Abstract
Background and objectives
Due to their professional characteristics and future career orientation, medical students have a deeper understanding of COVID-19 and enact disease prevention and control measures, which may cause psychological burden. We aimed to assess the psychological impact during the COVID-19 outbreak period(OP) and remission period(RP) among medical students.
Methods
We surveyed the medical students in Shantou University Medical College twice-during the OP and the RP, surveying psychological burden of COVID-19 lockdowns and its associated factors. 1069 respondents were recruited in OP and 1511 participants were recruited in RP. We constructed nomograms to predict the risk of psychological burden using risk factors that were screened through univariate analysis of the surveyed data set.
Results
There was a statistically significant longitudinal increment in psychological burden from OP to RP, and stress as well as cognition in psychological distress were the most dominant ones. Common impact factors of the depression, anxiety and stress included frequency of outdoor activities, mask-wearing adherence, self-perceived unhealthy status and exposure to COVID-19. In addition, the high frequency of handwashing was a protective factor for depression and anxiety. The C-index was 0.67, 0.74 and 0.72 for depression, anxiety and stress, respectively.
Conclusion
The psychological impact of COVID-19 was worse during the RP than during the OP. Thus, it's necessary to continue to emphasize the importance of mental health in medical students during the pandemic and our proposed nomograms can be useful tools for screening high-risk groups for psychological burden risk in medical students.
Keywords: COVID-19, Medical students, Psychological health, Nomogram
Background
Infectious diseases remain one of the largest threats to the well-being of the human race [1]. The coronavirus disease 2019 (COVID-19) has spread at a startling rate throughout China and several other countries, causing an outbreak of acute infectious pneumonia [2,3]. In China, many regions (i.e., cities or districts) initiated first-level responses and instituted mitigation policies to curtail further transmission of the virus [2,4]. For example, confirmed cases were quarantined, suspicious cases were monitored and restricted by house arrest, university campuses remained closed, and individuals were encouraged to stay at home as much as possible [5]. By early March 2020, more than 70% of infected patients had recovered and been discharged from hospital, and by April 7, 2020, most cities and districts were declared “low-risk areas” [6]. The World Health Organization (WHO) said that the restrictions enacted by China helped mitigate the spread of this highly contagious and fatal disease, and that the virus had entered a period of remission in China [7]. However, prolonged lockdown that substantially restrict routine activities for extended periods can adversely affects daily life, including work and study habit. Such measures can engender more serious mental health problems characterized by states of anxiety, depression, helplessness and hopelessness [8,9].
Numerous studies have evidence suggesting that the COVID-19 epidemic has led to a significant increase in mental health problems among the general public in China, manifesting in a host of cognitive, emotional, physiological and behavioral changes [2,10,11]. During the outbreak, colleges and universities postponed campus openings. Stressors such as fear of infection, prolonged duration of quarantine, maladjustment to remote learning platforms and family financial loss, among many others, can initiate or exacerbate mental health difficulties [12]. During the COVID-19 outbreak in Beijing China, a survey has suggested that 25.63% students were in a state of anxiety, and 31.87% students were in a state of anxiety [13]. Another study reported that 155,077 (50.9%) of the students in their sample self-reported significant symptoms of stress, and 1565 (0.5%) self-reported poorer mental health [12].
College students are a distinct group in that they are generally more tolerant of novel ideas (i.e., greater openness to experience), acquire information from multiple channels for information acquisition, and have high levels of social media engagement [12]. However, medical students are expected to hold a deeper understanding of this infectious disease and to enact disease prevention and control measure more effectively than their non-medical counterparts. As the main force and reserve talents of the future medical career, they shoulder the sacred mission of saving lives and protecting people's health, playing an extremely important role in the construction and development of health care. Due to their professional characteristics and future career orientation, they are not only moved by the dedication of the medical workers who are fearless of life and death, but also aware of the psychological impact that the medical profession may bring life-threatening.
