Abstract
The impact of different sociodemographic and clinical characteristics on the COVID-19-related morbidity and mortality rates have been studied extensively around the world; however, there is a dearth of data on the impact of different clinical and sociodemographic variables on the COVID-19-related outcomes in Saudi Arabia. This study aimed to identify those at high risk of worse clinical outcomes, such as hospitalization and longer length of stay (LOS) among young and middle-aged adults (18 to 55 years). In this questionnaire-based cross-sectional study, 706 patients with real-time polymerase chain reaction (RT-PCR) confirmed COVID-19 infection were interviewed. Patients’ demographic characteristics, dietary habits, medical history, and lifestyle choices were collected through phone interviews. Patients with chronic health conditions, such as diabetes and hypertension, reported a higher rate of hospitalization, ICU admission, oxygen-support needs, and a longer period of recovery and LOS. Multiple logistic regression showed that diabetes, hypertension, and pulmonary disease (e.g., asthma and chronic obstructive pulmonary disease (COPD)) were associated with a higher risk of hospitalization and longer LOS. Multiple logistic regression showed that symptoms of breathlessness, loss of smell and/or taste, diarrhea, and cough were associated with a longer recovery period. Similarly, breathlessness, vomiting, and diarrhea were associated with higher rates of hospitalization. The findings of this study confirm the similarity of the factors associated with worse clinical outcomes across the world. Future studies should use more robust designs to investigate the impact of different therapies on the COVID-19-related morbidity and mortality in Saudi Arabia.
Keywords: COVID-19, Coronavirus, SARS-CoV-2, Hypertension, Diabetes, Saudi Arabia
1. Introduction
Coronavirus disease 2019 (COVID-19) is an infectious disease that has spread to >200 countries with approximately 46 million confirmed cases and over 1.2 million deaths globally (Kroumpouzos et al., 2020). The disease affects the upper respiratory tract and is caused by a newly discovered strain of severe acute respiratory syndrome coronavirus (SARS-CoV-2) (Subbarao and Mahanty, 2020). In the past two decades, Coronavirus, a single-stranded RNA virus known for mild infections in humans and animals, caused two major breakouts. Acute respiratory syndrome coronavirus occurred in 2002–2003 (SARS-CoV) and middle east respiratory syndrome coronavirus (MERS-CoV) in 2012 with 10% and 36% mortality rates, respectively (Chen et al., 2020a, Hussain et al., 2020, Ksiazek et al., 2003).
According to preliminary international COVID-19 reports, the clinical manifestations are heterogeneous. The most common comorbidities reported in COVID-19 patients are diabetes (10–12%), hypertension (10–15%), and other vascular and cerebrovascular diseases (7–40%) (Alguwaihes et al., 2020, Almalki et al., 2020, Al Mutair et al., 2020, Al-Omari et al., 2020, Alqahtani et al., 2020, Guan et al., 2020, Huang et al., 2020, Li et al., 2020a, Liu et al., 2020, Sanyaolu et al., 2020, Shah et al., 2020, Sheshah et al., 2021, Wang et al., 2020a, Xu et al., 2020). Various studies have indicated that 20–51% of COVID-19 patients have at least one comorbidity (Guan et al., 2020, Huang et al., 2020, Li et al., 2020a, Liu et al., 2020, Sanyaolu et al., 2020, Schoen et al., 2019, Shah et al., 2020, Wang et al., 2020b, Wang et al., 2020a, Xu et al., 2020). Patient comorbidities have been associated with an increase in severity and mortality of viral infections including pandemic influenza A (H1N1) (Schoen et al., 2019), SARS-CoV (Chen et al., 2020b, Clark et al., 2020, Wang et al., 2020c, Yang et al., 2006, Yu et al., 2006), and MERS-CoV (Badawi and Ryoo, 2016, Banik et al., 2016). A systemic review of 4881 COVID-19 cases from different hospitals in China showed that the number of severe cases was significantly higher in patients with comorbidities than patients without comorbidities (Z. Wang et al., 2020). Hypertension was the most common comorbidity among severe cases (33.4%) followed by diabetes (14.4%) and other cardiovascular diseases (10.4%) (Z. Wang et al., 2020). In another study, hospitalized COVID-19 patients with comorbidities who were admitted to the ICU exceeded those admitted without comorbidities by two-folds (B. Li et al., 2020).
Determining the prevalence of the most commonly encountered underlying diseases can help to identify those at the highest risk for more severe complications and worse outcomes. To the best of our knowledge, there are limited national studies evaluating the demographic and baseline comorbidities of COVID-19 patients in Saudi Arabia. The objective of this study was to describe the demographics and baseline comorbidities of young and middle-aged (18–55 years) COVID-19 patients in Saudi Arabia. Furthermore, we evaluated the impact of these comorbidities on patient recovery periods, the severity of symptoms, and hospital admissions.
2. Materials and methods
2.1. Ethical approval
This study was approved by the Central Institutional Review Board Committee of Ministry of Health (Central IRB-MoH), Kingdom of Saudi Arabia (KSA) (IRB log No: 20-11E-date 17-06-2020).
2.2. Data source
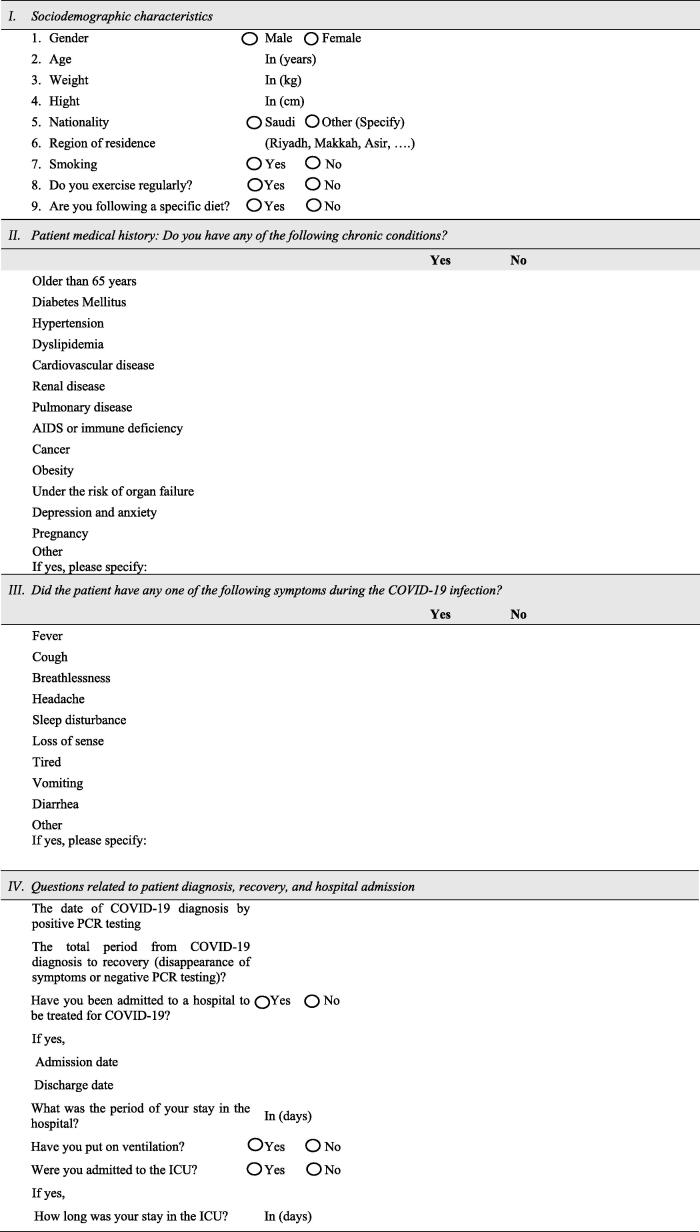
A cross-sectional study was conducted by interviewing recovered COVID-19 patients. Data of recruited patients from different regions of Saudi Arabia were obtained from the Saudi MoH registry of COVID-19 patients. Patient diagnosis with COVID-19 was confirmed by polymerase chain reaction (PCR) at MoH facilities between 1 May −30 June 2020. Patients were interviewed by three healthcare professionals using a newly developed data collection sheet that inquired about patient demographics, dietary habits, medical history, and lifestyle choices (Appendix A).
