Abstract
Background
A blood transfusion is an acute intervention, implemented to solve life and health‐threatening conditions on a short‐term basis. However, blood transfusions have adverse events, some of them potentially related to immune modulation or to a direct transmission of infectious agents (e.g. cytomegalovirus). Leukoreduction is a process in which the white blood cells are intentionally reduced in packed red blood cells (PRBCs) in order to reduce the risk of adverse reactions. The potential benefits of leukoreduced PRBCs in all types of transfused patients for decreasing infectious and non‐infectious complications remain unclear.
Objectives
To determine the clinical effectiveness of leukoreduction of packed red blood cells for preventing adverse reactions following allogeneic blood transfusion.
Search methods
We ran the most recent search on 10th November 2015. We searched the Cochrane Injuries Group's Specialised Register, Cochrane Central Register of Controlled Trials (CENTRAL, the Cochrane Library), MEDLINE (OvidSP), Embase(OvidSP), CINAHL Plus (EBSCO), LILACS (BIREME), and clinical trials registers. In addition, we checked the reference lists of all relevant trials and reviews identified in the literature searches.
Selection criteria
Randomised clinical trials including patients of all ages requiring PRBC allogeneic transfusion. Any study was eligible for inclusion, regardless of the length of participant follow‐up or country where the study was performed. The primary outcome was transfusion‐related acute lung injury (TRALI). Secondary outcomes were death from any cause, infection from any cause, non‐infectious complications and any other adverse event.
Data collection and analysis
At least two review authors independently performed study selection, 'Risk of bias' assessments and data extraction. We estimated pooled relative risk for dichotomous outcomes, and we measured statistical heterogeneity using I² statistic. The random‐effects model was used to synthesise results. We conducted a trial sequential analysis to assess the risk of random errors in cumulative meta‐analyses.
Main results
Thirteen studies, most including adult patients, met the eligibility criteria. We found no clear evidence of an effect of leukoreduced PRBC versus non‐leukoreduced PRBC in patients that were randomised to receive transfusion for the following outcomes:
TRALI: RR 0.96, 95% CI 0.67 to 1.36, P = 0.80 from one trial reporting data on 1864 trauma patients. The accrued information of 1864 participants constituted only 28.5% of the diversity‐adjusted required information size (DARIS) of 6548 participants. The quality of evidence was low. Death from any cause: RR 0.81, 95% CI 0.58 to 1.12, I² statistic = 63%, P = 0.20 from nine trials reporting data on 6485 cardiovascular surgical patients, gastro‐oncology surgical patients, trauma patients and HIV infected patients. The accrued information of 6485 participants constituted only 55.3% of the DARIS of 11,735 participants. The quality of evidence was very low. Infection from any cause: RR 0.80, 95% CI 0.62 to 1.03, I² statistic = 84%, P = 0.08 from 10 trials reporting data on 6709 cardiovascular surgical patients, gastro‐oncology surgical patients, trauma patients and HIV infected patients. The accrued information of 6709 participants constituted only 60.6% of the DARIS of 11,062 participants. The quality of evidence was very low. Adverse events: The only adverse event reported as an adverse event was fever (RR 0.81, 95% CI 0.64 to 1.02; I² statistic= 0%, P = 0.07). Fever was reported in two trials on 634 cardiovascular surgical and gastro‐oncology surgical patients. The accrued information of 634 participants constituted only 84.4% of the DARIS of 751 participants. The quality of evidence was low. Incidence of other non‐infectious complications: This outcome was not assessed in any included trial.
Authors' conclusions
There is no clear evidence for supporting or rejecting the routine use of leukoreduction in all patients requiring PRBC transfusion for preventing TRALI, death, infection, non‐infectious complications and other adverse events. As the quality of evidence is very low to low, more evidence is needed before a definitive conclusion can be drawn.
Plain language summary
White blood cells reduction in packed red blood cell transfusions for preventing adverse reactions
Background A blood transfusion is when blood is taken from one person and given to another person. Blood transfusions are given to solve life and health‐threatening medical conditions on a short‐term basis. However, blood transfusions have adverse events, some of them potentially related to an immune system response or due to the transmission of infectious agents (e.g. Human Immunodeficiency Virus). Leukoreduction is a process in which the white blood cells are intentionally removed from donated blood in order to reduce the risk of adverse reactions in people receiving the blood transfusion. The benefits of removing white blood cells with the intent of reducing infectious and non‐infectious complications in all types of transfused patients remains unclear. Removing white blood cells is costly. The USA and UK spend tens of millions each year on the procedure. In the USA, the procedure costs approximately USD $30 for each unit of blood product. It may not be worth spending so much money if there is no clear benefit to patients.
Clinical question What are the benefits and harms of removing white blood cells from donated blood for people receiving a blood transfusion?
Study characteristics We searched medical journals for reports of clinical trials which examined the effects of removing white blood cells from donated blood. We were interested in finding out whether the removal of white blood cells from donated blood resulted in patients receiving a blood transfusion having few complications such as transfusion‐related acute lung injury, death, infectious and non‐infectious complications, or any other adverse event. We included people of any age or sex, who received a blood transfusion for any reason. The evidence is based on studies retrieved up to 05 December 2014.
Main results We found 13 studies which included people who received a blood transfusion during heart or cancer surgery, or because they were injured, had cancer, HIV or sepsis.
We found no clear evidence showing either benefits or harms for removing white blood cells from donated blood. For all of the outcomes examined (transfusion‐related acute lung injury, death from any cause, infection from any cause, non‐infectious complication or any other adverse event), there was no sign of benefit or harm.
Quality of evidence The overall quality of evidence of the included studies ranges from very low to low. None of the studies included enough people to give a definitive answer about the usefulness of removing white blood cells from donated blood. New high‐quality studies, involving a few thousand people, are needed to enable us to know the true benefits and harms of this procedure.
Summary of findings
Summary of findings for the main comparison. Leukoreduced PRBCs versus non‐leukoreduced PRBCs for preventing adverse reaction from allogeneic blood transfusion.
| Leukoreduced PRBCs versus non‐leukoreduced PRBCs for preventing adverse reaction from allogeneic blood transfusion | ||||||
| Patient or population: Patients receiving RBC transfusion Settings: Any Intervention: Leukoreduced PRBCs Comparison: Non‐leukoreduced PRBCs | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| Non‐leukoreduced packed RBCs | Leukoreduced packed RBCs | |||||
| TRALI Follow‐up: mean 28 days | Study population | RR 0.96 (0.67 to 1.36) | 1864 (1 study) | ⊕⊕⊝⊝ low1 | TSA yielded an inconclusive result. | |
| 63 per 1000 | 61 per 1000 (42 to 86) | |||||
| Death due to any cause Follow‐up: median 2.5 months | Study population | RR 0.81 (0.58 to 1.12) | 6485 (9 studies) | ⊕⊝⊝⊝ very low2 | TSA yielded an inconclusive result. | |
| 93 per 1000 | 76 per 1000 (54 to 104) | |||||
| Infection from any cause Follow‐up: mean 2.5 months | Study population | RR 0.80 (0.62 to 1.03) | 6709 (10 studies) | ⊕⊝⊝⊝ very low3 | TSA yielded an inconclusive result. | |
| 204 per 1000 | 163 per 1000 (127 to 210) | |||||
| Adverse events Follow‐up: mean 3 months | Study population | RR 0.81 (0.64 to 1.02) | 634 (2 studies) | ⊕⊕⊝⊝ low4 | TSA yielded an inconclusive result. | |
| 387 per 1000 | 314 per 1000 (248 to 395) | |||||
| Non‐infectious complication | Study population | Not estimable | — | — | No trial assessed this outcome. | |
| Not estimable | Not estimable | |||||
| *The basis for the assumed risk was the median control group risk across studies. The corresponding risk (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio; TRALI: Transfusion‐related acute lung injury; RBC: Red blood cell; PRBC: Packed red blood cell; DARIS: Diversity‐adjusted required information size. | ||||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
1Downgraded by two due to imprecision: small sample size as compared with the calculated DARIS and the wide CI overlapping zones of no effect, as well as potential harm or benefit, or both. Few events reported. 2Downgraded due to: high risk of bias (Six of nine included studies have high or unclear risk of bias. ‐1); important heterogeneity (I² statistic: 63%, ‐1); and imprecision as reflected in the wide CI and an insufficient accrued information size compared with the DARIS (‐1).
3Downgraded due to: high risk of bias (Seven of 10 included studies were at high or unclear risk of bias, ‐1); important heterogeneity (I² statistic: 84%, ‐2); and imprecision due to the CI crossing the threshold of meaningful effect and an insufficient sample size as compared with the DARIS (‐1)
4Downgraded due to: high risk of bias (All included studies evaluated were at high risk of bias, ‐1) and imprecision due to the CI crossing the threshold of meaningful effect and an insufficient sample size as compared with the DARIS (‐1).
Background
Description of the condition
Blood transfusion is the infusion of both soluble and cell‐associated forms (red blood cells (RBCs), white blood cells (WBCs) and platelets) into a recipient (Vamvakas 2001). A blood transfusion is an acute intervention, implemented to solve life and health‐threatening conditions on a short‐term basis; and in general, its long‐term effects tend to be of secondary importance (Tsai 2010).
However, blood transfusion is associated with an increasing risk of infectious and non‐infectious adverse events (Wagner 2004; Hendrickson 2009; Sachs 2010). The incidence of non‐infectious transfusion reactions is greater than that of infectious complications (Lavoie 2011). Mortality associated with non‐infectious risks is also significantly higher and accounts for 87% to 100% of fatal complications of transfusions (Lavoie 2011).
The main non‐infectious adverse events to the patient are transfusion‐related acute lung injury (TRALI), which is considered the most severe non‐infectious complication (Renaudier 2009; Triulzi 2009; Vamvakas 2009); non‐haemolytic febrile transfusion reaction (NHFTR) (King 2004; Blajchman 2006; Hoffman 2008) and allergic reactions (Tenorio 2007). Less frequent are transfusion‐associated graft‐versus‐host disease (TA‐GVHD) (Dwyre 2008; Hoffman 2008; Rühl 2009) and transfusion‐related with an immunomodulation effect (TRIM) (Vamvakas 2006).
Several approaches have been considered to prevent adverse reactions related to transfusion (Martí‐Carvajal 2010; Lavoie 2011; Lindholm 2011; Tobian 2011). Transfusion of leukocyte‐reduced RBC concentrates is one of those approaches (Blajchman 2010; Blumberg 2010; Mukagatare 2010). Leukocytes (WBCs) in blood components can mediate febrile transfusion reactions, stimulate human leukocyte antigen (HLA) alloimmunization in transfusion recipients, and transmit some cell‐associated pathogens such as cytomegalovirus (CMV). Therefore, it is desirable to remove WBCs from transfusable blood components (Galel 2009).
Appendix 1 shows non‐infectious transfusion reaction definitions related to WBCs.
Description of the intervention
Leukoreduction is a process in which the WBCs are intentionally reduced by almost 99.99% in RBC concentrates (Shapiro 2004). There are many methods to conduct this approach; however, this process is currently performed using selective leukoreduction filters (Galel 2009). According to the U.S. Food and Drug Administration (FDA), leukocyte‐reduced RBC concentrates contain fewer than 5 × 106 WBCs/unit and at least 85% of the original RBCs (Galel 2009), and according to the Council of Europe < 1 × 106 total WBC/unit. Usually, most RBC leukofiltration is performed by blood collection centres within the first few days after collection (Galel 2009).
Leukoreduction in trauma patients
Safe transfusion products are a necessity for the successful treatment of trauma patients (Tien 2007; Theusinger 2009). It is unclear if leukoreduction of RBC concentrates is the best method of providing blood products for trauma patients (Nathens 2006; Phelan 2007; Watkins 2008). Retrospective studies have shown a reduction of infectious complications in injured patients treated with leukoreduced AlloBT; this effect appears more pronounced in patients receiving massive transfusion (> 6 units of PRBC) (Friese 2008).
Leukoreduction in surgery
Several studies have focused on the advantages of leukoreduced PRBC cells for transfusion in cardiac surgery (van de Watering 1998; Dzik 2002; Wallis 2002; Bilgin 2004; van Hilten 2004; Connery 2005); colorectal surgery (Jensen 1992; Houbiers 1994; Jensen 1996; Titlestad 2001; Dzik 2002; Skånberg 2007); gastrointestinal surgery (Tartter 1998; Dzik 2002; van Hilten 2004); and renal transplantation (Sanfilippo 1985; Opelz 1997; Hiesse 2001). However, some of the findings of these published trials are considered controversial. Furthermore, this approach has been used in patients with AIDS; but, is unclear if this alternative method is beneficial in this population (Collier 2001).
How the intervention might work
Leukoreduction works through multiple mechanisms for preventing adverse reactions:
To prevent TRALI: avoiding the transfer of leukocytes and reducing the cellular antibody interaction complexes that damage the endothelium of the lung (Triulzi 2009; Sachs 2011).
To avoid post‐transfusion infections through reducing some cell‐associated pathogens, such as CMV (Bilgin 2004; Blajchman 2004; van Hilten 2004; Connery 2005; Friese 2008).
To prevent immunomodulation: donor WBCs may suppress the recipient's immune system by interacting with it, producing susceptibility to many pathological conditions including cancer recurrence and other malignancies (Blajchman 2002; Dellinger 2004; Flohé 2007).
Why it is important to do this review
This Cochrane review is important for the following reasons:
Firstly, leukoreduction is expensive. About EUR 29 million/year are spent on implementing leukoreduction (AETSA 2007). Other studies reported costs ranging from CAD $26 million to 46 million annually (CCOHTA 1998). One study estimated the total cost of implementing leukoreduction was about USD 600 million dollars per year in USA (Shapiro 2004). It has also been reported that leukoreduction results in an increase of approximately USD 30/unit of blood product (Phelan 2007). More recently, Tsantes 2014 reported an incremental cost‐effectiveness ratio (ICER) of EUR 6916 to prevent one case of febrile non‐haemolytic transfusion reactions (FNHTR). Secondly, the potential role of leukoreduction for decreasing mortality and infection is controversial (AETSA 2007; Mukagatare 2010). Thirdly, several studies and meta‐analyses did not report conclusive results about leukoreduction, and showed methodological inconsistencies (Vamvakas 1996; Blumberg 1998; Jensen 1998; Fergusson 2004; Blumberg 2007; Vamvakas 2007). Therefore, it is important to conduct this Cochrane review to determine the potential benefits of leukoreduction procedure in patients requiring RBC concentrates, focused on the prevention of adverse reaction.
Objectives
To determine the clinical effectiveness of leukoreduction of packed red blood cells for preventing adverse reactions following allogeneic blood transfusion.
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs).
Types of participants
Patients requiring allogeneic packed RBC (PRBC) transfusion. Patients could be of any age.
Types of interventions
Intervention
Leukoreduced PRBCs.
Comparison
Non‐leukoreduced PRBCs.
We applied no limitations to the leukoreduction procedures used.
Types of outcome measures
Primary outcomes
Incidence of TRALI.
Secondary outcomes
Death due to any cause.
Infection from any cause (number of patients out of the total randomised).
Non‐infectious complications (Appendix 1).
Any other adverse event: “any untoward medical occurrence that may present during treatment with a pharmaceutical product but which does not necessarily have a causal relationship with this treatment” (Nebeker 2004).
We took the information size for the primary outcome of this Cochrane review from the relative risk reported in Nathens 2006. This study included trauma patients. A total sample size of 8781 participants was defined to assess a relative risk reduction on TRALI events of 25%, from a baseline incidence in the control of 6.31% (alpha level of 5% and power of 90%).
Search methods for identification of studies
In order to reduce publication and retrieval bias we did not restrict our search by language, date or publication status.
Electronic searches
The Cochrane Injuries Group Trials Search Co‐ordinator searched the following:
Cochrane Injuries Group Specialised Register (10/11/2015)
Cochrane Central Register of Controlled Trials (CENTRAL, the Cochrane Library) (issue 10 of 12, 2015)
MEDLINE (OvidSP) (1950 to November week 1, 2015)
Embase + Embase Classic (OvidSP) (1947 to 10/11/2015)
LILACS (BIREME) (1982 to 10/11/2015)
CINAHL Plus (EBSCO) (1937 to 10/11/2015)
Clinicaltrials.gov (www.clinicaltrials.gov) (10/1/2015)
WHO International Clinical Trials Registry Platform (http://apps.who.int/trialsearch/) (10/11/2015)
We have reported the search strategies in Appendix 2. We adapted the MEDLINE search strategy as necessary for the other databases. To the MEDLINE search strategy we added the Cochrane Highly Sensitive Search Strategy for identifying RCTs. To the EMBASE strategy we added the terms of the search strategy and study design terms as used by the UK Cochrane Centre (Lefebvre 2011).
Searching other resources
We also searched the following websites (25 November 2014):
US FDA (http://www.fda.gov).
European Medicines Agency (http://www.emea.europa.eu).
Scirus (www.scirus.com).
American Association of Blood Banks (AABB) (http://www.aabb.org).
Transfusion Evidence Library (http://transfusionguidelines.org).
In addition, we checked the reference lists of all relevant trials and reviews identified.
Data collection and analysis
We summarised data according to standard Cochrane methodologies, including the Cochrane Handbook of Systematic Reviews for Interventions (Higgins 2011) and the Methodological Expectations for Cochrane Intervention Reviews (MECIR) (Chandler 2013).
Selection of studies
Two review authors, Daniel Simancas‐Racines (DSR) and Ingrid Arévalo‐Rodriguez (IAR), independently assessed for inclusion all the potential studies identified from the literature searches. We consulted a third review author, Arturo Martí‐Carvajal (AMC) for any disagreements, which were resolved through discussion and consensus.
Data extraction and management
Two review authors, DSR and IAR, independently extracted data from the included trials. We consulted AMC and Dimelza Osorio (DO) in the event of any disagreements, which we resolved through discussion and consensus. Data were recorded for: eligibility criteria, demographics (age, gender and country), type of surgery, setting of the patients (i.e. cardiac surgery, intensive care unit (ICU)) outcomes. DSR recorded the data into a database. IAR and DO checked the data entered.
We contacted the trial author when a full‐text article was unavailable (see Appendix 3 for details).
Assessment of risk of bias in included studies
Two review authors, DSR and IAR, independently assessed the quality of each trial using a simple form following the domain‐based evaluation as described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We compared the assessments and discussed any discrepancies between the review authors. We consulted a third review author (AMC) to resolve any disagreement and to reach consensus.
For each included trial, we assessed risk of bias (as low, high or unclear) for each of the following domains:
Generation of random sequence (selection bias).
Concealment of treatment allocation (selection bias).
Blinding of participants and personnel (person delivering treatment) to treatment allocation (performance bias).
Blinding of outcome assessors to treatment allocation (detection bias).
Completeness of the outcome data (including checks for possible attrition bias through withdrawals, loss to follow‐up and protocol violations). For the incomplete outcome data domain, we considered as a high risk of bias RCTs that losses participants after transfusion intervention. Additionally, we considered high risk of bias (design bias) as those studies in which the patients were not transfused because inconsistency to determine inclusion criteria adequately or when a premature randomisation was done.
Selective reporting of outcomes (reporting bias).
Other sources of bias (other bias).
Measures of treatment effect
All outcomes in this Cochrane review were binary outcomes. We calculated the treatment effect with risk ratios (RRs) with 95% confidence intervals (CI).
Unit of analysis issues
The unit of analysis was the patient. We collected and analysed a single measurement for each outcome from each patient.
