Abstract
Background
Talaromyces marneffei (T. marneffei) infection has been associated with adult-onset immunodeficiency due to anti-IFN-γ autoantibodies. We aimed to investigate the clinical features of non-HIV-infected patients with T. marneffei infection in southern China.
Methods
Between January 2018 and September 2020, we enrolled patients with T. marneffei infection who were HIV-negative (group TM, n = 42), including anti-IFN-γ autoantibody-positive (group TMP, n = 22) and anti-IFN-γ autoantibody-negative (group TMN, n = 20) patients and healthy controls (group HC, n = 40). Anti-IFN-γ autoantibodies were detected by ELISA. Clinical characteristics and clinical laboratory parameters were recorded.
Results
Compared with anti-IFN-γ autoantibody-negative patients with T. marneffei infection, anti-IFN-γ autoantibody-positive patients did not have underlying respiratory disease; more frequently exhibited dissemination of systemic infections with severe pleural effusion; had higher WBC counts, C-reactive protein levels, erythrocyte sedimentation rates, and neutrophil and CD8+ T cell counts; had lower hemoglobin levels; and were more likely to have other intracellular pathogen infections. Most of these patients had poor outcomes despite standardized antimicrobial therapy.
Conclusion
T. marneffei-infected patients with higher anti-IFN-γ autoantibody titers have more severe disease and complex clinical conditions.
Keywords: Anti-IFN-γ autoantibodies, Talaromyces marneffei, Clinical features, Clinical outcome
Introduction
Immune deficiency, which is caused by anti-interferon-γ autoantibodies (anti-IFN-γ autoAbs), is an adult immune deficiency syndrome that was first described among patients with mycobacterial infection [1]. Patients have high titers of serum anti-IFN-γ autoAbs, which can inhibit signal transducer and activator of transcription 1 (STAT1) phosphorylation and interleukin-12 production, resulting in severe dysfunction of the Th1 response [2–4] and increased risk of infection by multiple intracellular pathogens, including nontuberculous Mycobacterium (NTM), Talaromyces marneffei (T. marneffei), Cryptococcus neoformans, and other intracellular pathogens [1–12]. Talaromycosis is a severe deep mycosis that mainly involves organs rich in monocyte-macrophages (i.e., the lungs, liver, and lymph nodes) and can be categorized into localized and disseminated disease. Disseminated disease is characterized by severe systemic symptoms and a high mortality rate [13].
T. marneffei infection has long been associated with acquired immunodeficiency syndrome caused by human immunodeficiency virus (HIV) infection [14]. In some regions, such as southern China, T. marneffei infection has historically been the major opportunistic infection associated with acquired immunodeficiency syndrome [15]. However, T. marneffei infection has been increasingly reported among non-HIV-infected patients with impaired cell-mediated immunity [16], and immune deficiency syndrome caused by anti-IFN-γ autoAbs is an important risk factor [11, 12]. However, the impact of anti-IFN-γ autoAbs on talaromycosis progression has not been clearly described.
In this study, we compared the clinical features and laboratory findings between T. marneffei-infected patients with and without high titers of serum anti-IFN-γ autoAbs. We further evaluated the impact of anti-IFN-γ autoAbs on the dynamic disease course. Our findings provide more evidence for the diagnosis and treatment of non-HIV-infected patients with T. marneffei infection and will contribute to improved prognosis and a reduced mortality rate.
Methods
Participants
In this prospective, multicenter cohort study, patients with T. marneffei infection (group TM) were recruited between January 2018 and September 2020 from 7 academic centers [The First Affiliated Hospital of Guangzhou Medical University (Guangzhou); The Third Affiliated Hospital of Sun Yat-sen University (Guangzhou); The First Affiliated Hospital of Guangxi Medical University and The Affiliated Tumor Hospital of Guangxi Medical University (Nanning); The First Affiliated Hospital of Zhejiang University School of Medicine (Zhejiang); The Shengli Clinical Medical College of Fujian Medical University (Fuzhou) and The Eighth Affiliated Hospital of Sun Yat-Sen University (Shenzhen)]. The inclusion criteria were as follows: 1) No laboratory evidence of HIV infection; 2) Clinical and/or imaging manifestations of T. marneffei infection; 3) Microbiological or pathological findings identified from sputum, tracheal aspirate, bronchoalveolar lavage fluid (BALF), lung biopsy sample, pleural effusion, bone marrow smear, skin hydrolipidic film exudate or lymph node smear consistent with any of the following manifestations: a) visible detection of fungi (rounded or oval-shaped with an obvious transverse septum) by microscopy after Wright staining; b) isolation of pathogens from culture; or c) pathological examination revealing T. marneffei infection with pyogenic granulomatous changes, central necrosis, and massive monocyte-macrophage infiltration [17].
Healthy controls (group HC) with normal routine blood test findings and chest radiography were recruited from the health checkup center in The First Affiliated Hospital of Guangzhou Medical University.
Participants with anti-IFN-γ autoAb titers exceeding the 99th percentile of group HC were classified as anti-IFN-γ autoAb-positive. We further divided group TM into group TMP (anti-IFN-γ autoAb-positive) and group TMN (anti-IFN-γ autoAb-negative).
We excluded study participants who were less than 18 years of age; had autoimmune disease, cancer, or immunodeficiency; or had received immunosuppressive medications within the previous 3 months.
Clinical assessment
We measured the level of anti-IFN-γ autoAbs and recorded the clinical characteristics and laboratory findings upon admission. For healthy controls, we documented age, sex, and race or ethnicity only. Patients with T. marneffei infection (group TM) were followed up at weeks 1 and 2 and months 1, 3, 6, 9 and 12 after antifungal treatment; at follow-up, the levels of anti-IFN-γ autoAbs were detected, and the clinical conditions were recorded. The epidemiological and clinical characteristics, laboratory findings, treatment and outcome data were extracted into a standardized case report from the electronic medical records. The definition for each outcome was defined as follows: 1) ‘Cured’ were defined as patients’ symptoms and signs disappearing completely, with the lesions in the lung and other involved organs markedly or completely absorbed and the laboratory indexes related to infection normalized; 2) ‘Improved’ were defined as patients’ symptoms and signs improving, with no new signs or symptoms of lung or other organ infection appeared, the lesions in the lungs and other organs were absorbed or there was no obvious deterioration, and the laboratory indicators related to infection were improved; 3) ‘Ineffective’ were defined as patients’ symptoms and signs worsening, or new symptoms or signs of lung or other organ infection occurring, with progression or no improvement in the lesions in the lungs or other organs and worsening or lack of improvement in the laboratory parameters related to infection. 4) ‘Recurrence’ were defined as patients’ clinical symptoms improving or the pathogen detection being negative after effective treatment and then reappearing with signs of pathogen infection, pathogen detection being positive again, or both. 5) Death. If data were missing or clarification was needed, we then obtained the data by direct communication with the attending physicians and other health care providers. All case records were independently reviewed by two senior physicians (Z.M.C. and Y.L.).
