Abstract
BACKGROUND:
Children under-five constitute 11.9% (n = 20,447,628) of the total population of Pakistan. Poor water and sanitation in Pakistan cause 97,900 deaths annually, 54,000 of whom are children under-five.
MATERIALS AND METHODS:
This study calculates an index for water and sanitation risk for children under-5 in Pakistan to give a detailed understanding and insight into the prevalent risks. Data from Pakistan Integrated Household Survey 2011–12 are used. Stata 15.0 was used for data analysis. A risk index was created by integrating hazard and vulnerability factors including toilet facilities, water source, mother's education, and the number of children in the household. Children were ranked according to their risk score in three categories: low risk, medium risk, and high risk. For each level of risk, profiles of children are created at the national, regional (urban, rural), and provincial levels.
RESULTS:
Out of 20.5 million children under-five in Pakistan, 71.6% live in rural areas. About 24.9% of children benefit from pipe-borne drinking water; 15.5% of children have toilets connected to the public sewerage system; 62.6% of the children have mothers who had no education; and 50.5% of children live in households with three or more children. It appeared that 57.5% of children are at high risk of poor water and sanitation as compared to merely 1.3% of children at low risk. Around 69.9% of children living in rural areas are at high risk compared to 24.6% of children in urban areas. In Balochistan, 77.9% of children are at high risk, the highest of all provinces.
CONCLUSION:
The majority of children under-five in Pakistan are at high risk owing to poor water and sanitation. A comprehensive public health program is needed to address the key indicators related to child health risk identified in this research such as safe drinking water, improved sanitation, education and mothers' awareness, and population growth.
Keywords: Child health, mother's education, Pakistan, pipe-borne drinking water, risk index, sanitation
Introduction
Globally, nearly three-quarter of all deaths of children under the age of five in 15 countries including Pakistan are due to diarrhea.[1] Lack of access by children under-5 to clean water and good sanitation is a huge public health problem in many developing countries. Around 2.1 billion people globally do not have access to safe drinking water and around 2.3 billion people lack access to basic sanitation. Moreover, over half a million children under-five die as a result of diarrhea annually.[2]
The situation is alarming because the number of people without adequate sanitation and safe drinking water is more than twice the people living in extreme poverty. Although with the passage of time, global poverty is declining, the number of vulnerable people with no access to clean water and sanitation is increasing.[3] Moreover, water contaminated with pathogenic microorganisms and inadequate sanitation leads to chronic ailments, morbidity, and mortality.[4] Diarrhea which results from unclean water and poor sanitation is the second major cause of child mortality.[5] Despite the joint efforts of the United Nations (UN) and World Health Organization (WHO), 850,000 people die annually as a result of improper hygiene, inadequate sanitation, and poor water infrastructure.[6]
Inadequate water and sanitation infrastructure affect almost half of the population, predominantly children under-five, in less developed countries. There is a strong correlation between unclean drinking water, lack of sanitation, and the prevalence of diarrhea, the major cause of mortality in children under-five.[7,8] Lack of access to clean drinking water and sanitation facilities lowers the chances of child survival and gravely affects infants and children.[9] On the other hand, children born into households with access to pipe-borne drinking water and improved toilet facilities are less prone to mortality.[10]
Maternal and child characteristics are also important determinants of child health and mortality. Children born to educated parents have a lower risk of mortality than those born to parents with no education.[11] Mother's education has a significant impact on a child's survival because of household's preferences and practices of health care, hygiene, nutrition, birth spacing, and disease treatment.[12] The average maternal educational level in the society cumulatively is more beneficial for child survival than the educational level of individual mothers.[13,14,15] The risk of mortality also increases with the increase in family size.[16]
Pakistan has appalling water and sanitation conditions,[17] which causes 97,900 deaths annually 54,000 of which are of children under the age of five.[18] A quarter of the people visiting hospitals in Pakistan suffer from water- and sanitation-related diseases.[3]
Although much work has been done on examining the factors associated with conditions of child health, developing a composite risk index for children with an examination of its determinants is required.[19] While Campos et al., assessed sanitation-related risk by developing a risk index, they did not attempt its empirical testing or link to national data. This is the motivation for this study.[20] The aim of this study was, therefore, to construct an index for water and sanitation risk to identify children under-five in Pakistan (from now referred as “children”) at risk and reveal the severity of their exposure to water and sanitation risk.
