Abstract
Introduction
The impact of the care for COVID-19 patients on nursing workload and planning nursing staff on the Intensive Care Unit has been huge. Nurses were confronted with a high workload and an increase in the number of patients per nurse they had to take care of.
Objective
The primary aim of this study is to describe differences in the planning of nursing staff on the Intensive Care in the COVID period versus a recent non-COVID period. The secondary aim was to describe differences in nursing workload in COVID-19 patients, pneumonia patients and other patients on the Intensive Care. We finally wanted to assess the cause of possible differences in Nursing Activities Scores between the different groups.
Methods
We analyzed data on nursing staff and nursing workload as measured by the Nursing Activities Score of 3,994 patients and 36,827 different shifts in 6 different hospitals in the Netherlands. We compared data from the COVID-19 period, March 1st 2020 till July 1st 2020, with data in a non-COVID period, March 1st 2019 till July 1st 2019. We analyzed the Nursing Activities Score per patient, the number of patients per nurse and the Nursing Activities Score per nurse in the different cohorts and time periods. Differences were tested by a Chi-square, non-parametric Wilcoxon or Student's t-test dependent on the distribution of the data.
Results
Our results showed both a significant higher number of patients per nurse (1.1 versus 1.0, p<0.001) and a significant higher Nursing Activities Score per Intensive Care nurse (76.5 versus 50.0, p<0.001) in the COVID-19 period compared to the non-COVID period. The Nursing Activities Score was significantly higher in COVID-19 patients compared to both the pneumonia patients (55.2 versus 50.0, p<0.001) and the non-COVID patients (55.2 versus 42.6, p<0.001), mainly due to more intense hygienic procedures, mobilization and positioning, support and care for relatives and respiratory care.
Conclusion
With this study we showed the impact of COVID-19 patients on the planning of nursing care on the Intensive Care. The COVID-19 patients caused a high nursing workload, both in number of patients per nurse and in Nursing Activities Score per nurse.
Key words: COVID-19, Intensive care, Nursing, Workload
What is already known
-
•
The COVID-19 pandemic had an impact on the planning of nursing staff on the Intensive Care Unit
-
•
The nursing workload of the COVID-19 patient as measured with the Nursing Activities is high compared to other Intensive Care patients.
What this paper adds
-
•
The higher nursing workload of COVID-19 patients is mainly due to more intense hygienic procedures, mobilization and positioning, support and care for relatives and respiratory care.
-
•
The higher nursing workload during the COVID-19 period was expressed in both a higher number of patients per nurse and a higher nursing workload per nurse.
-
•
The COVID-19 period showed that non-Intensive Care nurses can support the Intensive Care nurses in daily care, but the opportunities and restrictions of continuous deployment of these nurses in the Intensive Care needs further research
1. Introduction
It is generally recognized that the COVID-19 pandemic had a huge impact on nursing workload and the planning of the nursing staff on the Intensive Care Unit (ICU). Also in the Netherlands the COVID-pandemic hit hard. The ICU's were confronted with an increase in patients admitted, in an already existing situation of shortage of ICU nurses. The ICU bed capacity expanded from around 1100 beds in the normal situation to up to 1700 beds in April 2020 with the associated need for nursing staff (Dutch COVID-19, 2020). In the Netherlands the nursing workload on the ICU was also considered high by ICU nurses as indicated in a survey among 700 ICU nurses by the Dutch professional Association for ICU nurses (VandVN). Firstly, because they were confronted with an increase in numbers of patients per nurse. The high number of unplanned ICU admissions due to the COVID-pandemic caused an extreme pressure on the bed capacity on the ICU and therefore on the nursing staff (Dutch COVID-19, 2020). The ICU management was forced to alter normal nursing staff planning, and to bypass the Dutch Guidelines for Intensive Care which states that an ICU nurse in the Netherlands takes care for one or two patients per shift (NVIC 2017). During the peak of the COVID-19 crisis ICU nurses frequently had to take care for more than two patients per nurse. A study from Arabi et al. described different methods to expand the ICU staffing pool during the COVID-pandemic, e.g. optimizing ICU-nursing capacity by increasing the number of patients per nurse and the use of non-ICU staff to reinforce the ICU staff (Arabi et al., 2021). Also in the Netherlands the ICU nurses were supported by non-ICU nurses for basic care, but the ICU nurses were still responsible for the wellbeing of a higher number of patients during their shift. This is relevant as earlier research showed that the number of patients per nurse on an ICU is related to the patient outcome (West et al., 2014; Neuraz et al., 2015).
Secondly, in addition to an increased number of patients, the ICU nurses were also confronted with a new patient category with a complex care demand. The nursing workload of patients with COVID-19 pneumonia was perceived high compared to the average patient admitted to the ICU. Recent research showed that in Italy and Belgium the nursing workload as expressed with the Nursing Activities Score was higher in patients with COVID-19 compared to other ICU patients (Lucchini et al., 2020; Bruyneel et al., 2021). Moreover, due to the pressure on ICU beds there was no capacity left for planned surgical patients with a need for postoperative care on the ICU (Dutch COVID-19, 2020). This resulted in a decrease of planned admissions of less complex postoperative ICU patients; the available beds were mainly used for emergency medicine and surgery admissions. The combination of the potentially high nursing workload of both the COVID-19 patients and the other ICU patients could result in a higher workload per patient, and consequently a higher workload per nurse. Especially because the nurses had to take care of more than the normal number of patients. Recent research of Margadant et al. (2020) stated the importance of the nursing workload per ICU nurse; a higher Nursing Activities Score per nurse ratio was associated with a higher in-hospital mortality (Margadant et al., 2020). Therefore, it is important to look both at the number of patients per nurse and the nursing workload per nurse.
The primary aim of this study was to describe differences in the planning of nursing staff, expressed as the patient per nurse ratio on the ICU, and the impact of those differences on nursing workload in the COVID-period versus a recent non-COVID-period. The secondary aim of this study was to describe differences in ICU nursing workload according to the Nursing Activities Score of COVID-19 ICU patients and other ICU patients. We compared the workload of COVID-19 ICU patients with the workload of pneumonia patients from a recent non-COVID period. We also compared the workload of non-COVID patients during the COVID-period versus non-pneumonia patients in a recent non-COVID period. Lastly, we compared the workload of COVID-19 ICU patients with other ICU patients during the COVID-period. We finally wanted to assess the cause of possible differences in Nursing Activities Score between the different groups.