Dealing with missing data
We assessed the percentages of the overall dropouts for each included trial and per each randomisation arm, and we evaluated whether an intention‐to‐treat (ITT) analysis had been performed or could be performed with the available published information. We defined these dropouts as the percentage of lost patients who received an effective transfusion, over the total of transfused patients reported for each arm of the included studies.
Assessment of heterogeneity
We quantified statistical heterogeneity using the I² statistic. The I² statistic describes the percentage of total variation across trials that is due to heterogeneity rather than sampling error (Higgins 2003). We considered I² statistic between 50% and 74% as a moderate statistical heterogeneity, whereas a value of ≥ 75% represents high heterogeneity. We explored heterogeneity using a sensitivity analysis.
Assessment of reporting biases
We created a funnel plot to assess reporting bias for each outcome (Sterne 2011) where there were data from at least 10 trials (Higgins 2011).
Data synthesis
We summarized sufficiently comparable trials using the random‐effects model to accommodate the high heterogeneity, and used a fixed‐effect model for the sensitivity analysis. We carried out the main analysis based on the number of randomised participants, using an ITT analysis. All the analyses were carried out using RevMan 2014.
Subgroup analysis and investigation of heterogeneity
No data were available to perform the following subgroup analyses for the primary outcome (incidence of TRALI):
By type of post‐transfusion complication.
By technique or type of material used.
Immunosuppressed patient versus non‐immunosuppressed patient.
Massive transfusion (> 6 units PRBCs) versus less.
Sensitivity analysis
We performed the following sensitivity analysis for the primary outcome:
To assess the robustness of estimates, we used both fixed‐effect and random‐effects models for all outcomes and compared results.
We conducted a sensitivity analysis comparing trials with low risk of bias, with those at unclear or high risk of bias, according to attrition bias (Higgins 2011).
We also conducted a sensitivity analysis based on transfused patients to explore the high heterogeneity.
Trial sequential analysis
We carried out a trial sequential analysis (TSA) for every dichotomous outcome evaluated in this systematic review: TRALI, death from any cause, infection from any cause, and adverse events/fever.
TSA is a type of statistical power analysis that can be used to further investigate the relevance of results ("strength of evidence") yielded by a meta‐analysis (Wetterslev 2008). It is the counterpart of a sample size calculation as part of a conventional study design. TSA allows researchers to differentiate between "spurious" significant findings caused by random error in a data‐set with only small numbers of participants and trials and a "truly" significant result with sufficient statistical power. Thereby, TSA also accounts for repeated significance testing. The optimal information size and O'Brien‐Fleming alpha‐spending boundaries indicating the "real" significance threshold are constructed by providing the numbers for alpha level, power, control group risk and inter‐study heterogeneity (Thorlund 2011). TSA can be performed only if the information size (number of participants) is large enough as compared with the optimal information size, and only if the outcome is dichotomous. Further details can be found in the "User Manual for Trial Sequential Analysis (TSA)", provided by the Centre for Clinical Intervention Research of the Copenhagen Trial Unit (Thorlund 2011).
'Summary of findings' tables
We used the GRADE approach (Guyatt 2011b) to assess the overall quality of evidence. The GRADE approach appraises the quality of a body of evidence based on the extent to which one can be confident that an estimate of effect or association reflects the item being assessed. The quality of a body of evidence considers within‐study risk of bias (methodological quality), the directness of the evidence, heterogeneity of the data, precision of effect estimates and risk of publication bias (Balshem 2011; Brozek 2011; Guyatt 2011a; Guyatt 2011c; Guyatt 2011d; Guyatt 2011e; Guyatt 2011f; Guyatt 2011g; Guyatt 2011h). We created a ‘Summary of Findings’ table using GRADEpro GDT Guideline Development Tool (www.gradepro.org). We have presented the body of evidence in Table 1.
Results
Description of studies
See the Included studies section.
Results of the search
We identified 6244 references. Thirteen RCTs met our inclusion criteria (Sanfilippo 1985; Jensen 1996; Tartter 1998; van de Watering 1998; Collier 2001; Titlestad 2001; Wallis 2002; Bilgin 2004; van Hilten 2004; Boshkov 2006; Nathens 2006; Lapierre 2007; Donati 2014). See Figure 1.
1.
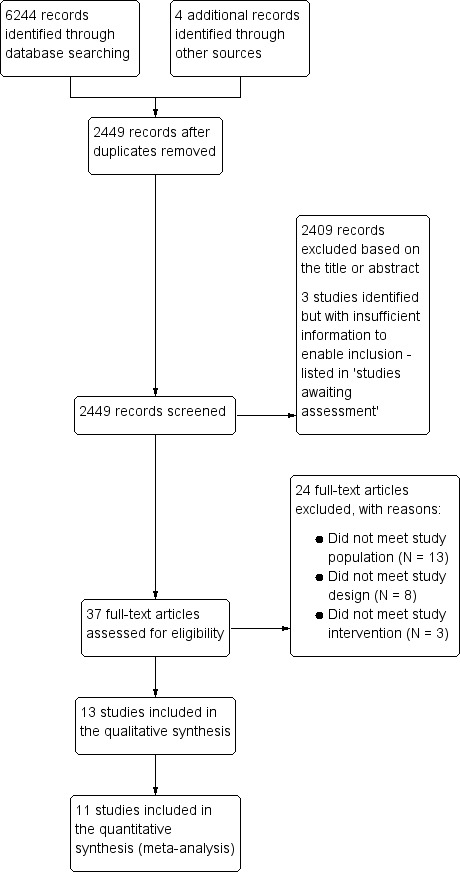
Study flow diagram.
We did not find any ongoing trials. Three studies were classified as awaiting assessment (Zhao 2004; NCT00810810; Waghmare 2012). There is insufficient information available about these studies to enable us to decide whether or not they should be included in the review. See Characteristics of studies awaiting classification.
Included studies
Methodology characteristics
Trials were published between 1985 and 2014. They were conducted in various countries: five in the USA (Sanfilippo 1985; Tartter 1998; Collier 2001; Boshkov 2006; Nathens 2006), three in the Netherlands (van de Watering 1998; Bilgin 2004; van Hilten 2004), two in Denmark (Jensen 1996; Titlestad 2001), one in France (Lapierre 2007), one in the UK (Wallis 2002) and one in Italy (Donati 2014).
All trials had a parallel study design; 11 comparing two groups and two trials comparing three groups (van de Watering 1998; Wallis 2002). The number of trial participants ranged from 20 (Donati 2014) to 1864 (Nathens 2006), with a median of 531 participants.
In three trials participants were monitored for one month or less (Jensen 1996; Nathens 2006; Donati 2014). In 10 trials participants were monitored for between two and 15 months. In 11 trials there was an a priori sample size estimation, and one trial did not report how the sample size was derived (Sanfilippo 1985). In one trial the data used were taken from the report's abstract, and there was no information about the sample size calculation (Boshkov 2006). All trials used patients as the randomisation unit and unit of analysis. All trials reported inclusion criteria. Exclusion criteria were not reported in the Boshkov 2006 study abstract.
Patient characteristics
All 13 included trials were conducted in adults, but two trials also included patients under 18 years of age: Collier 2001 (≥ 14 years) and Nathens 2006 (≥ 17 years). Twelve trials reported the gender of the participants; almost 60% of the included participants were men. Five trials involved cardiac surgery patients (van de Watering 1998; Wallis 2002; Bilgin 2004; van Hilten 2004; Boshkov 2006), four trials involved gastro‐oncology surgery patients (Jensen 1996; Titlestad 2001; van Hilten 2004; Lapierre 2007), one trial involved non‐surgical oncology patients (Lapierre 2007), one trial involved trauma patients (Nathens 2006), one trial included HIV infected patients (Collier 2001) and one trial involved patients with sepsis, severe sepsis or septic shock requiring ICU care (Donati 2014).
Interventions
Leukoreduction definition
The extent of leukoreduction differed across the studies: two studies obtained 0.1 to 0.3 × 106 per unit (Bilgin 2004; Titlestad 2001). Three trials reported 5 × 106 leukocytes per unit of blood after leukoreduction (Collier 2001; Wallis 2002; Nathens 2006). Jensen 1996 reported 1.2 × 109 per unit; van de Watering 1998 reported 1.2 ± 1.4 × 106 per unit; Tartter 1998 reported 2 × 105 per unit; and Lapierre 2007 less than 2 × 104 per unit. Four studies did not report definitions for leukoreduction (Sanfilippo 1985; van Hilten 2004; Boshkov 2006; Donati 2014).
Type of filters
Trials were conducted using different types of filters. Two trials used "Cellselect Optima" filters (Bilgin 2004; van de Watering 1998). Four trials used "BPF4" filters for blood leukoreduction (Tartter 1998; Titlestad 2001; Wallis 2002; Nathens 2006). Jensen 1996 used "RC 100" filters and two trials used "Sepacell RZ‐200B1" filters (Lapierre 2007; Donati 2014). Four trials did not report the type of filter used (Sanfilippo 1985; Collier 2001; van Hilten 2004; Boshkov 2006).
Control groups
Trials were conducted using different types of comparator groups. Five trials used "Buffy coat depleted packed cells (PCs)" as a comparison group (Jensen 1996; van de Watering 1998; Wallis 2002; Bilgin 2004; van Hilten 2004). Eight trials used "unmodified RBC transfusion" or standard RBCs as a comparison group (Sanfilippo 1985; Tartter 1998; Collier 2001; Titlestad 2001; Boshkov 2006; Nathens 2006; Lapierre 2007; Donati 2014). One trial also used "Red blood cells concentrate with plasma reduction" as a third non‐leukoreduced arm (Wallis 2002).
Cointervention
Three studies described the use of platelets as co‐intervention (Collier 2001; Bilgin 2004; Nathens 2006). Bilgin 2004 reported that platelets were all leukocyte‐depleted by filtration; Collier 2001 did not describe the platelet leukoreduction process, and Nathens 2006 reported that all patients received apheresis platelets when platelets were required. Lapierre 2007 reported that none of the patients received platelets concentrate.
Outcomes
One trial reported on TRALI (Nathens 2006).
Nine trials reported on death from any cause (Jensen 1996; van de Watering 1998; Collier 2001; Titlestad 2001; Wallis 2002; Bilgin 2004; van Hilten 2004; Nathens 2006; Lapierre 2007). Boshkov 2006 reported death only for the transfused patients group.
Ten trials reported on infection from any cause (Jensen 1996; Tartter 1998; van de Watering 1998; Collier 2001; Titlestad 2001; Wallis 2002; Bilgin 2004; van Hilten 2004; Nathens 2006; Lapierre 2007) the infections reported were: respiratory tract infections in six studies (Jensen 1996; van de Watering 1998; Titlestad 2001; Bilgin 2004; Nathens 2006; Lapierre 2007); urinary tract infections in five studies (Jensen 1996; van de Watering 1998; Bilgin 2004; Nathens 2006; Lapierre 2007); wound infections or surgical site infections in seven studies (Jensen 1996; Tartter 1998; van de Watering 1998; Titlestad 2001; Bilgin 2004; Nathens 2006; Lapierre 2007); bacteraemia or septicaemia in seven studies (Jensen 1996; van de Watering 1998; Collier 2001; Titlestad 2001; Bilgin 2004; Nathens 2006; Lapierre 2007); abdominal infection in three studies (Jensen 1996; Titlestad 2001; Nathens 2006). Collier 2001 included persons infected with HIV and CMV.
Three trials reported adverse events (Collier 2001; Wallis 2002; Lapierre 2007). One trial, Collier 2001, analysed fever episodes per transfusion, but not per study participant, thus it was not included in the meta‐analysis.
Donati 2014 and Sanfilippo 1985 reported only physiological outcomes. There were no relevant data to include in the analyses.
Excluded studies
We excluded 24 studies (see Characteristics of excluded studies) for the following reasons:
Use of other blood products in the intervention groups (Gilbert 1989; Jensen 1992; Houbiers 1994; Bowden 1995; Kao 1995; Gu 1996; Nielsen 1999; Hayashi 2000; Dzik 2002; Efstathiou 2003; Connery 2005; Gu 2009).
No transfusion in one of the study groups (Opelz 1997; de Vries 2004; Koskenkari 2005; Leal‐Noval 2005; Salamonsen 2005; So‐Osman 2010).
Non‐randomised clinical trial (Bracey 2002; de Vries 2003; Llewelyn 2004; Skånberg 2007), or a review article (van de Watering 2004; Vamvakas 2007).
Risk of bias in included studies
We have summarised the risk of bias in the included studies in Figure 2 and Figure 3.
2.
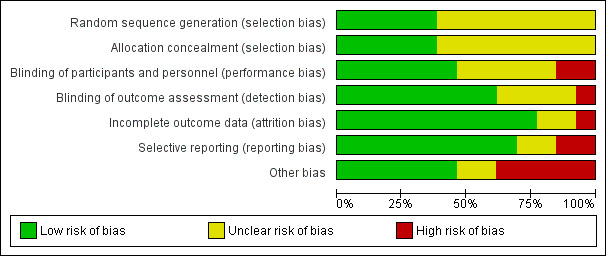
'Risk of bias' graph: review authors' judgements about each 'Risk of bias' item presented as percentages across all included studies.
3.
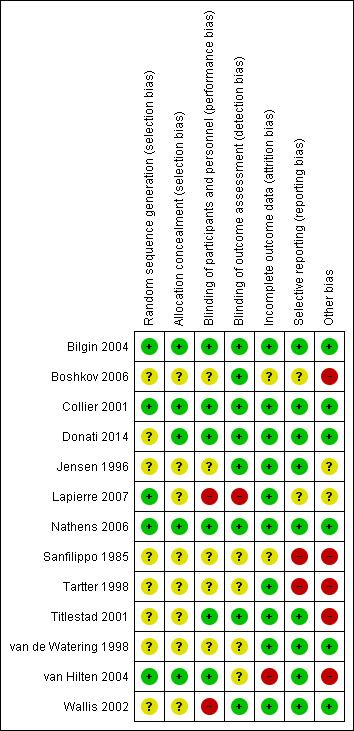
'Risk of bias' summary: review authors' judgements about each 'Risk of bias' item for each included study.
Allocation
Random sequence generation
In five trials there was low risk of bias related to the sequence generation method (Collier 2001; Bilgin 2004; van Hilten 2004; Nathens 2006; Lapierre 2007). Eight trials had unclear risk of bias (Sanfilippo 1985; Jensen 1996; Tartter 1998; van de Watering 1998; Titlestad 2001; Wallis 2002; Boshkov 2006; Donati 2014).
Allocation concealment
In five trials there was low risk of bias related to the method of allocation concealment (Collier 2001; Bilgin 2004; van Hilten 2004; Nathens 2006; Donati 2014). Eight trials had unclear risk of bias (Sanfilippo 1985; Jensen 1996; Tartter 1998; van de Watering 1998; Titlestad 2001; Wallis 2002; Boshkov 2006; Lapierre 2007).
Blinding
Blinding of participants and personnel
The risk of bias arising from the lack of blinding was rated as low in six trials (Collier 2001; Titlestad 2001; Bilgin 2004; van Hilten 2004; Nathens 2006; Donati 2014). The risk of bias from blinding was unclear in five trials (Sanfilippo 1985; Jensen 1996; Tartter 1998; van de Watering 1998; Boshkov 2006) and high in two studies (Wallis 2002; Lapierre 2007).
Blinding outcome assessment
Eight trials had a low risk of bias arising from the method of blinding outcome assessment (Jensen 1996; Collier 2001; Titlestad 2001; Wallis 2002; Bilgin 2004; Boshkov 2006; Nathens 2006; Donati 2014). Four studies were at unclear risk (Sanfilippo 1985; Tartter 1998; van de Watering 1998; van Hilten 2004) and one trial was at high risk of bias (Lapierre 2007).
Incomplete outcome data
Ten trials were judged to be at low risk of bias from incomplete outcome data (Jensen 1996; Tartter 1998; van de Watering 1998; Collier 2001; Titlestad 2001; Wallis 2002; Bilgin 2004; Nathens 2006; Lapierre 2007; Donati 2014). There was unclear risk of bias in two trials (Sanfilippo 1985; Boshkov 2006), and high risk of bias in one trial (van Hilten 2004).
Selective reporting
We judged nine trials as at low risk of reporting bias (Jensen 1996; van de Watering 1998; Collier 2001; Titlestad 2001; Wallis 2002; Bilgin 2004; van Hilten 2004; Nathens 2006; Donati 2014). Two trials were at unclear risk of bias (Boshkov 2006; Lapierre 2007), and two trials were at high risk of bias (Sanfilippo 1985; Tartter 1998).
Other potential sources of bias
Six trials appeared free of other potential sources of bias and we judged these trials to be at low risk of bias (van de Watering 1998; Collier 2001; Wallis 2002; Bilgin 2004; Nathens 2006; Donati 2014). Seven trials had design bias of different kinds: inconsistency in adequately determining inclusion criteria, premature randomisation (Sanfilippo 1985; Tartter 1998; van de Watering 1998; Titlestad 2001; van Hilten 2004; Boshkov 2006) or sample size bias (Lapierre 2007).
Effects of interventions
See: Table 1
Leukoreduced PRBC versus non‐leukoreduced PRBC
1. Primary outcomes
TRALI (analysis based on total randomised patients)
Overall analysis
One trial including 1864 participants showed no difference between treatment groups on TRALI (6.02% versus 6.31%) (RR 0.96, 95% CI 0.67 to 1.36; P = 0.80) (Nathens 2006). See Analysis 1.1.
1.1. Analysis.
Comparison 1 Leukoreduced PRBC versus non‐leukoreduced PRBC. Main analysis (randomised patients), Outcome 1 TRALI. Number of events of the total of randomised patients reported.
Quality of evidence (TSA and GRADE)
The accrued information of 1864 participants constituted only 28.5% of the diversity‐adjusted required information size (DARIS) of 6548 participants. We calculated DARIS based on a diversity of 4%; a proportion with the TRALI events of 6.3% in the control group; a relative risk reduction of 25%; an alpha of 5%; and a beta of 20% (power = 80%). With the inclusion of data from one trial, the Z‐value neither crossed the conventional statistical boundaries of 5% nor the Lan‐DeMets‐O'Brian‐Fleming boundaries. The TSA‐adjusted 95% CI overlapped with no effect (RR 1.0) and is compatible with both a potential benefit and a potential harm (RR 0.46 and RR 1.98, respectively); thus, the TSA yielded an inconclusive result. The quality of evidence was low (imprecision as reflected in the wide CI and only one trial with a small sample size as compared with the DARIS (‐2)).
In the analysis including "only transfused patients", compared to all patients results were similar (RR 0.98, 95% CI 0.74 to 1.29; P = 0.87; Analysis 2.1). We were unable to conduct other subgroup and sensitivity analyses because only one study measured this outcome. In this study, Nathens 2006, leukoreduction was performed pre‐storage.
2.1. Analysis.
Comparison 2 Leukoreduced PRBC versus non‐leukoreduced PRBC. Secondary analysis (transfused patients), Outcome 1 TRALI. Number of events of the total of transfused patients reported.
2. Secondary outcomes
Death due to any cause
Overall analysis (total randomised patients)
The meta‐analysis of nine trials including 6485 participants showed no difference between treatment groups in the risk of death from any cause (8.54% versus 9.34%; RR 0.81, 95% CI 0.58 to 1.12, I² statistic = 63%, P = 0.20) (Jensen 1996; van de Watering 1998; Collier 2001; Titlestad 2001; Wallis 2002; Bilgin 2004; van Hilten 2004; Nathens 2006; Lapierre 2007). See Analysis 1.2.
