Abstract
The coronavirus (COVID-19) pandemic has impacted young adults across a number of different domains. It is critical to establish the degree to which the COVID-19 pandemic has affected mental health and identify predictors of poor outcomes. Neuroticism and (low) respiratory sinus arrhythmia (RSA) are risk factors of internalizing disorders that might predict increased psychopathology symptoms. The present study included 222 undergraduate students from [name removed] in Long Island, NY. Before the COVID-19 pandemic, participants completed self-report measures of neuroticism and internalizing symptoms and an electrocardiogram. Between April 15th to May 30th, 2020, participants again completed the measure of internalizing symptoms and a questionnaire about COVID-19 experiences. The COVID-19 pandemic was associated with increased distress, fear/obsessions, and (low) positive mood symptoms. There was a Neuroticism x RSA interaction in relation to distress symptoms, such that greater pre-COVID-19 neuroticism was associated with increased distress symptoms, but only in the context of low RSA. These findings suggest the COVID-19 pandemic has contributed to increased internalizing symptoms in young adults, and individuals with specific personality and autonomic risk factors may be at heightened risk for developing psychopathology.
Keywords: COVID-19, Respiratory sinus arrhythmia, Neuroticism, Internalizing symptoms
1. Introduction
The coronavirus (COVID-19) pandemic has been an unprecedented crisis that has led to profound life changes. On January 21st, 2020, the first case of COVID-19 was identified in the U.S., and transmission accelerated from February to March, especially in higher density areas (Schuchat, 2020). By March 22nd, New York City was a global epicenter of the pandemic, accounting for over 5% of cases worldwide (Evelyn, 2020). On April 9th, there were more confirmed cases of COVID-19 in the state of New York than any other country (Winsor et al., 2020). Urgent measures were taken to control the spread of COVID-19, including a state-wide shelter-in-place order, and individuals had to adapt to shifting restrictions, home confinement, unexpected financial strain, and uncertainty regarding risk of infection.
The COVID-19 pandemic has been particularly stressful for college students. Many universities closed their dorms and moved to online instruction, which forced many students to suddenly move back home with their families or find new places to live (Gatteau & Bauman, 2020; Governor Cuomo's Press Office, 2020). Consequently, students had to cope with more challenging learning environments, occupational insecurity, and social isolation.
Emerging evidence suggests that life changes and strict lockdown measures have taken a significant toll on mental health, especially for those living in areas most affected by the pandemic (Brooks et al., 2020; Taquet et al., 2020). In a recent review about eight countries affected by the COVID-19 pandemic, results indicated that prevalence rates of anxiety and depression reached up to 51% and 48%, respectively (Xiong et al., 2020). Thus, initial evidence suggests that the COVID-19 pandemic has had a notable impact on internalizing disorders. Additionally, recent studies have found that college student status may be associated with greater psychopathology during COVID-19, including increased anxiety and depressive symptoms (Cao et al., 2020; Xiong et al., 2020).
There are still notable gaps in the literature on the COVID-19 pandemic and mental health. The majority of research aimed at characterizing the effect of the pandemic on mental health have been largely limited to samples from China and Europe. COVID-19 related experiences and increased psychopathology symptoms may vary as a function of geographical location, spread of disease, and government response, and it is critical to determine whether initial results generalize to other regions. Moreover, most studies have failed to consider what specific aspects of the COVID-19 pandemic contribute to changes in psychopathology, and it is unclear whether the pandemic is having a global impact on mental health or more specific experiences are associated with particular disorders and symptoms. Finally, few studies have examined longitudinal, within-person changes in symptoms among U.S. samples, and even fewer have sought to examine predictors of poor outcomes (Lee et al., 2020; Zhou et al., 2020). Thus, the current study aims to examine longitudinal, within-person changes in internalizing symptoms, pandemic-related experiences contributing to changes in symptoms, and pre-pandemic predictors of changes in symptoms among a U.S. population situated in one of the epicenters of the pandemic.