2.3. Data collection
Patient baseline sociodemographic characteristics and contact information were retrieved from the Saudi MOH registry of COVID-19 patients. Patient consent to participate in the study was obtained prior to starting each interview. Three healthcare professionals interviewed patients over the phone. The three healthcare professionals involved in data collection were trained using role-playing and a data collection protocol. Patient responses were recorded, and the data was stored in a safe and secure place. Only the investigators had access to the data, and the study adhered to the ethical principles of the Helsinki declaration. Each patient interview lasted between 15 and 20 min. Asymptomatic patients as well as those over the age of 55 years were excluded. The recovery period was defined as the time from diagnosis of COVID-19 with a positive PCR test until the disappearance of symptoms.
2.4. Methods of data analysis
Data was entered into an appropriately designed excel sheet. All statistical analyses were carried out using SPSS for windows version 25.0 (SPSS, Inc, Chicago. IL, USA). Missing values and outliers were identified and complemented by contacting the recovered patients prior to the statistical analysis process. Descriptive statistics, including frequency and percentage tables, graphs, means, and standard deviation (SD), were conducted for data presentation. Parametric tests, such as t test and analysis of variance (ANOVA), non-parametric tests, such as Mann-Whitney U and Kruskal–Wallis tests, for non-normal variables, correlation analysis, and multiple linear and logistic regressions were conducted as appropriate to examine the impact of age, gender, and different comorbidities on the recovery period, length of stay (LOS), and incidence of hospitalization. For categorical variables, Chi-square test was used. All hypotheses were tested at the 5% level of significance.
3. Results
3.1. Patient demographics
A random sample of 899 out of 117,882 recovered COVID-19 patients was selected using Microsoft Excel® spreadsheet software. However, 706 patients (78.53%) met the inclusion criteria and consented to participate in the study. The mean age was 33.0 ± 18.0 and the majority were male (57.6%). All patients were residents of Saudi Arabia and from different regions (northern, southern, eastern, western, and central). Twenty-five percent of patients were from Riyadh (central region), 22% from Makkah (western region), 22.4% from the Eastern region, 15% from the Asir region (southern region), and the remaining were from other parts of the country. The majority of patients (77.1%) were Saudi nationals, non-smokers (87.3%), and non-obese (94%). The patients’ average body weight was 78.1 ± 19.8 kg and the mean body mass index (BMI) was 28.2 ± 7.1. Approximately 30% of patients had at least one pre-existing medical condition (Table 1). The most common comorbidities were diabetes (9.6%), hypertension (7.4%), pulmonary diseases (7.9%), dyslipidemia (3.5%), and<1% of the participants had cancer (Table 1). The frequency and percentage distribution of respondents by the number of comorbidities are presented in Table 1. Approximately 21% of individuals had one chronic health condition, 6.2% had two comorbidities, and 3.1% had more than two comorbidities.
Table 1.
Demographics, comorbidities and symptoms in COVID-19 patients in Saudi Arabia.
| Variable | No. (%) | Variable (continued) | No. (%) |
|---|---|---|---|
| Demographic information | Smoking status | ||
| Total Number | 706 | Smoker | 90 (12.7) |
| Age, median [range] y | 33, [18, 55] | Non-smoker | 616 (87.3) |
| Sex | Number of comorbidities | ||
| Male | 407 (57.6) | None | 492 (69.7) |
| Female | 299 42.4) | 1 | 148 (21.0) |
| Nationality | 2 | 44 (6.2) | |
| Saudi | 544 (77.1) | >2 | 22 (3.1) |
| Non-Saudi | 162 (22.9) | Symptoms | |
| Comorbidities | Fever | 507 (71.8) | |
| Diabetes | 68 (9.6) | Fatigue | 450 (63.7) |
| Hypertension | 52 (7.4) | Loss of sense and smell | 447 (63.6) |
| Dyslipidemia | 25 (3.5) | Headache | 368 (52.1) |
| Cardiovascular diseases | 21 (3.0) | Cough | 296 (41.9) |
| Renal disease | 6 (0.8) | Breathlessness | 285 (40.4) |
| Pulmonary diseases | 56 (7.9) | Diarrhea | 267 (37.8) |
| Cancer | 5 (0.7) | Sleep disturbance | 194 (27.5) |
| Obesity | 42 (5.9) | Vomiting | 115 (16.3) |
| Depression | 15 (2.1) |
Most patients reported at least one of the following symptoms: fever (71.8%), fatigue (63.7%), loss of taste and/or smell (63.6%), headache (52.1%), cough (41.9%), breathlessness (40.4%), diarrhea (37.8%), sleep disturbances (27.5%), and vomiting (16.3%) (Table 1).
3.2. Effect of comorbidities on COVID-19 patients’ recovery period
The mean recovery period per day was remarkably longer for patients with comorbidities than patients without comorbidities, and the total number of patients who were admitted to hospitals was 197 patients (Table 2). Overall, the mean recovery period per day from COVID-19 for individuals with at least one chronic health condition was 14.1 ± 8.8 compared to 11.8 ± 8.9 for individuals without any underlying diseases (p < 0.001) (Table 3).
Table 2.
