Abstract
Dyslipidemia is a cardiovascular risk factor that is increasing in prevalence in the country. The need to treat and manage elevated cholesterol levels, both pharmacologic and non-pharmacologic, is of utmost importance. Different medical societies and groups bonded together to formulate the 2020 Philippine Clinical Practice Guidelines for dyslipidemia. The group raised nine clinical questions that are important in dyslipidemia management. A technical working group analyzed the clinical questions dealing with non-pharmacologic management, primary prevention for both non-diabetic and individuals with diabetes, familial hypercholesterolemia, secondary prevention, adverse events of statins and the use of other lipid parameters as measurement of risk for cardiovascular disease. Randomized controlled trials and meta-analyses were included in the GRADE-PRO analysis to come up with the statements answering the clinical questions. The statements were presented to a panel consisting of government agencies, members of the different medical societies, and private institutions, and the statements were voted upon to come up with the final statements of the 2020 practice guidelines. The 2020 CPG is aimed for the Filipino physician to confidently care for the individual with dyslipidemia and eventually lower his risk for cardiovascular disease.
Keywords: guidelines, dyslipidemia, cardiovascular prevention, familial hypercholesterolemia, diabetes mellitus
INTRODUCTION
The 2020 Clinical Practice Guidelines (CPG) for dyslipidemia is a collaboration of different stakeholders in the field of dyslipidemia, particularly the Philippine Heart Association (PHA), the Philippine Lipid and Atherosclerosis Society (PLAS), and the Philippine Society of Endocrinology, Diabetes, and Metabolism (PSEDM). Because of the different issues regarding special populations, the Philippine Society of Nephrology (PSN), Philippine Neurological Association (PNA), and the Philippine Pediatric Society (PPS) became part of this guideline formation. These guidelines are meant to provide physicians with a review of the latest available researches in the field of dyslipidemia to produce recommendations adaptable locally in the Philippines.
This is an update of the 2015 Clinical Practice Guidelines on the Management of Dyslipidemia in the Philippines (2015 CPG).1 The 2015 CPG covered topics on primary and secondary prevention, non-pharmacologic and pharmacologic treatment of dyslipidemia. When it was released, there were several questions on the management of special populations such as in kidney disease and the pediatric population. There were also issues on the adverse events of statin therapy. There were new clinical data that came out, particularly on ezetimibe, for secondary prevention that were not included in the 2015 CPG.
The objective of the 2020 CPG on Dyslipidemia is to provide evidence-based recommendations to effectively manage individuals with dyslipidemia. These recommendations aim to identify effective and feasible treatment regimens, both non-pharmacologic and pharmacologic, in dyslipidemia treatment.
METHODOlOGY
Experts in the fields of dyslipidemia, cardiology, endocrinology, pediatrics, neurology, nephrology and clinical epidemiology assembled to comprise the technical research committee (TRC). They reviewed the recommendations in the 2015 CPG,1 gathered questions frequently asked in lipid fora conducted in the past five years and discussed challenges in cholesterol management in the Philippines before proposing critical clinical questions to be answered by the 2020 CPG. These questions were presented to the steering committee for comments. Clinical questions were formulated by identifying the specific population, intervention and outcomes for each question. Systematic searches for relevant studies were carried out.
Various clinical outcomes were rated and ranked using the Grades of Recommendation, Assessment, Development and Evaluation (GRADE)2 categories of importance. The clinical outcomes were rated numerically on a 1-to-9 scale following the GRADE categories, where a score of 7-9 is critical; 4 -6 important; and 1- 3, of limited importance (Table 1). According to GRADE, ranking outcomes by their relative importance can help to focus attention on those outcomes that are considered most important and help to resolve or clarify disagreements.
Table 1.
Clinical outcomes used in 2020 Clinical Guidelines
| Clinical Outcomes | GRADE Category | Score |
|---|---|---|
| Total mortality | Critical | 9 |
| Cardiovascular death | Critical | 9 |
| Fatal and non-fatal myocardial infarction | Critical | 9 |
| Stroke or cerebrovascular disease | Critical | 9 |
| Major adverse CV events | Important | 7 |
| Coronary revascularization | Important | 6 |
CV, Cardiovascular; GRADE, Grading of Recommendations, Assessment, Development and Evaluations
Cardiovascular events were ranked as CRITICAL with a Score of 7. Coronary revascularization was assigned to be an IMPORTANT outcome with a GRADE PRO Score of 6. Additional important outcomes were added when deemed necessary for the particular clinical scenario (e.g., angina in ACS). Data on these six outcomes were extracted from the retrieved studies.