1.2. Analysis.
Comparison 1 Leukoreduced PRBC versus non‐leukoreduced PRBC. Main analysis (randomised patients), Outcome 2 Death. Number of events of the total of randomised patients reported.
Sensitivity analysis
We conducted three sensitivity analyses; none of which were statistically significant. The RRs using the fixed‐effect model were similar to that of the random effect model.
Including three studies with low risk of bias (Collier 2001; Bilgin 2004; Nathens 2006), compared to six studies at unclear or high risk of bias (RR 1.03, 95% CI 0.89 to 1.20; I² statistic = 38%, P = 0.66).
Including "only transfused patients", compared to all patients (RR 0.80, 95% CI 0.60 to 1.07, I² statistic: 60%, P = 0.13, Analysis 2.2).
Post‐storage leukoreduction, compared with pre‐storage leukoreduction (RR 0.74, 95% CI 0.53 to 1.04, I² statistic: 70%, P = 0.09).
2.2. Analysis.
Comparison 2 Leukoreduced PRBC versus non‐leukoreduced PRBC. Secondary analysis (transfused patients), Outcome 2 Death. Number of events of the total of transfused patients reported.
Reporting bias
We did not explore reporting biases since the meta‐analysis included fewer than 10 studies (Higgins 2011).
Quality of evidence (TSA and GRADE)
The accrued information of 6485 participants constituted only 55.2% of the DARIS of 11,735 participants. DARIS was calculated based on a diversity of 84%; a proportion of death from any cause of 9.34% in the control group (median proportion of deaths in the control group); a relative risk reduction of 25%; an alpha of 5%; and a beta of 20% (power = 80%). The Z‐value neither crossed the conventional statistical boundaries of 5% nor the Lan‐DeMets‐O'Brian‐Fleming boundaries. The TSA did not indicate futility, as the cumulative Z‐curve did not cross the futility wedge (Figure 4). The TSA‐adjusted 95% CI overlapped with no effect (RR 1.0) and is compatible with both a potential benefit and a potential harm (RR 0.51 and RR 1.27, respectively); thus, the TSA yielded an inconclusive result. The quality of evidence was very low (high risk of bias (‐1); important heterogeneity (‐1); and imprecision as reflected in the wide CI and an insufficient accrued information size compared with the DARIS (‐1)).
4.
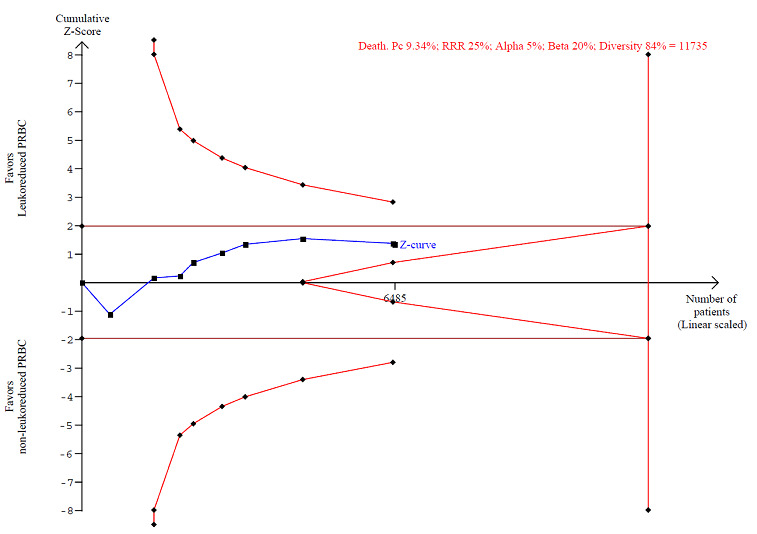
TSA calculated to reliably detect a 25% relative change in the incidence of death from any cause, assuming a control group event rate of 9.34% with a power of 80% at an alpha of 5%
Infection from any cause
Overall analysis (total randomised patients)
The meta‐analysis of 10 trials involving 6709 participants showed no difference between treatment groups in the risk of infection from any cause (17.7% versus 20.4%; RR 0.80, 95% CI 0.62 to 1.03; I² statistic = 84%, P = 0.08) (Jensen 1996; Tartter 1998; van de Watering 1998; Collier 2001; Titlestad 2001; Wallis 2002; Bilgin 2004; van Hilten 2004; Nathens 2006; Lapierre 2007). See Analysis 1.3.
1.3. Analysis.
Comparison 1 Leukoreduced PRBC versus non‐leukoreduced PRBC. Main analysis (randomised patients), Outcome 3 Infection. Number of events of the total of randomised patients reported.
Sensitivity analysis
The RR was different when we used the fixed‐effect model (RR 0.85, 95% CI 0.77 to 0.93; I² statistic = 84%, P = 0.0006); however, the results of TSA indicate this statistically significant result may be a spurious finding.
We performed three other sensitivity analyses, which showed no statistically significant differences:
Including three studies with low risk of bias (Collier 2001; Bilgin 2004; Nathens 2006), compared with seven studies at unclear or high risk of bias (RR 0.92, 95% CI 0.63 to 1.34; I² statistic = 83%, P = 0.67).
Including "only transfused patients", compared with all randomised patients (RR 0.76, 95% CI 0.58 to 1.00; I² statistic = 87%, P = 0.05, Analysis 2.3), and the heterogeneity remained high.
Post‐storage leukoreduction, compared with pre‐storage leukoreduction (RR 0.91, 95% CI 0.76 to 1.09; I² statistic = 65%, P = 0.32).
2.3. Analysis.
Comparison 2 Leukoreduced PRBC versus non‐leukoreduced PRBC. Secondary analysis (transfused patients), Outcome 3 Infection. Number of events of the total of transfused patients reported.
Reporting bias
After visual assessment of the funnel plot (Figure 5) and a formal assessment of the funnel plot asymmetry, applying the Egger's test (P = 0.09), we found no sign of reporting bias.
5.
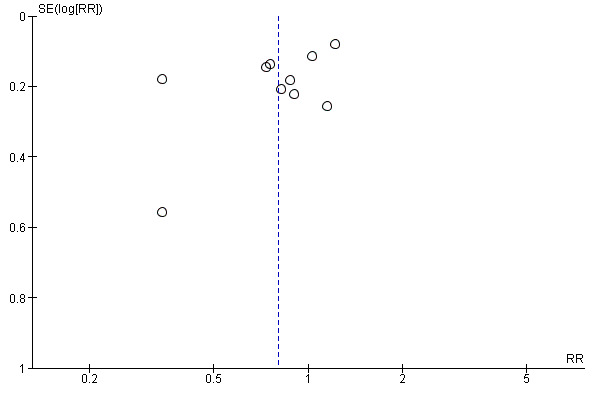
Funnel plot of comparison: 1 Leukoreduced PRBC versus non‐leukoreduced PRBC. Main Analysis (Randomised patients), outcome: 1.3 Infection. Number of events of the total of randomised patients reported.
Quality of evidence (TSA and GRADE)
The accrued information of 6709 participants constituted only 60.6% of the DARIS of 11,062 participants. We calculated DARIS based on a diversity of 86%; a proportion of infection from any cause of 20.4% in the control group (median proportion in the control group); a relative risk reduction of 25%; an alpha of 5%; and a beta of 20% (power = 80%). The Z‐value neither crossed the conventional statistical boundaries of 5% nor the Lan‐DeMets‐O'Brian‐Fleming boundaries. TSA did not indicate futility, as the Z‐curve did not cross the futility wedge (Figure 6). The TSA‐adjusted 95% CI overlapped the zone of no effect (RR 1.0) and is compatible with both a potential benefit and a potential harm (RR 0.57 and RR 1.12, respectively); thus, the TSA yielded an inconclusive result. The quality of evidence was very low (high risk of bias (‐1); important heterogeneity (‐2); and imprecision due to the CI crossing the threshold of meaningful effect and an insufficient sample size as compared with the DARIS (‐1)).
6.
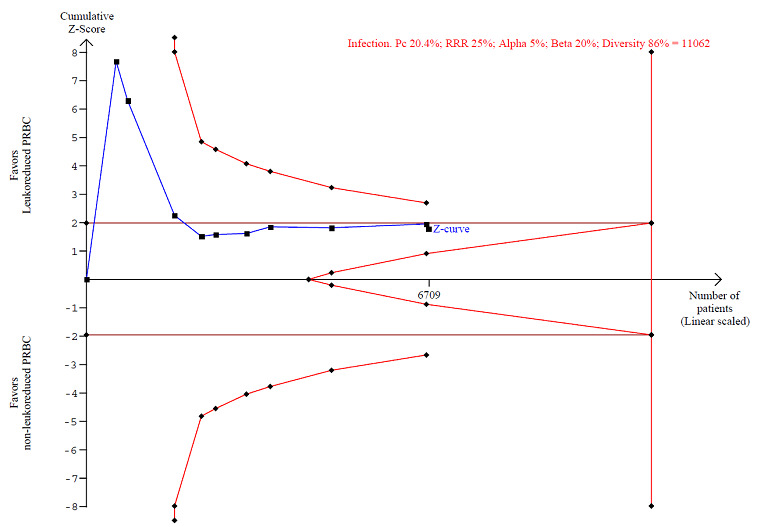
TSA calculated to reliably detect a 25% relative change in the incidence of infection from any cause, assuming a control group event rate of 20.4% with a power of 80% at an alpha of 5%.
Adverse events (fever)
Three trials reported adverse events. However, we excluded one trial reporting fever as a temperature increase of at least 1°C per transfusion from the meta‐analysis since fever was not analysed per study participant (Collier 2001).
Overall analysis (total randomised patients)
Two trials including 634 participants showed no difference between treatment groups in adverse events (31.9% versus 38.7%; RR 0.81, 95% CI 0.64 to 1.02; I² statistic = 0%, P = 0.07) (Wallis 2002). See Analysis 1.4.
1.4. Analysis.
Comparison 1 Leukoreduced PRBC versus non‐leukoreduced PRBC. Main analysis (randomised patients), Outcome 4 Adverse events. Number of events of the total of randomised patients reported.
Sensitivity analysis
In the sensitivity analysis comparing "transfused patients" with randomised patients, there was a statistically significant difference (RR 0.75, 95% CI 0.60 to 0.94, I² statistic = 0%, P = 0.01, Analysis 2.4); however, the results of TSA indicate this statistically significant result may be a spurious finding.
2.4. Analysis.
Comparison 2 Leukoreduced PRBC versus non‐leukoreduced PRBC. Secondary analysis (transfused patients), Outcome 4 Adverse events. Number of events of the total of transfused patients reported.
In a sensitivity analysis of data from one study, Wallis 2002, there was no difference when comparing post‐storage with pre‐storage leukoreduction (RR 0.81, 95% CI 0.64 to 1.04).
Reporting bias
We did not explore reporting biases since the meta‐analysis included fewer than 10 studies (Higgins 2011).
Quality of evidence (TSA and GRADE)
The accrued information of 634 participants constituted only 84.4% of the DARIS of 751 participants. DARIS was calculated based on a diversity of 0%; a proportion of infection from any cause of 38.7% in the control group (median proportion in the control group); a relative risk reduction of 25%; an alpha of 5%; and a beta of 20% (power = 80%). The Z‐value neither crossed the conventional statistical boundaries of 5% nor the Lan‐DeMets‐O'Brian‐Fleming boundaries. TSA did not indicate futility, as the Z‐curve did not cross the futility wedge (Figure 7). The TSA‐adjusted 95% CI overlapped with the zone of no effect (RR 1.0) and is compatible with both a potential benefit and a potential harm (RR 0.68 and RR 1.05, respectively); thus, the TSA yielded an inconclusive result. The quality of evidence was low (high risk of bias (‐1); and imprecision due to the CI crossing the threshold of meaningful effect and an insufficient sample size as compared with the DARIS (‐1)).
7.
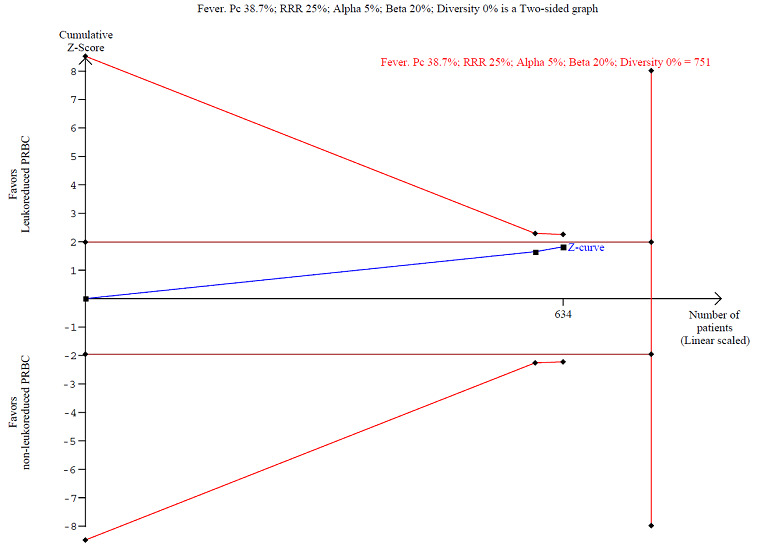
TSA calculated to reliably detect a 25% relative change in the incidence of fever, assuming a control group event rate of 38.7% with a power of 80% at an alpha of 5%.
Non‐infectious complications
The included trials did not assess this pre‐defined outcome.
Discussion
Summary of main results
In this systematic review we included 13 trials involving cardiovascular surgical, gastro‐oncology surgery, trauma and HIV patients who were randomised to receive leukoreduced compared with non‐leukoreduced PRBC transfusion. After analysis of the study data, we are unable to conclude whether or not leukoreduction of PRBC has an effect on preventing TRALI (one trial), death (nine trials), infection (10 trials) and other adverse events (fever, reported in two trials). The quality of evidence was low (TRALI and adverse events) to very low (death and infection) due to high heterogeneity, imprecision and high risk of bias. None of the included trials reported on other non‐infectious complications. The sensitivity analyses of trials at low risk of bias showed neither a beneficial or harmful effect of leukoreduction of PRBC on the pooled data regarding death, infection and adverse events.
Overall completeness and applicability of evidence
Overall completeness of evidence
We analysed 13 controlled clinical trials that met our predefined inclusion criteria. Two trials reported only physiological results and we excluded them from the meta‐analyses. Only one RCT evaluated the primary outcome (TRALI). However, we obtained data from 11 trials which contributed to the effect estimates of the secondary outcomes (death from any cause, infection from any cause and adverse events/fever). We found no trials evaluating non‐infectious complications other than TRALI (e.g. FNHTR). Therefore, the pre‐specified objectives and outcomes of our Cochrane review were partially addressed and the results are inconclusive. Consequently, the findings of this review should be interpreted with caution until more data are available.
Applicability of evidence
This Cochrane review is complex for a variety of reasons:
Firstly, regarding the population: the identified studies enrolled patients with different health problems, including trauma, cancer, cardiac disease and HIV‐infected patients. Some important patient populations were not studied at all (e.g. paediatric or obstetric patients) or were insufficiently assessed (e.g. one RCT of trauma patients). In this context, external validity may be limited due to a lack of studies analysing these populations. Furthermore, the effect of leukoreduction on some types of patients without a strong indication for leukoreduced PRBC has not been sufficiently evaluated: single‐transfused patients, patients without history of FNHTR, patients who are not receiving long‐term platelet transfusions and those who are not at risk of developing CMV disease.
Secondly, regarding the intervention, the included studies did not adequately report several aspects related to the transfusion of RBC that need to be considered when interpreting the results, namely: the use of leukoreduced or non‐leukoreduced platelets as a co‐intervention, the timing of leukoreduction (i.e. pre‐storage or post‐storage), the type of filter used (e.g. Cell select Optima, BPF4, RC 100, Sepacell RZ‐200B1), leucocyte reduction definition (e.g. 0.1 to 0.3 × 106 WBC/unit, 5 × 106, 2 × 105 per unit, etc.) and the type of transfusion (i.e. allogeneic or autologous).
Thirdly, regarding the outcomes: not all the included trials assessed relevant clinical outcomes. Relevant infections (e.g. CMV), non‐infectious complications (e.g. TRALI, FNHTR) and any other adverse events were not sufficiently assessed or reported (Schulz 2010). The various follow‐up intervals (28 days to 15 months) may represent another limitation for the assessment of outcomes.
Fourthly, regarding the costs: leukoreduction is widely implemented in clinical practice in many countries and some countries have established universal leukoreduction for blood transfusions (Laupacis 2001). However, the high costs related to this procedure deserve special attention. Even though the reintroduction of non‐leukoreduced products probably provides no clinical impact, it does entail economic consequences. Changing the strategy from performing universal to selective leukoreduction would result in an important decrease in the costs (e.g. almost EUR 30 million per year in Spain (AETSA 2007)). Tsantes 2014 reported an incremental cost‐effectiveness ratio (ICER) of EUR 6916 to prevent one case of FNHTR. Additionally, it is reasonable to consider other costs associated with maintaining dual inventories of leukoreduced PRBC and non‐leukoreduced PRBC.
Finally, as leukoreduction of PRBC was shown to have no effect on preventing TRALI, death, infection and other adverse events reported by RCTs, these results have to be adequately interpreted within the context of current clinical practice which differs internationally and among populations. Other strategies might be more cost‐effective than leukoreduction in terms of avoiding adverse events related to transfusion PRBC, such as the use of restrictive transfusion triggers (Carson 2012; Rohde 2014), that have shown effectiveness regardless of whether blood products are leukoreduced or not.
Quality of the evidence
The body of evidence available to date does not allow a definitive conclusion to be drawn about the benefits and harms of leukoreduction. The included RCTs had important methodological limitations: 1. poor and incomplete reporting of inclusion and exclusion criteria; 2. important attrition bias due to the exclusion of many patients included, but not transfused; 3. incomplete information on allocation concealment; 4. inadequate reporting of other blood components as co‐interventions; and 5. incomplete reporting of clinical outcomes of interest. Additionally, some of the included trials showed important inconsistency in the estimates of effect.
Potential biases in the review process
We applied Cochrane systematic review methodology to the search for and selection of studies for inclusion in the review. However, despite our effort to include all published studies evaluating leukoreduction for the prevention of adverse reactions from allogeneic blood transfusion, it is possible that not all relevant data were identified. The small number of trials identified in our review raises concerns about publication bias. In order to identify this potential bias we performed a funnel plot. However, this visual method was possible only for one outcome (infection of any cause), since fewer than 10 studies assessed the other outcomes.
We contacted trial authors during the identification of trials (see Appendix 3) to clarify some questions related to the eligibility criteria, but not while we completed data extraction and analysis. We took into account only published data during these processes, considering the missing information as reporting bias.
In the review protocol we defined the main analysis based on the ITT approach (Simancas‐Racines 2012). However, during the data extraction we identified an important number of patients included but not transfused. This may affect the precision of the effect estimations. In order to explore this scenario, we carried out a per‐protocol analysis (only transfused patients) which did not reflect relevant differences in relation to the primary outcome (TRALI) and secondary outcomes death and infection from any cause, but the secondary outcome adverse events (fever) showed differences.
A limitation of the review was not considering the effect of buffy coat depletion in the estimations through a sensitivity analysis, because we had not planned such analysis in advance. Another limitation was not considering the subgroup analysis of the potential effect of different types of filters used in the included studies for all outcomes. We planned this analysis in the review protocol only for the primary outcome.
