Abstract
Objectives
Even though SARS Cov2 outbreak management has been well-described, scant information is available in military settings. We aimed to describe a SARS Cov2 outbreak and its management on the Dixmude, a French landing helicopter dock.
Patients and methods
We performed an observational retrospective and monocentric study in a ship. Role 1 was reinforced by additional roles 1 and 2. Our analysis included all infected crew personnel. We described demographic data, outbreak course, and biological samples including Covid-19 diagnosis. All infected patients were monitored for 10 days.
Results
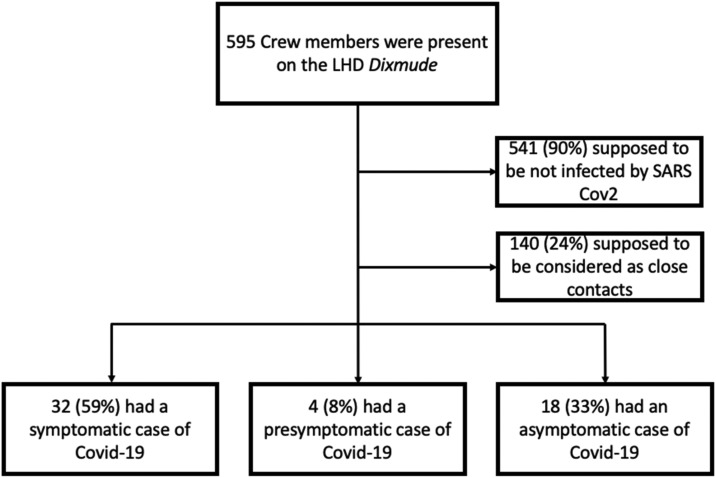
Between February 16th 2021 and March 12th 2021, 54 patients (10% of the entire crew) were included. No patient had previously been vaccinated against SARS Cov2. The global mission was maintained. The crew members were healthy, male, and young (median age 28 years) with no medical history. Ranks of every status were concerned. Covid-19 disease was mainly diagnosed by real-time reverse-transcriptase polymerase chain reaction (rt-PCR). Thirty-two patients (59%) were symptomatic, four (8%) were presymptomatic and 18 (33%) remained asymptomatic.
Conclusions
The present work describes specific SARS Cov2 outbreak management in an austere military environment. Early individual and global measures were set and implemented on board.
Keywords: Austere environment, Covid-19, Landing helicopter dock, SARS Cov2
1. Introduction
The Covid-19 pandemic has continued for more than a year [1], [2]. As of March 2021, more than 120,900,000 cases of SARS Cov2 virus infection had been reported around the world. Most medical care is provided in standard facilities with adapted staff and supply. An uncomplicated infected patient may easily be quarantined and thereby limit virus spreading. However, medical wards or intensive care units can be quickly overwhelmed [3]. While SARS Cov2 outbreak management has been well-described in civilian settings, less information in military settings is available. Managing a SARS Cov2 outbreak in a military context represents additional difficulties, including ongoing military operations, global military health, and austere environment [4], [5]. The French Landing Helicopter Dock (LHD) Dixmude was conducting operations in the Gulf of Guinea when a SARS Cov2 outbreak occurred on board. While military operations were delayed during the outbreak, the global mission proceeded uninterrupted. All medical care was provided on board except for two patients. In the present study, we describe the outbreak course during the mission, its characteristics, laboratory sample results, and key findings about management by both the medical staff and the French Navy.
2. Material and methods
We performed a retrospective, monocentric, and observational study. The intent of this investigation was to collect data designed to limit SARS Cov2 outbreak spread on board, to take urgent locally implemented measures to reduce SARS Cov2 outbreak risk on other French navy ships with ongoing military operations, and to decrease potential impact on the health of on-duty crews. During the investigation, it was necessary to deal with a B.1.1.7 SARS Cov2 variant that was identified and was spreading on board. The study was approved by the French Society for Anesthesia and Intensive Care ethics committee (IRB 00010254). Each patient's consent was recorded. A compliance declaration was sent to the CNIL (Commission Nationale de l’Informatique et des Libertés).
