Abstract
The da Vinci® single-port (SP) and multiport (Xi) approaches to robotic-assisted radical prostatectomy (RARP) are described by different authors in the literature, primarily comparing short-term outcomes of both modalities. To our knowledge, this is the first article comparing the surgical perspective and satisfaction of patients who underwent RARP with the SP and Xi platforms. To determine the patient surgical perspective and satisfaction in terms of pain control, return to normal activity, and overall results of surgery for two groups who underwent SP and Xi radical prostatectomy. The data from 71 consecutive patients who underwent SP RARP in a single center from June 2019 to April 2020 was compared to 875 patients who underwent Xi RARP in the same period. A single surgeon performed all procedures with a transperitoneal technique. After a propensity score match, two groups of 71 patients (SP and Xi) were selected and compared in the study. Patients were contacted by phone by two interviewers and a questionnaire was administered in English or Spanish. Patients were instructed not to disclose the type of robotic surgery they underwent, as interviewers were blinded to that information. A validated Surgical Satisfaction Questionnaire (SSQ-8) was used, along with an additional question from our institution asking about the satisfaction with the number of incision sites (GRI-1). Data were analyzed as continuous and discrete variables to compare the differences between the Xi and SP cohorts. A response rate of 85.9% (n = 61) in the Xi group and 73.2% (n = 52) in the SP group was captured. Overall satisfaction with surgical results was 80% and 88% in the Xi and SP cohorts, respectively. No statistical difference in responses was found between the Xi and SP cohorts for SSQ-8. However, GRI-1 demonstrated a statistically significant difference (P < 0.001) in terms of number of scars that favors the SP approach. Limitations of this study are the small sample size and recall bias. We found no statistical difference between the groups regarding the answers for SSQ-8 questionnaire; both groups were very satisfied. When assessing the number of incision sites with the GRI-1 question, patients who underwent MP had lower satisfaction rates compared to SP. These patients perceived the number of scars and their appearance as reason for lower satisfaction. We believe that future studies should consider patient’s postoperative perspective when adopting new platforms in order to combine adequate treatment with patient expectations. We performed a study assessing the postoperative satisfaction and perspectives of two groups of patients who underwent radical prostatectomy with two different robots (SP and Xi). There was no difference in patient satisfaction with the results of either the da Vinci® SP or Xi RARP except for the patients’ perception on their number of scars, which favored the SP group.
Keywords: Prostatectomy, Patient satisfaction, Robotic-assisted surgery, Surveys and questionnaires, Prostatic neoplasms
Introduction
Robotic-assisted radical prostatectomy (RARP) has become the gold standard surgical treatment for localized prostate cancer in the USA, owing to its decreased complications and early rehabilitation compared to the open approach [1]. Currently, the multiport da Vinci® Xi and Si (Intuitive Surgical, Sunnyvale, CA, USA) are the most commonly used platforms for RARP worldwide [2]. Continued advances in minimally invasive surgery (MIS) have led to the introduction of a potentially less invasive platform known as the da Vinci® single port (SP), which was granted FDA approval in November 2018 for urologic procedures [3, 4].
Comparison between these two robotic approaches (SP vs. multiport) on their intraoperative performances, early functional and oncological outcomes has been published [5]. These studies have found SP RALP to be technically feasible and safe with similar perioperative outcomes compared to the Xi, but the instrument limitations and increased cost of this novel technology must be considered [6]. Some groups have described decreased postoperative pain with increased opportunities for outpatient procedures, while other authors have reported no difference between the SP and multiport postoperative pain [5, 7]. Future reports of long-term outcomes with higher volume of patients will give additional insight regarding the best applications of the SP platform.
In this study, we compared the patient satisfaction describing their perspective on the quality of life following RARP using the SP and Xi robotic platforms. As the debate on these modalities would be incomplete without the patient experience, this study aims to assess, with postoperative questionnaire distribution, the patient surgical satisfaction in terms of pain control, ability to return to the daily activity (work or socially), and their surgical experience.
