Abstract
Background
The COVID-19 pandemic has resulted in over 225,000 excess deaths in the United States. A moratorium on elective surgery was placed early in the pandemic to reduce risk to patients and staff and preserve critical care resources. This report evaluates the impact of the elective surgical moratorium on case volumes and intensive care unit (ICU) bed utilization.
Methods
This retrospective review used a national convenience sample to correlate trends in the weekly rates of surgical cases at 170 Veterans Affairs Hospitals around the United States from January 1 to September 30, 2020 to national trends in the COVID-19 pandemic. We reviewed data on weekly number of procedures performed and ICU bed usage, stratified by level of urgency (elective, urgent, emergency), and whether an ICU bed was required within 24 hours of surgery. National data on the proportion of COVID-19 positive test results and mortality rates were obtained from the Center for Disease Control website.
Results
198,911 unique surgical procedures performed during the study period. The total number of cases performed from January 1 to March 16 was 86,004 compared with 15,699 from March 17 to May 17. The reduction in volume occurred before an increase in the percentage of COVID-19 positive test results and deaths nationally. There was a 91% reduction from baseline in the number of elective surgeries performed allowing 78% of surgical ICU beds to be available for COVID-19 positive patients.
Conclusion
The moratorium on elective surgical cases was timely and effective in creating bed capacity for critically ill COVID-19 patients. Further analyses will allow targeted resource allocation for future pandemic planning.
Keywords: COVID-19, Pandemic, Surgical Volume, Surgery
Introduction
With over 225,000 excess deaths through July 20201 and per capita mortality significantly higher than almost every other country with a developed economy,2 the United States response to the COVID-19 pandemic has come under heavy scrutiny.3 While other areas of the pandemic response have been evaluated, the shutdown of elective surgical services across the US has not been widely studied. In response to the early reports of overwhelmed hospitals in China4 and Italy,5 the Centers for Medicare and Medicaid Services6 and the American College of Surgeons7 recommended a moratorium on non-emergency surgery. The impact of these efforts on the number of surgical procedures, during the surge and the subsequent recovery phase, has not been evaluated at a national level or across multiple specialties.
The Veterans Health Administration (VA) is a government-funded single payer healthcare system that oversees the care of over nine million Veterans.8 On March 17th, in response to the COVID-19 pandemic, the VA deferred elective surgeries in order to provide surge capacity for Veterans and for potentially overwhelmed civilian healthcare institutions. The VA is uniquely positioned to provide data on the national impact of COVID-19 as it provides care at 170 acute care hospitals and 1,236 additional healthcare facilities across all states and federal districts of the US. We reviewed all surgical procedures performed at a VA facility before, during and after the initial surge of the pandemic to determine its impact on services and to establish patterns that might aid in further planning.
Methods
Study data were obtained from the VA Informatics and Computing Infrastructure database which stores all information obtained from the VA's electronic medical record (Computerized Patient Record System) which is used at all VA facilites.9 These data contain patient-specific information about outpatient encounters, inpatient admissions, transfers and procedures performed for every VA hospital in the country. Details about admission, discharge and transfer location are contained down to the level of each specific hospital ward. The study was approved by the University of Maryland Institutional Review Board and the VA Research and Development Office (IRB number HP-00090879) and the requirement for informed consent was waived.
We gathered information on all unique procedures performed in an operating room, including date, case urgency (elective, urgent and emergency) and current procedural terminology code, and need for post-operative surgical intensive care unit (ICU) admission. We separately identified all COVID-19 positive patients, regardless of whether they had surgery or not, requiring ICU admission between January 1, 2020 and September 30, 2020.There are separate labels for medical and surgical ICU admissions in the VA Informatics and Computing Infrastructure database. Unique patient identifiers associated with elective surgical procedures were matched with surgical ICU admissions within 24 hours of the date and time of surgery. Procedures and ICU bed utilization were aggregated on a weekly basis. National data on proportion of COVID-19 positive test results and mortality rates were obtained from the United States Department of Health and Human Services and Centers for Disease Control and Prevention websites.10 , 11
Finally, we used linear regression to determine the relationship between reduction in the number of elective surgical procedures performed per week and the number of ICU admissions for elective surgical procedures throughout the entire study period.
