Abstract
Pelvic fractures and sacroiliac joint (SI) diastasis are debilitating injuries which can drastically decrease an individual's functional capacity, and lead to significant morbidity and mortality. In younger, healthier populations, pelvic fractures are usually the result of sudden traumatic forces, such as a motor vehicle collision. Atraumatic pelvic fractures can also occur, and are most commonly due to age related changes and osteoporosis. Even with prompt surgical management, pelvic fractures often result in a host of challenging complications such as disruption of the SI joint with subsequent limitations in mobility and chronic pain. In this case report, we present a novel treatment of SI diastasis, secondary to corticosteroid induced osteoporosis and pelvic fractures. We performed percutaneous bilateral poly-methyl-methacrylate (PMMA) SI joint fusions under CT-guidance. Here we describe a case of bilateral SI joint CT guided percutaneous arthroplasty for osteoporotic SI joint diastasis and pelvic fractures, resulting in a rapid resolution of SI joint pain and restoration of the ability to ambulate in a previously wheelchair-bound patient. This may be of particular benefit in patients who are poor surgical candidates who experience osteoporotic fractures and would be otherwise unable to receive definitive operative management of their pathologic fractures.
Keywords: Interventional radiology, Percutaneous, Sacroiliac, PMMA, Bone Cement
Introduction
Pelvic fractures and sacroiliac joint (SI) diastasis are debilitating injuries which can drastically decrease an individual's functional capacity, and lead to significant morbidity and mortality. In younger, healthier populations, pelvic fractures are usually the result of sudden traumatic forces, such as a motor vehicle collision [1]. Atraumatic pelvic fractures can also occur, and are most commonly due to age related changes and osteoporosis [2]. Other underlying conditions leading to insufficiency fracture include chronic corticosteroid use, alcoholism, or prior irradiation [3]. The United States is trending toward a continued rise of age-related pelvic fractures and associated healthcare costs with their treatment due to the country's aging demographics [3].
Even with prompt surgical management, pelvic fractures often result in a host of challenging complications such as disruption of the SI joint with subsequent limitations in mobility and chronic pain. In literature, surgical approaches to treating SI diastasis vary. One study used open reduction and subsequent anterior stabilization using dynamic fasteners achieving union in all 10 participants but with several severe complications. Patients experienced foot drop, chronic pelvic pain, as well as limb length discrepancies [4]. Other investigators used a similar surgical approach and achieved union in most patients but also with significant complications including iatrogenic nerve injury and arthrosis of the joint [5,6]. Many patients suffering with SI joint disruptions are poor surgical candidates, further complicating definitive treatment. Non-surgical management options are varied and include NSAIDs, physical therapy, bracing, prolotherapy, and radiofrequency ablation [7]. Ultimately these options are of minimal effectiveness in reducing pain and restoring functionality [7].
We present a novel treatment of SI diastasis, secondary to corticosteroid induced osteoporosis and pelvic fractures. We performed percutaneous bilateral poly-methyl-methacrylate (PMMA) SI joint fusions under Computed Tomography (CT)-guidance. Fluoroscopically-guided PMMA injection has been previously described to treat chronic SI pain due to metastatic disease [8]. We describe a case of bilateral SI joint CT guided percutaneous arthroplasty for osteoporotic SI joint diastasis and pelvic fractures, resulting in a rapid resolution of SI joint pain and restoration of the ability to ambulate in a previously wheelchair-bound patient.
