Abstract
Mobile health tools may overcome barriers to social needs screening; however, there are limited data on the feasibility of using these tools in clinical settings. The objective was to determine the feasibility of using a mobile health system to screen for patients' social needs. In one large primary care clinic, the authors tested a tablet-based system that screens patients for social needs, transmits results to the electronic health record, and alerts providers. All adult patients presenting for a nonurgent visit were eligible. The authors evaluated the feasibility of the system and conducted follow-up surveys to determine acceptability and if patients accessed resources through the process. All providers were surveyed. Of the 252 patients approached, 219 (86.9%) completed the screen. Forty-three (19.6%) required assistance with the tablet, and 150 (68.5%) screened positive for at least 1 unmet need (food, housing, or transportation). Of the 150, 103 (68.7%) completed a follow-up survey. The majority agreed that people would learn to use the tablet quickly. Forty-eight patients (46.6%) reported contacting at least 1 community organization through the process. Of the 27 providers, 23 (85.2%) completed a survey and >70% agreed the system would result in patients having better access to resources. It was feasible to use a tablet-based system to screen for social needs. Clinics considering using mobile tools will need to determine how to screen patients who may need assistance with the tool and how to connect patients to resources through the system based on the burden of unmet needs.
Keywords: social determinants of health, health-related social needs, mobile health, health information technology, feasibility
Introduction
Social determinants of health (SDH), or the conditions in which people are born, grow, live, and age, have a profound impact on morbidity and mortality,1,2 and SDH have a greater impact on health than health care.2,3 SDH can lead to unmet social needs (eg, food insecurity, housing instability) that are associated with worse health.2,4 Given the prevalence and potential to lead to poor health, national organizations have recommended that health systems address patients' unmet social needs as part of clinical care.4–6 The National Academy of Medicine has specifically recommended that health systems capture social domains in the electronic health record (EHR) to improve population health.7,8
Given these national recommendations, a growing body of research has examined interventions to address patients' unmet social needs in clinical care settings. These studies have found that these interventions can improve patients' access to resources and may improve health outcomes.9–12 One area that remains unclear is how to effectively implement these strategies in busy clinical settings.13,14 Although health care providers recognize the impact that SDH have on patients' health, few routinely screen patients for social needs.15,16 Barriers to screening include a perceived lack of time, a limited understanding of how to address social needs, and the absence of tools to integrate interventions into the clinical workflow.16–18
One method that may overcome these barriers is mobile health technology. Mobile health tools, such as tablets that include health-related applications, have shown promise in addressing unmet social needs by connecting patients to community resources and reducing disparities in care by improving the receipt of preventive services.19–24 Mobile health tools have the potential to overcome barriers to screening for unmet social needs because they can collect patient-reported data without interfering with clinic workflow, provide patients with appropriate resources, and have the potential to integrate with the EHR.22,25,26 Although there has been growing interest in using mobile tools to address patients' unmet social needs,19,20,24,27 there are limited data about the feasibility of implementing these tools in busy clinical practices and patients' comfort with using them, particularly in clinics that serve low-income populations at high risk of having unmet social needs.
The primary objective of this study was to determine the feasibility and acceptability of using a mobile health system that allows patients to self-screen for social needs, transmits results to the EHR, and automatically alerts clinic providers of patients with unmet needs. The secondary objectives were to determine the efficacy of the system and the patient characteristics associated with screening positive in a clinic serving a predominantly low-income, underrepresented minority population.
Methods
Study design and setting
This single-arm study was conducted at an urban, community-based adult primary care clinic affiliated with Wake Forest Baptist Health (WFBH). The clinic is the largest primary care outpatient department in the WFBH system and the largest provider of Medicaid services in the state. The clinic provides care for more than 25,000 patients a year, more than 70% of whom are underrepresented minorities. The clinic serves as a teaching site for the internal medicine residency program and is staffed by 7 attending physicians, 4 advanced practice practitioners (APPs), 9 nurses, and 7 staff members. The clinic also has an on-site patient navigator, who is available to assist patients with accessing resources. Prior to this study, the adult primary care clinic was not systematically screening patients for social needs. The clinic uses EpicCare EHR (Epic Systems Corporation, Verona, WI).