Results
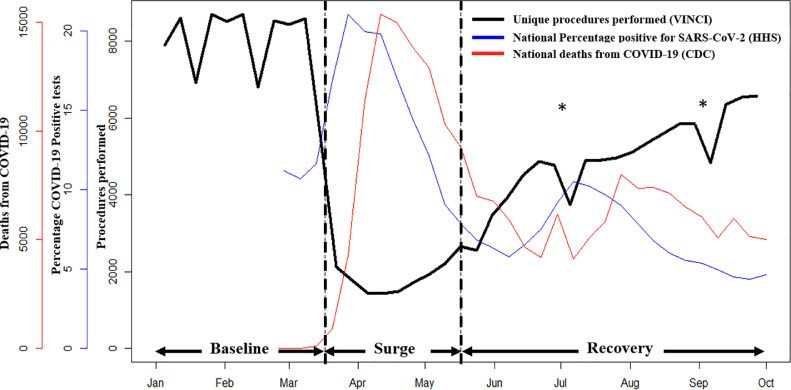
A total of 198,911 surgical procedures were performed between January 1 and September 30, 2020 at VA facilities nationwide. We identified three phases in response to the moratorium on elective procedures: a baseline phase from January 1 to March 16, a primary surge phase from March 17 through May 17, and a recovery phase from May 18 until September 30 (Fig. 1 ). There was a large decrease in the number of procedures performed upon issuance of the moratorium on March 17. The total number of cases performed from January 1 to March 16 was 86,004 compared with 15,699 from March 17 to May 17. The reduction in volume corresponded with an increase in the percentage of COVID-19 positive tests among all the tests performed nation-wide and in the national COVID-related mortality numbers (Fig. 1). The number of procedures performed did not increase above the nadir until the middle of April. An increase in procedures began gradually and corresponded with a consistently reducing trend in COVID-19 related mortality, both occurring in mid-April 2020. After this, there has been a steady increase in the number of procedures, corresponding with a decline in the COVID-19 mortality rate. During the recovery phase, there were two short-lived drops in case volumes that corresponded with government holidays- Independence Day (July 4) weekend and Labor Day (September 7).
Fig. 1.
The weekly number of surgical procedures performed at all Veterans Affairs Hospitals nationally between January 1 and September 30 2020 (black line, black axis), compared to national trends in percentage COVID-19 positivity (blue line, blue axis) and deaths due to COVID-19 (red line, red axis) in the United States. VINCI, Veterans Affairs Informatics and Computing Infrastructure; HHS, United States Department of Health and Human Services; CDC, Centers for disease control and prevention. *Drops in weekly procedures performed correspond with government holidays- Independence Day (July 4) and Labor Day (September 7). (Color version of figure is available online)
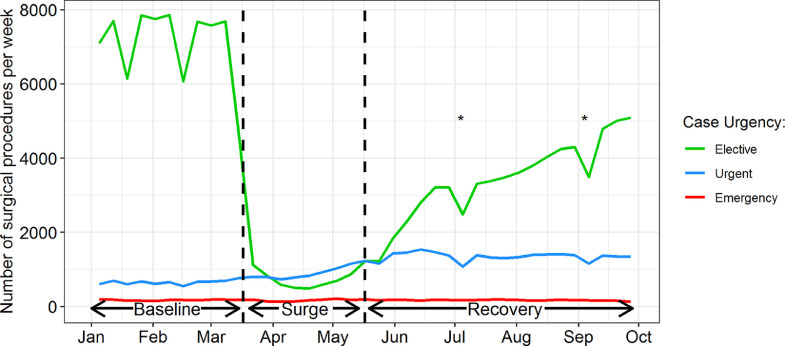
There was a 91% reduction from baseline in the number of elective procedures during the surge phase (Fig. 2 ). By mid-May the elective case volume began recovering and had returned to around 66% of baseline by the last week of September. Urgent procedures slowly increased during the surge and continued to do so early into the recovery phase, after which they have plateaued at twice the baseline (601/week versus 1,363/week). The largest proportional increase in urgent procedures during the surge occurred for urological (2.7 times baseline) and ophthalmological (1.6 times baseline) organ systems. The number of emergency cases remained stable from baseline through the surge and into the recovery phase.
Fig. 2.