The TRC members also looked at the most common adverse events affecting individuals on statin treatment. The following outcomes were analyzed using the GRADE-PRO software and were given the following scores (Table 2).
Table 2.
Adverse events outcomes used in 2020 Clinical Guidelines
| Adverse Outcomes | GRADE Category | Score |
|---|---|---|
| Hepatotoxicity | Critical | 8 |
| Rhabdomyolysis | Critical | 8 |
| Hemorrhagic conversion | Important | 6 |
| New onset diabetes | Important | 6 |
| Myopathy | Important | 6 |
| Intracranial hemorrhage | Important | 6 |
| Elevated liver transaminases | Important | 6 |
| Risk of dementia | Low | 3 |
GRADE, Grading of Recommendations, Assessment, Development and Evaluations
The TRC searched for all published studies, both local and international, pertaining to the clinical questions, with the use of electronic search engines and manual search. The literature search was conducted using the search engines PubMed, Scopus, Medline, Google Scholar, Cochrane reviews and other medical engines using search words relevant to each clinical question. The cut-off date of the search was February 1, 2020. Unpublished data were also retrieved, whenever possible. To formulate the recommendations, the Working Group used randomized controlled trials (RCTs), meta-analyses, and systematic reviews of studies carried out in individuals with or without established coronary heart disease/CVD and with or without risk factors for coronary heart disease/CVD, and diagnosed with elevated blood cholesterol. Prospective cohorts relevant to the clinical questions are discussed but were not included in the GRADE-PRO analysis.
Standardized tables were used to present the quality of the evidence and key results in a transparent and reproducible fashion. The statements were presented to a panel of experts who voted as to the level of recommendation using the Modified Delphi technique.3 This technique utilizes consensus strategy that systematically uses literature review, opinion of stakeholders and judgment of experts within a field to reach an agreement. It relies on the collective intelligence of group of members resulting in increased content validity.
THE 2020 ClINICAl PRACTICE GUIDElINES
Clinical Question 1. Lifestyle Modifications
Among individuals with dyslipidemia, regardless of their present condition or risk profile, should lifestyle modification (i.e., reduced fat diet, smoking cessation, regular physical activity) be advised to reduce overall cardiovascular risk?
Statements
For individuals at any level of cardiovascular risk, a low-fat, low-cholesterol diet, rich in fruits and vegetables, is RECOMMENDED.
For individuals at any level of cardiovascular risk, cigarette smoking cessation is STRONGLY RECOMMENDED.
For individuals at any level of cardiovascular risk, e-cigarette smoking/vaping CESSATION IS RECOMMENDED.
For individuals at any level of cardiovascular risk, adequate exercise is RECOMMENDED.
The practice guidelines recommend that lifestyle change play a major role in the management of dyslipidemia. A low-fat, low-cholesterol diet is recommended. We recommend that the Filipino individual with dyslipidemia utilize the Pinggang Pinoy that is advocated by the Food Nutrition and Research Institute of the Department of Health. It is a serving plate where half of the portion is of green and leafy vegetables, one-fourth serving of meat and the rest are fiber-rich carbohydrates.
The guidelines also strongly recommend that patients should stop smoking. The use of vaping or e-cigarettes is also not recommended for individuals with dyslipidemia. Exercising at least 150 minutes per week at moderate to high-intensity is also recommended.
PRIMARY PREVENTION
Clinical Question 2.1. Individuals with no prior ASCVD
Among non-diabetic individuals without ASCVD but with multiple risk factors, should statin therapy be given?
Statement
For individuals without diabetes aged ≥45 years with LDL-C ≥130 mg/dL AND ≥2 risk factors*, without atherosclerotic cardiovascular disease, statins are RECOMMENDED for the prevention of cardiovascular events.