2. Methods
2.1. Setting
We used data from the Dutch National Intensive Care Evaluation quality registry. Since 2016 all 80 Dutch ICUs participate in this registry (Van De Klundert et al., 2015). The Dutch National Intensive Care Evaluation quality registry contains a minimal dataset with demographic, physiological and diagnostic patient data, and in-hospital mortality of all admitted ICU patients in all Dutch hospitals. One of the optional modules in the quality registry is the nursing capacity module with data about nursing workload and the number of fulltime-equivalent nurses per shift. This capacity module is available since 2017. Among the 80 Dutch ICU's participating in the quality registry, eleven Dutch ICU's of eleven distinct hospitals participate in the nursing capacity module since the start in 2017. From the eleven participating ICU's in the capacity module, we included the data of six ICU's as we had to exclude five ICU's due to missing Nursing Activities Score; the nurses in those five ICU's were not able to collect the Nursing Activities Score during the COVID-19 period due to the high workload.
2.2. Participants and period definition
All patients with a date of admission between March 2020 and July 1st 2020 to the six ICU's participating in the nursing capacity module were included for the COVID-19 period. All patients with a date of admission between March 1st 2019 and July 1st 2019 on those ICU's were included for the non-COVID period.
2.3. Variables
We defined four ICU patient cohorts: (Dutch COVID-19, 2020) patients admitted with a confirmed COVID-19 infection [positive polymerase chain reaction (PCR) test and/or confirmed COVID-19 on CT-Thorax i.e. a COVID-19 Reporting and Data System score (CO-RADS) of ≥4 in combination with the lack of an alternative diagnosis (Prokop et al., 2020)] during the COVID-period, (2) patients admitted with a pneumonia [aspiration, bacterial, fungal, parasitic of viral pneumonia or pulmonary sepsis] during the non-COVID period; (3) all non-COVID patients admitted to the ICU during the COVID period; and (4) all non-pneumonia patients admitted to the ICU during the non-COVID period.
We used the Nursing Activities Score to measure the nursing workload on the ICU (Miranda et al., 2003). The Nursing Activities Score represents a total of 23 nursing activities in direct and indirect ICU patient care (e.g., hygiene procedures, mobilization and positioning, care of artificial airways, administration tasks) with a score representing the average time consumption per activity (supplement Table 1 ). A total score of 100 points has been defined equal to the time spent by one fulltime-equivalent nurse per shift. Validation with time measurements has shown that Nursing Activities Score explains 59–81% of the actual nursing time (Miranda et al., 2003; Margadant et al., 2021). The interrater reliability of the Nursing Activities Score showed variable results from low to good values (Kappa 0.02 – 0.69). The results are low for the items with categories of an estimated time by nurses (e.g. present at bedsite and observation for two hours or more) (Stuedahl et al., 2015). This subjective estimation can lead to differences in Nursing Activities Score -scores and subsequently to differences in the calculated need for nursing staff (Ducci and Padilha, 2008; Carmona-Monge et al., 2013). Despite this consideration the Nursing Activities Score is widely used in different countries all over the world as a tool for planning nursing staff in daily practice (Padilha et al., 2008; Hoogendoorn et al., 2019). The use of Nursing Activities Score on the Intensive Care is described in e.g. Belgium, Italy, the Netherlands, Norway, Spain, Portugal, Poland, Egypt, Greece and Brazil (Padilha et al., 2015; Bruyneel et al., 2019; Lucchini et al., 2014; Morais de et al., 2016).
Table 1.
Baseline characteristics.
| Patient factors: | COVID -patients versus pneumonia patients |
Significance | Non-COVID patients versus non-pneumonia patients |
Significance | ||
|---|---|---|---|---|---|---|
| Patient type | COVID-19 -patients | Pneumonia-patients | p-value | Non-COVID- patients | Non-pneumonia -patients | p-value |
| Number of patients – N (%) | 218 (13.8%) | 147 (6.1%) | 1367 (86.2%) | 2262 (93.9%) | ||
| ICU admission type: | ||||||
| Medical patients – N (%) | 217 (99.5) | 147 (100) | 1 | 447 (32.8)* | 828 (36.6)* | 0.019 |
| Elective surgical patients – N (%) | 1 (0.5) | 0 (0) | 1 | 678 (49.6)* | 1188 (52.5)* | 0.100 |
| Urgent surgery patients – N (%) | 0 (0) | 0 (0) | – | 239 (17.5)* | 245 (10.8)* | <0.001 |
| Comorbidities: | ||||||
| Diabetes Mellitus – N (%) | 53 (24.3) | 28 (19.0) | 0.263 | 251 (18.4) | 411 (18.2)* | 0.890 |
| Renal insufficiency – N (%) | 7 (3.2) | 16 (10.9) | 0.002 | 57 (4.2) | 147 (6.5)* | 0.005 |
| Cardiovascular insufficiency – N (%) | 6 (2.8) | 7 (4.8) | 0.404 | 76 (5.6) | 97 (4.3) | 0.098 |
| Respiratory insufficiency – N (%) | 26 (11.9) | 55 (37.4) | <0.001 | 145 (10.6)* | 277 (12.2)* | 0.151 |
| Apache-APS score – Median (IQR) | 50 (42 - 64)* | 54 (44 – 68) | 0.079 | 37 (27 - 51) | 38 (27 - 55)* | 0.079 |
| Age – Median (IQR) | 66 (58 - 74) | 68 (59 - 76) | 0.219 | 67 (58 - 73) | 66 (56 – 73) | 0.105 |
| BMI – Median (IQR) | 27.7 (25.2 - 30.2) | 25.7 (23.0 – 29.8) | 0.001 | 26.0 (23.2 - 29.4) | 26.2 (23.5 – 29.6) | 0.262 |
| Mechanical ventilation in first 24 h-N (%) | 181 (83.0) | 82 (55.8) | <0.001 | 779 (57.0) | 1373 (60.7) | 0.026 |
| Mortality | ||||||
| ICU-mortality - N (% | 63 (28.9)* | 28 (19.0) | 0.031 | 83 (6.1) | 160 (7.1)* | 0.240 |
| In hospital mortality – N (%) | 85 (39.0)* | 39 (26.5) | 0.017 | 133 (9.7) | 201 (8.9)* | 0.405 |
| Length of ICU stay in days – Median (IQR) | 14.0 (8.0 – 27.0) | 3.9 (1.5 – 6.8) | <0.001 | 0.9 (0.8 - 1.8) | 0.9 (0.8 – 2.0)* | 0.457 |
| Nursing Activities Scores – Median (IQR) | 55.2 (44.9 – 64.8) | 50 (40.4 – 55.6) | <0.001 | 42.6 (38.5 – 46.9) | 42.9 (29.5 – 51.0) | 0.037 |
Statistically significant difference compared to baseline characteristics of other hospitals in the NICE database.