Intervention
Through discussions with clinicians and patients, the research team developed a tablet-based digital health system to address patients' unmet social needs. The tablet used the existing electronic patient portal data capture function to assess patient-reported outcomes and incorporated questions from the Centers for Medicare & Medicaid Services Accountable Health Communities Core Health-Related Social Needs Questionnaire (in English and Spanish).12
For patients who agreed to participate in the study, a study coordinator would log in to the patient's electronic portal to access the questions on a tablet and tell the patient how to enter data. The coordinator was available to assist the patient if he/she requested help. Two questions were included to screen for food security, 2 questions were about housing, and 1 question assessed for lack of transportation (Table 1). These 3 domains (food, housing, and transportation) were chosen because the clinic providers and staff felt that these would be the highest needs for the patient population and there were local resources available to address patients' needs. Patients' responses were transmitted automatically and recorded in the clinical flow sheets in the EHR.
Table 1.
Tablet-Based Unmet Social Need Questionnaire
| Food security |
| 1. Within in the past 12 months, you worried that your food would run out before you got money to buy more. |
| [] Often true |
| [] Sometime true |
| [] Never true |
| 2. Within in the past 12 months, the food you bought just didn't last and you didn't have money to get more. |
| [] Often true |
| [] Sometime true |
| [] Never true |
| Housing |
| 3. What is your housing situation today? |
| [] I do not have housing (I am staying with others, in a hotel, in a shelter, living outside on the street, on a beach, in a car, abandoned building, bus or train station, or in a park) |
| [] I have housing today, but I am worried about losing housing in the future. |
| [] I have housing |
| 4. Think about the place you live. Do you have problems with any of the following? (check all that apply) |
| [] Bug infestation |
| [] Mold |
| [] Lead paint or pipes |
| [] Inadequate heat |
| [] Oven or stove not working |
| [] No or not working smoking detectors |
| [] Water leaks |
| [] None |
| Transportation |
| 5. Within the past 12 months, has lack of transportation kept you from medical appointments or from doing things needed for daily living? |
| [] Yes |
| [] No |
Questions included in tablet-based digital health system. A response of “sometimes true” or “often true” to either food insecurity question was considered a positive screen. Patients were considered to have a positive screen for problems with housing if they responded to the first question with any response other than “I have housing” or “none” to the second housing question. Patients were considered to have a positive screen for lack of transportation if they responded “yes” to the transportation question.
For those who screened positive for any unmet social needs, the system automatically provided a list of community resources in the patients' after visit summary. The list of resources included information about local organizations (eg, food pantries, organizations that assist with housing) and was developed after a review of all the available community-based organizations in the area. The system would only provide information on resources for the unmet need the patient reported. For example, if a patient screened positive for food insecurity, he/she would only receive the information about food resources. Additionally, the system sent an automated message in the EHR to notify the clinician who would be seeing the patient and the clinic's patient navigator that the patient had screened positive. If available, the navigator would meet with the patient at the time of the visit. If not, the navigator would contact the patient by phone to assess if the patient wanted further assistance.
Participant recruitment
From December 2018 to February 2019, the research team randomly selected 15 clinic sessions (1/2-day sessions) to screen patients using the tablet. All patients (ages ≥18 years) who presented for a nonurgent visit (eg, physical, return visit) during one of the selected sessions and spoke either English or Spanish were eligible. A study coordinator attempted to approach every patient in the waiting room prior to the scheduled visit.
Outcome measures
Feasibility
The RE-AIM (reach, effectiveness, adoption, implementation, maintenance) framework28 was used to assess the outcomes in this study. The research team evaluated number of patients eligible to be screened, the number who were able to complete the screen, and the results of the screen through data extraction from the EHR. The primary outcome was the feasibility of the system, and feasibility was defined as the reach or the proportion of patients approached who were able to complete the screen.
Acceptability
For all patients identified as having 1 unmet need, the team conducted 1-month follow-up phone surveys. The survey included questions from the System Usability Scale (SUS). SUS is a validated instrument used to measure the usability of a tool or system.29 The 3 items from the SUS that were most relevant to this study (ease of use, ease of learning to use the program, confidence using the program) were used and responses were measured on a 5-point Likert scale from strongly agree to strongly disagree.29,30 Study staff tried up to 5 times to call patients to complete the follow-up survey.
