Abstract
Galvanic skin response (GSR) Biofeedback uses training to reduce tension and anxiety and improve concentration and self-regulation. The study was aimed to evaluate this method as a form of rehabilitation and quantify the outcomes achieved by patients undergoing training using this technique. Six schizophrenic patients were enrolled in the study and underwent training based on the relaxation training module (CENTER), concentration training module (BALANCE), and self-regulation training module (INSECTS). Training sessions were held twice a week for 6 weeks. From the total group of subjects involved in the study, two patients had a statistically significant increase in measured values after the CENTER exercise, indicating that relaxation was achieved. Four patients showed a statistically significant decrease in measured values after the BALANCE exercise, which was reflective of an improvement in concentration. Three patients had a statistically significant decrease in measured values after the INSECTS exercise, which indicated an improvement in self-regulation. GSR Biofeedback may be used to complement the pharmacological treatment of patients diagnosed with schizophrenia.
1. Introduction
Schizophrenia is one of the most common causes of disability in young people [1]. Clinical diagnosis of schizophrenia requires finding specific clinical symptoms, persisting for a specific time. Eight dimensions of schizophrenia have been distinguished in the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-5): hallucinations, delusions, speech disorganisation, abnormal psychomotor behaviour, negative symptoms, cognitive disorders, depression, and mania [2].
Cognitive deficits dominating in schizophrenia patients are associated mainly with disorganisation and negative symptoms. Because they are chronic, they negatively affect the patients' overall social life [3–5]. Research shows that cognitive deficits are now present regardless of the disease stage and mainly concern functional disorders in the frontal and temporal lobes [6–13].
Despite multidirectional research, it is still difficult to clearly determine what factors are decisive for maintaining health or preventing the occurrence of disease in schizophrenia patients. It appears that the sense of coherence (SOC), a concept proposed by Antonovsky (a salutogenic model which assumes that health can only be preserved when there is a balance between stress and coping. This process is affected by biological factors, stressors, lifestyle, and coherence, all of which comprise an individual's interactions with the environment) is a crucial component in the recovery process and components such as a sense of comprehensibility, manageability, and meaningfulness fully explain this concept [14].
From the point of view of schizophrenia patients, Antonovsky's concept proves to be interesting because it concerns general life orientation and covers all areas associated with correct reception of external and internal information, activity, and personal resources. This salutogenic model plays an important role in coping with stress and problems in daily life.
Increasingly, new possibilities are being sought that, based on therapeutic interventions, would enable the reduction of deficits resulting from the disease. Today, much interest is focused on neuronal mechanisms, which, being physiological markers, can be used to guide treatment decisions regarding existing deficits. One such indicator is electrodermal activity (EDA), which provides information about emotions, cognitive processes, and behaviour, and hence also about the functioning of different brain areas. The galvanic skin response (GSR), both the general tonic-level electrodermal component (skin conductance level, SCL) and the phasic component (skin conductance responses, SCRs), is a measure used in the diagnosis and treatment of mental disorders, and Biofeedback training method based on GSR measurements allows to modulate a patient's emotional state as the need arises [15].
The ability to reduce stress presumably increases the patients' sense of coherence, protects them against relapse, enhances their cognitive processes, and improves their quality of life. Such a possibility is offered by GSR Biofeedback (GSR BF), which uses specially selected exercises to reduce the level of tension and anxiety and improve concentration and self-regulation. Importantly, the program provides an interesting interactive interface between the patient and the computer. The effects of this method are confirmed by numerous studies which describe a wide range of applications of this method in the rehabilitation of mentally ill patients with anxiety disorders [16–18], depression [19, 20], suicidal tendencies [21, 22], bipolar affective disorder [23, 24], and schizophrenia [25–27]. By analysing the electrodermal activity signal on baseline, phasic SCRs, and tonic SCL data, one can determine the phase of the disease, severity of symptoms, and the possibility of relapse. These extremely sensitive indicators reveal many features that are common to specific clinical entities, which, from the diagnostic point of view, are important for further treatment decisions [15].
Today, there are many studies available regarding the use of neurofeedback in the rehabilitation of people with mental disorders [28–31]. In addition, there is a lively discussion about the effectiveness of this method in psychiatry, and at the same time, it is recommended to continue research on this topic [32, 33]. While research on the meaning of the galvanic skin response in groups of patients with schizophrenia was carried out and the pioneer of these studies was Gruzelier [34, 35], currently, studies using GSR are not widely conducted. However, it is an important neurophysiological indicator as well as muscle (EMG) and brain (EEG) indicators.
This study was aimed to evaluate the GSR Biofeedback method as a form of rehabilitation and to demonstrate the outcomes achieved by schizophrenia patients undergoing training based on three modules: relaxation (CENTER), concentration (BALANCE), and self-regulation (INSECTS).
2. Materials
2.1. Characteristics of the Studied Group
The average patient age was 41 years (range: 34-45 years, median: 42.5); four patients were single and two were divorced. All patients came from large cities (over 100 thousand inhabitants); all were receiving a disability allowance and lived alone or with their parents. Three subjects had completed primary education (until 15 years of age), while the other three had completed secondary education (until 18 years of age). The mean number of subjects' hospitalisations was 8 stays (range: 4-15; median: 7) and was possibly associated with irregular treatment, alcohol consumption, or discontinuation of medication. The mean age at the time of the first hospitalisation was 21 years (range: 22-29; median: 24). Four patients did not report suicidal attempts and self-harm; two patients did report such episodes. All subjects were right-handed, took atypical neuroleptics, had no neuroleptic malignant syndrome (NMS) complications, and had no family history of schizophrenia; no drug allergies were reported; none had undergone major surgery; and none had problems with alcohol addiction. These details are presented in Table 1.
Table 1.
