Abstract
Background:
Bone contusions are commonly observed on magnetic resonance images (MRIs) in individuals who have sustained a non-contact anterior cruciate ligament (ACL) injury. Time from injury to image acquisition affects the ability to visualize these bone contusions, as contusions resolve with time.
Purpose:
To quantify the number of bone contusions and their locations (lateral tibial plateau (LTP), lateral femoral condyle (LFC), medial tibial plateau (MTP), and medial femoral condyle (MFC)) observed on MRIs of non-contact ACL injured knees acquired within 6 weeks of injury.
Study Design:
Descriptive laboratory study
Methods:
We retrospectively reviewed clinic notes, operative notes, and imaging of 136 subjects undergoing ACL reconstruction. The following exclusion criteria were applied: MRIs acquired beyond 6 weeks post-injury, contact ACL injury, and prior knee trauma. Fat-suppressed fast spin-echo T2-weighted MRIs were reviewed by a blinded musculoskeletal radiologist. The number of contusions and their locations (LTP, LFC, MTP, and MFC) were recorded.
Results:
Contusions were observed in 135 of 136 subjects. Eight subjects had one contusion (6%), 39 had two (29%), 41 had three (30%), and 47 had four (35%). The most common contusion patterns within each of these groups were 6 with LTP (75%) for one contusion, 29 with LTP/LFC (74%) for two contusions, 33 with LTP/LFC/MTP (81%) for three contusions, and 47 with LTP/LFC/MTP/MFC (100%) for four contusions. No sex differences were detected in contusion frequency in the four locations (p > 0.05). Among the included subjects, 50 had medial meniscal tears (37%) and 52 had lateral meniscus tears (38%).
Conclusions:
The most common contusion patterns observed were four locations (LTP/LFC/MTP/MFC) and three locations (LTP/LFC/MTP).
Clinical Relevance:
Data quantifying the frequency of different bone contusion patterns may be important to elucidating non-contact ACL injury mechanisms.
INTRODUCTION
The mechanisms leading to non-contact anterior cruciate ligament (ACL) injury have long been debated 5,23,36,37. With the increase in athletic participation of young children and females 24, ACL injury rates have also increased 1,29,52. This injury is a growing public health concern due to its immediate effects 32,38,43, the high cost of treatment 17, and its long-term sequelae, which include the early-onset of osteoarthritis (OA) 2,13,27,39. Currently, treatment options include ACL reconstruction or repair, physical rehabilitation, or both. However, the increased risk of early-onset OA remains regardless of treatment 27,46.
Although approximately $100 million is spent annually on prevention research 24, ACL injury rates remain high 1,52. The efficacy of prevention programs may be improved by better understanding the mechanisms of injury, which remain controversial. For example, valgus collapse is thought to be a main contributor to non-contact ACL injuries 6,18,19,23. However, another theory for how ACL injuries occur is landing on an extended knee 9,22,34. As strain in the ACL increases with knee extension 9,10,14, landing on an extended knee may put the ACL at high risk of rupture. Another mechanism of injury known as the contrecoup mechanism 21 has also been proposed. This mechanism involves anterior translation as the femur rotates externally, with the posterior aspect of the lateral tibial plateau making contact with the midportion of the lateral femoral condyle. The countercoup impact then occurs as the knee reduces and the medial compartments of the femur and tibia make contact 21. It is evident from the literature that there are a number of theories describing the non-contact injury mechanism, and it is possible that there may be more than one mechanism. Thus, it is imperative that more research is conducted to elucidate these injury mechanisms to improve prevention programs.
Bone contusions have emerged as a magnetic resonance imaging (MRI) marker of the impact between the femur and tibia occurring around the time of injury 16,45,48. Bone contusions are believed to result from increased inflammation, edema, and microtrabecular fractures in the subchondral bone caused by bone contact 16,28,40,45,50. Studies have hypothesized that lateral bruising is indicative of valgus collapse 21,40,45,47, and medial bruising is representative of extension and anterior tibial translation 48,49. However, it is difficult to predict injury mechanisms from static planar MR images alone.
In order to quantify the position of the knee near the time of injury from MR images, previous work used numerical optimization to position 3D anatomic models of the femur and tibia such that the overlap between the tibiofemoral bone contusions was maximized 22,34. This method predicted that the knee was positioned near extension, and indicated that a large anterior tibial translation occurred near the time of injury22,34. Furthermore, no significant differences were found between males and females in any of the kinematic variables measured 34. Importantly, these studies 22,34 investigated bone contusion patterns that involved the lateral tibial plateau (LTP), medial tibial plateau (MTP), lateral femoral condyle (LFC), and medial femoral condyle (MFC). However, it is unclear how common this bone bruise pattern occurs. For example, while some reports have focused on the presence of lateral compartment bone contusions 7,47,51, more recent studies have suggested that medial contusions occur at a higher frequency than previously described 48,49. One important factor that may influence the presence of bone contusions on MRI is the time from injury to MRI acquisition 16,48, as the bone contusions may resolve with time. Specifically, there remains a need to quantify the frequency of bone contusions patterns within a short time frame from non-contact ACL injury16,48. Therefore, the purpose of this study was to quantify the number of bone contusions and their locations (LTP, MTP, LFC, and MFC) observed on MRIs of non-contact ACL injured knees within 6 weeks of injury.