Methods
Study design and primary endpoint
We performed a retrospective study comparing the operative satisfaction and perspectives of two groups of patients who underwent RARP with the Xi and SP robot platforms. After a propensity score match (PS), the groups were compared, and the operative outcomes were described previously by our group [5]. In this study, the same patients were interviewed with a questionnaire regarding their postoperative experience in our center. The data was collected according to the Institutional Review Board (approval number 237998-44).
Propensity score matching
The covariates included in the PS were patient demographics (age, body mass index (BMI), Charlson comorbidity index), preoperative Sexual Health Inventory for Men (SHIM) and American Urological Association symptom scores (AUASS), prostate size, prostate specific antigen (PSA), D’Amico risk group, and degree of nerve sparing. The data of 71 consecutive SP patients were matched with 875 Xi patients who underwent surgery during the same period (from June 2019 to March 2020). PS analysis used the nearest-neighbor algorithm with a 1:1 ratio without replacement [8]. Covariates with a standardized difference (SDD) of <|0.15| were considered balanced. Finally, two groups of 71 patients were selected for the study.
Surgical Satisfaction Questionnaire (SSQ-8)
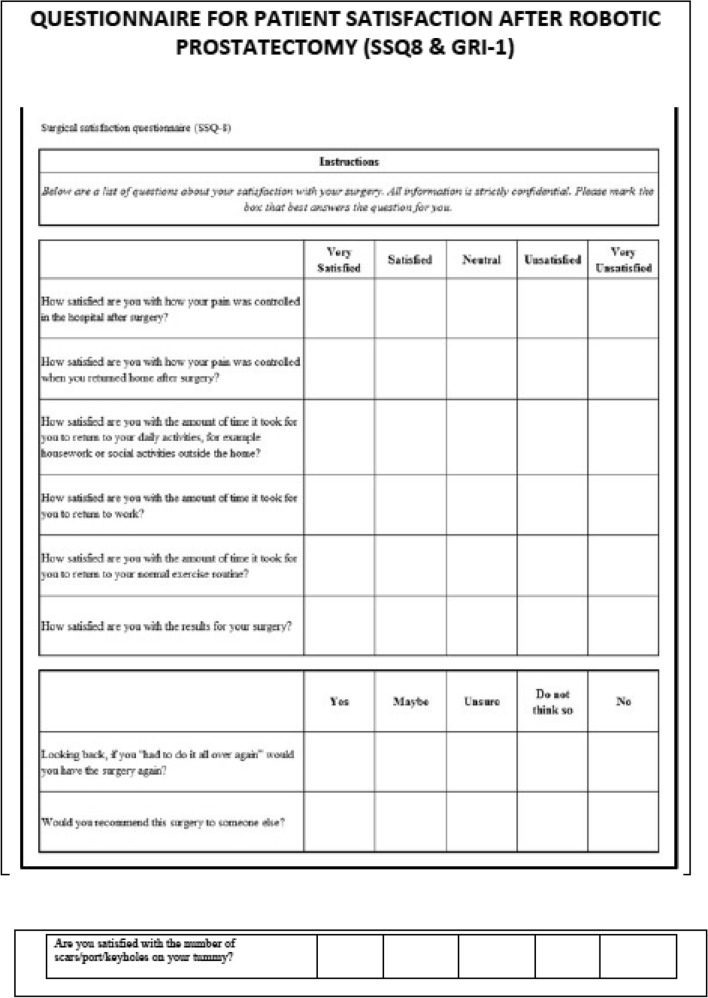
The SSQ-8 is a validated eight-item questionnaire that has been used previously to measure satisfaction in urogynecologic surgery. The advantage of this questionary is that it is not condition nor surgery-specific. This questionnaire has a test–retest reliability of 0.80 (P ≤ 0.2) [9]. Responses are recorded on a 5-point Likert scale from 1 = “very unsatisfied” to 5 = “very satisfied” for the first six questions or from 1 = “never” to 5 = “yes” for the last two questions. A higher degree of surgical satisfaction correlates with a higher score. Questions 1 and 2 address the pain subscale; questions 3, 4, and 5 address return to baseline subscale; and questions 6, 7, and 8 address global satisfaction subscale (see Appendix, Fig. 2).
Fig. 2.