Demographic data and data associated with the patients' disease.
| Variable | n | |
|---|---|---|
| Place of residence | Large city (above 100 thousand) | 6 |
| City (below 100 thousand) | 0 | |
| Village | 0 | |
| Living situation | Alone | 3 |
| With parents | 3 | |
| With family | 0 | |
| Education | Primary | 3 |
| Vocational | 0 | |
| Secondary | 3 | |
| University | 0 | |
| Employment | In profession | 0 |
| Outside profession | 0 | |
| Unemployed | 0 | |
| Benefit (awarded for a definite period) | 1 | |
| Disability benefit (awarded for an indefinite period) | 5 | |
| Marital status | Single | 4 |
| Married | 0 | |
| Divorced | 2 | |
| Widower | 0 | |
| Number of children | None | 4 |
| One child | 2 | |
| Family history—mother | No | 6 |
| Yes | 0 | |
| Family history—father | No | 6 |
| Yes | 0 | |
| Outpatient monitoring | Regular (once a month) | 4 |
| Irregular (less often than once a month) | 2 | |
| None | 0 | |
| Self-mutilation | None | 4 |
| Surface cuts | 1 | |
| Deep cuts | 1 | |
| Other | 0 | |
| Suicide attempts | No | 4 |
| Yes | 2 | |
| Causes of disease recurrence | Alcohol (occasional consumption) | 2 |
| Withdrawal of medicines | 3 | |
| No clear reason | 1 | |
| Substance use | None | 3 |
| Alcohol | 0 | |
| Drugs | 0 | |
| Nicotine | 3 | |
| Other | 0 | |
| Medication | Atypical | 6 |
| Typical | 0 | |
| Mixed | 0 | |
| NMS | No | 6 |
| Yes | 0 | |
| Allergies to medicines | No | 6 |
| Yes | 0 | |
| Total | 6 | |
3. Method
3.1. Design
Six schizophrenia patients in remission were included in the pilot study. Considering the main deficits, which patients experience in schizophrenia [1, 3, 4, 8–14] standard training based on the relaxation (CENTER), concentration (BALANCE), and self-regulation (INSECTS) modules on the Elmiko Digi-Track apparatus (Elmiko-Medical Company, Warsaw, Poland) was organised. Convenience sampling was used to recruit participants, who were patients of psychiatric day ward in one hospital in the eastern part of Poland and had to meet the following study inclusion criteria: a patient's informed consent, a clinical diagnosis of schizophrenia (DSM-V), age (18–50 years), right-handedness, no history of neurological diseases, and exclusion of mental impairment, dementia, and addiction to alcohol. To ensure anonymity, patients were given codes consisting of two letters BF (short for Biofeedback) and a number: BF-2, BF-3, BF-7, BF-8, BF-9, BF-10.
3.2. Procedure
The participants who did the CENTER exercise were instructed to bring bubbles appearing on the screen into a circle in the centre of the screen; the faster the person relaxed, the faster they placed the bubbles in the circle. Participants practising in the BALANCE module had the task of placing and holding a ball in the middle of a tilting board; correct performance of the task testified to increased activation. The exercise in the INSECTS module consisted of turning ants running across the screen into ladybugs by clicking on them with the mouse; correct performance showed that a balance in self-regulation had been achieved.
Each training module was analysed for the level of the participants' relaxation and activation. The results were analysed using a PC and included the following indicators: average, baseline SCL value (start value), maximum relaxation value (expressed as a percent or as an absolute value in kOhm), and the minimum relaxation value, which was also the maximum activation value (expressed as a percent or as an absolute value in kOhm) [36].
The initial/start value was calculated automatically and depended on the participant's level of activation at the beginning of the session (dashed line). The computer registered the patient's psychophysical state during each new session relative to the start value. The average was represented by a solid line which connected data points representing average relative changes in GSR. The relative position and distance between the two lines depended on the participant's initial activation state and the maximum and minimum values of relaxation and activation. The dashed line positioned above the solid line meant that the participant showed higher activation (a higher start value), which should decrease during the session. A decrease in the value associated with activation (solid line below dashed line) indicated an increase in the level of relaxation, and the data points connected by the solid line were averages of the values obtained during the whole session. A declining solid line with a small number of phasic activities (SCRs) indicated that relaxation dominated over activation. Conversely, a rising solid line and an increased number of SCRs showed that activation dominated over relaxation. The main goal of all the training sessions was to stabilize the participants' mental state and control and modulate it depending on their current psychophysical condition. Exercises in the three modules allowed to alleviate the complaints reported by the patients (they enhanced cognitive processes; improved concentration, memory, perceptiveness, and executive functions; and stabilized emotions).
The tests were performed in accordance with the adopted schedule. Measurements were made with electrodes attached to fingers (index and ring) of the left hand, coupled to a device which displayed the sequential training modules. The training time was determined by the computer, in accordance with the Elmiko Digi-Track apparatus (Elmiko-Medical Company, Warsaw, Poland) Instruction Manual, and the patients' results were recorded in graphic form at the end of each session. Demographic data were collected using a proprietary questionnaire, and hemispheric dominance was determined on the basis of Linksman's test [37] (Figure 1).
Figure 1.
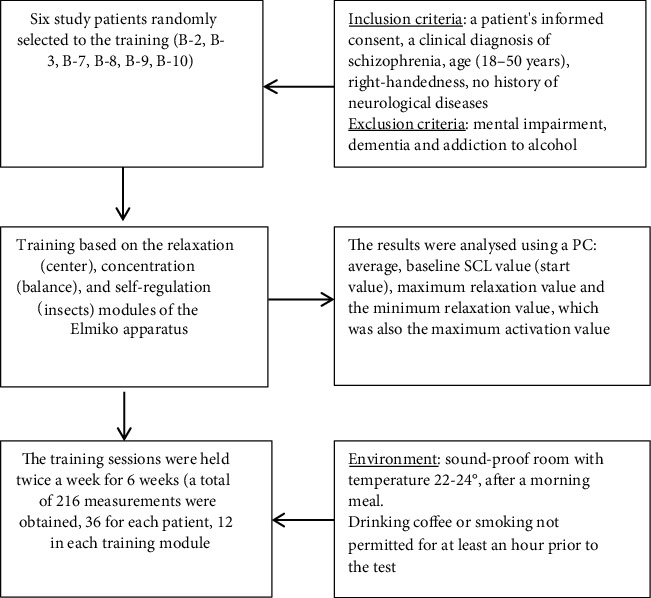
Research procedure.
3.3. Ethical Issues
The subjects had given their consent to participate in the exercises and were thoroughly acquainted with the procedure and the training method. They also provided a written statement on participation in the experiment. The study protocol was accepted by the Bioethics Committee of the Medical University of Lublin—approval no. KE-0254/35/2019.
3.4. Analysis
Statistical analyses were performed using the Statistica 9.1 package (StatSoft Polska). The study procedure included an analysis of changes in the initial values (I.V.) and mean values (M.V) for measurements obtained during sessions conducted in each module; the significance of the changes was determined using the Wilcoxon signed-rank test.
| (1) |
∑ R+ is the sum of positive ranks. ∑ R- is the sum of negative ranks.
The trend was established on the basis of the mean values of the initial measurements for each training day using the Spearman rank correlation coefficient.
| (2) |
d 2 i is the squares of the differences between the ranks of the corresponding values of the xi and yi characteristics. n is the number of data pairs (number of rows in the table).
