Abstract
Background
The use of point-of-care ultrasonography (POCUS) performed by general practitioners (GPs) in primary care settings is increasing. Previous studies have focused on GP-reported outcomes and little is known about patients’ perspectives on the use of POCUS technology within the general practice consultation. The purpose of this study was to examine patients’ experiences with POCUS in general practice within the areas where GPs have indicated that POCUS affected aspects of the consultation.
Methods
A questionnaire was developed using a mixed methods sequential design. Analytical themes from interviews with GPs were converted into items in a questionnaire by the research team. The questionnaire was then further developed in several rounds of pilot tests involving both patients and GPs. The final questionnaire was used in a cohort study conducted in 18 Danish office-based general practice clinics from January 2018 to August 2018. All patients examined with POCUS were asked to complete the questionnaire on tablets immediately after their consultation.
Results
Out of 691 patients examined, 564 (81.6%) questionnaires were available for analysis. The patients reported that they were well informed about the purpose (98%) and the results (97%) of the POCUS examination; however, 29% reported that they were not informed about the difference between POCUS and an imaging-specialist’s ultrasound examination. Almost all patients (99%) reported that POCUS was integrated naturally into the consultation, and 45% reported that POCUS improved the doctor-patient relationship.
The majority of patients felt that they had been more thoroughly examined (92%) and taken more seriously (58%) when POCUS was part of the consultation. They felt POCUS gave them a better understanding of their health problem (82%), made them feel more secure (86%) and increased their trust in the physician’s assessment (65%). Moreover, the patients reported that POCUS use improved the level of service (95%) they experienced and the quality of care (94%) in general practice.
Conclusion
We found that an examination including POCUS in general practice was a positive experience overall for the majority of patients. Future research should further explore reasons for patient confidence in POCUS and whether or not the reassuring value of POCUS is valid.
Trial registration
ClinicalTrials.gov Identifier: NCT03416608
Supplementary Information
The online version contains supplementary material available at 10.1186/s12875-021-01459-z.
Keywords: General practice, Family medicine, Primary care, Point-of-Care testing, Ultrasonography, Patient-reported outcome measures
Background
Evaluating patients’ perspectives is paramount when offering health care services [1]. For patients, both access to health care and quality of care are likely to be priorities [2]. Access to tools and tests in primary care that would traditionally only be available at hospitals may improve diagnostic capability at the front line, and could be seen by patients as an improvement in the provision of health care service overall. There is a risk, however, that a reallocation of resources and priorities may lead to maldistribution of medical resources resulting in a poorer health care service [3].
General practitioners (GPs) are increasingly using point-of-care ultrasound (POCUS) in their examination of selected patients [4–6]. Patients may regard diagnostic POCUS as an improved service to ensure earlier and more correct diagnosis and treatment. However, evidence for such positive effects from POCUS largely originates from hospital settings while the evidence from a general practice setting is scant [7–10]. As the epidemiology, presentation and spectrum of symptoms, pathology and diseases differ between primary and secondary care, the performance of a test will inevitably differ between the two sectors [11]. Still, a growing number of publications describe the use of POCUS within family medicine or office-based general practice [10, 12]. There are few studies describing essential long-terms outcomes i.e. diagnostic test accuracy including overdiagnosis, mortality, morbidity and health economics. Very few studies have explored the potential intended benefits and the potential unintended harms of POCUS use in general practice from the patient’s perspective, or the patient’s reaction to the introduction of POCUS technology in general practice [13–17].
In emergency medicine, POCUS has been reported to increase patient satisfaction [18, 19], but patient satisfaction is complex, difficult to measure as a single concept and several confounders need to be considered [20]. In general practice, patients usually seek care for less acute conditions than in emergency medicine. The general practice consultation is characterised by an emphasis on communication, continuity of care and a strong doctor-patient relationship [1, 21]. Introducing a time-consuming diagnostic test, like POCUS, may disturb the structure of the consultation and give less room for dialogue and the patient’s agenda. Indeed, one study from general practice in Norway [13] found that 29% of patients felt that GPs were putting too much emphasis on technology in the consultation, and 19% found that the ultrasound examination disturbed the doctor-patient relationship. In other settings, POCUS has been found to increase the physician’s confidence and the patient’s satisfaction with the physician’s skills and abilities [19]. Whether this finding also applies to office-based general practice has not yet been investigated.
We have previously explored GPs’ perspectives on the use of POCUS in an interview study [22]. According to the GPs, patients appreciated the use of POCUS and the reassurance it provided for them. They felt POCUS use improved the doctor-patient relationship, increased patient confidence and respect for the GP. However, the GPs also expressed concerns about patients’ trust in the technology and in their own ability to communicate the limitations of POCUS use in general practice. These findings highlighted the need to assess patients’ perspectives on the use of POCUS in the general practice consultation.
In the present study, we aimed to explore patients’ experiences with POCUS use in general practice within the areas where GPs indicated in a previous study [22] that POCUS had affected aspects of the consultation. Specifically, we aimed to explore the POCUS-related information provided to the patient, the influence of POCUS on the consultation, patient reassurance and patient satisfaction.
Methods
This cross-sectional study was developed using a mixed-method explorative sequential design [23]. Qualitative data collected in an interview study exploring the POCUS experiences of Danish GPs [22] was used to develop a quantitative patient questionnaire used in a cohort study measuring the use of POCUS in Danish general practice [24]. The protocol was prospectively registered in clinical trials (registration number: NCT03416608 10/01/2018) and reporting followed the STROBE checklist for cross-sectional studies.
Setting
This study was conducted in Danish, office-based general practices, where GPs were already using POCUS [24]. Denmark has a public health care system where patients are listed with a GP for primary health care. GPs act as gatekeepers to other treatment options in primary care and to secondary healthcare through a referral system. Consultations are free of change for patients, as GPs are paid through tax-financed remuneration and fee-for service [25]. Only a few Danish GPs perform POCUS and they receive no fee for the service.