Case report
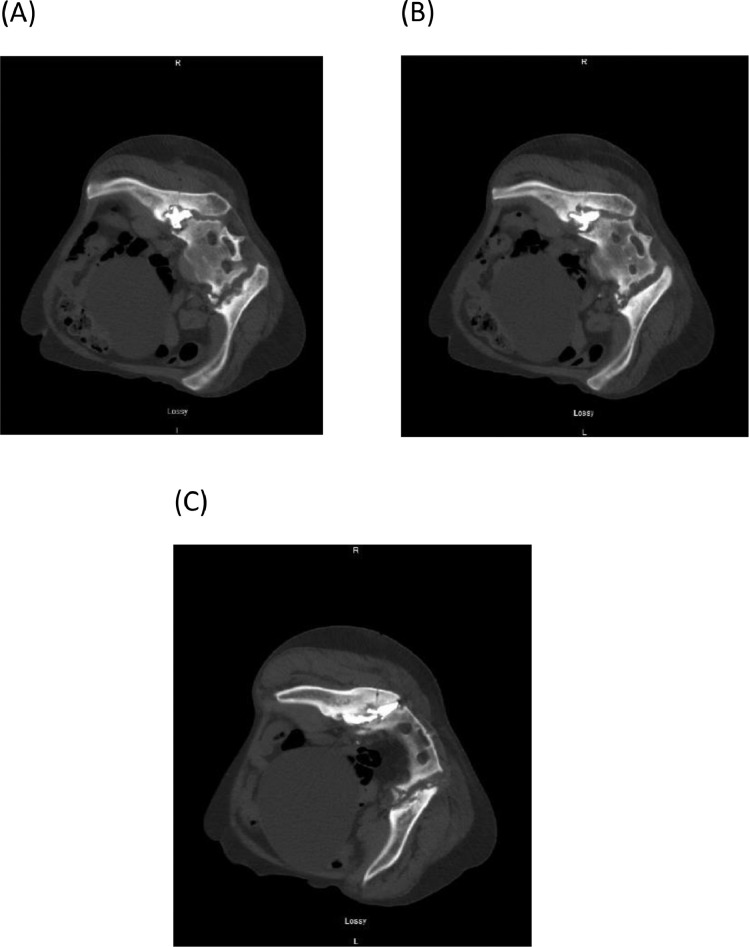
A 61-year-old non-ambulatory and wheelchair-bound woman initially presented to Interventional Radiology clinic with severe pelvic and lower back pain as a referral for possible sacroplasty from her orthopedic surgeon. Her medical history was significant for extensive degenerative spondylosis of the lumbosacral spine, debilitating severe osteoporosis and innumerable displaced fractures of her pelvic girdle and sacrum. She had a longstanding diagnosis of rheumatologic disease of uncertain etiology, favoring mixed connective tissue disorder (MCTD). Due to her rheumatologic disease, she had been prescribed long-term corticosteroids for many years, resulting in diffuse osteoporosis and innumerable insufficiency fractures of the axial skeleton. After careful review of her imaging, a large non-united fracture of the right iliac bone was seen, with severe diastasis, multiple fractures, and erosion of the bilateral sacroiliac joints (Fig. 1A-C). Multiple other displaced fractures of the iliac bones, sacrum, pubic rami, and left acetabulum were appreciated. These skeletal abnormalities had increased dramatically when compared to previous CT scans of the lumbosacral spine over the preceding six years. She had previously consulted with an orthopedic surgeon who did not recommend any acute orthopedic surgical intervention given the severity of osteoporotic burden and need for continued corticosteroid use for her rheumatologic disease, making her an overall poor surgical candidate. Her symptoms were most bothersome on her right side, to the point where she was wheelchair-bound secondary to SI joint pain.
Fig. 1.
Axial CT imaging showing bilateral SI joint diastasis with multiple osteoporotic fractures. Of note, non-united right iliac bone fracture may be appreciated.
The possibility of limited osteoplasty of the right iliac bone pathologic fracture or arthroplasty of the SI joint was discussed, as this had historically been utilized successfully in patients for treatment and management of painful metastatic lesions of the sacrum and ileum. The indications, contraindications, risks, benefits, efficacy, expectations, procedural issues, and alternative therapies were discussed, and she wished to electively pursue limited osteoplasty of the right iliac bone to potentially help with the debilitating pain that the patient experienced with weight bearing.