In the 2015 CPG1, we identified Risk Factor Counting as the method in identifying the risk of the Filipino individual for cardiovascular disease. We continue to recommend this as the available risk factor scores advocated by the different guidelines (e.g., ASCVD score) are not validated for Filipinos. The following risk factors were identified and if the individual has two (2) or more risk factors, (male sex, postmenopausal women, smoker, hypertension, BMI >25 kg/m2, family history of premature CHD, proteinuria, and left ventricular hypertrophy) the benefit for statin therapy in primary prevention is fulfilled and statin therapy is indicated.
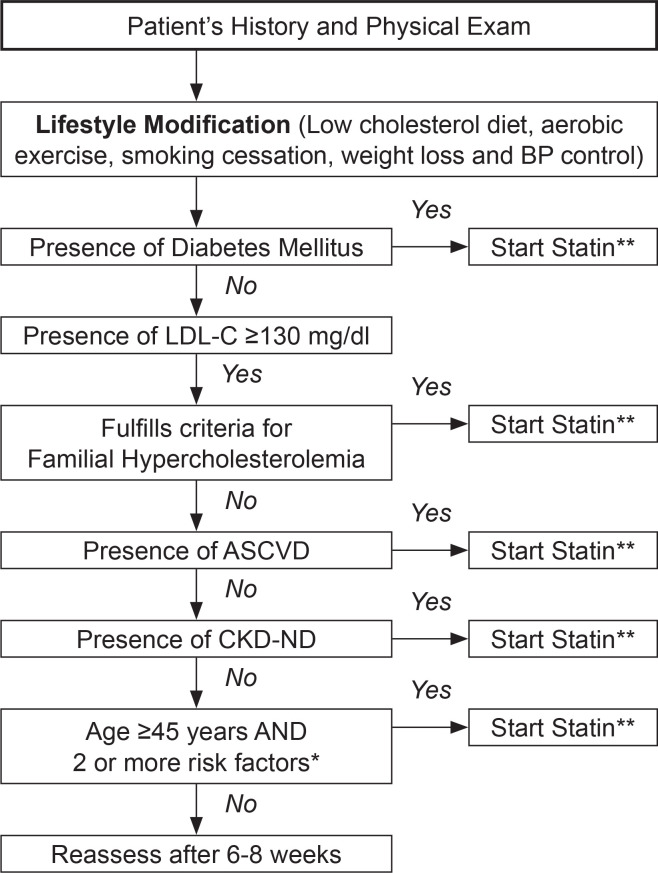
Figure 1 is a simplified algorithm that is advocated by the Philippine CPG in the management of dyslipidemia.
Figure 1.
Screening and treatment algorithm for the management of dyslipidemia.
Legend:
* Risk factors: male, smoker, hypertension ≥140/90 mmHg, BMI 25 kg/m2, family history of premature coronary heart disease, proteinuria, left ventricular hypertrophy and postmenopausal women
** The guideline recommends maximally-tolerated statin therapy to reach recommended target LDL-C levels
The use of statins for individuals with no clinical ASCVD (primary prevention) is recommended for patients aged 45 years and above with 2 or more risk factors with an LDL-C ≥130 mg/dL.
Clinical Question 2.2. Primary Prevention for Individuals with Diabetes Mellitus
Among individuals with diabetes without ASCVD, should statins be recommended?
Statement
For individuals with diabetes without evidence of ASCVD, statins are RECOMMENDED for primary prevention of cardiovascular events.
Evidence on the use of statins for primary prevention of cardiovascular outcomes were derived from 8 different clinical trials. The statin dose should be optimized to reach the LDL goal of less than 100 mg/dL for most persons with diabetes for primary prevention. For individuals with diabetes with >1 risk factor (refer to risk factors identified in primary prevention clinical question 2.1), LDL-C goal of less than 70 mg/dL is recommended. An LDL-C of <55 mg/dL should be attained for secondary prevention in individuals with diabetes who are at extremely high risk of having recurrent CV events due the previous occurrence of major cardiovascular events such as myocardial infarction, unstable angina or CVD (stroke).
Clinical Question 3. Familial Hypercholesterolemia
Among high risk individuals identified to have familial hypercholesterolemia, should statin therapy be initiated?
Statement
For individuals identified to have familial hypercholesterolemia, statin therapy is STRONGLY RECOMMENDED for the prevention of cardiovascular events.