METHODS
Following IRB approval, clinic notes, operative notes, and medical imaging (arthroscopic and MRI) were reviewed from subjects who had undergone ACL reconstruction between January 2010 and December 2013 by two fellowship-trained sports medicine orthopaedic surgeons. From the initial 236 subjects identified, the following exclusion criteria were applied: 1) MRIs acquired more than 6 weeks after injury, 2) contact ACL injury, 3) associated MCL tears, 4) history of ACLR or meniscal surgery, 5) previous knee trauma, 6) full thickness degenerative cartilage loss, 7) presence of rheumatoid arthritis or osteoarthritis, or 8) MRIs performed at another institution. Our intent was to include a sample size that met or exceeded that of previous studies that have quantified bone contusion patterns 25,49.
The type of injury (contact or non-contact) was determined by the initial clinical evaluation and history. The time between injury and MRI acquisition was noted via review of clinic notes, MRI reports, and operative notes. Fast spin-echo T2-weighted imaging parameters were as follows on a 1.5T MRI scanner (Signa, GE Healthcare): repetition time (TR) of 4000 ms, echo time (TE) of 70 ms, field of view (FOV) of 16 cm, matrix of 256×192 interpolated to 512×512 for display, number of excitations (NEX) of 2, slice thickness of 4 mm, and interslice gap of 0.4 mm. Fat saturation was used on all sequences, and all images were obtained in a knee coil.
The presence and location of contusions were determined by a musculoskeletal radiologist who was blinded to the purpose of the study. Contusions were defined as a focal or regional increase in signal intensity on these fat-saturated T2-weighted images in the bone marrow. The locations of contusions (Figure 1) were recorded categorically within each compartment, including the lateral tibial plateau (LTP), medial tibial plateau (MTP), lateral femoral condyle (LFC), and medial femoral condyle (MFC). Based on inclusion criteria, contusions caused by avulsions of ligaments were not considered in this study. Subjects were grouped according to the number of bone contusions (zero to four) present on MRI, as well as the location of the contusions. Furthermore, each compartment was divided into thirds in the anteroposterior direction and the location of the bone contusion within these thirds was noted. Additionally, medial or lateral meniscus tears were confirmed intraoperatively and recorded.
Figure 1:
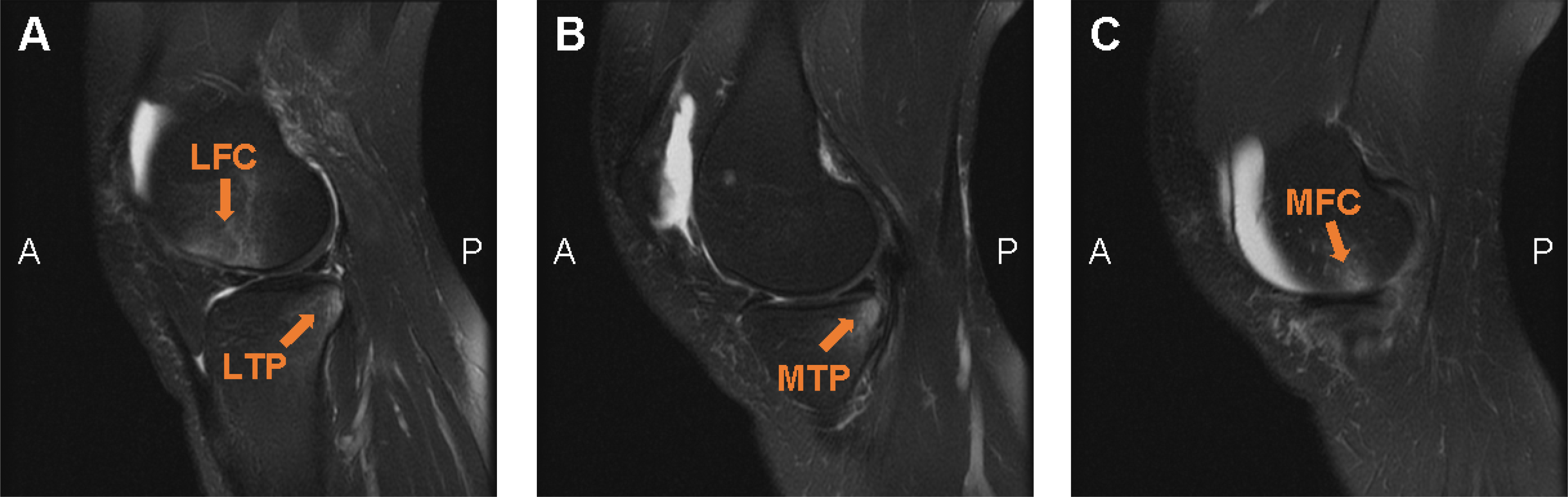
Representative T2 MR images (adapted from a previous study22) from a subject with a four contusion pattern, showing contusions (orange arrows) in the (A) LFC and LTP, (B) MTP, and (C) MFC. LFC = lateral femoral condyle. LTP = lateral tibial plateau. MTP = medial tibial plateau. MFC = medial femoral condyle. A = anterior. P = posterior.