Materials and Methods
The present study used the secondary data from the Pakistan Integrated Household Survey (PIHS) 2011–12 collected by the Pakistan Bureau of Statistics (PBS), Government of Pakistan. PIHS is a national-level survey which collects the data on various personal, social, and economic indicators from individuals in selected households. The Planning and Development Division and Statistics Division of Government of Pakistan provided the ethical and administrative approval to PBS for the PIHS 2011–12 survey vide No. 9 (11)/2009-10/PIA-III/PC and No. F.2-3/2004 (A-III) (FandA) 423 dated 08/10/2009, and 20/10/2009, respectively. Separate ethical approval for this study was not taken as the data are available in the public domain through the PBS website for academic purposes and also because there was no direct human subject engagement in this study. The survey involving 17,056 households nationwide was based on a sample of 16,897 children under-five belonging to 8718 households in Pakistan. PIHS population weights were included for the calculation of risk index and risk profiling. This study used Stata 15 for data management and statistical analysis.
Assessment of sanitation-related risk assumes that individuals are at risk of exposure to pathogens living in human excreta, which can cause illness.[20] Ingestion of pathogens combined with the vulnerability of the individual can determine the chances of picking up disease. In the environmental health risk assessment approach, developed and applied in Indonesia for city sanitation planning, priority areas were identified on the basis of several demographic, social, and individual characteristics such as poverty, population size and density, area of domicile (urban/rural), handwashing, water supply, wastewater and solid waste services, and drainage.[20] The present study follows the conceptual framework of rapid participatory sanitation system risk assessment (RPSSRA) which was developed by the International Water Association and University College London, which used a set of indicators to quantify the risk.[20] The RPSSRA methodology was then applied to assess sanitation-related risk in Maputo, Mozambique, to support urban sanitation planning. Indeed, knowledge of disease transmission can be helpful in planning and designing the necessary interventions for disease transmission.[21]
Following the disease transmission route proposed by Haruna, for the present study, the risk was defined by two main components: hazard and vulnerability.[21] Toilet facilities and sanitation infrastructure are crucial in determining the containment and disposal of human waste and the risk of being exposed to feces containing pathogens. In the absence of proper toilet facilities and sanitation infrastructure, the risk of diseases increases as the pathogens are more likely to emit into the environment. Therefore, quality and coverage of the sanitation system is vital for determination of sanitation hazard.[20] Similarly, water source and quality of water are important factors for waterborne diseases.[21] Hazard for children is measured through their access to toilets and tap water.
Lack of access to toilet facilities indicates unsafe sanitation, which can expose individuals to pathogens. The condition of the toilet can indicate the exposure to pathogens owing to improper containment of fecal matter. Lack of access to tap water indicates the risk of exposure to unsafe and contaminated water.
An individual's proclivity to contracting diseases is also related to socioeconomic factors such as type of dwelling, size of the household, education level, and poverty. A lot of young children living together, small and congested dwelling house, low educational levels, and poor household economic conditions can make one vulnerable to diseases and illness. Vulnerability of children is measured through their size and mother's education. Young children are more vulnerable to disease.[17] The number of children in a household is related to the susceptibility of children, particularly infants to morbidity and mortality.[22] Health and hygiene of children is associated with the mother's education.[21] Mother's awareness can prevent water and sanitation-borne diseases when water is boiled, handwashing is insisted on and other hygienic practices are promoted.[7]
For the construction of the risk index, the selected indicators were classified into three categories: low, medium, and high with their corresponding numerical values of 0.25, 0.5, and 0.75, respectively. The criteria for low, medium, and high categories for each indicator are outlined in Table 1.