After written informed consent was obtained, the patient underwent a percutaneous CT-guided right SI joint arthroplasty with PMMA bone cement. General anesthesia was initiated and patient was intubated for the procedure. The patient's right buttock was prepped in a sterile fashion and draped, and Lidocaine 1% solution was administered to anesthetize the skin and soft tissues. Of note, preliminary CT imaging demonstrated that the large non-united fracture of the right iliac bone seen in Figure 1C had completely healed (healing can be seen in Figures 2A, B). CT-guidance was used to insert two 11-gauge needles into the right SI joint diastasis (Fig. 3A-B). The needles were advanced through the bone using a hand-held drill. CT confirmed the appropriate position of needles within the right SI joint diastasis cavities. PMMA was injected through the needles into the right SI joint diastasis cavities under CT guidance (Fig. 4A-C). The needles were then removed, and a final post-procedural CT scan was performed revealing successful arthroplasty of the right SI joint without evidence of leak or intravasation of PMMA (Fig. 5A-C).
Fig. 2.
Peri-procedural imaging of right SI joint undergoing PMMA injection. Small fractures may be observed throughout (A,B), and of note, interval resolution of right non-united iliac bone fracture initially seen in Figure 1 from 3 months prior. Diastasis of RIGHT SI joint
Fig. 3.
Successful Placement of 2 11-gauge needles within SI joint for the purpose of PMMA injection.
Fig. 4.
Injection of PMMA within SI joint
Fig. 5.
Successful PMMA placement within right SI joint, with no evidence of leak, eruption, or extravasation
The patient's symptoms markedly improved over the course of approximately 10 days, allowing rapid restoration of weight-bearing ability on the patient's right side. However, the patient then complained of left pelvic pain with ambulation. A decision was then made to repeat the procedure on the left for presumed left SI joint pain.
Written informed consent was again obtained, and patient was anesthetized, steriley prepped and draped, and locally anesthetized with Lidocaine 1%. Preliminary CT imaging redemonstrated left sided sacral fractures and diastasis (Fig. 6A-C), and two 11-gauge needles were passed through the medial portion of the left iliac bone into the SI joint diastasis space using power drill assistance (Fig.7A-7B). Once satisfactory placement was confirmed, PMMA was injected through the needles into the left SI joint space (Fig. 7C). A post injection CT demonstrated satisfactory placement of the PMMA cement, without intravasation or leak outside the joint cavity (Fig.8A-C). A scout X-Ray was taken during the second procedure to show the right sided completed SI joint injection (Fig. 9).
Fig. 6.
Periprocedural imaging of left SI joint undergoing injection.
Fig. 7.
Placement of 2 11-gauge needles within left SI joint (7A, 7B) and injection of PMMA bone cement (7C).
Fig. 8.
Successful placement of PMMA within left SI joint, without evidence of leakage, eruption, or extravasation.
Fig. 9.
Scout film X-Ray of completed Right-Sided SI Joint Injection.
The patient was then seen 9 months after this left-sided PMMA injection (10 months after the right side was treated) and was markedly improved without pain at rest, ambulating without pain, and very satisfied with the result. She was able to transition from being wheelchair bound to fully ambulatory, and able to perform light cardiovascular exercise while on her feet without any SI joint pain. She had no immediate or long-term complications from the procedure and was followed for a full year without any reports of return of her pain or iatrogenic nerve injury.
Discussion
Although the concept of PMMA bone cement joint injection or percutaneous PMMA arthroplasty has been described in chronic SI joint pain, previous reports in the literature indicate its usage for pain secondary to metastatic disease [7,8]. The concept of utilizing this procedure for SI joint fractures due to osteoporosis and SI joint diastasis has not previously been described to our knowledge. The rapid improvement in this patient's symptoms and functional level with successful replication of the procedure on the patient's contralateral side presents a promising proof-of-concept with regards to chronic pain secondary to painful osteoporotic fractures and SI joint diastasis. Given the vast abundance of pelvic insufficiency fractures seen today [3], as well as the myriad of percutaneous approaches that an interventional radiologist has at their disposal, this novel application of PMMA injection suggests that many benefits of this procedure are yet to be explored. These applications certainly include fracture pathology within the sacrum and iliacus, and could be applied elsewhere in the body, as evidenced by the successes of PMMA injection seen within the spine in cases of degenerative scoliosis [9]. Potential limitations of this application include joint areas that require continued mobility, such as the glenohumeral joint, or acetabulofemoral joint. In the case of this patient, she later went on to develop another osteoporotic fracture of her right humeral head, which was determined ultimately to not be amenable to this procedure despite patient request given the functional and mobility-related restrictions that this may impose on a joint that relies more heavily on multi-dimensional movement. However, many other areas of non-operable, pathologic fracture-related pain are yet to be explored, and are supported by the outcomes seen in this patient.