The mean number of days between injury and MRI was compared across the groups with one, two, three, or four contusions using a single-factor analysis of variance. Sex differences among the contusion locations were determined using Chi-square tests for frequency (LFC, MFC, and MTP locations) and Fisher’s exact test as appropriate (LTP location). Differences were considered statistically significant where p < 0.05.
RESULTS
From January 2010 to December 2013, there were 236 ACL reconstructions performed by the two orthopaedic surgeons participating in this study. Of the 236 subjects, 100 subjects were excluded (51 had more than 6 weeks between the time of injury and MRI; 18 had associated degenerative joint disease; 18 had contact injuries; 7 had MRIs performed at external institutions; 3 had grade 2 or 3 MCL tears; 2 had chronic ACL tears; 1 had a prior meniscectomy). The remaining 136 subjects (58% of those screened) met the inclusion criteria. This group consisted of 54 males (mean age: 19 ± 4 years, range: 12 – 36 years) and 82 females (mean age: 18 ± 5 years, range: 13 – 40 years). The mean age for the entire group was 18 ± 5 years. The activities these subjects participated in during the injury were most commonly soccer, basketball, and football. The full list of sports by sex is given in Table 1. With regard to meniscal tears, 50 of the 136 included subjects (37%) had medial meniscus tears and 52 subjects had lateral meniscus tears (38%).
Table 1:
Activity During ACL Injury by Sex
| Activity | M (N = 54) | F (N = 82) | M+F (N = 136) |
|---|---|---|---|
| Soccer | 12 | 40 | 52 |
| Basketball | 15 | 17 | 32 |
| Football | 15 | 0 | 15 |
| Ultimate frisbee | 3 | 3 | 6 |
| Volleyball | 1 | 5 | 6 |
| Other | 1 | 3 | 4 |
| Lacrosse | 2 | 1 | 3 |
| Rugby | 2 | 1 | 3 |
| Field hockey | 0 | 2 | 2 |
| Gymnastics | 0 | 2 | 2 |
| Kickball | 0 | 2 | 2 |
| Skiing | 0 | 2 | 2 |
| Snowboard | 1 | 1 | 2 |
| Dance | 0 | 1 | 1 |
| Motocross | 1 | 0 | 1 |
| Racquet ball | 1 | 0 | 1 |
| Softball | 0 | 1 | 1 |
| Tennis | 0 | 1 | 1 |
The frequency and pattern of bone contusions according to compartment are shown in Figure 2. Only one subject’s MRI showed no contusions. Eight of the 136 subjects (6%) had only one bone contusion, all of which were in the lateral compartment: two (25%) were located on the LFC and six (75%) were on the LTP. The MRIs from 39 of the subjects (29%) showed two contusions in all six possible paired combinations of compartments. The most common pattern among two contusions was LTP/LFC (29 of 39 = 74%), followed by five subjects with LTP/MTP (13%), two with LTP/MFC (5%), two with MFC/LFC (5%), one with MTP/LFC (3%), and none with MFC/MTP (0%). A total of 41 subjects (30%) had three contusions, of which the most common pattern was LTP/LFC/MTP (33 of 41 = 81%). The remaining three contusion patterns comprised of LTP/LFC/MFC (7 subjects = 17%) and LTP/MFC/MTP (1 subject = 2%). Finally, 47 subjects (35%) had contusions in all four compartments. We did not detect significant differences in the average time between injury and MRI among the one to four bone contusion groups, with an average of 8 days for the zero contusion group, 15 days for the one contusion group, 18 days for the two contusion group, 14 days for the three contusion group, and 15 days for the four contusion group. The frequencies of contusions in each of the four compartments in males and females are reported in Table 2. No significant differences were noted in the frequencies of bone contusion compartments between males and females.