The weekly number of surgical procedures performed at all Veterans Affairs Hospitals nationally between January 1 and September 30 2020 comparing volumes by case urgency- elective (green), urgent (blue) and emergency (red). *Drops in weekly procedures performed correspond with government holidays- Independence Day (July 4) and Labor Day (September 7). (Color version of figure is available online)
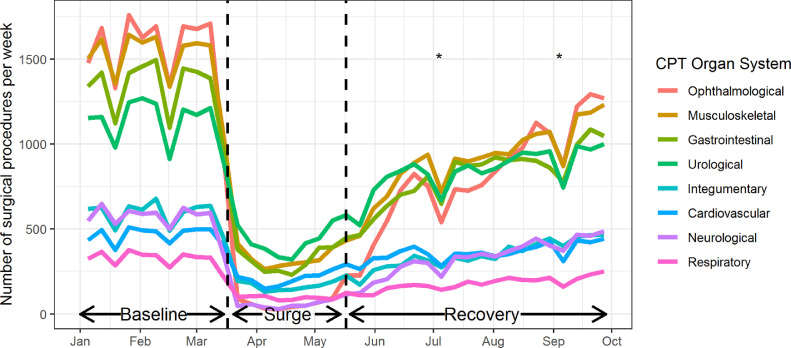
The most performed procedures during the baseline period by organ system were ophthalmological, musculoskeletal, gastrointestinal and urological (Fig. 3 ). During the surge period, the relative frequency distribution of procedures performed remained consistent, with the exception of ophthalmological procedures, which became the second least common (Table 1 ). Cardiovascular procedures dropped the least (44% of baseline); followed by urological procedures (38% of baseline), respiratory procedures (30% of baseline), and integumentary procedures (28% of baseline). During the recovery period, procedures on all organs systems demonstrated a linear increase to 52%-78% of baseline capacity by September 30.
Fig. 3.
The weekly number of surgical procedures performed by organ system, as defined by the first two digits of procedural current procedural terminology code, at all Veterans Affairs Hospitals nationally between January 1, 2020 and September 30 2020. *Drops in weekly procedures performed correspond with government holidays- Independence Day (July 4) and Labor Day (September 7). (Color version of figure is available online)
Table 1.
Average number of procedures performed in an operating room per week at Veterans Affairs hospitals nationally, divided by organ system.
| Baseline | Surge |
Recovery |
|||
|---|---|---|---|---|---|
| CPT organ system | Average number of procedures per week | Average number of procedures per week | % of baseline | Average number of procedures per week | % of baseline |
| Ophthalmological | 1,537.9 | 58.3 | 3.8 | 803.1 | 52.2 |
| Musculoskeletal | 1,497.1 | 324.1 | 21.7 | 891.3 | 59.5 |
| Gastrointestinal | 1,323.8 | 311.9 | 23.6 | 802.8 | 60.6 |
| Urological | 1,130.0 | 423.5 | 37.5 | 836.0 | 74.0 |
| Integumentary | 587.9 | 163.3 | 27.8 | 343.9 | 58.5 |
| Neurological | 560.5 | 54.3 | 9.7 | 325.1 | 58.0 |
| Cardiovascular | 462.9 | 205.0 | 44.3 | 359.2 | 77.6 |
| Respiratory | 323.4 | 95.3 | 29.5 | 177.1 | 54.8 |
CPT = Current procedural terminology.
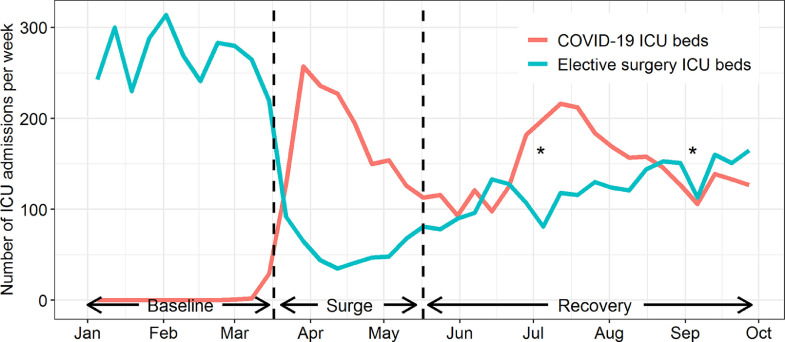
During the baseline period a total of 77,640 elective procedures were performed, of which 2865 (4%) required surgical ICU admission. This accounted for 67% (2865/4305) of all surgical ICU admissions, with urgent and emergency procedures accounting for the remainder. During the surge 7,007 elective procedures were performed of which 534 (8%) required surgical ICU beds. This accounted for 28% (534/1881) of all surgical ICU admissions. The weekly mean ± standard deviation number of elective procedures requiring postoperative surgical ICU admission dropped from 267 ± 30 at baseline to 58 ± 20 in the surge phase (78% decrease). This coincided with and was sufficient to accommodate the increasing number of COVID-19 positive patients requiring ICU admissions (Fig. 4 ). A linear model with weekly ICU bed utilization by surgical patients as the dependent variable and weekly elective procedures performed as the independent variable showed that 1 surgical ICU bed was saved for every 300 fewer elective procedures performed (model R20.95, P < 0.001).