Determination of anti-IFN-γ autoAb titers
Blood specimens were collected in 5 ml anticoagulant tubes. Serum was separated by centrifugation at 3000 rpm for 10 min and diluted 16-fold. The serum anti-IFN-γ autoAb titers were determined by using an enzyme-linked immunosorbant assay kit (USCN Life Science, Inc., Wuhan, China) based on the instructions of the manufacturer. The anti-IFN-γ autoAb titers were determined by comparing the optical density of the sample to the standard curve (detection range 3.12 ng/ml-200 ng/ml).
Statistical analysis
Data were analyzed using IBM SPSS Statistics for Windows, version 23 (SPSS Inc., Chicago, Illinois), and a P-value < 0.05 indicated statistical significance. Categorical data are presented as numbers and percentages, and continuous data are presented as medians and ranges or interquartile ranges (IQRs). Comparison of continuous data was performed using the Kruskal-Wallis test or Mann-Whitney test; Fisher’s exact test was used to compare categorical variables. Comparison of the levels of anti-IFN-γ autoAbs between each study group was performed using Student’s t-test, the F-test and analysis of variance. Analyses of the associations between anti-IFN-γ autoAb levels and factors of interest were carried out using linear correlation with the Pearson correlation coefficient. Associations between various possible risk factors and this clinical syndrome were calculated as odds ratios (ORs) and 95% confidence intervals (CIs). Independent risk factors were identified by binary logistic regression to adjust for possible risk factors, defined as variables with P < 0.05 in multivariable analysis.
Results
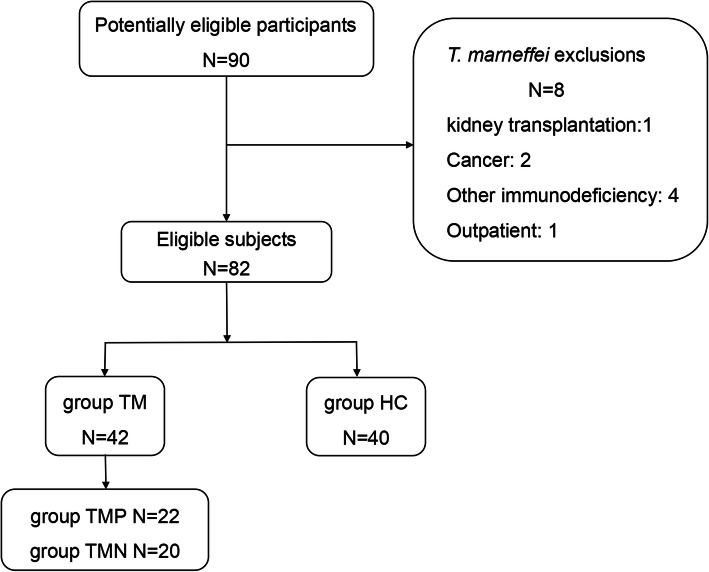
Of the 82 eligible participants, 42 had disseminated T. marneffei infection (group TM) and 40 were healthy controls (group HC). The enrollment flow chart is shown in Fig. 1.
Fig. 1.
Flow chart of patient recruitment. Group TM = Talaromyces marneffei. Group TMP = anti-IFN-γ autoantibody-positive group. Group TNN = anti-IFN-γ autoantibody-negative group
Baseline characteristics and anti-IFN-γ autoAb titers
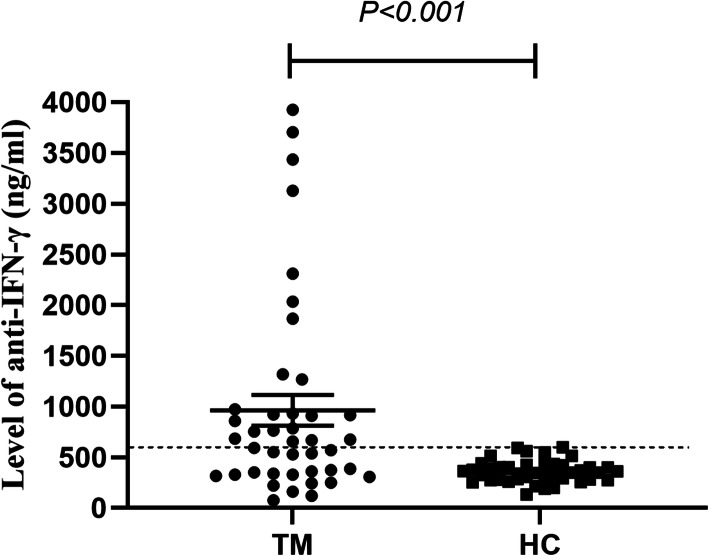
Sex distribution and age did not differ significantly between the two groups (Table 1). The anti-IFN-γ autoAb titers in group TM (median 661.33 ng/ml, range 334.88–941.29 ng/ml) were significantly higher than those in the healthy control group (median 353.97 ng/ml, range 277.40–422.38 ng/ml) (P < 0.001). Based on the 99th percentile of the anti-IFN-γ autoAb titers in group HC, the cutoff for anti-IFN-γ autoAb positivity was 594.49 ng/ml (Fig. 2). Twenty-two patients with T. marneffei infection were considered anti-IFN-γ autoAb-positive (group TMP) (Table 1).
Table 1.
Baseline characteristics of the participants
| Variable | Group TM (N = 42) | Group HC (N = 40) | P value |
|---|---|---|---|
| Age, years | 53 (33, 59) | 32 (27, 38) | 0.646 |
| Male sex, no. (%) | 27 (64.3%) | 18 (45.0%) | 0.094 |
| Anti-IFN-γ antibody-positive, no. (%) | 22 (52.4%) | 0 | 0.015 |
| Anti-IFN-γ antibody titer (ng/ml) | 661.33 (334.88, 941.29) | 353.97 (277.40, 422.38) | < 0.001 |
Fig. 2.
Levels of anti-IFN-γ autoAbs of atients with T. marneffei infection upon hospital admission and healthy controls. Each symbol represents an individual study participant. The dashed line indicates the estimated 99th percentile for the control group (group HC)
Comparison of clinical features between group TMP and group TMN
As shown in Table 2, no significant between-group differences were found when patients were stratified by age or sex. Significantly more patients with T. marneffei infection in group TMN than in group TMP had underlying respiratory disease (including chronic obstructive pulmonary disease, bronchiectasis and asthma) (P < 0.05). In addition to the lungs, the lymph nodes were the most common organs involved in both groups. Compared with patients in group TMN, patients in group TMP were more likely to have bone and skin involvement (P < 0.05). There were no significant between-group differences in the proportions of patients with fever, cough or sputum production, hemoptysis, dyspnea, chest pain, osteodynia or arthralgia, wasting, or moist rales. However, compared with patients in group TMN, patients in group TMP were more likely to develop pleural effusion (P < 0.05).
