Abstract
Vaginal cuff dehiscence is a rare but potentially life-threatening post-hysterectomy complication. Here we report two cases of vaginal cuff dehiscence with distinct imaging features and describe the CT findings of vaginal cuff dehiscence. Both patients underwent repair surgery, and the diagnoses were confirmed. Radiologic features of vaginal cuff dehiscence are uncommonly described in the literature. Vaginal cuff mural discontinuity and omental fat tissue or bowel herniation into the vaginal canal are the most common appearances of vaginal cuff dehiscence. Pelvic hematoma, bowel obstruction, and pneumoperitoneum can accompany. These two cases highlight the CT appearances, potential presentations, and management of vaginal cuff dehiscence in the emergency setting.
Keywords: Hysterectomy, postoperative, complication, iatrogenic, bleeding, pneumoperitoneum
Abbreviations: VCD, Vaginal cuff dehiscence; CT, Computed tomography; ER, Emergency room; CBC, Complete blood count
Introduction
Hysterectomy is the most commonly performed major gynecological operation worldwide [1]. Approximately one-third of women aged ≥50 years in the United States have had a hysterectomy [2]. Although rare, vaginal cuff dehiscence (VCD) is a potentially serious postoperative complication after hysterectomy that requires prompt resuscitation and surgical intervention.
VCD is partial or complete separation of the vaginal cuff edges that were previously sutured at the time of hysterectomy. VCD can be life-threatening in cases with bowel evisceration that may cause bowel infarction, peritonitis, sepsis, and shock [3]. It is typically diagnosed by clinical history and pelvic exam, but its low incidence can make the diagnosis overlooked in the emergency department, and radiologic features may help the diagnosis in selected patients. We present two VCD cases with different radiologic features on computed tomography (CT) to highlight its possible imaging characteristics, which may help radiologists recognize this relatively rare postoperative complication.
Case presentations
Case 1
A 40-year-old Gravida 5, Para 0 female with a past surgical history of total laparoscopic hysterectomy for fibroid uterus two months ago presented to the emergency room (ER) with heavy vaginal bleeding and pelvic pain that started during vaginal intercourse and continued post-coitus. The patient was cleared for routine activity and intercourse one week prior by gynecology, and she had vaginal intercourse for the first time since her hysterectomy. The patient was on lisinopril due to a history of hypertension but was otherwise healthy. The patient had a history of loop electrosurgical excision procedure and in vitro fertilization in the past. The patient denied using tobacco products, alcohol, drugs, or marijuana, and the family history was non-contributory.
The patient was not in immediate distress in ER, and the vital signs were normal. On physical exam, the patient had mild suprapubic tenderness without guarding or rebound. On the initial pelvic exam in ER, the external exam was unremarkable. There was a large amount of hemorrhagic products in the vagina on the speculum exam. There was no active bleeding. The serum hemoglobin level was 11.7 g/dL (reference level: 12.1-15.1 g/dL). Otherwise, the laboratory values were unremarkable. The patient was consulted to gynecology, and computed tomography (CT) was performed to evaluate the possible intraabdominal source of bleeding (Fig. 1).
Fig. 1.
Case 1. A-C. Contrast-enhanced axial (A), sagittal (B), and coronal (C) CT images show mural discontinuation (arrowheads) at the vaginal cuff, distention of the vaginal canal with high-density hemorrhage, pelvic free fluid (circle), and contrast extravasation (arrows) at the vaginal cuff that indicates active bleeding. D. Sagittal drawing of pelvis illustrates mural discontinuity at the vaginal cuff (arrowheads) and active bleeding (arrow). Mural discontinuation suggests vaginal cuff dehiscence.
The diagnosis of vaginal cuff dehiscence was confirmed on pelvic exam done by gynecology after CT scan. There was a complete apical vaginal cuff dehiscence with intraabdominal fat tissue protruding into the dehiscence without bowel evisceration. On bimanual exam, the fat tissue was easily reduced into the abdomen. There were no signs of infection or bowel injury. The vaginal cuff dehiscence was repaired vaginally. The patient was stable postoperatively with stable serum hemoglobin level and was discharged on postoperative day one.