Figure 2:
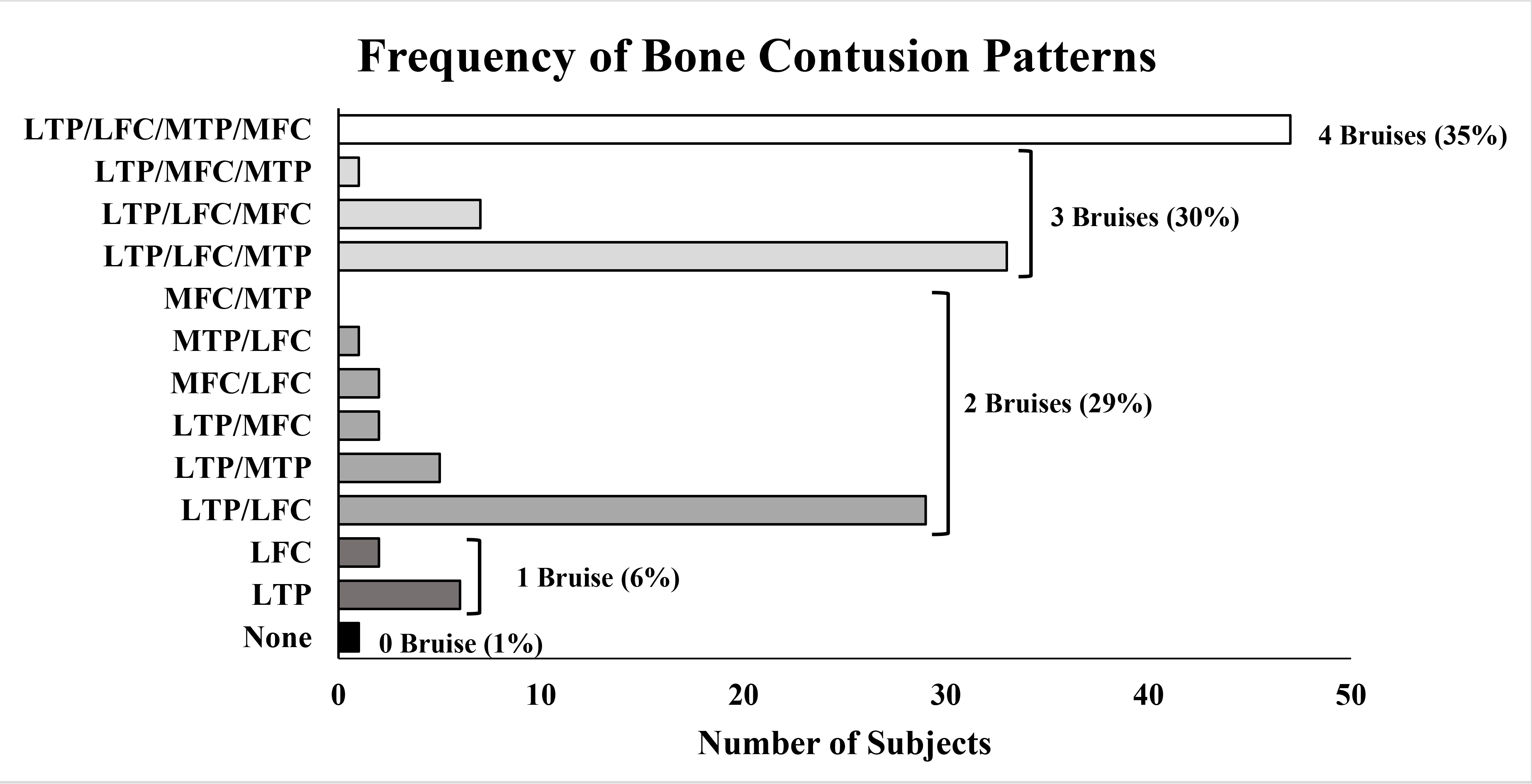
Frequency of bone contusion patterns by number of subjects. Patterns are also grouped by number of contusions (bruises). Percentages may not sum to 100 due to rounding.
Table 2:
Contusion Frequency by Compartment and Sex
| Compartment | Female Frequency (%) | Male Frequency (%) | P-value |
|---|---|---|---|
| LTP | 96 | 94 | 0.7 |
| LFC | 89 | 89 | 1.0 |
| MTP | 66 | 61 | 0.6 |
| MFC | 40 | 48 | 0.4 |
LTP = lateral tibial plateau. LFC = lateral femoral condyle. MTP = medial tibial plateau. MFC = medial femoral condyle.
All contusions were located primarily in the subchondral region. LTP and MTP contusions were all in the posterior third of their respective regions. LFC and MFC contusions were all centrally located in the anteroposterior direction within each compartment.
DISCUSSION
Bone contusions observed on MRI are frequently associated with ACL injury 16,20,25,35,36,45,48,49. These contusions may occur due to impact between the femur and tibia near the time of non-contact ACL injury, and therefore may provide insight into the position of the knee at the time of injury 41. In this study, we examined the number of bone contusions and their locations (LTP, LFC, MTP, and MFC) observed on MRIs of non-contact ACL injured knees within 6 weeks of injury. This is important because contusions fade with time from injury 16,48. Importantly, we found that patients with three and four bone contusions comprised 65% of those who were imaged within 6 weeks of non-contact ACL injuries.