Table 1.
Criteria for risk categories
| Dimension/indicator | Low (0.25) | Medium (0.50) | High (0.75) |
|---|---|---|---|
| Hazard: Type and quality of sanitation system | |||
| Toilet type | Flush connected to public sewerage | Pit and others | No toilet in the house |
| Source of drinking water | Piped water | Hand pump/motorized pumping/tube well | Well/pond/canal/river/others |
| Vulnerability: Demographics and mother’s awareness about hygiene | |||
| Number of children in household | One child | Two children | Three or more children |
| Mother’s education (schooling years) | Above 5 years | 5 years or less | No schooling |
Source: Proposed by authors
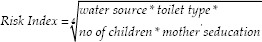
The general form of relative risk is defined as Risk Index = Hazard × Vulnerability, where hazards are water source (tap water; hand/motor pump/well; river/pond and others) and toilet type (no toilet; flush connected to public sewerage; pit and others). Vulnerability is the number of children in the household (1, 2, 3, or more) and mother's education (no schooling, primary [5 years] or less, or above primary).
Following Alkire and Foster, Mazziotta and Pareto, and UNDP, the risk index is computed by taking the geometric mean of the indicators outlined in Table 1.[23,24,25] The risk index is then calculated as:
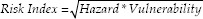
Therefore,
The risk index allows the ranking of children according to their respective risk scores. The children were grouped into three categories as follows: low risk: index score ≤0.25, medium risk: 0.25 < index score ≤0.5, and high risk: index score >0.5.
Results
Distribution of children in regions and provinces [Table 2] is quite comparable to the total population distribution in the respective regions and provinces except Punjab, which has a higher population growth than the other provinces. Only 24.9% of children have pipe-borne water, whereas for around 12.8% of children the water they consume is from unsafe open source [Table 3]. Although urban areas usually have improved public infrastructure, around 55% of children in urban areas have access to pipe-borne water as compared to only 13.5% in rural areas. The situation as regards the water source seems to be the worst in Khyber Pakhtunkhwa (KP) and Balochistan where 31.4% and 41.9% of children have unsafe (high risk) water, respectively. Punjab and Sindh, despite having the major proportion of the child population, have the lowest proportion of children exposed to unsafe (high risk) water sources (4.7% and 9.9%, respectively). The majority of children exposed to comparatively less, yet unsafe water source (medium risk) was also found in Punjab and Sindh, i.e., 77.2% and 60.6%, respectively. It is noteworthy that KP appears to have the highest proportion of children (37.3%) with low-risk water sources followed by Balochistan (31.9%). Punjab, although the largest province in terms of population and the recipient of the highest share in national budget, has the least access to tap water (low risk); only 18.1% of children in Punjab appear to have access to tap water.
Table 2.
Distribution of children and total national population by place of living (2011-2012)
| Children N (%) | Total national population N (%) | |
|---|---|---|
| Region | ||
| Urban | 5,810,176 (28.4) | 47,107,789 (27.5) |
| Rural | 14,637,451 (71.6) | 124,354,008 (72.5) |
| Provinces | ||
| Punjab | 11,700,399 (57.2) | 91,646,176 (53.4) |
| Sindh | 4,752,560 (23.2) | 39,744,468 (23.2) |
| KP | 2,990,238 (14.6) | 28,923,394 (16.9) |
| Balochistan | 1,004,431 (4.9) | 11,147,740 (6.5) |
Source: Authors’ calculations using PIHS 2011-2012. KP=Khyber Pakhtunkhwa, PHIS=Pakistan Integrated Household Survey
Table 3.
