Abstract
Patient: Female, 21-year-old
Final Diagnosis: Optic neuritis
Symptoms: Vision changes
Medication:—
Clinical Procedure: —
Specialty: Infectious Diseases • Neurology
Objective:
Rare co-existance of disease or pathology
Background:
Since the outbreak of the SARS-CoV-2 infection, extensive research has been conducted on the pulmonary implications of this novel disease. However, there has been limited data on the extrapulmonary manifestations. There have been few documented causes of optic involvement and little is understood about the pathophysiology around its presentation and the possible treatments to prevent long-term complications. Here, we describe a case of optic neuritis in a female patient concurrently infected with SARS-CoV-2. Given the plethora of evidence supporting neurological manifestations of the virus, we hypothesize that there is an association between our patient’s optic neuritis and her infection with SARS-CoV-2.
Case Report:
A 21-year-old woman with no past medical history who presented with blurry vision in her left eye. Optic neuritis was suspected with physical examination and confirmed with imaging of the optic nerve. Further diagnostic evaluation was nonsuggestive of multiple sclerosis and other demyelinating diseases; however, the patient was found to be positive for SARS-CoV-2. Steroids and remdesivir treatment were started, but without the presence of any respiratory symptoms. The patient’s symptoms completely resolved by day 5 of hospitalization and she was discharged home without any complications.
Conclusions:
Optic neuritis has remained an uncommon complication of SARS-CoV-2. This rather rare complication of SARS-CoV-2 is one that clinicians should be cognizant of due to the long-term implications of optic neuritis. Furthermore, it is pertinent to consider ophthalmic involvement in SARS-CoV-2 infection to appropriately guide patient care during the pandemic, as prompt treatment can lead to improved outcomes.
Keywords: Blindness, COVID-19, Optic Neuritis
Background
SARS-CoV-2 is an infectious disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that was first identified in Wuhan, China during an outbreak in the final months of 2019. Shortly after the outbreak in Wuhan, SARS-CoV-2 quickly began to spread worldwide. On March 11th, 2020, the World Health Organization (WHO) officially declared SARS-CoV-2 as a pandemic, which was the first to be declared since the Spanish Flu (H1N1) of 1918 [1–3]. Since then, the virus has spread to over 187 countries, with over 60 million cases identified and 1.5 million deaths [3]. Common clinical manifestations of SARS-CoV-2 include fever, nonproductive cough, dyspnea, and fatigue [3]. However, these symptoms have varied greatly amongst patients. Reports from around the world have shown that 81% of patients had mild pneumonia or none at all, yet 14% had severe respiratory distress and 5% had respiratory failure, septic shock, and/or multi-organ failure [4].
Although most experience pulmonary symptoms, recent evidence has suggested that the disease is not confined to the respiratory tract. Studies have shown associations between SARS-CoV-2 and anosmia, encephalitis, stroke, epileptic seizures, and optic neuritis [2,4,5]. Here, we describe a case of optic neuritis in a female patient concurrently infected with SARS-CoV-2. Given the plethora of evidence supporting neurological manifestations of the virus, we hypothesize that there is an association between our patient’s optic neuritis and her infection with SARS-CoV-2.