The Five-Factor Model is one of the most utilized and well-supported models of personality. This model purports that personality can be defined by five dimensional traits: neuroticism, extraversion, agreeableness, conscientiousness, and openness (McCrae & John, 1992). The Five-Factor Model has gained much traction over recent years, leading many researchers to investigate its links to psychopathology. Though research supports relationships between all five traits and various forms of psychopathology (Malouff et al., 2005), particular traits have shown more consistent, general relationships with psychopathology disorders and symptoms. Neuroticism, which reflects a trait disposition to experience negative emotions (Lahey, 2009), has often emerged as a robust, nonspecific risk factor for psychopathology (Klein et al., 2011). Research indicates that neuroticism shows strong relationships with internalizing disorders, suggesting that it may reflect a general liability for psychopathology (Kotov et al., 2010; Tackett et al., 2008). Indeed, initial evidence has indicated that greater neuroticism was associated with increased stress (Liu et al., 2020) and predicted increased negative affect (Kroencke et al., 2020) during the COVID-19 pandemic.
Heart rate variability (HRV) is another well-established transdiagnostic marker of risk for psychopathology (Beauchaine & Thayer, 2015). HRV is a measure of the autonomic nervous system's ability to flexibly respond and adapt to challenging stimuli in the environment Respiratory sinus arrhythmia (RSA) is an indicator of HRV that is thought to index vagal control of the parasympathetic nervous system. Like HRV, RSA is measured by examining the variations in time between consecutive heart beats, but, unlike HRV, RSA specifically examines this variation during respiration cycles. RSA measures the increase in heart rate during inhalation and a decrease in heart rate during exhalation. Thus, RSA is a measure of the parasympathetic modulation of the heart via the vagus nerve. Research suggests that lower resting RSA indexes poorer emotion regulation and executive functioning capabilities (Beauchaine, 2015; Hamilton & Alloy, 2016). Meta-analyses have found that blunted RSA is associated with anxiety and depressive disorders (Chalmers et al., 2014; Koenig et al., 2016) and is a marker of depression symptom severity and response to treatment (Chambers & Allen, 2002). However, no studies have examined whether RSA predicts changes in internalizing symptoms during the COVID-19 pandemic.
1.1. Present study
The present study aimed to: 1) investigate longitudinal, within-person changes in internalizing symptoms in a sample of college students living in one of the epicenters of the COVID-19 pandemic in New York, 2) identify specific pandemic related experiences that may be contributing to the rise in internalizing symptoms, and 3) conduct analyses examining pre-COVID-19 neuroticism and RSA as predictors of changes in internalizing symptoms. Pre-COVID-19 self-report measures of neuroticism, anxiety, and depression as well as RSA were collected from undergraduate students. Following the COVID-19 outbreak in New York, participants were invited to complete a follow-up assessment between April 17th and May 30th, which coincided with a spike in COVID-19 cases and shelter-in-place orders. The follow-up assessment included self-report measures of internalizing symptoms and COVID-19-related experiences. We hypothesized that there would be increased internalizing symptoms during the COVID-19 pandemic. We also conducted analyses examining what COVID-19 experiences were associated with changes in internalizing symptoms. Finally, given that high neuroticism and a blunted RSA have been associated with greater psychopathology, we hypothesized that greater neuroticism and lower RSA would predict greater increases in psychopathology. We also conducted an exploratory analysis examining whether there was an interaction between neuroticism and RSA in relation to changes in psychopathology. We hypothesized that the combination of both high neuroticism and blunted RSA would predict the greatest increases in psychopathology. We aimed to add to the extant literature highlighting the importance of neuroticism and RSA as a risk factors for psychopathology by examining whether these risk factors predicted sudden changes in internalizing symptoms in the context of a global pandemic.
2. Methods
2.1. Participants and procedures
Participants were undergraduate students from Stony Brook University in Long Island, New York. Between May 2018 and February 2020, participants (N = 893) completed self-report measures of personality and depression and anxiety symptoms as well as an electrocardiogram (ECG) while at rest as a part of 3 larger studies (see Supplemental Materials for more details). Exclusion criteria were an inability to read or write English, age less than 17 years old, or a lifetime history of a neurological disorder. Each study protocol was approved by Stony Brook University's Institutional Review Board.
All participants were invited to complete an online COVID-19 follow-up assessment that consisted of self-report measures of internalizing symptoms and COVID-19-related experiences, of which 229 students participated. Seven participants were excluded from analyses due to their absence of the RSA data, resulting in a final sample of 222 participants.