Fig. 4.
The weekly number of elective surgical procedures performed that required intensive care unit admission (green line) compared to COVID-19 patients requiring intensive care unit admission (red line) at all Veterans Affairs Hospitals nationally between January 1st and September 30 2020. *Drops in weekly procedures performed correspond with government holidays- Independence Day (July 4) and Labor Day (September 7). (Color version of figure is available online)
Discussion
This represents the first report of the nationwide impact of COVID-19 on surgical services in the United States. The response implemented for the pandemic resulted in a 91% reduction in the number of elective procedures during the surge. The response was timely in that the drop in volume was accomplished prior to an increase in the proportion of people testing positive for, and total number of people dying from COVID-19 nationwide. The recovery in surgical volume commenced by May 17, aligned well with falling COVID-19 related mortality in the US population, and corresponded with executive orders from state authorities on resumption of elective surgery.12 Procedural volumes had still not returned to baseline levels by September 30, 2020.
There was an increase in the number of cases coded as urgent during the surge and recovery phases of the pandemic. This may reflect increased disease severity, either as a result of delayed presentation to the hospital, or from COVID-19 infection-related complications. Alternatively, surgeons may be more inclined to code their cases as urgent in order to expedite the treatment of time-sensitive surgical pathology after the lockdown.
The reduction in elective procedural volume successfully released 78% of surgical intensive care beds with their attendant critical care and ventilatory support resources at VA facilities. There was an average weekly increase in the availability of 209 ICU beds during the surge when compared to baseline levels. Although a simple linear model of national procedural volume does not capture regional or procedure-specific variation, it suggests that the moratorium on elective surgery was a successful strategy for conserving resources to accommodate surge-related critical care demands.
Although the national moratorium on elective surgery provided adequate ICU bed capacity to absorb the increase in COVID-19 related ICU usage, the uneven geographic distribution of COVID-19 cases across the country likely created inefficiencies in where this ICU capacity was available. The wider implication for these data is the potential to provide regional statistical models that allow hospital leadership to adjust regional elective surgical services to provide capacity for anticipated COVID-19 demand. This would allow a more nuanced approach to surgical service restrictions based on regional infection transmission rates. It is likely that changes in local surgical case volumes were also influenced by state policies.
The VA healthcare system largely serves a cohort of older men with high comorbidity burden. As such, we are cautious in directly translating these results to community and academic hospitals that serve a wider population that were not represented in our sample, such as women and children. It is also worth noting that large tertiary care centers have a wide catchment area and accept transfers with critical ill COVID-19 patients from surrounding states. Also, the financial implications of reductions in elective surgical volume cannot be modelled effectively with data from the VA, a single-payer government funded institution. The goal of this analysis was not focused on evaluating ICU or general bed capacity. Indeed, this would likely be a difficult task since there was nation-wide variability and ongoing changes in creation of additional bed capacity in response to the pandemic. Our goal was to quantify ICU bed utilization by comparing number of admissions across different time periods. While most Veterans preferentially continue their care within the VA system, we did not have data on the small proportion that may have been treated at a non-VA facility. The VA's unified national medical records provide important information on the broad impact of the COVID-19 pandemic on surgical services across the country. A more detailed assessment of geographic variations in surgical services versus COVID-pandemic severity will facilitate further fine-tuning of the healthcare response to future surges or the next healthcare crisis. Although beyond the scope of this analysis, a more detailed study of various health system resources including ventilator, acute care bed, rehabilitation bed, and skilled nursing facility bed use associated with elective surgery will provide a more comprehensive assessment of how policy makers and administrators can adjust elective surgery case volume to safeguard overall healthcare resources during health crises.