Conclusion
CT-guided percutaneous PMMA bone cement SI joint arthroplasty is a relatively safe, fast, and minimally invasive procedure that can be used in the treatment of osteoporotic fractures contained within the diastatic sacroiliac joint. The rapid resolution of symptoms seen with this patient demonstrate the possible benefit of this procedure, as well as potential other applications of PMMA injection that are yet to be explored. This may be of particular benefit in patients who are poor surgical candidates who experience osteoporotic fractures and would be otherwise unable to receive definitive operative management of their pathologic fractures.
Publication History
Not previously published
Financial Disclosures
Dr. Gregory Johnston reports no disclosures. Adrian Berg reports no disclosures. Dr. Christopher Morris reports no disclosures.
Ethical Approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Footnotes
Funding: No funding to report.
Competing Interests: The authors declare that they have no conflict of interest.
References
- 1.Flint L., Cryer H.G. Pelvic fracture: the last 50 years. J Trauma. 2010;69(3):483–488. doi: 10.1097/TA.0b013e3181ef9ce1. [DOI] [PubMed] [Google Scholar]
- 2.Morrison A., Fan T, Sen S, Weisenfluh L. Epidemiology of falls and osteoporotic fractures: a systematic review. Clinicoecon Outcomes Res. 2013;(5):9–18. doi: 10.2147/CEOR.S38721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Connor T.J., Cole P.A. Pelvic Insufficiency Fractures. Geriatr Orthop Surg Rehabil. 2014;5(4):178–190. doi: 10.1177/2151458514548895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mohammed Elmanawy S.E., Youssef Salah, Salama Fathy. Treatment of sacroiliac joint disruption with anterior stabilization. The Egyptian Orthopaedic Journal. 2015;50(1):45. [Google Scholar]
- 5.Cao Q.Y., Wang M.Y., Wu X.B., Zhu S.W., Wu H.H. [Trans-sacroiliac joint with plate via the anterior approach in management of posterior pelvic injuries] Zhonghua Yi Xue Za Zhi. 2008;88(13):898–900. [PubMed] [Google Scholar]
- 6.Gansslen A., Pohlemann T., Krettek C. [Internal fixation of sacroiliac joint disruption] Oper Orthop Traumatol. 2005;17(3):281–295. doi: 10.1007/s00064-005-1133-3. [DOI] [PubMed] [Google Scholar]
- 7.Dreyfuss P., Dreyer S.J., Cole A, Mayo K. Sacroiliac joint pain. J Am Acad Orthop Surg. 2004;12(4):255–265. doi: 10.5435/00124635-200407000-00006. [DOI] [PubMed] [Google Scholar]
- 8.Nebreda C., Vallejo R, Aliaga L, Benyamin R. Percutaneous sacroplasty and sacroiliac joint cementation under fluoroscopic guidance for lower back pain related to sacral metastatic tumors with sacroiliac joint invasion. Pain Pract. 2011;11(6):564–569. doi: 10.1111/j.1533-2500.2010.00439.x. [DOI] [PubMed] [Google Scholar]
- 9.Filippiadis Dimitrios K., Papagelopoulos P, Kitsou M, Oikonomopoulos N, Brountzos E, Kelekis N. Percutaneous vertebroplasty in adult degenerative scoliosis for spine support: study for pain evaluation and mobility improvement. BioMed research international. 2013:2013. doi: 10.1155/2013/626502. [DOI] [PMC free article] [PubMed] [Google Scholar]