The nursing workload data in the capacity module of the Dutch National Intensive Care Evaluation quality registry consists of all nursing activities within the Nursing Activities Score with the data definitions according the updated guidelines published in 201,519 and the sum-score per patient. The Nursing Activities Score is collected in the Electronic Health Record by the ICU nurse, at the end of each shift. Nurses of the hospitals using the capacity module are trained in the use of Nursing Activities Score and the data definitions.
The nursing staff data in the capacity module of the Dutch National Intensive Care Evaluation quality registry consists of both the number of certified ICU nurses and trainee-ICU nurses actual present per shift and the number of operational beds per shift. The actual nursing staff data are retrospectively collected by the ICU management or secretary. This staff is also trained in the use of the capacity module and the data definitions. Data quality is assessed with a feedback system in the software on missing and extreme or abnormal data, both in the hospital Electronic Health System and within the database of the Dutch National Intensive Care Evaluation quality registry.
2.4. Statistical analysis
Depending on the variable distribution we used mean and standard deviation (SD) to describe normally distributed continuous variables and median and interquartile range (IQR) for non-normally distributed variables. Categorical variables were described by numbers and percentages. Differences between the cohorts were tested with a Chi-square test for categorical variables, a non-parametric Wilcoxon for non-normally distributed continuous variables and Student's t-test in case of normally distributed variables. Differences were considered statistically significant when they had a p-value of < 0.05. All statistical analyses were performed using R version 3.3.3.
3. Results
3.1. Baseline characteristics
We included data of 36,754 shifts (day, evening, night) of 3994 ICU patients: 218 patients with COVID-19 and 1367 non-COVID ICU patients in the COVID-19 period; 147 patients with pneumonia and 2262 non-pneumonia ICU patients in the non-COVID period. Table 1 shows the baseline characteristics of the four patient cohorts. Comparing the COVID-19 patients with the pneumonia patients, the COVID-19 patients showed a significant lower number of patients with chronic respiratory insufficiency (11.9% versus 37.4%, p<0.001), a higher Body Mass Index (Median Body Mass Index 27.7 versus 25.7, p = 0.001), higher number of patients requiring mechanical ventilation in the first 24 h on the ICU (83.0% versus 55.8%, p < 0.001), longer length of stay on the ICU (median LOS 14 days versus 3.9 days, p<0.001), a higher ICU mortality (28.9% versus 19,0%, p = 0.048) and in-hospital mortality (39.0% versus 26.5%, p = 0.017). The group of non-COVID patients during the COVID period showed a significant higher number of urgent surgery patients (17.5% versus 10.8%, p<0.001) compared to the non-pneumonia patients and a higher number of patients requiring mechanical ventilation in the first 24 h on the ICU (57% versus 60.7%, p = 0.03).
We also compared the baseline characteristics of the included patients from the six hospitals in our study with the patients of all other hospitals in the database of the Dutch National Intensive Care Evaluation registry (supplement Table 2 ). We found a difference in the distribution of patients between the groups. We found a significant lower number of medical patients (32.8% versus 51.8%, p<0.001), a higher number of elective surgery patients (49.6% versus 35.0%, p<0.001) and emergency surgical patients (17.5% versus 12.6%, p<0.001) in our study group compared to the patients in all hospitals. Also the Apache Acute Physiology Score (APS)-score and both the ICU and in-hospital mortality were higher in COVID-19 patients in our study group compared to COVID-19 patients in all other hospitals in the registry.
Table 2.
Comparing NAS-interventions per patient category.
| COVID-19 vs pneumonia patients |
Non-COVID vs. non-pneumonia ICU patients |
|||||
|---|---|---|---|---|---|---|
| COVID-19 ICU-patients | pneumonia patients | Significance | non-COVID ICU-patients | non-pneumonia ICU-patients | Significance | |
| Number of patients - N (%): | 221 (13.9) | 147 (6.1) | 1364 (86.1) | 2262 (93.9) | N/A | |
| Number of shifts N (%) | 7628 (44.0) | 2442(12.6) | 9694 (66.0) | 16,990 (87.4) | N/A | |
| NAS-intervention: | N (%) | N (%) | p-value | N (%) | N (%) | p-value |