4. Results
The tests were performed using three similar modules in accordance with the adopted schedule, at the same time intervals for all patients. The values measured in the studied group and the significance of the change between I.V. and M.V. are presented in Table 2.
Table 2.
Values measured in the studied group and significance of the change between I.V. and M.V.
| Patient: CODE | Method | Measurement | Average | Median | Min | Max | Bottom quartile | Upper quartile | Standard deviation |
|---|---|---|---|---|---|---|---|---|---|
| BF-2 | CENTER | I.V. | 160.17 | 128.5 | 79 | 329 | 101 | 220 | 77.41 |
| M.V. | 169.33 | 135 | 64 | 322 | 94.5 | 264 | 92.79 | ||
| Difference | 9.17 | 6 | -39 | 53 | -10 | 28 | 27.29 | ||
| Difference significance | Z = 1.020, p = 0.308 | ||||||||
| BALANCE | I.V. | 160.92 | 149 | 82 | 313 | 101.5 | 193.5 | 70.28 | |
| M.V. | 153.67 | 142 | 63 | 315 | 93.5 | 191.5 | 72.63 | ||
| Difference | -7.25 | -7 | -19 | 4 | -12.5 | -2 | 7.44 | ||
| Difference significance | Z = 2.589, p = 0.010 | ||||||||
| INSECTS | I.V. | 234.58 | 226.5 | 103 | 370 | 202.5 | 286 | 78.60 | |
| M.V. | 166.00 | 163.5 | 87 | 275 | 110 | 216.5 | 62.73 | ||
| Difference | -51.92 | -37 | -163 | 39 | -104 | -2 | 63.60 | ||
| Difference significance | Z = 2.490, p = 0.013 | ||||||||
| BF-3 | CENTER | I.V. | 772.00 | 734.5 | 504 | 1458 | 600.5 | 801 | 273.00 |
| M.V. | 841.17 | 742 | 508 | 1457 | 622.5 | 982.5 | 308.65 | ||
| Difference | 69.17 | 41 | -78 | 251 | -26 | 205 | 124.16 | ||
| Difference significance | Z = 1.336, p = 0.182 | ||||||||
| BALANCE | I.V. | 941.67 | 843 | 508 | 1831 | 717 | 1034.5 | 394.96 | |
| M.V. | 859.17 | 759 | 496 | 1695 | 597 | 978.5 | 368.79 | ||
| Difference | -82.50 | -94 | -253 | 30 | -143 | -0.5 | 88.72 | ||
| Difference significance | Z = 2.275, p = 0.023 | ||||||||
| INSECTS | I.V. | 1293.00 | 1122 | 552 | 2624 | 912.5 | 1620 | 559.87 | |
| M.V. | 1066.75 | 925.5 | 484 | 2300 | 777 | 1333 | 486.40 | ||
| Difference | 107.50 | 175.5 | -180 | 302 | -6.5 | 212 | 144.07 | ||
| Difference significance | Z = 2.118, p = 0.034 | ||||||||
| BF-7 | CENTER | I.V. | 310.58 | 265.5 | 159 | 636 | 217.5 | 398.5 | 139.31 |
| M.V. | 400.67 | 393 | 207 | 665 | 277 | 515 | 154.62 | ||
| Difference | 90.08 | 81.5 | -45 | 227 | 35.5 | 145.5 | 75.17 | ||
| Difference significance | Z = 2.746, p = 0.006 | ||||||||
| BALANCE | I.V. | 220.17 | 220 | 115 | 353 | 187 | 250.5 | 64.36 | |
| M.V. | 285.33 | 300.5 | 148 | 376 | 253 | 334 | 74.72 | ||
| Difference | 65.17 | 49 | 11 | 149 | 21.5 | 103 | 49.06 | ||
| Difference significance | Z = 3.059, p = 0.002 | ||||||||
| INSECTS | I.V. | 377.00 | 362.5 | 229 | 638 | 301.5 | 449 | 111.28 | |
| M.V. | 309.50 | 296.5 | 201 | 519 | 230 | 376 | 92.37 | ||
| Difference | 41.58 | 49.5 | -73 | 175 | 7 | 77.5 | 67.34 | ||
| Difference significance | Z = 1.922, p = 0.055 | ||||||||
| BF-8 | CENTER | I.V. | 467.58 | 387 | 221 | 1381 | 306.5 | 481 | 307.96 |
| M.V. | 511.58 | 425.5 | 247 | 1423 | 334 | 598 | 315.18 | ||
| Difference | 44.00 | 37.5 | -17 | 161 | 13.5 | 54.5 | 50.59 | ||
| Difference significance | Z = 2.667, p = 0.008 | ||||||||
| BALANCE | I.V. | 612.58 | 512 | 194 | 1654 | 397 | 711.5 | 374.80 | |
| M.V. | 611.83 | 535.5 | 227 | 1662 | 385 | 710.5 | 371.79 | ||
| Difference | -0.75 | 20.5 | -320 | 260 | -75 | 58.5 | 142.49 | ||
| Difference significance | Z = 0.157, p = 0.875 | ||||||||
| INSECTS | I.V. | 815.83 | 663.5 | 295 | 2698 | 496.5 | 869 | 625.78 | |
| M.V. | 726.42 | 684 | 184 | 2267 | 452 | 755.5 | 524.72 | ||
| Difference | -62.83 | -78 | -416 | 171 | -119.5 | 74.5 | 156.95 | ||
| Difference significance | Z = 1.334, p = 0.182 | ||||||||
| BF-9 | CENTER | I.V. | 663.58 | 484.5 | 120 | 1967 | 350.5 | 799.5 | 530.65 |
| M.V. | 613.58 | 536.5 | 130 | 1828 | 388.5 | 690 | 440.82 | ||
| Difference | -50.00 | 20 | -649 | 171 | -109.5 | 54.5 | 211.32 | ||
| Difference significance | Z = 0.078, p = 0.937 | ||||||||
| BALANCE | I.V. | 767.42 | 510.5 | 250 | 1849 | 434 | 990.5 | 554.76 | |
| M.V. | 698.58 | 501 | 243 | 1759 | 423.5 | 776.5 | 476.27 | ||
| Difference | -68.83 | -14.5 | -415 | 72 | -45 | -6.5 | 142.31 | ||
| Difference significance | Z = 2.275, p = 0.023 | ||||||||
| INSECTS | I.V. | 792.17 | 692 | 373 | 1716 | 504 | 1011 | 383.04 | |
| M.V. | 630.33 | 541.5 | 294 | 1664 | 442 | 698.5 | 363.36 | ||
| Difference | -120.25 | -63 | -473 | 129 | -224.5 | -4 | 173.86 | ||
| Difference significance | Z = 2.275, p = 0.023 | ||||||||
| BF-10 | CENTER | I.V. | 413.58 | 417.5 | 280 | 568 | 347 | 463.5 | 83.57 |
| M.V. | 427.92 | 418 | 276 | 695 | 317 | 486.5 | 131.69 | ||
| Difference | 14.33 | 23 | -116 | 237 | -34 | 35.5 | 86.38 | ||
| Difference significance | Z = 0.549, p = 0.583 | ||||||||
| BALANCE | I.V. | 446.08 | 445 | 220 | 674 | 335.5 | 549 | 138.46 | |
| M.V. | 448.00 | 407.5 | 212 | 845 | 328 | 528.5 | 176.75 | ||
| Difference | 1.92 | 1.5 | -197 | 229 | -14.5 | 26.5 | 97.63 | ||
| Difference significance | Z = 0.275, p = 0.784 | ||||||||
| INSECTS | I.V. | 472.83 | 439 | 309 | 780 | 383.5 | 549.5 | 133.60 | |
| M.V. | 364.17 | 364.5 | 196 | 534 | 293 | 430.5 | 94.53 | ||