Case 2
A 40-year-old Gravida 2, Para 2 female with a history of total laparoscopic hysterectomy, bilateral salpingectomies, right oophorectomy, and sling surgery eleven weeks ago presented to ER with vaginal bleeding and acute abdominal pain that started during sexual intercourse. The patient was cleared by gynecology for vaginal intercourse, and this was the first time she had penetrative vaginal intercourse since her hysterectomy. After the abortion of the intercourse, the patient had a syncopal episode during showering with a brief loss of consciousness. Although the patient's bleeding was improved, the abdominal pain gradually worsened in time. The patient was otherwise healthy and denied using tobacco products, alcohol, or drugs, and the family history was non-contributory. The patient reported using marijuana occasionally.
On the physical exam, the patient was pale and hypotensive (85/56 mm Hg) in ER. The other vital signs were normal. The patient had moderate lower abdominal tenderness without guarding or rebound on the physical exam. The pelvic exam was deferred to gynecology due to patient discomfort. Complete blood count (CBC) showed leukocytosis (19.5 × 1000/ul, reference range 3.9-11.0 × 1000/ul) with neutrophilia (85%). Otherwise, CBC and basic metabolic panel were unremarkable. CT (Figs. 2 and 3) was done due to concerns for intra-abdominal postoperative complications.
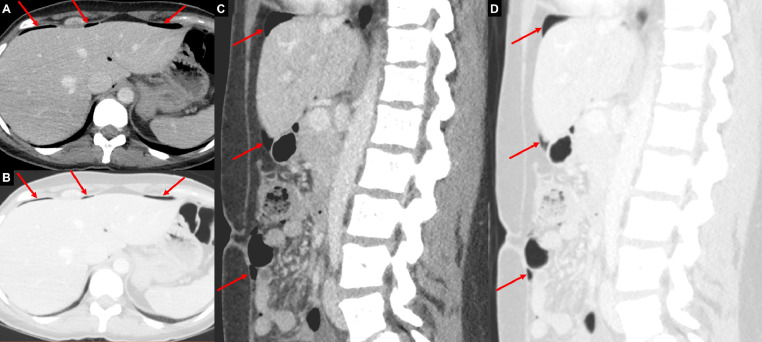
Fig. 2.
Case 2: Axial (A, B) and sagittal (C, D) CT images from the abdomen with soft tissue (A, C) and lung (B, D) windows demonstrate foci of free intraabdominal air (red arrows) at the anterior non-dependent abdomen.
Fig. 3.
Case 2: A. Axial contrast-enhanced CT image from pelvis demonstrates mild thickening and enhancement (dashed arrows) at the peritoneal reflection of the cul-de-sac, suspicious for inflammation. B. Sagittal contrast-enhanced CT image from pelvis shows mural discontinuity (arrowheads) at the vaginal cuff and protruding fat tissue (arrow) into the vaginal canal, compatible with vaginal cuff dehiscence. C. Intraoperative image from laparoscopic repair surgery shows a 2 cm defect (arrowheads) at the vaginal cuff, confirming vaginal cuff dehiscence. The intravaginal sponge is seen at the defect. D. Sagittal illustration of the pelvis demonstrates protruding intraabdominal fat tissue (yellow arrow) through the defect (arrowheads) at the vaginal cuff and intraabdominal free air (red arrows).
The pelvic exam that was done by gynecology revealed a 2 cm vaginal cuff dehiscence with a small prolapsing fat tissue that was reduced easily on the bimanual exam. There was no bowel evisceration or active bleeding. The patient was started on ampicillin and gentamicin and underwent laparoscopic repair of the vaginal cuff. The sigmoid colon was overlying the vaginal cuff with some inflammation and adhesions to the cul-de-sac, which was easily taken down. The 2 cm defect at the vaginal cuff was seen, and the cuff's edges were debrided and approximated. The patient tolerated the procedure well, and antibiotics were resumed for 24 hours. Hematology was consulted due to left ovarian vein thrombosis, which was considered as a provoked thrombotic event since it occurred within three months of surgery, and the patient was started on Apixaban for three months. The patient's vital signs and serum hemoglobin levels on repeat CBC were stable. The patient was discharged on post-op day one in good condition with instructions to follow up with gynecology and hematology.