At the end of the study period, an online survey was conducted with providers at the clinic. All 27 providers (attending physicians, APPs, nurses, and staff members) were eligible to complete the survey. Questions included concerned providers' acceptance of the process, facilitators and barriers, and the effect on clinic workflow based on questions from the provider acceptability survey developed by the Ottawa Hospital Research Institute.31 The team also assessed provider characteristics including age, sex, race/ethnicity, provider type, and number of years in practice. Providers were initially sent the survey followed by a reminder email once a week for 3 additional weeks.
Efficacy
During the 1-month follow-up surveys with patients, the research team assessed if patients reported accessing any resources through the process. The team also assessed if patients learned about any new resources.
Covariates
For all patients eligible to be screened, we team obtained age, sex, race/ethnicity (white, African American, Hispanic, or other/unknown) through data extraction from the EHR. The team also assessed insurance type (private, public, or self-pay) and patients' Charlson comorbidity index (CCI), which was calculated based on the diagnoses listed in the patients' medical record and categorized as none, mild, moderate, or severe.32
Statistical analysis
Bivariate analyses were performed to test the association between all covariates and if a patient reported having at least 1 unmet social need using chi-square test. The team then evaluated the association between all covariates and if a patient reported having at least 1 unmet social need using multivariable logistic regression. Additionally, bivariate analyses and multivariable logistic regression were performed to evaluate the association between covariates and if a patient reported accessing at least 1 community resource. A 2-sided hypothesis test was used and α <0.05 was considered significant. All analyses were conducted using Stata 15.0 (StataCorp LLC, College Station, TX). The Wake Forest School of Medicine Institutional Review Board approved this study.
Results
Feasibility
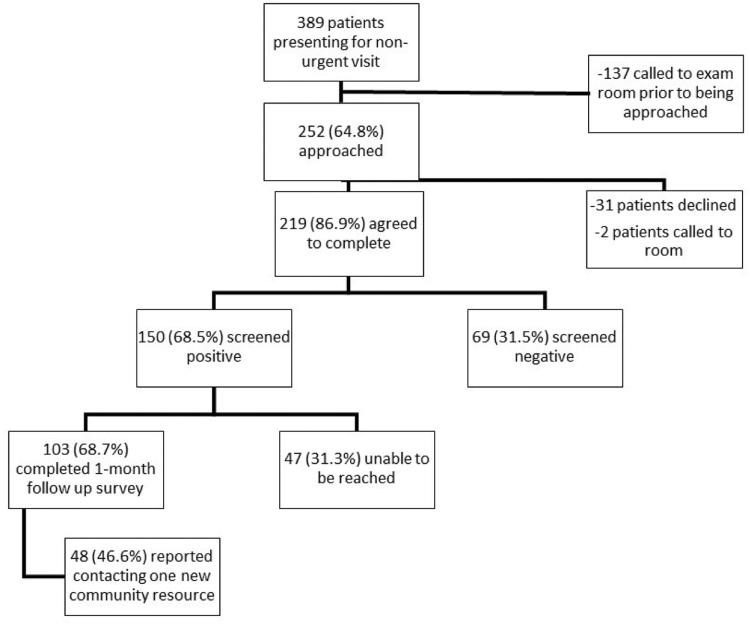
In the 15 half-day sessions selected, 389 patients were eligible. Of the eligible patients, 252 (64.8%) were approached by the study coordinator, and the other 137 patients were called back to the exam room before they could be approached (Figure 1). There were no significant differences in covariates (age, sex, race/ethnicity, insurance, or CCI) between patients who were approached and those who were not. Of the 252 patients, 31 (12.3%) declined and 221 (87.7%) agreed to complete the tablet screening. There were no significant differences in covariates between those who agreed and those who declined. Of the 31 who declined; 13 reported they did not need or qualify for resources, 5 reported that they did not have time, 1 required a sign language interpreter, and 12 did not provide a reason.
FIG. 1.
Study flow diagram.