Agreements and disagreements with other studies or reviews
Reviews and meta‐analyses on postoperative infection and death related to the leukoreduction of blood products have been carried out previously. However, as far as we know, no systematic reviews focused on non‐infectious complications, such as TRALI or FNHTR, have yet been published. In the overall analysis of death from any cause, the findings of other reviews are in accordance with our results. Nevertheless, one systematic review showed a 50% reduction in the probability of postoperative infection (Blumberg 2007) and another review analysing "only patients who received transfusion" found a statistically significant reduction of 40% in postoperative infection, but a non‐significant reduction in mortality (Fergusson 2004).
These two reviews have several limitations. They included studies with other blood components apart from leukoreduced PRBC cells as interventions, as well as non‐randomised studies. Moreover, heterogeneity between studies was not taken into account and the risk of bias of included studies was not appropriately assessed. Furthermore, some relevant studies were not included.
Authors' conclusions
Implications for practice.
There is no clear evidence for supporting or rejecting the routine use of leukoreduction in all patients requiring PRBC transfusion for preventing TRALI, death from any cause, infection from any cause, non‐infectious complications and other adverse events. The quality of evidence is very low to low. Given that leukoreduction is a very expensive procedure, clinicians and policy makers may need to reconsider whether transfusing leukoreduced PRBC is suitable for all types of patients, especially for patients without a strong indication for leucocyte reduction. In countries where leukoreduction has not been universally implemented yet, selective leukoreduction is an option to be considered until better evidence on the effectiveness or harms of this procedure is available.
Implications for research.
Taking into account the inconclusive evidence found in this Cochrane review, further research is needed to assess the relative efficacy, safety and cost‐effectiveness of leukoreduction in different clinical settings and for different conditions. Researchers should consider that premature randomisation is an important issue because it may cause attrition bias and affect the interpretation of the results; in this case, it may affect the true effect of leukoreduced PRBC. Further research should also consider aspects of the study design (Chan 2013), such as verifying the inclusion and exclusion criteria before randomisation. Researchers should also improve the reporting of interventions and co‐interventions (Schulz 2010), for example whether or not a blood transfusion includes other components or not (e.g. leukoreduced or non‐leukoreduced platelets). Moreover, further studies should address all relevant outcomes (Gabriel 2012), such as death from any cause, infectious complications (e.g. risk of CMV transmission, or at least, evaluate the risk of CMV reactivation from transfused leukoreduced PRBC cells), non‐infectious complications (e.g. TRALI, NHFRT) and any other adverse events related to the PRBC transfusion.
Notes
In future versions of this review we will also include, for all outcomes:
a subgroup analysis by medical condition
a subgroup analysis by type of filter
a sensitivity analysis by buffy coat
Acknowledgements
Daniel Simancas‐Racines is a Ph.D. candidate at the Department of Pediatrics, Gynecology and Obstetrics, and Preventive Medicine, Universitat Autònoma de Barcelona, Spain.
We thank Ms. Marta Roqué i Figuls, Iberoamerican Cochrane Centre, for her advice on statistical analysis; Dr. Christian Gluud, Centre for Clinical Intervention Research, Denmark, for his advice on interpreting the trial sequential analyses; and Ms. Maria Victoria Leo Rosas for revising and improving the grammar and style of the review.
This project was supported by the UK National Institute for Health Research, through Cochrane Infrastructure funding to the Cochrane Injuries Group. The views and opinions expressed are those of the authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Appendices
Appendix 1. Non‐infectious adverse reactions
| Term | Definition | Reference |
| Allergic reactions | Allergic reactions are probably the most frequent, occurring in 1% to 2% of all transfusion reactions. The symptoms range from local or diffuse pruritus, urticaria, erythema and cutaneous flushing to anaphylactic allergic reactions occurring within minutes of the transfusion. Anaphylactoid reactions fall in between the two ends of the spectrum. Uncomplicated allergic reactions are associated with increased histamine (increased during storage), cytokines, mast cell activators (i.e. leukotrienes), and other vasoactive substances (C3a and C5a) produced by donor leukocytes during storage. |
Tenorio 2007 |
| Febrile non‐haemolytic transfusion reactions (FNHTR) | FNHTR are defined as a temperature rise of at least 1°C in association with a transfusion or up to 4h after that may be accompanied by chills or rigors. Such reactions are due to acquired antibodies to donor leukocyte antigens or pyrogenic cytokines (IL‐1, IL‐6, IL‐8 and TNF‐D) elaborated by leukocytes present in the blood components or products. | Tenorio 2007 |
| Transfusion‐related acute lung injury (TRALI) (clinical definition) | The earliest definition of TRALI included all patients who developed acute respiratory distress, moderate to severe hypoxaemia (PaO2 30 to 50 mmHg), rapid onset of pulmonary edema, mild to moderate hypotension, and fever (defined as a 18°C to 28°C rise in body temperature from pre‐transfusion baseline) within 6 hours of receiving a plasma‐containing blood transfusion. The definition excluded patients if they had underlying cardiac or respiratory disease. | Goldman 2005; Toy 2005 |
| TRALI (histopathological definition) | As evidenced by interstitial lung leak and lung histology that showed septal thickening, with inflammatory infiltrate consisting mainly of granulocytes was observed in mice transfused with large amounts (4.5 mg/kg) of a murine IgG subclass II. | Looney 2006 |
| Non‐hemolytic febrile transfusion reaction (NHFTR) | Leukocyte apoptosis or monocyte activation, or both, may cause cytokines to accumulate in the blood products during storage. Symptoms/signs: fever, chills. | Heddle 1999; King 2004; Hoffman 2008 |
| Transfusion‐associated graft‐versus‐host disease (TA‐GVHD) | When viable immunological T cells present in blood products are introduced into an immuno‐incompetent host who cannot destroy the donor lymphocytes. Symptoms/signs: nausea, vomiting, anorexia, fever, watery diarrhoea, liver function abnormality, bone marrow aplasia, skin rash, icterus and renal failure. | Hoffman 2008; Rühl 2009 |
Appendix 2. Search strategies
Cochrane Injuries Group Specialised Register
"blood transfusion" AND (leuk* OR leuc* OR plasmapheresis OR cytapheres OR apheresis)
Cochrane Central Register of Controlled Trials (CENTRAL, the Cochrane Library)
#1MeSH descriptor Blood Component Removal explode all trees #2MeSH descriptor Leukocyte Reduction Procedures explode all trees #3MeSH descriptor Cytapheresis explode all trees #4(plasmapheresis or cytapheres* or apheresis or plateletpheresis or pheresis or phereses or aphereses or leukapheresis or leucapheresis) #5(Leukoreduc* or leukodeplet* or leukofilt* or leukocyte‐reduc* or leucoreduc* or leucodeplet* or leucofilt* or desleucotizat*) #6buffy coat‐depleted #7leukocyte count or leukocyte free or leucocyte count or leucocyte free #8((Blood or white blood cell* or WBC or plasma) NEAR/3 (reduc* or deplet* or replete* or remov* or filtrat* or filter* or cytapheresis)) #9((leukocyte* or leucocyte*) NEAR/3 (reduc* or deplet* or replete* or remov* or filtrat* or filter*)) #10(#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9) #11MeSH descriptor Blood Transfusion explode all trees #12((allogenic or allogeneic) NEAR/3 blood transfusion*) #13(blood component* NEAR/3 transfusion*) #14((erythrocyte* or leukocyte* or platelet* or RBC or red blood cell* or WBC or white blood cell* or thrombocyte* or blood) NEAR/3 Transfusion*) #15(#11 OR #12 OR #13 OR #14) #16(#10 AND #15)
Medline (OvidSP)
1.exp Blood Component Removal/ 2.exp Leukocyte Reduction Procedures/ 3.exp cytapheresis/ 4.(plasmapheresis or cytapheres* or apheresis or plateletpheresis or pheresis or phereses or aphereses or leukapheresis or leucapheresis).ab,ti. 5.(Leukoreduc* or leukodeplet* or leukofilt* or leukocyte‐reduc* or leucoreduc* or leucodeplet* or leucofilt* or desleucotizat*).mp. 6.buffy coat‐depleted.ab,ti. 7.(leukocyte count or leukocyte free or leucocyte count or leucocyte free).ab,ti. 8.((Blood or white blood cell* or WBC or plasma) adj3 (reduc* or deplet* or replete* or remov* or filtrat* or filter* or cytapheresis)).ab,ti. 9.((leukocyte* or leucocyte*) adj3 (reduc* or deplet* or replete* or remov* or filtrat* or filter*)).ab,ti. 10.or/1‐9 11.exp Blood Transfusion/ 12.((allogenic or allogeneic) adj3 blood transfusion*).ab,ti. 13.(blood component* adj3 transfusion*).ab,ti. 14.((erythrocyte* or leukocyte* or platelet* or RBC or red blood cell* or WBC or white blood cell* or thrombocyte* or blood) adj3 Transfusion*).ab,ti. 15.or/11‐14 16.10 and 15 17.randomi?ed.ab,ti. 18.randomized controlled trial.pt. 19.controlled clinical trial.pt. 20.placebo.ab. 21.clinical trials as topic.sh. 22.randomly.ab. 23.trial.ti. 24.17 or 18 or 19 or 20 or 21 or 22 or 23 25.(animals not (humans and animals)).sh. 26.24 not 25 27.26 and 16
Embase + Embase Classic (OvidSP)
1. exp Blood Component Removal/ 2. exp Leukocyte Reduction Procedures/ 3. exp cytapheresis/ 4. (plasmapheresis or cytapheres* or apheresis or plateletpheresis or pheresis or phereses or aphereses or leukapheresis or leucapheresis).ti,ab. 5. (Leukoreduc* or leukodeplet* or leukofilt* or leukocyte‐reduc* or leucoreduc* or leucodeplet* or leucofilt* or desleucotizat*).ti,ab. 6. buffy coat‐depleted.ti,ab. 7. (leukocyte count or leukocyte free or leucocyte count or leucocyte free).ti,ab. 8. ((Blood or white blood cell* or WBC or plasma) adj3 (reduc* or deplet* or replete* or remov* or filtrat* or filter* or cytapheresis)).ti,ab. 9. ((leukocyte* or leucocyte*) adj3 (reduc* or deplet* or replete* or remov* or filtrat* or filter*)).ti,ab. 10. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 11. exp blood transfusion/ 12. ((allogenic or allogeneic) adj3 blood transfusion*).ti,ab. 13. (blood component* adj3 transfusion*).ti,ab. 14. ((erythrocyte* or leukocyte* or platelet* or RBC or red blood cell* or WBC or white blood cell* or thrombocyte* or blood) adj3 Transfusion*).ti,ab. 15. 11 or 12 or 13 or 14 16. 10 and 15 17. exp Randomized Controlled Trial/ 18. exp controlled clinical trial/ 19. placebo.ab. 20. randomi?ed.ti,ab. 21. *Clinical Trial/ 22. randomly.ab. 23. trial.ti. 24. 17 or 18 or 19 or 20 or 21 or 22 or 23 25. exp animal/ not (exp human/ and exp animal/) 26. 24 not 25 27. 16 and 26
CINAHL Plus (EBSCO)
S1 (MH "Blood Component Removal+") S2 (MH "Cytapheresis+") S3 TX plasmapheresis or cytapheres* or apheresis or plateletpheresis or pheresis or phereses or aphereses or leukapheresis or leucapheresis S4 TX Leukoreduc* or leukodeplet* or leukofilt* or leukocyte‐reduc* or leucoreduc* or leucodeplet* or leucofilt* or desleucotizat S5 TX buffy coat‐depleted S6 TX leukocyte count or leukocyte free or leucocyte count or leucocyte free S7 TX (Blood or white blood cell* or WBC or plasma) N3 (reduc* or deplet* or replete* or remov* or filtrat* or filter* or cytapheresis) S8 TX (leukocyte* or leucocyte*) N3 (reduc* or deplet* or replete* or remov* or filtrat* or filter*) S9 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 S10(MH "Blood Transfusion+") S11 TX (allogenic or allogeneic) N3 blood transfusion* S12 TX blood component* N3 transfusion* S13 TX (erythrocyte* or leukocyte* or platelet* or RBC or red blood cell* or WBC or white blood cell* or thrombocyte* or blood) N3 Transfusion* S14 S10 or S11 or S12 or S13 S15 S9 and S14 S16 (MH "Clinical Trials") S17 PT clinical trial* S18 TX clinical N3 trial* S19 TI ( (singl* N3 blind*) or (doubl* N3 blind*) or (trebl* N3 blind*) or (tripl* N3 blind*) ) or TI ( (singl* N3 mask*) or (doubl* N3 mask*) or (trebl* N3 mask*) or (tripl* N3 mask*) ) or AB ( (singl* N3 blind*) or (doubl* N3 blind*) or (trebl* N3 blind*) ) or AB ( (singl* N3 mask*) or (doubl* N3 mask*) or (trebl* N3 mask*) or (tripl* N3 mask*) ) S20 TX randomi?ed N3 control* N3 trial* S21 (MH "Placebos") S22 TX placebo* S23(MH "Random Assignment") S24 TX random* N3 allocat* ‐ S25 MH quantitative studies ‐ S26 S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 ‐ S27 S15 and S26 Limiters ‐ Exclude MEDLINE records
LILACS
((Pt randomized controlled trial OR Pt controlled clinical trial OR Mh randomized controlled trials OR Mh random allocation OR Mh double‐blind method OR Mh single‐blind method) AND NOT (Ct animal AND NOT (Ct human and Ct animal)) OR (Pt clinical trial OR Ex E05.318.760.535$ OR (Tw clin$ AND (Tw trial$ OR Tw ensa$ OR Tw estud$ OR Tw experim$ OR Tw investiga$)) OR ((Tw singl$ OR Tw simple$ OR Tw doubl$ OR Tw doble$ OR Tw duplo$ OR Tw trebl$ OR Tw trip$) AND (Tw blind$ OR Tw cego$ OR Tw ciego$ OR Tw mask$ OR Tw mascar$)) OR Mh placebos OR Tw placebo$ OR (Tw random$ OR Tw randon$ OR Tw casual$ OR Tw acaso$ OR Tw azar OR Tw aleator$) OR Mh research design) AND NOT (Ct animal AND NOT (Ct human and Ct animal)) OR (Ct comparative study OR Ex E05.337$ OR Mh follow‐up studies OR Mh prospective studies OR Tw control$ OR Tw prospectiv$ OR Tw volunt$ OR Tw volunteer$) AND NOT (Ct animal AND NOT (Ct human and Ct animal))) AND (Medicina Transfusional or la transfusión or As transfusões or blood transfusion or Transfusión Sanguínea)
Clinicaltrials.gov
( leuk* OR leuc* OR plasmapheresis OR cytapheres OR apheresis ) [DISEASE] AND transfusion [TREATMENT]
WHO Clinical Trials Registry Platform Search Portal (http://apps.who.int/trialsearch/)
Condition: leuk* OR leuc* OR plasmapheresis OR cytapheres OR apheresis
Recruitment status: ALL
Appendix 3. Study authors contacted
| Trial author | Date of contact | Reply |
| Dr. Boshkov and Dr and Dr. Van Winkle (donna.vanwinkle@med.va.gov; vog.av.dem@elkniwnav.annod) Study: "Prestorage Leukoreduction of Transfuesed Red Cells Is Associated with Significant Ongoing 2‐12 Month Survival Benefit in Cardiac Surgery Patients". |
08 October 2014 | None yet |
| Dr Morris (morrisc@ohsu.edu) and Dr. Van Winkle (donna.vanwinkle@med.va.gov; vog.av.dem@elkniwnav.annod) Study: "Prestorage Leukoreduction of Transfused Red Cells Is Associated with Significant Ongoing 2–12 Month Survival Benefit in Cardiac Surgery Patients" (Blood journal as one of the abstracts from the ASH Annual Meeting (2006 108: Abstract 578). Study included (Boshkov 2006). Data extraction from abstract only. |
08 October 2014 | None yet |
| Dr. Nelson (knelson@psbc.org) and Dr. Aldea (aldea@u.washington.edu). Study: "Immunomodulation Following Transfusion" (ClinicalTrials.gov NCT00810810) |
04 December 2014 | None yet |
| Dr. van de Watering (l.vandewatering@sanquin.nl, l.m.g.van_de_Watering@lumc.nl) Study: van de Watering 1998 |
22 May 2015 | The author provided more details about follow‐up |
| Dr. van Hilten (j.vanhilten@sanquin.nl) Poster “Characterization of the effects of leukocyte‐filtered red blood cell transfusions in major surgery” related to the study van Hilten 2004 |
22 May 2015 | The author clarified the relation between two references |
| Dr. Waghmare and Dr. Desai (no email found, we contacted through ResearchGate) Poster: "Open Labeled, Randomized, Controlled Trial Comparing Leukodepleted (Filtered) Blood Transfusion and Non‐Leukodepleted (Unfiltered) Blood Transfusion in Cases of Severe Falciparum Malaria." Published in Chest 10/2012; 142(4_MeetingAbstracts):232A. |
23 May 2015 | None yet |
| Dr. Zhao (shumingzhao@yahoo.com and through ResearchGate) Study: "Clinical assessment of preventing febrile nonhaemolytic transfusion reaction by leukocyte‐depleted blood transfusion". And the poster "Prevention and reduction of febrile nonhaemolytic transfusion reaction by leucocyte filtration blood transfusion" |
25 July 2015 | None yet |
Data and analyses
Comparison 1. Leukoreduced PRBC versus non‐leukoreduced PRBC. Main analysis (randomised patients).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 TRALI. Number of events of the total of randomised patients reported | 1 | 1864 | Risk Ratio (M‐H, Random, 95% CI) | 0.96 [0.67, 1.36] |
| 2 Death. Number of events of the total of randomised patients reported | 9 | 6485 | Risk Ratio (M‐H, Random, 95% CI) | 0.81 [0.58, 1.12] |
| 3 Infection. Number of events of the total of randomised patients reported | 10 | 6709 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.62, 1.03] |
| 4 Adverse events. Number of events of the total of randomised patients reported | 2 | 634 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.64, 1.02] |
| 4.1 Fever | 2 | 634 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.81 [0.64, 1.02] |
Comparison 2. Leukoreduced PRBC versus non‐leukoreduced PRBC. Secondary analysis (transfused patients).