Recent study on mental health effects of on COVID-19 are largely cross-sectional [14], and focus on health professionals 15, 16, 17, 18, 19 or ordinary college students [20], they also lack data on longitudinal changes in the mental health status of medical students throughout the COVID-19 epidemic. The aim of our longitudinal study was to assess the psychological effects of COVID-19 lockdowns during the outbreak period and remission periods in medical students in China, so as to provide a theoretical basis for future psychological interventions by using a nomogram model to identify risk and protective factors.
Methods
Participants and procedures
This longitudinal study was conducted from February 9 to February 15 and from April 16 to April 26, 2020, which encompassed the outbreak period (OP) and remission period (RP) of COVID-19 epidemic in China [4,21]. Medical students from Shantou University Medical College were invited to participate and fulfill the questionnaire. Due to restrictions limiting, face-to-face interactions and isolate themselves [21], the questionnaire was completed remotely and anonymously via an online survey platform anonymously (Survey Star). For quality control, questionnaires completed within <100 s and those who incomplete data were excluded . Ethical approval was obtained from the Research Ethics Board of the University of Shantou university (project no. SUMC-2020-01). All respondents provided informed consent.
Measures
Data were collected using a self-administered questionnaire that included demographic information and information on the psychological burden (i.e., presence of psychological distress, depression, stress and anxiety) of COVID-19 lockdowns and its associated factors. The psychological distress subscales are composed of three items (related to cognition, emotion and behavior), and the critical threshold of ≥11 was used to determine the presence of group differences on measures of psychological distress. The 21-item Depression Anxiety Stress Scales (DASS-21), a well-validated psychometric to measure the core symptoms of depression, anxiety, and stress [22] was deemed suitable for application within the context of the COVID-19 epidemic. Each subscales consisted of seven items and the subscale scores (depression, anxiety, and stress) ranged from normal to extremely severe [23]. The cut-off score of >9 is considered to indicate the presence of depression, a cut-off score of >7 is considered indicative of the presence of anxiety and a cut-off score of >14 is considered indicative of the presence of stress. Finally, participants were queried on their frequency of engagement in outdoor activities during the peak and remission periods, mask-wearing adherence, their health status, hand hygiene, and COVID-19 exposure, among others.
Statistical analyses
All the statistical analysis were carried out with IBM SPSS Statistics, version 24.0 (IBM Corp.,Armonk, NY) and R (version 3.3.2). Categorical variables for basic characteristics were expressed as percentages (%), while continuous variables for the participants’ ages and their psychological burden scores were expressed as the mean and standard deviation (SD). The independent samples t-test was performed to compare the psychological impact between the first and second survey. Two datasets were integrated, and multivariate logistic regression analysis was conducted to assess risk factors for psychological burden. P values below 0.05 were considered to be statistically significant.
To predict the risk of psychological burden, we proposed visual nomograms (one for depression, one for anxiety, and one for stress) which is composed of graphical lines of risk factors, points, total points, in order to predict the risk of psychological burden. The length of each risk factor's line was made to reflect the regression coefficient estimated by multiple logistic regression analysis [24]. We used Harrell's C-index and the Hosmer-Lemeshow test to assess the proposed nomogram. Harrell's C-statistic was calculated by 1 000-fold bootstrap resampling iterations to an initial fitted logistic model in the derivation set. The concordance index ranges from 0 to 1, with 1 indicating perfect concordance, 0.5 indicating no better concordance than would be expected by chance, and 0 indicating perfect discordance [25].
Results
Participant characteristics
The response rates were 94.85% (1069 of 1127 medical students) and 94.85% (1511 of 1653 medical students) in the first and second survey, respectively. A comparison of the demographic description of the respondents between the OP and RP are shown in Table 1 . The majority of respondents in the OP were female (58.65%), had a mean age of 20.93 years, were unmarried (98.78%) and were junior students (51.45%). Similarly, the majority of respondents in the remission period were female (53.01%), had a mean age of 21.21 years and were unmarried (98.78%); however, more senior students (51.09%) characterized this sample relative to that of the outbreak period. No statistically significant differences were found between two groups, with the exception of age and gender. We considered that the differences were attributed to the relatively small number of participants who responded during the OP than during the RP, and thus, we justified the inclusion of age and sex as covariates in all subsequent analyses.
Table 1.