Case Report
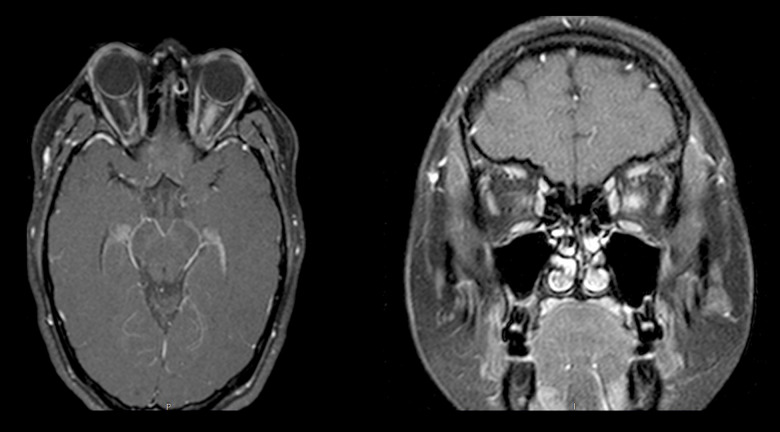
A 21-year-old woman with no past medical history presented with blurry vision in her left eye (Table 1). Prior to this presentation, she had a one-week history of severe headaches associated with pain with movements in all directions in her left eye as well as nausea and insomnia. She was seen 3 days prior in the Emergency Department with similar symptoms. A head CT scan without contrast at that time was normal. At the initial visit, she denied prior similar episodes and any other symptoms. SARS-CoV-2 PCR nasal swab was positive but the patient denied any respiratory symptoms. An MRI of the brain revealed non-enhancing T2/flair subcortical white-matter hyperintensi-ties, mainly in the frontal lobes, that may be associated with demyelinating disease (Figure 1). There was also abnormal T2 flair hyperdense signals in the left optic nerve reflecting acute optic neuritis, confirmed with an MRI of the left orbit (Figure 1). A SARS-CoV-2 nasal PT-PCR swab was positive. She also had IgG antibodies against SARS-CoV-2 and CSF studies were unremarkable with no oligoclonal bands or signs of infectious etiology present. Neuromyelitis-optica (NMO) antibodies and MOG antibody reflex titers, syphilis, and HIV tests were all negative. She was started on methylprednisolone and remdesivir. The patient’s vision returned to normal 5 days after initiation of treatment. She was discharged with oral steroids and with instructions to follow up in the neuro-ophthalmology clinic. One months after initial presentation, ophthalmologic evaluation showed no visual deficits and a fundoscopic examination was normal.
Table 1.
Ophthalmological examination done on day 1 of hospitalization.
| Right | Left | |
|---|---|---|
| Base Eye Exam | ||
| Visual Acuity (Snellen-Linear) | ||
| Dist sc | 20/20 | HM (hand motion) |
| Tonometry | ||
| Pressure | 21 | 23 |
| Slit Lamp and Fundus Exam | ||
| External Exam | ||
| External | Normal | Normal |
| Slit Lamp Exam | ||
| Lids/Lashes | Normal | Normal |
| Conjunctiva/Sclera | White and quiet | White and quiet |
| Cornea | Clear | Clear |
| Anterior Chamber | Deep and quiet | Deep and quiet |
| Iris | Round and reactive | Round, +APD |
| Lens | Clear | Clear |
| Vitreous | Normal | Normal |
| Fundus Exam | ||
| Disc | Mild temporal burring of optic disc with nasal sparing, no elevation | Disc elevation 360 with obscuration of vessels as they leave the disc |
| Macula | Normal | Normal |
| Vessels | Normal | Tortuous |
| Periphery | Normal | Normal |
Figure 1.
Axial and coronal views of brain on MRI, showing optic neuritis of the left optic nerve.
Discussion
SARS-CoV-2 has led to a variety of complications among those infected; however, optic neuritis is one of the rarest to be reported thus far. There have been cases in the literature but most patients have concurrent respiratory symptoms [6].
Neuro-ophthalmic involvement, which is more predominant in animal species (feline and mice models), has been associated with other forms of coronaviruses, with complications ranging from conjunctivitis to more severe forms such as optic neuritis or retinitis [7].
In humans, there have been documented cases of ocular manifestations of coronavirus infection extending far back to the SARS-CoV infection outbreak in 2003. In a small study done in 2004, tear samples from 36 suspected patients were sent for RT-PCR testing for SARS-CoV. Three samples tested positive for RNA; nevertheless, this demonstrated the possibility of transmission through ocular tissue and the need for protective eye equipment when in close contact with infected patients [8]. The mechanism of uptake into ocular tissue has not been well studied but one proposed theory is that the presence of angiotensin-converting-enzyme-2 (ACE-2) receptor on ocular tissues binds ACE-2 on the SARS-CoV-2, allowing the virus to infiltrate specific tissues in the body, resulting in a diverse range of complications [9].
The mechanism of ophthalmic complications secondary to SARS-CoV-2 infection is one that has been debated and is the subject of studies, especially in animal models. Human studies related to ophthalmic manifestations have been lacking but may be important as they may provide further information of mechanism of transmission. One theory that has been discussed is direct inflammation of the nerves, resulting in myelin damage. This phenomenon was demonstrated when mice were inoculated with MHV-A56; isolated optic nerve sheaths and parenchyma were found to be infiltrated with inflammatory cells [10]. Complete resolution of the optic neuritis was noted at day 15 of infection, similar to that observed in our patient. However, no treatment was given to the mice in the laboratory setting, whereas our patient received remdesivir and corticosteroids. Another theory that has been discussed is ischemia to specific nerves secondary to the hypercoagulable state, which has been observed in patients with SARS-CoV-2 infection. The hypoxic state created by microemboli, which is thought to be secondary to a combination of endothelial inflammation and increased thrombin generation, may result in ischemic optic neuropathy. In one small study, magnetic resonance spectroscopy showed white-matter changes similar to those seen in oxygen deprivation [11]. It remains inconclusive if the changes seen were secondary to hypoxia or direct viral attack on brain tissue; however, these findings support the possibility of central nervous system dysfunction secondary to SARS-CoV-2 infection.