Participants ranged from 17 to 40-years-old (M = 19.6 years, SD = 2.50 years). The sample was predominantly female (75.7%) and spoke English as their first language (65.3%). Participant racial/ethnic identity included 46.4% Asian, 28.8% White, 12.6% Latinx, 5.4% Black, and 6.8% “Other”.
2.2. Measures
2.2.1. Pre and during COVID-19
2.2.1.1. Inventory of depression and anxiety symptoms (IDAS-II)
The IDAS-II is a 99-item self-report questionnaire that measures a range of depression, anxiety, and bipolar symptoms over the past two weeks (Watson et al., 2012). Each symptom is rated on a 5-point Likert scale from not as all (1) to extremely (5). Individual items are scored to create a total of 18 subscales. In the present study, the IDAS-II was used a diagnostic screener. Additionally, distress, fear/obsessions, and positive mood symptom composites were calculated using the factor weights from Watson et al. (2012) that has since been replicated using normed data (Nelson et al., 2018). The IDAS-II demonstrated good to excellent internal consistency at the pre-COVID-19 and COVID-19 assessment (α ranged from 0.71–0.88 and 0.73–0.90, respectively).
2.2.2. Pre COVID-19
2.2.2.1. Big Five Inventory (BFI)
The BFI (John & Srivasta, 1999) is a 44-item self-report questionnaire of the Big Five personality traits. All questions are answered on a 5-point Likert scale ranging from strongly disagree (1) to strongly agree (5). Higher scores on each trait subscale reflect greater presence of the trait. The present study focused on the 8-item neuroticism subscale (α = 0.80).
2.2.2.2. Respiratory sinus arrhythmia (RSA)
ECG was recorded during a 4-to-6-min rest period at the beginning of the lab session (see Supplemental Materials for more details). All ECG data were recorded via two sintered Ag/AgCl electrodes as part of the Biosemi ActiveTwo System (Cortech Solutions, Wilmington, North Carolina). Once participants were seated in a sound-attenuated booth, two electrodes were placed on participants to record heart rate: one on the sternum and the other below the left clavicle. ECG data acquisition used a bandpass filter of DC-200 Hz at a sampling rate of 1024 Hz.
All ECG data were initially processed using QRSTool (Allen et al., 2007), and all artifacts were identified and corrected by hand. After initial correction, inter-beat interval series were extracted for each recording block. Next, each block was entered into CardioEdit (Brain-Body Center, University of Illinois at Chicago; for more details see Lewis et al., 2012) for visual inspection and artifact correction. After data were processed, average RSA was calculated using CardioBatch.
2.2.3. COVID-19
2.2.3.1. Pandemic experiences survey
We created a survey designed to assess various life changes and concerns related to the COVID-19 pandemic. This 26-item self-report questionnaire contains a range of question types, including “check all that apply,” Yes/No, and multiple-choice, that make up five subscales: life changes (14 items), concerns about infection (2 items), concerns about school (4 items), concerns about home confinement (3 items), and concerns about basic needs (3 items). Higher scores on these subscales indicate more life changes or greater concerns.
2.3. Data analysis
A repeated-measures analysis of covariance (ANCOVA) was used to examine change in IDAS-II symptoms. Mean-centered age at the pre-COVID-19 assessment was entered as a covariate to control for potential developmentally-normative symptom increases from pre-COVID-19 to COVID-19. Age at the pre-COVID-19 assessment was entered as a covariate, and time (pre-COVID-19 vs. COVID-19) was entered as a within-subject factor. Cohen's d was calculated as an effect size index of the magnitude of difference between IDAS- II. IDAS-II symptom change was examined for all 18 subscales, but only the distress, fear/obsessions, and positive mood symptom composites were examined for the analyses involving COVID-19 experiences, neuroticism, and RSA. We chose to focus our analyses on the higher-order symptom composites to limit the number of overall analyses and because there were no a priori hypotheses regarding specific symptom subscales.
The relationships between change in IDAS-II symptom composites and pandemic experiences were examined with a multi-step analytical approach. First, symptom composite residuals were computed by regressing pre-COVID-19 symptoms on COVID-19 symptoms. Second, partial correlations between the symptom composite residuals and pandemic experiences were conducted, adjusting for age at the pre-COVID-19 assessment, time between assessments, and pre-COVID-19 study type. Finally, multivariable linear regressions were conducted to examine the unique associations between the symptom composite residuals and pandemic experiences. Symptom composite residual of interest served as the dependent variable while age at the pre-COVID-19 assessment, time between assessments, pre-COVID-19 study type, other symptom composite residuals, and all pandemic experiences composites were included as independent variables. Separate analyses were conducted for all three symptom composite residuals.