Comparison of characteristics between outbreak and remission period.
| Outbreak Period(n = 1069) | Remission Period(n = 1511) | P-value | |
|---|---|---|---|
| Age | 20.93 ± 1.64 | 21.21 ± 1.69 | P < 0.001 |
| Gender | P = 0.005 | ||
| male | 442(41.35%) | 710(46.99%) | |
| female | 627(58.65%) | 801(53.01%) | |
| Grade | P = 0.203 | ||
| Senior | 519(48.55%) | 772(51.09%) | |
| Junior | 550(51.45%) | 739(48.91%) | |
| Marital status | P = 0.053 | ||
| Unmarried | 1056(98.78%) | 1477(97.75%) | |
| Married | 13(1.22%) | 34(2.25%) |
Data is n (%) or mean±SD.
Psychological burden between the OP and RP
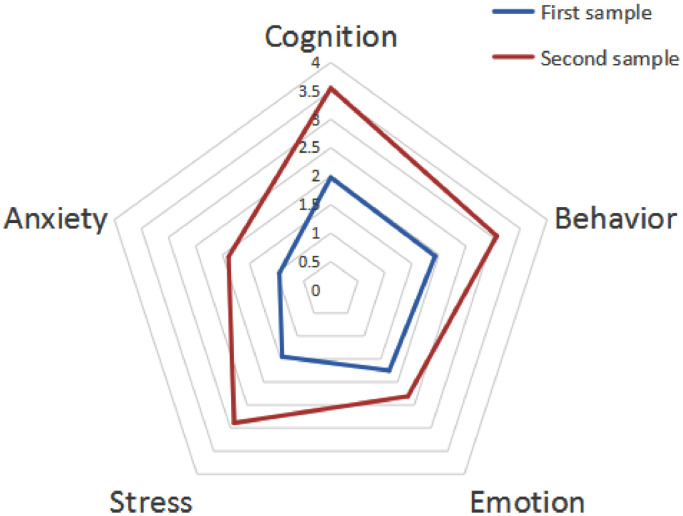
Table 2 presents the various types of psychological burden reported by medical students during the COVID-19 epidemic from OP to RP. The t–test results indicated that from the OP to the RP, measures of psychological burden, namely stress (t = –10.94,P < 0.001), anxiety (t = –8.56,P < 0.001) and psychological distress(t = –10.94,P < 0.001) all increased significantly. For the three dimensions of psychological distress, levels of cognition(t = –13.86,P < 0.001), emotion(t = –5.30,P < 0.001), behavior (t = –10.28,P < 0.001) increased significantly between the OP and the RP(Table 2). Mental health during the RP was significantly worse than in the OP, the most predominant symptoms of which were stress as well as cognition in psychological distress were the most dominant ones. A more intuitive result are shown in Fig. 1 .
Table 2.
Psychological burden of medical students.
| Outbreak period | Remission period | t value | P value | |
|---|---|---|---|---|
| Psychological Distress | 5.65 ± 6.74 | 8.93 ± 8.45 | −10.94 | <0.001 |
| Cognition | 1.98 ± 2.58 | 3.55 ± 3.17 | −13.86 | <0.001 |
| Emotion | 1.75 ± 2.45 | 2.31 ± 2.96 | −5.30 | <0.001 |
| Behavior | 1.93 ± 2.53 | 3.07 ± 3.09 | −10.28 | <0.001 |
| Stress | 1.45 ± 2.88 | 2.89 ± 3.80 | −10.95 | <0.001 |
| Anxiety | 0.95 ± 2.27 | 1.89 ± 3.30 | −8.56 | <0.001 |
| Depression | – | 2.73 ± 3.82 | – | – |
Data is mean±SD.
Figure 1.
Radar plot with the distribution of psychological burden mean scores of Chinese medical students during OP and RP.