Table 2.
Comparison of clinical characteristics between group TMP and group TMN during the first visit
| Variable | Group TMP (N = 22) | Group TMN (N = 20) | P value |
|---|---|---|---|
| Age, years | 52.0 (34.8, 58.0) | 54.5 (29.0, 63.8) | 0.734 |
| Male sex, no. (%) | 14 (63.6%) | 13 (65.0%) | 1.0 |
| Anti-IFN-γ antibody titer (ng/ml) | 926.31 (760.02, 2103.20) | 332.40 (243.51,491.89) | <0.001 |
| Time from symptom onset to diagnosis | 149.5 (57.2, 272.3) | 98.5 (22.3154.5) | 0.107 |
| Coexisting respiratory disease, no. (%) | 3 (13.6%) | 10 (50.0%) | 0.019 |
| Bronchiolitis | 0 | 4 (20.0%) | 0.043 |
| COPD | 2 (9.1%) | 4 (20.0%) | 0.400 |
| COPD with bronchiectasis | 0 | 2 (10.0%) | 0.221 |
| Asthma | 1 (4.5%) | 0 | 0.476 |
| Extrapulmonary organ involvement, no. (%) | 18 (81.8%) | 11 (55.0%) | 0.096 |
| Skin | 10 (45.5%) | 3 (15.0%) | 0.047 |
| Lymph node | 18 (81.8%) | 11 (55.0%) | 0.096 |
| Liver | 2 (9.1%) | 1 (5.0%) | 1.000 |
| Spleen | 2 (9.1%) | 0 | 0.489 |
| Bone | 9 (40.9%) | 1 (5.0%) | 0.010 |
| Symptoms, no. (%) | |||
| Fever | 12 (54.5%) | 6 (30.0%) | 0.131 |
| Cough | 17 (77.3%) | 17 (85.0%) | 0.700 |
| Sputum production | 14 (63.6%) | 15 (75.0%) | 0.514 |
| Hemoptysis | 4 (18.2%) | 3 (15.0%) | 1.0 |
| Dyspnea | 6 (27.3%) | 3 (15%) | 0.460 |
| Chest pain | 9 (40.9%) | 6 (30.0%) | 0.531 |
| Osteodynia/Arthralgia | 7 (31.8%) | 3 (15.0%) | 0.284 |
| Wasting | 13 (59.0%) | 10 (50.0%) | 0.757 |
| Moist rales | 6 (27.3%) | 8 (40.0%) | 0.515 |
| Pleural effusion | 13 (59.1%) | 3 (15.0%) | 0.005 |
| Co-infection, no. (%) | 12 (55.0%) | 4 (20.0%) | 0.029 |
| Outcome, no. (%)a | |||
| Cured | 0 | 2 (10.0%) | – |
| Improved | 2 (9.1%) | 4 (20.0%) | – |
| Ineffective | 6 (27.3%) | 0 | – |
| Recurrence | 1 (4.5%) | 0 | – |
| Death | 3 (13.6%) | 0 | – |
aData were available for 12 patients in group TMP and 6 patients in group TMN during the longitudinal follow-up
Group TMP = anti-IFN-γ autoantibody-positive group
Group TMN = anti-IFN-γ autoantibody-negative group
COPD Chronic obstructive pulmonary disease
NTM Nontuberculous Mycobacterium
The laboratory findings are shown in Table 3. Patients in group TMP had markedly higher leukocyte counts, neutrophil counts, eosinophil counts, erythrocyte sedimentation rates and C-reactive protein levels and lower hemoglobin levels than patients in group TMN (P < 0.05). Immunoglobulin levels were available for 32 patients. Patients in group TMP were more likely to have higher IgG antibody levels than those in group TMN. T cell counts were available for 25 patients, with median CD3+ T cell and CD8+ T cell counts of 1425.0 cells/μl and 631.0 cells/μl, respectively, in group TMP. These counts were significantly higher than those in group TMN. Modest between-group differences were identified when patients were stratified by the percentage of neutrophils and the platelet count.
Table 3.
Comparison of laboratory findings between group TMP and group TMN during the first visit
| Variable | Group TMP (N = 22) | Group TMN (N = 20) | P value |
|---|---|---|---|
| White cell count (*109 cells/L) | 13.4 (9.3, 18.0) | 7.7 (5.8, 12.0) | 0.012 |
| Absolute neutrophil count (*109 cells/L) | 10.7 (6.9, 13.3) | 5.1 (3.6, 11.4) | 0.019 |
| Neutrophil ratio (neut %) | 0.76 (0.7, 0.9) | 0.7 (0.6, 0.8) | 0.120 |
| Eosinophil count (*109 cells/L) | 0.4 (0.1, 0.6) | 0.1 (0.1, 0.3) | 0.030 |
| Hemoglobin (g/L) | 89.7 (69.0,123.8) | 111.0 (93.8129.8) | 0.049 |
| Platelet count (*109 cells/L) | 310.5 (226.2485.7) | 312.0 (189.0,408.0) | 0.569 |
| Erythrocyte sedimentation rate (mm/h)a | 98.0 (72.0, 102.0) | 52.0 (15.9, 88.0) | 0.008 |
| C-reactive protein (mg/dL)b | 7.7 (3.3, 15.7) | 72.5 (14.9, 137.2) | 0.002 |
| Immunoglobulinc | |||
| Ig G (g/L) | 28.7 (17.5, 34.0) | 17.7 (13.7, 25.8) | 0.026 |
| Ig A (g/L) | 1.1 (0.8,1.5) | 1.2 (0.9,2.2) | 0.400 |
| Ig M (g/L) | 2.6 (1.5, 2.8) | 2.2 (1.5,2.9) | 0.880 |
| T cell countd | |||
| CD3+ T cell count (cells/μl) | 1425.0 (109.1, 1945.0) | 830.5 (355.51302.3) | 0.011 |
| CD4+ T cell count (cells/μl) | 685.0 (419.0, 965.5) | 433.0 (111.3844.5) | 0.247 |
| CD8+ T cell count (cells/μl) | 631.0 (499.0, 1132.0) | 333.5 (151.0, 467.0) | <0.001 |
aErythrocyte sedimentation rate data were missing for 8 patients (19%)
bC-reactive protein data were missing for 12 patients (28.5%)
cImmunoglobulin data were missing for 10 patients (23.8%)
dT cell count data were missing for 17 patients (40.5%)
Group TMP = anti-IFN-γ autoantibody-positive group
Group TMN = anti-IFN-γ autoantibody-negative group
Moreover, the white blood cell count and erythrocyte sedimentation rate correlated significantly with the levels of anti-IFN-γ autoAbs in group TM (Fig. 3A-B). In addition, there was an apparent correlation between neutrophils and anti-IFN-γ autoAbs. (Fig. 3C). Univariate logistic regression analysis of patients in group TM showed that underlying respiratory disease (P = 0.031) and pleural effusion (P = 0.018) were independent factors associated with the appearance of anti-IFN-γ autoAb positivity (Table 4).