| Difference | -64.42 | -30 | -259 | 54 | -162.5 | 25 | 109.06 | ||
| Difference significance | Z = 1.451, p = 0.147 | ||||||||
| Whole group: | CENTER | I.V. | 464.58 | 380 | 79 | 1967 | 242.5 | 577 | 343.02 |
| M.V. | 494.04 | 424.5 | 64 | 1828 | 288 | 629.5 | 332.94 | ||
| Difference | 29.46 | 30 | -649 | 251 | -9.5 | 62 | 118.11 | ||
| Difference significance | Z = 3.517, p = 0.0004 | ||||||||
| BALANCE | I.V. | 524.81 | 424 | 82 | 1849 | 226 | 674.5 | 421.57 | |
| M.V. | 509.43 | 398.5 | 63 | 1759 | 264 | 655.5 | 378.37 | ||
| Difference | -15.38 | -5 | -415 | 260 | -24 | 31.5 | 108.63 | ||
| Difference significance | Z = 0.676, p = 0.498 | ||||||||
| INSECTS | I.V. | 664.24 | 492.5 | 103 | 2698 | 346.5 | 820.5 | 512.26 | |
| M.V. | 543.86 | 413 | 87 | 2300 | 274 | 701.5 | 441.66 | ||
| Difference | -25.06 | -9.5 | -473 | 302 | -104.5 | 54.5 | 144.10 | ||
| Difference significance | Z = 1.252, p = 0.211 | ||||||||
Legend: CENTER: relaxation training module; BALANCE: concentration training module; INSECTS: self-regulation training module; I.V.: initial measurement value (kOhm); M.V.: mean measurement value for the entire task (kOhm); Difference: a difference between I.V. and M.V.; Z: a result of the Wilcoxon signed-rank test; p: statistical significance. BF-2, BF-3, BF-7, BF-8, BF-9, BF-10: randomly selected patients from the Biofeedback group (patient code).
The analyses were based on 12 measurements for each patient. For patient BF-2, no statistically significant changes in the CENTER measurements (Z = 1.020, p = 0.308) were observed during the exercise, but such changes did occur when the patient did the BALANCE exercise (Z = 2.589, p = 0.010), in which a decrease was visible in the measured values, indicating activation. For the INSECTS module, statistically significant changes were noted (Z = 2.490, p = 0.013) during the exercise, associated with a reduction in measured values. The above data suggest that the patient did not achieve relaxation when training with the CENTER module but did achieve an improvement in concentration and self-regulation when doing the BALANCE and INSECTS exercises, respectively. Also, in case of patient BF-3, no statistically significant changes in the CENTER measurements were noted (Z = 1.336, p = 0.182) during the exercise, but such changes did occur when the BALANCE module was used (Z = 2.275, p = 0.023), for which a decrease was visible in the measured values, indicating activation. Statistically significant changes were also noted (Z = 2.118, p = 0.034) during the INSECTS exercise, which were associated with a reduction in measured values. The above data suggests that the patient did not achieve relaxation during the exercises using the CENTER module but did achieve an improvement in concentration and self-regulation when training in the BALANCE and INSECTS modules, respectively. Similarly, in case of patient BF-9, no statistically significant changes in the CENTER measurements were observed (Z = 0.078, p = 0.937) during the exercise, in contrast to the BALANCE exercise (Z = 2.275, p = 0.023), during which a decrease in the difference in values, representing activation, was noted. Statistically significant changes, associated with a reduction in the measured values, were also found for the INSECTS module (Z = 2.275, p = 0.023). The above data suggests that during the exercises in the CENTER module, the patient did not achieve relaxation, but training in the BALANCE and INSECTS modules improved the patient's concentration and self-regulation.
In the case of patient BF-7, statistically significant increases in the CENTER measurements (Z = 2.746, p = 0.006) and the BALANCE measurements (Z = 3.059, p = 0.002) were observed during training, which indicated that relaxation and an improvement in concentration were achieved. For the INSECTS module, no statistically significant changes were noted (Z = 1.922, p = 0.055) during the exercise, which meant that the patient achieved lower values of the parameters measured, which pointed to problems with self-regulation. For patient BF-8, statistically significant changes were noted in the CENTER measurements (Z = 2.667, p = 0.008) during exercises, but no such changes were seen for the BALANCE (Z = 0.157, p = 0.875) and INSECTS (Z = 1.334, p = 0.182) modules. The above data indicates that during the BALANCE and INSECTS exercises, the patient achieved lower values of the parameters measured, which were indicative of problems with self-regulation and concentration. The higher differences in measured values for the CENTER module are suggestive of increased relaxation.
In case of patient BF-10, no statistically significant changes during training were noted in the CENTER (Z = 0.549, p = 0.583), BALANCE (Z = 0.275, p = 0.784), and INSECTS (Z = 1.451, p = 0.147) measurements. The above data indicates that the parameters measured increased during training in the CENTER and BALANCE modules, indicating that the patient had problems with relaxation and concentration, respectively. A decrease in the measured values during the INSECTS exercise was reflective of problems with self-regulation.