Familial hypercholesterolemia (FH) is a dominantly inherited gene disorder resulting from gene mutations in the LDL-receptor pathway that cause markedly elevated LDL-C from birth. Untreated FH leads to premature death from coronary artery disease due to accelerated atherosclerosis. Early diagnosis and treatment are vital in prevention of CV events in this high-risk population (Dutch Lipid Network Criteria) (Table 3). The recommendations in this local guideline is to give statin therapy for all identified FH patients for primary prevention. For familial hypercholesterolemia, the recommended statin therapy is the high-intensity dose of statin, with a target LDL-C of less than <70 mg/dl in FH patients without target organ damage, and <55 mg/dl for FH individuals with target organ damage.
Table 3.
Dutch lipid network criteria on the diagnosis of heterozygous familial hypercholesterolemia4
| Criteria | Points |
|---|---|
| Family history | |
| First-degree relative with known premature* coronary and vascular disease, OR First-degree relative with known LDL-C level above the 95th percentile | 1 |
| First-degree relative with tendinous xanthomata and/or arcus cornealis OR Children aged less than 18 years with LDL-C level above the 95th percentile | 2 |
| Clinical history | |
| Patient with premature* coronary artery disease | 2 |
| Patient with premature* cerebral or peripheral vascular disease | 1 |
| Physical examination | |
| Tendinous xanthomata | 6 |
| Arcus cornealis prior to age 45 years | 4 |
| Cholesterol levels in mg/dl (mmol/liter) | |
| LDL-C ≥330 mg/dL (≥8.5) | 8 |
| LDL-C 250 – 329 mg/dL (6.5–8.4) | 5 |
| LDL-C 190 – 249 mg/dL (5.0–6.4) | 3 |
| LDL-C 155 – 189 mg/dL (4.0–4.9) | 1 |
| DNA analysis | |
| Functional mutation in the LDLR,b apo Bc or PCSK9d gene | 8 |
|
Diagnosis (diagnosis is based on the total number of points obtained) | |
| Definite familial hypercholesterolemia | >8 |
| Probable familial hypercholesterolemia | 6-8 |
| Possible familial hypercholesterolemia | 3-5 |
| Unlikely familial hypercholesterolemia | <3 |
Premature: ≤55 years in men; <60 years in women; LDL-C, low density lipoprotein cholesterol; FH, familial hypercholesterolemia; LDLR, low density lipoprotein receptor; Apo B, apolipoprotein B; PCSK9, proprotein convertase subtilisin/kexin type 9.
Clinical Question 4. Dyslipidemia in the Pediatric Population
Among pediatric population at risk for premature cardiovascular disease, should screening with fasting lipid profile be recommended?
Statement
Among pediatric population (≤19 years old) at risk for development of atherosclerosis and premature cardiovascular disease, screening with a fasting lipid profile is RECOMMENDED.
The screening for dyslipidemia in childhood is made on the basis of early identification and control of pediatric dyslipidemia that will reduce the risk and severity of cardiovascular disease (CVD) in adulthood (Table 4). There has been no solid evidence so far with regards the screening recommendation for dyslipidemia among the pediatric age group. In this CPG, the screening guidelines that have been suggested are the following: Selective screening for those at risk. Universal screening to identify those with risk factors for familial hypercholesterolemia at 9-11 years old and 17-21 years old.
Table 4.
| Traditional Risk Factors | Other conditions |
|---|---|
| Dyslipidemia |
|
| Obesity |
|
| Diabetes mellitus (Type 1 or 2) |
|
| Hypertension |
|
| Family history of premature CVD |
|
| Smoke exposure |
|
| |
| |
| |
|
CVD, cardiovascular disease; HIV, human immunodeficiency virus
Clinical Question 5. Individuals with Chronic Kidney Disease
Among individuals with chronic kidney disease who are not on dialysis, should statins be given to reduce CV risk?
Statement
Among individuals with chronic kidney disease who are not on dialysis, statins are RECOMMENDED for the prevention of cardiovascular events.
Dyslipidemia is common but not universal in CKD. Kidney dysfunction leads to a profound dysregulation of lipoprotein metabolism, resulting in multiple lipoprotein abnormalities. The recommendation in this local guideline is to give statins for individuals with CKD not on dialysis. For individuals who are on renal replacement therapy and post-transplant, this local guideline recommends referring patients to nephrologists for lipid management.