Distribution of children for selected indicators and risk categories (2011-2012)
| Indicators/risk category | National level | Province level | |||||
|---|---|---|---|---|---|---|---|
| Pakistan (n=20,447,627)% | Urban (n=5,810,176) % | Rural (n=14,637,451)% | Punjab (n=11,700,399)% | Sindh (n=4,752,560) % | KP (n=2,990,238)% | Balochistan (n=1,004,431) % | |
| Water source | |||||||
| Tap water (low risk) | 24.9 | 54.8 | 13.5 | 18.1 | 29.6 | 37.3 | 31.9 |
| Hand/motor pump (medium risk) | 62.3 | 36.8 | 72.0 | 77.2 | 60.6 | 31.3 | 26.2 |
| River/pond etc., (high risk) | 12.8 | 8.4 | 14.5 | 4.7 | 9.9 | 31.4 | 41.9 |
| Toilet type | |||||||
| Flush toilet connected to public sewerage (low risk) | 15.5 | 47.9 | 3.3 | 16.8 | 25.4 | 3.0 | 2.4 |
| Flush with pit or dry raise toilet (medium risk) | 64.8 | 51.3 | 70.0 | 62.0 | 60.6 | 80.6 | 62.9 |
| No toilet (high risk) | 19.6 | 0.9 | 26.8 | 21.3 | 14.0 | 16.4 | 34.8 |
| Mother’s education | |||||||
| No education (high risk) | 62.6 | 37.5 | 72.1 | 54.3 | 63.0 | 77.2 | 91.0 |
| Primary or below (medium risk) | 12.6 | 12.9 | 12.6 | 15.8 | 12.1 | 6.8 | 3.9 |
| Above primary (low risk) | 24.8 | 49.7 | 15.4 | 29.9 | 24.9 | 16.0 | 5.1 |
| Number of children in household | |||||||
| One (low risk) | 16.8 | 20.3 | 15.4 | 17.6 | 17.2 | 15.5 | 11.8 |
| Two (medium risk) | 32.7 | 34.3 | 32.1 | 34.0 | 34.6 | 29.0 | 25.2 |
| Three or more (high risk) | 50.5 | 45.3 | 52.5 | 48.4 | 48.2 | 55.6 | 63.0 |
| Risk index | |||||||
| Low (0.25) | 1.3 | 4.5 | 0.0 | 1.0 | 3.2 | 0.1 | 0.1 |
| Medium (>0.25≤0.5) | 41.3 | 70.9 | 30.1 | 46.6 | 41.1 | 32.3 | 22.0 |
| High (>0.5) | 57.5 | 24.6 | 69.9 | 52.5 | 55.7 | 67.6 | 77.9 |
Source: Authors’ calculations using PIHS 2011-2012. KP=Khyber Pakhtunkhwa, PIHS=Pakistan Integrated Household Survey
In terms of sanitation and hygiene, only 15.5% of children live in houses with flush toilets connected to the public sewerage system, while around one-fifth of children do not have toilets in their homes [Table 3]. The situation is dire in rural areas where more than a quarter of the children do not have access to a proper toilet. Of the provinces, the highest proportion of children with no toilets is Balochistan (34.8%), followed by Punjab (21.3%). Another interesting fact is that 62.6% of the mothers have no education, while a mere 24.8% of the children's mothers have above primary education [Table 3]. Although the picture seems bleak in rural areas where 72.1% of the children's mothers have had no schooling, more than 50% of mothers in the urban areas have none or little primary education. The worst of the provinces with regard to mothers' education is Balochistan where 91% of mothers have had no education, and KP follows with 77.2%. Punjab appears to have the highest percentage of mothers with more than primary education (29.9%) which is nevertheless unsatisfactory.
The majority of children (50.5%) live in households with three or more children, while only 16.8% of the children live in a household with a single child [Table 3]. Except for Balochistan, there does not appear to be huge differences across regions and provinces in terms of the number of children in the household. However, the majority of children in Pakistan appear to be vulnerable to water- and sanitation-related risks [Table 3].
The estimated index indicates that the majority (57.5%) of children in Pakistan are at high risk, whereas only a small fraction (1.3%) of children are exposed to water- and sanitation-related risks [Table 3]. The majority of children (69.9%) at high risk are found in rural areas with poor infrastructure and socioeconomic conditions. The picture is no different across provinces where most of the children face conditions of high risk. Although the situation seems terrible in Balochistan where 77.9% of children are exposed to high risk, it is the least populated province. On the other hand, the situation is more terrible in Punjab which has more than half the number of children, 52.5% of whom are at high risk.