Next, we employed partial correlations separately for each pre-COVID-19 predictor (neuroticism and RSA) and symptom composite residuals, once again adjusting for age at the pre-COVID-19 assessment, time between assessments, and pre-COVID-19 study type. Finally, a multiple linear regression was conducted to determine the interaction between neuroticism and RSA in relation to change in symptom composites. The Johnson-Neyman approach was used to elucidate the RSA values in which a significant relationship exists between neuroticism and change in symptoms. All analyses were computed in IBM SPSS Statistics 26.0, and the Finsaas and Goldstein (2020) approach was used for identifying the region of significance.
3. Results
3.1. Psychiatric symptoms
Table 1 displays descriptive and inferential statistics for IDAS-II symptom composites before and during the COVID-19 pandemic.1 The IDAS-II symptom composites showed small to large effect size changes.
Table 1.
IDAS-II symptom composites before and during the COVID-19 pandemic.
| Pre-COVID-19 |
COVID-19 |
F | p | Cohen's d | |
|---|---|---|---|---|---|
| M (SD) | M (SD) | ||||
| Distress | 72.72 (25.47) | 84.61 (28.15) | 56.91 | <.001 | 0.51 |
| Fear/obsessions | 34.0 (12.11) | 39.03 (13.23) | 32.37 | <.001 | 0.38 |
| Positive mood | 21.84 (6.79) | 17.12 (5.75) | 154.42 | <.001 | −0.84 |
Note. IDAS-II = Inventory of Depression and Anxiety Symptoms; M = mean; SD = standard deviation.
As shown in Table 2 , an increase in distress symptoms was associated with a greater number of life changes and both concerns about infection and basic needs. An increase in fear/obsessions symptoms was associated with greater concerns about infection and basic needs. A decrease in positive mood symptoms was associated with greater concerns about school and home confinement.
Table 2.
Partial correlations between change in internalizing symptoms and COVID-19 experiences.
| Pandemic experiences | IDAS-II symptom dimensions |
||
|---|---|---|---|
| Distress | Fear/obsessions | Positive mood | |
| Life changes | .14⁎ | .13 | −.05 |
| Infection concerns | .16⁎ | .24⁎⁎ | −.08 |
| School concerns | .12 | .02 | −.25⁎⁎⁎ |
| Home confinement concerns | .08 | .04 | −.29⁎⁎⁎ |
| Basic needs concerns | .18⁎⁎ | .21⁎⁎ | −.05 |
Note. IDAS-II = Inventory of Depression and Anxiety Symptoms.
p < .05.
p < .01.
p < .001.
As shown in Table 3 , an increase in the fear/obsession symptoms was uniquely associated with greater concerns about infection. A decrease in the positive mood symptoms was associated with greater concerns about school and home confinement.
Table 3.
Standardized beta coefficients for independent relationship between change in depression and anxiety symptoms and COVID-19 experiences.
| Pandemic experiences | IDAS-II symptom dimensions |
||
|---|---|---|---|
| Distress | Fear/obsessions | Positive mood | |
| Life changes | .02 | .03 | .03 |
| Infection concerns | −.04 | .12⁎⁎ | −.08 |
| School concerns | .06 | −.06 | −.15⁎ |
| Home confinement concerns | −.03 | .05 | −.23⁎⁎⁎ |
| Basic needs concerns | .01 | .07 | −.01 |
Note. IDAS-II = Inventory of Depression and Anxiety Symptoms.
p < .05.
p < .01.
p < .001.
3.2. Predictors of symptom changes
As shown in Table 4 , neuroticism was the only pre-pandemic risk factor associated with change in the IDAS-II symptom composites. Specifically, greater pre-COVID-19 neuroticism was associated with greater increases in the distress symptoms and decreases in the positive mood symptoms.
Table 4.