SECONDARY PREVENTION
Clinical Question 6. Individuals with Acute Coronary Syndrome
Among individuals with acute coronary syndrome (ACS), should statins be given?
Statements
For individuals with ACS, early high-intensity statin that is maximally-tolerated is RECOMMENDED and should not be discontinued.
Statins should be given to ACS patients immediately
Timing of therapy is critical among patients with acute coronary syndrome. Early intervention is advocated to optimize recovery and minimize complications. The adage “time is muscle,” is based on the principle of the necessity for immediate action during the golden period in which myocardial ischemic damage is still potentially reversible or myocyte necrosis can still be contained and much of the myocardium in the ischemic penumbra can still be salvaged.
Evidence on the appropriate statin intensity for secondary prevention in individuals with ASCVD were obtained from four (4) trials7-10 that compared varying statin regimens. High-intensity statins reduce LDL-C by >50% compared to low-intensity statins which reduce LDL-C by less than 30% (Table 5).
Table 5.
Statin treatment intensity
| Treatment intensity | % lDl-C reduction | Drug regimen |
|---|---|---|
| Low intensity | <30 % | Fluvastatin 20 - 40 mg |
| Pravastatin 10 - 20 mg | ||
| Simvastatin 10 mg | ||
| Moderate intensity | 30% - 50% | Atorvastatin 10 - 20 mg |
| Fluvastatin 80 mg | ||
| Rosuvastatin 5 - 10 mg | ||
| Simvastatin 20 - 40 mg | ||
| Pravastatin 40 - 80 mg | ||
| Pitavastatin 2 - 4 mg | ||
| High intensity | >50% | Atorvastatin 40 - 80 mg |
| Rosuvastatin 20 - 40 mg | ||
LDL-C, low density lipoprotein cholesterol
NON-STATIN THERAPY
Clinical Question 7.1. Use of Ezetimibe
Among individuals with ASCVD, should ezetimibe be given on top of statin therapy?
Statement
For individuals with documented ACS, and target LDL-C has not been reached despite maximallytolerated high-intensity statin therapy, ezetimibe may be added on top of statin therapy to get to goal LDL-C.
Ezetimibe is an important adjunct medication in lowering LDL-C in the body. This guideline recommends that ezetimibe be given to patients with documented ACS on maximally tolerated statin therapy not at goal LDL-C levels.
Clinical Question 7.2. Use of Fibrates
Among individuals with ASCVD, should fibrates be given on top of statin therapy once LDL-C goal is achieved?
Statements
Among individuals without diabetes not at goal LDL-C, routinely adding fibrates on top of statin therapy is NOT RECOMMENDED for primary or secondary prevention of cardiovascular disease.
Among individuals with diabetes, routinely adding fibrates on top of statin therapy is NOT RECOMMENDED for primary or secondary prevention of cardiovascular disease.
However, adding fibrates to statins may be considered among MEN with controlled diabetes, low HDL-C (<35 mg/dl) and persistently high triglycerides (>200 mg/dl) for prevention of CV disease.
Clinical Question 7.3. Use of Omega Fatty Acids
Among individuals with ASCVD, should omega fatty acids be given on top of statin therapy once LDL-C goal is achieved?
Statements
Among individuals with ASCVD, omega fatty acids (EPA+DHA) given on top of statin therapy is NOT RECOMMENDED.
Among individuals with ASCVD on statin therapy at goal LDL-C, but with persistently high triglyceride levels of 150-499 mg/dl, omega fatty acids (pure EPA) MAY be given.
FOUR PATIENT GROUPS
The 2020 CPG recommends that individuals be divided into four patient groups (Table 6). The cholesterol targets are based on clinical data and expert opinions of the voting panel.
Table 6.
Cholesterol targets for different patient groups
| Patient Groups | lDl-C Target | hDl-C Target | Triglyceride Target |
|---|---|---|---|
| Individuals with no clinical ASCVD | <130 mg/dL | >40 mg/dl in males / >50 mg/dl in females | <150 mg/dl |
| Individuals with DM | <100 mg/dL | >40 mg/dl in males / >50 mg/dl in females | <150 mg/dl |
| With ≥1 risk factors / target organ damage | <70 mg/dL | ||
| With ASCVD | <55 mg/dL | ||
| Individuals with clinical ASCVD | <55 mg/dL | 40 mg/dl in males / >50 mg/dl in females > | <150 mg/dl |
| FH without ASCVD or without major risk factor / target organ damage | <70 mg/dL | 40 mg/dl in males / >50 mg/dl in females > | <150 mg/dl |
| FH with ASCVD or with ≥1 risk factors / target organ damage | <55 mg/dL |
ASCVD, atherosclerotic cardiovascular disease; DM, diabetes mellitus; FH, familial hypercholesterolemia
STATIN ADVERSE EVENTS
Clinical Question 8. Use of Statin Therapy
-
Among individuals taking statin therapy, what is the risk of developing adverse effects?