Discussion
Regarding access to safe drinking water, the reason for extremely high incidence of waterborne diseases like diarrhea in children in Pakistan is the fact that less than a quarter of the children have access to safe water.[17] The pattern of access to pipe-borne drinking water in urban and rural areas appears to be in line with the WHO, which identified that 61% of urban children and 25% of rural children have access to pipe-borne water.[3] On the one hand, the provision of pipe-borne water is lowest in Punjab, and the quality is extremely poor. Old underground water and sewerage intermingle owing to leakage, inadequate spacing, and faulty joints. These are some of the major factors resulting in the poor quality of pipe-borne water in Punjab.[4] Poor sanitation and hygiene are evident from the fact that 19.6% of children do not have access to a toilet, while only 15.5% of children have safe toilets, which could be the reason for the appalling health conditions of children in Pakistan.[17] Poor water quality and lack of access to adequate sanitation infrastructure increase the risk of waterborne diseases such as diarrhea in children.[8] Apart from diarrhea, stunting is also an adverse consequence of inadequate provision of water and sanitation infrastructure. A 2-year-old child who has poor drinking water and poor sanitation is likely to be 1 cm shorter and would experience 50% more episodes of diarrhea.[8] In Zimbabwe, infants born in households with pipe-borne water and improved toilet facilities have 12% and 38% less risk of mortality, respectively.[22] A survey from 70 low- and middle-income countries for the period 1986–2007 revealed that children with access to improved sanitation had 13% less chances of diarrhea and 27% less risk of stunting.[5] The importance of access to improved water and sanitation is highlighted by Cha et al.,(2017), suggesting that interventions to improve water and sanitation can potentially reduce diarrhea by 25%.[26]
The majority of mothers (62.6%) are uneducated. The concentration of uneducated mothers is more in the rural areas (72.1%) which is in line with the population of children in the rural areas (72.5%). The real concern is that 37.5% of the children in urban areas have uneducated mothers, while the proportion of children in urban areas is 27.5%. The lack of education of the mothers is an important contributor to the vulnerability of children to water and sanitation risk as unhygienic practices of illiterate mothers is a factor in children's health risk as regards water and sanitation.[7,11,19,21,26] The vulnerability to risk is also aggravated by the concentration of children in households. There is not much difference in the concentration of children in households in urban or rural areas as 45.3% of the children in urban areas live in households with three or more children as compared to 52.5% in rural areas. This also reflects the density of the population in Pakistan. Increased vulnerability of children in households with three or more children in Pakistan appears in line with the findings of Kembo and Ginneken (2009) and Murtaza et al., (2015) which suggested that with the increase in the number of children in a household comes a rise in a child's vulnerability to water- and sanitation-related diseases.[22,17]
The distressing condition of child health in Pakistan is that only 1.3% of children seem to be at low water- and sanitation-related risks. These conditions are worst in Punjab where the majority (53.5%) of children live, but only 1% of whom children are in the low-risk category as opposed to 52.5% of children at high risk.
Indeed the findings of this study are comparable to those of Campos et al., (2015), though not free of limitations.[20] Although the composite index developed in this study is based on the RPSSRA tool, there is indeed room for improvement of reliability of the index particularly in terms of selection of hazard and vulnerability indicators and the way the indicators are defined, i.e., low, medium, and high. It should be acknowledged that various indicators would contribute to the overall risk index in different degrees. Therefore, the risk index should use the appropriate weights for the corresponding indicators – a task for future work. Furthermore, application of the risk index to other developing countries would enable the comparison and robustness of the risk indicators for the assessment of environmental and sanitation risk in children in developing countries. The results of the study could be updated and further explored by using the latest data.