2.1. Ship description and crew
The LHD Dixmude has a crew of 215 seamen, and can embark up to 650 additional persons; for this mission, there were 595 persons aboard. The LHD Dixmude is one of the three amphibious assault ships of the French Navy. By air or amphibiously, projection capacities allow helicopters, troops, or vehicle landing. Here, its main missions in the Gulf of Guinea were to manage a possible evacuation of French nationals from African countries, to combat regional maritime piracy and to perform military operations in the framework of international partnerships. The hospital aboard represents a 750 m2 and 34-bed inpatient facility with four medical bedrooms, a four-bed intensive care unit, and a large 12-bed room. Navy role 1 was reinforced by Army role 1 and role 2. Role 1's aim is to provide global and primary care. Role 2's mission is to provide surgical or critical care. The medical staff consisted in two general practitioners, one anesthetist-intensivist, one certified registered nurse anesthetist, four nurses, four medical auxiliaries, one radiological manipulator and one laboratory assistant. The available oxygen supply aboard was 290,000L (29,50 L-oxygen bottles at 200 bar pressure). Two turbine-driven transport ventilators (Elisée 350, ResMed) were available. No high flow oxygen device or noninvasive ventilation device were present on board. However, three portable oxygen concentrators (SeQual Integra 10-OM) were available. A CT-scanner was likewise deployed.
2.2. Outbreak occurrence
Before departure, every crew member was subjected to a nasopharyngeal real-time Reverse-Transcriptase Polymerase Chain Reaction (rt-PCR) test following a one-week quarantine. No one was previously vaccinated against SARS Cov2 but all members were up-to-date with influenza and yellow fever vaccinations. All crew personnel received malaria prophylaxis by daily doxycycline intake. General measures against SARS Cov2 spreading were followed on board with mask wearing, social distancing, and frequent hand disinfection, whereas some shared spaces remained open. After eight days at sea, the LHD reached Dakar (Senegal). A three-day stop was organized with standard isolation measures (same as above). No physical contact with local Senegalese people was reported by any crew member. On February 16th, three days after leaving the port of Dakar, crew members consulted at the hospital presenting with SARS Cov2 symptoms. As soon as the French Navy knew an outbreak was occurring on board, it was decided to head for Abidjan (Ivory Coast) to facilitate patient evacuation, putting major military operations on hold. Between February 23rd and February 27th, with Ivorian help nasopharyngeal swab specimens from all crew members were obtained. Infantry soldiers disembarked for isolation on land after testing, while the ship sailed during a week, after which the military detachment went back on the ship. On March 9th, considering that the epidemic curve was decreasing, the LHD could continue its mission.
Management was performed as follows: each identified patient was isolated in the ship hospital for 10 days. Each patient had to be symptom-free (shortness of breath or fever) during two days before exit. Close contacts were defined as persons sharing quarters or activities within one meter distance for at least 15 minutes; they were quarantined for 7 days with exit rt-PCR testing.
2.3. Laboratory testing
The presence of SARS Cov2 infection was determined by rt-PCR testing (GeneXpert™) or antigen testing (CovidViro™). No additional tool was available aboard to determine SARS Cov2 variance. Whenever rt-PCR was required, cycle threshold (CT) (reflecting the number of nucleic acid amplification cycles that occur before the material generates a signal positive) was recorded. As stated above, repeated SARS Cov2 testing by rt-PCR was obtained on completion of 10 days of isolation, after which a crew member could be eligible for return to duty. Repeated biological samples were obtained in symptomatic patients.