In the present study, we observed a high frequency of medial compartment bruising in addition to lateral compartment bruising. Specifically, we observed a frequency of medial compartment bruising of 72% of subjects. This finding is congruent with a recent study which found medial compartment bruising in 42.5% of the femoral condyles and 61.6% of the tibial plateaus assessed 49. Additionally, another study noted that approximately 40% of femoral condyles and 60% of tibial plateaus had medial bruising 48. These findings are in contrast to several earlier publications, which noted mostly lateral compartment contusions 16,31,45 and described minimal frequency of medial compartment contusions (ranging between 19% and 35%) 7,47,51. However, in these previous studies, it is unclear whether imaging was performed within 6 weeks of injury. As bone contusions are likely to resolve with increased time from injury 16,48, it is likely important to consider the time between injury and MRI when assessing presence and location of bone contusions. Regardless of contusion site, the volume of contusions present on MRIs decreases as time from injury increases 8. Therefore, larger and more severe contusions, which occur more commonly in the lateral compartments 44, may persist longer than the typically less severe medial contusions. Thus, differences between the present study’s and prior studies’ findings 16,31,45 may be due to differences in the time from injury that the MRIs were acquired.
Additionally, we found that nearly all (99%) of the 136 subjects with non-contact ACL injury exhibited bone contusions on MRIs, which is similar to what has been reported previously 4,33,51. The present study also found a high proportion involving three or four bone contusions (88 of 136 = 65%) (Figure 2). This finding is similar to that of a previous study, which also quantified the frequency of contusion patterns by compartment (medial, lateral) and surface (tibial plateau, femoral condyle). This study 25 found that three or four contusions were observed in nearly half of their subjects (40 of 81 = 49%). However, contusions were observed in all four compartments in only 11% of subjects, while the present study found that the four compartment bruising pattern was the most common, occurring in 35% of subjects. These differences may also be due to the present study requiring that the time between injury and MRI acquisition to be within 6 weeks.
Variability in reported bone contusion pattern frequencies 12,53 may stem from several other factors in addition to time from injury. For instance, differences in MRI sequences may affect the appearance of the bone contusions 35. Furthermore, advancements in MRI technology, such as increased magnetic field strengths, have resulted in an overall increase in the signal-to-noise ratio 30, which may also affect the appearance of bone contusions. Additionally, physicians are using MRI scans more frequently in their practices 3,11,15,42, including acutely after knee injuries 8, which may account for differences in the observed prevalence of bone contusions in more recent studies.
In this study, we did not detect a significant difference between sexes in the prevalence of bone contusions in the LTP, LFC, MTP, and MFC. These results are similar to conclusions drawn by previous studies 36. For example, Wittstein et al. reviewed 73 subjects with non-contact ACL injuries and also found no significant sex differences in the locations of tibial and femoral contusions 49. This may imply that the knee was not positioned differently between males and females at the time of injury. This finding is in line with previous studies that have used 3D bone models derived from MRIs of non-contact injured subjects with the four bone contusion pattern (LTP/LFC/MTP/MFC) to quantitatively predict the position of the knee near the time of injury 22,34. This prior work also showed no significant differences in the predicted injury positions between males and females 34. Thus, our results, along with prior literature 34,36,49, suggest that while males and females may have different ACL injury risk profiles, males and females may not sustain ACL injuries via disparate mechanisms.
While the findings of the present study improve our understanding of the frequency of different bone contusion patterns in non-contact ACL injured knees, future work can mitigate some of the limitations of this study. For example, these bone contusions could be further stratified by contusion intensity and volume 26 to provide more detail on injury severity and perhaps more insight on potential injury mechanisms. Furthermore, future studies may examine the time course of contusions after these injuries, which could be accomplished by acquiring multiple MRIs from the same ACL injured subjects over the course of several weeks to months. Additional future directions may also involve developing and refining computational tools designed to use bone contusions to predict the position of injury 22,34.
In summary, our results quantify the frequencies of specific bone contusion patterns in patients with non-contact ACL injuries, who underwent MR imaging within 6 weeks of injury. Our findings indicate that patients with three and four bone contusions comprised 65% of those who were imaged within 6 weeks of injury. The most commonly observed pattern was the four contusion pattern, which was present in 35% of patients. Importantly, we found no statistically significant differences between males and females in bone contusion frequencies by compartment, which may suggest that the knee position at the time of injury is similar for both sexes. Knowledge of the frequency and distribution of bone contusions may be used help elucidate mechanisms of ACL injury. Specifically, this information can be used in computational models to predict the position of the knee at the time of injury.
Acknowledgements
The authors thank Don Kirkendall, ELS, for his editorial assistance.