The obtained data imply that in two out of the six patients, the values of the parameters measured increased significantly after the CENTER exercise, which means that the exercise helped the subjects relax. In four out of the six patients, the values of the parameters measured decreased significantly after exercises in the BALANCE module, which indicated an improvement in concentration (reduced relaxation). In three out of the six patients, the values of the parameters measured decreased significantly after the INSECTS exercise, showing that it had a positive effect on the level of self-regulation. Details regarding the effects of the therapy together with the type of changes observed are shown in Table 3.
Table 3.
Therapy effects and the type of change that occurred in the studied group by training module.
| Patient: CODE |
Change type | CENTER | BALANCE | INSECTS | |||
|---|---|---|---|---|---|---|---|
| Number of measurements | % | Number of measurements | % | Number of measurements | % | ||
| BF-2 (12 measurements) | Relaxation (increase in value) | 7 | 58.33 | 3 | 25.00 | 1 | 8.33 |
| No change in value | 0 | 0.00 | 0 | 0.00 | 1 | 8.33 | |
| Activation (decrease in value) | 5 | 41.67 | 9 | 75.00 | 10 | 83.33 | |
| BF-3 (12 measurements) | Relaxation (increase in value) | 7 | 58.33 | 3 | 25.00 | 9 | 75.00 |
| Activation (decrease in value) | 5 | 41.67 | 9 | 75.00 | 3 | 25.00 | |
| BF-7 (12 measurements) | Relaxation (increase in value) | 11 | 91.67 | 12 | 100.00 | 10 | 83.33 |
| Activation (decrease in value) | 1 | 8.33 | 0 | 0.00 | 2 | 16.67 | |
| BF-8 (12 measurements) | Relaxation (increase in value) | 10 | 83.33 | 7 | 58.33 | 4 | 33.33 |
| Activation (decrease in value) | 2 | 16.67 | 5 | 41.67 | 8 | 66.67 | |
| BF-9 (12 measurements) | Relaxation (increase in value) | 8 | 66.67 | 1 | 8.33 | 3 | 25.00 |
| Activation (decrease in value) | 4 | 33.33 | 11 | 91.67 | 9 | 75.00 | |
| BF-10 (12 measurements) | Relaxation (increase in value) | 8 | 66.67 | 7 | 58.33 | 5 | 41.67 |
| Activation (decrease in value) | 4 | 33.33 | 5 | 41.67 | 7 | 58.33 | |
| Total (72 measurements) | Relaxation (increase in value) | 51 | 70.83 | 33 | 45.83 | 32 | 44.44 |
| No change in value | 0 | 0.00 | 0 | 0.00 | 1 | 1.39 | |
| Activation (decrease in value) | 21 | 29.17 | 39 | 54.17 | 39 | 54.17 | |
The data shows that during the GSR Biofeedback training, measurements recorded in 71% of the patients were associated with relaxation in the CENTER module, in 54% of the patients the measurements were associated with activation in the BALANCE module, and in 54% of the patients, they were associated with activation in the INSECTS module. Activation and relaxation were understood as any, even the smallest, change in the measured values.
In a further part of the study, a trend determined on the basis of the mean initial measurement values (I.V.) calculated at the beginning of each session on a given day of experiment was analysed. Spearman's correlation coefficient was used to evaluate the trend measured (Table 4). The analysis indicates that there is a statistically significant increasing trend in four (out of the six) randomly studied patients (BF-2, BF-3, BF-7, BF-9). The positive correlation coefficient indicates that with the successive measurements, the mean initial measurement value (I.V.) increased.
Table 4.
Trend determined on the basis of the mean I.V. measurements on a given day.
| Patient CODE | R S | p |
|---|---|---|
| BF-2 | 0.769 | 0.003 |
| BF-3 | 0.797 | 0.002 |
| BF-7 | 0.692 | 0.013 |
| BF-8 | 0.364 | 0.245 |
| BF-9 | 0.825 | 0.001 |
| BF-10 | 0.483 | 0.112 |
R S: Spearman's correlation coefficient; p: statistical significance.
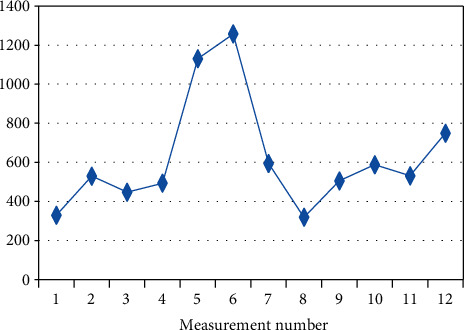
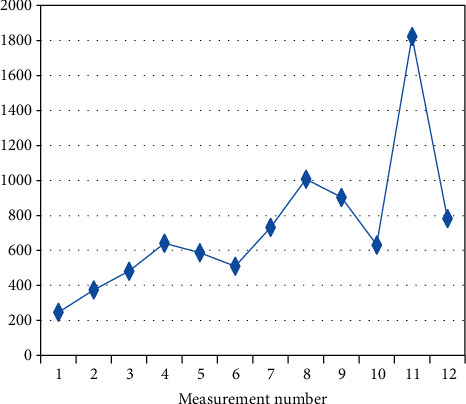
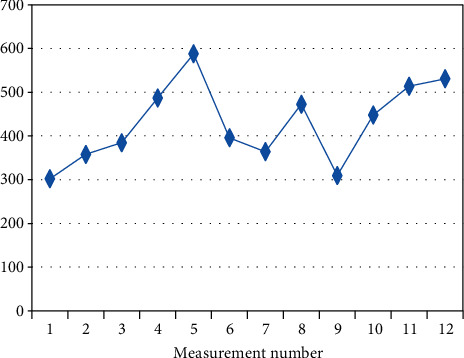
The figures below present changes in the mean initial values of I.V. measurements in the individual patients on a given day (Figures 2–7).
Figure 2.
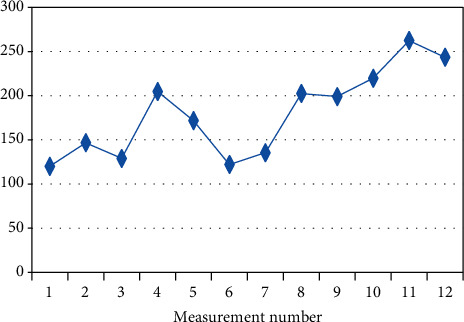
Changes in the mean measurement values (I.V.) in patient BF-2 (Rs = 0.769, p = 0.003) on a given day.
Figure 3.
