Abstract
Background
The complete lockdown caused by the COVID-19 pandemic had imposed a new behavior and lifestyle especially in terms of diet, physical activity, and the management of patients with chronic diseases.
Aim
The present study aimed to analyze the impact of lockdown on the monitoring and care of type 2 diabetes mellitus (T2DM) patients in a Moroccan population from the Doukkala region.
Subjects and methods
We conducted a retrospective observational study including 121 T2DM patients recruited from the Diabetes Diagnosis and Treatment Center of El Jadida city. Demographic, anthropometric, and biochemical data of our T2DM patients were recorded before and after lockdown that lasted 82 days. All patients have signed an informed consent after being informed about the purely scientific aims of the study.
Results
Our sample involved 84 women and 37 men with an age average of 57.31 ± 0.91 years. The effects of lockdown were more marked in women than in men: women showed a significant tendency to gain weight (from 78.13 ± 1.36 kg to 81.80 ± 1.45 kg; p-value < 0.000), that impacted the body mass index (p-value < 0.000); they also showed significant increases in HbA1c values (p-value = 0.001), significant decrease in systolic blood pressure (p-value = 0.0302) and a surprising increase in high-density lipoprotein cholesterol (p-value = 0.0132). The prevalence of metabolic syndrome in the women sample increased from 46.4% to 54.8% after the lockdown. In men, the negative effect of lockdown was observed only in HbA1c that values increased significantly from 8.66 ± 0.21% to 9.51 ± 0.25% (p-value = 0.0127).
Conclusion
Our results reveal that lockdown had impacted negatively the health status of T2DM patients, especially women. We suggest an urgent development of programs aiming to improve the hygiene of life and to reduce the impact of future crises on patients suffering chronic diseases such as T2DM.
Keywords: COVID-19, SARS-CoV-2, Lockdown, Type 2 diabetes mellitus, Impact, Complications, Morocco
1. Introduction
The novel coronavirus (SARS-CoV-2) disease known as COVID-19 has arisen and spread very quickly around all the world, becoming pandemic [1]. Currently, it has led to more than 100 million cases of infection and more than 2 million deaths by the 20th February 2021. Towards the beginning of the pandemic, one of the measures adopted by the governments of different countries (especially the most affected ones) was the complete lockdown nationwide.
Since the detection of the first case of COVID-19, on the beginning of March 2020 [3], Morocco gradually puts in place a set of measures to counterattack its rapid spread. Nevertheless, during this period, around 480,948 cumulated cases of COVID-19 have been confirmed in Morocco, causing 8548 deaths [2].
In this way, by the 20th of March 2020, the Moroccan government decreed a full lockdown nationwide as a response to the state of health emergency [4]. It included a set of strict measures that have restricted the free movement of people (except those who present an authorization), requested the closure of public places, shortened the opening hours of shops, and reduced the maximum capacity of public transports [5].
This lockdown imposed brutal changes in the lifestyle and the behaviors of the populations, especially in terms of physical activity and diet, that are known to play an important role in the management of chronic diseases (like obesity, type 2 diabetes mellitus (T2DM), and coronary complications) [6,7]. Otherwise, the lockdown may have also impacted the monitoring of these chronic diseases by making difficult the medication access (eg. Insulin) and blood glucose tests, especially for people living in rural areas. Moreover, the lockdown might be an important source of anxiety and stress especially for patients with T2DM and coronary complications, since they have been considered as a high-risk group according to the scientific community and health authorities [5,8].
A systematic review showed that the national prevalence of T2DM in Morocco was 12.4% in 2016 [9]. Some regional studies in Morocco reported a prevalence of 13.5% in the general population of two cities in central Morocco (El Jadida and Khemisset) [10] and 19% among women in Meknes city [11]. In terms of management quality of this chronic disease in Moroccan patients, more than half fail to achieve the recommended care goals [12].
Despite the high prevalence of T2DM in Morocco, data on the lockdown effects are still lacking, while in other countries, studies underlined that the discontinuation of surveillance during the lockdown period has negatively affected patients with T2DM [[13], [14], [15], [16], [17]].