SSQ-8 & GRI-1 Questionnaire
In addition to the eight questions in the SSQ-8, a non-validated question from our institution was added, named (GRI-1). Responses to GRI-1 are reported on a similar 5-point Likert scale to SSQ; all questions are available in Appendix (Fig. 2).
GRI-1: “How satisfied or unsatisfied are you with the number of skin incisions/scars following surgery?”.
Questionnaire distribution
In January 2021, two authors (JN and MM) administered the questionnaire survey over the telephone rather than in person or mail due to the ongoing SARS-CoV-2 (Covid-19) pandemic. A total of 142 patients (71 SP and 71 Xi) were selected as described in “Propensity score matching”. All 142 patients were randomized via computer algorithm, interviewers only had access to the patient’s name and phone number to ensure the interviewers were blinded to which robotic procedure the patient had (SP or Xi). Patients were asked at the beginning of the interview not to disclose which robotic platform they had during their surgery.
The interviewers confirmed the patient identity and obtained verbal consent for the survey. Patients were made aware at the beginning that participation was completely voluntary. The questionnaire was verbally distributed in English and Spanish, as all patients were English and/or Spanish speakers. All patients were contacted a maximum of three times.
All data collected from survey responses received by the interviewers were documented and sent to an unblinded author who identified which robotic approach (SP or Xi group) each patient underwent after data collection. Data was analyzed between the two groups after completion of all interviews.
Surgical technique
Patients having RARP with the multiport da Vinci® Xi platform underwent a standard six-port transperitoneal approach with an early retrograde athermal nerve-sparing technique [10]. A similar transperitoneal technique was performed with the da Vinci® SP, while using an additional assistant port as previously described [11]. Postoperative pelvic drains are not placed with either robotic platform.
Postoperative care and follow-up
An Enhanced Recovery After Surgery (ERAS) pathway with multimodal pain management and transversus abdominis plane (TAP) anesthetic block is utilized [12]. Pain is controlled using non-opiate analgesia and the Foley catheter is removed in 5 days.
After the Foley removal, all patients have the first appointments at 6 weeks, and then every 3 months after surgery for the first year. At these appointments, oncologic and functional outcomes are addressed with biochemical recurrence defined as PSA > 0.2 ng/mL in 2 consecutive exams and redistributing SHIM and AUASS questionnaires. We define continence as the use of no pads and potency as the ability to achieve and maintain erections adequate for sexual intercourse (with or without use of phosphodiesterase type-5 inhibitors) [6].
Statistical analysis
Statistical analysis and described data were performed and presented based on established guidelines [13]. Continuous variables are presented as mean ± standard deviation (SD) or median and interquartile range (IQR) while categorical and ordinal variables are described as frequencies and proportions.
Exploratory analysis using the Shapiro–Wilk test of normality found that none of the variables for either surgical modality was normally distributed. Additional review of quantiles supported this, and all questions demonstrated right hand skew. To determine variance, the F test was used and found that the true ratio of variances for all survey questions between the two cohorts was not equal to 1. Two-sided Mann–Whitney U tests were performed for the eight validated SSQ-8 questions and for our institution’s question (GRI-1) as continuous variables, to compare the difference between the Xi and SP cohorts. These items are discrete and considered as categorical variables as well, therefore, a Fisher’s exact was used by combining questionnaire responses 1–3 (‘very unsatisfied’, ‘unsatisfied’, ‘neutral’) due to the small sample size in these responses.
A sample size of 94 patients (47 in each cohort) is needed to detect a 20% difference (i.e., answering a ‘5’ vs a ‘4’) in answer response between the two groups, with a two-sided significance of 5% and 80% power. A two-tailed test with P < 0.05 was considered statistically significant. Statistical analysis was performed using R version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria) and Stata version 16 (Stata Corp., College Station, TX, USA).
Results
Patient demographics
A total of 142 patients (71 SP and 71 Xi) were included to answer the questionnaires proposed in this study. The preoperative demographics after the 1:1 PS are illustrated in Table 1.
Table 1.