Participants and recruitment
Twenty GPs working in 18 general practices were enrolled stepwise between January 15th 2018 and August 15th 2018 to account for seasonal variation. During a full month within the timeframe, each participating GP invited all patients, who had been examined with POCUS in the practice, to participated in this study. The general practice clinics were solo-practices and partnership-practices of different sizes and were located in both urban and rural areas. The participating GPs had different POCUS training and background characteristics which have been reported previously [24]. To be included in the study, patients had to be listed with the GP and be able to provide informed consent. In case of children, one or both parents had to provide informed consent depending on their custody arrangements.
Data collection
There was no experimental intervention in this study as the GPs were already using POCUS in their examination of patients. The POCUS examinations performed reflected normal daily practice in the included clinics, and apart from project information and data collections, the study did not influence patient assessment and treatment. POCUS was used for both diagnostic and procure-related purposes. A variety of different organs were scanned including heart, lung, abdominal, gynaecological, obstetric and musculoskeletal examinations [24].
After the consultation, patients examined with POCUS were asked to complete a questionnaire using tablets provided by the project. The GPs accessed the online questionnaire on the tablets using a SurveyXact (Rambøll, Aarhus, Denmark) app, and inserted a unique de-identifier number for each patient before handing over the tablet to the patient. The patients completed the questionnaire in the waiting room of the clinic and data were transferred directly to the SurveyXact database. A paper edition of the questionnaire was available for patients who felt uncomfortable using a tablet. The GPs had no access to the completed patient questionnaires.
In a separate questionnaire, GPs registered data on the examined patients using the same de-identifier numbers. The main results of this registration have been reported previously [24]. For the present study, we included the GPs’ registration of their confidence in their main tentative diagnosis after using POCUS.
Developing the questionnaire
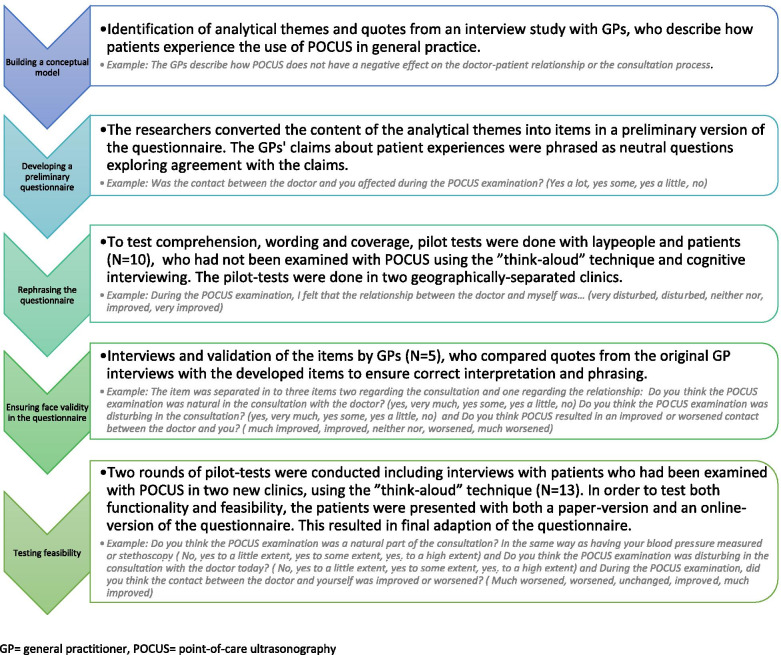
The items in the patient questionnaire were developed using mixed method integration. A preceding interview study with 13 Danish GPs who used POCUS in their daily practice [22] had identified the following themes regarding the patient experience: (1) Information given to the patient; POCUS influence on (2) the consultation, (3) patient reassurance, and (4) patient satisfaction. The research group converted the analytical text and quotes within each domain into items in a preliminary version of the questionnaire, which was then tested and further developed by involving both patients and GPs as elaborated in Fig. 1. The development of the GP questionnaire has been reported previously [24].
Fig. 1.
Developing the questionnaire. GP = general practitioner, POCUS = point-of-care ultrasonography
Outcome measures
The patients were asked to provide the following background characteristics: age, gender, current employment, level of education and whether they had been examined with ultrasonography previously.
Furthermore, they were asked if they had received information about: (1) the purpose of the examination; (2) the result of the examination, and (3) information about the difference between a specialist’s ultrasound examination and a GP’s ultrasound examination.
Regarding the influence of POCUS on the consultation, patients were asked if they felt POCUS was: (1) a natural part of the consultation or (2) disruptive to the consultation process. The patients were also asked: (3) whether POCUS had affected the doctor-patient relationship and (4) whether they believed POCUS had made a difference to the treatment they received.
Dimensions of patient reassurance were explored by asking the patients if the use of POCUS had: (1) made them feel more or less thoroughly examined; (2) given them a better or poorer understanding of their health problem; (3) made them feel more or less secure; (4) increased or decreased their confidence in the GP’s assessment of their health problem, and (5) made them feel more or less taken seriously.
Dimensions of patient satisfaction were assessed by asking the patients if they felt the use of POCUS had increased or decreased: (1) the level of service, or (2) the overall quality of care. Patients were also asked to: (3) evaluate their overall experience with POCUS as either positive or negative, and to (4) declare if they were likely to recommend POCUS to other patients with the same health problem. The full patient questionnaire is available in Additional file 1.
In the GP questionnaire, the GP’s confidence in their main tentative diagnosis for the patient was registered after POCUS as either highly increased, increased, unchanged, decreased, or highly decreased confidence.