Fig. 3.
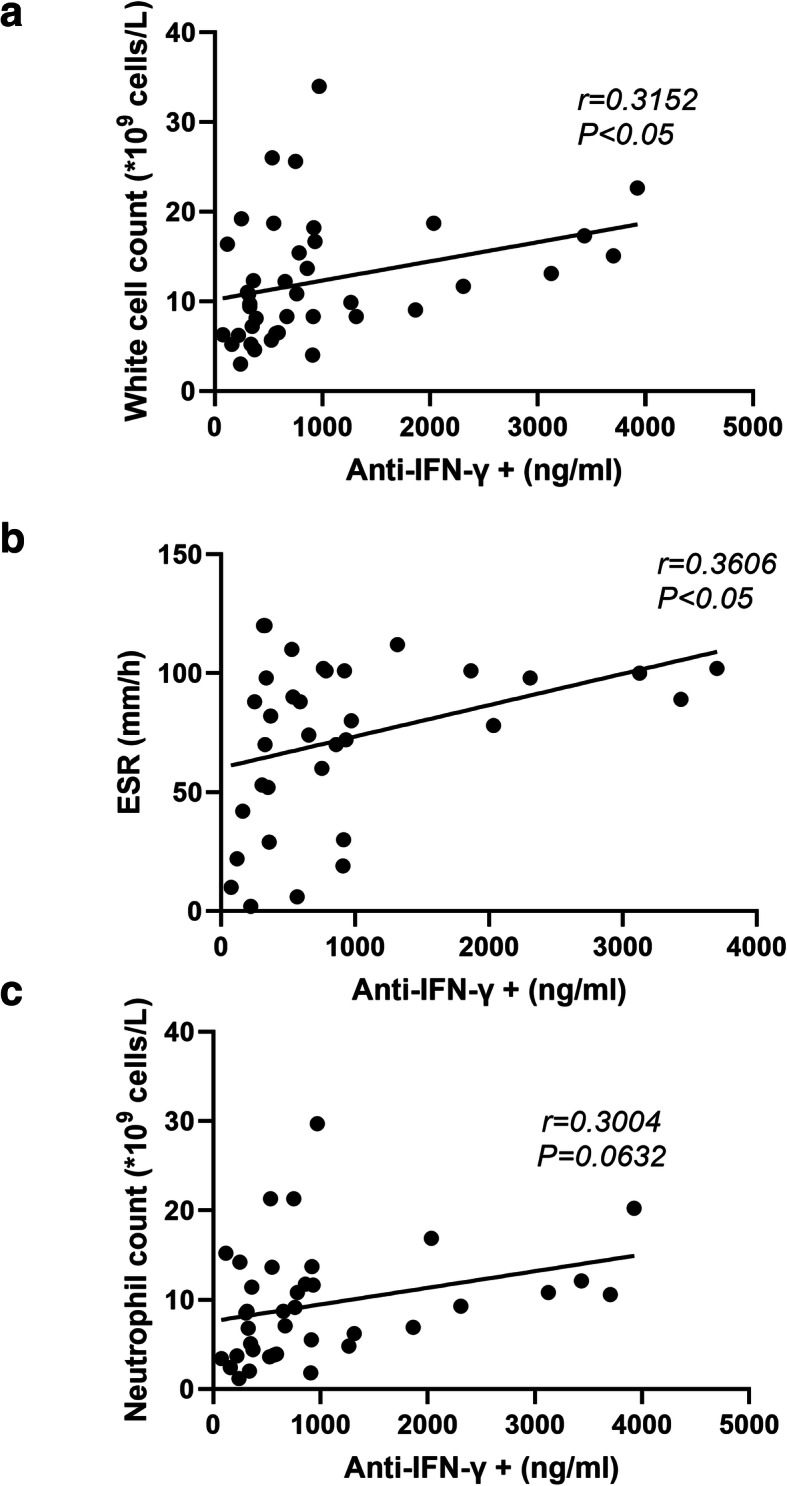
Pearson correlation analysis of serum anti-IFN-γ autoAbs and inflammatory markers among patients with T. marneffei infection. a Correlation between anti-IFN-γ autoAbs and white-cell count. b Correlation between anti-IFN-γ autoAbs and erythrocyte sedimentation rate. c Correlation between anti-IFN-γ autoAbs and absolute neutrophil count. ESR = Erythrocyte sedimentation rate
Table 4.