One or more of the authors has declared the following potential conflict of interest or source of funding: National Institutes of Health funding was received from the following grants AR065527, AR074800, and AR075399. T.E.L. has received education payments from Prodigy Surgical and Wright Medical; nonconsulting fees from Arthrex; and hospitality payments from Arthrex and Wright Medical. J.R.W. has received education payments from Prodigy Surgical; nonconsulting fees from Arthrex; and hospitality payments from Aesculap Biologics. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
REFERENCES
- 1.Agel J, Rockwood T, Klossner D. Collegiate ACL Injury Rates Across 15 Sports: National Collegiate Athletic Association Injury Surveillance System Data Update (2004–2005 Through 2012–2013). Clin J Sport Med. 2016;26(6):518–523. [DOI] [PubMed] [Google Scholar]
- 2.Andriacchi TP, Briant PL, Bevill SL, Koo S. Rotational changes at the knee after ACL injury cause cartilage thinning. Clin Orthop Relat Res. 2006;442:39–44. [DOI] [PubMed] [Google Scholar]
- 3.Baker LC. Acquisition of MRI equipment by doctors drives up imaging use and spending. Health Aff (Millwood). 2010;29(12):2252–2259. [DOI] [PubMed] [Google Scholar]
- 4.Bisson LJ, Kluczynski MA, Hagstrom LS, Marzo JM. A prospective study of the association between bone contusion and intra-articular injuries associated with acute anterior cruciate ligament tear. The American journal of sports medicine. 2013;41(8):1801–1807. [DOI] [PubMed] [Google Scholar]
- 5.Boden BP, Sheehan FT, Torg JS, Hewett TE. Noncontact anterior cruciate ligament injuries: mechanisms and risk factors. J Am Acad Orthop Surg. 2010;18(9):520–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boden BP, Torg JS, Knowles SB, Hewett TE. Video Analysis of Anterior Cruciate Ligament Injury : Abnormalities in Hip and Ankle Kinematics. The American journal of sports medicine. 2009;37:252–259. [DOI] [PubMed] [Google Scholar]
- 7.Bretlau T, Tuxoe J, Larsen L, Jorgensen U, Thomsen HS, Lausten GS. Bone bruise in the acutely injured knee. Knee Surg Sports Traumatol Arthrosc. 2002;10(2):96–101. [DOI] [PubMed] [Google Scholar]
- 8.Davies NH, Niall D, King LJ, Lavelle J, Healy JC. Magnetic resonance imaging of bone bruising in the acutely injured knee--short-term outcome. Clin Radiol. 2004;59(5):439–445. [DOI] [PubMed] [Google Scholar]
- 9.Englander ZA, Baldwin EL 3rd, Smith WAR, Garrett WE, Spritzer CE, DeFrate LE. In Vivo Anterior Cruciate Ligament Deformation During a Single-Legged Jump Measured by Magnetic Resonance Imaging and High-Speed Biplanar Radiography. The American journal of sports medicine. 2019:363546519876074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Englander ZA, Cutcliffe HC, Utturkar GM, et al. In vivo assessment of the interaction of patellar tendon tibial shaft angle and anterior cruciate ligament elongation during flexion. J Biomech. 2019;90:123–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Espeland A, Natvig NL, Loge I, Engebretsen L, Ellingsen J. Magnetic resonance imaging of the knee in Norway 2002–2004 (national survey): rapid increase, older patients, large geographic differences. BMC Health Serv Res. 2007;7:115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Filardo G, Andriolo L, di Laura Frattura G, Napoli F, Zaffagnini S, Candrian C. Bone bruise in anterior cruciate ligament rupture entails a more severe joint damage affecting joint degenerative progression. Knee Surg Sports Traumatol Arthrosc. 2019;27(1):44–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fithian DC, Paxton LW, Goltz DH. Fate of the anterior cruciate ligament-injured knee. Orthop Clin North Am. 2002;33(4):621–636, v. [DOI] [PubMed] [Google Scholar]
- 14.Fleming BC, Ohlen G, Renstrom PA, Peura GD, Beynnon BD, Badger GJ. The effects of compressive load and knee joint torque on peak anterior cruciate ligament strains. The American journal of sports medicine. 2003;31(5):701–707. [DOI] [PubMed] [Google Scholar]
- 15.Glynn N, Morrison WB, Parker L, Schweitzer ME, Carrino JA. Trends in utilization: has extremity MR imaging replaced diagnostic arthroscopy? Skeletal Radiol. 2004;33(5):272–276. [DOI] [PubMed] [Google Scholar]
- 16.Graf BK, Cook DA, De Smet AA, Keene JS. “ Bone bruises” on magnetic resonance imaging evaluation of anterior cruciate ligament injuries. The American journal of sports medicine. 1993;21(2):220–223. [DOI] [PubMed] [Google Scholar]