Univariate analysis of COVID-19 patients’ mean recovery period, hospital admission, ICU admission, patient need for an oxygen ventilator, and length of hospital stay by comorbidity.
| Diabetes | Hypertension | Dyslipidemia | Cardiovascular | Renal | Pulmonary | Cancer | Obesity | Deprerssion | At least one comorbidity | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Recovery Period | Cases with comorbidity (days, mean ± SD) | 15.0 ± 10.8 | 15.8 ± 9.9 | 15.1 ± 7.5 | 16.1 ± 10.3 | 15.2 8.5 | 15.8 ± 9.4 | 13 ± 8.3 | 13.2 ± 8.3 | 13.2 ± 4.8 | 14.1 ± 8.8 |
| Cases without comorbidity (days, mean ± SD) | 12.3 ± 8.8 | 12.3 ± 8.9 | 12.4 ± 9.0 | 12.4 ± 8.9 | 12.5 ± 9.0 | 12.3 ± 9.2 | 12.5 ± 9.0 | 12.5 ± 9.4 | 12.5 ± 9.1 | 11.8 ± 8.9 | |
| P (t test) | 0.017 | 0.007 | 0.150 | 0.066 | 0.473 | 0.004 | 0.087 | 0.422 | 0.774 | 0.001 | |
| Hospital Admission | Cases with comorbidity)% admitted( | 55.9 | 67.3 | 64.0 | 52.4 | 83.3 | 48.2 | 80.0 | 23.8 | 0 | 40.7 |
| Cases without comorbidity (% admitted) | 25.1 | 24.0 | 26.7 | 27.3 | 27.6 | 26.3 | 27.7 | 28.3 | 28.7 | 22.6 | |
| OR unadjusted | 3.78 | 6.20 | 4.87 | 2.93 | 13.14 | 2.61 | 10.45 | 0.79 | 0.71 | 2.35 | |
| p-value (χ2 test) | 0.001 | 0.001 | 0.001 | 0.012 | 0.002 | 0.001 | 0.009 | 0.529 | 0.015 | 0.001 | |
| LOS in Hospital | Cases with comorbidity (days, median-IQR) | 1.5–8 | 6–12.7 | 7–10 | 4–10 | 10.5–10.5 | 0–8 | 13–12 | 0–0.25 | 0–0 | 0–7 |
| Cases without comorbidity (days, median-IQR) | 0-0.25 | 0–0 | 0–1 | 0–1 | 0–1.7 | 0–1 | 0–2 | 0–2 | 0–2 | 0–0 | |
| p-value (ManWhtiney) | 0.001 | 0.001 | 0.001 | 0.011 | 0.004 | 0.004 | 0.005 | 0.253 | 0.045 | 0.001 | |
| ICU Admission | Cases with comorbidity)% admitted( | 8.8 | 11.5 | 8.0 | 14.3 | 0 | 10.7 | 0 | 7.1 | 0 | 6.1 |
| Cases without comorbidity (% admitted) | 2.5 | 2.4 | 2.9 | 2.8 | 3.1 | 2.5 | 3.1 | 2.9 | 3.2 | 1.8 | |
| OR unadjusted | 3.76 | 5.20 | 2.87 | 5.84 | – | 4.75 | – | 2.61 | 0.96 | 3.47 | |
| p-value (χ2 test) | 0.004 | 0.001 | 0.152 | 0.003 | 0.659 | 0.001 | 0.687 | 0.121 | 0.483 | 0.003 | |
| Need for Ventilator | Cases with comorbidity)% admitted( | 7.4 | 11.5 | 4.0 | 14.3 | 0 | 3.6 | 20.0 | 4.8 | 0 | 4.2 |
| Cases without comorbidity (% admitted) | 0.9 | 0.8 | 1.5 | 1.2 | 1.6 | 1.4 | 1.4 | 1.4 | 1.6 | 0.4 | |
| OR unadjusted | 8.36 | 16.9 | 2.79 | 14.10 | – | 2.64 | 17.3 | 3.64 | – | 10.75 | |
| p-value (χ2 test) | 0.001 | 0.001 | 0.315 | 0.001 | 0.757 | 0.205 | 0.001 | 0.084 | 0.622 | 0.001 |
Table 3.
One-way ANOVA analysis of COVID-19 patients’ mean recovery period, length of hospital stay, and hospital admission by number of comorbidities.
|
Recovery period |
Length of hospital stay |
Admission to hospital |
||||
|---|---|---|---|---|---|---|
| Number of comorbidities | Cases with comorbidity (days, mean ± SD) | p-value (one way ANOVA) | Cases with comorbidity (days, mean ± SD) | p-value (one way ANOVA) | Cases with comorbidity (% admitted) | p-value (one way ANOVA) |
| None | 11.8 ± 8.9 | 0.001 | 1.7 ± 3.9 | 0.001 | 22.6 | 0.001 |
| 1 | 13.5 ± 9.4 | 3.4 ± 6.7 | 32.4 | |||
| 2 | 15.1 ± 9.3 | 3.9 ± 7.1 | 43.2 | |||
| >2 | 17.5 ± 8.9 | 12.7 ± 9.9 | 90.9 | |||
The mean recovery period per day by the number of comorbidities indicated a significant difference between recovery periods (Table 3). Individuals with more than two diseases took 17.5 ± 8.9 days on average to recover compared to 13.5 ± 9.4 and 15.1 ± 11.4 days for individuals with one and two comorbidities, respectively (p < 0.001) (Table 3).
The results of the multiple linear regression model for the recovery period per day by comorbidities, age, and gender are shown in Table 4. The overall model was significant at 5% and the value of coefficient of determination suggested that 68% of the variation in the recovery period among the study population was explained by the variables included in the model. Age, gender, renal disease, and pulmonary diseases (e.g., asthma and chronic obstructive pulmonary disease (COPD)) were found to be significant predictors of the recovery period. Every one-year increase in age resulted in a 17% increase in the recovery period. The mean difference of recovery periods between male and female participants was 4.28 days. Controlling for all other variables, individuals with renal diseases took 5.7 more days to recover and pulmonary diseases increased the recovery period by 3.7 days.
Table 4.