Statin-associated Muscle Symptoms
New-onset Diabetes
Dementia / cognitive dysfunction / intracerebral hemorrhage
Statements
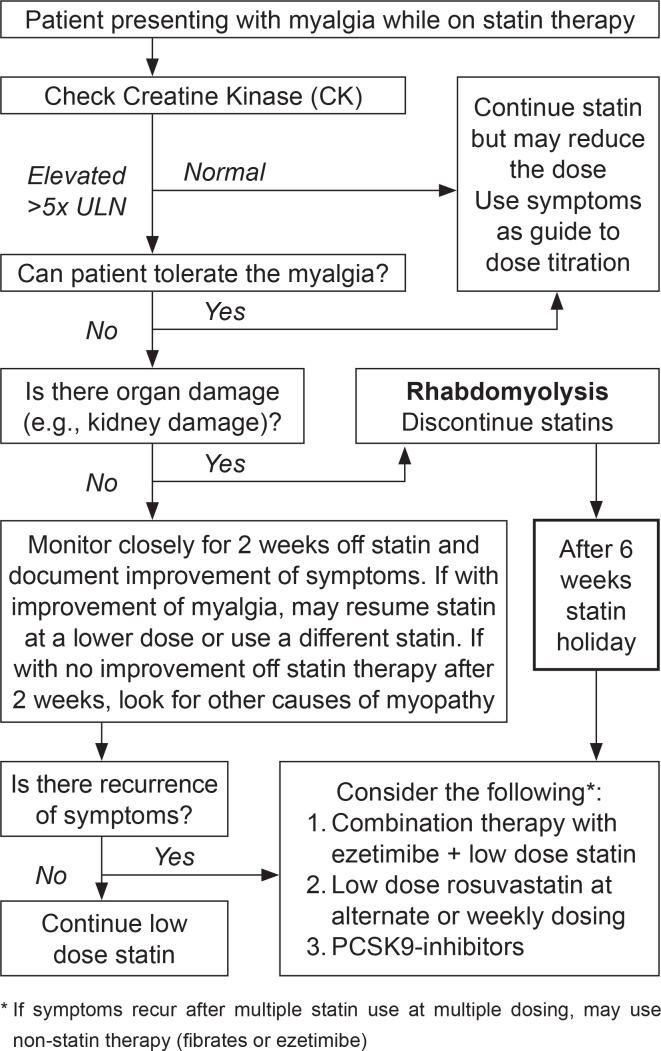
Treatment with statins is associated with a low risk of developing statin-associated muscle symptoms (SAMS), but the benefits of cardiovascular risk reduction outweigh the risk (Figure 2).
Treatment with statins is associated with an increased risk of new-onset diabetes mellitus, but the benefits of statin treatment for cardiovascular risk reduction outweigh the risk.
Treatment with statins is not associated with the development of dementia and cognitive dysfunction
Treatment with statins is not associated with an increased risk of intracerebral hemorrhage
Figure 2.
Algorithm for Statin-induced Myopathy.
ADDITIONAl TARGETS TO REDUCE CARDIOVASCUlAR RISK
Clinical Question 9.1. Use of non-HDL-C
Among individuals on statin therapy who have achieved their LDL-C goal, should non-high density lipoprotein cholesterol (non-HDL-C) be used as additional target to reduce CV events?
Statement
Among individuals on statin therapy who have achieved their LDL-C goal, an elevated computed non-HDL-C may be used as an additional therapeutic target to further reduce CV events.