Conclusion
This is the first study using an index to identify exposure to water and sanitation risk in children in Pakistan. Identifying the children exposed to water- and sanitation-related risks will help in designing focused policies and directing resources to the areas or groups most in need.
The study suggests that a multidimensional effort is needed to reduce children's exposure to water and sanitation risks in Pakistan. Interventions such as improvement in water quality and source, toilet type, handwashing, and water filtration can significantly reduce the vulnerability of children. The public policy in Pakistan should initiate intervention programs like WASH more aggressively to improve the public health in general and child health in particular. To address the alarming situation of risk to children, the policy must also focus on improving the socioeconomic conditions in Pakistan. Emphasis on women's education, increasing awareness of hygiene, and allocating resources for the improvement of infrastructure should be on the national agenda for change in Pakistan. Health and hygiene awareness can also be promoted by engaging and mobilizing individuals, businesses, local communities, and the media. It is crucial to protect vulnerable children residing in hazard-prone settlements.
Innovative ideas and initiatives for social upliftment such as engaging the public through community partnership and ownership may be effective in promoting and improving health conditions, especially in the rural areas where the public sector is not as visible as in urban areas. Focus on low-cost community-built and financed primary sewerage and low-cost toilets may be effective in improving sanitation − after awareness, cost-effectiveness is the key to creating demand. Funds should be provided to build toilets in the homes of poor and hazard-prone families of children residing in the poorest quintiles. Planning for clean water and sanitation infrastructure should be decentralized and provinces and local governments must take the initiative by encouraging local communities and nongovernmental organizations to improve public health.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
This paper is extracted from the dissertation submitted by the corresponding author at the University of Essex in 2019.
References
- 1.International Vaccine Access Center. Johns Hopkins Bloomberg School of Public Health. Pneumonia and Diarrhea Progress Report. 2018. [[Last accessed on 2019 Jan 05]]. Available from: https://stoppneumonia.org/wp-content/uploads/2018/11/Pneumonia-and-Diarrhea-Progress-Report-2018.pdf .
- 2.UNICEF. Progress on Drinking Water, Sanitation and Hygiene: 2017 Update and SDG Baselines. [[Last accessed on 2018 Aug 10]]. Available from: https://www.who.int/water_sanitation_health/publications/jmp-2017/en/
- 3.WHO/UNICEF. Progress on Drinking Water, Sanitation and Hygiene. 2014. [[Last accessed on 2018 Aug 15]]. Available from: https://www.who.int/water_sanitation_health/publications/2014/jmp-report/en/
- 4.Nabeela F, Azizullah A, Bibi R, Uzma S, Murad W, Shakir SK, et al. Microbial contamination of drinking water in Pakistan – A review. Environ Sci Pollut Res Int. 2014;21:13929–42. doi: 10.1007/s11356-014-3348-z. [DOI] [PubMed] [Google Scholar]
- 5.Fink G, Günther I, Hill K. The effect of water and sanitation on child health: Evidence from the demographic and health surveys 1986-2007. Int J Epidemiol. 2011;40:1196–204. doi: 10.1093/ije/dyr102. [DOI] [PubMed] [Google Scholar]
- 6.UN. World Water Development Report 2016. [[Last accessed on 2018 May 18]]. Available from: http://www.unwater.org/publications/world-water-developmentreport-2016/
- 7.Khan A, Danish S, Ashfaq A, Ahmad F, Ali WS, Khan M. Knowledge, attitude and practices of mothers regarding diarrheal risk factors and management in under 5 children: A cross sectional survey in Dadu and Badin districts of Sindh, Pakistan. J Dow Univ Health Sci. 2016;10:19–24. [Google Scholar]