Of the 252 patients approached, 219 patients (86.9%) completed the tablet-based screen (2 were called to the visit room prior to starting). Of the 219 patients, 43 patients (19.6%) required assistance (eg, reading the questions, help entering responses). The 219 patients who completed the tablet-based screening had a similar mean age, sex, race/ethnicity, and payor mix to the overall population seen at the clinic. The majority of patients who completed the screen were female, African American, and had public insurance (Table 2). Approximately two thirds (68.5%, n = 150) screened positive for at least 1 unmet social need (116 [53.0%] for food insecurity, 86 [39.3%] for housing problems, and 74 [33.8%] for lack of transportation). In bivariate analysis, patients who screened positive were more likely to not have insurance (28.0% vs 13.0%, P = 0.02), but there were no significant differences in other covariates. In multivariable analysis, there were no significant differences in covariates between patients who screened positive and those who screened negative.
Table 2.
Bivariate Analysis of Study Population Characteristics
| Total (N = 219) | Screen (-) (n = 69) | Screen (+) (n = 150) | P | ||
|---|---|---|---|---|---|
| Sex | 0.50 | ||||
| Male | 93 (42.5) | 27 (39.1) | 66 (44.0) | ||
| Female | 126 (57.5) | 42 (60.9) | 84 (56.0) | ||
| Age (SD) | 53.8 (13.8) | 54.0 (15.8) | 53.7 (12.9) | 0.86 | |
| Range (18–86 years) | |||||
| Race/Ethnicity | 0.64 | ||||
| Black | 140 (63.9) | 42 (60.9) | 98 (65.3) | ||
| White | 50 (22.8) | 19 (27.5) | 31 (20.7) | ||
| Hispanic | 28 (12.8) | 8 (11.6) | 20 (13.3) | ||
| Other | 1 (0.5) | 0 (0.0) | 1 (0.7) | ||
| Insurance | 0.02 | ||||
| Public | 159 (72.6) | 55 (79.7) | 104 (69.3) | ||
| Private | 9 (4.1) | 5 (7.3) | 4 (2.7) | ||
| None | 51 (23.3) | 9 (13.0) | 42 (28.0) | ||
| Charlson Comorbidity Index | 0.23 | ||||
| None | 48 (21.9) | 20 (29.0) | 28 (18.7) | ||
| Mild | 73 (33.3) | 22 (31.9) | 51 (34.0) | ||
| Moderate | 28 (12.8) | 7 (10.1) | 21 (14.0) | ||
| Severe | 42 (19.2) | 15 (21.7) | 27 (18.0) | ||
| Missing | 28 (12.8) | 5 (7.3) | 23 (15.3) |
SD, standard deviation.
Patient and provider acceptability
Patient
Of the 150 patients who screened positive, 103 (68.7%) completed a 1-month follow-up survey. There were no significant differences in covariates between those who completed a follow-up survey and those who did not. The majority of respondents either agreed or strongly agreed that the tablet-based system was easy to use (81.6%), thought most people would learn to use the tablet quickly (85.4%), and felt very confident using it (87.4%).
Provider
Of the 27 providers eligible, 23 (85.2%) completed the acceptability survey. Of the 23 respondents, 7 (30.4%) were attending physicians, 4 (17.4%) were APPs, 8 (34.9%) were nurses, and 4 (17.4%) were other staff members (eg, front desk staff). Respondents had practiced a median of 22 years (range 1–42 years) and had been at the clinic for a median of 4 years (range 1–29 years). The majority (N = 17; 73.9%) were female. Eight respondents (27.6%) reported “always” asking patients about unmet social needs prior to the start of the study. More than 80% of respondents agreed or strongly agreed that it is essential for the clinic to provide information about community resources (Table 3). More than 70% agreed or strongly agreed that using the system was compatible with the way things should be done, would result in patients having better access to resources, and was a suitable method to assist patients. Eleven (47.8%) providers agreed or strongly agreed that the system would save time, and only 2 (8.7%) providers disagreed or strongly disagreed. The remaining 10 (43.5%) felt it would neither save nor increase time. One provider did report that she was worried that implementing screening would create expectations for patients about resources that the clinic would be unable to fulfill.
Table 3.
