20 mg once daily for a total of 3 months, and she will be followed in the thrombosis clinic.
Discussion
BNT162b2 mRNA COVID-19 (Pfizer-BioNTech) is currently used for SARS-CoV-2 massive vaccination campaigns worldwide. A medium of 2 months safety profile in 43 252 participants was provided by the BNT162b2 mRNA COVID-19 vaccine trial, which showed safety profiles similar to those of other viral vaccines. Of note, only 4 reported adverse drug reactions (ADRs) were considered serious, and they included: ventricular arrhythmia, axillary lymphadenopathy, leg paresthesia, and shoulder injury. Other ADRs were mild to moderate local or systematic reactions [6]. Also, hypersensitivity-related ADRs were observed in 0.63% of vaccinated people, including few anaphylaxis reactions [2]. Recently, many cases of VITT have been reported, with incidence apparently between 1 in 125 000 and 1 in 1 million, with most of them attributed to the ChAdOx1 nCoV-19 Vaccine [7], and only 1 reported case of DVT was linked to the BNT162b2 mRNA COVID-19 vaccine [5].
VITT usually presents as new onset of thrombocytopenia and confirmed venous or arterial thrombosis within 4 to 16 days after receiving COVID-19 vaccination [8]. The typically shared laboratory findings were: platelet count less than 150×109 /L, raised D-dimer, and inappropriately low fibrinogen level. The proposed mechanism of VITT is linked to the presence of antibodies to platelet factor 4-polyanion complexes (PF4), which induce a massive platelet activation via the Fc receptor, similarly to the cases of heparin-induced thrombocytopenia (HIT) that are detected by HIT ELISA assay [8]. In our patient, HIT ELISA was positive with optical density (OD) of 0.6, and the patient had normal platelet counts, which is similar to some previously reported cases of HIT [9]. Unfortunately, the HIT functional assa y– Serotonin Release Assay (SRA) or Heparin-Induced Platelet Aggregation (HIPA) – is not available in Oman; therefore, it was not sent for confirmation.
Chronic sequelae of COVID-19 resulting in immune-thrombotic changes can cause a wide range of clinical manifestations, which have been linked with severe COVID-19 courses requiring hospitalization, and typically occurring 30 to 90 days after discharge [10,11]. Thus, for those 2 reasons, the likelihood of COVID-19-related VTE in our patient was low.
It is well known that estrogen-containing OCPs increase the risk of venous thromboembolism (VTE) by effacing hemostasis pathways. VTE association with OCP has been observed with higher doses of estrogen (> 50 mcg). Moreover, the risk is higher with early use, specifically in the first 6 to 12 months of initiation [12]. Our patient reported using a combined OCP for the past 20 years with no interruption, and she was on a small dose of estrogen in the form of ethinylestradiol 30 mcg only.
Clinical assessment of our patient was not suggestive of other autoimmune diseases or occult malignancy as a precipitating factor for VTE. In the absence of an obvious explanation for the extensive DVT and bilateral PEs, and the proximity of COVID-19 vaccination, we believe that our patient’s presentation is probably related to a rare ADR of BNT162b2 mRNA COVID-19 (Pfizer-BioNTech).
Conclusions
This case demonstrates a rare occurrence of extensive thromboembolism in 59-year-old woman, 7 days after receiving the Pfizer–BioNTech vaccine, with no other possible explanation for her VTE. At present, there are few reports of thrombosis among millions of COVID-19 vaccine recipients, supporting the association of COVID-19 vaccines and spontaneous HIT as a possible new rare vaccine-related ADR. However, further data are needed to support such an association.
Footnotes
Conflict of Interest
None.
Declaration of Figures Authenticity
All figures submitted have been created by the authors who confirm that the images are original with no duplication and have not been previously published in whole or in part.
References:
- 1.WHO Coronavirus (COVID-19) Dashboard [Internet] World Health Organization; 2021. [cited 5/4/2021]. https://covid19.who.int. [Google Scholar]
- 2.Banerji A, Wickner PG, Saff R, Stone CA, Jr, et al. mRNA Vaccines to prevent COVID-19 disease and reported allergic reactions: Current evidence and suggested approach. J Allergy Clin Immunol Pract. 2021;9(4):1423–37. doi: 10.1016/j.jaip.2020.12.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greinacher A, Thiele T, Warkentin TE, et al. Thrombotic thrombocytopenia after ChAdOx1 nCov-19 vaccination. N Engl J Med. 2021;384(22):2092–101. doi: 10.1056/NEJMoa2104840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cines DB, Bussel JB. SARS-CoV-2 vaccine-induced immune thrombotic thrombocytopenia. N Engl J Med. 2021 doi: 10.1056/NEJMe2106315. [Online ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carli G, Nichele I, Ruggeri M, et al. Deep vein thrombosis (DVT) occurring shortly after the second dose of mRNA SARS-CoV-2 vaccine. Intern Emerg Med. 2021;16(3):803–4. doi: 10.1007/s11739-021-02685-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Polack FP, Thomas SJ, Kitchin N, et al. Safety and efficacy of the BNT162b2 mRNA COVID-19 Vaccine. N Engl J Med. 2020;383(27):2603–15. doi: 10.1056/NEJMoa2034577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pai M, Grill A, Ivers N, et al. Vaccine induced prothrombotic thrombocytopenia VIPIT following AstraZeneca COVID-19 vaccination. Science Briefs of the Ontario COVID-19 Science Advisory Table. 2021;1:7. [Google Scholar]
- 8.Oldenburg J, Klamroth R, Langer F, et al. Diagnosis and management of vaccine-related thrombosis following AstraZeneca COVID-19 vaccination: Guidance statement from the GTH. Hamostaseologie. 2021 doi: 10.1055/a-1469-7481. [Online ahead of print] Erratum in: Hamostaseologie. 2021 May 12 ] [DOI] [PubMed] [Google Scholar]
- 9.Greinacher A, Selleng K, Warkentin TE. Autoimmune heparin-induced thrombocytopenia. J Thromb Haemost. 2017;15(11):2099–114. doi: 10.1111/jth.13813. [DOI] [PubMed] [Google Scholar]
- 10.Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–18. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Levi M, Thachil J, Iba T, Levy JH. Coagulation abnormalities and thrombosis in patients with COVID-19. Lancet Haematol. 2020;7(6):e438–e40. doi: 10.1016/S2352-3026(20)30145-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gialeraki A, Valsami S, Pittaras T, et al. Oral contraceptives and HRT risk of thrombosis. Clin Appl Thromb Hemost. 2018;24(2):217–25. doi: 10.1177/1076029616683802. [DOI] [PMC free article] [PubMed] [Google Scholar]