Partial correlations between personality, RSA, and change in internalizing symptoms.
| Predictors | IDAS-II symptom dimensions |
||
|---|---|---|---|
| Distress | Fear/obsessions | Positive mood | |
| Neuroticism | .15* | .06 | −.16* |
| RSA | −.04 | −.08 | .02 |
Note. IDAS-II = Inventory of Depression and Anxiety Symptoms.
* p < .05, ** p < .01, *** p < .001.
We were interested in investigating whether RSA moderated the association between neuroticism and any of the internalizing symptom composites. Three regression models were explored, and all models included age at the pre-COVID-19 assessment, time between assessments, and pre-COVID study type as covariates. Of the three models, only the model predicting distress symptoms showed a significant interaction between neuroticism and distress after adjusting for covariates, F(7,214) = 3.293, p = .002; R 2 = 0.097. Neuroticism also independently predicted increases in distress (β = 2.96, p = .046) and decreases in positive mood symptoms (β = −0.76, p = .017).
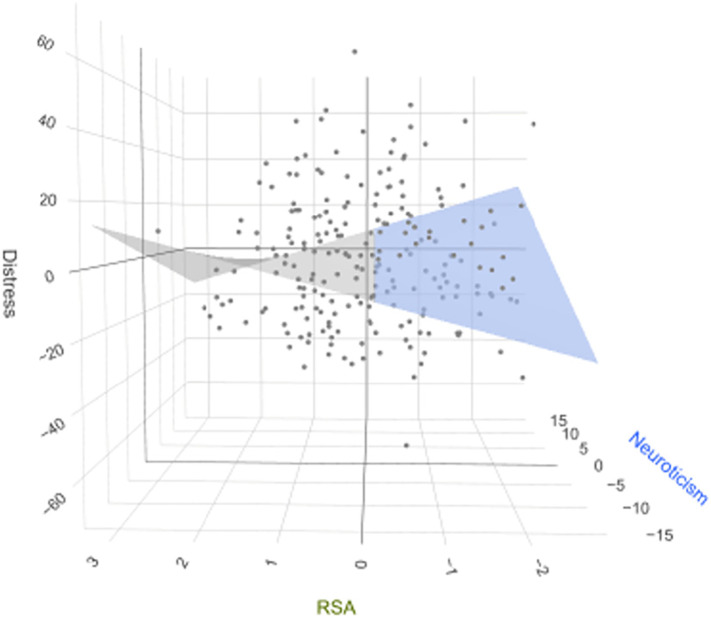
Fig. 2 presents a visualization of the resulting Neuroticism by RSA interaction predicting distress symptoms using the Johnson-Neyman approach. Results indicated a significant Neuroticism x RSA interaction, β = −2.91; p = .042, and the Johnson-Neyman technique revealed a significant relationship between neuroticism and residual distress symptoms when RSA was below −0.13 (below the mean) (p < .05; 46% of sample), but not at higher levels (p > .05; 54% of sample). This interval was calculated using false discovery rate adjusted t = 2.31 (Esarey & Sumner, 2018).
Fig. 2.
3D plot illustrating the conditional effect of neuroticism on residual distress symptoms as function of RSA. The blue represents the region of significance (ROS) where the relationship between neuroticism and residual distress symptoms is statistically significant (−0.16 ≥ RSA ≥ −2.80; ROC includes 46% of the sample), which is determined using the Johnson-Neyman technique. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
4. Discussion
The present study examined longitudinal, within-person changes in internalizing symptoms from before to during the COVID-19 pandemic in a sample of college students living in a major epicenter of the pandemic. In line with our hypothesis, participants experienced within-person increases in symptoms with effect sizes ranging from small to large. Further, we found that specific COVID-19 related concerns were uniquely associated with fear/obsessions and positive mood symptom changes. Regression analyses revealed that pre-COVID-19 neuroticism predicted increased distress symptoms, but only among those with low RSA. Altogether, these results underscore the detrimental mental health consequences of the COVID-19 pandemic and suggest that college students with a combination of autonomic and personality risk factors may be an especially vulnerable population during the pandemic.
The positive mood symptom composite showed the largest within-person change, such that positive mood decreased during COVID-19. In contrast, change in distress symptoms showed a medium effect size, and change in fear/obsession symptoms showed a small effect size. Our analyses controlled for pre-COVID-19 assessment age, so it is unlikely that any resulting changes in symptoms are a product of normative developmental increases in internalizing symptoms. The present study is largely consistent with the extant cross-sectional and limited domestic longitudinal data showing high rates of stress and internalizing symptoms among adults during the early months of the pandemic (Xiong et al., 2020; Zhou et al., 2020). Overall, these results contribute to the growing body of literature seeking to understand the adverse mental health impact of the COVID-19 pandemic.