Provider Acceptability
| Never (N (%)) | Sometimes (N (%)) | Always (N (%)) | |
|---|---|---|---|
| Prior to this study, how often did you ask patients about any social needs that they may have? | 3 (13.0) | 12 (52.2) | 8 (34.8) |
| Strongly agree/agree (N (%)) | Neither (N (%)) | Strongly disagree/disagree (N (%)) | |
| It is essential our clinic provide information about resources to address the following: | |||
| 1. Food | 19 (82.6) | 2 (8.7) | 2 (8.7) |
| 2. Housing | 19 (82.6) | 2 (8.7) | 2 (8.7) |
| 3. Transportation | 20 (87.0) | 2 (8.7) | 1 (4.4) |
| In general, the tablet-based screening process: | |||
| 1. This strategy is compatible with the way I think things should be done | 18 (78.3) | 4 (17.4) | 1 (4.4) |
| 2. This strategy is more cost-effective that my usual approach to helping patients with unmet social needs | 11 (47.8) | 8 (34.8) | 4 (17.4) |
| 3. Compared with my usual approach, this strategy will result in my patients having better access to resources | 17 (73.9) | 5 (21.7) | 1 (4.4) |
| 4. Using this strategy will save me time | 11 (47.8) | 10 (43.5) | 2 (8.7) |
| 5. This strategy is a reliable method of helping patients with unmet social needs | 15 (65.2) | 7 (30.4) | 1 (4.4) |
| 6. Pieces or components of this strategy can be used by themselves | 14 (60.9) | 7 (30.4) | 2 (8.7) |
| 7. This strategy is suitable for helping patients access resources | 18 (78.3) | 4 (17.4) | 1 (4.4) |
| 8. Using this strategy does not involve making major changes to the way I usually do things | 15 (65.2) | 4 (17.4) | 4 (17.4) |
| 9. There is a high probability that using this strategy may cause/result in more benefit than harm | 16 (69.6) | 2 (8.7) | 5 (21.7) |
Efficacy
Of the 103 patients who completed a follow-up survey, 48 (46.6%) reported contacting at least 1 community organization through the process. There were no significant differences in covariates between patients who contacted an organization and those who did not. Eighty-seven (84.5%) respondents agreed or strongly agreed that the resources were helpful and that they learned about new resources through the process.
Discussion
This study found that it was feasible to use a mobile health system to screen patients for unmet social needs as 86.9% of patients approached completed the screening and 68.5% were identified as having at least 1 unmet need. Additionally, this study found that both patients and providers found it acceptable to use the system in the clinic. The referral process used also was efficacious in assisting patients with obtaining resources. This study adds to the growing body of social prescribing research by showing that it is feasible and acceptable to screen for patients' unmet social needs using mobile tools in a busy clinical setting that serves a predominantly low-income population.
Few clinicians routinely screen for social needs because they feel they lack the time, knowledge, and tools to address social risk factors in busy clinical settings.16–18 Mobile health tools could be a method to overcome these barriers.22,25,26 Patients from vulnerable populations at high risk for unmet needs may have difficulty with or feel uncomfortable completing questionnaires on a tablet.33,34
This study found that using a tablet to assess patients' food, housing, and transportation needs was feasible. However, almost 20% of patients did require assistance with the tablet, such as help with entering responses and needing someone to read the questions. The research team did not assess if this was because of patient preference or literacy issues. Clinics considering implementing mobile tools to screen for social needs, though, should consider how to screen patients who may have difficulty with the tool, as one fifth of patients may need assistance.
In addition to overcoming clinic barriers to integrating social needs screening, using a tablet-based system may be a more effective and efficient manner to screen than verbally asking patients or using a written questionnaire. Prior studies have noted that patients screened for social needs are more likely to screen positive when using a tablet or paper-based form compared to the clinician asking verbally.19,27,35 This could be because of fear or social desirability, but patients have been more likely to report sensitive information when they are asked “anonymously.” Additionally, over time providers often modify verbal screening questions, which can result in the validity of a survey tool being weakened; this would not occur with an electronic or paper-based screen. Using a paper-based form creates an additional step of requiring a person to enter the data in the EHR.14 The team used the data capture functionality that is already available in the electronic patient portal with the digital health system, so the screening results were directly captured in the EHR.