The presented data on the VA's national response to the COVID-19 pandemic show that it is possible to generate a swift reduction in surgical case volume in the face of an emerging public health crisis. The back log of elective surgical cases must be balanced with the risk of COVID-19 transmission by considering: (1) the rate of regional COVID-19 transmission, (2) the local rate of ICU bed utilization by elective surgical patients, and (3) the local rate of ICU bed utilization by COVID-19 patients. In restoring surgical services, it may be necessary to prioritize cardiovascular and oncological services due to the time-sensitive nature of these procedures and potential for further surges necessitating periods of reduced activity.
Conclusion
The COVID-19 pandemic has placed an immense strain on healthcare systems around the United States and globally. Empirical evidence of national trends in surgical services within the VA system during the pandemic surge indicate that the restriction in elective surgery was timely and successful in conserving enough critical care resources to accommodate the increased COVID-related demands. These practice patterns provide feedback on the implementation of strategies for the provision and optimization of non-COVID patient care, as healthcare systems are forced to make difficult decisions about resource allocation during different phases of the pandemic.
Author Contributions
BKL conceived and designed the study. NP, TS, MMC, and RL collected data. NP, TS, MMC, RL, BE and JDS analyzed and interpreted data. All authors provided critical revisions and approved the final version of the manuscript.
Acknowledgment
This work was supported by the Veterans Affairs awards HSRD C19-20-407, RRD RX000995 and CSRD CX001621, and NIH awards NS080168, NS097876 and AG000513 (BKL); National Institutes of Health awards AG028747, DK072488 (JDS); National Institutes of Health T32 AG00262 (NKP)
Disclosure
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
References
- 1.Woolf SH, Chapman DA, Sabo RT, Weinberger DM, Hill L, Taylor DDH. Excess deaths from COVID-19 and other causes, March-July 2020. JAMA. 2020 doi: 10.1001/jama.2020.19545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bilinski A, Emanuel EJ. COVID-19 and excess all-cause mortality in the US and 18 comparison countries. JAMA. 2020 doi: 10.1001/jama.2020.20717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Editors Dying in a leadership vacuum. N Engl J Med. 2020 doi: 10.1056/NEJMe2029812. [DOI] [PubMed] [Google Scholar]
- 4.Lei S, Jiang F, Su W, et al. EClinicalMedicine; 2020. Clinical Characteristics and Outcomes of Patients Undergoing Surgeries During The Incubation Period of COVID-19 Infection. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doglietto F, Vezzoli M, Gheza F, et al. Factors associated with surgical mortality and complications among patients with and without coronavirus disease 2019 (COVID-19) in Italy. JAMA Surg. 2020 doi: 10.1001/jamasurg.2020.2713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Medicare and Medicaid Services. Non-emergent, elective medical services, and treatment recommendations. https://www.cms.gov/Files/Document/31820-Cms-Adult-Elective-Surgery-and-Procedures-Recommendations.Pdf. Published 2020. Accessed September 28, 2020.
- 7.American College of Surgeons. COVID-19: Guidance for Triage of Non-Emergent Surgical Procedures. https://www.facs.org/covid-19/clinical-guidance/triage. Published 2020. Accessed September 28, 2020.
- 8.Veterans Affairs Health Administration . 2020. U.S. Department of Veterans Affairs.https://www.va.gov/health/ PublishedAccessed September 15, 2020. [Google Scholar]
- 9.U.S. Department of Veterans Affairs . 2018. VA Informatics and Computing Infrastructure (VINCI) homepage.https://www.hsrd.research.va.gov/for_researchers/vinci/ Accessed September 28, 2020. [Google Scholar]
- 10.United States Department of Health and Human Services. COVID-19 Diagnostic Laboratory Testing (PCR Testing) Time Series | HealthData.gov. https://healthdata.gov/dataset/covid-19-diagnostic-laboratory-testing-pcr-testing-time-series. Published 2020. Accessed October 15, 2020.
- 11.Centers for Disease Control and Prevent. Provisional COVID-19 Death Counts by Sex, Age, and State | Data | Centers for Disease Control and Prevention. https://data.cdc.gov/NCHS/Provisional-COVID-19-Death-Counts-by-Sex-Age-and-S/9bhg-hcku/data. Published 2020. Accessed October 15, 2020.
- 12.American College of Surgeons . 2020. COVID-19: Executive Orders by State on Dental, Medical, and Surgical Procedures.https://www.facs.org/covid-19/legislative-regulatory/executive-orders Published. [Google Scholar]