Sample size
This was a first descriptive study, hence, no specific sample size calculation was made. Based on a previous questionnaire study from 2016 [4], we estimated that around 75 Danish GPs were using POCUS at the time of the study. We believed that we would be able to recruit 20 of these to participate in the study. Based on the interview study [22], we estimated that GPs would use POCUS 2–3 times a day, and assuming a participation rate of 80%, we expected to include a total of 640–960 patients.
Statistics
Data were collected using single-choice items with categorical response categories collected on nominal or assumed ordinal scales. Therefore, the results were reported using frequencies. Associations between the GPs’ reported confidence in the tentative diagnosis on an ordinal scale from highly decreased confidence to highly increased confidence, and the dimensions of patient’s reassurance was tested using Goodman and Kruskal’s gamma. Fischers exact test was used to test if the found frequencies statistically differed from the expected frequencies. A test probability of less than 0.05 was considered statistically significant.
Results
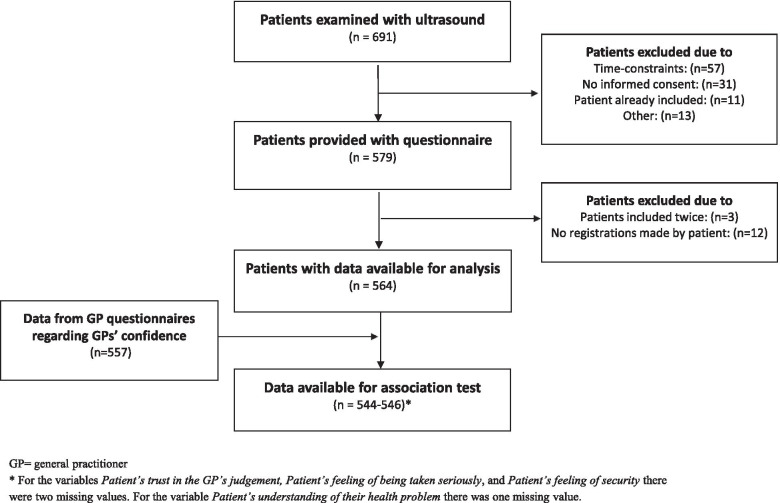
A total of 691 patients were examined with POCUS corresponding to an individual average daily use per GP between 0.6 and 3.9 ultrasound examinations. Patient questionnaires from 564 patients were available for analysis (Fig. 2). Background characteristics of participating patients are presented in Table 1.
Fig. 2.
Patients included in the study. GP = general practitioner. * For the variables Patient’s trust in the GP’s judgement, Patient’s feeling of being taken seriously, and Patient’s feeling of security there were two missing values. For the variable Patient’s understanding of their health problem there was one missing value
Table 1.
Patient characteristics
| Patient characteristics(N = 564) | N (%) |
|---|---|
| Agea | |
| < 20 years | 13 (2) |
| 20–39 years | 164 (29) |
| 40–59 years | 199 (35) |
| 60–79 years | 157 (28) |
| > 79 years | 29 (5) |
| Gendera | |
| Male | 186 (33) |
| Female | 376 (67) |
| Employment | |
| Currently working | 308 (55) |
| Unemployed | 15 (3) |
| Currently a student | 44 (8) |
| Retired | 160 (28) |
| Other | 33 (6) |
| Level of education after primary school | |
| Short specialized trainingb | 6 (1) |
| Trade/technical/vocational trainingb | 126 (22) |
| Short education (corresponding to an Associate’s degree) | 67 (12) |
| Medium education (corresponding to a Bachelor’s degree) | 159 ( 28) |
| Longer education (corresponding to a Master’s degree) | 61 (11) |
| Other education | 68 (12) |
| Currently a student | 25 ( 4) |
| Do not know | 39 (7) |
| Place of residence | |
| Capital Region of Denmark | 145 (26) |
| Region Zealand | 25 (4) |
| Region of Southern Denmark | 190 (34) |
| Central Denmark Region | 99 (18) |
| North Denmark Region | 105 (19) |
POCUS Point-of-care ultrasonography
aIn comparison missing patients had a mean age of 46 years and were 50% male
b No high-school requirement
Information given to the patient
Ninety-eight percent of patient participants reported that they felt very informed (N = 488) or informed to some extent (N = 65) about the purpose of the POCUS examination, whereas fewer than 2% felt informed to a lesser extent (N = 9) or not informed (N = 1). Ninety-seven percent reported that they had been informed about the result of the POCUS examination (very informed: N = 456; informed to some extent: N = 81 or to a lesser extent: N = 20), and only 1% reported that they were not informed about the results of the ultrasound examination (N = 5).
Regarding information about the difference between a POCUS examination performed by a GP in primary care and a specialist’s examination in the secondary sector, patients reported that they had been: very informed: 28% (N = 158); informed to some extent: 27% (N = 150); informed to a lesser extent:16% (N = 88), or not informed about this difference: 29% (N = 165).
POCUS influence on the consultation
Ninety-nine percent of patients reported that POCUS was integrated as a natural part of the GP consultation (to a high extent: N = 471; to some extent: N = 75; to a lesser extent: N = 13). Ninety-six percent reported that POCUS was not disruptive in the consultation, while the remaining 4% said that POCUS was disruptive (to a high extent: N = 7; to some extent: N = 4, or to a lesser extent: N = 4).
Fifty-five percent (N = 310) reported that POCUS did not affect the doctor-patient relationship, whereas 45% reported that they felt the doctor-patient relationship was very much improved (N = 105) or improved (N = 146) by POCUS. Only one patient reported that POCUS made the relationship worse.