Comparison of preoperative parameters of SP and Xi group after 1:1 PS matching
| Parameter | SP group (n = 71) | Xi group (n = 71) | P value | SDD |
|---|---|---|---|---|
| Median age, years (IQR) | 64 (57–69) | 64 (57–67) | 0.6 | 0.05 |
| Median PSA ng/ml (IQR) | 5.5 (4.3–7.8) | 5.3 (4.3–6.8) | 0.8 | 0.15 |
| Median BMI kg/m2 (IQR) | 25.3 (23.2–27.3) | 25.2 (24.1–26.7) | 0.4 | − 0.19 |
| Median preoperative SHIM score (IQR) | 20 (15–25) | 21 (16–24) | 0.8 | − 0.08 |
| Median preoperative AUASS (IQR) | 7 (3–12) | 7 (3–12) | 0.7 | − 0.05 |
| Biopsy ISUP grade group, n (%) | ||||
| Grade group 1 | 20 (28) | 19 (27) | 0.03 | |
| Grade group 2 | 35 (49) | 36 (51) | − 0.03 | |
| Grade group 3 | 13 (18) | 13 (18) | 0 | |
| Grade group 4 | 3 (4.2) | 2 (2.8) | 0.08 | |
| Grade group 5 | 0 (0) | 1 (1.4) | − 0.17 |
BMI body mass index, SHIM Sexual Health Inventory for Men, AUASS American Urological Association Symptom Score, ISUP International Society of Urological Pathology
Questionnaire administration
Median postoperative time to administer the questionnaire was 12 months (range 8–19 months). Each patient was called a maximum of three times if initial attempts were unsuccessful, and the average interview time was 4 min. In the Xi group, 61 patients completed the entire interview, a response rate of 85.9%. In the SP group, 52 patients completed the questionnaire, a response rate of 73.2%.
Patient satisfaction and perspectives
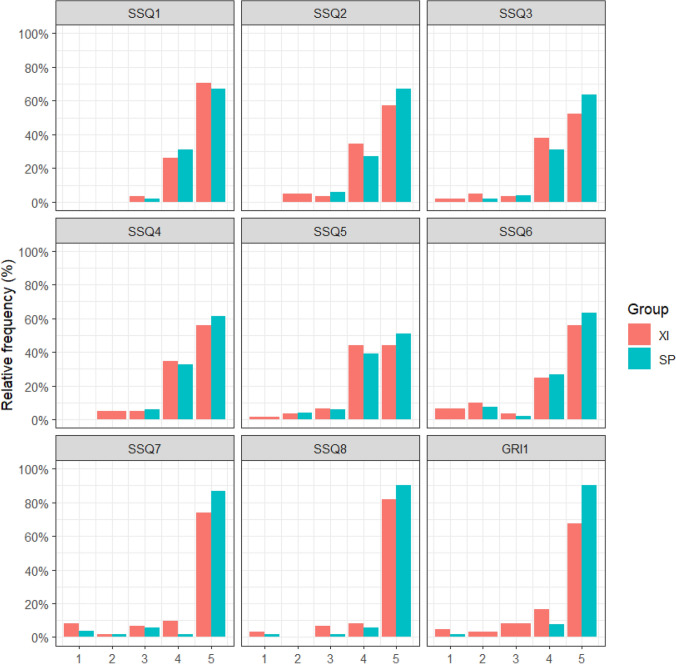
Distribution of patient responses on the SSQ-8 is illustrated in Fig. 1. On the SSQ-8, questions 1–2 address pain, 97% of Xi patients and 98% of SP patients were ‘very satisfied’ or ‘satisfied’ with their pain control following surgery in hospital and 91% and 94% of Xi and SP patients were ‘very satisfied’ or ‘satisfied’ once discharged, respectively. Questions 3–5, evaluating quality-of-life following surgery, showed 90% of Xi patients and 94% of SP patients being either ‘very satisfied’ or ‘satisfied’ with the time it took to return to their daily activities, work, and exercise. Overall satisfaction with the results of the surgery was 80% and 88% in the Xi and SP cohorts, respectively. When asked if the patient would recommend the surgery to a friend, 90% and 96% of Xi and SP, respectively, responded ‘yes’ or ‘maybe’. No statistical difference in responses was found between the Xi and SP cohorts for the eight SSQ-8 questions (Table 2).
Fig. 1.
Patient questionnaire response (percentage of answered questions x scores from 1 to 5)
Table 2.