In this context, we carried out, for the first time in Morocco, a retrospective observational epidemiological study using anthropometric and biochemical data from T2DM patients, with the goal to analyze the impact of the COVID-19 pandemic’s lockdown on the monitoring and care of T2DM patients in the Doukkala region.
2. Subjects and methods
2.1. Subjects
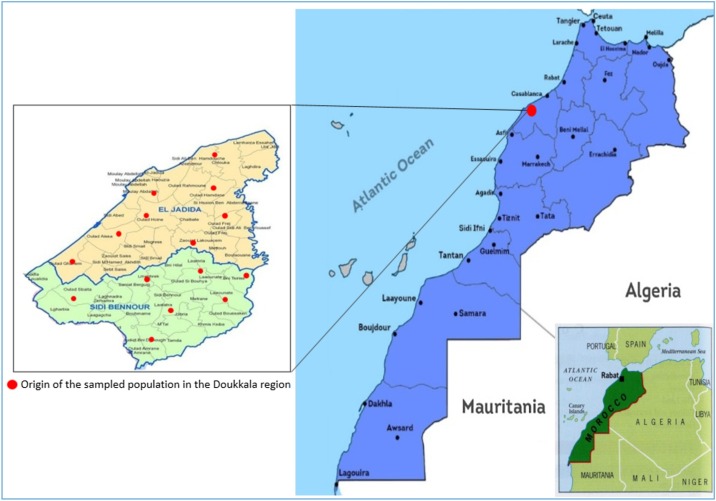
A total of 129 T2DM patients have initially met the eligibility criteria. Among them, 8 (6.2%) were excluded due to missing data. The final sample consisted of 121 patients (84 women and 37 men) aged between 36 and 85 years, all originate from the Doukkala region, Morocco (Fig. 1 ) and whose T2DM evolution is followed for at least one year. This sample was obtained from an institutional center of Diabetes Diagnosis and Treatment of El Jadida city, affiliated to the Moroccan Ministry of Health.
Fig. 1.
Map of the Doukkala region and its chief town El Jadida city (Morocco).
2.2. Ethical considerations
Our study was approved by the Moroccan Ministry of Health (Ref N°: 910 DELM/24) and all procedures followed the Helsinki declaration. The participants have provided a written informed consent after being informed about the purely scientific objectives and the interest of the study.
2.3. The study protocol
In this retrospective observational study, biochemical, socio-demographic, and anthropometric data were collected from each patient before lockdown (between the 1st November 2019 and 19th March 2020) and after lockdown (between 6th July 2020 and 29th December 2020) through their medical record and a well-established questionnaire.
Anthropometric measures were taken using the same protocol for all patients: subjects were weighed, without shoes and other items that could potentially add extra weight, and height was measured as the nearest centimeter while standing up using a wall stadiometer. Body mass index (BMI) was estimated using the standard formula. Stress caused by the family, job, grieving, and public road accident was noted by direct questions to the patients. Physical activity was assessed according to the guidelines of the minimum necessary activity [18,19]. Thus, patients practicing less than 30 min of moderate activity per day were considered physically inactive.
Biochemical parameters including fasting plasma glucose (FPG) [20], hemoglobin-A1c (HbA1c) [21], total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), triglycerides (TG) were assayed by the enzymatic spectrophotometric method [22]. Low-density lipoprotein cholesterol (LDL-C) values, were estimated using Friedewald's formula (for those with triglycerides below 4.5 g/L). Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured as recommended by the American Heart Association [23], using a standard mercury sphygmomanometer, after a rest period of at least 10 min. The threshold values for SBP and DBP were respectively 130 mmHg and 85 mmHg. Patients undergoing treatment were independently considered hypertensive. Finally, metabolic syndrome (MetS) was diagnosed according to the criteria of the International Diabetes Federation (IDF) [24].
2.4. Statistical analyzes
For continuous variables, anthropometric and biochemical data were summarized with descriptive statistics (mean value ± standard deviation) and compared both before and after the lockdown using a paired Student’s t-test. For categorical variables, data were presented as valid frequencies. All statistical analyzes were done using the SPSS package (IBM SPSS Statistics for Windows, version 25) [25]. The ggplot2 package [26] was used to produce the bar charts of weight, BMI, SBP, HbA1c, and HDL-C in R [27]. The significance level was set at 5 % for all statistical analyzes.