- 17.Herzog MM, Marshall SW, Lund JL, Pate V, Spang JT. Cost of Outpatient Arthroscopic Anterior Cruciate Ligament Reconstruction Among Commercially Insured Patients in the United States, 2005–2013. Orthop J Sports Med. 2017;5(1):2325967116684776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hewett TE, Myer GD, Ford KR. Reducing knee and anterior cruciate ligament injuries among female athletes: a systematic review of neuromuscular training interventions. J Knee Surg. 2005;18(1):82–88. [DOI] [PubMed] [Google Scholar]
- 19.Hewett TE, Torg JS, Boden BP. Video analysis of trunk and knee motion during non-contact anterior cruciate ligament injury in female athletes: lateral trunk and knee abduction motion are combined components of the injury mechanism. British journal of sports medicine. 2009;43(6):417–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jelic D, Masulovic D. Bone bruise of the knee associated with the lesions of anterior cruciate ligament and menisci on magnetic resonance imaging. Vojnosanit Pregl. 2011;68(9):762–766. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan PA, Gehl RH, Dussault RG, Anderson MW, Diduch DR. Bone contusions of the posterior lip of the medial tibial plateau (contrecoup injury) and associated internal derangements of the knee at MR imaging. Radiology. 1999;211(3):747–753. [DOI] [PubMed] [Google Scholar]
- 22.Kim SY, Spritzer CE, Utturkar GM, Toth AP, Garrett WE, DeFrate LE. Knee Kinematics During Noncontact Anterior Cruciate Ligament Injury as Determined From Bone Bruise Location. The American journal of sports medicine. 2015;43(10):2515–2521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koga H, Nakamae A, Shima Y, et al. Mechanisms for noncontact anterior cruciate ligament injuries: knee joint kinematics in 10 injury situations from female team handball and basketball. The American journal of sports medicine. 2010;38(11):2218–2225. [DOI] [PubMed] [Google Scholar]
- 24.Laible C, Sherman OH. Risk factors and prevention strategies of non-contact anterior cruciate ligament injuries. Bull Hosp Jt Dis (2013). 2014;72(1):70–75. [PubMed] [Google Scholar]
- 25.Lattermann C, Jacobs CA, Reinke EK, et al. Are Bone Bruise Characteristics and Articular Cartilage Pathology Associated with Inferior Outcomes 2 and 6 Years After Anterior Cruciate Ligament Reconstruction? Cartilage. 2017;8(2):139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li X, Ma BC, Bolbos RI, et al. Quantitative assessment of bone marrow edema-like lesion and overlying cartilage in knees with osteoarthritis and anterior cruciate ligament tear using MR imaging and spectroscopic imaging at 3 Tesla. J Magn Reson Imaging. 2008;28(2):453–461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lohmander LS, Englund PM, Dahl LL, Roos EM. The long-term consequence of anterior cruciate ligament and meniscus injuries: osteoarthritis. The American journal of sports medicine. 2007;35(10):1756–1769. [DOI] [PubMed] [Google Scholar]
- 28.Lynch TC, Crues JV 3rd, Morgan FW, Sheehan WE, Harter LP, Ryu R. Bone abnormalities of the knee: prevalence and significance at MR imaging. Radiology. 1989;171(3):761–766. [DOI] [PubMed] [Google Scholar]
- 29.Mall NA, Chalmers PN, Moric M, et al. Incidence and trends of anterior cruciate ligament reconstruction in the United States. The American journal of sports medicine. 2014;42(10):2363–2370. [DOI] [PubMed] [Google Scholar]
- 30.Maubon AJ, Ferru JM, Berger V, et al. Effect of field strength on MR images: comparison of the same subject at 0.5, 1.0, and 1.5 T. Radiographics. 1999;19(4):1057–1067. [DOI] [PubMed] [Google Scholar]
- 31.Mink JH, Deutsch AL. Occult cartilage and bone injuries of the knee: detection, classification, and assessment with MR imaging. Radiology. 1989;170(3 Pt 1):823–829. [DOI] [PubMed] [Google Scholar]
- 32.Neuman P, Kostogiannis I, Friden T, Roos H, Dahlberg LE, Englund M. Knee laxity after complete anterior cruciate ligament tear: a prospective study over 15 years. Scand J Med Sci Sports. 2012;22(2):156–163. [DOI] [PubMed] [Google Scholar]
- 33.Nishimori M, Deie M, Adachi N, et al. Articular cartilage injury of the posterior lateral tibial plateau associated with acute anterior cruciate ligament injury. Knee Surg Sports Traumatol Arthrosc. 2008;16(3):270–274. [DOI] [PubMed] [Google Scholar]