Patient satisfaction comparison
| Parameter | MP | SP | P value |
|---|---|---|---|
| Response rate, N (%) | 61/71 (86) | 52/71 (73) | |
| Median SSQ1 (IQR)a | 5 (4–5) | 5 (4–5) | 0.76 |
| Median SSQ2 (IQR)a | 5 (4–5) | 5 (4–5) | 0.27 |
| Median SSQ3 (IQR)a | 5 (4–5) | 5 (4–5) | 0.21 |
| Median SSQ4 (IQR)a | 4 (4–5) | 5 (4–5) | 0.45 |
| Median SSQ5 (IQR)a | 5 (4–5) | 4.5 (4–5) | 0.53 |
| Median SSQ6 (IQR)a | 5 (4–5) | 5 (4–5) | 0.25 |
| Median SSQ7 (IQR)a | 5 (4–5) | 5 (5–5) | 0.11 |
| Median SSQ8 (IQR)a | 5 (5–5) | 5 (5–5) | 0.20 |
| Median SSQ total score (IQR)b | 38 (32–40) | 38 (34–40) | 0.24 |
| Median GRI-1 (IQE)a | 5 (4–5) | 5 (5–5) | < 0.001 |
aScore ranges: 1–5
bScore ranges: 8–40
Question GRI-1 revealed 84% of patients in the Xi cohort and 98% in the SP cohort were either ‘very satisfied’ or ‘satisfied’ with the number of incisions or scars after surgery, which demonstrated a statistically significant difference (P < 0.001) (Table 2).
Discussion
We report a study of surgical satisfaction among patients undergoing RARP with either the da Vinci® SP or da Vinci® Xi robotic platforms. To our knowledge, this is the first study addressing patient satisfaction among these two contemporary robotic surgical modalities.
The multiport approach to RARP has traditionally utilized 5–6 port insertions, while the SP RARP has one or two incisions (SP plus one). The less invasive access provided by the SP robot has raised different questions regarding pain scores and cosmetic results compared to the multiport surgery. Our experience using the SP was previously described in different articles and it is similar in terms of postoperative pain scores compared to the Xiv. Minimizing invasiveness theoretically should positively impact patient’s functional status and quality of life, yet a study that addresses these outcomes, seen with the patient perspective, is not yet available [14].
The SSQ-8 is a validated questionnaire that has been utilized within urogynecology, [10, 15, 16] and otolaryngology [17] studies, among others. The advantage of using this questionnaire is that it is not condition nor surgery-specific. Therefore, it can be adapted to another types of surgeries and specialties, such as robotic surgery. In the field of urogynecology, this questionnaire was employed to gauge patient satisfaction on differing stress urinary incontinence corrective surgeries. Urinary incontinence of all types (urge, stress or mixed) in men and women results in poor health-related quality of life [18]. Thus, patient satisfaction after surgeries known to cause incontinence, particularly prostatectomy, needs to be assessed. Within the scope of urologic oncology research, the SSQ-8 was used as a secondary outcome measure in a trial evaluating outpatient RARP in patients with localized prostate cancer (AMBUPRO ClinicalTrials.gov identifier: NCT04319146).
Since the da Vinci® multiport robot was approved by the US Food and Drug Administration (FDA), it has afforded laparoscopic surgeons with enhanced visualization, increased dexterity, tremor reduction, and an ergonomic advantage. Simultaneous to the evolution of robotic surgery, the laparoscopic single-site surgery (LESS) approach was described, through one incision rather than multiple ports [19]. However, LESS has a steep learning curve and was historically used in renal/upper urinary tract surgery as opposed to pelvic surgery [20]. Pioneers of minimal invasive prostatectomy, Menon and Vallancien, published their experience of developing a robotic program safely even when laparoscopic experience was limited [21]. A Cochrane systematic review found robotic surgery has led to decreased postoperative hospital stay compared to open surgery [22]. Additionally, RARP advantages include reduced operative time, blood loss, and perioperative morbidity [23]. These advantages have allowed for direct adoption of robotic surgery among open surgeons with two decades of multiport prostatectomy pushing the robotic commercial industry to further optimization.