Multivariate logistic regression analysis of factors associated with the appearance of anti-IFN-γ autoantibody positivity
| Variable | Univariable OR (95% CI) | P value | Multivariable OR (95% CI) | P value |
|---|---|---|---|---|
| White-cell count (*109 cells/L) | 1.134 (1.007, 1.277) | 0.038 | 1.035 (0.906, 1.183) | 0.610 |
| Hemoglobin (g/L) | 0.973 (0.947, 1.001) | 0.057 | 0.985 (0.948, 1.024) | 0.454 |
| Coexisting respiratory disease | 0.158 (0.035, 0.708) | 0.016 | 0.094 (0.011, 0.809) | 0.031 |
| Pleural effusion | 8.185 (1.839, 36.424) | 0.006 | 11.162 (1.517, 82.164) | 0.018 |
| Extrapulmonary organ involvement | 3.682 (0.911, 14.876) | 0.067 | 0.469 (0.046, 4.834) | 0.525 |
OR Odds ratio, CI Confidence interval
Clinical courses and outcomes of patients with T. marneffei infection
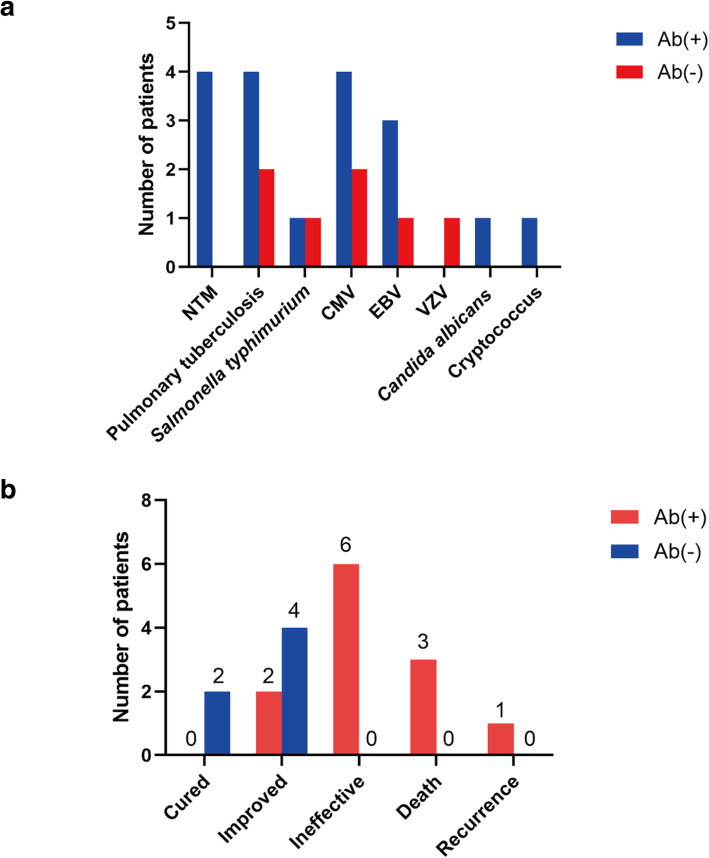
Of the 42 patients, 12 (55.0%) in group TMP and 4 (20.0%) in group TMN (P < 0.05, Table 2) were coinfected with other intracellular pathogens. Among patients in group TMP, 4 with disseminated NTM diseases (n = 4; 18.2%), 3 with active pulmonary tuberculosis and 1 with spinal tuberculosis, (n = 4; 18.2%), 4 with positive results of cytomegalovirus (CMV) DNA detection in BALF (n = 4; 18.2%), 3 with positive results of Epstein-Barr virus (EBV) DNA detection in BALF (n = 3; 13.6%), 1 with positive results of Salmonella typhimurium culture in sputum (n = 1; 4.5%), and 1 with positive results of Candida albicans culture in sputum (n = 1; 4.5%). Among patients in group TMN, 2 with active pulmonary tuberculosis (n = 2; 10.0%), 2 with positive results of cytomegalovirus (CMV) DNA detection in BALF (n = 2; 10.0%), 1 with positive results of Epstein-Barr virus (EBV) DNA detection in BALF (n = 1; 5.0%), 1 with positive results of Salmonella typhimurium culture in blood (n = 1; 4.5%), 1 with positive results of Cryptococcus spp culture in BALF (n = 1; 4.5%) and 1 with varicella zoster virus detected (VZV) DNA detection in blood (n = 1; 5.0%) (Fig. 4A).
Fig. 4.
Clinical courses and outcomes of patients with T. marneffei infectio. a Coinfected pathogens among patients with T. marneffei infection. b Clinical outcome of patients with T. marneffei infection after 12 months of treatment. NTM = Nontuberculous Mycobacterium; CMV = Cytomegalovirus; VZV = Varicella zoster virus; EBV = Epstein-Barr virus
In addition, data were available for 12 patients in group TMP and 6 patients in group TMN during the longitudinal follow-up. The treatment among patients included intravenous amphotericin B 0.6–1.0 mg/kg/day for 2 weeks, followed by oral itraconazole or voriconazole 400 mg/day for maintenance therapy. Despite long-term intensive treatment, patients in group TMP had a worse prognosis than patients in group TMN. In group TMP, 2 patients developed fatal disseminated infection and died within the first 30 postoperative days (premature mortality) because of multiple organ failure, 1 patient underwent 6 months of treatment and also complicated with secondary tuberculosis, and eventually died due to severe infections, 6 patients had persistent T. marneffei infection with a poor response after treatment. Furthermore, and one patient experienced clinical recurrence at 12 months. (Fig. 4B).
Discussion
In this study, we confirmed that anti-IFN-γ autoAbs are an important risk factor for T. marneffei infection among non-HIV-infected patients. Most patients who were anti-IFN-γ autoAb-positive did not have any underlying respiratory disease and frequently had systemic dissemination with major pleural effusion. In addition, the leukocyte count and the levels of C-reactive protein and other inflammatory markers in these patients were significantly higher than those in anti-IFN-γ autoAb-negative patients. Despite the progression of T. marneffei infection, the anti-IFN-γ autoAb titer did not decrease after targeted treatment, and most patients had a poor outcome (such as death or recurrence of infection).
Anti-IFN-γ autoAbs have previously been shown to be an important risk factor for T. marneffei infections. Our data also supported this important finding. A large number of anti-IFN-γ autoAb-positive patients were found in group TM. This might be related to the high prevalence of anti-IFN-γ autoAb-associated HLA class II DRB1*16:02 and DQB1*05:02 alleles in the Asian population [18, 19]. Both Guangdong and Guangxi provinces are located in southern China, where T. marneffei are endemic due to the humid climate.
Since the 1990s, an increasing number of patients with T. marneffei infection have been reported among non-HIV-infected patients with impaired cell-mediated immunity. The comorbidities included primary adult-onset immunodeficiency due to anti-IFN-γ autoAbs and secondary immunocompromise, including that resulting from autoimmune disease or the use of immunosuppressive drugs such as novel anticancer targeted therapies and kinase inhibitors [16], but infections have been found even in patients with normal immunity [20]. The pathogenesis of anti-IFN-γ autoAb-positive patients was different from that of anti-IFN-γ autoAb-negative patients who had normal immunity and suffered from chronic lung diseases (such as COPD, bronchiectasis or asthma). Chronic lung diseases can lead to lung structural damage in various ways, resulting in impaired natural immune function and thereby changing the microenvironment that offers a niche for respiratory microorganisms. Furthermore, dysmicrobiosis might have increased the susceptibility of the hosts to T. marneffei infection [21, 22]. As a result, the lungs were the dominant organs involved, whereas anti-IFN-γ autoAb-positive patients were more likely to develop systemic dissemination of T. marneffei infection and pleural effusion [8]. Most patients with T. marneffei infection had pleural effusion characterized by yellowish exudates, with marked elevation of protein levels and nucleated cell counts [23]. Multiple organs might also be involved, especially the bone and skin, which might readily predispose patients to the development of Sweet syndrome [24].