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 TRALI. Number of events of the total of transfused patients reported | 1 | 268 | Risk Ratio (M‐H, Random, 95% CI) | 0.98 [0.74, 1.29] |
| 2 Death. Number of events of the total of transfused patients reported | 10 | 4060 | Risk Ratio (M‐H, Random, 95% CI) | 0.80 [0.60, 1.07] |
| 3 Infection. Number of events of the total of transfused patients reported | 10 | 3557 | Risk Ratio (M‐H, Random, 95% CI) | 0.76 [0.58, 1.00] |
| 4 Adverse events. Number of events of the total of transfused patients reported | 2 | 544 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.60, 0.94] |
| 4.1 Fever | 2 | 544 | Risk Ratio (M‐H, Fixed, 95% CI) | 0.75 [0.60, 0.94] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bilgin 2004.
| Methods | Design: Parallel group RCT Country: The Netherlands Multicentre study: Yes (two university hospitals: Academic Medical Center and Leiden University Medical Center) Setting: Hospital Follow‐up: 90 days Unit of allocation: Patients Unit of analysis: Patients |
|
| Participants | Inclusion criteria: Adults > 18 years undergoing valve surgery Exclusion criteria: Those with a medical indication for leukocyte‐depleted erythrocytes or who had received blood transfusions within the previous three months Patients enrolled: 496 Patients randomised: 474 Buffy coat‐depleted packed cells: 237 Leukocyte‐depleted erythrocytes (LDs): 237 Patients transfused: not clearly reported Patients considered for the analysis: 474 Main characteristics of patients: Age: Buffy coat‐depleted packed cells group = 66.6 ± 12.5 years; LD group = 65.3 ± 14.7 years Percentage of men: Buffy coat‐depleted packed cells group = 57%; LD group = 52% Percentage of erythrocyte transfusions more or equal to four: Buffy coat‐depleted packed cells group= 55.3%; LD group= 61.2% Storage time of the units: Buffy coat‐depleted packed cells group = 19.7 ± 5.4 ; LD group = 17.4 ± 5 Percentage of use of aprotinin: Buffy coat‐depleted packed cells group = 37.1; LD group = 36.3 |
|
| Interventions |
Co‐intervention:
|
|
| Outcomes | Primary:
Secondary:
Quote: "An independent safety committee monitored the interim results of the primary end point." (Page 2757). |
|
| Notes | Trial registration: Not reported Funding: This study was financially supported by the Netherlands Heart Foundation (grant 98.183) (Page 2760) Rol of sponsor: Not reported A priori sample size estimation: Yes Conducted: Between June 1999 and May 2001 Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "a straightforward randomizations was performed by using a fixed block size (n=24) to ensure a balance between the randomizations groups" (Page 2756). |
| Allocation concealment (selection bias) | Low risk | Quote: "...the technicians randomly assigned the patients by opening a sealed and numbered envelope." "In the hospital electronic information system, a code was used during the study period to hide the random assignment" (Page 2756). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The patients, surgeons, anaesthesiologists, and the trial coordinators were blinded to the random assignment, as the technicians placed uniform study labels on the description on the erythrocyte bags" (Page 2756). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The patients, surgeons, anesthesiologists, and the trial coordinators were blinded to the random assignment, as the technicians placed uniform study labels on the description on the erythrocyte bags. In the hospital electronic information system, a code was used during the study period to hide the random assignment" (Page 2756). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss after transfusion: 0.4% (2/474) Loss after transfusion in prestorage by filtration of LDs (LDs): 0.8% (2/237) Loss after transfusion in Buffy coat–depleted packed cells (PCs): 0% (0/237) Loss after transfusion. Imbalance between comparison groups: 0.8% |
| Selective reporting (reporting bias) | Low risk | Comment: The study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified (convincing text of this nature may be uncommon). |
| Other bias | Low risk | The study appears to be free of other sources of bias. |
Boshkov 2006.
| Methods | Design: Parallel group RCT Country: USA Multicentre study: Yes (three centre trial) Setting: Hospital Follow‐up: 2 to 12 months Unit of allocation: Patients Unit of analysis: Patients |
|
| Participants | Inclusion criteria:
Exclusion criteria: Not reported in the abstract
Prestorage leukoreduced RBC (LR‐RBCs): The number of patients is not clearly reported in the abstract. Standard RBCs (S‐RBCs): The number of patients is not clearly reported in the abstract.
Main characteristics of patients: "Groups were statistically equivalent demographically and by all Society of Thoracic Surgery risk criteria". |
|
| Interventions |
Co‐intervention: not reported in the abstract |
|
| Outcomes | Primary:
Secondary: Not reported in the abstract. |
|
| Notes | Trial registration: Not reported in the abstract Funding: Not reported in the abstract Role of sponsor: Not reported in the abstract A priori sample size estimation: Not reported in the abstract Conducted: Not reported in the abstract Declared conflicts of interest: "No relevant conflicts of interest to declare" (reported in the abstract) Other relevant information: All study characteristics were obtained from the abstract. We tried to contact two trial authors by email, but no response has not yet been obtained |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "patients (undergoing coronary artery bypass grafting, cardiac valve replacement, or a combination of the two) were pre‐operatively randomised to receive either LR‐ or S‐RBCs (Abstract). Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Allocation concealment (selection bias) | Unclear risk | Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "Patients and clinicians were blinded as to product type" (Abstract). The blinding methods are not clearly reported. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Patients and clinicians were blinded as to product type" (Abstract). Comments: No blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | "562 patients (45.8%) were transfused: 304 received LR‐RBCs and 258 S‐RBCs" (Abstract) Loss after transfusion: Not reported in the abstract Loss after transfusion LR group: Not reported in the abstract Loss after transfusion Control group: Not reported in the abstract Loss after transfusion. Imbalance between comparison groups: Not reported in the abstract. Comment: Insufficient reporting of attrition/exclusions to permit judgement of ‘low risk’ or ‘high risk’ (e.g. number randomised not stated, no reasons for missing data provided). |
| Selective reporting (reporting bias) | Unclear risk | Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’ (Abstract data). |
| Other bias | High risk | Design bias: 1226 patients randomised; only 562 (45.8) were transfused. |
Collier 2001.
| Methods | Design: Parallel group RCT Country: USA Multicentre study: Yes (11 academic medical centres) Setting: Hospital Follow‐up: 12 months Unit of allocation: Patients Unit of analysis: Patients |
|
| Participants | Inclusion criteria: Those 14 years of older, with confirmed HIV infection and documented CMV infection (by chart or antibody testing), Karnofsky performance score of ≥ 40, expected survival of more than 1 month, symptomatic anaemia requiring red blood concentrates transfusion and no received transfusions within 72 hours of enrolment. Exclusion criteria: Those with a surgical reason for transfusion, a priori history for transfusion, renal failure requiring dialysis, thrombocytopenic purpura, used intravenous immunoglobulin within 6 weeks of entry or those that had started new antiretroviral drugs or systematic immunomodulators within 2 weeks of entry.
Leukoreduced red blood concentrates transfusion: 265 Unmodified red blood concentrates transfusion: 266
Main characteristics of patients: Age: Leukoreduced group = 38.3 ± 8.2 years; Unmodified group = 38.4 ± 8.3 years Percentage of men: Leukoreduced group = 79%; Unmodified group = 79% Percentage of antiretroviral therapy‐potent combination: Leukoreduced group = 27%; Unmodified group = 22% Karnofsky score: Leukoreduced group = 71.4 ± 13.2; Unmodified group = 70.9 ± 12.8 CD4 cells/μL, median: Leukoreduced group = 16 (3 to 71.5); Unmodified group = 12.5(4 to 76) |
|
| Interventions |
Cointervention: Leukoreduced platelets if was required. |
|
| Outcomes |
|
|
| Notes | Trial registration: Not reported Funding: This study was financially supported by Roche Molecular systems and National Heart, Lung and Blood Institute (contract RR00046) (Page 1600). Role of sponsor: Reagents: Funding/Support: Reagents for detection and quantitation of CMVDNA by polymerase chain reaction were contributed by Roche Molecular Systems (Alameda,Calif). Support provided by National Heart was not detailed A priori sample size estimation: Yes Conducted: July 1995 through June 1999 Declared conflicts of interest: Trial authors received research funding from Roche |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The study was a randomised, double blind, comparative study" (Page 1593). Quote: "Treatment allocation was made centrally by the study coordinating center, using stratified permuted blocks with dynamic balancing within each center" (Page 1593). |
| Allocation concealment (selection bias) | Low risk | Quote: "Treatment allocation was made centrally by the study coordinating center, using stratified permuted blocks with dynamic balancing within each center" (Page 1593). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The participants, investigators, study coordinators, and persons having any contact with the patients were blinded to study treatment assignments. Blood bank technical staff who prepared the blood products were aware of the treatment assignments" (Page 1593). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "The participants, investigators, study coordinators, and persons having any contact with the patients were blinded to study treatment assignments. Blood bank technical staff who prepared the blood products were aware of the treatment assignments" (Page 1593). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss after transfusion: 9.8% (51/521) Loss after transfusion LR group: 10.8 (28/259) Loss after transfusion Control group: 8.8% (23/262) Imbalance between comparison groups: 2% |
| Selective reporting (reporting bias) | Low risk | Comment: The study protocol is available and all of the study's pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way. |
| Other bias | Low risk | Comment: The study appears to be free of other sources of bias. |
Donati 2014.
| Methods | Design: Parallel group RCT Country: Italy Multicentre study: No Setting: Hospital Follow‐up: Not clearly reported, outcomes were measured up to 1 hour after blood transfusion Unit of allocation: Patients Unit of analysis: Patients |
|
| Participants | Inclusion criteria: Adult patients admitted to ICU of the AOU Ospedali Riuniti of Ancona with sepsis, severe sepsis or septic shock as diagnosed according to standard criteria and requiring blood transfusion for haemoglobin (Hb) levels of less than 8 g/dL or as indicated by the attending physician in accordance with the local hospital guidelines. Exclusion criteria: Aged < 18 years, previous blood transfusions during ICU stay, previous history of coagulation disorders, cardiogenic or hemorrhagic shock, pregnancy and factors impeding the sublingual microcirculation evaluation (oral surgery and maxillofacial trauma)
Leukodepleted RBC transfusion: 10 Non‐leukodepleted RBC transfusion: 10
Main characteristics of patients: Age: Non‐leukodepleted group = 70 (65 to 72) years; leukodepleted group = 74 (64 to 79) years Percentage of men: Non‐leukodepleted group = 50%; leukodepleted group = 70% |
|
| Interventions |
Cointervention: Related to sepsis treatment (fluid therapy, vasopressors and inotropic agents, antibiotics, etc.) |
|
| Outcomes |
|
|
| Notes | Trial Registration: NCT01584999 Funding: Not reported Role of sponsor: Not reported A priori sample size estimation: Yes Conducted: February 2011 and 2012 Declared conflicts of interest: One trial author "CI is the inventor of Sidestream Dark Field imaging technology" technique used to measure the outcomes, this author "holds shares in MicroVision Medical and was a consultant for this company more than four years ago but has had no further contact with the company since then. He declares that he has no other competing interests in this field other than his commitment to promoting the importance of the microcirculation during patient care and no other relationships or activities that could appear to have influenced the submitted work. HV holds the position of chief scientific officer in GlycoCheck BV. The other authors declare that they have no competing interests". |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not reported. |
| Allocation concealment (selection bias) | Low risk | "Blood product randomization was performed through sealed envelopes by a physician at the blood bank" (Page 2). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | "a physician at the blood bank blindly provided the blood bags to the ICU; neither the attending physician nor the investigators nor the patients were aware of the type of RBCs transfused" (Page 2). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | "a physician at the blood bank blindly provided the blood bags to the ICU; neither the attending physician nor the investigators nor the patients were aware of the type of RBCs transfused" (Page 2). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: All patients transfused were analysed. Patients lost to follow‐up: None. |
| Selective reporting (reporting bias) | Low risk | Comment: The study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | — |
Jensen 1996.
| Methods | Design: Parallel group RCT Country: Denmark Multicentre study: Yes (2 university departments of colorectal surgery; page 844). Setting: Hospital Follow‐up: 30 days after surgery Unit of allocation: Patients Unit of analysis: Patients |
|
| Participants | Inclusion criteria: Patients admitted for elective colorectal surgery Exclusion criteria: < 18 years of age, need for emergency surgery, or immunosuppressive treatment, except steroids
Leucocyte‐depleted red cells group: 290 Buffy‐coat‐poor red cells group: 299
Main characteristics of patients: Age = Median (range): Leucocyte‐depleted red cells group = 69 (35 to 89) years; Buffy‐coat‐poor red cells group = 68 (29 to 92) years Percentage of men: Leucocyte‐depleted red cells group = 50%; buffy‐coat‐poor red cells group = 48% Number of procedures: Sigmoid resection: Leucocyte‐depleted red cells group = 11; Buffy‐coat‐poor red cells group = 19 Blood loss = Median (range): Leucocyte‐depleted red cells group = 715 (50 to 3500) mL; Buffy‐coat‐poor red cells group = 805 (10 to 4300) mL. |
|
| Interventions |
Cointervention: Quote: "All patients received an intravenous dose of cefuroxime 3 g and metronidazole 1.5 g after induction of anaesthesia" (Page 842). |
|
| Outcomes | This RCT did not specify by primary or secondary outcomes.
|
|
| Notes | Trial Registration: Not reported. Funding: Not reported. Role of sponsor: Not stated. A priori sample size estimation: Yes. Conducted: Between January 1992 and January 1995. Declared conflicts of interest: Not reported. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "were randomly allocated using sealed envelopes to receive either..." (Page 841). Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "were randomly allocated using sealed envelopes to receive either..." (Page 841) Use of opaque envelopes is not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Physicians who were blinded to the transfusion protocol performed follow‐up examinations..." (Page 842). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: All patients transfused were analysed. (Page 842). |
| Selective reporting (reporting bias) | Low risk | Comment: The study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Unclear risk | Comment: Sample size estimation took into account loss to follow‐up due to no transfusion. |
Lapierre 2007.
| Methods | Design: Parallel group RCT Country: France Multicentre study: No Setting: Hospital Follow‐up: 6 months Unit of allocation: Patients Unit of analysis: Patients |
|
| Participants | Inclusion criteria: "Patients included in the trial were more than 18 years of age and of both sexes and were to undergo surgery for cancer...with a transfusion‐during‐surgery (TdS) risk greater than 30 percent". Exclusion criteria: "Patients were not eligible for inclusion if they presented contraindications to the use of UN‐RBCs or presented any RBC antibodies and/or anti‐HLA and/or antigranulocyte alloimmunization" (page 1692).
Unmodified RBCs (UN‐RBC): 19 Leukoreduced RBCs (LR‐RBC): 18
Main characteristics of patients: Age = Median (range): Unmodified RBCs group = 56 (40 to 73) years; Leukoreduced RBCs group= 54 (37 to 65) years Percentage of men: Unmodified RBCs group = 33%; Leukoreduced RBCs group = 47% Tumour location: Pelvis: Unmodified RBCs group = 11; Leukoreduced RBCs group = 8. Head and neck: Unmodified RBCs group = 6; Leukoreduced RBCs group = 7. Miscellaneous: Unmodified RBCs group = 1; Leukoreduced RBCs group = 2 Blood loss = Median (range): Unmodified RBCs group = 1500 (300 to 3650) mL; Leukoreduced RBCs group = 1325 (300 to 6800) mL |
|
| Interventions |
Cointervention: Two patients (11%) in the unmodified RBCs group and three patients (18%) received fresh‐frozen plasma. None of the patients received platelet concentrate. |
|
| Outcomes | "The main endpoint of the study was to compare immune status in both treatment groups" (page 1692). This was measured through surrogate variables (i.e. microchimerism, peripheral blood cell counts and cytokine production capacity). However, other outcomes were described: "In addition to immune status, other factors compared between the two groups were survival and incidence of nosocomial infection" (page 1694). | |
| Notes | Trial registration: ClinicalTrials database NCT00180869 Funding: "grants from the French Association for Cancer Research (L'Association pour la Recherche sur le Cancer [9653]) and the French Association for Blood Transfusion Research (L'Association pour la Recherche enTransfusion [081997])" (page 1691) Role of sponsor: Not stated A priori sample size estimation: Yes Conducted: between 15 September 1997 and 28 February 1998 Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The randomization was performed centrally by computer in the Gustave Roussy Cancer Institute Biostatistics Unit after the investigator had sent a fax indicating the minimization factors of the patient" (page 1693). |
| Allocation concealment (selection bias) | Unclear risk | Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "Patients and surgeons were not blinded of the treatment allocation" (page 1693). |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Quote: "Patients and surgeons were not blinded of the treatment allocation" (page 1693). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | 36 patients were transfused: 18 received unmodified RBCs (UN‐RBC) and 18 received Leukoreduced RBCs (LR‐RBC). Loss after transfusion: 2.77% (1/36). Loss after transfusion LR group: 1 died during surgery. Loss after transfusion Control group: None. Loss after transfusion. Imbalance between comparison groups: 5%. |
| Selective reporting (reporting bias) | Unclear risk | Survival after perioperative transfusion is reported in Figure 2. However, number of death is not clearly reported. |
| Other bias | Unclear risk | Comment: Sample size estimate was calculated based on Th2 polarization. It is unclear what dropout rate was considered in the sample size estimation of 75 participants. |
Nathens 2006.
| Methods | Design: Parallel group RCT Country: USA Multicentre study: No Setting: Hospital Follow‐up: 28 days after randomisation Unit of allocation: Patients Unit of analysis: Patients |
|
| Participants | Inclusion criteria: Age of above 17 years and red cell transfusion within 24 hours of injury Exclusion criteria: Those with an anticipated survival of less than 48 hours, active infection at presentation, receipt of blood products for the current injury before randomisation, individuals with blood group AB Rh negative or B Rh negative, patients with clinically significant red cell alloantibodies requiring an antiglobulin crossmatch, recipients with prior requirements for irradiation, leukoreduction, od CMV protection, subjects enrolled in a concurrent study of pre‐hospital hypertonic saline resuscitation or incarcerated subjects.