Discussion
The incidence of VCD is reported between 0.14% to 4.1%, and it can occur at any time after hysterectomy. It has been reported three days after the operation, as well as 30 years after [4,5]. However, the mean time to VCD was found to be 7 weeks after total laparoscopic hysterectomy and 13 weeks after total abdominal hysterectomy [6]. The patients with VCD most commonly present with acute onset vaginal bleeding, abdominal pain, watery discharge, or all of these. Although intercourse, defecation, or Valsalva can precipitate VCD, spontaneous VCD comprises most of the cases in the general population [1,7,8]. However, in premenopausal patients, VCD predominantly occurs after coitus [9]. Pelvic prolapsus is also an important risk factor in postmenopausal patients [10]. Vaginal cuff infection or a postoperative pelvic fluid collection (hematoma or abscess) abutting the vaginal cuff can contribute to VCD [11]. The laparoscopic and robotic approaches are associated with a greater risk compared to abdominal and vaginal techniques [1,8,12].
VCD can cause evisceration of the bowel, adnexa, and omentum, which may lead to serious complications, including bowel ischemia, bowel necrosis, ileus, bacteremia, peritonitis, and sepsis. Therefore, early diagnosis is critical, which requires a high index of suspicion [1].
The diagnosis of VCD is mainly based on the clinical history and pelvic examination. However, its low incidence may cause ambiguity in diagnosis and delayed patient management [13]. Hence, suspected intraabdominal hemorrhage, persistent abdominal distention and pain, suspected infection, peritonitis, and abnormal vaginal examination, including discharge and vaginal cuff discontinuity, are usual clinical indications for post-hysterectomy CT imaging [11]. Therefore, radiologic findings may suggest VCD in selected patients and aid clinicians in rapid patient management.
The normal vaginal cuff should be smooth, continuous, and symmetric without adjacent mesenteric fat heterogeneity on CT (Fig. 4). As in our first patient, mural discontinuity at the vaginal cuff can indicate VCD. Intraabdominal fat herniation into the vaginal cuff should be carefully searched for in post-hysterectomy patients with vaginal pain and bleeding because it may be the first diagnostic clue in clinically subtle cases. In suspected VCD cases, the radiologist can recommend a focused physical examination [11]. If there is bowel herniation, it can cause mechanical bowel obstruction, which would cause dilated bowel loops with the transition point at the vaginal cuff level. Enhancement and thickening of the peritoneal folds and fascial planes can be seen in cases with accompanying pelvic infection, which may predispose to VCD [14]. Additional findings should be looked for, including pelvic abscess, hematoma, active bleeding, or pneumoperitoneum. In patients with intraabdominal free air and recent hysterectomy history, identifying VCD can prevent unnecessary exploratory surgery, which may cause increased patient morbidity and mortality [15].
Fig. 4.
Normal vaginal cuff after hysterectomy in a 37-year-old female. A. Sagittal contrast-enhanced CT image from the pelvis demonstrates blind-ending vagina with an intact vaginal cuff (yellow arrows). B. Sagittal illustration of the normal blind-ending vagina and intact vaginal cuff (arrows). The intraabdominal fat tissue (star) is not protruding from the vaginal cuff.
CT also can be used in selecting the approach of surgical repair by identifying possible bowel ischemia and necrosis in the bowel evisceration patients [13]. Therefore, signs of bowel ischemia, including bowel wall thickening, mesenteric fat stranding, and pneumatosis, should be communicated with the clinician.
VCD patients undergo surgical repair, but there is no consensus in the literature regarding the best approach. In clinically stable patients without bowel evisceration or peritonitis, a vaginal approach is typically preferred, and contrarily, a transabdominal or laparoscopic approach is generally recommended for the patients with signs of peritonitis, bowel ischemia, or bowel evisceration [1,13]. Bowel resection is required in some cases if ischemia is present. In the cases of profuse bleeding and shock, initial adequate fluid resuscitation is critical [16].
In this case report, we described CT findings of two cases of vaginal cuff dehiscence. To our knowledge, this is the first case report that depicts the CT features of this relatively rare complication after hysterectomy. Thus, radiologists should be familiar with the findings of vaginal cuff dehiscence and suggest the diagnosis in the appropriate clinical setting.
Footnotes
Competing interest: none
Informed consent: Informed consent has been obtained in order to perform CT scan and subsequent clinical examination according to internal hospital guidelines. All patient identifying information has been removed from the images and the case report.