Patients who tested positive for anti-IFN-γ autoAbs also had more significantly elevated inflammatory responses characterized by elevated leukocyte and neutrophil counts, erythrocyte sedimentation rates and C-reactive protein levels, markers indicating more exuberant infections in patients with anti-IFN-γ autoAbs. This is in accordance with previous studies such as by Angkasekwinai N et al. [25]. Neutrophils play an important role in the development of innate immunity. Neutrophils are the frontline barrier for eradicating the invasion of microbial pathogens and have powerful phagocytic capacity. In addition, neutrophils have been implicated in the production of the chemokine myeloperoxidase [26]. Neutrophil-derived IL-17A [27] also induces the release of IFN-γ, which promotes the antibacterial activity of macrophages [28]. We also observed a notable bone marrow response in this patient population, which was more prone to developing anemia [10] and leukocytosis [11]. A significant increase in CD8+ T cells was observed in anti-IFN-γ autoAb-positive patients. IFN-γ is indispensable for fighting infections because of its ability to regulate various protective functions and sustain the activity of both CD4+ and CD8+ T cells [29]. Conversely, IFN-γ produced by CD8+ T cells promotes the expression of major histocompatibility complex molecules on the surface of target cells to enhance antigen presentation and enhances the ability of macrophages and dendritic cells to phagocytose pathogens [30]. We speculate that the autoAbs might have affected the normal function of IFN-γ, leading to compensatory proliferation of these immune cells.
The patients were prospectively followed for up to 12 months, thus allowing us to estimate the correlation between the autoAb titer and disease progression. However, the anti-IFN-γ autoAb level did not correlate significantly with the clinical course, which was consistent with the findings from a previous study [31]. In addition, anti-IFN-γ autoAb-positive patients were more likely to be coinfected with other intracellular pathogens, especially NTM [32, 33]. Despite the initiation of standardized antimicrobial therapy, the patients’ conditions did not improve, and some deteriorated even further. There is no well-established standard therapy to reduce the titer of anti-IFN-γ autoAbs. However, one study reported a significant improvement in clinical symptoms after plasma exchange therapy [10]. Supplementation of IFN-γ recombinant protein [34], cyclophosphamide [35, 36] and B cell depletion with an anti-CD20 antibody [37, 38] have also been successfully used as adjuvant therapies in combination with antimicrobial therapy in a small number of patients. Prospective randomized clinical trials are needed to determine the therapeutic efficiency of these strategies.
Some limitations of our study need to be acknowledged. First, our sample size was relatively small, and therefore, selection bias might have affected the interpretation of our data. Second, for some patients, documentation of the laboratory findings during the longitudinal follow-up was incomplete, which hampered assessment of associations with the therapeutic response. Moreover, this was an observational cohort study with a limited duration of follow-up, and additional immunological experiments are needed to further explore the underlying mechanism.
Conclusion
We outlined the clinical characteristics of T. marneffei-infected patients with immunodeficiency due to the presence of anti-IFN-γ autoAbs. These patients were more likely than anti-IFN-γ autoAb-negative patients to have systemic dissemination of infection and heightened inflammatory responses. More studies are needed to explore how to reduce the production of autoAbs, which might help to manage T. marneffei infection in patients with anti-IFN-γ autoAbs.
Acknowledgments
We thank the patient; the nurses and clinical staffs who are providing care for the patient; staffs at the respiratory medicine department of hospital; staffs at the clinical lab of hospital; technical staffs of the department of State Key Laboratory of Respiratory Disease for excellent assistance. Furthermore, we would also like to thank AJE team for polishing the English language of this manuscript.
Abbreviations
- anti-IFN-γ autoAbs
Anti-interferon-γ autoantibodies
- NTM
Nontuberculous Mycobacterium
- T. marneffei
Talaromyces marneffei
- HIV
Human immunodeficiency virus
- IQRs
Interquartile ranges
- COPD
Chronic obstructive pulmonary disease
- Group TMP
Anti-IFN-γ autoantibody-positive group
- Group TNN
Anti-IFN-γ autoantibody-negative group
- ORs
Odds ratios
- CIs
Confidence intervals
- CMV
Cytomegalovirus
- VZV
Varicella zoster virus
- EBV
Epstein-Barr virus
Authors’ contributions
All authors fulfilled the contribution requirements as per the International Committee of Medical Journal Editors role of authors and contributor guidelines. Chen ZM, Li ZT, Zhang JQ and Ye F conceived of and designed the study. Chen ZM, Guan WJ and Ye F carried out the analyses and wrote the first draft of the manuscript. Zhan YQ, Qiu Y, Lei ZY, Li SQ, Zhou H, Lin S, Zeng W and Liu J carried out the patient’s recruitment and clinical sample collection. Chen ZM and Li Z contributed to the handling and testing of samples. Chen ZM and Lin Y contributed to the collection of data from the electronic medical records. All authors contributed to data acquisition, data analysis, or data interpretation and reviewed and approved the final version of the manuscript.
Funding
This work was funded by the open fund of State Key Laboratory of Respiratory Diseases (SKLRD-OP-201913); The independent fund of State Key Laboratory of Respiratory Diseases (SKLRD-Z-202019); The Guangzhou Institute of Respiratory Health Open Project (2019GIRHZ06).
Availability of data and materials
The data-sets generated and/or analysed during the current study are not publicly available due to the presence of sensitive (confidential) participants’ information but are available from the corresponding author on reasonable request.
Declaration
Ethics approval and consent to participate
The study was carried out in accordance with the Declaration of Helsinki. The study was approved by the Ethics Committee of the First Affiliated Hospital of Guangzhou Medical University (reference number 2019026). All methods were carried out in accordance with relevant guidelines and regulations. All included subjects and legally authorized representative/next of kin of all deceased participants gave their oral and written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors report no conflicts of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhao-Ming Chen, Zheng-Tu Li, Yang-Qing Zhan and Wei-Jie Guan contributed equally to this work.
Contributor Information
Jian-Quan Zhang, Email: jqzhang2002@126.com.
Feng Ye, Email: tu276025@gird.cn, Email: yefeng@gird.cn.