3. Results
The present study focused on 121 T2DM patients with an age average of 57.31 ± 0.91 years, including 84 women (69.4%) and 37 men (30.6%), and all living in the Doukkala region, Morocco. The socio-economic and environmental characteristics of the studied sample are summarized in Table 1 . The age of diabetes in our sample is comprised between one and thirty five years with an average of 9.97 ± 0.67 years. Most of them live in urban areas (63.6%) and are illiterate (57 %). About half (48.8%) can be considered sedentary because of their physical inactivity. Around 81% of our sample was affected by stress during the lockdown period.
Table 1.
Socio-demographic and environmental parameters by gender of the studied sample.
| Total (n = 121) | Women (n = 84) | Men (n = 37) | |
|---|---|---|---|
| Age, years (mean ± SD) | 57.31 ± 0.91 | 56.44 ± 1.10 | 59.30 ± 1.60 |
| Age of T2DM (mean ± SD) | 9.97 ± 0.67 | 9.52 ± 0.73 | 10.97 ± 1.36 |
| Residence, n (%) | |||
| Rural | 44 (36.4) | 29 (34.5) | 15 (40.5) |
| Urban | 77 (63.6) | 55 (65.5) | 22 (59.5) |
| Educational level, n (%) | |||
| Illiterate | 69 (57.0) | 59 (70.2) | 10 (27.0) |
| Primary | 25 (20.7) | 14 (16.7) | 11 (29.7) |
| Secondary | 13 (10.7) | 7 (8.3) | 6 (16.2) |
| Superior | 14 (11.5) | 4 (4.8) | 10 (27.0) |
| Physical activity, min/day (mean ± SD)A | 26. 56 ± 2.42 | 23.63 ± 2.97 | 33.21 ± 3.99 |
| Physical activity (<30 min/day)A, n (%) | |||
| No | 59 (48.8) | 47 (56.0) | 12 (32.4) |
| Yes | 62 (51.2) | 37 (44.0) | 25 (67.6) |
| StressA, n (%) | 98 (81.0) | 67 (79.76) | 31 (83.78) |
| Family | 56 (57.1) | 42 (62.7) | 14 (45.2) |
| Job | 19 (19.4) | 12 (17.9) | 7 (22.6) |
| Grieving | 7 (7.1) | 3 (4.5) | 4 (12.9) |
| MultistressB | 16 (16.3) | 10 (14.9) | 6 (19.4) |
T2DM: type 2 diabetes mellitus; SD: standard deviation.
Data obtained after lockdown.
Family, job, grieving, and public road accident.
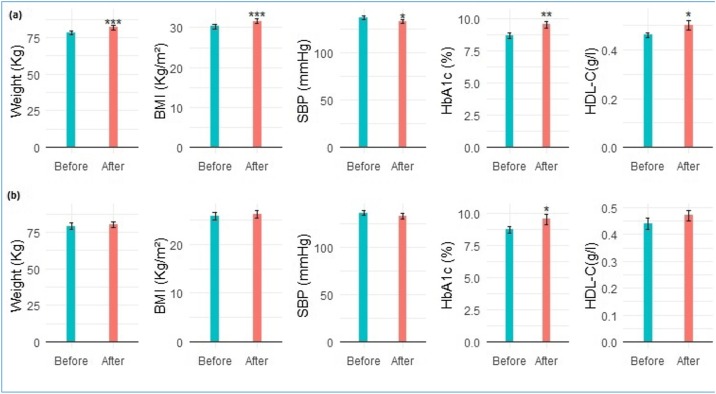
The anthropometric and biochemical parameters are represented in Table 2 . Concerning anthropometric parameters, the most striking observation was the discrepancy in results according to gender. In fact, after the lockdown, women showed a highly statistically significant increment in weight (p-value < 0.000), going from 78.13 ± 1.36 kg to 81.80 ± 1.45 kg. This last has also acted significantly on the BMI in women (p-value < 0.000) which went from 30.25 ± 0.54 kg/m2 before to 31.64 ± 0.57 kg/m2 after the lockdown (Fig. 2 ).