Multiple regression analyses for the recovery period, length of stay, and hospital admissions controlling for comorbidities, age, and gender.
|
Recovery period |
Length of hospital stay |
Admission to hospital |
||||
|---|---|---|---|---|---|---|
| Variable | β adjusted (95% CI) | p-value | β adjusted (95% CI) | p-value | OR adjusted (95% CI) | p-value |
| Age | 0.17 (0.12–0.21) | 0.001 | 0.08 (0.05–0.11) | 0.001 | 1 (0.99–1.01) | 0.734 |
| Male gender | 4.28 (3.40–5.35) | 0.001 | −0.54 (−1.16–0.07) | 0.056 | 0.44 (0.34–0.58) | 0.001 |
| Diabetes | 1.29 (−0.98–3.55) | 0.254 | 2.36 (0.93–3.79) | 0.001 | 2.62 (1.55–4.42) | 0.001 |
| Hypertension | −0.86 (−3.31–1.60) | 0.493 | 2.96 (1.42–4.51) | 0.001 | 2.84 (1.59–5.05) | 0.001 |
| Dyslipidemia | −0.71(−3.85–2.43) | 0.657 | 0.27 (−1.71–2.26) | 0.712 | 1.59 (0.72–3.49) | 0.251 |
| Cardiovascular | 1.53 (−2.02–5.08) | 0.398 | 1.6 (−0.64–3.84) | 0.161 | 1.58 (0.65–3.88) | 0.314 |
| Renal | 5.7 (0.90–11.3) | 0.046 | 2.3 (−1.27–5.88) | 0.206 | 3.05 (0.59–15.6) | 0.181 |
| Pulmonary | 3.7 (1.28–6.12) | 0.003 | 3.33 (1.81–4.86) | 0.001 | 2.32 (1.30–4.13) | 0.004 |
| Cancer | na | – | 6.09 (1.46–10.7) | 0.01 | na | – |
| Depression | na | – | −2.75 (−5.45–0.05) | 0.046 | na | – |
| R2 | 0.68 | – | 0.35 | – | – | – |
The multiple regression model for having at least one comorbidity as a predictor of the recovery period while controlling for age and gender are shown in Table 5. The variables included in the model explained 67% of the variation in recovery periods. Having at least one chronic health condition increased the recovery period by 1.52 days.
Table 5.
Multiple regression analyses for the recovery period, length of hospital stay, and hospital admission controlling for comorbidity, age, and gender.
|
Recovery period |
Length of hospital stay |
Admission to hospital |
||||
|---|---|---|---|---|---|---|
| Variable | β adjusted (95% CI) | p-value | β adjusted (95% CI) | p-value | OR adjusted (95% CI) | p-value |
| Age | 0.16 (0.12–0.20) | 0.001 | 0.1 (0.07–0.17) | 0.001 | 1.01 (1.00–1.02) | 0.051 |
| Male gender | 4.42 (3.50–5.40) | 0.001 | −0.87(-1.5–0.2) | 0.005 | 0.39 (0.31–0.51) | 0.001 |
| Presence of ≥ 1 chronic health condition | 1.52 (0.08–2.97) | 0.041 | 2.50(1.6–3.4) | 0.001 | 2.20 (1.61–3.18) | 0.001 |
| R2 | 0.66 | – | 0.29 | – | – | – |
3.3. Effect of comorbidities on COVID-19 patients’ hospital admissions
The presence of comorbidities was significantly associated with being admitted to the hospital in COVID-19 patients (Table 2). Individuals with renal disease, hypertension, dyslipidemia and diabetes were 13.14 (p < 0.001), 6.23 (p < 0.001), 4.87 (p < 0.001) and 3.78 (p < 0.001) times more likely to be admitted to hospital during their infection with COVID-19, respectively (Table 2). In addition, individuals with at least one disease were 2.35 times more likely to be admitted to the hospital compared with patients with no comorbidities (p < 0.001) (Table 2).
ICU admission was significantly associated with having diabetes, hypertension, cardiovascular disease, and pulmonary disease as well as those with at least one chronic health condition (Table 2). Twenty-one cases (6.1%) with at least one chronic health condition were admitted to ICU compared to 12 cases (1.8%) without disease, and patients with at least one disease were 3.47 times more likely to be admitted to the ICU compared to participants with no comorbidities (Table 2).
The need for mechanical ventilation was significantly associated with having diabetes, hypertension, cardiovascular disease, as well as having at least one comorbidity. Patients with at least one chronic health condition were 10.75 times more likely to have mechanical ventilation as compared to participants without comorbidities.
A strong association was identified between the number of comorbidities in COVID-19 patients and hospital admissions. about 90% of patients with more than two comorbidities were admitted to the hospital compared to only 22.6% of individuals without comorbidities (p < 0.001) (Table 3).
Results of multiple regression analysis of hospital admissions as an outcome variable controlling for age, gender, and comorbidities are shown in Table 4. Gender, diabetes, hypertension, and pulmonary disease (e.g., asthma and chronic obstructive pulmonary disease (COPD)) were found to be significant predictors of hospital admission in COVID-19 patients. The male patients had 56% lower odds of being admitted in comparison to their female counterparts (p < 0.001). Keeping all other variables constant patients with hypertension were 2.84 times more likely to be admitted to the hospital compared to patients without hypertension. Patients with diabetes were 2.62 times more likely to be admitted to the hospital controlling for other comorbidities, age, and gender.
Further analysis investigated the effect of comorbidities on the hospital length of stay, ICU admission, and use of oxygen ventilation. There were significant differences in the length of hospitalization for all comorbidities except for obesity (Table 2). The longest hospitalization period was for patients with cancer disease (median 13.0) followed by renal patients (median 10.5). Multiple regression analysis of the association between the mean recovery period, hospital admission, and length of hospital stay and patient comorbidities are presented in Table 4. Thirty-five percent of the variation in hospitalization period were explained by the variables investigated.
Multiple logistic regression model for having at least one comorbidity as a predictor of being admitted to the hospital and controlling for age and gender is reported in Table 5. The OR suggests that COVID-19 patients with at least one comorbidity had more than twice the odds of being admitted to the hospital compared with those without comorbidities while controlling for age and gender (p < 0.001).
3.4. Effect of COVID-19 symptoms on patients’ recovery periods
Table 6, Table 7 summarize the results of the differences in recovery periods based on the experienced symptoms. Significant differences in recovery periods were identified for all COVID-19 symptoms in symptomatic patients as opposed to asymptomatic patients. The mean recovery duration for patients with vomiting was 16.0 days, followed by 15.4 and 15.2 for patients with breathlessness and diarrhea, respectively (p < 0.001) (Table 6).
Table 6.