Although our findings show an overall worsening of internalizing symptoms across participants during the pandemic, these changes seem to be driven by specific pandemic-related experiences. For instance, greater basic need concerns and infection concerns were both associated with greater fear/obsessions symptoms. Increased distress symptoms were also associated with infection concerns and basic needs concerns, but additionally increased life changes. Conversely, lower positive mood symptoms were associated with greater school concerns and home confinement concerns. Given that each symptom composite showed a unique relationship with COVID-19- related experiences, with the exceptions of basic needs concerns and infection concerns, this suggests that different aspects of the pandemic may be contributing to particular changes in internalizing symptoms.
Controlling for all other symptom dimensions, multivariable linear regression analyses indicated that infection concerns, which included concerns regarding a COVID-19 infection and the perceived likelihood of infection, were independently related to increases in the fear/obsessions symptom composite. These results suggest that living near an epicenter of the pandemic where the likelihood of infection is high may uniquely contribute to increases in fear/obsessions related symptoms. Conversely, school concerns and home confinement concerns were both independently associated with decreases in the positive mood symptom composite. This provides evidence to suggest that school-related challenges, such as the sudden transition to online teaching platforms, as well as strict lockdown measures, may be contributing to lower positive mood. The distress symptom composite showed no independent associations with specific COVID-19 pandemic experiences, indicating that while pandemic experiences may have some independent relationships with symptom changes, these experiences may also be contributing to a higher order factor (e.g., broader internalizing dimension), which is associated with changes across all three internalizing symptom composites.
The present study found that greater pre-COVID-19 neuroticism predicted increased distress and decreased positive mood symptoms. This result is consistent with extant personality literature indicating the neuroticism is a robust predictor of psychopathology (Klein et al., 2011). The present study also found an interaction between neuroticism and RSA in relation to increased distress symptoms during the COVID-19 pandemic. These results are consistent with prior international studies showing that individuals with higher levels of neuroticism are more likely to experience increased stress and negative affect during COVID-19 (Kroencke et al., 2020; Liu et al., 2020). However, the current study extends these findings by using more comprehensive measures of psychopathology to assess for within-person symptom changes and examining neuroticism in conjunction with an autonomic risk factor. These findings also add to the personality literature by highlighting neuroticism as an important risk factor for sudden changes in internalizing symptoms in the context of an unprecedented crisis.
The present study contains many important strengths including, its longitudinal design, thorough and well-validated measures of personality and psychopathology, assessment of specific pandemic-related experiences, and a sample located in one of the epicenters of the pandemic. However, several limitations should also be considered. First, although the current student sample was fairly diverse, it is important to extend the findings of the present study to other student samples and young adult clinical samples heavily impacted by COVID-19. Second, the time between the pre-COVID-19 assessment and COVID-19 assessment varied widely; however, we controlled for time between the pre-COVID-19 to COVID-19 assessments and study type in all analyses to account for this discrepancy. Third, although the IDAS-II was used as a diagnostic screener, diagnostic interviews are still required to confirm categorical psychopathology. Additionally, although we chose to investigate resting state RSA, other measures of RSA may also be important to consider. Lastly, the psychometric properties of the Pandemic Experiences Survey are not as sound as other more rigorously tested measures due to the time constraint in developing this measure. Thus, this questionnaire does not have factorial, convergent, or discriminant validity.
Future studies are encouraged to monitor symptom change over the course of the pandemic, especially among those with high neuroticism and low RSA, to determine whether heightened internalizing symptoms present in the beginning of the pandemic are transitory or sustained throughout the pandemic and if personality and autonomic vulnerability factors are predictors of symptom trajectories and/or other long-term mental health outcomes. Measures of neuroticism and RSA are relatively low cost and do not take much time to administer. Therefore, it may be advantageous for clinicians and researchers to use these methods to target samples that may be more reactive to pandemic related experiences and in need of additional mental health resources.
Data availability statement
Research data are not shared.