Nomogram prognostic model
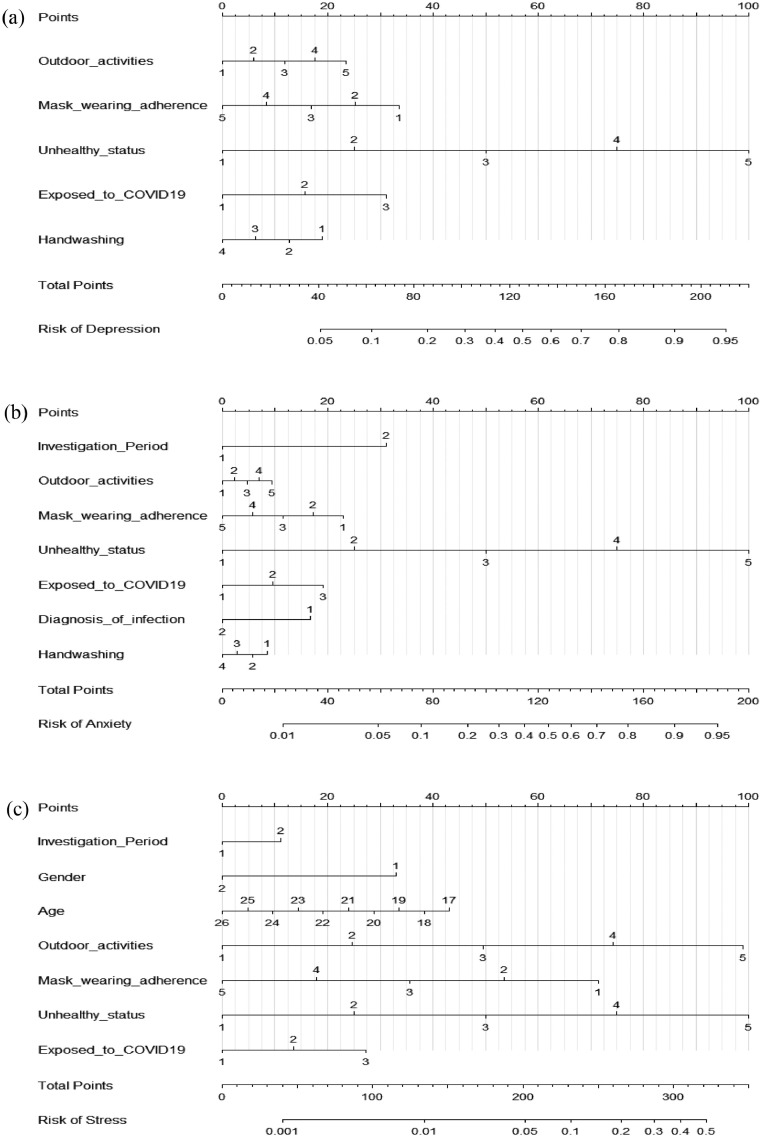
We constructed a nomogram to predict the risk of psychological burden using risk factors that were screened through univariate analysis of the surveyed data set (Supplementary Table 1). The developed nomogram is shown in Fig. 2 .
Figure 2.
Nomogram to estimate probability of (a)depression rate, (b)anxiety rate and (c)stress rate at COVID-19. Gender: 1, male; 2, female. Investigation Period: 1, outbreak period; 2, remission period. Outdoor activities: 1, never; 2, seldom; 3, Sometimes; 4, usually; 5, always. Mask wearing adherence:1, never; 2, seldom; 3, Sometimes; 4, usually; 5, always. Unhealthy status: 1, never; 2, seldom; 3, Sometimes; 4, usually; 5, always. Exposed to COVID-19: 1, yes; 2, no; 3, uncertainty. Diagnosis of infection: 1, yes; 2, no. Handwashing: 1, 0–5 times per day; 2, 6–10 times per day; 3,11–15 times per day; 4,more than 15 times per day. .
The longer the length of line, the greater the impact of the risk factors on the prevalence rates of depression, anxiety, and stress. Each risk factor has its corresponding ‘points’. For example, as shown in the Fig. 2a, an ‘Outdoor activities’ level of 5 which is proven to have the greatest impact on the prevalence of depression corresponded to 23 points. Given that the risk factor line for ‘Outdoor activities’ level of 5 was relatively longer than that of other factors, it can be interpreted that the effect of the extent of ‘always outdoor activities’ was largest. The cumulative sum of these ‘points’ was referred to as the ‘total points’. Compute the sum of points for all predictors, and denote this value as the Total points. Identify the value of the Linear predictor (LP) associated with the total points by placing a vertical ruler onto the nomogram.