- 8.Checkley W, Gilman RH, Black RE, Epstein LD, Cabrera L, Sterling CR, et al. Effect of water and sanitation on childhood health in a poor Peruvian Peri-Urban community. Lancet. 2004;363:112–8. doi: 10.1016/S0140-6736(03)15261-0. [DOI] [PubMed] [Google Scholar]
- 9.Abou-Ali H. Goteburg University: Scandinavian Working Papers in Economics 112; 2003. The Effect of Water and Sanitation on Child Mortality in Egypt. Department of Economics. [Google Scholar]
- 10.Bennett J. Correlates of child mortality in Pakistan: A hazards model analysis. Pak Dev Rev. 1999;38:85–118. [PubMed] [Google Scholar]
- 11.Sijbesma C. Sanitation and hygiene in South Asia: Progress and challenges. Waterlines. 2008;27:184–204. [Google Scholar]
- 12.Mosley WH, Chen LC. An analytical framework for the study of child survival in developing countries.1984. Bull World Health Organ. 2003;81:140–5. [PMC free article] [PubMed] [Google Scholar]
- 13.Gebretsadik S, Gabreyohannes E. Determinants of under five mortality in high mortality regions of Ethiopia: An analysis of the 2011 Ethiopia demographic and health survey data. Int J Popul Res. 2016;(2):1–7. [doi: 10.1155/2016/1602761] [Google Scholar]
- 14.Zerai A. Preventive health strategies and infant survival in Zimbabwe. Afr Dev. 1997;22:101–29. [Google Scholar]
- 15.Sedhain P Water, Sanitation. Socioeconomic Status and Prevalence of Waterborne Diseases: A Cross-Sectional Study at Makwanpur District, Nepal. The Artic University of Norway. Master's Thesis 2014. [[Last accessed on 2018 Jul 10]]. Available from: https://hdl.handle.net/10037/6503 .
- 16.Hutton G, Haller L WHO. Evaluation of the Costs and Benefits of Water and Sanitation Improvements at the Global Level. 2004. [[Last accessed on 2020 Dec 15]]. Available from: https://apps.who.int/iris/handle/10665/68568 .
- 17.Murtaza F, Mustafa T, Awan R. Child health inequalities and its dimensions in Pakistan. J Family Community Med. 2015;22:169–74. doi: 10.4103/2230-8229.163036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.WB. Washington: 2013. [[Last accessed on 2020 Sep 01]]. Economic Impacts of Inadequate Sanitation in Pakistan: Economics of Sanitation Initiative. Available from: http://hdl.handle.net/10986/17375 . [Google Scholar]
- 19.Murtaza F. Colchester: University of Essex; 2019. Determinants of Water and Sanitation Risk in Children Under Five Years of Age in Pakistan [Dissertation] [Google Scholar]
- 20.Campos LC, Ross P, Nasir ZA, Taylor H, Parkinson J. Development and application of a methodology to assess sanitary risks in Maputo, Mozambique. Environ Urban. 2015;27:371–88. [Google Scholar]
- 21.Haruna BB. Sanitation health risk and safety planning in urban residential neighbourhoods. ATBU J Environ Technol. 2017;10:160–73. [Google Scholar]
- 22.Kembo J, Ginneken JK. Determinants of Infant and Child Mortality in Zimbabwe: Results of Multivariate Hazard Analysis. Demogr Res. 2009;21:367–84. [Google Scholar]
- 23.Alkire S, Foster J. Counting and multidimensional poverty measurement. J Public Econ. 2011;95:476–87. [Google Scholar]
- 24.Mazziotta M, Pareto A. Methods for constructing composite indices: One for all or all for one. Riv Ital Econ Demogr Stat. 2013;67:67–80. [Google Scholar]
- 25.UNDP. New York, NY: UNDP; 2015. [[Last accessed on 2018 Sep 01]]. Training Material for Producing National Human Development Reports, Occasional Paper. Available from: http://hdr.undp.org/sites/default/files/hdi_training.pdf . [Google Scholar]
- 26.Cha S, Lee J, Seo D, Park BM, Mansiangi P, Bernard K, et al. Effects of improved sanitation on diarrheal reduction for children under five in Idiofa, DR Congo: A cluster randomized trial. Infect Dis Poverty. 2017;6:137. doi: 10.1186/s40249-017-0351-x. [DOI] [PMC free article] [PubMed] [Google Scholar]