Table 2.
Anthropometric and biochemical parameters of patients before and after a lockdown in women and men.
| Women (n = 84) |
Men (n = 37) |
|||||
|---|---|---|---|---|---|---|
| Before | After | Before | After | |||
| Parameters | Mean ± SD | Mean ± SD | p-Value | Mean ± SD | Mean ± SD | p-Value |
| Weight (kg) | 78.13 ± 1.36 | 81.80 ± 1.45 | 0.0000 *** | 79.00 ± 2.29 | 80.24 ± 2.04 | 0.2401 NS |
| BMI (kg/m²) | 30.25 ± 0.54 | 31.64 ± 0.57 | 0.0000 *** | 25.73 ± 0.83 | 26.18 ± 0.76 | 0.1986 NS |
| SBP (mmHg) | 137.06 ± 2.06 | 132.88 ± 1.79 | 0.0302* | 136.41 ± 2.77 | 133.00 ± 2.96 | 0.1852 NS |
| DBP (mmHg) | 78.87 ± 1.13 | 78.55 ± 1.06 | 0.7802 NS | 79.35 ± 1.46 | 77.46 ± 1.65 | 0.2602 NS |
| FPG (g/L) | 1.84 ± 0.07 | 1.91 ± 0.08 | 0.4458 NS | 1.98 ± 0.17 | 1.99 ± 0.14 | 0.9413 NS |
| HbA1c (%) | 8.66 ± 0.21 | 9.51 ± 0.25 | 0.0010** | 8.69 ± 0.28 | 9.50 ± 0.40 | 0.0127 * |
| TC (g/L) | 1.88 ± 0.05 | 1.87 ± 0.04 | 0.8131 NS | 1.78 ± 0.08 | 1.78 ± 0.07 | 0.8875 NS |
| LDL-C (g/L) | 1.17 ± 0.05 | 1.10 ± 0.04 | 0.1978 NS | 0.97 ± 0.05 | 1.02 ± 0.05 | 0.3890 NS |
| HDL-C (g/L) | 0.46 ± 0.01 | 0.50 ± 0.02 | 0.0132* | 0.44 ± 0.02 | 0.47 ± 0.02 | 0.0543 NS |
| TG (g/L) | 1.50 ± 0.11 | 1.45 ± 0.11 | 0.3790 NS | 1.26 ± 0.09 | 1.32 ± 0.13 | 0.3540 NS |
| Uric acid (mg/L) | 44.14 ± 1.78 | 44.53 ± 1.77 | 0.6529 NS | 44.99 ± 2.71 | 47.35 ± 2.59 | 0.3233 NS |
| ALT (U/l) | 21.51 ± 1.15 | 20.31 ± 0.91 | 0.3049 NS | 21.84 ± 1.56 | 21.51 ± 1.40 | 0.7661 NS |
| AST (U/l) | 21.13 ± 1.13 | 20.85 ± 0.97 | 0.7853 NS | 21.81 ± 1.56 | 21.97 ± 1.77 | 0.8407 NS |
| Creatinine (mg/L) | 8.37 ± 0.26 | 8.52 ± 0.30 | 0.4194 NS | 9.74 ± 0.40 | 9.96 ± 0.40 | 0.5060 NS |
| Urea (g/L) | 0.31 ± 0.02 | 0.32 ± 0.01 | 0.5042 NS | 0.37 ± 0.02 | 0.36 ± 0.02 | 0.7474 NS |
SD: standard deviation; BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure; FPG: fasting plasma glucose; HbA1c: hemoglobin A1c; TC: Total cholesterol LDL-C: low-density lipoprotein-cholesterol; TG: triglyceride; HDL-C: high-density lipoprotein-cholesterol; ALT: alanine transaminase; AST: aspartate transaminase; NS: not significant.
Significant.
Highly significant.
Very highly significant.
Fig. 2.
Graphical representations of anthropometric and biochemical parameters before and after a lockdown in T2DM patients (women (a) and men (b)).
In terms of SBP (Fig. 2), we observed a significant reduction in women after the lockdown (p-value = 0.0302) but the value is still higher than the threshold value.