Common impact factors of the depression, anxiety, and stress included frequency of outdoor activities, mask-wearing adherence, self-perceived unhealthy status, and exposure to COVID-19. In addition, the high frequency of handwashing was found to be a protective factor against depression and anxiety. Medical students were more likely to have anxiety and stress during the RP than the OP. Furthermore, a diagnosis of infection was found to be a unique risk factor for anxiety. The results were shown in Fig. 2.
The Hosmer–Lemeshow test and C-index were applied to validate the model. The Hosmer–Lemeshow test showed no statistically significantly differences between predicted and actual outcomes, (χ2 = 5.18, P = 0.638; χ2 = 6.97, P = 0.0.539; and χ2 = 5.93, P = 0.655, respectively). The C-index was 0.67 (95%CI, 0.64–0.70), 0.74(95%CI, 0.69–0.79), and 0.72(95%CI,0.66–0.78) for depression, anxiety, and stress, respectively. The closer the C-index gets to 1, the greater the predictive value afforded by this regression model [26,27]. The models discriminate to a good extent, indicating that the predicted probability of psychological burden in medical students can be judged as very high.
Discussion
Our study investigated the temporal changes in psychological health status in Chinese medical students from the outbreak to the remission phase of the COVID-19 pandemic. A Meta-analysis [28] of medical students before the COVID-19 outbreak found that anxiety among medical students was common and more likely to occur among medical students in the Middle East and Asia, which suggested that greater attention should be paid to the mental health status of this population. A subsequent the Meta-anlysis found that following the COVID-19 outbreak, the self-reported anxiety levels of medical students did not differ significantly [29]. At the beginning of the outbreak, although the medical students were more alert to the virus, it did not have a huge adverse psychological impact on the students' psychology. Moreover, our study likewise found that medical students' psychological burden was superior to that of the RP in the early stages of the OP. This may be that the mental health consequences of COVID-19 could persist over extended periods, and that mental health problems could peak after—rather than during— the actual pandemic [4,30].
Our results were consistent with the prediction and showed that the score of psychological burden score of medical students during the COVID-19 RP was higher than during the OP, indicating greater psychological burden. Firstly, the epidemic in China has entered a period of remission, the epidemic trend of the COVID-19 has shifted from China to abroad, however, domestic travel agencies remained vigilant, entertainment, shopping areas and stadiums were still restricted or closed, and the government's recommended home isolation has not been lifted, which means people's activities are still restricted. With the reduction in face-to-face communication, loneliness and anxiety can readily occur, thereby increasing psychological burden. In addition, although the epidemic in China has been alleviated, various colleges and universities still use portals and web-based applications to provide lectures or other teaching activities to further mitigate the risk to patients and students alike [31,32]. Medical schools officially canceled formal teaching on wards and delayed the examination, hindering the education of medical students in the face of the newly emerging epidemic [31,33]. Not only the uncertainty and potential negative will effects on academic development would have adverse effects on students’ psychological health [34], but also the sudden increase in academic tasks would lead to bad feeling, such as stress and anxiety, among medical students. Thirdly, senior students in this study accounted for approximately half of the study sample. In China, most new graduates are required to complete their final dissertation, prepare for graduation and consider the issue of employment option before June: the closer they get to the graduation time, the more likely they are to have pre-employment stress. A meta analysis [35] revealed that the impact of online learning appeared to be greater on senior students, most likely due to a more intensive curriculum. Affected by the epidemic, the employment prospects are poor in 2020, and various job fairs have been postponed or cancelled entirely. Medical students are more likely to be nervous and anxious.
To make the bias minimized, we used a novel and validated prognostic model. The nomogram, which was considered as a trustworthy method for accurately predicting prognosis [26], can visualize the results of complex regression equations, making the prediction model more easily understood.