Standard transfusion: 935 Leukoreduced transfusion: 929
Main characteristics of patients included in full analysis. Age: Standard group = 42.1 ± 18 years; Leukoreduced group = 42.3 ± 19 years Percentage of men: Standard group = 69%; Leukoreduced group = 66% Percentage of penetrating injury mechanism: Standard group = 18%; Leukoreduced group = 19% Injury Severity Score: Standard group = 25.5 ± 11; Leukoreduced group = 23.9 ± 11 |
|
| Interventions |
Cointerventions: "All patients received apheresis platelets when platelets were required" (Page 343). |
|
| Outcomes |
Note: TRALI was assessed by Watkins 2008 as a secondary analysis. |
|
| Notes | Trial registration: www.clinicaltrials.gov, August 23, 2005. Registration No.: NCT00135291 Funding: National Institutes of Health (NIH) Role of sponsor: The sponsor had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review or approval of the manuscript. A priori sample size estimation: Yes Conducted: Between 3 February 2003 and 30 August 2004. Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "The hospital‐based transfusion support service performed the randomization in a 1:1 ratio, using a permuted block scheme (block size of six)" (Page 344). |
| Allocation concealment (selection bias) | Low risk | Quote: "Using preprinted sealed opaque envelopes containing the study identification number and randomization arm (listed as arm 1 or arm 2) to conceal allocation" (Page 344). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Before unit issue, the transfusion service added a Food and Drug Admnistration approved study label to blind the leukoreduction process; the transfusion report accompanying the red cell unit was also blinded" (Page 343). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Before unit issue, the transfusion service added a Food and Drug Admnistration approved study label to blind the leukoreduction process; the transfusion report accompanying the red cell unit was also blinded" (Page 343). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss after transfusion: 5% (16/324). Loss after transfusion LR group: 7% (11/156). Loss after transfusion Control group: 3% (5/168). Imbalance between comparison groups: 4%. |
| Selective reporting (reporting bias) | Low risk | Comments: The study protocol is available and all of the study's pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way. |
| Other bias | Low risk | Comment: The study appears to be free of other sources of bias. |
Sanfilippo 1985.
| Methods | Design: Parallel group RCT Country: USA Multicentre study: No Setting: Hospital Follow‐up: 1 year Unit of allocation: Patients Unit of analysis: Patients |
|
| Participants | Inclusion criteria: All potential cadaver renal allograft recipients Exclusion criteria: Not clearly reported
PRBCs group: 42 Leukocyte poor red cells group: 45 Mixed group: 20
Main characteristics of patients included in full analysis were not fully stated: Quote: "there were no significant differences between transfusion groups in terms of demographic factors, including number of transfusions, age, race, sex, degree of HLA match, number of diabetics or the use of ATG posttransplant" (Page 117). |
|
| Interventions |
Cointerventions: "All transplant recipients received conventional maintenance immunosuppressive therapy with azathioprine and prednisone, and antithymocyte globulin (ATG) and/or bolus methylprednisolone was used for the treatment of rejection episodes" (Page 117). |
|
| Outcomes | This RCT did not specify by primary or secondary outcomes.
|
|
| Notes | Trial registration: Not reported. Funding: National Kidney Foundation of North Carolina Role of sponsor: Not stated A priori sample size estimation: No Conducted: Between September 1980 and June 1982 Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "...after obtaining informed consent, patients were randomly assigned to receive" (Page 116). Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Allocation concealment (selection bias) | Unclear risk | Quote: "...after obtaining informed consent, patients were randomly assigned to receive..." (Page 116). Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Incomplete outcome data (attrition bias) All outcomes | Unclear risk | Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Selective reporting (reporting bias) | High risk | Comment: The study report fails to include results for a key outcome that would be expected to have been reported for such a study. |
| Other bias | High risk | Design bias. |
Tartter 1998.
| Methods | Design: Parallel group RCT Country: USA Multicentre study: No Setting: Hospital Follow‐up: Unclear. Quote: "Patients were followed up daily in the hospital until discharge (...) and contacted by phone following discharge to elicit possible symptoms of infection". Unit of allocation: Patients Unit of analysis: Patients |
|
| Participants | Inclusion criteria: Those scheduled for inpatient gastrointestinal surgery under general anaesthesia Exclusion criteria: Not clearly reported
Filtered group: 106 Unfiltered group: 118
Main characteristics of patients: Age (Unclear if median or mean): Filtered group = 54 years; Unfiltered group = 50 years Percentage of men: Filtered group = 49%; Unfiltered group = 50% Hematocrit (Unclear if median or mean): Filtered group = 38; Unfiltered group = 37 Percentage of hypertension: Filtered group = 14%; Unfiltered group = 10% Percentage of diagnosis of malignancy: Filtered group = 38%; Unfiltered group = 38% |
|
| Interventions |
Cointerventions: "Preoperative preparation included intravenous antibiotics for all patients and bowel cleansing with Golytely for patients in whom transection of the colon or rectum was anticipated" (Page 463) |
|
| Outcomes | This RCT did not specify by primary or secondary outcomes.
|
|
| Notes | Trial Registration: Not reported. Funding: Pall Corporation, Gel Cove, NY Role of sponsor: Not stated. A priori sample size estimation: Unclear. Trial authors reported the criteria for sample size calculation, including a 60% of dropout rate ("40% of gastrointestinal surgery patients at our institution receive blood transfusions"). The software or method for sample size calculation is not reported. Using the ARCSINUS approximation, and using the same criteria reported by authors, 174 subjects are necessary in first group and 174 in the second to find as statistically significant a proportion difference, expected to be of 0.2 in group 1 and 0.05 in group 2, with an anticipated drop‐out rate of 60%. The study included 224 participants (118 and 106 patients in each group), 59 were transfused (26%) and 50 participants received allogeneic RBC transfusions. Conducted: Between 1 August 1993 and 31 January 1994 Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly allocated by the study personnel in the blood bank" (Page 463). Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Allocation concealment (selection bias) | Unclear risk | Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: all patients transfused were analysed (Page 842). |
| Selective reporting (reporting bias) | High risk | This RCT did not report mortality. Comment: The study report fails to include results for a key outcome that would be expected to have been reported for such a study. |
| Other bias | High risk | Design bias. Sample size bias. Trial authors reported the criteria for sample size calculation, including a 60% of dropout rate ("40% of gastrointestinal surgery patients at our institution receive blood transfusions"). The software or method for sample size calculation is not reported. Using the ARCSINUS approximation, and using the same criteria reported by the study authors, 174 subjects are necessary in first group and 174 in the second to find as statistically significant a proportion difference, expected to be of 0.2 in group 1 and 0.05 in group 2, with an anticipated drop‐out rate of 60%. The study included 224 participants (118 and 106 patients respectively), 59 were transfused (26%) and 50 participants received allogeneic RBC transfusions. |
Titlestad 2001.
| Methods | Design: Parallel group RCT Country: Denmark Multicentre study: No Setting: Hospital Follow‐up: 30 days Unit of allocation: Patients Unit of analysis: Patients |
|
| Participants | Inclusion criteria: Patients admitted —acute and elective— to the Department of Colorectal surgery, undergoing open colorectal surgery Exclusion criteria: Those receiving blood transfusions within the final 3 months prior to surgery and those below 18 years
Leukocyte‐depleted erythrocyte suspensions group (LD‐SAGM): 139 patients Buffycoat‐depleted group: 140 patients
Main characteristics of patients: Age: Median/range: Leukocyte‐depleted erythrocyte group = 71 (66 to 77) years; Leukocyte‐depleted erythrocyte = 73 (62 to 79) years Percentage of men: LD‐SAGM group = 51%; Non‐leukocyte‐depleted erythrocyte suspensions (SAGM) group = 60% Number of malignant colorectal disease: LD‐SAGM group = 37; SAGM group = 56 Hemoglobin: Median/range: LD‐SAGM group = 12.6 (10.6 to 14.2) g/dL; SAGM group = 12.4 (11.1 to 13.9) g/dL |
|
| Interventions |
Cointervention: "all patients received perioperative prophylactic antibiotics intravenously (3 g ampicillin or 3 g cefuroxim and 1.5 g metronidazol)" (Page 149). Platelet transfusion as co‐intervention was not reported |
|
| Outcomes | This RCT did not specify by primary or secondary outcomes.
|
|
| Notes | Trial registration: Not reported Funding: Not reported Role of sponsor: Not reported A priori sample size estimation: Yes (but not fulfilled) Conducted: Between May 1997 and November 1999 Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were allocated in the blood bank to receive either..." Page 148. Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Allocation concealment (selection bias) | Unclear risk | Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "The blood units were supplied by the blood bank, and all units were blinded. White labels were placed on the unit product code numbers, but bar code labels were intact, ensuring safe handling" (Page 149). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "Surgeons who were blinded to the transfusion protocol performed the follow‐up examinations" (Page 149). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Loss after transfusion: 10.4% (13/125). Loss after transfusion LR group: 12.7 % (7/55). Loss after transfusion Control group: 8.5% (6/70). Imbalance between comparison groups: 4.2%. |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | High risk | Sample size bias. "Discontinued study due to large exclusions than expected, as well as higher rates of infection, insufficient sample size" (Page 149). The estimation of sample size bias considered 10% of random error and did not reported it. Design bias. Industry bias: Unclear. |
van de Watering 1998.
| Methods | Design: Parallel group RCT Country: The Netherlands Multicentre study: No Setting: Hospital Follow‐up: 60 days after surgery Unit of allocation: Patients Unit of analysis: Patients |
|
| Participants | Inclusion criteria: Adults patients undergoing Coronary Artery Bypass grafting (CAGB) surgery, cardiac valve surgery or a combination of both, who had not received blood within the last 6 months. Exclusion criteria: None clearly reported
Packed cells without buffy coat: 306 Fresh‐filtered units: 305 Stored‐filtered units: 303
Main characteristics of patients: Age: Standard packed cells without buffy coat group = 64.4 ± 9.5 years; Fresh‐filtered units group = 62.9 ± 9.8 years. Stored‐filtered units group = 63.3 ± 9.1 years Percentage of men: Standard packed cells without buffy coat group = 72%; Fresh‐filtered units group = 74%. SF group = 68% Percentage of history of myocardial infarction: Standard packed cells without buffy coat group = 50.3%; Fresh‐filtered units group = 44.6%. Stored‐filtered units group = 46.4% Preoperative Hb: Standard packed cells without buffy coat group = 8.8 ± 0.9 mmol/L; Fresh‐filtered units group = 8.9 ± 0.9 mmol/L. Stored‐filtered units group = 8.8 ± 0.9 mmol/L Postoperative Hb: Standard packed cells without buffy coat group = 6.6 ± 0.7 mmol/L; Fresh‐filtered units group = 6.6 ± 0.7 mmol/L. Stored‐filtered units group = 6.5 ± 0.7 mmol/L |
|
| Interventions |
Cointervention: Quote: "Antibiotic prophylaxis was given for 24 hours with CABG and for 48 hours with valve or combined surgery" (Page 563). |
|
| Outcomes |
|
|
| Notes | Trial registration: Not reported Funding: NPBI bv, Emmer‐Compascuum, The Netherlands Role of sponsor: Not reported A priori sample size estimation: unclear. Trial authors reported the only two criteria for sample size calculation (the proportion expected in each group). The dropout rate expected is not reported. Conducted: Between March 1992 and August 1994 Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "patients were, by means of a randomizations list at the hospital transfusion service, randomly allocated..." (Page 563). |
| Allocation concealment (selection bias) | Unclear risk | Comment: Insufficient information to permit judgement of ‘low risk’ or ‘high risk’. |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: "The surgeons and anesthetists were blind to the randomizations result" (Page 563). |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "The surgeons and anesthetists were blind to the randomization result" (Page 563). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: All patients transfused were analysed (Page 567). |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | Low risk | |
van Hilten 2004.
| Methods | Design: Parallel group RCT Country: The Netherlands Multicentre: Yes, 19 hospitals (3 university, 10 clinical, 6 general) Setting: Hospital Follow‐up: 15 months Unit of allocation: Patients Unit of analysis: Patients |
|
| Participants | Inclusion criteria: Patients with ruptured aortic aneurysm elective non‐ruptured AA surgery or gastrointestinal oncology) Exclusion criteria: Those aged under 18 years, had received transfusions in the three month before the date of randomisation, or had a previous adverse reaction to blood transfusions or had a specific indications for filtered products.
Non‐filtered products: 605 Filtered products: 595
Main characteristics of patients allocated to groups (transfused+non‐transfused): Age: Non‐filtered group = 67 ± 11 years; Filtered group = 66 ± 11.5 years Percentage of men: Non‐filtered group = 69%; Filtered group = 68% Percentage of patients transfused: Non‐filtered group = 53%; Filtered group = 51% Duration of surgery: Non‐filtered group = 210 min; Filtered group = 205 min |
|
| Interventions |
|
|
| Outcomes | Primary:
Secondary:
|
|
| Notes | Trial registration: www.clinicaltrials.gov, 23 August 2005. Registration No.: NCT00135291 Funding: Health insurance Board, the Netherlands, The National Sanquin Bllod banks. Role of sponsor: Not reported A priori sample size estimation: Yes Conducted: Since June 2000 until December 2001 Declared conflicts of interest: Yes Note: 22 patients because of administrative and logistic errors. The intake of patients in the study had to be stopped at the end of 2001 because of the implementation of universal leucocyte depletion of RBCs in The Netherlands. This measure was taken by the Dutch Ministry of Health in an effort to reduce the risk of possible transmission of variant Creutzfeldt‐Jacob disease in non‐filtered transfusions. |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "randomisation was performed either by telephone (central registration of randomisation) or by opening numbered and sealed envelopes at the hospital blood transfusion services. The transfusion service ensured that the released RBCs appeared identical" (Page 2). |
| Allocation concealment (selection bias) | Low risk | Quote: "randomisation was performed either by telephone (central registration of randomisation) or by opening numbered and sealed envelopes at the hospital blood transfusion services. The transfusion service ensured that the released RBCs appeared identical" (Page 2). |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "Neither the identity of the patient nor the randomisation group was stored in the main database. The actual randomisation was provided to the statistician only at the final analysis. (Page 2). |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: "During the study, protocol violations were reported monthly to the national trial office. Patients who received products in violation of randomisation remained in the assigned arm for intention to treat analysis." (Page 2). |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Loss after transfusion: 9.35% (51/545). Loss after transfusion filtered RBC transfusions: 11% (30/267). Loss after transfusion non‐filtered RBC transfusions: 7.5% (21/278). Imbalance between comparison groups: 3.5%. Comment: Missing outcome data are balanced in numbers across study groups. However, reasons for missing outcome data are likely to be related to true outcome (Protocol violations). |
| Selective reporting (reporting bias) | Low risk | The study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified. |
| Other bias | High risk | Design bias. |
Wallis 2002.
| Methods | Design: Parallel group RCT Country: UK Multicentre study: No Setting: Hospital Follow‐up: 3 months after discharge Unit of allocation: Patients Unit of analysis: Patients |
|
| Participants | Inclusion criteria: Patients admitted for elective coronary artery bypass grafting or aortic or mitral valve replacement, either singly or in combination Exclusion criteria: Those with a history of recurrent infections, had a current blood disorder, were taking steroid or other immunosuppressive drugs or received transfusions within the past 12 months
Plasma reduced group: 198 patients Buffy coat‐depleted group: 204 patients WBC filtered group: 195 patients
Main characteristics of patients (included non‐transfused): Age: Plasma reduced group = 62.2 ± 9.1 years; Buffy coat‐depleted group = 62.4 ± 8.1 years. WBC filtered group = 61.7 ± 8.6 years Gender ratio (men to women): Plasma reduced group = 2.9; Buffy coat‐depleted group = 2.6; WBC filtered group= 2.9 Preoperative Hb in g/dL: Plasma reduced group = 14.2 ± 1.2; Buffy coat‐depleted group = 14.1 ± 1.2. WBC filtered group = 14.2 ± 1.2 Discharge Hb in g/dL: Plasma reduced group = 11.3 ± 0.9; Buffy coat‐depleted group = 11.3 ± 1. WBC filtered group = 11.1 ± 0.9 |
|
| Interventions |
|
|
| Outcomes | Primary
Secondary:
|
|
| Notes | Trial registration: Not reported Funding: This study was supported in part by a grant from the Northern and Yorkshire R & D directorate of the National Health Service Role of sponsor: Not reported A priori sample size estimation: Yes Conducted: Not reported Declared conflicts of interest: Not reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: "Patients were randomly assigned to receive, in the event of a transfusion, PR, BCD, or WCF blood" (Page 1128). |
| Allocation concealment (selection bias) | Unclear risk | Quote: "Randomization by sealed envelopes was carried out in the hospital blood transfusion department at the time of the admission clinic" (Page 1128). Use of opaque envelopes is not reported. |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: "The surgical staff were not blinded as to the blood component given, but were unaware of the randomization when the first decision to transfuse was made" (Page 1128). |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: Collection and review of data to determine postoperative infections and other variables were carried out without knowledge of the randomization or type of blood given" (Page 1128). |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Comment: All patients transfused were analysed. |
| Selective reporting (reporting bias) | Low risk | The study protocol is unavailable but it is clear that the published reports include all expected outcomes, including those that were pre‐specified (convincing text of this nature may be uncommon). |
| Other bias | Low risk | Comment: The study appears to be free of other sources of bias. |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bowden 1995 | The study population received other blood components along with or different from PRBC transfusion. |
| Bracey 2002 | Non‐randomised clinical trial. |
| Connery 2005 | Study protocol included patients with no indication of RBCs. Intervention poorly specified. |
| de Vries 2003 | No control group. |
| de Vries 2004 | No transfusion intervention. |
| Dzik 2002 | Study protocol included patients with no indication of RBCs. |
| Efstathiou 2003 | Autologous transfusion as intervention. |
| Gilbert 1989 | The study population received other blood components along with or different from PRBC transfusion. |
| Gu 1996 | The study population received other blood components along with or different from PRBC transfusion. |
| Gu 2009 | Autologous transfusion as intervention. |
| Hayashi 2000 | Autologous transfusion as intervention. |
| Houbiers 1994 | Study protocol included patients with no indication of RBCs. |
| Jensen 1992 | The study population received other blood components along with or different from PRBC transfusion. |
| Kao 1995 | The study population received other blood components along with or different from PRBC transfusion (platelets intervention). |
| Koskenkari 2005 | No transfusion intervention. |
| Leal‐Noval 2005 | No transfusion intervention. |
| Llewelyn 2004 | Non‐randomised clinical trial. |
| Nielsen 1999 | Study protocol included patients with no indication of RBCs. |
| Opelz 1997 | Control group did not receive transfusion. |
| Salamonsen 2005 | No transfusion intervention. |
| Skånberg 2007 | Non‐randomised clinical trial. |
| So‐Osman 2010 | Did not report a control group. |
| Vamvakas 2007 | Meta‐analysis. |
| van de Watering 2004 | Narrative review. |
Characteristics of studies awaiting assessment [ordered by study ID]
NCT00810810.
| Methods | Study design: Parallel group RCT Allocation: Randomized Endpoint classification: Efficacy study Intervention model: Parallel assignment Masking: Single blind (Investigator) Primary purpose: Prevention |
| Participants | Inclusion criteria:
Exclusion criteria:
Condition requiring high volume transfusion therapy. |
| Interventions | Active comparator 1: Standard blood components Transfusion, if ordered by physician, with unfiltered RBCs and apheresis platelets Experimental 2: Leukoreduced blood components Transfusion, if ordered by a physician, of leukoreduced RBCs and apheresis platelets Experimental: 3 Leukoreduced and irradiated Transfusion, if ordered by physician, of gamma irradiated leukoreduced RBCs and gamma irradiated apheresis platelets |
| Outcomes | Primary outcomes:
Secondary outcomes:
(Time frame: 0 to 5 weeks after surgery) |
| Notes | This study has been completed, but we did not find any publication related to it in the search. Inclusion or exclusion decision cannot be made because sufficient information is not currently available. |
Waghmare 2012.
| Methods | Study Design: RCT Allocation: Randomized Endpoint classification: Efficacy study Intervention model: Parallel assignment Masking: Open labeled Primary purpose: Prevention |
| Participants | Sixty‐four consecutive ICU. All had severe falciparum malaria and required blood transfusion. Pregnant women and patients with previous blood transfusion were excluded. |
| Interventions | Filtered group: Leukodepleted blood transfusion using bedside leukodepletion filter versus regular Control group: non‐leukodepleted blood transfusion |
| Outcomes | Death from all cases at 28 days, incidence of Acute Respiratory Distress Syndrome and sepsis, severity of multiple organ dysfunction, and length of ICU stay in the two treatment groups. Patients were studied over 16 months. |
| Notes | Registration number: Unknown Inclusion or exclusion decision cannot be made because sufficient information is not currently available. |
Zhao 2004.
| Methods | Study design: RCT Allocation: Randomized Endpoint classification: Efficacy study Intervention model: Parallel assignment Masking: Unknown Primary purpose: Prevention |
| Participants | One hundred patients with cirrhosis of liver, gastric ulcer and cancer were selected to receive RBC concentrates with leukocyte filtration. Another group of 50 patients with liver necrosis, gastric ulcer and cancer were selected to receive non‐filtered RBC concentrates. Two hundred and forty patients with acute or chronic leukaemia, aplastic anaemia, multiple myeloma, thrombocytopenia purpura, diabetes mellitus, cirrhosis of liver, upper gastrointestinal haemorrhage, severe hepatitis, burn and cancer post radioactive or chemical treatment were divided into 2 groups with 120 patients in each one and selected randomly to receive platelet concentrates. |
| Interventions | RBC concentrates with leukocyte filtration versus non‐filtered RBC concentrates. |
| Outcomes | incidence rates of febrile nonhaemolytic transfusion reactions (FNHTR). |
| Notes | Registration number: Unknown. Inclusion or exclusion decision cannot be made because sufficient information is not currently available. |
Differences between protocol and review
In order to improve the quality of this Cochrane review, we made the following changes from the original protocol (Simancas‐Racines 2012):
Data synthesis included a second meta‐analysis: 'only transfused patients' as a sensitivity analysis. We performed this analysis due to the important number of patients not transfused as reported in most of the included studies. This analysis complements the main analysis planned in the review protocol: events reported among the total number of randomised patients.