References
- 1.Cronin B, Sung VW, Matteson KA. Vaginal cuff dehiscence: risk factors and management. Am J Obstet Gynecol. 2012;206(4):284–288. doi: 10.1016/j.ajog.2011.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Quick Stats: Percentage of Women Aged ≥50 Years Who have had a hysterectomy, by Race/Ethnicity and Year — National Health Interview Survey, United States, 2008 and 2018. MMWR Morb Mortal Wkly Rep. 2019;68:935. doi: 10.15585/mmwr.mm6841a3external. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomopoulos T, Zufferey G. Totally laparoscopic treatment of vaginal cuff dehiscence: A case report and systematic literature review. International Journal of Surgery Case Reports. 2016;25:79–82. doi: 10.1016/j.ijscr.2016.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cardosi RJ, Hoffman MS, Roberts WS, Spellacy WN. Vaginal evisceration after hysterectomy in premenopausal women. Obstet Gynecol. 1999;94(5 Pt 2):859. doi: 10.1016/s0029-7844(99)00530-x. [DOI] [PubMed] [Google Scholar]
- 5.Moen MD, Desai M, Sulkowski R. Vaginal evisceration managed by transvaginal bowel resection and vaginal repair. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(3):218–220. doi: 10.1007/s00192-003-1056-1. [DOI] [PubMed] [Google Scholar]
- 6.Agdi M, Al-Ghafri W, Antolin R, Arrington J, O'Kelley K, Thomson AJ. Vaginal vault dehiscence after hysterectomy. J Minim Invasive Gynecol. 2009;16(3):313–317. doi: 10.1016/j.jmig.2009.01.006. [DOI] [PubMed] [Google Scholar]
- 7.Iaco PD, Ceccaroni M, Alboni C, Roset B, Sansovini M, D'Alessandro L. Transvaginal evisceration after hysterectomy: is vaginal cuff closure associated with a reduced risk? Eur J Obstet Gynecol Reprod Biol. 2006;125(1):134–138. doi: 10.1016/j.ejogrb.2005.08.009. [DOI] [PubMed] [Google Scholar]
- 8.Hur HC, Guido RS, Mansuria SM, Hacker MR, Sanfilippo JS, Lee TT. Incidence and patient characteristics of vaginal cuff dehiscence after different modes of hysterectomies. J Minim Invasive Gynecol. 2007;14(3):311–317. doi: 10.1016/j.jmig.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen ML, Anyikam AL, Paolucci M. Vaginal cuff dehiscence with adnexal mass evisceration after abdominal hysterectomy. Int J Surg Case Rep. 2013;4(5):518–520. doi: 10.1016/j.ijscr.2013.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sterk E, Stonewall K. Vaginal cuff dehiscence - A potential surgical emergency. Am J Emerg Med. 2020;38(3):691. doi: 10.1016/j.ajem.2019.09.013. e1-.e2. [DOI] [PubMed] [Google Scholar]
- 11.Tonolini M. Multidetector CT of expected findings and complications after hysterectomy. Insights Imaging. 2018;9(3):369–383. doi: 10.1007/s13244-018-0610-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kho RM, Akl MN, Cornella JL, Magtibay PM, Wechter ME, Magrina JF. Incidence and characteristics of patients with vaginal cuff dehiscence after robotic procedures. Obstet Gynecol. 2009;114(2 Pt 1):231–235. doi: 10.1097/AOG.0b013e3181af36e3. [DOI] [PubMed] [Google Scholar]
- 13.Bleull S, Smith H, Shapiro R. Transvaginal management of vaginal cuff dehiscence with bowel evisceration following delayed diagnosis. Case Rep Obstet Gynecol. 2017;2017 doi: 10.1155/2017/4985382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Revzin MV, Mathur M, Dave HB, Macer ML, Spektor M. Pelvic inflammatory disease: Multimodality imaging approach with clinical-pathologic correlation. Radiographics. 2016;36(5):1579–1596. doi: 10.1148/rg.2016150202. [DOI] [PubMed] [Google Scholar]
- 15.Munger D, Iannamorelli M, Galvez C, Service C. Vaginal Cuff Dehiscence Presenting with Free Air 60 Days after Robotic-Assisted Hysterectomy. Case Rep Surg. 2017;2017 doi: 10.1155/2017/5052634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cole JM, Abbas PI, Kamat A, Curtis M, Bonville DJ. Vaginal Rupture and Evisceration in a Patient With Chronic Rectocele: A Case Report and Literature Review2019.