Univariate analysis of COVID-19 patients’ mean recovery period and hospital admission by symptoms.
|
Recovery period |
Admission to hospital |
||||||
|---|---|---|---|---|---|---|---|
| Cases with symptom (days, mean ± SD) | Cases without symptom (days, mean ± SD) | p-value | Cases with symptom (% admitted) | Cases without symptom (% admitted) | OR Unadjusted | p-value | |
| Fever | 13.5 ± 9.3 | 10.0 ± 7.7 | 0.001 | 36.4 | 16.3 | 2.79 | 0.001 |
| Cough | 14.9 ± 9.0 | 11.2 ± 8.8 | 0.001 | 37.1 | 26.4 | 1.67 | 0.001 |
| Breathlessness | 15.4 ± 9.3 | 10.6 ± 8.2 | 0.001 | 43.2 | 22.1 | 2.78 | 0.001 |
| Headache | 13.3 ± 9.2 | 11.7 ± 8.8 | 0.017 | 27.4 | 34.5 | 0.78 | 0.024 |
| Sleep disturbance | 13.8 ± 8.4 | 12.1 ± 9.1 | 0.025 | 27.3 | 32.3 | 0.78 | 0.187 |
| Loss of sense | 13.8 ± 9.2 | 10.4 ± 8.4 | 0.001 | 30.6 | 31.6 | 0.95 | 0.801 |
| Tired | 13.7 ± 9.3 | 10.4 ± 8.0 | 0.001 | 31.4 | 30.2 | 1.05 | 0.443 |
| Vomiting | 16.0 ± 8.9 | 11.9 ± 8.8 | 0.001 | 46.4 | 28.3 | 2.24 | 0.001 |
| Diarrhea | 15.2 ± 9.6 | 10.9 ± 8.2 | 0.001 | 38.9 | 26.3 | 1.78 | 0.001 |
Table 7.
Multiple regression analyses of COVID-19 patients’ mean recovery period, hospital admission based on reported symptoms controlling for age and gender.
|
Recovery period |
Admission to hospital |
|||
|---|---|---|---|---|
| Variable | β adjusted (95% CI) | P (test) | OR adjusted (95% CI) | P (t test) |
| Age | 0.11 (0.07–0.15) | 0.001 | 1.01 (1.00–1.02) | 0.031 |
| Gender | 2.44 (1.44–2.51) | 0.001 | 0.38 (0.29–0.51) | 0.001 |
| Fever | 1.42 (-0.01–2.8) | 0.054 | 1.11 (0.76–1.61) | 0.573 |
| Cough | 1.35 (0.02–2.69) | 0.048 | 1.06 (0.75–1.49) | 0.755 |
| Breathlessness | 3.08 (1.72–4.43) | 0.001 | 2.33 (1.66–3.35) | 0.001 |
| Headache | −0.53 (-1.88–0.83) | 0.444 | 0.45 (0.32–0.63) | 0.001 |
| Sleep disturbance | −1.08 (-2.63–0.46) | 0.170 | – | – |
| Loss of sense | 2.46 (1.13–3.80) | 0.001 | – | – |
| Tired | 1.09 (-0.3–2.49) | 0.122 | – | – |
| Vomiting | 1.25 (-0.09–3.5) | 0.051 | 1.56 (1.00–2.42) | 0.048 |
| Diarrhea | 1.78 (0.35–3.19) | 0.015 | 1.36 (0.95–1.95) | 0.093 |
| R2 | 0.71 | – | – | – |
A multiple linear regression model for the recovery period by symptoms of COVID-19 and controlling for age and gender is presented in Table 7. Symptoms of cough, breathlessness, loss of taste and/or smell, and diarrhea were the most commonly reported symptoms. Breathlessness increased the recovery period by 3.08 days compared to patients with no breathlessness (p < 0.001). A loss of taste and/or smell, diarrhea, and cough increased the recovery period by 2.46 days (p < 0.001), 1.78 days (p < 0.015), and 1.35 days (p < 0.05), respectively. The factors included in the model explained 71% of the variation in the recovery period among participants.
3.5. Effect of COVID-19 symptoms on patients’ hospital admissions
Six symptoms were found to have a significant association with hospital admission among COVID-19 patients: fever, cough, breathlessness, headache, vomiting, and diarrhea (p < 0.05) (Table 6). Logistic regression analysis of hospital admissions as an outcome variable by symptoms and controlling for age and gender are presented in Table 7. Breathlessness, headache, and vomiting were all associated with hospital admissions. COVID-19 patients with breathlessness were 2.33 times more likely to be admitted to the hospital (p < 0.001), and patients with vomiting were 1.56 more likely to be admitted (p < 0.05).
4. Discussion
This study examined the impact of different comorbidities and symptoms on the COVID-19-related recovery period, risk of hospitalization, and LOS. Also, the impact of different comorbidities on the risk of ICU admission and the need for mechanical ventilation were also examined. Although these results might not be novel due to the fact that similar findings were presented in other studies, they provide new insights on the impact of different comorbidities and COVID-19-related symptoms on various outcomes among those who survived the infection.
The presence of chronic health conditions, such as, diabetes, hypertension, and chronic renal disease increases the risk of COVID-19-related hospitalization, LOS, and increases the duration of recovery. These findings are consistent with previously published studies that showed higher risk of COVID-19-related morbidity and mortality among patients with multiple comorbidities (Banik et al., 2016, Li et al., 2020b, Yang et al., 2006, Yu et al., 2006). Radwan et al. conducted a systematic review of the clinical characteristics, comorbidities, and severity of COVID-19 patients (Radwan et al., 2020), and Mudatsir et al. published a systematic review and meta-analysis of the predictors of COVID-19 severity (Mudatsir et al., 2021). Patients with hypertension, chronic kidney disease, chronic obstructive pulmonary disease, and cancer were two to six times more likely to experience severe cases. Hypertension and diabetes are the most common commodities in severe cases of COVID-19 and have been associated with an increase in severity and ICU admissions of COVID-19 patients (Li et al., 2020b, Wang et al., 2020a). Approximately 21% of the study population had at least one comorbidity, which is higher than the proportion of COVID-19 patients with multiple comorbidities reported in other studies that ranged from 15 to 81.9% (Palmieri et al., 2020, Posso et al., 2020, Richardson et al., 2020, Wang et al., 2020a). However, national studies conducted in Saudi Arabia by Alsofayan et al. and Khan et al. in the initial stages of the pandemic reported that 20.1–29% of patients had one or more comorbidity (Alsofayan et al., 2020, Khan et al., 2020a). The present study included COVID-19 patients from different regions in Saudi Arabia. The most commonly reported comorbidities were diabetes (9.6%), hypertension (7.4%), and pulmonary disease (e.g., asthma and chronic obstructive pulmonary disease (COPD)) (7.9%). Alsofayan et al. reported that the most common comorbidities were pulmonary disease (10.1%), hypertension (8.8%), and diabetes (7.6%) (Alsofayan et al., 2020). Khan et al. found that pulmonary conditions (12.5%), hypertension (11.6%), and diabetes (11.3%) were most frequently reported (A. Khan et al., 2020). Fever (72.5%), feeling tired (63.4%), and loss of taste and/or smell (62.5%) were the most commonly reported symptoms in contrast to fever, cough, sore throat, and runny nose reported in previously published studies (Alsofayan et al., 2020, Khan et al., 2020a).