Intravenous (methylprednisolone 1 g/day for 3 days) followed by oral steroids (prednisone 1 mg/kg/day for 11 days remain the choice of treatment for optic neuritis of this etiology [12]. Most case reports showed full resolution of symptoms within 2 to 3 weeks after initiation of steroids [12].
Conclusions
In the absence of demyelinating disease and other causes of optic neuritis being unlikely, the patient’s presentation and improvement after treatment with steroid and remdesivir may indicate a causal relationship with SARS-CoV-2. This rather rare complication of SARS-CoV-2 is one that clinicians should be cognizant of due to the long-term implications of optic neuritis. The rapid spread of SARS-COV-2 has created a global burden that has altered the norms of socializing, working, and traveling. This drastic change in our activities of daily living warrants in-depth research on the virus. More data on the subject may result in earlier interventions, which may lead to better outcomes, as seen in our patient. Overall, this further emphasizes that SARS-CoV-2 infection causes a systemic disease rather than an isolated pulmonary pathology.
Footnotes
Conflict of Interest
None.
References:
- 1.Centers for Disease Control and Prevention. Centers for Disease Control and Prevention; 2019. 1918 Pandemic (H1N1 virus) [Internet] [cited 2020Dec10]. https://www.cdc.gov/flu/pandemic-resources/1918-pandemic-h1n1.html. [Google Scholar]
- 2.Zhou S, Jones-Lopez EC, Soneji DJ, et al. Myelin oligodendrocyte glyco-protein antibody-associated optic neuritis and myelitis in COVID-19. J Neuroophthalmol. 2020;40(3):398–402. doi: 10.1097/WNO.0000000000001049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chauhan S. Comprehensive review of coronavirus disease 2019 (COVID-19) Biomed J. 2020;43(4):334–40. doi: 10.1016/j.bj.2020.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khatoon F, Prasad K, Kumar V. Neurological manifestations of COVID-19: available evidences and a new paradigm. J Neurovirol. 2020;26(5):619–30. doi: 10.1007/s13365-020-00895-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pezzini A, Padovani A. Lifting the mask on neurological manifestations of COVID-19. Nat Rev Neurol. 2020;16(11):636–44. doi: 10.1038/s41582-020-0398-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.François J, Collery AS, Hayek G, et al. Coronavirus sisease 2019-associated ocular neuropathy with panuveitis: A case report. JAMA Ophthalmol. 2021;139(2):247–49. doi: 10.1001/jamaophthalmol.2020.5695. [DOI] [PubMed] [Google Scholar]
- 7.Seah I, Agrawal R. Can the coronavirus disease 2019 (COVID-19) affect the eyes? A review of coronaviruses and ocular implications in humans and animals. Ocul Immunol Inflamm. 2020;28(3):391–95. doi: 10.1080/09273948.2020.1738501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Loon SC, Teoh SC, Oon LL, et al. The severe acute respiratory syndrome coronavirus in tears. Br J Ophthalmol. 2004;88(7):861–63. doi: 10.1136/bjo.2003.035931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhang H, Penninger JM, Li Y, Zhong N, Slutsky AS. Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med. 2020;46(4):586–90. doi: 10.1007/s00134-020-05985-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shindler KS, Kenyon LC, Dutt M, et al. Experimental optic neuritis induced by a demyelinating strain of mouse hepatitis virus. J Virol. 2008;82(17):8882–86. doi: 10.1128/JVI.00920-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Catharino AMS, Neves MAO, Nunes NSM, et al. COVID-19 related optic neuritis: Case report. J Clin Neurol Neurosci. 2020;1:10. [Google Scholar]
- 12.Sawalha K, Adeodokun S, Kamoga GR. COVID-19-induced acute bilateral optic neuritis. J Investig Med High Impact Case Rep. 2020;8:2324709620976018. doi: 10.1177/2324709620976018. [DOI] [PMC free article] [PubMed] [Google Scholar]