References
- 1.Doffinger R, Helbert MR, Barcenas-Morales G, Yang K, Dupuis S, Ceron-Gutierrez L, Espitia-Pinzon C, Barnes N, Bothamley G, Casanova JL, Longhurst HJ, Kumararatne DS. Autoantibodies to interferon-gamma in a patient with selective susceptibility to mycobacterial infection and organ-specific autoimmunity. Clin Infect Dis. 2004;38(1):e10–e14. doi: 10.1086/380453. [DOI] [PubMed] [Google Scholar]
- 2.Browne SK, Burbelo PD, Chetchotisakd P, Suputtamongkol Y, Kiertiburanakul S, Shaw PA, Kirk JL, Jutivorakool K, Zaman R, Ding L, Hsu AP, Patel SY, Olivier KN, Lulitanond V, Mootsikapun P, Anunnatsiri S, Angkasekwinai N, Sathapatayavongs B, Hsueh PR, Shieh CC, Brown MR, Thongnoppakhun W, Claypool R, Sampaio EP, Thepthai C, Waywa D, Dacombe C, Reizes Y, Zelazny AM, Saleeb P, Rosen LB, Mo A, Iadarola M, Holland SM. Adult-onset immunodeficiency in Thailand and Taiwan. N Engl J Med. 2012;367(8):725–734. doi: 10.1056/NEJMoa1111160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xie YL, Rosen LB, Sereti I, Barber DL, Chen RY, Hsu DC, Qasba SS, Zerbe CS, Holland SM, Browne SK. Severe paradoxical reaction during treatment of disseminated tuberculosis in a patient with neutralizing anti-IFNgamma autoantibodies. Clin Infect Dis. 2016;62(6):770–773. doi: 10.1093/cid/civ995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yerramilli A, Huang G, Griffin D, et al. Disseminated Nontuberculous Mycobacterial Infection Associated With Acquired Immunodeficiency Due to Anti-Interferon gamma Autoantibodies. Open Forum Infect Dis. 2019;6:ofz131. doi: 10.1093/ofid/ofz131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van de Vosse E, Hoeve MA, Ottenhoff TH. Human genetics of intracellular infectious diseases: molecular and cellular immunity against mycobacteria and salmonellae. Lancet Infect Dis. 2004;4(12):739–749. doi: 10.1016/S1473-3099(04)01203-4. [DOI] [PubMed] [Google Scholar]
- 6.Höflich C, Sabat R, Rosseau S, et al. Naturally occurring anti–IFN-γ autoantibody and severe infections with Mycobacterium cheloneae and Burkholderia cocovenenans. Blood. 2004;103(2):673–675. doi: 10.1182/blood-2003-04-1065. [DOI] [PubMed] [Google Scholar]
- 7.Tang BSF, Chan JFW, Chen M, Tsang OTY, Mok MY, Lai RWM, Lee R, Que TL, Tse H, Li IWS, To KKW, Cheng VCC, Chan EYT, Zheng B, Yuen KY. Disseminated Penicilliosis, recurrent Bacteremic Nontyphoidal salmonellosis, and Burkholderiosis associated with acquired immunodeficiency due to autoantibody against gamma interferon. Clin Vaccine Immunol. 2010;17(7):1132–1138. doi: 10.1128/CVI.00053-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wongkulab P, Wipasa J, Chaiwarith R, Supparatpinyo K. Autoantibody to interferon-gamma associated with adult-onset immunodeficiency in non-HIV individuals in northern Thailand. PLoS One. 2013;8(9):e76371. doi: 10.1371/journal.pone.0076371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Phoompoung P, Ankasekwinai N, Pithukpakorn M, Foongladda S, Umrod P, Suktitipat B, Mahasirimongkol S, Kiertiburanakul S, Suputtamongkol Y. Factors associated with acquired anti IFN- γ autoantibody in patients with nontuberculous mycobacterial infection. PLoS One. 2017;12(4):e0176342. doi: 10.1371/journal.pone.0176342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Angkasekwinai N, Suputtamongkol Y, Phoompoung P, Pithukpakorn M, Wongswat E, Umrod P, Tongsai S, Foongladda S. Clinical outcome and laboratory markers for predicting disease activity in patients with disseminated opportunistic infections associated with anti-interferon-γ autoantibodies. PLoS One. 2019;14(4):e0215581. doi: 10.1371/journal.pone.0215581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zeng W, Qiu Y, Tang S, Zhang J, Pan M, Zhong X. Characterization of Anti-Interferon-gamma Antibodies in HIV-Negative Patients Infected With Disseminated Talaromyces marneffei and Cryptococcosis. Open Forum Infect Dis. 2019;6:ofz208. doi: 10.1093/ofid/ofz208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guo J, Ning XQ, Ding JY, Zheng YQ, Shi NN, Wu FY, Lin YK, Shih HP, Ting HT, Liang G, Lu XC, Kong JL, Wang K, Lu YB, Fu YJ, Hu R, Li TM, Pan KS, Li XY, Huang CY, Lo YF, Chang IYF, Yeh CF, Tu KH, Tsai YH, Ku CL, Cao CW. Anti-IFN-gamma autoantibodies underlie disseminated Talaromyces marneffei infections. J Exp Med. 2020;217:12. doi: 10.1084/jem.20190502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chitasombat M, Supparatpinyo K. Penicillium marneffei infection in Immunocompromised host. Curr Fungal Infect Rep. 2013;7(1):44–50. doi: 10.1007/s12281-012-0119-5. [DOI] [Google Scholar]
- 14.Vanittanakom N, Cooper CJ, Fisher MC, Sirisanthana T. Penicillium marneffei infection and recent advances in the epidemiology and molecular biology aspects. Clin Microbiol Rev. 2006;19(1):95–110. doi: 10.1128/CMR.19.1.95-110.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong S, Siau H, Yuen KY. Penicilliosis marneffei--west meets east. J Med Microbiol. 1999;48(11):973–975. doi: 10.1099/00222615-48-11-973. [DOI] [PubMed] [Google Scholar]
- 16.Chan JF, Lau SK, Yuen KY, Woo PC. Talaromyces (Penicillium) marneffei infection in non-HIV-infected patients. Emerg Microbes Infect. 2016;5(1):e19. doi: 10.1038/emi.2016.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaplan JE, Benson C, Holmes KK, Brooks JT, Pau A, Masur H. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep. 2009;58:1–207. [PubMed] [Google Scholar]
- 18.Pithukpakorn M, Roothumnong E, Angkasekwinai N, Suktitipat B, Assawamakin A, Luangwedchakarn V, Umrod P, Thongnoppakhun W, Foongladda S, Suputtamongkol Y. HLA-DRB1 and HLA-DQB1 are associated with adult-onset immunodeficiency with acquired anti-interferon-gamma autoantibodies. PLoS One. 2015;10(5):e0128481. doi: 10.1371/journal.pone.0128481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ku CL, Lin CH, Chang SW, et al. Anti-IFN-gamma autoantibodies are strongly associated with HLA-DR*15:02/16:02 and HLA-DQ*05:01/05:02 across Southeast Asia. J Allergy Clin Immunol. 2016;137:945–8.e8. doi: 10.1016/j.jaci.2015.09.018. [DOI] [PubMed] [Google Scholar]