We carried out a sensitivity analysis "excluding post‐storage leukoreduction studies" to explore the effect of this variable on the effect estimate.
We conducted a TSA to assess the risk of random errors in the cumulative meta‐analyses.
We changed our criteria for assessing the statistical heterogeneity in the meta‐analyses. In the protocol it was classified an I² statistic value of 40 to 60% as moderate, and 75% and above as high. In the review, we have now defined moderate heterogeneity as an I² statistic of 50 to 74%, and high as 75% or above.
Contributions of authors
All review authors contributed to the conception and design of this Cochrane review. Doctors Simancas‐Racines, Arevalo‐Rodriguez and Osorio contributed to the analysis and interpretation of data, and drafted the manuscript. All review authors contributed by commenting on the review critically for intellectual content and gave final approval of the document to be published.
Sources of support
Internal sources
-
Universidad Tecnológica Equinoccial, Ecuador.
Academic
Fundación Universitaria de Ciencias de la Salud, Bogotá D.C., Colombia.
External sources
-
Iberoamerican Cochrane Center, Spain.
Academic
Declarations of interest
IA‐R: None known.
AM‐C: None known.
DO: None known.
DS‐R: None known.
New
References
References to studies included in this review
Bilgin 2004 {published data only}
- Bilgin YM, Watering LM, Eijsman L, Versteegh MI, Brand R, Oers MH, et al. Double‐blind, randomized controlled trial on the effect of leukocyte‐depleted erythrocyte transfusions in cardiac valve surgery. Circulation 2004;109(22):2755‐60. [PUBMED: 15148271] [DOI] [PubMed] [Google Scholar]
Boshkov 2006 {published data only}
- Boshkov LK, Chien G, VanWinkle D, Furnary AP, Wu Y, Grunkemeirer GI, et al. Prestorage leukoreduction of transfused packed red cells is associated with significant ongoing 1‐12 month survival benefit cardiac surgery patients. Blood 2006;108:578. [Google Scholar]
Collier 2001 {published data only}
- Collier AC, Kalish LA, Busch MP, Gernsheimer T, Assmann SF, Lane TA, et al. Leukocyte‐reduced red blood cell transfusions in patients with anemia and human immunodeficiency virus infection: the Viral Activation Transfusion Study: a randomized controlled trial. JAMA 2001;285(12):1592‐601. [PUBMED: 11268267] [DOI] [PubMed] [Google Scholar]
- Lane TA, Gernsheimer T, Mohandas K, Assmann SF. Signs and symptoms associated with the transfusion of WBC‐reduced RBCs and non‐WBC‐reduced RBCs in patients with anemia and HIV infection: results from the Viral Activation Transfusion Study. Transfusion 2002;42(2):265‐74. [PUBMED: 11896345] [DOI] [PubMed] [Google Scholar]
Donati 2014 {published data only}
- Donati A, Damiani E, Luchetti M, Domizi R, Scorcella C, Carsetti A, et al. Microcirculatory effects of the transfusion of leukodepleted or non‐leukodepleted red blood cells in patients with sepsis: a pilot study. Critical Care 2014;18(1):R33. [PUBMED: 24528648] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jensen 1996 {published data only}
- Jensen LS, Kissmeyer‐Nielsen P, Wolff B, Qvist N. Randomised comparison of leucocyte‐depleted versus buffy‐coat‐poor blood transfusion and complications after colorectal surgery. Lancet 1996;348(9031):841‐5. [PUBMED: 8826808] [DOI] [PubMed] [Google Scholar]
Lapierre 2007 {published data only}
- Lapierre V, Aupérin A, Robinet E, Ferrand C, Oubouzar N, Tramalloni D, et al. Immune modulation and microchimerism after unmodified versus leukoreduced allogeneic red blood cell transfusion in cancer patients: results of a randomized study. Transfusion 2007;47(9):1691‐9. [PUBMED: 17725736] [DOI] [PubMed] [Google Scholar]
Nathens 2006 {published data only}
- Nathens AB, Nester TA, Rubenfeld GD, Nirula R, Gernsheimer TB. The effects of leukoreduced blood transfusion on infection risk following injury: a randomized controlled trial. Shock 2006;26(4):342‐7. [PUBMED: 16980879] [DOI] [PubMed] [Google Scholar]
- Watkins TR, Rubenfeld GD, Martin TR, Nester TA, Caldwell E, Billgren J, et al. Effects of leukoreduced blood on acute lung injury after trauma: a randomized controlled trial. Critical Care Medicine 2008;36(5):1493‐9. [PUBMED: 18434890] [DOI] [PubMed] [Google Scholar]
Sanfilippo 1985 {published data only}
- Sanfilippo FP, Bollinger RR, MacQueen JM, Brooks BJ, Koepke JA. A randomized study comparing leukocyte‐depleted versus packed red cell transfusions in prospective cadaver renal allograft recipients. Transfusion 1985;25(2):116‐9. [PUBMED: 3885483] [DOI] [PubMed] [Google Scholar]
Tartter 1998 {published data only}
- Tartter PI, Mohandas K, Azar P, Endres J, Kaplan J, Spivack M. Randomized trial comparing packed red cell blood transfusion with and without leukocyte depletion for gastrointestinal surgery. American Journal of Surgery 1998;176(5):462‐6. [PUBMED: 9874434] [DOI] [PubMed] [Google Scholar]
Titlestad 2001 {published data only}
- Titlestad IL, Ebbesen LS, Ainsworth AP, Lillevang ST, Qvist N, Georgsen J. Leukocyte‐depletion of blood components does not significantly reduce the risk of infectious complications. Results of a double‐blinded, randomized study. International Journal of Colorectal Disease 2001;16(3):147‐53. [PUBMED: 11459288] [DOI] [PubMed] [Google Scholar]
van de Watering 1998 {published data only}
- Watering LM, Hermans J, Houbiers JG, Broek PJ, Bouter H, Boer F, et al. Beneficial effects of leukocyte depletion of transfused blood on postoperative complications in patients undergoing cardiac surgery: a randomized clinical trial. Circulation 1998;97(6):562‐8. [PUBMED: 9494026] [DOI] [PubMed] [Google Scholar]
van Hilten 2004 {published data only}
- Lange MM, Hilten JA, Watering LM, Bijnen BA, Roumen RM, Putter H, et al. Leucocyte depletion of perioperative blood transfusion does not affect long‐term survival and recurrence in patients with gastrointestinal cancer. The British Journal of Surgery 2009;96(7):734‐40. [PUBMED: 19526613] [DOI] [PubMed] [Google Scholar]
- Hilten JA, Watering LM, Bockel JH, Velde CJ, Kievit J, Brand R, et al. Effects of transfusion with red cells filtered to remove leucocytes: randomised controlled trial in patients undergoing major surgery. BMJ 2004;328(7451):1281. [PUBMED: 15142885] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wallis 2002 {published data only}
- Wallis JP, Chapman CE, Orr KE, Clark SC, Forty JR. Effect of WBC reduction of transfused RBCs on postoperative infection rates in cardiac surgery. Transfusion 2002;42(9):1127‐34. [PUBMED: 12430668] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Bowden 1995 {published data only}
- Bowden RA, Slichter SJ, Sayers M, Weisdorf D, Cays M, Schoch G, et al. A comparison of filtered leukocyte‐reduced and cytomegalovirus (CMV) seronegative blood products for the prevention of transfusion‐associated CMV infection after marrow transplant. Blood 1995;86(9):3598‐603. [PUBMED: 7579469] [PubMed] [Google Scholar]
Bracey 2002 {published data only}
- Bracey AW, Radovancevic R, Nussmeier NA. Leukocyte‐depleted blood in open‐heart surgery patients: effects on outcome. Transfusion 2002;42(Suppl):5S. [Google Scholar]
Connery 2005 {published data only}
- Connery CP, Toumpoulis IK, Anagnostopoulos CE, Hillel Z, Rahman FG, Katritsis D, et al. Does leukofiltration reduce pulmonary infections in CABG patients? A prospective, randomized study with early results and mid‐term survival. Acta Cardiologica 2005;60(3):285‐93. [PUBMED: 15999468] [DOI] [PubMed] [Google Scholar]
de Vries 2003 {published data only}
- Vries AJ, Gu YJ, Post WJ, Vos P, Stokroos I, Lip H, et al. Leucocyte depletion during cardiac surgery: a comparison of different filtration strategies. Perfusion 2003;18(1):31‐8. [PUBMED: 12705648] [DOI] [PubMed] [Google Scholar]
de Vries 2004 {published data only}
- Vries AJ, Gu YJ, Oeveren W. Leucocyte filtration of residual heart‐lung machine blood in children undergoing congenital heart surgery. Perfusion 2004;19(6):345‐9. [PUBMED: 15619967] [DOI] [PubMed] [Google Scholar]
Dzik 2002 {published data only}
- Dzik WH, Anderson JK, O'Neill EM, Assmann SF, Kalish LA, Stowell CP. A prospective, randomized clinical trial of universal WBC reduction. Transfusion 2002;42(9):1114‐22. [PUBMED: 12430666] [DOI] [PubMed] [Google Scholar]
Efstathiou 2003 {published data only}
- Efstathiou A, Vlachveis M, Tsonis G, Asteri T, Psarakis A, Fessatidis IT. Does leukodepletion during elective cardiac surgery really influence the overall clinical outcome?. The Journal of Cardiovascular Surgery 2003;44(2):197‐204. [PUBMED: 12813383] [PubMed] [Google Scholar]
Gilbert 1989 {published data only}
- Gilbert GL, Hayes K, Hudson IL, James J. Prevention of transfusion‐acquired cytomegalovirus infection in infants by blood filtration to remove leucocytes. Neonatal Cytomegalovirus Infection Study Group. Lancet (London, England) 1989;1(8649):1228‐31. [PUBMED: 2566781] [DOI] [PubMed] [Google Scholar]
Gu 1996 {published data only}
- Gu YJ, Vries AJ, Boonstra PW, Oeveren W. Leukocyte depletion results in improved lung function and reduced inflammatory response after cardiac surgery. The Journal of Thoracic and Cardiovascular Surgery 1996;112(2):494‐500. [PUBMED: 8751518] [DOI] [PubMed] [Google Scholar]
Gu 2009 {published data only}
- Gu YJ, Vries AJ, Hagenaars JA, Oeveren W. Leucocyte filtration of salvaged blood during cardiac surgery: effect on red blood cell function in concentrated blood compared with diluted blood. European Journal of Cardio‐Thoracic Surgery 2009;36(5):877‐82. [PUBMED: 19608429] [DOI] [PubMed] [Google Scholar]
Hayashi 2000 {published data only}
- Hayashi Y, Sawa Y, Nishimura M, Ichikawa H, Kagisaki K, Ohtake S, et al. Clinical evaluation of leukocyte‐depleted blood cardioplegia for pediatric open heart operation. The Annals of Thoracic Surgery 2000;69(6):1914‐9. [PUBMED: 10892946] [DOI] [PubMed] [Google Scholar]
Houbiers 1994 {published data only}
- Houbiers JG, Brand A, Watering LM, Hermans J, Verwey PJ, Bijnen AB, et al. Randomised controlled trial comparing transfusion of leucocyte‐depleted or buffy‐coat‐depleted blood in surgery for colorectal cancer. Lancet 1994;344(8922):573‐8. [PUBMED: 7914960] [DOI] [PubMed] [Google Scholar]
- Watering LM, Brand A, Houbiers JG, Klein Kranenbarg WM, Hermans J, Velde C. Perioperative blood transfusions, with or without allogeneic leucocytes, relate to survival, not to cancer recurrence. The British Journal of Surgery 2001;88(2):267‐72. [PUBMED: 11167879] [DOI] [PubMed] [Google Scholar]
Jensen 1992 {published data only}
- Jensen LS, Andersen AJ, Christiansen PM, Hokland P, Juhl CO, Madsen G, et al. Postoperative infection and natural killer cell function following blood transfusion in patients undergoing elective colorectal surgery. The British Journal of Surgery 1992;79(6):513‐6. [PUBMED: 1611441] [DOI] [PubMed] [Google Scholar]
- Jensen LS, Hokland M, Nielsen HJ. A randomized controlled study of the effect of bedside leucocyte depletion on the immunosuppressive effect of whole blood transfusion in patients undergoing elective colorectal surgery. The British Journal of Surgery 1996;83(7):973‐7. [PUBMED: 8813790] [DOI] [PubMed] [Google Scholar]
Kao 1995 {published data only}
- Kao KJ, Mickel M, Braine HG, Davis K, Enright H, Gernsheimer T, et al. White cell reduction in platelet concentrates and packed red cells by filtration: a multicenter clinical trial. The Trap Study Group. Transfusion 1995;35(1):13‐9. [PUBMED: 7998062] [DOI] [PubMed] [Google Scholar]
Koskenkari 2005 {published data only}
- Koskenkari J, Rimpiläinen J, Biancari F, Surcel HM, Kaukoranta P, Kiviluoma K, et al. Leukocyte depleting filter attenuates myocardial injury during elective coronary artery bypass surgery. Scandinavian Cardiovascular Journal 2005;39(6):358‐68. [PUBMED: 16352489] [DOI] [PubMed] [Google Scholar]
Leal‐Noval 2005 {published data only}
- Leal‐Noval SR, Amaya R, Herruzo A, Hernández A, Ordóñez A, Marín‐Niebla A, et al. Effects of a leukocyte depleting arterial line filter on perioperative morbidity in patients undergoing cardiac surgery: a controlled randomized trial. The Annals of Thoracic Surgery 2005;80(4):1394‐400. [PUBMED: 16181877] [DOI] [PubMed] [Google Scholar]
Llewelyn 2004 {published data only}
- Llewelyn CA, Taylor RS, Todd AA, Stevens W, Murphy MF, Williamson LM. The effect of universal leukoreduction on postoperative infections and length of hospital stay in elective orthopedic and cardiac surgery. Transfusion 2004;44(4):489‐500. [PUBMED: 15043563] [DOI] [PubMed] [Google Scholar]
Nielsen 1999 {published data only}
- Nielsen HJ, Hammer JH, Krarup AL, Nielsen LM, Reimert CM, Pedersen AN, et al. Prestorage leukocyte filtration may reduce leukocyte‐derived bioactive substance accumulation in patients operated for burn trauma. Burns 1999;25(2):162‐70. [PUBMED: 10208393] [DOI] [PubMed] [Google Scholar]
Opelz 1997 {published data only}
- Opelz G, Vanrenterghem Y, Kirste G, Gray DW, Horsburgh T, Lachance JG, et al. Prospective evaluation of pretransplant blood transfusions in cadaver kidney recipients. Transplantation 1997;63(7):964‐7. [PUBMED: 9112348] [DOI] [PubMed] [Google Scholar]
Salamonsen 2005 {published data only}
- Salamonsen RF, Anderson J, Anderson M, Bailey M, Magrin G, Rosenfeldt F. Total leukocyte control for elective coronary bypass surgery does not improve short‐term outcome. The Annals of Thoracic Surgery 2005;79(6):2032‐8. [PUBMED: 15919304] [DOI] [PubMed] [Google Scholar]
Skånberg 2007 {published data only}
- Skånberg J, Lundholm K, Haglind E. Effects of blood transfusion with leucocyte depletion on length of hospital stay, respiratory assistance and survival after curative surgery for colorectal cancer. Acta Oncologica 2007;46(8):1123‐30. [PUBMED: 17851860] [DOI] [PubMed] [Google Scholar]
So‐Osman 2010 {published data only}
- So‐Osman C, Nelissen R, Slaa R, Coene L, Brand R, Brand A. A randomized comparison of transfusion triggers in elective orthopaedic surgery using leucocyte‐depleted red blood cells. Vox Sanguinis 2010;98(1):56‐64. [PUBMED: 19656349] [DOI] [PubMed] [Google Scholar]
Vamvakas 2007 {published data only}
- Vamvakas EC. White‐blood‐cell‐containing allogeneic blood transfusion and postoperative infection or mortality: an updated meta‐analysis. Vox Sanguinis 2007;92(3):224‐32. [PUBMED: 17348871] [DOI] [PubMed] [Google Scholar]
van de Watering 2004 {published data only}
- Watering L. What has universal leucodepletion given us: evidence from clinical trials?. Vox Sanguinis 2004;87 Suppl 2:139‐42. [PUBMED: 15209899] [DOI] [PubMed] [Google Scholar]
References to studies awaiting assessment
NCT00810810 {published data only}
- Immunomodulation Following Transfusion. https://clinicaltrials.gov/ct2/show/NCT00810810.
Waghmare 2012 {published data only}
- Waghmare N, Desai N, Karnad D. Open Labeled, Randomized, Controlled Trial Comparing Leukodepleted (Filtered) Blood Transfusion and Non‐Leukodepleted (Unfiltered) Blood Transfusion in Cases of Severe Falciparum Malaria. Chest. Glenview (IL): Proceedings of the CHEST 2012 Annual Meeting, Atlanta (GA), October 2012; Vol. 142:Meeting Abstracts: 232A.
Zhao 2004 {published data only}
- Zhao S, Chen X, Hu J, Li R. Clinical assessment of preventing febrile nonhemolytic transfusion reaction by leukocyte‐depleted blood transfusion. Zhongguo Shi Yan Xue Ye Xue Za Zhi [Journal of Experimental Hematology] 2002;10(6):568‐70. [PUBMED: 12513724 ] [PubMed] [Google Scholar]
Additional references
AETSA 2007
- Aguado M, Villegas R, Márquez S, Corbacho B, Navarro J. Universal leukorreduction. A systematic review of the literature and an economic assessment. Executive summary [Leucorreducción universal de productos sanguíneos. Revisión Sistemática de la Literatura y Evaluación Económica.]. Agencia de Evaluación de Tecnologías Sanitarias de Andalucía 2007:1‐95.