| 1. Monitoring and titration 1.a. Hourly vital signs | 1793 (23.5) | 747 (30.6) | <0.001 | 4796 (49.5) | 5031 (29.6) | <0.001 |
| 1b. Present at bedside or active ≥2 h | 4455(58.4) | 780 (31.9) | <0.001 | 4261 (44.0) | 4855 (28.6) | <0.001 |
| 1c. Present at bedside and active ≥ 4 h | 1331 (17.4) | 355 (14.5) | <0.001 | 546 (5.6) | 2041 (12) | <0.001 |
| 2. Laboratory, | 5761 (75.5) | 1493 (61.1) | <0.001 | 5614 (57.9) | 8813 (51.9) | <0.001 |
| 3. Medication | 5551 (72.8) | 1638 (67.1) | <0.001 | 5776 (59.6) | 9241 (54.4) | <0.001 |
| 4. Hygienic procedures | ||||||
| 4. a. Performing hygiene procedures | 3729 (48.9) | 1611 (66.0) | <0.001 | 7677 (79.2) | 9468 (55.7) | <0.001 |
| 4. b. Performing hygiene procedures > 2 h/shift | 2406 (31.5) | 218 (8.9) | <0.001 | 1465 (15.1) | 1758 (10.3) | <0.001 |
| 4. c. Performing hygiene procedures > 4 h/shift | 1424 (18.7) | 12 (0.5) | <0.001 | 197 (2.0) | 239 (1.4) | <0.001 |
| 5. Care of drains | 50 (0.7) | 740 (30.3) | <0.001 | 3562 (36.7) | 6264 (36.9) | 0.836 |
| 6. Mobilization and positioning 6.a. Performing procedures once/shift | 3327(43.6) | 533 (21.8) | <0.001 | 6097 (62.9) | 3219 (18.9) | <0.001 |
| 6.b. Performing procedures > once/shift or with two nurses | 986 (12,9) | 814 (33.3) | <0.001 | 1214 (12.5) | 4494 (26.5) | <0.001 |
| 6.c. Performing mobilization procedures with three or more nurses | 1284 (16.8) | 87 (3.6) | <0.001 | 173 (1.8) | 253 (1.5) | 0.065 |
| 7. Support and care of relatives and patient 7.a. Support and care of relatives or patient for about 1 hour/shift | 4624 (60.6) | 1138 (46.6) | <0.001 | 6566 (67.7) | 6702 (39.4) | <0.001 |
| 7.b. Support and care of relatives or patient or about 3 h /shift | 810 (10.6) | 104 (4.3) | <0.001 | 423 (4.4) | 830 (4.9) | 0.053 |
| 8. Administrative and managerial tasks | ||||||
| 8.a. Performing routine tasks | 6065 (79.5) | 1802 (73.8) | <0.001 | 7676 (79.2) | 11,064 (65.1) | <0.001 |
| 8.b. Performing tasks for about 2 h/shift | 1126 (14.8) | 50 (2) | <0.001 | 1792 (18.5) | 551 (3.2) | <0.001 |
| 8.c. Performing tasks for about 4 h /shift | 301 (3.9) | 4 (0.2) | <0.001 | 26 (0.3) | 35 (0.2) | 0.349 |
| 9. Respiratory support | 7270 (95.3) | 1758 (72) | <0.001 | 7617 (78.6) | 9765 (57.5) | <0.001 |
| 10. Care of artificial airways | 6593 (86.4) | 1062 (43.5) | <0.001 | 4036 (41.6) | 5192 (30.6) | <0.001 |
| 11. Treatment for improving lung function | 4470(58.6) | 913 (37.4) | <0.001 | 2242 (23.1) | 3801 (22.4) | 0.149 |
| 12. Vasoactive medication | 2624 (34.4) | 524 (21.5) | <0.001 | 2885 (29.8) | 4350 (25.6) | <0.001 |
| 13. Intravenous replacement of large fluid loss | 42 (0.6) | 116 (4.8) | <0.001 | 327 (3.4) | 1127 (6.6) | <0.001 |
| 14. Left atrium monitoring | 0 (0) | 0 (0) | – | 247 (2.6) | 0 (0) | <0.001 |
| 15. Cardiopulmonary resuscitation after arrest | 6 (0.1) | 1 (0) | 0.708 | 6 (0.1) | 25 (0.1) | 0.057 |
| 16. Hemofiltration and dialysis techniques | 732 (9.6) | 72 (2.9) | <0.001 | 463 (4.8) | 874 (5.1) | 0.191 |
| 17. Quantitative urine output measurements | 7229 (94.8) | 1764 (72.2) | <0.001 | 8414 (86.8) | 11,049 (65.0) | <0.001 |
| 18. Measurements of intracranial pressure | 0 (0) | 0 (0) | – | 7 (0.1) | 12 (0.1) | 1 |
| 19. Treatment of complicated metabolic acidosis/alkalosis | 0 (0) | 0 (0) | – | 0 (0) | 0 (0) | – |
| 20. Intravenous hyperalimentation | 122 (1.6) | 15 (0.6) | 0.001 | 594 (6.1) | 609 (3.6) | <0.001 |
| 21. Enteral feeding | 6893 (90.4) | 1346 (55.1) | <0.001 | 3186 (32.9) | 5882 (34.6) | 0.002 |
| 22. Specific interventions in the ICU | 309 (4.1) | 721 (29.5) | <0.001 | 484 (5.0) | 4029 (23.7) | <0.001 |
| 23. Specific interventions outside the ICU | 220 (2.9) | 38 (1.6) | <0.001 | 859 (8.9) | 431 (2.5) | <0.001 |
3.2. Results workload per nurse
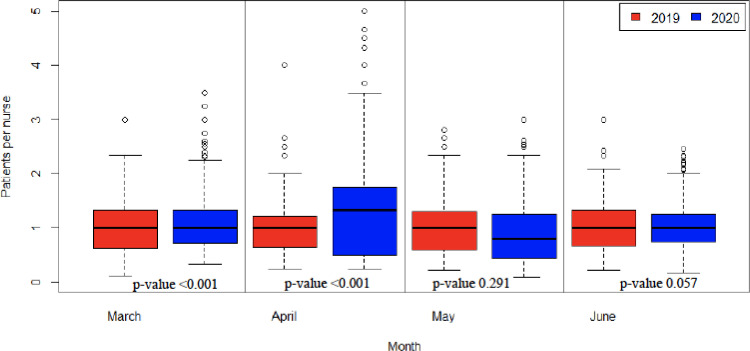
We found a significant higher number of patients per nurse in the COVID-period compared to the non-COVID period (Median (IQR) 1.1 (0.8 – 1.5) versus 1.0 (0.7 – 1.3), p<0.001). Fig. 1 shows the differences in number of patients per ICU nurse per month of the COVID and the non-COVID periods. The number of patients per ICU nurse was significant higher in the months April and May in the COVID-period compared to the non-COVID-period, with an increase of 30% in April 2020 compared to 2019 (Median (IQR) 1.3 (0.9 – 1.8) versus 1.0 (0.6 – 1.2), p<0.001) (Table 3 ). In April 2020 some ICU nurses took care for up to 5 patients per shift. This is more than double the maximum of two patients per nurse as stated by the Dutch Guidelines for Intensive Care.
Fig. 1.
Differences in numbers of patients per ICU-nurse; comparing months in 2019 to same months in 2020.
Table 3.