POCUS influence on patients’ sense of reassurance
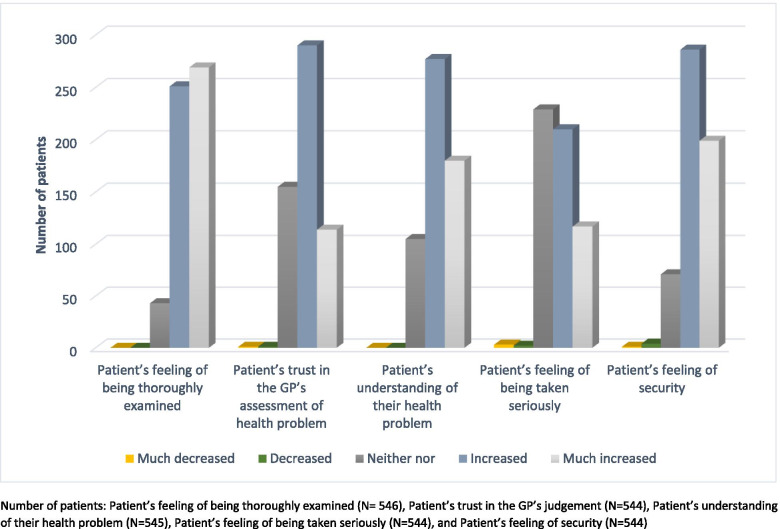
As illustrated in Fig. 3, 92% of patients reported that they felt much more thoroughly (N = 269) or more thoroughly (N = 251) examined after POCUS, while the remaining patients reported that POCUS had no influence in that regard (N = 43). Notably, no patients reported that POCUS made them feel less thoroughly examined.
Fig. 3.
Dimensions of patient reassurance measured in the questionnaire. Number of patients: Patient’s feeling of being thoroughly examined (N = 546), Patient’s trust in the GP’s judgement (N = 544), Patient’s understanding of their health problem (N = 545), Patient’s feeling of being taken seriously (N = 544), and Patient’s feeling of security (N = 544)
Eighty-one percent reported that POCUS had provided them with a much better (N = 180) or better (N = 277) understanding of their health problem, while 19% reported that POCUS had not changed their understanding (N = 105). No patients reported that POCUS had given them a poorer understanding.
Eighty-six percent reported that POCUS had made them feel much more secure (N = 199) or more secure (N = 286), while 13% (N = 71) felt POCUS had made no change in that regard and 1% felt POCUS had made them feel much less secure (N = 1) or less secure (N = 4).
Sixty-five percent reported that their trust in the GP’s assessment of their health problem was much increased (N = 114) or increased (N = 290) after POCUS; 27% (N = 155) reported that their trust had not changed, and fewer than 1% reported that their trust had decreased (N = 2).
Fifty-eight percent reported that the use of POCUS had made them feel that they had been taken much more seriously (N = 117) or more seriously (N = 210); 41% reported that POCUS had made no change in that regard, while 1% reported that they felt they had been taken much less seriously (N = 3) or less seriously (N = 2).
Improved care
Eighty percent of patients reported that they believed POCUS had a very large influence (N = 129) or a large influence (N = 320) on the care that they received at the GP’s office, and 5% reported that POCUS had very little influence (N = 2) or little influence (N = 24) on the care that they had received. Fifteen percent reported no difference (N = 87).
In more general terms, 95% of patients reported that POCUS very much improved (N = 287) or improved (N = 253) the service at the GP’s office, while 4% reported no difference. Ninety-four percent reported that POCUS very much improved (N = 250) or improved (N = 278) the quality of care in general practice while 4% reported no difference. Notably, no patients found that POCUS decreased service or quality of care in general practice.
Overall patient experience
Ninety-six percent of patients reported that they had a very positive (N = 334) or positive (N = 220) experience of being examined using POCUS at the GP’s office. The remaining eight patients reported that the experience had been neither positive nor negative. Hence, no patients reported having a negative overall experience.
Ninety-two percent reported that they would most likely (N = 351) or likely (N = 169) recommend the POCUS examination to others; 7% reported that they would neither recommend nor discourage the examination, and one patient reported that it was most unlikely that they would recommend the examination to others.
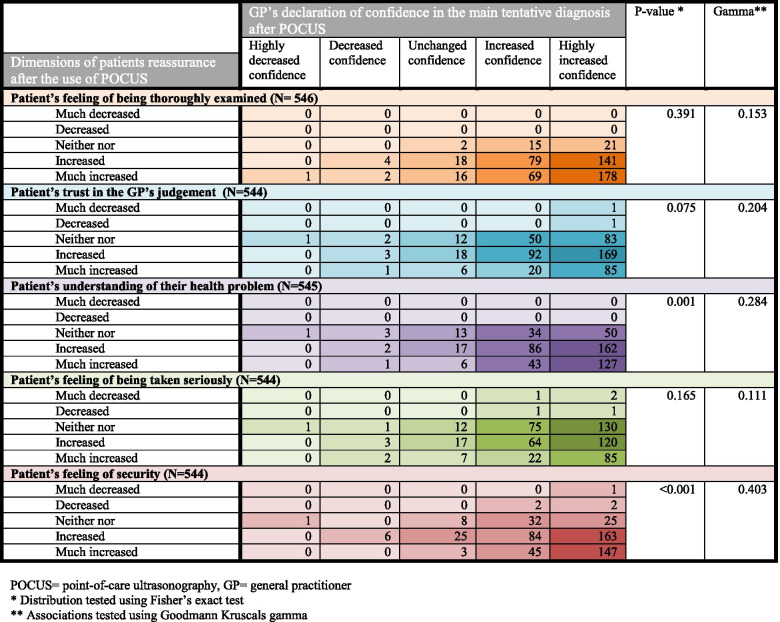
Association between patient reassurance and GP confidence
As illustrated in Fig. 4, the distribution of data was unidirectional. However, we found no strong associations between the GPs’ confidence in the main diagnosis and the dimensions of patient reassurance. A relationship beyond chance was found between the GPs’ confidence in the main diagnosis after POCUS and the patient’s declaration of increased understanding of their health problem, and the patient’s sense of security.