Despite 20% of patients needing assistance, the majority of respondents in the follow-up survey reported that the tablet was easy to use and thought most people would be able to learn to use the tablet quickly. Providers had a similarly positive response. More than 70% of respondents felt that using a digital health tool was a suitable method to assist patients and would result in patients having better access to resources. Approximately half of providers even thought that the system would save time.
One provider raised concerns, not with the tablet itself, but that implementing screening would create expectations from patients that the clinic would be unable to meet. Patients and families are supportive of clinics screening for unmet social needs because of the impact social factors have on health and because conducting screening shows that the clinic cares about the broader social issues affecting patients.36–38 Patients and families also do not necessarily expect the clinic to address all of their social needs.36,37
Although it was not one of the primary objectives, the research team did find that the tool was efficacious in connecting patients with resources. Several recent studies have shown that tablet-based tools are a potentially effective method to connect individuals to resources. Although there are differences in the type of social needs screened for in the studies and the outcomes assessed, the team found similar results in the number of patients who reported obtaining resources through these mobile tools.19,20,24,27 Further research is needed to determine if mobile tools that address patients' unmet social needs are effective in improving health.
For health systems interested in implementing tablet-based social needs screening, a key question will be determining how clinics will connect patients to resources. Even though prior studies have reported that 30%–50% of patients decline assistance,10,39 the team provided all patients who screened positive with a list of community resources and notified the clinic patient navigator. This was done because, through discussions with the clinic in developing the system, providers felt more comfortable providing information and notifying the navigator of everyone who screened positive. Additionally, one study found that patients who receive information about community resources in clinical settings often share this information with family and friends.40
With 69% of patients screening positive though, it was a large volume of patients for a single navigator to contact, assess interest, and provide assistance. Although in-person assistance may be more effective,11 balancing the ability of clinic staff to provide more comprehensive assistance with the proportion of patients with unmet needs will be increasingly important for health systems to consider as social needs screening becomes more prevalent. Also, developing methods to send automated referrals or directly connect patients to community resources may be needed. Since the study period, the tool has been modified to include a question asking if patients are interested in receiving assistance in order to focus on those who are most interested in obtaining resources and reduce the burden on clinic personnel.
Limitations
There are several limitations to this study that should be acknowledged. First, this study occurred at 1 clinic site that serves a predominantly low-income population, so the results may not be generalizable to other clinics. The clinic is the largest provider of Medicaid services in the state, so this study does provide important data on the feasibility of integrating social needs screening using a mobile device in a population at high risk of having unmet needs.
Second, the research team was only able to determine if participants accessed resources by self-report. At the time of this study, North Carolina began implementing NCCARE360, the first statewide resource platform to allow for electronic referrals to community resources and to notify providers if individuals connect to those resources (https://www.ncdhhs.gov/about/department-initiatives/healthy-opportunities/nccare360). The digital health system tested in the present study could be integrated with this platform and allow for more direct measures to assess if patients obtain resources. Third, patients who screened positive received both a paper-based list of resources and were able to meet with the patient navigator, so it is not clear if one or both interventions increased patients' access to resources.
Conclusion
As an increasing number of clinics and health systems are interested in addressing patients' unmet social needs, further research is needed to understand how social needs screening can most effectively and efficiently be implemented in busy clinical practices. There is growing interest in using mobile tools to collect patient-reported data on social factors, and this study found that it is feasible and acceptable to patients and providers to use a mobile health system to screen patients for social needs. Almost 20% of patients needed assistance, though, and a larger number of patients screened positive for unmet needs than expected. Clinics considering using mobile tools will need to consider how to screen patients who may need assistance with the tool and how the tool can best connect patients to resources based on the burden of unmet social needs in the clinic.
Acknowledgments
We would like to thank Petro Gjini for his assistance with data collection. We could like to thank the patients, staff, and clinicians at the Wake Forest Downtown Health Plaza for their assistance, participation, and engagement in the study.
Author Disclosure Statement
The authors declare that there are no conflicts of interest.