Moreover, previous studies have found a positive relationship between patient satisfaction and their pain control, recovery to physical activity, and reduction of functional limitations. In our study, satisfaction with pain control was similar between the two cohorts. Both groups of patients returned to their normal activities after surgery without differences between robotic platform used. It is understood that treatment satisfaction is complex and derived from quality-of-life experience and functional changes [24]. Generally, despite the robotic approach, our patients were highly satisfied with the overall results of their surgery.
Previous studies evaluating regret after RARP found correlation of dissatisfaction with outcomes such as urinary and sexual deterioration [25] and interestingly, Sanda et al. [26] found that changes in quality of life (QoL) were also related to overall satisfaction among patients and their partners. While our early outcomes did not demonstrate a difference in continence and potency, these variables were not assessed by our questionnaire, because we need long-term follow-up as our data mature.
Our intention with a non-validated institution question GRI-1: “How satisfied or unsatisfied are you with the number of incision/port/keyholes after surgery?” was to assess the patient’s point of view raised by the robotic surgery community (Does the number of incisions really matter for the patient?) Future studies will aim to further validate this question as it relates to SP platforms. The responses to this question were the only answers found to have a significant difference, and we have found that patients undergoing Xi RARP had lower satisfaction rates from GRI-1. Due to the invaluable nature of the patient perspective, a selection of unsolicited comments were grouped according to Xi or SP (see Appendix, Table 3). On review of these comments to understand GRI-1 discrepancy; it appears patients in XI group thought they had too many scars, or that some were too painful. It is important to note that cosmetic concerns affect patients differently, and once SP is proven to be equivalent, then counselling the patient on the options will be paramount [27]. Despite this difference, it can be presumed the invasiveness of both procedures is similar from our results of the SSQ-8.
Table 3.
Patient's Comments
| SP cohort comments | Xi cohort comments |
|---|---|
| Skin incisions are not even noticeable so very happy | I was amazed this surgery didn’t slow me down at all, I mean less incisions would've been better |
| Very happy with scars, hardly can see them | The six incisions really hurt |
| Couldn’t be better, only had two incisions, no pain after surgery, no pain when I went home | I don’t even know how many incisions I even had |
| I wish I had fewer incisions and it is an improvement on the old way | I don’t think the number of incisions really matters |
During the study, the interviewers received the dataset with the robotic modality omitted and patients sorted by name. Interviews were conducted in English and Spanish, without the need for translation to another language. It is appreciated that a telephone administered questionnaire may have shortcomings compared to face to face; a study assessed this difference in children and showed little difference and even advantageous with the lack of visual distortions or tension/tension release signs between interviewee and interviewer [28]. Our limitations are the study was retrospective and interviewing patients’ months after surgery introduces recall bias. However, to our knowledge, this is the first study comparing the surgical perspective and satisfaction of patients who underwent RARP with two different robotic platforms.
Conclusion
We found no statistical difference between the groups regarding the answers for SSQ-8 questionnaire; both groups were very satisfied. However, when assessing the number of incision sites with the GRI-1 question, patients who underwent Xi described lower satisfaction rates which we hypothesis is due to number of scars. We believe that future studies should consider the patient postoperative perspective when adopting new platforms in order to combine adequate treatment with patient expectations.
Appendix 1
See Fig. 2.
Appendix 2
See Table 3.