- 20.Lee PP, Chan KW, Lee TL, et al. Penicilliosis in children without HIV infection--are they immunodeficient? Clin Infect Dis. 2012;54(2):e8–e19. doi: 10.1093/cid/cir754. [DOI] [PubMed] [Google Scholar]
- 21.O'Dwyer DN, Dickson RP, Moore BB. The lung microbiome, immunity, and the pathogenesis of chronic lung disease. J Immunol. 2016;196(12):4839–4847. doi: 10.4049/jimmunol.1600279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dickson RP, Martinez FJ, Huffnagle GB. The role of the microbiome in exacerbations of chronic lung diseases. Lancet. 2014;384(9944):691–702. doi: 10.1016/S0140-6736(14)61136-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Qiu Y, Zeng W, Zhang H, Zhong X, Tang S, Zhang J. Comparison of pleural effusion features and biomarkers between talaromycosis and tuberculosis in non-human immunodeficiency virus-infected patients. BMC Infect Dis. 2019;19(1):745. doi: 10.1186/s12879-019-4376-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chan JF, Trendell-Smith NJ, Chan JC, et al. Reactive and infective dermatoses associated with adult-onset immunodeficiency due to anti-interferon-gamma autoantibody: Sweet's syndrome and beyond. Dermatology. 2013;226(2):157–166. doi: 10.1159/000347112. [DOI] [PubMed] [Google Scholar]
- 25.Angkasekwinai N, Suputtamongkol Y, Phoompoung P, Pithukpakorn M, Wongswat E, Umrod P, Tongsai S, Foongladda S. Clinical outcome and laboratory markers for predicting disease activity in patients with disseminated opportunistic infections associated with anti-interferon-gamma autoantibodies. PLoS One. 2019;14(4):e0215581. doi: 10.1371/journal.pone.0215581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yamaguchi R, Kawata J, Yamamoto T, Ishimaru Y, Sakamoto A, Ono T, Narahara S, Sugiuchi H, Hirose E, Yamaguchi Y. Mechanism of interferon-gamma production by monocytes stimulated with myeloperoxidase and neutrophil extracellular traps. Blood Cells Mol Dis. 2015;55(2):127–133. doi: 10.1016/j.bcmd.2015.05.012. [DOI] [PubMed] [Google Scholar]
- 27.Cai S, Batra S, Langohr I, Iwakura Y, Jeyaseelan S. IFN-gamma induction by neutrophil-derived IL-17A homodimer augments pulmonary antibacterial defense. Mucosal Immunol. 2016;9(3):718–729. doi: 10.1038/mi.2015.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang G, Lin A, Han Q, Zhao H, Tian Z, Zhang J. IFN-gamma protects from apoptotic neutrophil-mediated tissue injury during acute listeria monocytogenes infection. Eur J Immunol. 2018;48(9):1470–1480. doi: 10.1002/eji.201847491. [DOI] [PubMed] [Google Scholar]
- 29.Kak G, Raza M, Tiwari BK. Interferon-gamma (IFN-γ): exploring its implications in infectious diseases. Biomolecular Concepts. 2018;9(1):64–79. doi: 10.1515/bmc-2018-0007. [DOI] [PubMed] [Google Scholar]
- 30.Andersen MH, Schrama D, Thor SP, Becker JC. Cytotoxic T cells. J Invest Dermatol. 2006;126(1):32–41. doi: 10.1038/sj.jid.5700001. [DOI] [PubMed] [Google Scholar]
- 31.Tham EH, Huang CH, Soh JY, Thayalasingam M, Lee AJ, Lum LHW, Poon LM, Lye DCB, Chai LYA, Tambyah PA, Lee BW, Shek LPC. Neutralizing anti-interferon-gamma autoantibody levels may not correlate with clinical course of disease. Clin Infect Dis. 2016;63(4):572–573. doi: 10.1093/cid/ciw351. [DOI] [PubMed] [Google Scholar]
- 32.Zhang J, Huang X, Zhang X, Zhu Y, Liao K, Ma J, Wang G, Guo Y, Xie C. Coinfection of disseminated Talaromyces marneffei and mycobacteria kansasii in a patient with papillary thyroid cancer: a case report. Medicine (Baltimore) 2017;96(52):e9072. doi: 10.1097/MD.0000000000009072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Su SS, Zhang SN, Ye JR, Xu LN, Lin PC, Xu HY, Wu Q, Li YP. Disseminated Talaromyces marneffei and Mycobacterium avium infection accompanied Sweet's syndrome in a patient with anti-interferon-gamma autoantibodies: a case report. Infect Drug Resist. 2019;12:3189–3195. doi: 10.2147/IDR.S218836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lin CH, Chi CY, Shih HP, Ding JY, Lo CC, Wang SY, Kuo CY, Yeh CF, Tu KH, Liu SH, Chen HK, Ho CH, Ho MW, Lee CH, Lai HC, Ku CL. Identification of a major epitope by anti-interferon-gamma autoantibodies in patients with mycobacterial disease. Nat Med. 2016;22(9):994–1001. doi: 10.1038/nm.4158. [DOI] [PubMed] [Google Scholar]
- 35.Chetchotisakd P, Anunnatsiri S, Nanagara R, Nithichanon A, Lertmemongkolchai G. Intravenous cyclophosphamide therapy for anti-IFN-gamma autoantibody-associated Mycobacterium abscessus infection. J Immunol Res. 2018;2018:6473629–6473627. doi: 10.1155/2018/6473629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Laisuan W, Pisitkun P, Ngamjanyaporn P, Suangtamai T, Rotjanapan P. Prospective Pilot Study of Cyclophosphamide as an Adjunct Treatment in Patients With Adult-Onset Immunodeficiency Associated With Anti-interferon-gamma Autoantibodies. Open Forum Infect Dis. 2020;7:ofaa035. doi: 10.1093/ofid/ofaa035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Browne SK, Zaman R, Sampaio EP, Jutivorakool K, Rosen LB, Ding L, Pancholi MJ, Yang LM, Priel DL, Uzel G, Freeman AF, Hayes CE, Baxter R, Cohen SH, Holland SM. Anti-CD20 (rituximab) therapy for anti-IFN-gamma autoantibody-associated nontuberculous mycobacterial infection. Blood. 2012;119(17):3933–3939. doi: 10.1182/blood-2011-12-395707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hong GH, Ortega-Villa AM, Hunsberger S, Chetchotisakd P, Anunnatsiri S, Mootsikapun P, Rosen LB, Zerbe CS, Holland SM. Natural history and evolution of anti-interferon-gamma autoantibody-associated immunodeficiency syndrome in Thailand and the United States. Clin Infect Dis. 2020;71(1):53–62. doi: 10.1093/cid/ciz786. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data-sets generated and/or analysed during the current study are not publicly available due to the presence of sensitive (confidential) participants’ information but are available from the corresponding author on reasonable request.