Patients per nurse and NAS per nurse per month.
| Patients per nurse– Median (IQR) |
NAS per nurse - Median (IQR) |
|||||
|---|---|---|---|---|---|---|
| 2020 | 2019 | p-value | 2020 | 2019 | p-value | |
| March | 1.1 (0.9 – 1.4) | 1.0 (0.6 – 1.3) | <0.001 | 70.1 (55.7 – 91.3) | 45.6 (27.0 – 72.1) | <0.001 |
| April | 1.3 (0.9 – 1.8) | 1.0 (0.6 – 1.2) | <0.001 | 89.6 (63.8 – 117.2) | 45.2 (27.5 – 68.7) | <0.001 |
| May | 0.9 (0.7 – 1.2 | 1.0 (0.6 – 1.3) | 0.291 | 64.9 (46.4 – 79.1) | 45.9 (24.5 – 70.8) | <0.001 |
| June | 1.3 (0.9 – 1.3) | 1.0 (0.6 – 1.2) | 0.057 | 56.6 (37.7 – 74.3) | 48.8 (26.7 – 71.5) | 0.002 |
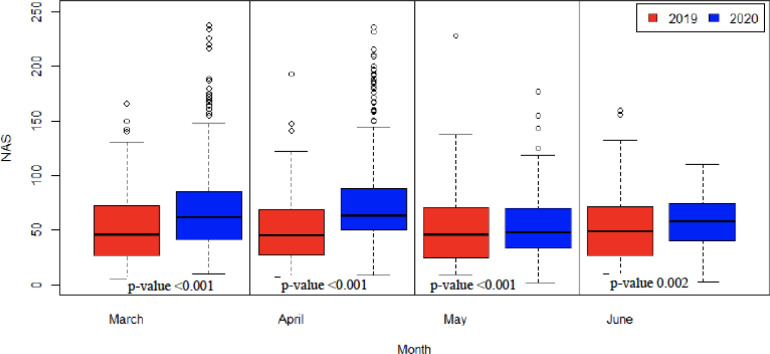
We further found a higher Nursing Activities Score per ICU nurse in the COVID-period compared to the non-COVID-period (Median (IQR) 69.8 (50.1 – 90) versus 46.6 (26.4 – 70.7), p<0.001). Fig. 2 shows the differences in Nursing Activities Score per ICU nurse per month of the COVID and the non-COVID periods. The mean Nursing Activities Score per ICU nurse was significant higher in each month of the COVID-period compared to the non-COVID-period with a peak of 98% increase in April 2020 compared to 2019 (Median (IQR) 89.6 (63.8 – 117.2) versus 45.2 (27.5 – 68.7), p<0.001) (Table 3).
Fig. 2.
Differences in NAS per ICU-nurse comparing months in 2019 to same months in 2020.
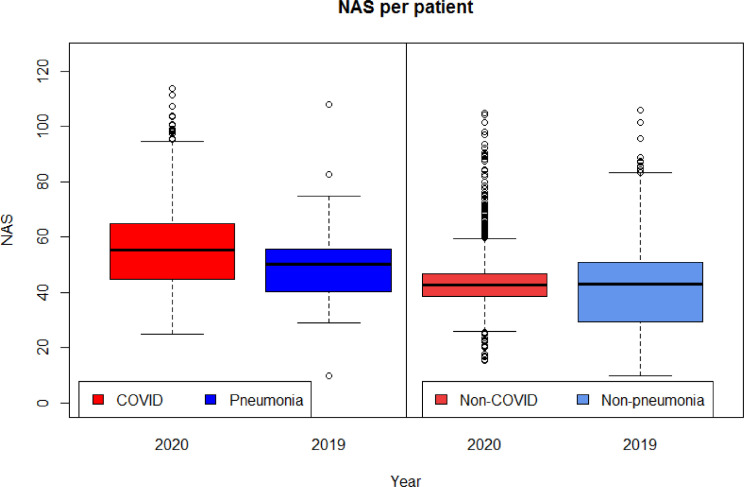
3.3. Results differences in nursing workload per patient category
Fig. 3 shows the mean Nursing Activities Score per patient for the COVID-19 patients compared with the pneumonia patients and the non-COVID-19 patients compared to the non-pneumonia patients. We found a significant higher Nursing Activities Score in COVID-19 patients compared to the pneumonia patients (Median (IQR) 55.2 (44.9 – 64.8) vs 50 (40.4 – 55.6), p<0.001). The Nursing Activities Score of both groups of other ICU patients (non-COVID-19 patients during the pandemic and non-pneumonia patients in a recent non-COVID-period) was not significantly different (Median (IQR): 42.6 (38.5 – 46.9) vs 42.9 (29.5 – 51.0), p 0.037). We also compared the Nursing Activities Score per patient of the COVID-19 patients to the other ICU patients in the COVID period. We found a significant higher Nursing Activities Score in COVID-19 patients (Median (IQR) 55.2 (44.9 – 64.8) vs 42.6 (38.5 – 46.9), p<0.001).
Fig. 3.
Differences in NAS per patient of COVID-19 versus pneumonia patients and non-COVID versus non-pneumonia patients.
Comparing the type of nursing interventions of the COVID-19 patients with the pneumonia patients, we found a significant difference in all the nursing interventions except for one intervention; care for the patients with a cardiopulmonary resuscitation after arrest in the past 24 h (Table 2). Remarkable differences were visible in performing hygienic procedures, mobilization and positioning, support and care for relatives, respiratory care and specific intervention in and outside the ICU. In 18.7% of the COVID-19 patients the nurse needed > 4 h for hygienic procedures (item 4c) where this was scored in 0.5% of the pneumonia patients admitted during the non-COVID period (p<0.001). Mobilization and positioning with 3 nurses or more (item 6c) was scored in 16.8% of the COVID-19 patients where this was scored in 3.6% of the pneumonia patients admitted during the non-COVID period (p<0.001). Support and care for relatives was scored more often in COVID-19 patients compared to pneumonia patients, both for item 7a - about 1 hour (67.8% versus 46.6%, p<0.001) as well as item 7b - >4 h (10.7% versus 4.3%, p<0.001). The nursing interventions for respiratory care were in all three items (item 9 - respiratory support, item 10 - care of artificial airways, i.e. tracheostoma or tube, and item 11 - treatment for improving lung function) higher for COVID-19 ICU patients compared to the pneumonia patients. We saw a decrease in the number of patients with a specific intervention on the ICU (item 22) in COVID-19 patients compared to pneumonia patients (4.1% versus 29.5%, p<0.001) and an increase in patients with a specific intervention outside the ICU (item 23) (2.9% versus 1.6%, p<0.001).