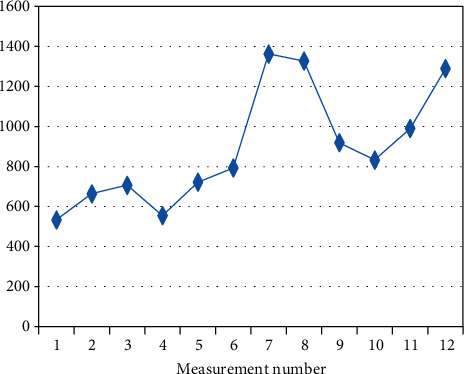
Changes in the mean measurement values (I.V.) in patient BF-3 (Rs = 0.797, p = 0.002) on a given day.
Figure 4.
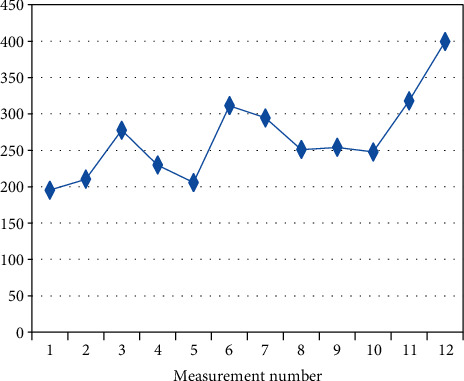
Changes in the mean measurement values (I.V.) in patient BF-7 (Rs = 0.692, p = 0.013) on a given day.
Figure 5.
Changes in the mean measurement values (I.V.) in patient BF-8 (Rs = 0.364, p = 0.245) on a given day.
Figure 6.
Changes in the mean measurement values (I.V.) in patient BF-9 (Rs = 0.825, p = 0.001) on a given day.
Figure 7.
Changes in the mean measurement values (I.V.) in patient BF-10 (Rs = 0.483, p = 0.112) on a given day.
5. Discussion
The present preliminary study of GSR Biofeedback as a neurorehabilitation method shows that it is an interesting option that might be employed to supplement pharmacotherapy in schizophrenia patients. As the initial results indicate, the therapy effectively improves cognitive processes, which implies that it can also improve concentration and self-regulation, as well as reducing tension, anxiety, and fear. The obtained data based on the self-regulation process are confirmed by other authors, including Birbaumer et al. [38] and Mathiak et al. [39], who compared this process to a mechanism associated with learning and instrumental conditioning based on reinforcing and rewarding specific behaviours. Those authors are of the opinion that the dopaminergic system is involved in the coding of the reward pathway (substantia nigra—SN/tegmental area—VTA), playing an important role in self-regulation during the whole training process.
A similar opinion was presented by Sulzer, who emphasised a positive correlation between SN/VTA regulation, skin conductance (GSR), and emotional stimulation. According to this author, this correlation provides evidence for a positive effect of the therapy and a “control over secretion of endogenous dopamine” [40]. Stoeckel et al. (2014) are of the opinion that the appropriately selected Neurotherapy methods are a prerequisite for improvement in cognitive functions, “inducing a process of the brain function transformation” and influencing overall functioning [41]. Koush and colleagues state that “brain training” can be understood as positively acquired behavioural feedback improving psychical function and developing the functional network of the brain through visual exercises [42].
The high effectiveness of Biofeedback therapy is also emphasised by other authors, who note that regulation of brain waves based on regular training reduces fear, anxiety, and stress levels, that is, those symptoms which are frequently a problem for patients with mental disorders [43–45]. It is possible that this relationship is an effect of mental status modulation, and the process of instrumental conditioning is associated with morphological and functional changes in dendrites and neuroplasticity of the brain [46].
The preliminary results presented in this paper appear to confirm this process, as four (out of the six) participants subjected to training using GSR Biofeedback, obtained positive therapy outcomes, and the statistically significant increasing trend showed that the mean initial value (I.V.) of the measurements increased with each successive training session. The study indicates that in two out of the six subjects, a statistically significant increase in the measured values occurred during exercises in the CENTER module, which indicated that relaxation was achieved by those patients. In three patients, a statistically significant drop in measured values was noted after they had done the BALANCE exercise, which was reflective of an improvement in concentration. In three patients, a statistically significant drop in measured values was noted after the INSCECTS exercise, which was indicative of an improvement in self-regulation.
Possibly, each successive exercise performed in the individual modules resulted in regular improvement, and changes in action potentials (sprouting process) released the so-called priming process (long-term potentiation—LTP) and a sequential cycle for the formation of new chemical synaptic connections. In consequence, the cyclic training sessions led to positive therapy outcomes [44, 46, 47].
The positive effect of the therapy confirms the inverse relationship between the central and the autonomic activities, as discussed, among others, by Lim. The author noted a negative correlation between the amplitude of SCRs and the amplitudes of the N200 potential and of alpha and beta waves [45]. A similar opinion is presented by Campo [27], who found a negative correlation between SCRs and exacerbation of schizophrenia symptoms (positive and negative), and by Iacono [48], who observed a relationship between electrodermal activity and the alpha (drop) and delta (increase) rhythms. This inverse correlation indicates that modulation of the patient's mental condition based on GSR Biofeedback influences cortical transformation, and the positive effect of the therapy manifests as the reduction of adverse symptoms and improvement in coherence, as demonstrated in the present preliminary study.
Our study has some limitations which are mostly related to the model of apparatus which was used in GSR Biofeedback training and limited electrodermal measurements possible. Other limitations in this study include the small sample size and the use of convenience sampling methodology.
6. Conclusions
According to the results of this present pilot study, GSR Biofeedback may be considered as a new neurorehabilitation technique that could complement pharmacological treatment of patients diagnosed with schizophrenia, improving their individual capabilities and social functioning using their own resources.
Undoubtedly, further studies in a larger cohort are needed to formulate sound and consistent conclusions. The present study was a pilot experiment, but it already provided promising results, which warrant further investigation. From the point of view of the mentally ill patient, every method that can improve their social functioning and quality of life is worth exploring.
Acknowledgments
This research was funded by the Ministry of Science and Higher Education of the Republic of Poland, funds for statutory activities (grant number 550).
Data Availability
All data is available with the authors on reasonable request.
Conflicts of Interest
The authors declare that there is no conflict of interest.