2.4. Data collection
The study population consisted in SARS Cov2-infected crew members. We defined a confirmed case of Covid-19 as one in which a nasopharyngeal swab specimen was positive for SARS Cov2 by either rt-PCR or antigen test. Among confirmed cases, we defined symptomatic, presymptomatic, or asymptomatic cases as follows: symptomatic patients presented symptoms when the first laboratory test was positive; presymptomatic patients developed symptoms after the first laboratory test was positive; asymptomatic patients never developed symptoms despite their positive laboratory test. We collected the patients’ medical records: age, sex, medical history, weight, crew type and work department, rank status, tobacco status. Patient follow-up was carried out twice a day by a doctor/nurse team during 10 days. More frequently recorded data could be proposed for patients at risk of severe Covid-19 or presenting progressive symptoms. A nurse shift rotation occurred every 24 hours. The twice-daily collected data included: daily symptoms, temperature, blood pressure and pulse oximetry. Data were pre-anonymized using a random allocating number. Pre-defined variables were collected using Microsoft Excel 2010 (Microsoft Corporation, Redmond, Washington).
2.5. Statistical analysis
Quantitative variables were reported as median [interquartile range; IQR]. Qualitative data were reported as absolute value and percentage. Statistical analysis for qualitative data comparison was performed according to Chi2 test; P = 0.05 was defined as a significant difference.
3. Results
3.1. Outbreak timeline details
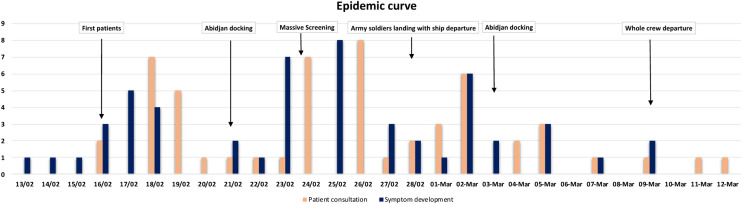
Between February 16th and March 12th, a total of 54 patients (10% of the entire crew) were tested positive for SARS Cov2, and 130 crew members were considered as close contacts. By questioning the first patients, we learned that SARS Cov2 symptom onset began on February 13th, the day of departure from Dakar harbor. Among confirmed cases, 32 patients (59%) were symptomatic, four (8%) were presymptomatic and 18 (33%) remained asymptomatic. Rt-PCR SARS Cov2 test was performed in 35 (65%) patients while antigen test results were obtained in 19 (35%) patients. The flow chart diagram is presented on Fig. 1 . By March 1st, the hospital was fully occupied and some patients had to be placed in isolation on another deck. Fig. 2 depicts the epidemic curve as first-day symptom development. The higher clinician–patient ratio was reached on March 2nd (1:11).
Fig. 1.
Flow chart: distribution of personnel according to case status.
Fig. 2.
Epidemic curve and the hospital tension. The left axis represents the number of confirmed infected patients over time. The right axis represents the number of patients present in the hospital over time. Data are presented as number of patients.
3.2. Patient characteristics
All patients were military, fit and healthy, and they met standards for sea duty. Most of them were young people (median age 28 years [22–31]) and male (n = 45, 83%). Median weight was 76 kg [70–82]. Table 1 summarizes patient characteristics. One patient presented a sleep apnea requiring home-noninvasive ventilation and another had undergone splenectomy. Two symptomatic patients had had a SARS Cov2 medical history two and four months before. Symptom onset combined with low CT detection through rt-PCR diagnosis tended to show active infection. Crew members of every rank status were concerned in one way or another by SARS Cov2 infection and no statistical differences were noted. The single smoking area on board was suspected as the initial trigger for virus spreading. Among infected patients, there were significantly more tobacco users than in non-infected crew, n = 15/54 vs. n = 82/541 respectively; P = 0.027. Two departments appeared particularly affected by virus spreading: the amphibious unit (n = 11, 20%; P < 0.001) and the galleys (n = 10, 19%; P < 0.001). Attack rate among LHD crew was significantly higher than among embarked land army (P < 0.001). One member of the medical staff presented an uncomplicated SARS Cov2 infection.
Table 1.