Comparing the nursing interventions of the non-COVID patients with the non-pneumonia patients we saw remarkable differences in performing hygienic procedures (item 4), mobilization and positioning (item 6), support and care for relatives (item 7), respiratory care (item 9, 10) and interventions outside the ICU (item 23). We saw an increase in the performance of hygienic procedures in category a - less than two hours (79,2% versus 55,7%, p<0.001) and in the category b - more than two hours (15.1% versus 10.3%, p<0.001). In the category mobilization and positioning (item 6) we saw a decrease in the category b - performing procedures >2 h per shift, any frequency (12.5% versus 26,5%, p<0.001) and an increase in the category a – performing procedures once per shift (62,9% versus 18.9%, p<0.001). The support and care for relatives for about one hour (item 7a) was higher for the non-COVID-19 ICU patients compared to the non-pneumonia ICU patients (67.7% versus 39.4%, p<0.001). The respiratory care was higher for the non-COVID ICU patients compared to the non-pneumonia patients with respect to the respiratory support (item 10) (78.5% versus 57.5%, p<0.001) and the care of artificial airways i.e. tracheostoma or tube (item 11) (41,7% versus 30.6%, p<0.001). We saw an increase of interventions outside the ICU (item 23) for the non-COVID ICU patients compared to the non-pneumonia patients (8,9% versus 2,5%, p<0.001).
4. Discussion
Our results showed that the increasing demand for nursing care during the COVID-period was recognizable in both a higher number of patients per nurse and a higher mean Nursing Activities Score per nurse, compared to the same months in 2019. Although the number of new admissions on the ICU was lower, the Nursing Activities Score per nurse and the number of patients per nurse were higher. The increase of the Nursing Activities Score per nurse was also disproportionate higher compared to the increase of the number of patients per nurse. This can be explained by the higher Nursing Activities Score per patient but also by the long length of stay of COVID-19 ICU patients. The continuous influx of COVID-19 patients in combination with a long length of stay and therefore a delayed outflow contributed to a high pressure on ICU beds. This pressure on the ICU beds resulted in cancelation of many planned post-operative patients, e.g. cardiac surgery patients. This is visible in the baseline characteristics; the total number of admissions in the COVID-period was lower compared to the non-COVID period, with also a lower number of planned surgical patients.
The percentage of unplanned surgical patients compared to the total ICU patientpopulation in the COVID-19 period was higher compared to the non-COVID period. Earlier research showed that the nursing workload of unplanned (medical and surgical) admissions is higher compared to planned (surgical) admissions (Hoogendoorn et al., 2021). During the COVID-19 period the percentage of patients with an unplanned admission, both medical and surgical, was increased. Comparing the baseline characteristics of the patients in our study with the baseline characteristics of all hospitals in the database of the Dutch National Intensive Care Evaluation, we must consider that there is a difference in the distribution of medical and elective or urgent surgical patients between the groups. However, the mean workload of the non-COVID patients during this period was not increased in our study, probably because the percentage of urgent admissions was still relatively low. Also the Apache Acute Physiology Score-score of the COVID-19 patients was higher in our study compared to the COVID-19 patients in all other hospitals. There is no unambiguous explanation for this difference. It is possible that the higher Apache Acute Physiology Score-score had an effect on the nursing workload, but the nursing workload is impacted by more aspects than the severity of illness (Altafin et al., 2014).
Although the number of patients per nurse and the Nursing Activities Score per nurse were both increased during the COVID-period, this should be interpreted with caution. To expand the nursing staff also in the Netherlands non-ICU nursing staff was deployed on the ICU during the COVID-19 period. The ICU nurses were supported in the daily care for the ICU patients by e.g., general nurses or anesthesia nurses. They supported in basic care, but also in special procedures such as turning the patient into prone position and back or daily hygienic procedures. It is important to mention that the number of non-ICU nurses has not been included in the data in the capacity registry of the Dutch National Intensive Care Evaluation and therefore not in our analysis because we did not have a data entry field for this kind of nurse. This should be considered when interpreting the results of the Nursing Activities Score per ICU nurse, especially in the month April 2020. The Nursing Activities Score was filled in by the ICU nurse but the time the non-ICU nurse spend at bedside is not mentioned in all the items of the Nursing Activities Score. If the non-ICU nurse support in the mobilization procedures it is incorporated in item 6b because the ICU nurse is performing the procedure with 2 nurses but the dressing procedures of the non-ICU nurse are not incorporated. This should also be considered interpreting the number of patients per nurse. During the COVID-period the nurse took care for even up to 5 patients per nurse, but the nurse might be supported by a non-ICU nurse. Despite this support, the ICU nurse held the overall responsibility for the care of the patients. The supervision of a general or anesthesia nurse was a new aspect for an ICU nurse. This could mean that the ICU nurses were taking care for three or even more critically ill patients and were supervising a general or anesthesia nurse in the process of daily care. Although the support for the ICU nurses enlightened their task, the new coordinating role added to their responsibilities and therefore to their workload.
Our second aim was to describe differences in nursing workload of COVID-19 patients versus pneumonia patients and differences in nursing workload of non-COVID and non-pneumonia patients admitted to the ICU. The results of our study clearly showed that COVID-19 patients cause a significantly higher ICU nursing workload compared to pneumonia patients in the non-COVID period. This confirms our expectation that the care for a COVID-19 patient requires more time from an ICU nurse than the care for a regular pneumonia patient. This higher workload was mainly due to nursing interventions like monitoring and titration with bedside observation, respiratory care, mobilization, hygienic procedures and taking care for the patient and his or her relatives. The increase in time for monitoring and titration with bedside observations is possibly related to the hygiene procedures. It is conceivable that the increase of the time that ICU nurses stayed at the bedside for observation, monitoring and titration was influenced by the time the nurses needed for complex dressing procedures for the use of personal protection equipment (Lucchini et al., 2020). The ICU nurses perceived those complex dressing procedures as an aggravating factor in the workload and avoided extra dressing procedures by staying at the bedside. This could also be responsible for the increase in time needed for hygienic procedures. It should be noted that a substantial part of the COVID-19 patients is categorized in category 4a, although isolation is part of the definition of 4b. This can be explained by the use of cohort-isolation for COVID-patients in several hospitals. After entering the cohort-unit with the personal protection equipment the nurse could take care for the patients with the standard hygienic procedures. Working a few hours on the cohort-unit without leaving the unit and without being able to take a break and wearing the personal protection equipment all the time however was still an aggravating factor in the nursing workload (Leng et al., 2021). Due to the special procedures in the COVID-period there was also an increase in the time needed for the standard hygienic procedures in non-COVID patients.