The result of the nomogram were consistent with the radar plot, in that during RP of the epidemic, the risk of experiencing anxiety and stress as a medical students is higher than during the OP. Another finding is that good health can reduce the psychological burden of medical students. With the increase of the frequency of physical discomfort, the risk of negative emotion (depression, anxiety, and stress) is greater. This is consistent with physical symptoms reported and with the mental health literature indicating that the presence of physical symptoms was associated with higher mean scores in the DASS anxiety, stress, and depression subscales during the COVID-19 outbreak [36]. Due to the interaction between physical discomfort and psychological burden, it is crucial not to neglect physical symptoms, as they may be a reflection of underlying psychological distress [36]. Furthermore, students who were poorly adherent to wear a mask were more likely to develop negative emotions than those were adherent. Medical masks can effectively limit the spread of the COVID-19 virus and reduce the risk of infection. In the early stages of the epidemic in China, work and production were suspended due to the Chinese Spring Festival, resulting in a shortage in mask supply. Coupled with the rapid spread of COVID-19, the fact that personal protection (e.g., masks) cannot be guaranteed, so an adequate supply of masks can effectively reduce the negative mood of students. Our study found that people who were suspected or confirmed cases have an increased risk of psychological impact compared to those without contacted. The nomograms show that students were at greater risk of negative emotion if they are were unsure whether they had been exposed. Furthermore, the psychological burden of medical students with exposure to COVID-19 was higher than that of students who were not exposed. Previous a large cross-sectional study from China observed that the risk of depression symptoms in students with a family member who was a confirmed cases was three times higher than that in students with no family history of infection [37]. The severity and fatality of the disease were high. Medical students who were uncertain or exposed to suspected/susceptible people would worry about infecting COVID-19, due to poor health or exposure to the epidemic. Thus, these students were prone to tension and anxiety.
Limitations
Our study had some limitations. Firstly, we were unable to directly compare individual participants longitudinally from the OP to RP, due to the anonymous nature of the questionnaires. But non-anonymity may cause investigators to deliberately cover up the truth. Secondly, although our study shows that the nomograms have certain accuracy in predicting the probability of psychological burden of medical students during COVID-19, large-scale data are still needed for external recommendations, which will help verify the accuracy of our results are more reliable. Thirdly, more large scale cohort studies are needed to investigate the long-term psychological health effects of COVID-19 on medical students.
Conclusions
The psychological impact of COVID-19 was worse during the RP than during the OP. Thus, educational and health authorities should continue to emphasize the importance of mental health in medical students during the pandemic and are encouraged to implement regular health assessments to promote serious psychological well-being. Our proposed nomograms can be a useful tool for screening high-risk groups for psychological burden risk in Chinese medical students in order to identify at-risk individuals and help inform preventative measures.
Authors’ contributions
Kaiting Zhang conducted the data gathering. Kaiting Zhang and Zeting Lin performed the statistical analyses. Kaiting Zhang and Yixiang Peng drafted the manuscript. Zeting Lin contributed to manuscript preparation. Liping Li designed and conceived of the study, and supervised data gathering, data analysis, and manuscript preparation. All authors contributed to the interpretation of the data and offered critical revisions of the draft. All authors read and approved the final manuscript.
Funding
This study was supported by grant from the Shantou Science and Technology Project(CN) (to Liping Li (SFK[2020]16–5). Researchers had scientific independence to choose the study design, collect, analyse, and interpret data, and write the report.
Ethics approval and consent to participate
The research content and process was approved by the Institutional Review Board of Shantou University Medical College (Project No. SUMC-2020-01). No changes were made to the primary or secondary outcomes after trial approval. All participants gave their written informed consent.
Consent for publication
The funders had no role in the study design, data collection, data analysis, data interpretation, writing of the manuscript, and decision to submit.
Declaration of Competing Interest
We declare no competing interests
Acknowledgements
We would like to thank all the participants for this project.
Footnotes
Supplementary material associated with this article can be found in the online version at https://doi.org/10.1016/j.ejpsy.2021.06.003.