Declarations
Conflict of interest
Author Jonathan Noël, author Marcio Covas Moschovas, author Marco Sandri, author Seetharam Bhat, author Travis Rogers, author Sunil Reddy, author Cathy Corder and author Vipul Patel declare that they have no conflict of interest.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kowalczyk KJ, Levy JM, Caplan CF, et al. Temporal national trends of minimally invasive and retropubic radical prostatectomy outcomes from 2003 to 2007: results from the 100% Medicare sample. Eur Urol. 2012;61:803–809. doi: 10.1016/j.eururo.2011.12.020. [DOI] [PubMed] [Google Scholar]
- 2.Mazzone E, Mistretta FA, Knipper S, et al. Contemporary national assessment of robot-assisted surgery rates and total hospital charges for major surgical uro-oncological procedures in the United States. J Endourol. 2019;33(6):438–447. doi: 10.1089/end.2018.0840. [DOI] [PubMed] [Google Scholar]
- 3.Moschovas MC, Bhat S, Rogers T, Thiel D, Onol F, Roof S, Sighinolfi MC, Rocco B, Patel V. Applications of the da Vinci single port (SP) robotic platform in urology: a systematic literature review. Minerva Urol Nefrol. 2020 doi: 10.23736/S0393-2249.20.03899-0. [DOI] [PubMed] [Google Scholar]
- 4.Moschovas MC, Seetharam Bhat KR, Onol FF, Rogers T, Ogaya-Pinies G, Roof S, Patel VR. Single-port technique evolution and current practice in urologic procedures. Asian J Urol. 2021;8(1):100–104. doi: 10.1016/j.ajur.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moschovas MC, Bhat S, Sandri M, et al. Comparing the approach to radical prostatectomy using the multiport da Vinci xi and da vinci sp robots: a propensity score analysis of perioperative outcomes. Eur Urol. 2021;79(3):393–404. doi: 10.1016/j.eururo.2020.11.042. [DOI] [PubMed] [Google Scholar]
- 6.Saidian A, Fang AM, Hakim O, Magi-Galluzzi C, Nix JW, Rais-Bahrami S. Perioperative outcomes of single vs multi-port robotic assisted radical prostatectomy: a single institutional experience. J Urol. 2020;204(3):490–495. doi: 10.1097/ju.0000000000000811. [DOI] [PubMed] [Google Scholar]
- 7.Lenfant L, Sawczyn G, Aminsharifi A, et al. Pure single-site robot-assisted radical prostatectomy using single-port versus multiport robotic radical prostatectomy: a single-institution comparative study. Eur Urol Focus. 2020 doi: 10.1016/j.euf.2020.10.006. [DOI] [PubMed] [Google Scholar]
- 8.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–3107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haff RE, Stoltzfus J, Lucente VR, Murphy M. The surgical satisfaction questionnaire (SSQ-8): a validated tool for assessment of patient satisfaction following surgery to correct prolapse and/or incontinence. J Minim Invasive Gynecol. 2011;18(6):S49–S50. doi: 10.1016/j.jmig.2011.08.171. [DOI] [Google Scholar]
- 10.Covas Moschovas M, Bhat S, Onol FF, et al. Modified apical dissection and lateral prostatic fascia preservation improves early postoperative functional recovery in robotic-assisted laparoscopic radical prostatectomy: results from a propensity score-matched analysis. Eur Urol. 2020;78(6):875–884. doi: 10.1016/j.eururo.2020.05.041. [DOI] [PubMed] [Google Scholar]
- 11.Covas Moschovas M, Bhat S, Rogers T, et al. Technical modifications necessary to implement the da Vinci single-port robotic system. Eur Urol. 2020;78(3):415–423. doi: 10.1016/j.eururo.2020.01.005. [DOI] [PubMed] [Google Scholar]
- 12.Rogers T, Bhat KRS, Moschovas M, Onol F, Jenson C, Roof S, Gallo N, Sandri M, Gallo B, Patel V. Use of transversus abdominis plane block to decrease pain scores and narcotic use following robot-assisted laparoscopic prostatectomy. J Robot Surg. 2021;15(1):81–86. doi: 10.1007/s11701-020-01064-9. [DOI] [PubMed] [Google Scholar]
- 13.Assel M, Sjoberg D, Elders A, et al. Guidelines for reporting of statistics for clinical research in urology. Eur Urol. 2019;75(3):358–367. doi: 10.1016/j.eururo.2018.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Checcucci E, De Cillis S, Pecoraro A, et al. Single-port robot-assisted radical prostatectomy: a systematic review and pooled analysis of the preliminary experiences. BJU Int. 2020;126(1):55–64. doi: 10.1111/bju.15069. [DOI] [PubMed] [Google Scholar]