References
- 1.Kahn R. Why Kraepelin was right: schizophrenia as a cognitive disorder. Neuropsychiatry and Neurophisiology. 2014;9(2):41–47. (in Polish) [Google Scholar]
- 2.Widiger T., Samuel D. Diagnostic categories or dimensions? A question for the diagnostic and statistical manual of mental disorders-fifth edition. Journal of Abnormal Psychology. 2005;114(4):494–504. doi: 10.1037/0021-843X.114.4.494. [DOI] [PubMed] [Google Scholar]
- 3.Heaton R., Gladsjo J., Palmer B., Kuck J., Marcotte T., Jeste D. Stability and course of neuropsychological deficits in schizophrenia. Archives of General Psychiatry. 2001;58(1):24–32. doi: 10.1001/archpsyc.58.1.24. [DOI] [PubMed] [Google Scholar]
- 4.Harvey P. Cognitive impairment in elderly patients with schizophrenia: age related changes. International Journal of Geriatric Psychiatry. 2001;16(1):78–85. doi: 10.1002/1099-1166(200112)16:1+<::aid-gps565>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 5.Bralet M., Navarre M., Eskenazi A., Lucas-Ross M., Falissard B. Interest of a new instrument to assess cognition in schizophrenia: the brief assessment of cognition in schizophrenia (BACS) Encephale. 2008;34(6):557–562. doi: 10.1016/j.encep.2007.12.005. [DOI] [PubMed] [Google Scholar]
- 6.Censits D., Ragland J., Gur R. Neuropsychological evidence supporting a neurodevelopmental model of schizophrenia: a longitudinal study. Schizophrenia Research. 1997;24(3):289–298. doi: 10.1016/S0920-9964(96)00091-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoff P., Beer D. Introductory remarks on the translation of Emil Kraepelins paper Die Erscheinungsformen des Irreseins (1920) History of Psychiatry. 1992;3(12):499–503. doi: 10.1177/0957154X9200301206. [DOI] [PubMed] [Google Scholar]
- 8.Mohamed S., Paulsen J., O’Leary D., Arndts S., Andreasen N. Generalized cognitive deficits in schizophrenia: a study of first-episode patients. Archives of General Psychiatry. 1999;56(8):749–754. doi: 10.1001/archpsyc.56.8.749. [DOI] [PubMed] [Google Scholar]
- 9.Riley E. M., McGovern D., Mockler D., et al. Neuropsychological functioning in first-episode psychosis -- evidence of specific deficits. Schizophrenia Research. 2000;43(1):47–55. doi: 10.1016/S0920-9964(99)00177-2. [DOI] [PubMed] [Google Scholar]
- 10.Saykin A., Shtasel D., Gur R., et al. Neuropsychological deficits in neuroleptic naive patients with First-Episode schizophrenia. Archives of General Psychiatry. 1994;51(2):124–131. doi: 10.1001/archpsyc.1994.03950020048005. [DOI] [PubMed] [Google Scholar]
- 11.Schuepbach D., Keshavan M., Kmiec J., Sweeney J. Negative symptom resolution and improvements in specific cognitive deficits after acute treatment in first-episode schizophrenia. Schizophrenia Research. 2002;53(3):249–261. doi: 10.1016/S0920-9964(01)00195-5. [DOI] [PubMed] [Google Scholar]
- 12.Townsend L., Malla A., Norman R. Cognitive functioning in stabilized first-episode psychosis patients. Psychiatry Research. 2001;104(2):119–131. doi: 10.1016/S0165-1781(01)00302-X. [DOI] [PubMed] [Google Scholar]
- 13.Addington D., Addington J., Robinson G. Attributional style and depression in schizophrenia. Canadian Journal of Psychiatry. 1999;44(7):697–700. doi: 10.1177/070674379904400708. [DOI] [PubMed] [Google Scholar]
- 14.Witkowska-Łuć B. Schizofrenia i poczucie koherencji (Schisophrenia and sense of coherence) Psychiatria Polska. 2017;73:1–10. doi: 10.12740/PP/OnlineFirst/69697. (in Polish) [DOI] [PubMed] [Google Scholar]
- 15.Braithwaite J., Watson D., Jones R., Rowe M. Przewodnik do analizy aktywności elektrotermicznej (EDA) i odpowiedzi przewodnictwa skóry (SCRs) do eksperymentów psychologicznych [A guide for analysing electrodermal activity (EDA) and skin conductance responses for psychological experiments] Psychofizjologia. 2013;49:1017–1034. [Google Scholar]
- 16.Singh R., Conjeti S., Benerjee R. A comparative evaluation of neural network classifiers for stress level analysis of automotive drivers using physiological signals. Biomedical Signal Processing and Control. 2013;8(6):740–754. doi: 10.1016/j.bspc.2013.06.014. [DOI] [Google Scholar]
- 17.Chattopadh P., Bond A., Lader M. Characteristics of galvanic skin response in anxiety states. Journal of Psychiatric Research. 1975;12(4):265–270. doi: 10.1016/0022-3956(75)90005-9. [DOI] [Google Scholar]
- 18.Crider A. Personality and electrodermal response lability: an interpretation. Applied Psychophysiology and Biofeedback. 2008;33(3):141–148. doi: 10.1007/s10484-008-9057-y. [DOI] [PubMed] [Google Scholar]
- 19.Williams K., Iacono W., Remick R. Electrodermal activity among subtypes of depression. Biological Psychiatry. 1985;20(2):158–162. doi: 10.1016/0006-3223(85)90075-7. [DOI] [PubMed] [Google Scholar]
- 20.Jandl M., Steyer J., Kaschka W. Suicide risk markers in major depressive disorder: a study of electrodermal activity and event-related potentials. Journal of Affective Disorders. 2010;123(1-3):138–149. doi: 10.1016/j.jad.2009.09.011. [DOI] [PubMed] [Google Scholar]
- 21.Thorell L., Wolfersdorf M., Straub R., Steyer J., Hodgkinson S., Kaschka W. Electrodermal hyporeactivity as a trait marker for suicidal propensity in uni- and bipolar depression. Journal of Psychiatric Research. 2013;47(12):1925–1931. doi: 10.1016/j.jpsychires.2013.08.017. [DOI] [PubMed] [Google Scholar]
- 22.Corvell W. Clinical assessment of suicide risk in depressive disorder. CNS Spectrums. 2006;11(6):455–461. doi: 10.1017/S109285290001467X. [DOI] [PubMed] [Google Scholar]
- 23.Iacono W., Lykken D., Peloquin L. Electrodermal activity in euthymic unipolar and bipolar affective disorders. Archives of General Psychiatry. 1983;40(5):557–565. doi: 10.1001/archpsyc.1983.01790050083010. [DOI] [PubMed] [Google Scholar]