Non-HDL-C is the difference between the total cholesterol levels and HDL-C and quantifies all atherogenic lipoprotein particles. Target non-HDL in various guidelines set it as 30 mg/dL above target LDL-C. In patients with atherogenic dyslipidemia such as those with metabolic syndrome, type 2 diabetes mellitus and obesity, non-HDL-C determination is recommended as an additional tool providing a better estimate of risk beyond LDL-C. The non-fasting HDL computation has prognostic value in clinical trials as a therapeutic target.
Clinical Question 9.2. Use of Apolipoprotein B-100
Among individuals on statin therapy who have achieved their LDL-C goal, should apolipoprotein B-100 be used as additional target to reduce CV events?
Statement
Among individuals on statin therapy who have achieved their LDL-C goal, an elevated apolipoprotein B-100 may be used as an additional therapeutic target to further reduce CV event.
limitations of the Guidelines
Several limitations were encountered during the process of creating the 2020 CPG. The evidence obtained from the trials only involved randomized controlled trials and some meta-analyses. Observational studies were only used as references. This approach, however, resulted in a comprehensive set of evidence-based clinical recommendations. The clinical trials did not include Filipino patients, thus analysis and grading of evidence were downgraded. Thus, we can only RECOMMEND the statements in this guideline. We hope in the future that more clinical trials be made with Filipino patients as subjects.
CONCLUSIONS
The clinical statements were made by the TRC and the recommendations revolve around the holistic management of dyslipidemia. Lifestyle modification should be recommended to all patients regardless of their CVD risk. Dosing of statin therapies should be based on individual risk factors. We recommend a lower LDL-C target, particularly for secondary prevention. The simplified algorithm was provided to serve as a quick reference in the management of dyslipidemia for clinicians.
The 2020 CPG is designed to be a guide for clinicians in managing dyslipidemia for the Filipino patient. This, however, should not replace sound clinical judgment by doctors and the ultimate decision for treatment should involve both clinician and the patient.
Acknowledgments
The authors would like to express their gratitude to the members of the steering committee and the representatives of the different medical organizations who comprised the expert panel, for their valuable inputs during the creation of the guidelines.
Steering Committee:
Adriel Guerrero (Philippine Lipid and Atherosclerosis Society)
Gilbert Villela (Philippine Heart Association)
Jeremy Jones Robles (Philippine Society of Endocrinology, Diabetes and Metabolism) Maaliddin Biruar (Philippine Society of Nephrology)
Roberto Mirasol (Philippine Lipid and Atherosclerosis Society)
Romeo Esagunde (Philippine Neurological Association)
Expert Panel
Leilani Asis (Philippine Society of Hypertension)
Federick Cheng (Philippine Lipid and Atherosclerosis Society)
Michael Villa (Philippine Society of Endocrinology, Diabetes and Metabolism)
Arlene Afaga (Philippine Society of Nephrology)
Encarnita Limpin (Philippine College of Physicians)
Nemencio Nicodemus, Jr. (Philippine College of Physicians)
Florence Santos (Philippine Medical Association)
Jennifer Manzano (Philippine Neurological Association)
Ma. Bernadette Azcueta (Philippine Pediatric Society)
Jane Eflyn Bunyi (Philippine Academy of Family Physicians)
Emma Gaspar Trinidad (Philippine Heart Association)
Mildred Udarbe (Food and Nutrition Research Institute)
Romeo Merino (Manila Doctors Hospital)
Mark Anthony Cepeda (Philippine Health Insurance) [Non-voting]
Statement of Authorship
All authors certified fulfillment of ICMJE authorship criteria.
Author Disclosure
Drs. Imelda Caole-Ang, Maria Margarita Balabagno, Agnes Baston, Ruzenette Felicitas Hernandez, Ma. Cristina Macrohon-Valdez and Maria Theresa Rosqueta have nothing to disclose.
Dr. Lourdes Ella Gonzalez-Santos reports personal fees from LRI-Therapharma, Sanofi-Aventis, Servier Philippines, Merck Sharpe and Dohme, Astra Zeneca, Menarini, Novartis, Natrapharm, Pascual, Amgen; research grant from Cardinal Santos Medical Center, outside the submitted work.
Dr. Raymond Oliva reports connection to Astellas Pharma Philippines, outside the submitted work.
Dr. Cecilia Jimeno is the Vice Editor-in-Chief of JAFES; reports speaking engagements from Natrapharm, Novartis, Servier Philippines, LRI-Therapharma; CME grant from OEP, Cathay; Advisory board of MSD, outside the submitted work.