Balshem 2011
- Balshem H, Helfand M, Schünemann HJ, Oxman AD, Kunz R, Brozek J, et al. GRADE guidelines: 3. Rating the quality of evidence. Journal of Clinical Epidemiology 2011;64(4):401‐6. [PUBMED: 21208779] [DOI] [PubMed] [Google Scholar]
Blajchman 2002
- Blajchman MA. Immunomodulation and blood transfusion. American Journal of Therapeutics 2002;9(5):389‐95. [PUBMED: 12237730] [DOI] [PubMed] [Google Scholar]
Blajchman 2004
- Blajchman MA, Goldman M, Webert KE, Vamvakas EC, Hannon J, Delage G. Proceedings of a consensus conference: the screening of blood donors for variant CJD. Transfusion Medicine Reviews 2004;18(2):73‐92. [PUBMED: 15067588] [DOI] [PubMed] [Google Scholar]
Blajchman 2006
- Blajchman MA. The clinical benefits of the leukoreduction of blood products. The Journal of Trauma 2006;60(6 Suppl):S83‐90. [PUBMED: 16763486] [DOI] [PubMed] [Google Scholar]
Blajchman 2010
- Blajchman MA, Glynn SA, Josephson CD, Kleinman SH, State‐of‐the Science Symposium Transfusion Medicine Committee. Clinical trial opportunities in Transfusion Medicine: proceedings of a National Heart, Lung, and Blood Institute State‐of‐the‐Science Symposium. Transfusion Medicine Reviews 2010;24(4):259‐85. [PUBMED: 20851330] [DOI] [PubMed] [Google Scholar]
Blumberg 1998
- Blumberg N. Perioperative allogeneic blood transfusion does not cause adverse sequelae in patients with cancer: a meta‐analysis of unconfounded studies. The British Journal of Surgery 1998;85(8):1163‐4. [PUBMED: 9718033] [PubMed] [Google Scholar]
Blumberg 2007
- Blumberg N, Zhao H, Wang H, Messing S, Heal JM, Lyman GH. The intention‐to‐treat principle in clinical trials and meta‐analyses of leukoreduced blood transfusions in surgical patients. Transfusion 2007;47(4):573‐81. [PUBMED: 17381614] [DOI] [PubMed] [Google Scholar]
Blumberg 2010
- Blumberg N, Heal JM, Gettings KF, Phipps RP, Masel D, Refaai MA, et al. An association between decreased cardiopulmonary complications (transfusion‐related acute lung injury and transfusion‐associated circulatory overload) and implementation of universal leukoreduction of blood transfusions. Transfusion 2010;50(12):2738‐44. [PUBMED: 20561296] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brozek 2011
- Brozek JL, Akl EA, Compalati E, Kreis J, Terracciano L, Fiocchi A, et al. Grading quality of evidence and strength of recommendations in clinical practice guidelines part 3 of 3. The GRADE approach to developing recommendations. Allergy 2011;66(5):588‐95. [PUBMED: 21241318] [DOI] [PubMed] [Google Scholar]
Carson 2012
- Carson JL, Carless PA, Hebert PC. Transfusion thresholds and other strategies for guiding allogeneic red blood cell transfusion. Cochrane Database of Systematic Reviews 2012, Issue 4. [DOI: 10.1002/14651858.CD002042.pub3; PUBMED: 22513904] [DOI] [PMC free article] [PubMed] [Google Scholar]
CCOHTA 1998
- Gibis B, Baladi JF. Leukoreduction: the techniques used, their effectiveness and costs. Canadian Coordinating Office for Health Technology Assessmnet (CCOHTA). https://www.cadth.ca/sites/default/files/pdf/leukoreduct_tr_e.pdf (accessed 15 August 2015). [IBSN 1‐895561‐60‐4]
Chan 2013
- Chan AW, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin JA, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ Clinical Research 2013;346:e7586. [PUBMED: 23303884] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chandler 2013
- Chandler J, Churchill R, Higgins J, Lasserson T, Tovey D. Methodological standards for the conduct of new Cochrane Intervention Reviews. Version 2.3. 02 December 2013. http://editorial‐unit.cochrane.org/sites/editorial‐unit.cochrane.org/files/uploads/MECIR_conduct_standards%202.3%2002122013_0.pdf (accessed 20 September 2014).
Dellinger 2004
- Dellinger EP, Anaya DA. Infectious and immunologic consequences of blood transfusion. Critical Care 2004;8(Suppl 2):S18‐23. [PUBMED: 15196317] [DOI] [PMC free article] [PubMed] [Google Scholar]
Dwyre 2008
- Dwyre DM, Holland PV. Transfusion‐associated graft‐versus‐host disease. Vox Sanguinis 2008;95(2):85‐93. [PUBMED: 18544121] [DOI] [PubMed] [Google Scholar]
Fergusson 2004
- Fergusson D, Khanna MP, Tinmouth A, Hébert PC. Transfusion of leukoreduced red blood cells may decrease postoperative infections: two meta‐analyses of randomized controlled trials. Canadian Journal of Anaesthesia (Journal Canadien d'Anesthésie) 2004;51(5):417‐24. [PUBMED: 15128625] [DOI] [PubMed] [Google Scholar]
Flohé 2007
- Flohé S, Kobbe P, Nast‐Kolb D. Immunological reactions secondary to blood transfusion. Injury 2007;38(12):1405‐8. [PUBMED: 18048035] [DOI] [PubMed] [Google Scholar]
Friese 2008
- Friese RS, Sperry JL, Phelan HA, Gentilello LM. The use of leukoreduced red blood cell products is associated with fewer infectious complications in trauma patients. American Journal of Surgery 2008;196(1):56‐61. [PUBMED: 18513694] [DOI] [PubMed] [Google Scholar]
Gabriel 2012
- Gabriel SE, Normand SL. Getting the methods right‐‐the foundation of patient‐centered outcomes research. The New England Journal of Medicine 2012;367(9):787‐90. [PUBMED: 22830434] [DOI] [PubMed] [Google Scholar]
Galel 2009
- Galel SA, Nguyen DD, Fontaine MJ, Goodnough LT, Viele MK. Transfusion Medicine. In: Greer JP, Foerster J, Rodgers GM, Paraskevas F, Glader B, Arber DA editor(s). Wintrobe's Clinical Hematology. 12th Edition. Vol. 1, Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2009:672‐721. [Google Scholar]
Goldman 2005
- Goldman M, Webert KE, Arnold DM, Freedman J, Hannon J, Blajchman MA. Proceedings of a consensus conference: towards an understanding of TRALI. Transfusion Medicine Reviews 2005;19(1):2‐31. [PUBMED: 15830325] [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- Evidence Prime, Inc. GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University. Evidence Prime, Inc, 2015.
Guyatt 2011a
- Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction‐GRADE evidence profiles and summary of findings tables. Journal of Clinical Epidemiology 2011;64(4):383‐94. [PUBMED: 21195583] [DOI] [PubMed] [Google Scholar]
Guyatt 2011b
- Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso‐Coello P, Rind D, et al. GRADE guidelines 6. Rating the quality of evidence‐‐imprecision. Journal of Clinical Epidemiology 2011;64(12):1283‐93. [PUBMED: 21839614] [DOI] [PubMed] [Google Scholar]
Guyatt 2011c
- Guyatt GH, Oxman AD, Kunz R, Atkins D, Brozek J, Vist G, et al. GRADE guidelines: 2. Framing the question and deciding on important outcomes. Journal of Clinical Epidemiology 2011;64(4):395‐400. [PUBMED: 21194891] [DOI] [PubMed] [Google Scholar]
Guyatt 2011d
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 7. Rating the quality of evidence‐‐inconsistency. Journal of Clinical Epidemiology 2011;64(12):1294‐302. [PUBMED: 21803546] [DOI] [PubMed] [Google Scholar]
Guyatt 2011e
- Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 8. Rating the quality of evidence‐‐indirectness. Journal of Clinical Epidemiology 2011;64(12):1303‐10. [PUBMED: 21802903] [DOI] [PubMed] [Google Scholar]
Guyatt 2011f
- Guyatt GH, Oxman AD, Montori V, Vist G, Kunz R, Brozek J, et al. GRADE guidelines: 5. Rating the quality of evidence‐‐publication bias. Journal of Clinical Epidemiology 2011;64(12):1277‐82. [PUBMED: 21802904] [DOI] [PubMed] [Google Scholar]
Guyatt 2011g
- Guyatt GH, Oxman AD, Vist G, Kunz R, Brozek J, Alonso‐Coello P, et al. GRADE guidelines: 4. Rating the quality of evidence‐‐study limitations (risk of bias). Journal of Clinical Epidemiology 2011;64(4):407‐15. [PUBMED: 21247734] [DOI] [PubMed] [Google Scholar]
Guyatt 2011h
- Guyatt GH, Oxman AD, Sultan S, Glasziou P, Akl EA, Alonso‐Coello P, et al. GRADE guidelines: 9. Rating up the quality of evidence. Journal of Clinical Epidemiology 2011;64(12):1311‐6. [PUBMED: 21802902] [DOI] [PubMed] [Google Scholar]
Heddle 1999
- Heddle NM. Pathophysiology of febrile nonhemolytic transfusion reactions. Current Opinion in Hematology 1999;6(6):420‐6. [PUBMED: 10546797] [DOI] [PubMed] [Google Scholar]
Hendrickson 2009
- Hendrickson JE, Hillyer CD. Noninfectious serious hazards of transfusion. Anesthesia and Analgesia 2009;108(3):759‐69. [PUBMED: 19224780] [DOI] [PubMed] [Google Scholar]
Hiesse 2001
- Hiesse C, Busson M, Buisson C, Farahmand H, Bierling P, Benbunan M, et al. Multicenter trial of one HLA‐DR‐matched or mismatched blood transfusion prior to cadaveric renal transplantation. Kidney International 2001;60(1):341‐9. [PUBMED: 11422770] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327(7414):557‐60. [PUBMED: 12958120] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0[updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hoffman 2008
- Hoffman R, Furie B, McGlave P, Silberstein LE, Shattil SJ, Benz EJ, et al. Hematology: Basic Principles and Practice. 5th Edition. London: Churchill Livingstone, 2008. [Google Scholar]
Jensen 1998
- Jensen LS. Benefits of leukocyte‐reduced blood transfusions in surgical patients. Current Opinion in Hematology 1998;5(6):376‐80. [PUBMED: 9814642] [DOI] [PubMed] [Google Scholar]
King 2004
- King KE, Shirey RS, Thoman SK, Bensen‐Kennedy D, Tanz WS, Ness PM. Universal leukoreduction decreases the incidence of febrile nonhemolytic transfusion reactions to RBCs. Transfusion 2004;44(1):25‐9. [PUBMED: 14692963] [DOI] [PubMed] [Google Scholar]
Laupacis 2001
- Laupacis A, Brown J, Costello B, Delage G, Freedman J, Hume H, et al. Prevention of posttransfusion CMV in the era of universal WBC reduction: a consensus statement. Transfusion 2001;41(4):560‐9. [PUBMED: 11316911] [DOI] [PubMed] [Google Scholar]
Lavoie 2011
- Lavoie J. Blood transfusion risks and alternative strategies in pediatric patients. Paediatric Anaesthesia 2011;21(1):14‐24. [PUBMED: 21155923] [DOI] [PubMed] [Google Scholar]
Lefebvre 2011
- Lefebvre C, Manheimer E, Glanville J. Chapter 6: Searching for studies. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 (updated March 2011). The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Lindholm 2011
- Lindholm PF, Annen K, Ramsey G. Approaches to minimize infection risk in blood banking and transfusion practice. Infectious Disorders Drug Targets 2011;11(1):45‐56. [PUBMED: 21303341] [DOI] [PubMed] [Google Scholar]
Looney 2006
- Looney MR, Su X, Ziffle JA, Lowell CA, Matthay MA. Neutrophils and their Fc gamma receptors are essential in a mouse model of transfusion‐related acute lung injury. The Journal of Clinical Investigation 2006;116(6):1615‐23. [PUBMED: 16710475] [DOI] [PMC free article] [PubMed] [Google Scholar]
Martí‐Carvajal 2010
- Martí‐Carvajal AJ, Solà I, González LE, Leon de Gonzalez G, Rodriguez‐Malagon N. Pharmacological interventions for the prevention of allergic and febrile non‐haemolytic transfusion reactions. Cochrane Database of Systematic Reviews 2010, Issue 6. [DOI: 10.1002/14651858.CD007539] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mukagatare 2010
- Mukagatare I, Monfort M, Marchin J, Gerard C. The effect of leukocyte‐reduction on the transfusion reactions to red blood cells concentrates [Effet de la déleucocytation des concentrés érythrocytaires sur les réactions transfusionnelles]. Transfusion Clinique et Biologique 2010;17(1):14‐9. [PUBMED: 20106700] [DOI] [PubMed] [Google Scholar]
Nebeker 2004
- Nebeker JR, Barach P, Samore MH. Clarifying adverse drug events: a clinician's guide to terminology, documentation, and reporting. Annals of Internal Medicine 2004;140(10):795‐801. [PUBMED: 15148066] [DOI] [PubMed] [Google Scholar]
Phelan 2007
- Phelan HA, Sperry JL, Friese RS. Leukoreduction before red blood cell transfusion has no impact on mortality in trauma patients. Journal of Surgical Research 2007;138(1):32‐6. [PUBMED: 17161430] [DOI] [PubMed] [Google Scholar]
Renaudier 2009
- Renaudier P, Rebibo D, Waller C, Schlanger S, Vo Mai MP, Ounnoughene N, et al. Pulmonary complications of transfusion (TACO‐TRALI) [Complications pulmonaires de la transfusion (TACO–TRALI)]. Transfusion Clinique et Biologique 2009;16(2):218‐32. [PUBMED: 19446484] [DOI] [PubMed] [Google Scholar]
RevMan 2014 [Computer program]
- The Cochrane Collaboration, The Nordic Cochrane Centre. Review Manager (RevMan). Version 5.3. Copenhagen: The Cochrane Collaboration, The Nordic Cochrane Centre, 2014.
Rohde 2014
- Rohde JM, Dimcheff DE, Blumberg N, Saint S, Langa KM, Kuhn L, et al. Health care‐associated infection after red blood cell transfusion: a systematic review and meta‐analysis. JAMA 2014;311(13):1317‐26. [PUBMED: 24691607] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rühl 2009
- Rühl H, Bein G, Sachs UJ. Transfusion‐associated graft‐versus‐host disease. Transfusion Medicine Reviews 2009;23(1):62‐71. [PUBMED: 19056035] [DOI] [PubMed] [Google Scholar]
Sachs 2010
- Sachs UJ. Non‐infectious serious hazards in plasma transfusion. Transfusion and Apheresis Science 2010;43(3):381‐6. [PUBMED: 20934385] [DOI] [PubMed] [Google Scholar]
Sachs 2011
- Sachs UJ, Wasel W, Bayat B, Bohle RM, Hattar K, Berghöfer H, et al. Mechanism of transfusion‐related acute lung injury induced by HLA class II antibodies. Blood 2011;117(2):669‐77. [PUBMED: 21030555] [DOI] [PubMed] [Google Scholar]
Schulz 2010
- Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Medicine 2010;8:18. [PUBMED: 20334633] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shapiro 2004
- Shapiro MJ. To filter blood or universal leukoreduction: what is the answer?. Critical Care 2004;8 Suppl 2:S27‐30. [PUBMED: 15196319] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sterne 2011
- Sterne JAC, Egger M, Moher D (editors). Chapter 10: Addressing reporting biases. In: Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Tenorio 2007
- Tenorio GC, Gupte SC, Munker R. Transfusion Medicine and Immunohematology. In: Munker R, Hiller E, Glass J, Paquette R editor(s). Modern Hematology. 2nd Edition. Totowa, NJ: Humana Press Inc, 2007:401‐32. [ISBN‐13: 978‐1‐58829‐557‐6] [Google Scholar]
Theusinger 2009
- Theusinger OM, Spahn DR, Ganter MT. Transfusion in trauma: why and how should we change our current practice?. Current Opinion in Anaesthesiology 2009;22(2):305‐12. [PUBMED: 19390257] [DOI] [PubMed] [Google Scholar]
Thorlund 2011 [Computer program]
- Thorlund K, Engstrøm J, Wetterslev J, Brok J, Imberger G, Gluud C. User manual for trial sequential analysis (TSA). Version available from www.ctu.dk/tsa. Copenhagen, Denmark: Copenhagen Trial Unit: Centre for Clinical Intervention Research, 2011.
Tien 2007
- Tien H, Nascimento B Jr, Callum J, Rizoli S. An approach to transfusion and hemorrhage in trauma: current perspectives on restrictive transfusion strategies. Canadian Journal of Surgery 2007;50(3):202‐9. [PUBMED: 17568492] [PMC free article] [PubMed] [Google Scholar]
Tobian 2011
- Tobian AA, Savage WJ, Tisch DJ, Thoman S, King KE, Ness PM. Prevention of allergic transfusion reactions to platelets and red blood cells through plasma reduction. Transfusion 2011;51(8):1676‐83. [PUBMED: 21214585] [DOI] [PubMed] [Google Scholar]
Toy 2005
- Toy P, Popovsky MA, Abraham E, Ambruso DR, Holness LG, Kopko PM, et al. Transfusion‐related acute lung injury: definition and review. Critical Care Medicine 2005;33(4):721‐6. [PUBMED: 15818095] [DOI] [PubMed] [Google Scholar]
Triulzi 2009
- Triulzi DJ. Transfusion‐related acute lung injury: current concepts for the clinician. Anesthesia and Analgesia 2009;108(3):770‐6. [PUBMED: 19224781] [DOI] [PubMed] [Google Scholar]
Tsai 2010
- Tsai AG, Hofmann A, Cabrales P, Intaglietta M. Perfusion vs. oxygen delivery in transfusion with "fresh" and "old" red blood cells: the experimental evidence. Transfusion and Apheresis Science 2010;43(1):69‐78. [PUBMED: 20646963] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tsantes 2014
- Tsantes AE, Kyriakou E, Nikolopoulos GK, Stylos D, Sidhom M, Bonovas S, et al. Cost‐effectiveness of leucoreduction for prevention of febrile non‐haemolytic transfusion reactions. Blood Transfusion 2014;12(2):232‐7. [PUBMED: 24931843] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vamvakas 1996
- Vamvakas EC, Carven JH, Hibberd PL. Blood transfusion and infection after colorectal cancer surgery. Transfusion 1996;36(11‐12):1000‐8. [PUBMED: 8937412] [DOI] [PubMed] [Google Scholar]
Vamvakas 2001
- Vamvakas EC, Blajchman MA. Deleterious clinical effects of transfusion‐associated immunomodulation: fact or fiction?. Blood 2001;97(5):1180‐95. [PUBMED: 11222359] [DOI] [PubMed] [Google Scholar]
Vamvakas 2006
- Vamvakas EC. Deleterious clinical effects of allogenic blood tranfusion‐related immunomodulation. Facts or fiction? An update through 2005. American Journal of Clinical Pathology 2006;126(Suppl 1):S71‐85. [DOI: 10.1309/9B7RWAYVVLCL58WW] [DOI] [Google Scholar]
Vamvakas 2009
- Vamvakas EC, Blajchman MA. Transfusion‐related mortality: the ongoing risks of allogeneic blood transfusion and the available strategies for their prevention. Blood 2009;113(15):3406‐17. [PUBMED: 19188662 ] [DOI] [PubMed] [Google Scholar]
Wagner 2004
- Wagner SJ. Transfusion‐transmitted bacterial infection: risks, sources and interventions. Vox Sanguinis 2004;86(3):157‐63. [PUBMED: 15078249] [DOI] [PubMed] [Google Scholar]
Watkins 2008
- Watkins TR, Rubenfeld GD, Martin TR, Nester TA, Caldwell E, Billgren J, et al. Effects of leukoreduced blood on acute lung injury after trauma: a randomized controlled trial. Critical Care Medicine 2008;36(5):1493‐9. [PUBMED: 18434890] [DOI] [PubMed] [Google Scholar]
Wetterslev 2008
- Wetterslev J, Thorlund K, Brok J, Gluud C. Trial sequential analysis may establish when firm evidence is reached in cumulative meta‐analysis. Journal of Clinical Epidemiology 2008;61(1):64‐75. [PUBMED: 18083463] [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Simancas‐Racines 2012
- Simancas‐Racines D, Martí‐Carvajal AJ, Hidalgo R, Bangdiwala S. Leukoreduction for the prevention of adverse reactions from allogeneic blood transfusion. Cochrane Database of Systematic Reviews 2012, Issue 3. [DOI: 10.1002/14651858.CD009745] [DOI] [PMC free article] [PubMed] [Google Scholar]