Fig. 4.
Associations between patient reassurance and general practitioners’ confidence in diagnosis. POCUS = point-of-care ultrasonography, GP = general practitioner. * Distribution tested using Fisher’s exact test. ** Associations tested using Goodmann Kruscals gamma
Discussion
Summary of main findings
In this study, we found that most patients felt they were well informed about the purpose and the results of the POCUS examinations. However, only half of the patients felt very informed or informed to some extent about the difference between a GP POCUS and an imaging-specialist’s ultrasound examination. Almost all (99%) patients reported that POCUS was integrated naturally into the GP consultation and 45% reported that POCUS may even have improved the doctor-patient relationship.
POCUS use had a large influence on patient reassurance: 92% felt more thoroughly examined, 85% felt they had been taken more seriously, and 86% felt more secure after being examined using POCUS. Eighty-eight percent reported an increased understanding of their health problem and 65% had an increased trust in the GP’s assessment of their health problem after the use of POCUS. Although we found that the majority of GPs reported an increased confidence in their diagnosis after POCUS, no strong association was found between the GPs’ increased confidence and the patients’ sense of reassurance.
Finally, we found that the vast majority of patients said that POCUS use improved their experience of the level of service and quality of care in general practice, and no patients reported having a negative experience with the use of POCUS in general practice.
Strengths and limitations
The questionnaire was developed based on extensive preceding qualitative work. However, the items originated from interviews with GPs and not patients. Hence, it is possible that interviews with patients preceding this study would have revealed aspects of the patient experience that we did not include. Nevertheless, all dimensions of the items in the questionnaire were pilot-tested with patients giving some assurance that they were relevant to patient experience.
Although, we had a 97% participation rate, we had expected to include more patients. The participating GPs reported that the study registrations were time consuming and, therefore, fewer patients were examined with POCUS during the study period. A larger sample may have provided more diversity in the results.
Generalisability may have been compromised as the GPs performing POCUS in this study are likely to constitute a selected sub-group of GPs with a special interest in ultrasonography. These GPs choose to use POCUS in their daily work without receiving a fee or remuneration for the extra service or their time. It is possible that the GPs’ enthusiasm for the technology affected the consultations and created a more positive atmosphere, which may have influenced patients’ experiences. Hence, it is unknown if similar results would be found in a larger or more diverse group of GPs.
To avoid recall bias, patients completed the questionnaires in the clinic’s waiting room immediately after their consultation, but this may have affected their responses. The high response rate could reflect the inability of some patients to say ‘no’ to participation, as the questionnaire was presented to them by the GP. Hence, we cannot reject some potential response bias where patients’ answers are in favour of their GPs.
This was a first descriptive study examining patient experiences with the use of POCUS in general practice, and as such we did not adjust for possible confounders. However, the distribution of data was strongly unidirectional. The lack of a comparator in our study design makes us unable to determine whether our findings are, in fact, a result of the use of POCUS or a more general expression of loyalty, trust and satisfaction with the GP. However, the phrasing of the questions was specifically designed to elicit the impact of POCUS.
Findings in context
Despite a growing number of publications describing the use of POCUS in general practice, little attention has been given to patients’ perspectives on the use of the technology [12]. Previous studies have explored patient experiences with POCUS in general practice using questionnaires administered immediately after the consultation [16], after 15 to 30 days [15], and after three [13] or four [17] months following the examination. Although using various designs and items to measure patients’ experiences, all studies reported that POCUS aligned well with patient preferences.
Accordingly, we found an overall positive experience with the GPs’ use of POCUS assessed immediately after the consultation. Three previous studies from general practice found that patients preferred having the examination performed at the GP’s office rather than going to the hospital [15–17]. Using discrete-choice methodology, one of the studies from a rural general practice [16] even found that patients were willing to trade off diagnostic accuracy to have the examination performed locally at the GP’s office. Hence, the high patient satisfaction reported in the present study may be explained merely by the availability of the test and patient expectations that the GP will take an active diagnostic approach in the consultation [26–29]. However, a POCUS examination is not a replacement for the traditional comprehensive ultrasound examination performed by an imaging-specialist [30, 31]. POCUS examinations are typically restricted to ruling in or ruling out a specific condition e.g. the presence or absence of a gallbladder stone, without exploring the surrounding areas. The premise for POCUS is that it is an abbreviated procedure, acceptable for the purpose. POCUS is superior to traditional ultrasound examinations in terms of accessibility, speed and availability, but it is inferior in terms of range and its ability to rule out disease [30]. Awareness of the limitations and communicating the differences between the two examinations is important to avoid false expectations about what the examinations can provide. We found that not all patients reported having received such information. This might confirm the findings from the preceding qualitative study [22], where GPs reported that, despite informing patients about the limitations of POCUS, they felt unsure about whether patients understood the differences between a specialist’s and a generalist’s examination. A perception gap between the information provided and the patients’ understanding of the information has been found regarding other tests too [32].
The GPs in our study all used POCUS on a weekly basis. However, their training and usage varied a lot, resulting in different competence levels [33]. Our study did not compare how this might have affected the patients’ perceptions of trust and confidence in the examination. Another possible explanation for high patient satisfaction with POCUS use is the reliance on diagnostic tests. Patients have been found to appreciate the use of point-of-care tests in general practice [27] and to put a lot of emphasis on diagnostic tests [26, 34, 35]without necessarily understanding their limitations, pitfalls and the potential unintended harms [34]. Studies have found that for some diseases reliance on the traditional physical examination of patients is questionable [36, 37]and patients, as well as doctors, may be aware of this. The mere availability of a diagnostic test may lead to wish-fulfilling medicine, where diagnostic examinations are performed upon patient request to meet patient expectations or to provide reassurance [38]. GPs undertaking POCUS must be aware of this risk and communicate their medical reasoning to patients. However, providing reassurance for patients is both important and common in general practice [39] and GPs have been found to use diagnostic tests to reassure themselves and patients [35, 40]. Measuring dimensions of reassurance immediately after the consultation, we found that patients felt an increased trust in their GP and a sense of security. However, studies have suggested that the immediate reassuring value of pregnancy-related ultrasound is not long-lasting [34, 41]and evidence does not support long-term reassurance by diagnostic tests [42, 43].