Dr. Eddieson Gonzales reports personal fees for module development from Gertz Pharma; speaking engagements from Menarini, OEP, Zydus, Ajanta, Astra Zeneca, Servier Philippines, Novartis and research grants from Innogen and Cathay Drug, outside the submitted work.
Dr. Deborah Ona reports speaking engagements from Upjohn, Astra Zeneca, Sanofi, Servier, MSD, outside the submitted work.
Dr. Jude Erric Cinco reports personal fees from LRI-Therapharma, Pfizer, Getz Pharma, Abbott, Marcburg, Sanofi Aventis, Corbridge, D`elex Pharma, outside the submitted work.
Dr. Mia Fojas reports personal fees as Advisory Board for Abbott; Speakers’ Bureau for Pfizer and MSD; CME grant from OEP; module development for Innogen, outside the submitted work.
Dr. Felix Eduardo Punzalan reports personal fees for speaking engagements from Sanofi-Aventis, Servier Philippines, Aspen, Novartis; Advisory board of Merck Sharpe and Dohme and GX Pharma, outside the submitted work.
Dr. Elmer Jasper Llanes reports research grants and honorarium from LRI-Therapharma, Orient Europherme and Natrpaharm; honorarium from Servier Philippines, Astra Zeneca and Merck Sharpe and Dohme, outside the submitted work.
Funding Source
Funding for this 2020 CPG is through a grant from PLAS, PHA, PSEDM, PPS, PSN and PNA.
References
- 1.Philippine Lipid and Atherosclerosis Society / Philippine Heart Association / Philippine Society of Endocrinology, Diabetes and Metabolism . 2015 Clinical Practice Guidelines for the Management of Dyslipidemia in the Philippines. https://www.philheart.org/index.php/guidelines/142-dyslipidemia-guidelines. Accessed February 1, 2020.
- 2.GRADE your evidence and improve your guideline in development in health care. https://gradepro.org
- 3.Eubank Breda, Mohtadi NG, Lafve MR, et al. Using the modified Delphi method to establish clinical consensus for the diagnosis and treatment of patients with rotator cuff pathology. BMC Med Res Methodol. 2016;16:56. PMID: . PMCID: . 10.1186/s12874-016-0165-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pijlman A, Huijgen R, Verhagen SN, et al. Evaluation of cholesterol lowering treatment of patients with familial hypercholesterolemia: A large cross-sectional study in The Netherlands. Atherosclerosis. 2010;209(1):189–94. PMID: . 10.1016/j.atherosclerosis.2009.09.014. [DOI] [PubMed] [Google Scholar]
- 5.Expert Panel on Integrated Guidelines for cardiovascular health and risk reduction in children and adolescents, National Heart, Lung and Blood Institute. Expert panel on integrated guidelines for cardiovascular health and risk reduction in children and adolescents: Summary report. Pediatrics. 2011;128 (Suppl 5):S213-56. PMID: . PMCID: . 10.1542/peds.2009-2107C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bamba V. Update on screening, etiology, and treatment of dyslipidemia in children. J Clin Endocrinol Metab. 2014;99(9):3093-102. PMID: . 10.1210/jc.2013-3860. [DOI] [PubMed] [Google Scholar]
- 7.Armitage J, Bowman L, Wallendszus K, et al. Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12,064 survivors of myocardial infarction: A double-blind randomised trial. Lancet. 2010; 376(9753):1658-69. PMID: . PMCID: . 10.1016/S0140-6736(10)60310-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Lemos JA, Blazing MA, Wiviott SD, et al. Early intensive vs a delayed conservative simvastatin strategy in patients with acute coronary syndromes: Phase Z of the A to Z trial. JAMA. 2004;292(11): 1307-16. PMID: . 10.1001/jama.292.11.1307. [DOI] [PubMed] [Google Scholar]
- 9.LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352(14):1425-35. PMID: . 10.1056/NEJMoa050461. [DOI] [PubMed] [Google Scholar]
- 10.Pedersen TR, Faergeman O, Kastelein JJ, et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: The IDEAL study: A randomized controlled trial. JAMA. 2005;294(19):2437-45. PMID: . 10.1001/jama.294.19.2437. [DOI] [PubMed] [Google Scholar]