- 24.Schneider D., Regenbogen C., Kellermann T., et al. Empathic behavioral and physiological responses to dynamic stimuli in depression. Psychiatry Research. 2012;200(2-3):294–305. doi: 10.1016/j.psychres.2012.03.054. [DOI] [PubMed] [Google Scholar]
- 25.Brekke J., Raine S., Ansel M. Neuropsychological and psychophysiological correlates of psychosocial functioning in schizophrenia. Schizophrenia Bulletin. 1997;23(1):19–28. doi: 10.1093/schbul/23.1.19. [DOI] [PubMed] [Google Scholar]
- 26.Schell A., Dawson M., Rissling A., et al. Electrodermal predictors of functional outcome and negative symptoms in schizophrenia. Psychophysiology. 2005;42(4):483–492. doi: 10.1111/j.1469-8986.2005.00300.x. [DOI] [PubMed] [Google Scholar]
- 27.Campo J., Merkelbach H., Nijman H., Yeates-Frederikx M., Allertz W. Skin conductance and schizophrenic symptomatology. Acta Neuropsychiatr. 2000;12(4):177–182. doi: 10.1017/S0924270800035353. [DOI] [PubMed] [Google Scholar]
- 28.Arns M., Batail J.-M., Bioulac S., et al. Neurofeedback en psychiatrie : une technique du present ? Encephale. 2017;43(2):135–145. doi: 10.1016/j.encep.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 29.Omejc N., Rojc B., Battaglini P., Marusic U. Review of the therapeutic neurofeedback method using electroencephalography: EEG Neurofeedback. Bosnian Journal of Basic Medical Sciences. 2019;19(3):213–220. doi: 10.17305/bjbms.2018.3785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Markiewicz R., Masiak J. Evaluation of cognitive deficits in schizophrenia using event-related potentials and rehabilitation influences using EEG biofeedback in patients diagnosed with schizophrenia. Psychiatria Polska. 2019;53(6):1261–1273. doi: 10.12740/PP/OnlineFirst/102622. [DOI] [PubMed] [Google Scholar]
- 31.Chen T., Lin I. The learning effects and curves during high beta down-training neurofeedback for patients with major depressive disorder. Journal of Affective Disorders. 2020;266:235–242. doi: 10.1016/j.jad.2020.01.175. [DOI] [PubMed] [Google Scholar]
- 32.Micoulaud Franchi J., Jeunet C., Lotte F. Neurofeedback: a challenge for integrative clinical neurophysiological studies. Clin Neurophisiol. 2020;50(1):1–3. doi: 10.1016/j.neucli.2020.01.001. [DOI] [PubMed] [Google Scholar]
- 33.Batail J., Bioulac S., Cabestaing F., et al. EEG neurofeedback research: A fertile ground for psychiatry? Encephale. 2019;45(3):245–255. doi: 10.1016/j.encep.2019.02.001. [DOI] [PubMed] [Google Scholar]
- 34.Gruzelier J. Clinical attributes of schizophrenic skin conductance responders and non-responders. Psychological Medicine. 1976;6(2):245–249. doi: 10.1017/S0033291700013787. [DOI] [PubMed] [Google Scholar]
- 35.Bernstein A., Frith C., Gruzelier J., et al. An analysis of the skin conductance orienting response in samples of American, British, and German schizophrenics. Biological Psychology. 1982;14(3-4):155–211. doi: 10.1016/0301-0511(82)90001-1. [DOI] [PubMed] [Google Scholar]
- 36.Sławiński A. Instrukcja obsługi VERIM (R) Personal Edition & ProNet wersja 3.6 [Instruction Manual. VERIM (R) Personal Edition & ProNet version 3.6] 2017. https://verim.pl/wp-content/uploads/2017/05/VERIM-Polski-2017-11-02.pdf accessed 17.05.2021.
- 37.Linksman R. W jaki sposób szybko się uczyć [How to Learn Anything Quickly?] Warszawa: Wydawnictwo Świat Książki; 2005. [Google Scholar]
- 38.Birbaumer N., Ruiz S., Sitaram R. Learned regulation of brain metabolism. Trends in Cognitive Sciences. 2013;17(6):295–302. doi: 10.1016/j.tics.2013.04.009. [DOI] [PubMed] [Google Scholar]
- 39.Mathiak K., Koush Y., Dyck M., et al. Social reinforcement can regulate localized brain activity. European Archives of Psychiatry and Clinical Neuroscience. 2010;260(S2):132–136. doi: 10.1007/s00406-010-0135-9. [DOI] [PubMed] [Google Scholar]
- 40.Sulzer J., Sitaram R., Blefari M., et al. Neurofeedback-mediated self-regulation of the dopaminergic midbrain. NeuroImage. 2013;1(75):176–184. doi: 10.1016/j.neuroimage.2013.02.041. [DOI] [PubMed] [Google Scholar]
- 41.Stoeckel L., Garrison K., Ghosh S. Optimizing real time fMRI neurofeedback for therapeutic discovery and development. NeuroImage- Clin. 2014;5:245–255. doi: 10.1016/j.nicl.2014.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Koush Y., Rosa M., Robineau F., et al. Connectivity-based neurofeedback: dynamic causal modeling for real-time fMRI. NeuroImage. 2013;1(81):422–430. doi: 10.1016/j.neuroimage.2013.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Trousselard M., Canini F., Claverie D., Cunqui C., Putois B., Franck N. Cardiac coherence training to reduce anxiety in remitted schizophrenia, a pilot study. Applied Psychophysiology and Biofeedback. 2016;41(1):61–69. doi: 10.1007/s10484-015-9312-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Maren S. Synaptic Mechanisms of Associative Memory in the Amygdala. Neuron. 2005;47(6):783–786. doi: 10.1016/j.neuron.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 45.Lim C., Gordon E., Rennie C., Wright J. Dynamics of SCR, EEG and ERP activity in an oddball paradigm with short interstimulus intervals. Psychophysiology. 1999;36(5):543–551. doi: 10.1111/1469-8986.3650543. [DOI] [PubMed] [Google Scholar]
- 46.Kossut M. Mechanizmy plastyczności mózgu [Mechanisms of brain plasticity] Warszawa, Poland: PZWL; 1993. (in Polish) [Google Scholar]
- 47.Chapman P., Kairis E., Keenan C. Long-term synaptic potentiation in the amygdala. Synapse. 1990;6(3):271–278. doi: 10.1002/syn.890060306. [DOI] [PubMed] [Google Scholar]
- 48.Iacono W. Bilateral electrodermal habituation-dishabituation and resting EEG in remitted schizophrenics. The Journal of Nervous and Mental Disease. 1982;170(2):91–101. doi: 10.1097/00005053-198202000-00005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data is available with the authors on reasonable request.