The diagnostic accuracy of a test and the pre-test probability of a condition have to be taken into account before GPs and patients can actually be assured that a diagnostic test (including POCUS) can, with reasonable certainty, rule in or rule out a condition [45]. GPs performing POCUS must be aware of this and the potential false reassurance that having a POCUS examination may provide for patients and themselves. Likewise, GPs must consider the risk of overdiagnosis, overdetection and possibly overtreatment following the introduction of an additional test [12, 45, 46]. Hence, GPs must continue to practice generalist medicine up to a certain level before handing the patient over to secondary care, informing patients about the limitations and risks of point-of-care examinations and referring patients to imaging specialists in case of doubt.
Implications
The increasing pressure on general practice in terms of more elderly and multi-morbid patients and more treatments transferred to primary care calls for faster and more precise diagnoses at the GP’s office. POCUS may be a valuable tool in this respect, but prudence must be exercised to ensure the quality of the examinations performed by GPs and the correct allocation of health care resources. The availability of high-resolution, affordable and portable ultrasound devices, together with the introduction of POCUS training in medical schools [47, 48] and residency programmes [49], makes it plausible that POCUS will be more commonly used in general practice in the future. This study suggests that patients appreciate POCUS use in general practice, however, a thorough evaluation of POCUS use should include an evaluation of experience of care, population prognoses and health and cost of care [50]. Although recent studies describing the use of focused POCUS in general practice have reported promising results [12], more high-quality research is needed to evaluate the diagnostic precision and impact of POCUS use in general practice including the patients’ prognoses and the impact on the health care sector as a whole.
Conclusion
We found that being examined with POCUS by GPs in general practice was a positive experience overall for the majority of patients. They felt that POCUS was integrated as a natural part of the consultation and most patients felt reassured after the POCUS examination. More than nine out of ten patients reported that POCUS increased the perception of level of service and quality of care in general practice. Generally, patients reported that they were well informed about why they needed the POCUS examination and the results, but almost half of patients felt ill-informed about the differences between POCUS in general practice and an imaging specialist’s ultrasound examination.
Supplementary Information
Acknowledgements
The authors would like to thank the participating GPs and patients for their individual contributions and the Danish Society for Ultrasound in General Practice (DAUS) for non-financial support of the study.
Abbreviations
- GP
General Practitioner
- POCUS
Point-of-care ultrasonography
Authors' contributions
CAA, JB, TRR and MBJ all helped design and develop the questionnaire. CAA, JB and TRR conducted the pilot tests. CAA and MBJ analysed the data and drafted the first version of the manuscript. All authors contributed significantly to the revision of the manuscript and agreed on the final version for submission to BMC Family Practice.
Funding
This study was conducted as an independent research project funded by The Danish Research Foundation for General Practice.
Availability of data and materials
The anonymised questionnaires and datasets are available and stored at Center for General practice at Aalborg University, Denmark according to regulations by the Danish Data Protection Agency. Anonymised data are available on request by contacting the corresponding author.
Declarations
Ethics approval and consent to participate
All patients and GPs provided written consent to participate in the study. All study data were pseudo-anonymised using a de-identifier number and the investigators were blinded to the identity of participating patients. In addition, the GPs were blinded to the results, as they could not access the completed patient questionnaires on the tablets. The study was conducted in accordance with the ethical principles for medical research described in the declaration of Helsinki. The study was approved by the Danish data protection agency (reference number 2017–41-5273) and the Committee of Multipractice Studies in General Practice (MPU-20–2016). The study was also notified to the Regional Committee on Health Research Ethics, who responded that approval was not needed according to Danish legislation.
Consent for publication
All participating GPs and patients have provided their written consent for participation in the study and for the publication of the results.
Competing interests
The authors have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Camilla Aakjær Andersen, Email: caakjaer@dcm.aau.dk.
John Brodersen, Email: john.brodersen@sund.ku.dk.
Torsten Rahbek Rudbæk, Email: trahbek@hotmail.com.
Martin Bach Jensen, Email: mbj@dcm.aau.dk.