Among the biochemical parameters evaluated, only HbA1c and HDL-C showed significant variation after the lockdown (Table 2). HbA1c values have increased significantly from 8.66 ± 0.21% to 9.51 ± 0.25% (p-value = 0.001) in women and from 8.69 ± 0.28% to 9.50 ± 0.40% (p-value = 0.0127) in men (Fig. 2) which may indicate a morbid consequence.
About HDL-C (considered as good cholesterol), an increase was observed in both sexes (Fig. 2), but the variation was only significant in women (p-value = 0.0132).
For MetS (Table 3 ), a noticeable increment in its prevalence was observed only in women after lockdown. Indeed, the percentage went from 46.43% before to 54.76% after lockdown and could be linked to the increment of BMI (mandatory criterion of MetS according to the IDF definition).
Table 3.
The metabolic syndrome (MetS) as a complication of T2DM patients.
| Women |
Men |
|||
|---|---|---|---|---|
| Before (n = 39) | After (n = 46) | Before (n = 4) | After (n = 5) | |
| Metabolic syndrome n (%) | 39 (46.43) | 46 (54.76) | 4 (10.81) | 5 (13.51) |
| Factor1 + factor2, n (%) | 32 (82.1) | 41 (89.1) | 4 (100) | 5 (100) |
| Factor1 + factor3, n (%) | 25 (64.1) | 25 (54.3) | 2 (50) | 2 (40) |
| Factor1 + factor4, n (%) | 18 (46.2) | 19 (41.3) | 1 (25) | 2 (40) |
| Factor1 + factor2 + factor3, n (%) | 22 (56.4) | 25 (54.3) | 2 (50) | 2 (40) |
| Factor1 + factor2 + factor4, n (%) | 16 (41.0) | 19 (41.3) | 1 (25) | 2 (40) |
| Factor1 + factor2 + factor3 + factor4, n (%) | 15 (38.5) | 18 (39.1) | 1 (25) | 1 (20) |
Factor1: BMI > 30 kg/m², factor2: SBP ≥ 130 or DBP ≥ 85 mmHg or specific treatment, factor3: HDL-C < 0.4 g/L (men) and <0.5 g/L (women) or specific treatment, factor4: TG > 1.7 g/L or specific treatment. BMI: body mass index; SBP: systolic blood pressure; DBP: diastolic blood pressure; TG: triglyceride; HDL-C: high-density lipoprotein-cholesterol.
To verify and evaluate the profile of MetS on our T2DM patients, we established all the possible combinations of risk factors. Table 3 illustrates that the association of T2DM and “BMI > 30 kg/m2 + SBP ≥ 130 or DBP ≥ 85 mmHg or specific treatment” is the most frequent one particularly in women (82.1% before versus 89.1% after lockdown).
4. Discussion
The present work aimed to examine the effects of the national lockdown due to the COVID-19 pandemic on the state of health of Moroccan patients with T2DM. To our knowledge, this is the first Moroccan study that addresses this important topic. Globally, our results indicate that the lockdown had negatively impacted the health status of our T2DM patients, especially women. Indeed, significant deteriorations in both anthropometric and biochemical parameters have been observed after the lockdown. In congruence with previous studies, our patients have shown a tendency to gain weight and to increase their BMI after the lockdown [13,16,28,29]. However, only women showed a statistically significant increment in weight, which is known to be influenced by diet behaviors and physical activity [30]. During the lockdown, these factors were disturbed by a poor diet control and high limitation of physical activity. According to our data, the observed differences in weight gain between men and women could be explained by gender differences in familial stress and physical activity (Table 1). In this way, previous studies highlighted the gender differences in eating behavior in response to stress, anxiety, and reduced physical activity [29,31,32]. For example, it has been shown that, in Spanish patients with T2DM, women have increased their snack consumption, and sugary food during the lockdown period [33]. Concerning physical activity, our results reflect that men were likely more active than women. The benefits of physical activity are not to be demonstrated, in addition to their importance against stress, and obesity, they have innumerable positive effects on health by increasing endurance, resistance, immunity boost, …, and reducing the risk of cardiovascular diseases, T2DM, and other complications [33].