Characteristics of infected Covid-19 patients.
| n (%) | Median (IQR) | |
|---|---|---|
| Demographic characteristics | ||
| Age (years) | 28 [22–31] | |
| Sex (Male) | 45 (83) | |
| Weight (kg) | 76 [70–82] | |
| Tobacco users | 15 (28) | |
| Smoking area visitors | 8 (15) | |
| Crew type | ||
| Ship's crew | 37 (68) | |
| Land army | 15 (28) | |
| Stranger army | 2 (4) | |
| Rank status | ||
| Officer | 5 (10) | |
| Non-commissioned officer | 17 (31) | |
| Enlisted | 32 (59) | |
| Diagnosis tool | ||
| rt-PCR | 35 (65) | |
| CT value | 16 [16–1] | |
| Antigen test | 19 (35) | |
| Clinical course | ||
| Asymptomatic | 18 (33) | |
| Presymptomatic | 4 (8) | |
| Symptomatic | 32 (59) | |
| Unit | ||
| Amphibious Unit | 11 (20) | |
| Galleys | 10 (19) | |
| Others | 33 (61) |
The median delay from symptom onset to hospitalization was 1 day [0–1]. Symptom distribution was unspecific: fever, cough, shortness of breath, diarrhea…
3.3. Laboratory samples
Rt-PCR was necessary for SARS Cov2 diagnosis in 35 (65%) patients while antigen test results were obtained in 19 (35%) patients. Median rt-PCR CT was 28 [16–40]. Asymptomatic cases were similar according to screening tool (rt PCR n = 12 (54%) or antigenic test n = 10 (46%); P = 0,6). SARS Cov2 variance was analyzed by the Ivoirian Pasteur Institute during the LHD mission and in the Sainte Anne Military Teaching Hospital (France). Malaria and dengue testing were performed in every patient presenting with fever, and all tests remained negative.
4. Discussion
To the best to our knowledge, ours is the first report describing a SARS Cov2 outbreak (the only one on board) in an austere environment during an uninterrupted Navy mission. The main hypothesis regarding crew contamination incriminates the Dakar stopover. Initial contamination from France was less likely; the first symptom occurred eleven days following departure from Europe, after a week of isolation. An U.K SARS Cov2 variant was identified once the mission ended and found to be endemic in France and Senegal. Kasper et al. provided details of the epidemic course on the U.S.S Theodore Roosevelt [4]. Conditions on board similar to ours were common: healthy and fit people, confined areas, and an austere environment. That said, more patients were involved. Similar elements were found in our analysis: rapid virus spreading on board, patient characteristics, and symptom distribution. More generally, confined areas play a major role in virus spreading and constitute a potential trigger for SARS Cov2 outbreak. While on the USS Roosevelt, Kasper and al. found a relationship between a higher risk of being infected in confined areas versus open areas, due to our small sample size we did not find any such relationship. In our study, the places noted as triggers for virus spreading were the smoking area and galleys (kitchens). A significant difference was found between attack rate among LHD crew and land army. Even if the shared locations were the same (meal time, fitness areas…), the LHD crew was more exposed than the other categories because of the tasks they had to fulfill throughout the mission. On the contrary, land activities were reduced during the outbreak. In crowded places, presymptomatic and asymptomatic persons’ role as SARS Cov2 carriers is all the more important, especially among the navy crew. As detailed on the flow chart, the number of non-infected cases has been presumed because the rate of asymptomatic cases was high, and massive screening occurred 10 days after a first patient was found to be infected; in addition, some rt PCR tests yielded negative results. The number of identified close contacts was not high because the definition was restricted, and many infected patients belonged to the same work team. Due to narrow passageways on board and close quarters, multiple physical contacts occurred, and close contact was in all likelihood underestimated.
Another SARS Cov2 outbreak occurred on the French aircraft carrier Charles de Gaulle. Bilicky et al. reported a posteriori that more than half of the crew members were infected, probably due to higher population density on aircraft than on LHDs [5]. Both of these outbreaks led to mission ending and were managed ashore in standard medical facilities. Serologic testing showed that 69 sailors (4%) were antibody-positive albeit never tested with rt-PCR. These results should draw the attention of all medical staff working in an austere environment.