Based on results of this study, the mean recovery time of COVID-19 patients with at least one comorbidity was two days longer in comparison to patients without comorbidities. Moreover, multiple comorbidities were associated with prolonged recovery time. These findings were consistent even among hospitalized COVID-19 patients. Furthermore, the risk of hospitalization increases as the number of comorbidities increases. (Table 3). In addition, LOS, ICU admission, and the need for mechanical ventilation were significantly higher in patients with at least one comorbidity (Table 2). These findings highlight the impact of comorbidities on the severity of COVID-19 and are in line with previously published studies (Badawi and Ryoo, 2016, Li et al., 2020b, Wang et al., 2020a). Diseases such as diabetes and hypertension have a negative impact on patient innate immunity. Several reports have linked these diseases to the onset of cytokine storm, which is the exacerbation of a pro-inflammatory state, and generation of oxidative stress that leads to tissue damage and poor prognosis (Dharmashankar and Widlansky, 2010, Erener, 2020, Hojyo et al., 2020, Tisoncik et al., 2012). Severe COVID-19 ICU patients typically present with higher plasma levels of cytokines associated with cytokine storm than non-ICU patients (Huang et al., 2020).
Not only do the presence of comorbidities increase the severity of COVID-19, but they also lead to an increased economic burden on the healthcare system (A. A. Khan et al., 2020). Based on our data, comorbidities in COVID-19 patients were associated with longer recovery time, higher rates of hospital admissions, longer periods of hospitalization, higher rates of ICU admissions, and increased rates of mechanical ventilation. These additional management and treatment measures increase the burden on hospital systems and increases medical expenditures (Gupta et al., 2020, Kassir et al., 2020, Reddy, K.P., Shebl, F.M., Foote, J.H.A., Harling, G., Scott, J.A., Panella, C., et al ., 2020). An increase in direct medical costs of COVID-19 management was associated with case severity and the need for longer hospitalization, the need for ICU admission, and mechanical ventilation (A. Khan et al., 2020b, Rees et al., 2020).
Diabetes, hypertension and pulmonary disease were associated with an increased risk of hospitalization even after controlling for other comorbidities, age, and gender. This is consistent with another cohort study of 7337 COVID-19 patients with or without type 2 diabetes mellitus, which showed a higher risk of hospital admissions among patients with diabetes than those without diabetes (Zhu et al., 2020). The study also concluded that poorly controlled glucose levels substantially increased disease severity and mortality rates (Zhu et al., 2020). Moreover, a recent retrospective cohort study including nearly 67,000 patients from over 600 hospitals in the United States concluded that obesity and both diabetes and hypertension with chronic complications are associated with a higher risk of mortality (Goodman et al., 2020). Another meta-analysis of multiple studies in China reported a four-fold increase in mortality due to COVID-19 in patients with COPD (Zhao et al., 2020). The presence of comorbidities aggravates COVID-19 severity and increases the likelihood of COVID-19-related hospital admissions.
Although this study highlighted the impact of different comorbidities and COVID-19-related symptoms on recovery period, hospitalization rate, LOS, ICU admission, and the need of mechanical ventilation, multiple limitations have to be acknowledged. First, the study only included those who recovered from COVID-19 infection which can introduce selection bias. Moreover, the data was self-reported which increases the risk of information bias. In addition, the study included a small number of recovered COVID-19 patients which limits the generalizability of the findings despite the fact the included sample was randomly selected and participants were from different regions. Finally, the study did not examine the impact of different treatments on any of the examined outcomes (e.g., rate of hospitalization, recovery period, and LOS).
In conclusion, the characteristics of COVID-19 patients who were admitted to hospitals among young and middle-aged adults are not different than those from older age groups. Common comorbidities, such as, diabetes, hypertension, and pulmonary diseases might worsen the prognosis of COVID-19 patients. Diabetes, hypertension, and pulmonary diseases are potential risk factors of worse COVID-19-related outcomes. More efforts should be exercised to protect patients with one or more comorbidities from being exposed to the infection. Additionally, recommendations, such as, prioritizing the management of COVID-19 patients with multiple comorbidities and encouraging the administration of COVID-19 vaccines for those at-risk groups, should adopted. Future studies should retrieve data from more reliable sources and include both COVID-19 survivors and non-survivors to investigate the impact of different treatment protocols on the rates of morbidity and mortality.
Funding
The Financial fund was provided by King Abdul-Aziz City for Science and Technology (General Directorate for Fund and Grants) to (King Saud University) to implement this Work through Fast Track Program for COVID-19 Research Project (No.5-20-01-001-0058).
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Central Institutional Review Board of Saudi Ministry of Health (protocol code 20-11E and date of approval 17-06-2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data will be available from the corresponding author on request.
CRediT authorship contribution statement
Amer S. Alali: Conceptualization, Software, Writing - original draft. Abdulaziz O. Alshehri: Conceptualization, Investigation, Resources. Ahmed Assiri: Conceptualization, Visualization, Project administration. Shahd Khan: Investigation. Munirah A. Alkathiri: Investigation. Omar A. Almohammed: Conceptualization, Methodology, Software, Formal analysis. Waleed Badoghaish: Software. Saeed M. AlQahtani: Software, Investigation, Writing - review & editing. Musaad A. Alshammari: Methodology. Mohamed Mohany: Methodology, Formal analysis. Faisal F. Alamri: Conceptualization, Methodology, Validation. Yazed AlRuthia: Conceptualization, Formal analysis, Writing - review & editing. Faleh Alqahtani: Conceptualization, Methodology, Validation, Resources, Data curation, Writing - review & editing, Supervision, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would thank for the financial support provided by King Abdul-Aziz City for Science and Technology (General Directorate for Fund and Grants) to (King Saud University) to implement this Work through Fast Track Program for COVID-19 Research Project (No. 5-20-01-001-0058). In addition, authors would also thank the assistant deputy of planning and organizational excellence at the Saudi Ministry of Health for their help in facilitating the communications with patients.
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Amer S. Alali, Email: a.alali@psau.edu.sa.
Abdulaziz O. Alshehri, Email: 439105704@student.ksu.edu.sa.
Ahmed Assiri, Email: aasssiri@moh.gov.sa.
Shahd Khan, Email: 441204353@student.ksu.edu.sa.
Munirah A. Alkathiri, Email: 436200445@student.ksu.edu.sa.
Omar A. Almohammed, Email: oalmohammed@ksu.edu.sa.
Waleed Badoghaish, Email: wbaoghaish@ut.edu.sa.
Saeed M. AlQahtani, Email: smaalqahtani@kku.edu.sa.
Musaad A. Alshammari, Email: malshammari@ksu.edu.sa.
Mohamed Mohany, Email: mmohany@ksu.edu.sa.