The SBP has shown a little betterment in our T2DM patients after the lockdown, even if these values remain higher than the thresholds indicated by IDF [24]. However, this variation was statistically significant in women while being non-significant in men. This improvement is most likely linked to the observed increases in HDL-C levels after the lockdown, as these ones contribute to the amelioration of lipid transport and normal blood pressure [34]. The increment of HDL-C in T2DM patients during the lockdown was also observed in other previous studies [28,33].
Concerning HbA1c, our findings highlight a significant increment in both sexes after the lockdown period, in congruence with previous studies [13,16,31,35]. This increment can be associated with both the duration of the lockdown, weight gain, and the deterioration in glycemic control [31,34,36,37]. This last result was observed also in T1DM patients in India after lockdown [37]. In contrast, the lockdown has improved the glycemic control in European patients with T1DM [38,39] and the authors suggested that having more time for self-management may help patients to improve their glycemic control.
For metabolic syndrome, only women showed an increased prevalence after the confinement. The incidence increased by about 8.33 %, which could increase the risk of micro-and macro-vascular complications and other comorbidities [40].
In summary, our results reveal that the 82 days of lockdown had impacted negatively the health status of T2DM patients in the Doukkala region – especially women. Some parameters as weight and HbA1c values have significantly increased, and a trend towards complications such as MetS was observed. These negative consequences could be attributed to the change in lifestyle, restrictions on medical monitoring, and non compliance with instructions. It seems urgent to develop awareness policies on the importance of a healthy diet, physical activity as well as the regular monitoring of the basic biochemical parameters (Glycaemia, HbAc1, and HDL-C …) that can constitute a major factor in improving the quality of life in the Moroccan population, especially those suffering chronic diseases. In the same way, emotional/mental support and telemedicine in times of crisis (such as lockdown period) can also be recommended to better deal with stress, and to ensure follow-up of the patients in remote areas.
Conflict of interests
None.
Funding resources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Acknowledgments
The authors thank all patients for their participation in the study, and all the staff of the “Diabetes Diagnosis and Traitment Center of El Jadida” for their disposition.
References
- 1.Lai C.-C., Shih T.-P., Ko W.-C., Tang H.-J., Hsueh P.-R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrobial Agents. 2020;55:105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moroccan-Ministry-of-Health . 2021. The Official Coronavirus Portal in Morocco. Available: http://www.covidmaroc.ma/Pages/Accueilfr.aspx (Accessed 21 February 2021. [Google Scholar]
- 3.WHO . World Health Organization; 2020. Coronavirus Disease 2019 (COVID-19): Situation Report, 43. 03-03. [Google Scholar]
- 4.Xinhua . 2020. Morocco Declares 1-Month State of Medical Emergency Over COVID-19. March 23. Available: http://www.china.org.cn/world/Off_the_Wire/2020-03/23/content_75846513.htm (Accessed 26 February 2021) [Google Scholar]
- 5.CESE . Conseil Economique, Social et Environnemental; 2020. Les impacts sanitaires, économiques et sociaux de la pandémie de la “Covid-19” et leviers d’actions envisageables.https://www.cese.ma/ [Google Scholar]
- 6.World-Health-Organization . 2018. Morocco: World Health Day "together against diabetes". Available: http://www.emro.who.int/fr/mor/morocco-news/journee-mondiale-de-la-sante-ensemble-contre-le-diabete.html (Accessed 23 February 2021) [Google Scholar]
- 7.World-Health-Organization . 2017. Cardiovascular diseases (CVDs) Available: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (Accessed 27 February 2021) [Google Scholar]