- 15.Murphy M, Sternschuss G, Haff R, van Raalte H, Saltz S, Lucente V. Quality of life and surgical satisfaction after vaginal reconstructive vs obliterative surgery for the treatment of advanced pelvic organ prolapse. Am J Obstet Gynecol. 2008;198(5):573.e1–573.e7. doi: 10.1016/j.ajog.2007.12.036. [DOI] [PubMed] [Google Scholar]
- 16.Culligan PJ, Lewis C, Priestley J, Mushonga N. Long-term outcomes of robotic-assisted laparoscopic sacrocolpopexy using lightweight y-mesh. Female Pelvic Med Reconstr Surg. 2020;26(3):202–206. doi: 10.1097/SPV.0000000000000788. [DOI] [PubMed] [Google Scholar]
- 17.Sardiwalla Y, Jufas N, Morris DP. Long term follow-up demonstrating stability and patient satisfaction of minimally invasive punch technique for percutaneous bone anchored hearing devices. J Otolaryngol Head Neck Surg. 2018;47:71. doi: 10.1186/s40463-018-0316-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Coyne KS, Kvasz M, Ireland AM, Milsom I, Kopp ZS, Chapple CR. Urinary incontinence and its relationship to mental health and health-related quality of life in men and women in Sweden, the United Kingdom, and the United States. Eur Urol. 2012;61(1):88–95. doi: 10.1016/j.eururo.2011.07.049. [DOI] [PubMed] [Google Scholar]
- 19.Box G, Averch T, Cadeddu J, et al. Nomenclature of natural orifice translumenal endoscopic surgery (NOTES) and laparoendoscopic single-site surgery (LESS) procedures in urology. J Endourol. 2008;22:2575–2581. doi: 10.1089/end.2008.0471. [DOI] [PubMed] [Google Scholar]
- 20.Sanchez-Salas RE, Barret E, Watson J, Stakhovskyi O, Cathelineau X, Rozet F, Galiano M, Rane A, Desai MM, Sotelo R, Vallancien G. Current status of natural orifice trans-endoscopic surgery (NOTES) and laparoendoscopic single site surgery (LESS) in urologic surgery. Int Braz J Urol. 2010;36(4):385–400. doi: 10.1590/s1677-55382010000400002. [DOI] [PubMed] [Google Scholar]
- 21.Menon M, Shrivastava A, Tewari A, Sarle R, Hemal A, Peabody JO, Vallancien G. Laparoscopic and robot assisted radical prostatectomy: establishment of a structured program and preliminary analysis of outcomes. J Urol. 2002;168(3):945–949. doi: 10.1097/01.ju.0000023660.10494.7d. [DOI] [PubMed] [Google Scholar]
- 22.Ilic D, Evans SM, Allan CA, Jung JH, Murphy D, Frydenberg M. Laparoscopic and robotic-assisted versus open radical prostatectomy for the treatment of localised prostate cancer. Cochrane Database Syst Rev. 2017;9(9):CD009625. doi: 10.1002/14651858.CD009625.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ploussard G. Robotic surgery in urology: facts and reality. What are the real advantages of robotic approaches for prostate cancer patients? Curr Opin Urol. 2018;28(2):153–158. doi: 10.1097/mou.0000000000000470. [DOI] [PubMed] [Google Scholar]
- 24.Schroeck FR, Krupski TL, Sun L, et al. Satisfaction and regret after open retropubic or robot-assisted laparoscopic radical prostatectomy. Eur Urol. 2008;54(4):785–793. doi: 10.1016/j.eururo.2008.06.063. [DOI] [PubMed] [Google Scholar]
- 25.Lindsay J, Uribe S, Moschonas D, et al. Patient satisfaction and regret after robot-assisted radical prostatectomy: a decision regret analysis. Urology. 2020;149:122. doi: 10.1016/j.urology.2020.12.015. [DOI] [PubMed] [Google Scholar]
- 26.Sanda MG, Dunn RL, Michalski J, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. N Engl J Med. 2008;358(12):1250–1261. doi: 10.1056/NEJMoa074311. [DOI] [PubMed] [Google Scholar]
- 27.McCarus SD. Scar assessment for patients undergoing minimal invasive hysterectomy. Surg Technol Int. 2014;25:150–156. [PubMed] [Google Scholar]
- 28.Vogl S. Telephone versus face-to-face interviews: mode effect on semistructured interviews with children. Sociol Methodol. 2013;43(1):133–177. doi: 10.1177/0081175012465967. [DOI] [Google Scholar]