Faisal F. Alamri, Email: alamrif@ksau-hs.edu.sa, alamrif@ksau-hs.edu.sa.
Yazed AlRuthia, Email: yazeed@ksu.edu.sa, yazeed@ksu.edu.sa.
Faleh Alqahtani, Email: afaleh@ksu.edu.sa.
Appendix A. English Version of the Questionnaire
References
- Alguwaihes, A.M., Al-Sofiani, M.E., Megdad, M., Albader, S.S., Alsari, M.H., Alelayan, A., Jammah, A.A., 2020. Diabetes and Covid-19 among hospitalized patients in Saudi Arabia: a single-centre retrospective study. Cardiovascular Diabetology, 19(1), 1-12. [DOI] [PMC free article] [PubMed]
- Almalki Z.S., Khan M.F., Almazrou S., Alanazi A.S., Iqbal M.S., Alqahtani A., Alahmari A.K. Clinical characteristics and outcomes among COVID-19 hospitalized patients with chronic conditions: a retrospective single-center study. J. Multidisciplinary Healthcare. 2020;13:1089. doi: 10.2147/JMDH.S273918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Mutair A., Alhumaid S., Alhuqbani W.N., Zaidi A.R.Z., Alkoraisi S., Al-Subaie M.F., Alsharafi A.A. Clinical, epidemiological, and laboratory characteristics of mild-to-moderate COVID-19 patients in Saudi Arabia: an observational cohort study. Eur. J. Med. Res. 2020;25(1):1–8. doi: 10.1186/s40001-020-00462-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Omari A., Alhuqbani W.N., Zaidi A.R.Z., Al-Subaie M.F., AlHindi A.M., Abogosh A.K. Clinical characteristics of non-intensive care unit COVID-19 patients in Saudi Arabia: A descriptive cross-sectional study. J. Infect. Public Health. 2020;13:1639–1644. doi: 10.1016/j.jiph.2020.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alqahtani A.M., AlMalki Z.S., Alalweet R.M., Almazrou S.H., Alanazi A.S., Alanazi M.A., AlGhamdi S. Assessing the severity of illness in patients with coronavirus disease in Saudi Arabia: a retrospective descriptive cross-sectional study. Front. Public Health. 2020;8:775. doi: 10.3389/fpubh.2020.593256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alsofayan Y.M., Althunayyan S.M., Khan A.A., Hakawi A.M., Assiri A.M. Clinical characteristics of COVID-19 in Saudi Arabia: A national retrospective study. J. Infect. Public Health. 2020;13:920–925. doi: 10.1016/j.jiph.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badawi A., Ryoo S.G. Prevalence of comorbidities in the Middle East respiratory syndrome coronavirus (MERS-CoV): a systematic review and meta-analysis. Int. J. Infect. Dis. 2016;49:129–133. doi: 10.1016/j.ijid.2016.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Banik G.R., Alqahtani A.S., Booy R., Rashid H. Risk factors for severity and mortality in patients with MERS-CoV: Analysis of publicly available data from Saudi Arabia. Virol. Sin. 2016;31:81–84. doi: 10.1007/s12250-015-3679-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, Y., Gong, X., Wang, L., Guo, J., 2020. Effects of hypertension, diabetes and coronary heart disease on COVID-19 diseases severity: A systematic review and meta-analysis. medRxiv. https://doi.org/10.1101/2020.03.25.20043133.
- Clark A., Jit M., Warren-Gash C., Guthrie B., Wang H.H.X., Mercer S.W. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Glob. Heal. 2020;8:e1003–e1017. doi: 10.1016/S2214-109X(20)30264-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dharmashankar K., Widlansky M.E. Vascular endothelial function and hypertension: Insights and directions. Curr. Hypertens. Rep. 2010;12:448–455. doi: 10.1007/s11906-010-0150-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erener S. Diabetes, infection risk and COVID-19. Mol. Metab. 2020;39 doi: 10.1016/j.molmet.2020.101044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman K.E., Magder L.S., Baghdadi J.D., Pineles L., Levine A.R., Perencevich E.N. Impact of sex and metabolic comorbidities on COVID-19 mortality risk across age groups: 66, 646 Inpatients Across 613 U.S. Hospitals. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa1787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guan W., Ni Z., Hu Y.u., Liang W., Ou C., He J., Liu L. Clinical characteristics of coronavirus disease 2019 in China. N. Engl. J. Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta M., Abdelmaksoud A., Jafferany M., Lotti T., Sadoughifar R., Goldust M. COVID-19 and economy. Dermatol. Ther. 2020;33 doi: 10.1111/dth.13329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hojyo S., Uchida M., Tanaka K., Hasebe R., Tanaka Y., Murakami M. How COVID-19 induces cytokine storm with high mortality. Inflamm. Regen. 2020;40:37. doi: 10.1186/s41232-020-00146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C., Wang Y., Li X., Ren L., Zhao J., Hu Y., Zhang L., Fan G. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain, A., Bhowmik, B., do Vale Moreira, N.C., 2020. COVID-19 and diabetes: Knowledge in progress. Diabetes Res. Clin. Pract. 162, 108142. https://doi.org/10.1016/j.diabres.2020.108142. [DOI] [PMC free article] [PubMed]
- Kassir, M., Gupta, M., Abdelmaksoud, A., Goldust, M., 2020. How to manage high-risk asymptomatic COVID-19 carriers; COVID-19 poses a huge threat to public health and to dermatology specialty as well. Dermatol. Ther. https://doi.org/10.1111/dth.14064. [DOI] [PubMed]
- Khan, A., Althunayyan, S., Alsofayan, Y., Alotaibi, R., Mubarak, A., Arafat, M., et al., 2020. Risk factors associated with worse outcomes in COVID-19: A retrospective study in Saudi Arabia. East. Mediterr. Heal. J. 26, 1371–1380. https://doi.org/10.26719/emhj.20.130. [DOI] [PubMed]
- Khan, A.A., Alruthia, Y., Balkhi, B., Alghadeer, S.M., Temsah, M.H., Althunayyan, S.M., et al., 2020. Survival and estimation of direct medical costs of hospitalized covid-19 patients in the kingdom of saudi arabia (Short title: Covid-19 survival and cost in saudi arabia). Int. J. Environ. Res. Public Health 17, 1–13. https://doi.org/10.3390/ijerph17207458. [DOI] [PMC free article] [PubMed]
- Kroumpouzos G., Gupta M., Jafferany M., Lotti T., Sadoughifar R., Sitkowska Z., Goldust M. COVID-19: A relationship to climate and environmental conditions? Dermatol. Ther. 2020;33 doi: 10.1111/dth.13399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ksiazek T.G., Erdman D., Goldsmith C.S., Zaki S.R., Peret T., Emery S. A novel coronavirus associated with severe acute respiratory syndrome. N. Engl. J. Med. 2003;348:1953–1966. doi: 10.1056/nejmoa030781. [DOI] [PubMed] [Google Scholar]