Funding Information
This study was supported by the Wake Forest Department of Internal Medicine and the Center for Healthcare Innovation. Dr. Palakshappa is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award number K23HL146902. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funding organization had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- 1. Solar O, Irwin A. A conceptual framework for action on the social determinants of health. Social Determinants of Health Discussion Paper 2 (Policy and Practice). www.who.int/sdhconference/resources/ConceptualframeworkforactiononSDH_eng.pdf Accessed January31, 2020
- 2. Adler NE, Stewart J. Health disparities across the lifespan: meaning, methods, and mechanisms. Ann N Y Acad Sci 2010;1186:5–23 [DOI] [PubMed] [Google Scholar]
- 3. Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959–2017. JAMA 26 2019;322:1996–2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Alderwick H, Gottlieb LM. Meanings and misunderstandings: a social determinants of health lexicon for health care systems. Milbank Q 2019;97:407–419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Daniel H, Bornstein SS, Kane GC. Addressing social determinants to improve patient care and promote health equity: an american college of physicians position paper. Ann Intern Med 17 2018;168:577–578 [DOI] [PubMed] [Google Scholar]
- 6. Council on Community Pediatrics. Poverty and Child Health in the United States. Pediatrics 2016;137:e20160339. [DOI] [PubMed] [Google Scholar]
- 7. National Academy of Medicine. Capturing social and behavioral domains in electronic health records: phase 1. Washington, DC: National Academy of Sciences, 2014 [PubMed] [Google Scholar]
- 8. Adler NE, Stead WW. Patients in context—EHR capture of social and behavioral determinants of health. N Engl J Med 19 2015;372:698–701 [DOI] [PubMed] [Google Scholar]
- 9. Alderwick HAJ, Gottlieb LM, Fichtenberg CM, Adler NE. Social prescribing in the U.S. and England: emerging interventions to address patients' social needs. Am J Prev Med 2018;54:715–718 [DOI] [PubMed] [Google Scholar]
- 10. Berkowitz SA, Hulberg AC, Standish S, Reznor G, Atlas SJ. Addressing unmet basic resource needs as part of chronic cardiometabolic disease management. JAMA Intern Med 2017;177:244–252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gottlieb LM, Hessler D, Long D, et al. Effects of social needs screening and in-person service navigation on child health: a randomized clinical trial. JAMA Pediatr 2016:e162521. [DOI] [PubMed] [Google Scholar]
- 12. Center for Medicare & Medicaid Services. Accountable Health Communities Model. 2018; https://innovation.cms.gov/initiatives/ahcm/ Accessed March30, 2020
- 13. Gold R, Gottlieb L. National data on social risk screening underscore the need for implementation research. JAMA Netw Open 2019;2:e1911513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gold R, Bunce A, Cowburn S, et al. Adoption of social determinants of health EHR tools by community health centers. Ann Fam Med 2018;16:399–407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Cottrell EK, Dambrun K, Cowburn S, et al. Variation in electronic health record documentation of social determinants of health across a national network of community health centers. Am J Prev Med 2019;57:S65–S73 [DOI] [PubMed] [Google Scholar]
- 16. Fraze TK, Brewster AL, Lewis VA, Beidler LB, Murray GF, Colla CH. Prevalence of screening for food insecurity, housing instability, utility needs, transportation needs, and interpersonal violence by US physician practices and hospitals. JAMA Netw Open 2019;2:e1911514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. DeVoe JE, Bazemore AW, Cottrell EK, et al. Perspectives in primary care: a conceptual framework and path for integrating social determinants of health into primary care practice. Ann Fam Med 2016;14:104–108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Byhoff E, Freund KM, Garg A. Accelerating the implementation of social determinants of health interventions in internal medicine. J Gen Intern Med 2018;33:223–225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Gottlieb L, Hessler D, Long D, Amaya A, Adler N. A randomized trial on screening for social determinants of health: the iScreen study. Pediatrics 2014;134:e1611–1618 [DOI] [PubMed] [Google Scholar]
- 20. Hassan A, Scherer EA, Pikcilingis A, et al. Improving social determinants of health: effectiveness of a web-based intervention. Am J Prev Med 2015;49:822–831 [DOI] [PubMed] [Google Scholar]