Appendix. Supplementary materials
Reference
- 1.Lee A.M., Wong J.G., McAlonan G.M., Cheung V., Cheung C., Sham P.C., et al. Stress and psychological distress among SARS survivors 1 year after the outbreak. Can J Psychiatry. 2007;52(4):233–240. doi: 10.1177/070674370705200405. [DOI] [PubMed] [Google Scholar]
- 2.Bao Y., Sun Y., Meng S., Shi J., Lu L. 2019-nCoV epidemic: address mental health care to empower society. Lancet. 2020;395(10224):e37–e38. doi: 10.1016/S0140-6736(20)30309-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Xu X.W., Wu X.X., Jiang X.G., Xu K.J., Ying L.J., Ma C.L., et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ. 2020;368:m606. doi: 10.1136/bmj.m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Duan H., Yan L., Ding X., Gan Y., Kohn N., Wu J. Impact of the COVID-19 pandemic on mental health in the general Chinese population: changes, predictors and psychosocial correlates. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hellewell J., Abbott S., Gimma A., Bosse N.I., Jarvis C.I., Russell T.W., et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020;8(04):e488–e496. doi: 10.1016/S2214-109X(20)30074-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.PRC NHCot. Circular of the State Council in response to the Joint Prevention and Control Mechanism of novel coronavirus's pneumonia epidemic situation on the issuance of guidelines on epidemic Prevention and Control measures for Enterprises and institutions in different risk areas to return to work and return to production, http://www.gov.cn/zhengce/content/2020-04/09/content_5500685.htm;2020 [Accessed 9 April 2020].
- 7.Zhu Z., Liu Q., Jiang X., Manandhar U., Luo Z., Zheng X., et al. The psychological status of people affected by the COVID-19 outbreak in China. J Psychiatr Res. 2020;129:1–7. doi: 10.1016/j.jpsychires.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huang Y., Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liang Y., Wu K., Zhou Y., Huang X., Zhou Y., Liu Z. Mental health in frontline medical workers during the 2019 novel coronavirus disease epidemic in China: a comparison with the general population. Int J Environ Res Public Health. 2020;17(18):6550. doi: 10.3390/ijerph17186550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Li X., Lv S., Liu L., Chen R., Chen J., Liang S., et al. COVID-19 in Guangdong: immediate perceptions and psychological impact on 304,167 college students. Front Psychol. 2020;11:2024. doi: 10.3389/fpsyg.2020.02024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feng Y., Zong M., Yang Z., Gu W., Dong D., Qiao Z. When altruists cannot help: the influence of altruism on the mental health of university students during the COVID-19 pandemic. Glob Health. 2020;16(1):61. doi: 10.1186/s12992-020-00587-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang Y., Liu Y., Liu L., Wang X., Luo N., Li L. Clinical outcomes in 55 patients with severe acute respiratory syndrome coronavirus 2 who were asymptomatic at hospital admission in Shenzhen, China. J Infect Dis. 2020;221:1770–1774. doi: 10.1093/infdis/jiaa119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kang L., Ma S., Chen M., Yang J., Wang Y., Li R., et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav Immun. 2020;87:11–17. doi: 10.1016/j.bbi.2020.03.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tan B.Y.Q., Chew N.W.S., Lee G.K.H., Jing M., Goh Y., Yeo L.L.L., et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann Intern Med. 2020;173(04):317–320. doi: 10.7326/M20-1083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Joob B., Wiwanitkit V. Traumatization in medical staff helping with COVID-19 control. Brain Behav Immun. 2020;87:10. doi: 10.1016/j.bbi.2020.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shi Y., Wang J., Yang Y., Wang Z., Wang G., Hashimoto K., et al. Knowledge and attitudes of medical staff in Chinese psychiatric hospitals regarding COVID-19. Brain Behav Immun Health. 2020;4 doi: 10.1016/j.bbih.2020.100064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shao Y., Shao Y., Fei J.M. Psychiatry hospital management facing COVID-19: from medical staff to patients. Brain Behav Immun. 2020;88:947. doi: 10.1016/j.bbi.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cao W., Fang Z., Hou G., Han M., Xu X., Dong J., et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., et al. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gloster A.T., Rhoades H.M., Novy D., Klotsche J., Senior A., Kunik M., et al. Psychometric properties of the depression anxiety and stress Scale-21 in older primary care patients. J Affect Disord. 2008;110(3):248–259. doi: 10.1016/j.jad.2008.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lyvers M., Carlopio C., Bothma V., Edwards M.S. Mood, mood regulation expectancies and frontal systems functioning in current smokers versus never-smokers in China and Australia. Addict Behav. 2013;38(11):2741–2750. doi: 10.1016/j.addbeh.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 24.Chung S.M., Park J.C., Moon J.S., Lee J.Y. Novel nomogram for screening the risk of developing diabetes in a Korean population. Diabetes Res Clin Pract. 2018;142:286–293. doi: 10.1016/j.diabres.2018.05.036. [DOI] [PubMed] [Google Scholar]
- 25.Rouzier R., Pusztai L., Delaloge S., Gonzalez-Angulo A.M., Andre F., Hess K.R., et al. Nomograms to predict pathologic complete response and metastasis-free survival after preoperative chemotherapy for breast cancer. J Clin Oncol. 2005;23(33):8331–8339. doi: 10.1200/JCO.2005.01.2898. [DOI] [PubMed] [Google Scholar]
- 26.Zhou Z.R., Wang W.W., Li Y., Jin K.R., Wang X.Y., Wang Z.W., et al. In-depth mining of clinical data: the construction of clinical prediction model with R. Ann Transl Med. 2019;7(23):796. doi: 10.21037/atm.2019.08.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chung S.M., Park J.C., Moon J.S., Lee J.Y. Novel nomogram for screening the risk of developing diabetes in a Korean population. Diabetes Res Clin Pract. 2018;142:286–293. doi: 10.1016/j.diabres.2018.05.036. [DOI] [PubMed] [Google Scholar]
- 28.Quek T.T., Tam W.W., Tran B.X., Zhang M., Zhang Z., Ho C.S., et al. The global prevalence of anxiety among medical students: a meta-analysis. Int J Environ Res Public Health. 2019;16(15):2735. doi: 10.3390/ijerph16152735. 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lasheras I., Gracia-García P., Lipnicki D.M., Bueno-Notivol J., López-Antón R., de la Cámara C., et al. Prevalence of anxiety in medical students during the COVID-19 pandemic: a rapid systematic review with meta-analysis. Int J Environ Res Public Health. 2020;17(18):6603. doi: 10.3390/ijerph17186603. 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gunnell D., Appleby L., Arensman E., Hawton K., John A., Kapur N., et al. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatry. 2020;7(06):468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Alsafi Z., Abbas A.R., Hassan A., Ali M.A. The coronavirus (COVID-19) pandemic: adaptations in medical education. Int J Surg. 2020;78:64–65. doi: 10.1016/j.ijsu.2020.03.083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Longhurst G.J., Stone D.M., Dulohery K., Scully D., Campbell T., Smith C.F. Strength, Weakness, Opportunity, Threat (SWOT) analysis of the adaptations to anatomical education in the United Kingdom and republic of Ireland in response to the Covid-19 pandemic. Anat Sci Educ. 2020;133(3):301–311. doi: 10.1002/ase.1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ahmed H., Allaf M., Elghazaly H. COVID-19 and medical education. Lancet Infect Dis. 2020;20(7):777–778. doi: 10.1016/S1473-3099(20)30226-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhou S.J., Zhang L.G., Wang L.L., Guo Z.C., Wang J.Q., Chen J.C., et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry. 2020;29(6):749–758. doi: 10.1007/s00787-020-01541-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Li H.Y., Cao H., Leung D.Y.P., Mak Y.W. The psychological impacts of a COVID-19 outbreak on college students in China: a longitudinal study. Int J Environ Res Public Health. 2020;17(11):3933. doi: 10.3390/ijerph17113933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chew N.W.S., Lee G.K.H., Tan B.Y.Q., Jing M., Goh Y., Ngiam N.J.H., et al. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–565. doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang Z.H., Yang H.L., Yang Y.Q., Liu D., Li Z.H., Zhang X.R., et al. Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: a large cross-sectional study. J Affect Disord. 2020;275:188–193. doi: 10.1016/j.jad.2020.06.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.