CRediT authorship contribution statement
Aline K. Szenczy: Writing – original draft, Writing – review & editing, Formal analysis, Methodology. Brady D. Nelson: Conceptualization, Investigation, Funding acquisition, Supervision, Writing – review & editing, Formal analysis, Methodology.
Declaration of competing interest
Authors have no conflicts of interest to disclose.
Acknowledgments
This work was funded by an award to Dr. Brady D. Nelson from the Stony Brook University College of Arts & Sciences.
Footnotes
When we controlled for sex, all analyses remained the same.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.paid.2021.111053.
Appendix A. Supplementary data
Supplementary material
References
- Allen J.J., Chambers A.S., Towers D.N. The many metrics of cardiac chronotropy: A pragmatic primer and a brief comparison of metrics. Biological Psychology. 2007;74(2):243–262. doi: 10.1016/j.biopsycho.2006.08.005. [DOI] [PubMed] [Google Scholar]
- Beauchaine T.P. Respiratory sinus arrhythmia: A transdiagnostic biomarker of emotion dysregulation and psychopathology. Current Opinion in Psychology. 2015;3:43–47. doi: 10.1016/j.copsyc.2015.01.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine T.P., Thayer J.F. Heart rate variability as a transdiagnostic biomarker of psychopathology. International Journal of Psychophysiology. 2015;98(2 Pt 2:338–350. doi: 10.1016/j.ijpsycho.2015.08.004. [DOI] [PubMed] [Google Scholar]
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., Rubin G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Research. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chalmers J.A., Quintana D.S., Abbott M.J.A., Kemp A.H. Anxiety disorders are associated with reduced heart rate variability: A meta-analysis. Frontiers in Psychiatry. 2014;5:80. doi: 10.3389/fpsyt.2014.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers A.S., Allen J.J.B. Vagal tone as an indicator of treatment response in major depression. Psychophysiology. 2002;39(6):861–864. doi: 10.1111/1469-8986.3960861. [DOI] [PubMed] [Google Scholar]
- Esarey J., Sumner J.L. Marginal effects in interaction models: Determining and controlling the false positive rate. Comparative Political Studies. 2018;51(9) doi: 10.1177/0010414017730080. [DOI] [Google Scholar]
- Evelyn, K. (2020, March 22). New York has 5% of Covid-19 cases worldwide as city becomes battlefront|Coronavirus|The Guardian. https://www.theguardian.com/world/2020/mar/22/new-york-coronavirus-cases-worldwide-covid19.
- Finsaas M.C., Goldstein B.L. Do simple slopes follow-up tests Lead us astray? Advancements in the visualization and reporting of interactions. Psychological Methods. 2020;26(1):38–60. doi: 10.1037/met0000266. [DOI] [PubMed] [Google Scholar]
- Gatteau R., Bauman D. Stony Brook University News; 2020. Campus residences announces move-out requirement to reduce density.https://news.stonybrook.edu/university/campus-residences-announces-move-out-requirement-to-reduce-density/ , March 17. [Google Scholar]
- Governor Cuomo'’s Press Office Governor Cuomo signs executive order closing schools statewide for two weeks 2020. https://www.governor.ny.gov/news/governor-cuomo-signs-executive-order-closing-schools-statewide-two-weeks , March 16.