- 8.HCP . 2020. Enquête sur l’impact du coronavirus sur la situation économique, sociale et psychologique des ménages: note de synthèse des principaux résultats.https://www.hcp.ma/Enquete-sur-l-impact-du-coronavirus-sur-la-situation-economique-sociale-et-psychologique-des-menages-Note-de-synthese_a2506.html April 23. [Google Scholar]
- 9.W. H. Organization . 2018. Noncommunicable diseases country profiles 2018. [Google Scholar]
- 10.Gharbi M.B., Elseviers M., Zamd M., Alaoui A.B., Benahadi N., Trabelssi E.H. Chronic kidney disease, hypertension, diabetes, and obesity in the adult population of Morocco: how to avoid “over”-and “under”-diagnosis of CKD. Kidney Int. 2016;89:1363–1371. doi: 10.1016/j.kint.2016.02.019. [DOI] [PubMed] [Google Scholar]
- 11.El Boukhrissi F., Bamou Y., Ouleghzal H., Safi S., Balouch L. Prevalence of risk factors for cardiovascular disease and metabolic syndrome among women in the region of Meknes, Morocco. Médecine des maladies Métaboliques. 2017;11:188–194. [Google Scholar]
- 12.Ahmed Chetoui K.K., El Kardoudi A., Boutahar K., Chigr F., Najimi M. Epidemiology of diabetes in Morocco: review of data, analysis and perspectives. Int. J. Scientific Eng. Res. 2018;9:1310–1316. [Google Scholar]
- 13.Önmez A., Gamsızkan Z., Özdemir Ş., Kesikbaş E., Gökosmanoğlu F., Torun S. The effect of COVID-19 lockdown on glycemic control in patients with type 2 diabetes mellitus in Turkey. Diabetes Metab. Syndr. 2020;14:1963–1966. doi: 10.1016/j.dsx.2020.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Verma A., Rajput R., Verma S., Balania V.K., Jangra B. Impact of lockdown in COVID 19 on glycemic control in patients with type 1 diabetes mellitus. Diabetes Metab. Syndr. 2020;14:1213–1216. doi: 10.1016/j.dsx.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khare J., Jindal S. Observational study on effect of lock down due to COVID 19 on glycemic control in patients with diabetes: experience from Central India. Diabetes Metab. Syndr. 2020;14:1571–1574. doi: 10.1016/j.dsx.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khare J., Jindal S. Observational study on effect of lock down due to COVID 19 on HBA1c levels in patients with diabetes: experience from Central India. Prim. Care Diabetes. 2021 doi: 10.1016/j.pcd.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Khader M.A., Jabeen T., Namoju R. A cross sectional study reveals severe disruption in glycemic control in people with diabetes during and after lockdown in India. Diabetes Metab. Syndr. 2020;14:1579–1584. doi: 10.1016/j.dsx.2020.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.t. World Health Organization . World Health Organization; 2010. Global Recommendations on Physical Activity for Health. [PubMed] [Google Scholar]
- 19.D’Isanto T., Manna A., Altavilla G. Health and physical activity. Sport Sci. 2017;10:100–105. [Google Scholar]
- 20.Zhong Q., Chen Y., Qin X., Wang Y., Yuan C., Xu Y. Colorimetric enzymatic determination of glucose based on etching of gold nanorods by iodine and using carbon quantum dots as peroxidase mimics. Microchim. Acta. 2019;186:161. doi: 10.1007/s00604-019-3291-2. [DOI] [PubMed] [Google Scholar]
- 21.Khashoggi H., Pignalosa S., Russo C., Pieri M., Bernardini S. New HPLC instrument performance evaluation in HbA1c determination and comparison with capillary electrophoresis. Scand. J. Clin. Lab. Invest. Suppl. 2018;78:393–397. doi: 10.1080/00365513.2018.1487072. [DOI] [PubMed] [Google Scholar]
- 22.McNamara J.R., Schaefer E.J. Automated enzymatic standardized lipid analyses for plasma and lipoprotein fractions. Clin. Chim. Acta. 1987;166:1–8. doi: 10.1016/0009-8981(87)90188-4. [DOI] [PubMed] [Google Scholar]
- 23.Perloff D., Grim C., Flack J., Frohlich E.D., Hill M., McDonald M. Human blood pressure determination by sphygmomanometry. Circulation. 1993;88:2460–2470. doi: 10.1161/01.cir.88.5.2460. [DOI] [PubMed] [Google Scholar]
- 24.Federation I.D. The IDF consensus worldwide definition of the metabolic syndrome. IDF Commun. 2006:1–24. [Google Scholar]