The workload of the respiratory care was higher, which is in line with the higher number of ventilated COVID-19 ICU patients. The increase of workload in the category ‘Performing mobilization procedures with three or more nurses with any frequency’ can be explained by the frequency of turning patients into prone- or supine position as this became standard in the treatment of COVID-19 ICU patients (Bruyneel et al., 2021; Azoulay, 2020; Coppo et al., 2020). We also found a difference in workload in the support and care of the patient and his or her relatives. This might have been influenced by both the high ICU-mortality in COVID-19 patients (28.9%) as well as by visiting limitations during the COVID-pandemic. As a result of those limitations nurses worked with video conferencing with the family (Negro et al., 2020). This video conferencing required a subsequent need for extra nursing time. This aspect can also explain the increase in needed time for support and care of the patient and his or her relatives for the non-COVID-patients because they were confronted with the same visiting limitations.
Comparing the workload of COVID-19 patients of this study with results of other studies we found a higher Nursing Activities Score for COVID-19 patients in the study in Belgium (mean 92.0). A possible explanation could be the length of the shift, which is 12 h instead of the 8-hours shift in our study. Also in Italy the Nursing Activities Score for COVID-19 patients was slightly higher than in our study (mean 84.0), which represented the nursing activities in 24 h (Lucchini et al., 2020). However, in both studies the increase of the Nursing Activities Score of COVID-19 patients compared to other ICU patients was 28 – 33%, which is comparable with the 30% increase we found in our study.
Due to the combination of a higher workload per patient, the increase of the proportion of those patients compared to the total ICU patient population due to the long ICU length of stay, there was an increasing demand for the need for nursing care per ICU patient. This can also explain changes in care for the non-COVID patients as e.g. the mobilization procedures; we saw a significant increase in category a – performing procedures once per shift with a decrease in category b - Performing procedures more frequently than once/shift or with two nurses, any frequency. The high demand of the care for COVID-patients may have put pressure on the available nursing time for the other non-COVID patients, visible in the decrease of frequency of mobilization procedures.
4.1. Strengths and limitations
A strength of this study is the large amount of Nursing Activities Score from patients in both the COVID-period and the non-COVID period. The number of participating hospitals was limited, but we included data of all shifts and patients in both periods. The included ICUs were representative of Dutch ICU's regarding hospital type (teaching and non-teaching hospitals) and geographical location. The included patients were representative compared to the patients of all the other ICU's in the Dutch National Intensive Care Evaluation registry, except for the Apache Acute Physiology Score-score and the higher mortality in COVID-patients. The mortality in our study group was however comparable with the mortality in another COVID-19 study about COVID in the Netherlands (Dutch COVID-19, 2020). Another strength is that we were able to analyze the raw which enabled insight in which aspects the Nursing Activities Score differed between the groups.
Within this research we did not analyze every aspect of the nursing workload. As COVID-19 is a new disease it is possible that the workload in the beginning of the pandemic period was higher due to the unfamiliarity with these kinds of patients. It is possible that this unfamiliarity and lack of knowledge about the clinical course of COVID-19 had an impact on interventions such as being bedside. Analysis of the workload in next COVID-19 waves can help us in this respect.
Another limitation is that we do not have data on non-ICU (general or anesthesia) nursing staff in our capacity module. The Nursing Activities Score was scored by the ICU nurse, but the support of a non-ICU nurse can influence (lower) the time needed for the nursing interventions. We do not know the exact impact of the support by other staff on the workload of the ICU nurses. But, however helpful the support of non-ICU nurses in daily care has been, this support also added a dimension of coordination and supervision to the role of the ICU nurse Unfortunately we were not able to analyze the impact of this change of the nursing role of the ICU nurse on the nursing workload. However, we have indicated from this period that participation of other nurses in the daily care on an ICU is possible. They can support the ICU nurse in e.g., mobilization of the patient, hygienic procedures or assistance in patient and family care. Further research should focus on opportunities and restrictions on the changing and coordinating role of the ICU nurse.
5. Conclusion
This study showed a higher nursing workload during the COVID-19 period, expressed in both a higher number of patients per nurse and a higher nursing workload per nurse. The higher workload per nurse can be explained by the higher workload of COVID-19 patients compared to pneumonia patients, an increase of the proportion of COVID-19 patients on the total patient population on the ICU and their long length of stay. This higher workload of COVID-19 was mainly due to nursing interventions as being bedside, respiratory care, mobilization and positioning e.g. turning into prone- or back position, hygienic procedures and taking care for the patient and his or her relatives. During the COVID-19 period non-ICU nurses supported the ICU nurses in basic care for ICU patients. However, the opportunities and restrictions of continuous deployment of other nurses in daily care to reduce the ICU nursing workload needs further research. This remains a relevant issue, also after the COVID-19 pandemic, given the shortages of ICU nurses. Further research is also needed to analyze the impact of the high workload on patient outcome.
Declaration of Competing Interest
The author M.E. Hoogendoorn and co-authors S. Brinkman, J.J. Spijkstra, R.J. Bosman, and N.F. de Keizer are members of the board of NICE. The funding by the NICE foundation does not alter the authors' adherence to the policies of Critical Care Nursing on sharing data and materials.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ijnurstu.2021.104005.