References
- 1.Kebede S. Ask patients “What matters to you?” rather than “What’s the matter?”. BMJ. 2016;354:i4045. doi: 10.1136/bmj.i4045. [DOI] [PubMed] [Google Scholar]
- 2.Neil Rao N, Foo L, Sutaria S. Revisiting the access imperative. May 15, 2018. Available from: https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/revisiting-the-access-imperative#. Accessed 26 June 2020
- 3.Hart JT. The Inverse Care Law. Lancet. 1971;297(7696):405–412. doi: 10.1016/S0140-6736(71)92410-X. [DOI] [PubMed] [Google Scholar]
- 4.Andersen CA, Jensen MBB, Toftegaard BS, Vedsted P, Harris M, Group ÖR Primary care physicians’ access to in-house ultrasound examinations across Europe: a questionnaire study. BMJ Open. 2019;9(9):e030958. doi: 10.1136/bmjopen-2019-030958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bornemann P, Jayasekera N, Bergman K, et al. Point-of-care ultrasound: Coming soon to primary care? J Fam Pract. 2018;67(2):70–80. [PubMed]
- 6.Myklestul HC, Skonnord T, Brekke M. Point-of-care ultrasound (POCUS) in Norwegian general practice. Scand J Prim Health Care. 2020;21:1–7. doi: 10.1080/02813432.2020.1753385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Via G, Hussain A, Wells M, et al. International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr. 2014;27(7):683.e1–683.e33. doi: 10.1016/j.echo.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 8.Volpicelli G, Elbarbary M, Blaivas M, et al. International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38(4):577–591. doi: 10.1007/s00134-012-2513-4. [DOI] [PubMed] [Google Scholar]
- 9.Olgers TJ, Azizi N, Blans MJ, et al. Point-of-care ultrasound (PoCUS) for the internist in acute medicine: a uniform curriculum. Neth J Med. 2019;77(5):168–176. [PubMed] [Google Scholar]
- 10.Sorensen B, Hunskaar S. Point-of-care ultrasound in primary care: A systematic review of generalist performed point-of-care ultrasound in unselected populations. Ultrasound J. 2019;11(1):31. doi: 10.1186/s13089-019-0145-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Guyatt G, et al. Users' Guides to the Medical Literature: A Manual for Evidence-Based Clinical Practice. New York: McGraw-Hill Professional; 2015. [Google Scholar]
- 12.Andersen CA, Holden S, Vela J, et al. Point-of-care ultrasound in general practice: A systematic review. Ann Fam Med. 2019;17:61–69. doi: 10.1370/afm.2330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glaso M, Medias IB, Straand J. Diagnostic ultrasound in general practice. Tidsskr Nor Laegeforen. 2007;127(15):1924–1927. [PubMed] [Google Scholar]
- 14.Rosenthal TC, Siepel T, Zubler J, et al. The use of ultrasonography to scan the abdomen of patients presenting for routine physical examinations. J Fam Pract. 1994;38(4):380–385. [PubMed] [Google Scholar]
- 15.Pertierra-Galindo N, Salvo-Donangelo L, Salcedo-Joven MI, Roman-Crespo B, Torres F. Study of patient satisfaction when performing an ultrasound in primary care. SEMERGEN. 2019;45(4):239–250. doi: 10.1016/j.semerg.2018.08.007. [DOI] [PubMed] [Google Scholar]
- 16.Wordsworth S, Scott A. Ultrasound scanning by general practitioners: Is it worthwhile? J Public Health Med. 2002;24(2):88–94. doi: 10.1093/pubmed/24.2.88. [DOI] [PubMed] [Google Scholar]
- 17.Eggebo TM, Sorvang S, Dalaker K. Ultrasonic diagnosis of the upper abdomen performed in general practice. Tidsskr Nor Laegeforen. 1990;110(9):1096–1098. [PubMed] [Google Scholar]
- 18.Lindelius A, Törngren S, Nilsson L, et al. Randomized clinical trial of bedside ultrasound among patients with abdominal pain in the emergency department: Impact on patient satisfaction and health care consumption. Scand J Trauma Resusc Emerg Med. 2009;17:60. doi: 10.1186/1757-7241-17-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Howard ZD, Noble VE, Marill KA, Sajad D, Rodrigues M, Bertyzzi B, LIteplo AS. Bedside ultrasound maximizes patient satisfaction. J Emerg Med. 2014;46(1):46–53. doi: 10.1016/j.jemermed.2013.05.044. [DOI] [PubMed] [Google Scholar]
- 20.Batbaatar E, Dorjdagva J, Luvsannyam A, Savino MM, Amenta P. Determinants of patient satisfaction: a systematic review. Perspect Public Health. 2017;137(2):89–101. doi: 10.1177/1757913916634136. [DOI] [PubMed] [Google Scholar]
- 21.Williams S, Weinman J, Dale J, Newman S. Patient expectations: What do primary care patients want from the GP and how far does the meeting expectations affect patient satisfaction? Fam Prac. 1995;12(2):193–201. doi: 10.1093/fampra/12.2.193. [DOI] [PubMed] [Google Scholar]
- 22.Andersen CA, Davidsen AS, Brodersen J, et al. Danish general practitioners have found their own way of using point-of-care ultrasonography in primary care: a qualitative study. BMC Fam Pract. 2019;20(1):89. doi: 10.1186/s12875-019-0984-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs-principles and practices. Health Serv Res. 2013;48:2134–2156. doi: 10.1111/1475-6773.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Andersen CA, Brodersen J, Davidsen AS, Graumann O, Jensen MB. Use and impact of point-of-care ultrasonography in general practice: a prospective observational study. BMJ Open. 2020;10(9):e037664. doi: 10.1136/bmjopen-2020-037664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pedersen KM, Andersen JS, Søndergaard J. General practice and primary health care in Denmark. J Am Board Fam Med. 2012;25(suppl 1):S34–S38. doi: 10.3122/jabfm.2012.02.110216. [DOI] [PubMed] [Google Scholar]
- 26.van Bokhoven MA, Pleunis-van Empel MCH, Koch H, Grol RPTM, Dinant G, van der Weijden T. Why do patients want to have their blood tested? A qualitative study of patient expectations in general practice. BMC Fam Prac. 2006;7:75. doi: 10.1186/1471-2296-7-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Laurence CO, Gialamas A, Bubner T, Yelland L, Willson L, Ryan P, Beilby J, Point-of-care Testing in General Practice Trial Management Group. Patient satisfaction with point-of-care testing in general practice. Br J Gen Pract. 2010;60(572):e98–104. 10.3399/bjgp10X483508. [DOI] [PMC free article] [PubMed]