Regarding the SARS Cov2 outbreak on LHD Dixmude, the main challenge was to adapt the hospital on board designed for the care of trauma patients, until it was possible to open up an area for Covid-19 patient isolation on another deck at a time when the medical staff was largely overwhelmed. On the other hand, a reinforced medical staff, a large on-board hospital, biological facilities and CT scan equipment create a setting more favorable to medical care than on other ships. In addition, personal protective equipment (PPE) is common among the French military [6], [7], it consists in goggle protection, long-sleeved water-resistant gowns and gloves, filtering facepiece FFP2, apron, head, and shoe cover. Notwithstanding this equipment, one of our caregivers presented an uncomplicated SARS Cov2 infection. Fortunately, our medical capacity was not reduced insofar as he could record medical data daily.
Antigen test kits are an attractive alternative way for Covid-19 testing despite their predictive positive value being weaker than that of rt-PCR [8]; resources are often scarce in austere environments, and antigen tests effectively contribute to SARS Cov2 screening and probably reduced virus spreading on board. The other advantage provided by rt PCR screening is the CT count, which can in some cases indicate an early or a late stage in the illness course. A second test can in theory be performed 48 hours later to indicate the stage, but we did not receive enough screening tests.
All told, SARS Cov2 vaccination might have prevented this outbreak. However, vaccine availability did not allow vaccination for the entire crew before the deployment. Moreover, while a longer period in quarantine could be more effective, it might mean that certain military operations would have to be suspended. It also bears mentioning that while daily doxycycline prophylaxis against malaria was constant during the outbreak, it did not prove effective against SARS Cov2, a result congruent with other studies [9]. As soon as the SARS Cov2 outbreak occurred, LHD Dixmude's crew set and implemented measures on board which consisted in closing shared locations (fitness, break areas), keeping face masks on at all times (except during sleep), twice-daily and intensive disinfection, continuous social distancing and staggered meal schedules. To minimize the risk of deploying with SARS Cov2 virus circulating on board, a 10-day isolation period was required for all crew members with positive rt-PCR SARS Cov2 test results. These measures were applied throughout the outbreak. The crew was sensitized by the medical staff to the need for early consultation in case of symptoms; this may have helped to contain the epidemic and allow LHD Dixmude to continue its mission.
As Nelson commented in an editorial [10], lessons from military experience are relevant to management of SARS Cov2 outbreaks in austere environment with rare medical supplies and could be applied in other contexts such as civilian cruises [11]. In any event, management in an austere environment with ongoing military operations close to a foreign country compelled us to adjust our medical care strategy in view of reducing both infection risk and operational risk. The military context is a major parameter. Critical Covid-19 patient evacuation would not have been easy to manage. Indeed, only a single helicopter allowing a 3-person load, which is no way designed to carry a Covid-19 patient requiring ventilation, was on board. In fact, at an early stage we evacuated two patients by air; they presented with shortness of breath and profound neutropenia. On this topic, critical Covid-19 patient evacuation has been performed on a similar French amphibious assault ship. In a case series, Nguyen et al. reported on the safety and feasibility of multiple critical Covid-19 patient evacuation [12]. The main difference with our study was a peacetime setting in inland waters; the aim was to deploy medical military prowess to help Corsican civilian healthcare and to manage critical Covid-19 patients; no military operations were at risk.
Our study has several limitations. First, our sample population is small, unvaccinated, and obviously restricted to a single site. That said, while ours is a retrospective study, no further research is needed to confirm our results; nowadays, any austere facility must be able to deal with a local SARS Cov2 outbreak. Especially during the first days of a mission, a bundle of global and personal measures must be followed, including screening of all symptomatic patients. To conclude, vaccination against Covid-19 among deployed militaries is now mandatory.
5. Conclusion
We have evoked military healthcare system adaptation in an austere and hostile environment. Keeping a SARS Cov2 outbreak under control remains a challenge for the medical staff. Our study assesses the feasibility of having it managed onboard. A few key findings should be borne in mind: it is essential to take invariant parameters such as closed spaces and close contact, scarce medical resources, and a military context with several ongoing operations into full account. With a standard bundle involving personal protective equipment, identification of infected patients, early quarantine for close contacts and SARS Cov2 testing for the entire crew, the Covid-19 epidemic curve decreased and the military operations were not put at risk. Today, SARS Cov2 vaccination is likely to provide further immunity for military operations and should pronouncedly decrease the Covid-19 infection risk.