- Li, B., Yang, J., Zhao, F., Zhi, L., Wang, X., Liu, L., et al., 2020. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin. Res. 109, 531–538. Cardiol. https://doi.org/10.1007/s00392-020-01626-9. [DOI] [PMC free article] [PubMed]
- Li X., Xu S., Yu M., Wang K., Tao Y., Zhou Y., Shi J. Risk factors for severity and mortality in adult COVID-19 inpatients in Wuhan. J. Allergy Clin. Immunol. 2020;146:110–118. doi: 10.1016/j.jaci.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu K., Fang Y.Y., Deng Y., Liu W., Wang M.F., Ma J.P. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin. Med. J. (Engl) 2020;133:1025–1031. doi: 10.1097/CM9.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mudatsir, M., Fajar, J.K., Wulandari, L., Soegiarto, G., Ilmawan, M., Purnamasari, Y., et al., 2021. Predictors of COVID-19 severity: a systematic review and meta-analysis. F1000 Res. 9, 1107. https://doi.org/10.12688/f1000research.26186.2. [DOI] [PMC free article] [PubMed]
- Palmieri L., Vanacore N., Donfrancesco C., Lo Noce C., Canevelli M., Punzo O. Clinical characteristics of hospitalized individuals dying with COVID-19 by age group in Italy. J. Gerontol. Ser. A. 2020;75:1796–1800. doi: 10.1093/gerona/glaa146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posso M., Comas M., Román M., Domingo L., Louro J., González C. Comorbidities and mortality in patients with COVID-19 aged 60 years and older in a university hospital in Spain. Arch. Bronconeumol. 2020;56:756–758. doi: 10.1016/j.arbres.2020.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radwan, N.M., Mahmoud, N.E., Alfaifi, A.H., Alabdulkareem, K.I., 2020. Comorbidities and severity of coronavirus disease 2019 patients. Saudi Med. J. 41, 1165–1174. https://doi.org/10.15537/smj.2020.11.25454. [DOI] [PMC free article] [PubMed]
- Reddy, K.P., Shebl, F.M., Foote, J.H.A., Harling, G., Scott, J.A., Panella, C., et al., 2020. Cost-effectiveness of public health strategies for COVID-19 epidemic control in South Africa: A microsimulation modelling study. medRxiv. 33, e13329. https://doi.org/10.1101/2020.06.29.20140111. [DOI] [PMC free article] [PubMed]
- Rees E.M., Nightingale E.S., Jafari Y., Waterlow N.R., Clifford S., Carl C.A. COVID-19 length of hospital stay: A systematic review and data synthesis. BMC Med. 2020;18:270. doi: 10.1186/s12916-020-01726-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson S., Hirsch J.S., Narasimhan M., Crawford J.M., McGinn T., Davidson K.W. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York city area. JAMA - J. Am. Med. Assoc. 2020;323:2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanyaolu A., Okorie C., Marinkovic A., Patidar R., Younis K., Desai P., Hosein Z., Padda I., Mangat J., Altaf M. Comorbidity and its impact on patients with COVID-19. SN Compr. Clin. Med. 2020;2:1069–1076. doi: 10.1007/s42399-020-00363-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoen K., Horvat N., Guerreiro N.F.C., De Castro I., De Giassi K.S. Spectrum of clinical and radiographic findings in patients with diagnosis of H1N1 and correlation with clinical severity. BMC Infect. Dis. 2019;19:964. doi: 10.1186/s12879-019-4592-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah P., Owens J., Franklin J., Mehta A., Heymann W., Sewell W. Demographics, comorbidities and outcomes in hospitalized Covid-19 patients in rural southwest Georgia. Ann. Med. 2020;52:354–360. doi: 10.1080/07853890.2020.1791356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheshah E., Sabico S., Albakr R.M., Sultan A.A., Alghamdi K.S., Al Madani K., Al-Daghri N.M. Prevalence of diabetes, management and outcomes among Covid-19 adult patients admitted in a specialized tertiary hospital in Riyadh, Saudi Arabia. Diabetes Res. Clin. Pract. 2021;172 doi: 10.1016/j.diabres.2020.108538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Subbarao K., Mahanty S. Respiratory virus infections: understanding COVID-19. Immunity. 2020;395:507–513. doi: 10.1016/j.immuni.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tisoncik J.R., Korth M.J., Simmons C.P., Farrar J., Martin T.R., Katze M.G. Into the eye of the cytokine storm. Microbiol. Mol. Biol. Rev. 2012;76:16–32. doi: 10.1128/mmbr.05015-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, B., Li, R., Lu, Z., Huang, Y., 2020. Does comorbidity increase the risk of patients with covid-19: Evidence from meta-analysis. Aging (Albany. NY) 12, 6049–6057. https://doi.org/10.18632/AGING.103000. [DOI] [PMC free article] [PubMed]
- Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J., Wang B., Xiang H., Cheng Z., Xiong Y., Zhao Y., Li Y., Wang X., Peng Z. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA - J. Am. Med. Assoc. 2020;323:1061–1069. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z., Deng H., Ou C., Liang J., Wang Y., Jiang M., Li S. Clinical symptoms, comorbidities and complications in severe and non-severe patients with COVID-19: A systematic review and meta-analysis without cases duplication. Medicine (Baltimore) 2020;99 doi: 10.1097/MD.0000000000023327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X.W., Wu X.X., Jiang X.G., Xu K.J., Ying L.J., Ma C.L. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: Retrospective case series. BMJ. 2020;368 doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J.K., Feng Y., Yuan M.Y., Yuan S.Y., Fu H.J., Wu B.Y. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet. Med. 2006;23:623–628. doi: 10.1111/j.1464-5491.2006.01861.x. [DOI] [PubMed] [Google Scholar]
- Yu C.M., Wong R.S.M., Wu E.B., Kong S.L., Wong J., Yip G.W.K. Cardiovascular complications of severe acute respiratory syndrome. Postgrad. Med. J. 2006;82:140–144. doi: 10.1136/pgmj.2005.037515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Q., Meng M., Kumar R., Wu Y., Huang J., Lian N. The impact of COPD and smoking history on the severity of COVID-19: A systemic review and meta-analysis. J. Med. Virol. 2020;92:1915–1921. doi: 10.1002/jmv.25889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu L., She Z.G., Cheng X., Qin J.J., Zhang X.J., Cai J., Lei F. Association of blood glucose control and outcomes in patients with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020;31:1068–1077.e3. doi: 10.1016/j.cmet.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]