- Hamilton J.L., Alloy L.B. Atypical reactivity of heart rate variability to stress and depression across development: Systematic review of the literature and directions for future research. Clinical Psychology Review. 2016;50:67–79. doi: 10.1016/j.cpr.2016.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- John O.P., Srivastava S. In: Handbook of Personality: Theory and Research. Pervin L.A., John O.P., editors. Vol. 2. Guilford Press; New York: 1999. The Big Five Trait Taxonomy: History, Measurement, and Theoretical Perspectives; pp. 102–138. [Google Scholar]
- Klein D.N., Kotov R., Bufferd S.J. Personality and depression: Explanatory models and review of the evidence. Annual Review of Clinical Psychology. 2011;7:269–295. doi: 10.1146/annurev-clinpsy-032210-104540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig J., Kemp A.H., Beauchaine T.P., Thayer J.F., Kaess M. Depression and resting state heart rate variability in children and adolescents — A systematic review and meta-analysis. Clinical Psychology Review. 2016;46:136–150. doi: 10.1016/j.cpr.2016.04.013. [DOI] [PubMed] [Google Scholar]
- Kotov R., Gamez W., Schmidt F., Watson D. Linking “Big” personality traits to anxiety, depressive, and substance use disorders: A meta-analysis. Psychological Bulletin. 2010;136(5):768–821. doi: 10.1037/a0020327. [DOI] [PubMed] [Google Scholar]
- Kroencke L., Geukes K., Utesch T., Kuper N., Back M.D. Neuroticism and emotional risk during the COVID-19 pandemic. Journal of Research in Personality. 2020;89 doi: 10.1016/j.jrp.2020.104038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lahey B.B. Public health significance of neuroticism. American Psychologist. 2009;64(4):241–256. doi: 10.1037/a0015309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee C.M., Cadigan J.M., Rhew I.C. Increases in loneliness among young adults during the COVID-19 pandemic and association with increases in mental health problems. Journal of Adolescent Health. 2020;67(5):714–717. doi: 10.1016/j.jadohealth.2020.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis G.F., Furman S.A., McCool M.F., Porges S.W. Statistical strategies to quantify respiratory sinus arrhythmia: Are commonly used metrics equivalent? Biological Psychology. 2012;89(2):349–364. doi: 10.1016/j.biopsycho.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Lithopoulos A., Zhang C.-Q., Garcia-Barrera M.A., Rhodes R.E. Personality and perceived stress during COVID-19 pandemic: Testing the mediating role of perceived threat and efficacy. Personality and Individual Differences. 2020;168(9) doi: 10.1016/j.paid.2020.110351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malouff J.M., Thorsteinsson E.B., Schutte N.S. The relationship between the five-factor model of personality and symptoms of clinical disorders: A meta-analysis. Journal of Psychopathology and Behavioral Assessment. 2005;27(2) doi: 10.1007/s10862-005-5384-y. [DOI] [Google Scholar]
- McCrae R.R., John O.P. An introduction to the five-factor model and its applications. Journal of Personality. 1992;60(2):175–215. doi: 10.1111/j.1467-6494.1992.tb00970.x. [DOI] [PubMed] [Google Scholar]
- Nelson G.H., O’Hara M.W., Watson D. National norms for the expanded version of the inventory of depression and anxiety symptoms (IDAS-II) Journal of Clinical Psychology. 2018;74(6):953–968. doi: 10.1002/jclp.22560. [DOI] [PubMed] [Google Scholar]
- Schuchat A. Public health response to the initiation and spread of pandemic COVID-19 in the United States, February 24–April 21, 2020. MMWR. Morbidity and Mortality Weekly Report. 2020;69(18):551–556. doi: 10.15585/mmwr.mm6918e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tackett J.L., Quilty L.C., Sellbom M., Rector N.A., Bagby R.M. Additional evidence for a quantitative hierarchical model of mood and anxiety disorders for DSM-V: The context of personality structure. Journal of Abnormal Psychology. 2008;117(4):812–825. doi: 10.1037/a0013795. [DOI] [PubMed] [Google Scholar]
- Taquet M., Luciano S., Geddes J.R., Harrison P.J. Bidirectional associations between COVID-19 and psychiatric disorder: Retrospective cohort studies of 62 354 COVID-19 cases in the USA. The Lancet Psychiatry. 2020;8(2):130–140. doi: 10.1016/S2215-0366(20)30462-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D., O’Hara M.W., Naragon-Gainey K., Koffel E., Chmielewski M., Kotov R.…Ruggero C.J. Development and validation of new anxiety and bipolar symptom scales for an expanded version of the IDAS (the IDAS-II) Assessment. 2012;19(4):399–420. doi: 10.1177/1073191112449857. [DOI] [PubMed] [Google Scholar]
- Winsor M., Shapiro E., Pereira I. More coronavirus cases in New York than any single country. ABC News. 2020 https://abcnews.go.com/Health/coronavirus-live-updates-crew-member-usns-mercy-hospital/story?id=70059072 , April 9. [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L.…McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Journal of Affective Disorders. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., Macgeorge E.L., Myrick J.G. Mental health and its predictors during the early months of the covid-19 pandemic experience in the United States. International Journal of Environmental Research and Public Health. 2020;17(17) doi: 10.3390/ijerph17176315. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
Research data are not shared.