- 25.Spss I. IBM SPSS Corp. [Google Scholar]; Armonk, NY: 2017. IBM SPSS Statistics for Windows, Version 25. [Google Scholar]
- 26.Wickham H. ggplot2. Wiley Interdiscip. Rev. Comput. Stat. 2011;3:180–185. [Google Scholar]
- 27.R. Developer Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2019. R: A Language and Environment for Statistical Computing. [Google Scholar]
- 28.Karatas S., Yesim T., Beysel S. Impact of lockdown COVID-19 on metabolic control in type 2 diabetes mellitus and healthy people. Prim. Care Diabetes. 2021 doi: 10.1016/j.pcd.2021.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pellegrini M., Ponzo V., Rosato R., Scumaci E., Goitre I., Benso A. Changes in weight and nutritional habits in adults with obesity during the “lockdown” period caused by the COVID-19 virus emergency. Nutrients. 2020;12:2016. doi: 10.3390/nu12072016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fidler Mis N., Braegger C., Bronsky J., Campoy C., Domellöf M., Embleton N.D. Sugar in infants, children and adolescents: a position paper of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition Committee on Nutrition. J. Pediatr. Gastroenterol. Nutr. 2017;65:681–696. doi: 10.1097/MPG.0000000000001733. [DOI] [PubMed] [Google Scholar]
- 31.Alshareef R., Al Zahrani A., Alzahrani A., Ghandoura L. Impact of the COVID-19 lockdown on diabetes patients in Jeddah, Saudi Arabia. Diabetes Metab. Syndr. 2020;14:1583–1587. doi: 10.1016/j.dsx.2020.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zachary Z., Brianna F., Brianna L., Garrett P., Jade W., Alyssa D. Self-quarantine and weight gain related risk factors during the COVID-19 pandemic. Obes. Res. Clin. Pract. 2020 doi: 10.1016/j.orcp.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ruiz-Roso M.B., Knott-Torcal C., Matilla-Escalante D.C., Garcimartín A., Sampedro-Nuñez M.A., Dávalos A. COVID-19 lockdown and changes of the dietary pattern and physical activity habits in a cohort of patients with type 2 diabetes mellitus. Nutrients. 2020;12:2327. doi: 10.3390/nu12082327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nasri H., Yazdani M. The relationship between serum LDL-cholesterol, HDL-cholesterol and systolic blood pressure in patients with type 2 diabetes. Kardiol. Pol. 2006;64:1364–1368. [PubMed] [Google Scholar]
- 35.Ghosal S., Sinha B., Majumder M., Misra A. Estimation of effects of nationwide lockdown for containing coronavirus infection on worsening of glycosylated haemoglobin and increase in diabetes-related complications: a simulation model using multivariate regression analysis. Diabetes Metab. Syndr. 2020 doi: 10.1016/j.dsx.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gummesson A., Nyman E., Knutsson M., Karpefors M. Effect of weight reduction on glycated haemoglobin in weight loss trials in patients with type 2 diabetes. Diabetes Obes. Metab. 2017;19:1295–1305. doi: 10.1111/dom.12971. [DOI] [PubMed] [Google Scholar]
- 37.Verma A., Rajput R., Verma S., Balania V.K., Jangra B. Impact of lockdown in COVID 19 on glycemic control in patients with type 1 diabetes mellitus. Diabetes Metab. Syndr. 2020;14(5):1213–1216. doi: 10.1016/j.dsx.2020.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fernández E., Cortazar A., Bellido V. Impact of COVID-19 lockdown on glycemic control in patients with type 1 diabetes. Diabetes Res. Clin. Pract. 2020;166 doi: 10.1016/j.diabres.2020.108348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dover A.R., Ritchie S.A., McKnight J.A., Strachan M.W.J., Zammitt N.N., Wake D.J., Forbes S., Stimson R.H., Gibb F.W. Assessment of the effect of the COVID-19 lockdown on glycaemic control in people with type 1 diabetes using flash glucose monitoring. Diabet. Med. 2021;38(1) doi: 10.1111/dme.14374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chung H.S., Seo J.A., Kim S.G., Kim N.H., Kim D.M., Chung C.H. Relationship between metabolic syndrome and risk of chronic complications in koreans with type 2 diabetes. Korean Diabetes J. 2009;33:392–400. [Google Scholar]