Human and animal rights
The authors declare that the work described has not involved experimentation on humans or animals.
Informed consent and patient details
The authors declare that they obtained a written informed consent from the patients and/or volunteers included in the article and that this report does not contain any personal information that could lead to their identification.
Disclosure of interest
The authors declare that they have no competing interest.
Funding
This work did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributions:
Johan SCHMITT wrote the manuscript and provided patient care on board.
Emmanuel GENET provided patient care on board and helped to write the manuscript.
Marc DANGUY DES DESERTS helped to write the manuscript and made some corrections to figures.
Sophie CHAUVET ATIN and Pierre Julien CUNGI provided patient care on land and performed screening of the patients.
Philippe ARIES and Christophe GIACARDI helped to write the manuscript, and performed the analysis described within the methods section.
Sophie VELLIEUX provided patient care on board, and helped to write the manuscript.
Acknowledgement
None.
All authors declare that they had full access to all the data in the study and agree to submission journal.
References
- 1.World Health Organization. Coronavirus disease (Covid-19) outbreak. Available: https://www.who.int/emergencies/diseases/novel-coronavirus-2019.
- 2.Zhu N., Zhang D., Wang W., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gagliano A., Villani P.G., Co’FM, et al. COVID-19 epidemic in the middle province of northern Italy: impact, logistics, and strategy in the first line Hospital. Disaster Med Public Health Prep. 2020:1–5. doi: 10.1017/dmp.2020.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kasper M.R., Geibe J.R., Sears C.L., et al. An outbreak of Covid 19 on an aircraft carrier. N Engl J Med. 2020;383:2417–2426. doi: 10.1056/NEJMoa2019375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bilicky O., Paleiron N., Janvier F. An outbreak of Covid-19 on an aircraft carrier. N Engl J Med. 2021;384(10):976. doi: 10.1056/NEJMc2034424. [DOI] [PubMed] [Google Scholar]
- 6.Marolleau B., Rias M., Delahaye A., Aillet L., Weibel M., Romanat P. The military intensive care field hospital, a unique experience in the fight against Covid 19. Soins. 2020;65(849):22–27. doi: 10.1016/S0038-0814(20)30239-5. [DOI] [PubMed] [Google Scholar]
- 7.Danguy Des Deserts M., Mathais Q., Luft A., Escarment J., Pasquier P. Conception and deployment of a 30-bed field military intensive care hospital in Eastern France during the 2020 COVID-19 pandemie. Anaesth Crit Care Pain Med. 2020;39(3):361–362. doi: 10.1016/j.accpm.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirostu Y., Maejima M., Shibusawa M., et al. Comparison of automated SARS Cov-2 antigen test for COVID 19 infection with quantitative RT-PCR using 313 nasopharyngeal swabs, including from seven serially followed patients. Int J Infect Dis. 2020;99:397–402. doi: 10.1016/j.ijid.2020.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cavalcanti A.B., Zampieri F.G., Rosa R.G., et al. Hydroxychloroquine with or without Azithromycine in Mild-to-Moderate Covid-19. N Engl J Med. 2020;383(21):2041–2052. doi: 10.1056/NEJMoa2019014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Michael N.L. SARS Cov 2 in the US Military–Lessons for Civil Society. N Engl J Med. 2020;383(25):2472–2473. doi: 10.1056/NEJMe2032179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Earhart K.C., Beadle C., Miller L.K., et al. Outbreak of influenza in highly vaccination crew of US Navy ship. Emerg Infect Dis. 2001;7:463–465. doi: 10.3201/eid0703.010320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nguyen C., Montcriol A., Janvier F., et al. Critical COVID-19 patient evacuation on an amphibious assault ship: feasibility and safety. A case series. BMJ Mil Health. 2020;0:1–5. doi: 10.1136/bmjmilitary-2020-001520. [DOI] [PubMed] [Google Scholar]