- 28.Lauridsen GB, Sørensen MS, Hansen MP, Rathe JØ, Jarbøl DE. Consultation expectations among patients with respiratory tract infection symptoms. Dan Med J. 2017;64(6):A5385. [PubMed] [Google Scholar]
- 29.Kenten C, Bowling A, Lambert N, Howe A, Rowe G. A study of patient expectations in a Norfolk general practice. Health Expect. 2010;13:273–284. doi: 10.1111/j.1369-7625.2010.00603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Weile J, Brix J, Moellekaer AB. Is point-of-care ultrasound disruptive innovation? F0rmulating why POCUS is different from conventional comprehensive ultrasound. Crit Ultrasound J. 2018;10(1):25–33. doi: 10.1186/s13089-018-0106-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364(8):749–757. doi: 10.1056/NEJMra0909487. [DOI] [PubMed] [Google Scholar]
- 32.Petersen GB, Damhus CS, Jønsson ABR, Brodersen J. The perception gap: how the benefits and harms of cervical cancer screening are understood in information material focusing on informed choice. Health Risk Soc. 2020;22(2):177–196. doi: 10.1080/13698575.2020.1778645. [DOI] [Google Scholar]
- 33.Andersen CA, Hedegård HS, Løkkegaard T, Frølund J, Jensen MB. Education of general practitioners in the use of point-of-care ultrasonography: a systematic review. Fam Pract. 2020:cmaa140. doi: 10.1093/fampra/cmaa140. [DOI] [PubMed]
- 34.Roberts J, Griffiths FE, Verran A, Ayre C. Why do women seek ultrasound scans from commercial providers during pregnancy? Sociol Health Illn. 2015;37(4):594–609. doi: 10.1111/1467-9566.12218. [DOI] [PubMed] [Google Scholar]
- 35.van der Weijden T, van Bokhoven MA, Dinant G, et al. Understanding laboratory testing in diagnostic uncertainty: a qualitative study in general practice. Br J Gen Pract. 2002;52(485):974–980. [PMC free article] [PubMed] [Google Scholar]
- 36.Jauhar S. The demise of the physical exam. N Engl J Med. 2006;354(6):548–551. doi: 10.1056/NEJMp068013. [DOI] [PubMed] [Google Scholar]
- 37.Kugler J, Verghese A. The physical exam and other forms of fiction. J Gen Intern Med. 2010;25(8):756–757. doi: 10.1007/s11606-010-1400-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Asscher ECA, Bolt I, Schermer M. Wish-fulfilling medicine in practice: a qualitative study of physician arguments. J Med Ethics. 2012;38:327–331. doi: 10.1136/medethics-2011-100103. [DOI] [PubMed] [Google Scholar]
- 39.Giroldi E, Veldhuijzen W, Leijten C, Welter D, van der Weijden T, Muris J, van der Vleuten C. No need to worry: an exploration of general practitioners’ reassuring strategies. BMC Fam Prac. 2014;15:133. doi: 10.1186/1471-2296-15-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Michael-Corsten M, Donner-Banzhoff N. Beyond accuracy: hidden motives in diagnostic testing. Fam Prac. 2018;35(2):222–227. doi: 10.1093/fampra/cmx089. [DOI] [PubMed] [Google Scholar]
- 41.Thomas GM, Roberts J, Griffiths FE. Ultrasound as a technology of reassurance? How pregnant women and health care professionals articulate ultrasound reassurance and its limitations. Sociel Helath Illn. 2017;39(6):893–907. doi: 10.1111/1467-9566.12554. [DOI] [PubMed] [Google Scholar]
- 42.Rolfe A, Burton C. Reassurance after diagnostic testing with a low pretest probability of serious disease: Systematic review and meta-analysis. JAMA Intern Med. 2013;173(6):407–416. doi: 10.1001/jamainternmed.2013.2762. [DOI] [PubMed] [Google Scholar]
- 43.van Ravesteijn H, van Dijk I, Darmon D, et al. The reassuring value of diagnostic tests: a systematic review. Patient Educ Couns. 2012;86(1):3–8. doi: 10.1016/j.pec.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 44.Austin LC, Reventlow S, Sandøe P, et al. The structure of medical decisions: uncertainty, probability and risk in five common choice situations. Health Risk Soc. 2013;15(1):27–50. doi: 10.1080/13698575.2012.746286. [DOI] [Google Scholar]
- 45.Lumbreras B, Donat L, Hernández-Aguado I. Incidental findings in imaging diagnostic tests: a systematic review. Br J Radiol. 2010;83(988):276–289. doi: 10.1259/bjr/98067945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shabanzadeh DM, Sørensen LT, Jørgensen T. A prediction rule for risk stratification of incidentally discovered gallstones: results from a large cohort study. Gastroenterology. 2016;150:156–167. doi: 10.1053/j.gastro.2015.09.002. [DOI] [PubMed] [Google Scholar]
- 47.Baltarowich OH, Di Salvo DN, Scoutt LM, et al. National ultrasound curriculum for medical students. Ultrasound Q. 2014;30(1):13–19. doi: 10.1097/RUQ.0000000000000066. [DOI] [PubMed] [Google Scholar]
- 48.Dietrich CF, Hoffmann B, Abramowicz J, et al. Medical student ultrasound education: a WFUMB position paper, part I. Ultrasound Med Biol. 2019;45(2):271–281. doi: 10.1016/j.ultrasmedbio.2018.09.017. [DOI] [PubMed] [Google Scholar]
- 49.American Academy of Family Physicians (AAFP). AAFP recommended curriculum guidelines for family medicine residents point of care ultrasound. 2016; Available from: https://www.aafp.org/dam/AAFP/documents/medical_education_residency/program_directors/Reprint290D_POCUS.pdf. Accessed 7 May 2020
- 50.Berwick DM, Nolan TW, Whittington J. The triple aim: care, health and cost. Health Affairs. 2008;27(3):759–769. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The anonymised questionnaires and datasets are available and stored at Center for General practice at Aalborg University, Denmark according to regulations by the Danish Data Protection Agency. Anonymised data are available on request by contacting the corresponding author.