- 34.Owusu-Akyaw KA, Kim SY, Spritzer CE, et al. Determination of the Position of the Knee at the Time of an Anterior Cruciate Ligament Rupture for Male Versus Female Patients by an Analysis of Bone Bruises. The American journal of sports medicine. 2018;46(7):1559–1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Papalia R, Torre G, Vasta S, et al. Bone bruises in anterior cruciate ligament injured knee and long-term outcomes. A review of the evidence. Open Access J Sports Med. 2015;6:37–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Patel SA, Hageman J, Quatman CE, Wordeman SC, Hewett TE. Prevalence and location of bone bruises associated with anterior cruciate ligament injury and implications for mechanism of injury: a systematic review. Sports Med. 2014;44(2):281–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Quatman CE, Hewett TE. The anterior cruciate ligament injury controversy: is “valgus collapse” a sex-specific mechanism? British journal of sports medicine. 2009;43(5):328–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: a meta-analysis of nonoperative versus operative treatment. The American journal of sports medicine. 2014;42(11):2769–2776. [DOI] [PubMed] [Google Scholar]
- 39.Roos H, Adalberth T, Dahlberg L, Lohmander LS. Osteoarthritis of the knee after injury to the anterior cruciate ligament or meniscus: the influence of time and age. Osteoarthritis Cartilage. 1995;3(4):261–267. [DOI] [PubMed] [Google Scholar]
- 40.Rosen MA, Jackson DW, Berger PE. Occult osseous lesions documented by magnetic resonance imaging associated with anterior cruciate ligament ruptures. Arthroscopy. 1991;7(1):45–51. [DOI] [PubMed] [Google Scholar]
- 41.Sanders TG, Medynski MA, Feller JF, Lawhorn KW. Bone contusion patterns of the knee at MR imaging: footprint of the mechanism of injury. Radiographics. 2000;20 Spec No:S135–151. [DOI] [PubMed] [Google Scholar]
- 42.Solomon DH, Katz JN, Carrino JA, et al. Trends in knee magnetic resonance imaging. Med Care. 2003;41(5):687–692. [DOI] [PubMed] [Google Scholar]
- 43.Sommerlath KG, Gillquist J. The effect of anterior cruciate ligament resection and immediate or delayed implantation of a meniscus prosthesis on knee joint biomechanics and cartilage. An experimental study in rabbits. Clin Orthop Relat Res. 1993(289):267–275. [PubMed] [Google Scholar]
- 44.Song GY, Zhang H, Wang QQ, Zhang J, Li Y, Feng H. Bone Contusions After Acute Noncontact Anterior Cruciate Ligament Injury Are Associated With Knee Joint Laxity, Concomitant Meniscal Lesions, and Anterolateral Ligament Abnormality. Arthroscopy. 2016;32(11):2331–2341. [DOI] [PubMed] [Google Scholar]
- 45.Speer KP, Spritzer CE, Bassett III FH, Feagin JR JA, Garrett JR WE. Osseous injury associated with acute tears of the anterior cruciate ligament. The American journal of sports medicine. 1992;20(4):382–389. [DOI] [PubMed] [Google Scholar]
- 46.Stiebel M, Miller LE, Block JE. Post-traumatic knee osteoarthritis in the young patient: therapeutic dilemmas and emerging technologies. Open Access J Sports Med. 2014;5:73–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Vellet AD, Marks PH, Fowler PJ, Munro TG. Occult posttraumatic osteochondral lesions of the knee: prevalence, classification, and short-term sequelae evaluated with MR imaging. Radiology. 1991;178(1):271–276. [DOI] [PubMed] [Google Scholar]
- 48.Viskontas DG, Giuffre BM, Duggal N, Graham D, Parker D, Coolican M. Bone bruises associated with ACL rupture: correlation with injury mechanism. The American journal of sports medicine. 2008;36(5):927–933. [DOI] [PubMed] [Google Scholar]
- 49.Wittstein J, Vinson E, Garrett W. Comparison Between Sexes of Bone Contusions and Meniscal Tear Patterns in Noncontact Anterior Cruciate Ligament Injuries. The American journal of sports medicine. 2014;42(6):1401–1407. [DOI] [PubMed] [Google Scholar]
- 50.Yao L, Lee JK. Occult intraosseous fracture: detection with MR imaging. Radiology. 1988;167(3):749–751. [DOI] [PubMed] [Google Scholar]
- 51.Yoon KH, Yoo JH, Kim KI. Bone contusion and associated meniscal and medial collateral ligament injury in patients with anterior cruciate ligament rupture. J Bone Joint Surg Am. 2011;93(16):1510–1518. [DOI] [PubMed] [Google Scholar]
- 52.Zbrojkiewicz D, Vertullo C, Grayson JE. Increasing rates of anterior cruciate ligament reconstruction in young Australians, 2000–2015. Med J Aust. 2018;208(8):354–358. [DOI] [PubMed] [Google Scholar]
- 53.Zhang L, Hacke JD, Garrett WE, Liu H, Yu B. Bone Bruises Associated with Anterior Cruciate Ligament Injury as Indicators of Injury Mechanism: A Systematic Review. Sports Med. 2019;49(3):453–462. [DOI] [PubMed] [Google Scholar]