- 21. Wu S, Ell K, Jin H, et al. Comparative effectiveness of a technology-facilitated depression care management model in safety-net primary care patients with type 2 diabetes: 6-month outcomes of a large clinical trial. J Med Internet Res 2018;20:e147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Matthew-Maich N, Harris L, Ploeg J, et al. Designing, implementing, and evaluating mobile health technologies for managing chronic conditions in older adults: a scoping review. JMIR Mhealth Uhealth 2016;4:e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Miller DP Jr., Denizard-Thompson N, Weaver KE, et al. Effect of a digital health intervention on receipt of colorectal cancer screening in vulnerable patients: a randomized controlled trial. Ann Intern Med 2018;168:550–557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Tung EL, Abramsohn EM, Boyd K, et al. Impact of a low-intensity resource referral intervention on patients' knowledge, beliefs, and use of community resources: results from the Community Rx trial. J Gen Intern Med 2019. DOI: 10.1007/s11606-019-05530-5. PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lyles CR, Altschuler A, Chawla N, et al. User-centered design of a tablet waiting room tool for complex patients to prioritize discussion topics for primary care visits. JMIR Mhealth Uhealth 2016;4:e108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Patel V, Hale TM, Palakodeti S, Kvedar JC, Jethwani K. Prescription tablets in the digital age: a cross-sectional study exploring patient and physician attitudes toward the use of tablets for clinic-based personalized health care information exchange. JMIR Res Protoc 2015;4:e116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Cullen D, Woodford A, Fein J. Food for thought: a randomized trial of food insecurity screening in the emergency department. Acad Pediatr 2019;19:646–651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. RE-AIM. Improving Public Health Relevance and Population Health Impact. www.re-aim.org Accessed January30, 2020
- 29. Sauro J. Measuring usability with the system usability scale (SUS). https://measuringu.com/sus/ Accessed March29, 2020
- 30. Miller DP Jr., Weaver KE, Case LD, et al. Usability of a novel mobile health iPad app by vulnerable populations. JMIR Mhealth Uhealth 2017;5:e43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. O'Connor A, Cranney A. User manual—acceptibility [document on the Internet]. Ottawa: Ottawa Hospital Research Institute, © 1996 (modified 2002; cited 2019 01 30) http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Acceptability.pdf Accessed March29, 2020 [Google Scholar]
- 32. Huang YQ, Gou R, Diao YS, et al. Charlson comorbidity index helps predict the risk of mortality for patients with type 2 diabetic nephropathy. J Zhejiang Univ Sci B 2014;15:58–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Hess R, Santucci A, McTigue K, Fischer G, Kapoor W. Patient difficulty using tablet computers to screen in primary care. J Gen Intern Med 2008;23:476–480 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Brahmandam S, Holland WC, Mangipudi SA, et al. Willingness and ability of older adults in the emergency department to provide clinical information using a tablet computer. J Am Geriatr Soc 2016;64:2362–2367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Palakshappa D, Goodpasture M, Albertini L, Brown CL, Montez K, Skelton JA. Written versus verbal food insecurity screening in one primary care clinic. Acad Pediatr 2019. DOI: 10.1016/j.acap.2019.10.011 PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. De Marchis EH, Hessler D, Fichtenberg C, et al. Part I: a quantitative study of social risk screening acceptability in patients and caregivers. Am J Prev Med 2019;57(6S1):S25–S37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Byhoff E, De Marchis EH, Hessler D, et al. Part II: a qualitative study of social risk screening acceptability in patients and caregivers. Am J Prev Med 2019;57(6S1):S38–S46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Palakshappa D, Doupnik S, Vasan A, et al. Suburban families' experience with food insecurity screening in primary care practices. Pediatrics 2017;140;e20170320 [DOI] [PubMed] [Google Scholar]
- 39. Bottino CJ, Rhodes ET, Kreatsoulas C, Cox JE, Fleegler EW. Food insecurity screening in pediatric primary care: can offering referrals help identify families in need? Acad Pediatr 2017;17:497–503 [DOI] [PubMed] [Google Scholar]
- 40. Lindau ST, Makelarski JA, Abramsohn EM, et al. CommunityRx: A real-world controlled clinical trial of a scalable, low-intensity community resource referral intervention. Am J Public Health 2019;109:600–606 [DOI] [PMC free article] [PubMed] [Google Scholar]