Appendix. Supplementary materials
References
- Altafin J.A.M., Grion C.M.C.G., Tanita M.T., Festti J., Cardoso L.T.Q., Veiga C.F.F., Kamiji D., Barbosa A.R.G., Matsubara C.T., Lara A.B., Lopes C.C.B., Blum D., Matsuo T. Nursing activities score and workload in the intensive care unit of a university hospital. Rev.Bras.Ter.Intensiva. 2014;26(3):292–298. doi: 10.5935/0103-507X.20140041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arabi Y.M., Azoulay E., Dorzi-Al H.M., Phua J., Salluh Binnie A, Hodgson C., Angus D.C., Cecconi M., Du B., Fowler R., Gomersall C.D., Horby P., Juffermans N.G., Kesecioglu J., Kleinpell R., Machado F.R., Martin G.S., Meygroidt G., Rhodes A., Rowan K., Timsit J.F., Vincent J.L., Citerio G. How the COVID-19 pandemic will change the future of critical care. Intensive Care Med. 2021;47:282–291. doi: 10.1007/s00134-021-06352-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azoulay E.K.N. A 5-point strategy for improved connection with relatives of critically ill patients with COVID-19. Lancet Respiratory Medicine. 2020;8(6):52. doi: 10.1016/S2213-2600(20)30223-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruyneel A., Gallani M.C., Tack J., d’Hondt A., Canipel S., Franck S., Reper P., Pirson M. Impact of COVID-19 on nursing time in intensive care units in belgium. Intensive Crit. Care Nurs. 2021 doi: 10.1016/j.iccn.2020.102967. Epub(Oct 28) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruyneel A., Tack J., Droguet M., Maes J., Wittebole X., Reis Miranda D., DiPierdomenico L. Measuring the nursing workload in intensive care with the nursing activities score (NAS): a prospective study in 16 hospitals in belgium. J Crit Care. 2019;54:205–211. doi: 10.1016/j.jcrc.2019.08.032. [DOI] [PubMed] [Google Scholar]
- Carmona-Monge F.J., Rollan Rodriguez G.M., Quiros Herranz C., Garcia Gomez S., Marin-Morales D. Evaluation of the nursing workload through the nine equivalents for nursing manpower use scale and the nursing activities score: a prospective correlation study. Intensive Crit. Care Nurs. 2013;29(4):228–233. doi: 10.1016/j.iccn.2013.03.003. [DOI] [PubMed] [Google Scholar]
- Coppo A., Bellani G., Winterton D., Di Pierro M., Soria A., Faverio P., Cairo M., Mori S., Messinesi G., Contro E., Bonfanti P., Benini A., Valsecchi M.G., Antolini L., Foti G. Feasibility and physiological effects of prone positioning in non-intubated patients with acute respiratory failure due to COVID-19 (PRON-COVID): a prospective cohort study. Lancet Respiratory Medicine. 2020;8(8):765–774. doi: 10.1016/S2213-2600(20)30268-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ducci A.J., Padilha K.G. Nursing activities score: a comparative study about retrospective and prospective applications in intensive care units. ACTA PAUL ENFERMAGEM. 2008;21(4):581–587. [Google Scholar]
- Dutch COVID-19 Research Consortium collaboration National Intensive Care Evaluation. One year of COVID-19 in the netherlands – a dutch narrative. Netherlands Journal of Critical Care. 2020;29(2) [Google Scholar]
- Hoogendoorn M., Brinkman S., Spijkstra J.J., Bosman R.J., Margadant C.C., Haringman J., De Keizer N. Association between objective nursing workload with nursing activity score and perceived nursing workload with NASA-TLX. Int J Nurs Stud. 2021 doi: 10.1016/j.ijnurstu.2020.103852. Feb:114. [DOI] [PubMed] [Google Scholar]
- Hoogendoorn M., Margadant C.C., Brinkman S., Spijkstra J.J .HJ., De Keizer N. Workload scoring systems in the intensive care and their ability to quantify the need for nursing time: a systematic literature review. Int J Nurs Stud. 2019 doi: 10.1016/j.ijnurstu.2019.103408. [DOI] [PubMed] [Google Scholar]
- Leng M., Wei L., Shi X., Cao G., Wei Y., Xu Hong, Zhang X., Zhang W., Xing S., Wei H. Mental distress and influencing factors in nurses caring for patients with COVID-19. Nurs. Crit. Care. 2021;26(2):94–101. doi: 10.1111/nicc.12528. 1. [DOI] [PubMed] [Google Scholar]
- Lucchini A., De Felippis C., Elli S., et al. Nursing activities score (NAS): 5 years of experience in the intensive care units of an italian university hospital. Intensive Crit. Care Nurs. 2014;30(3):152–158. doi: 10.1016/j.iccn.2013.10.004. [DOI] [PubMed] [Google Scholar]
- Lucchini A., Giani M., Elli S., Villa S., Rona R., Foti G. Nursing activities score is increased in COVID-19 patients. Intensive Crit. Care Nurs. 2020 doi: 10.1016/j.iccn.2020.102876. april(23) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Margadant C., Wortel S., Hoogendoorn M., et al. The nursing activities score per nurse ratio is associated with in-hospital mortality, whereas patients per nurse ratio is not. Crit. Care Med. 2020;48(1):3–9. doi: 10.1097/CCM.0000000000004005. [DOI] [PubMed] [Google Scholar]
- Margadant C.C .HM., Bosman R.J., Spijkstra J.J., Brinkman S., de Keizer N.F. Validation of the nursing activity score (NAS) using time-and-motion techniques in dutch intensive care units. Netherlands Journal of Critical Care. 2021;29(1) [Google Scholar]
- Miranda D., Nap R., de Rijk A., Schaufeli W., Iapichino G. TISS Working Group Therapeutic Intervention Scoring System. Nursing activities score. Crit. Care Med. 2003;31:374–382. doi: 10.1097/01.CCM.0000045567.78801.CC. [DOI] [PubMed] [Google Scholar]
- Morais de C.M., Faria Simães Mendes, Clara Maria, Silva Candeias A.L., Rodrigues Sousa M.P., Viecili Hoffmeister L., Gomes S.L. Validation of the nursing activities score in portuguese intensive care units. REV BRASIL ENFERMAGEM. 2016;69(5):826–832. doi: 10.1590/0034-7167-2016-0147. [DOI] [PubMed] [Google Scholar]
- Negro A., Mucci M., Beccaria P., Borghi G., Capocasa T., Cardinali M., Pasculli N., Ranzani R., Villa G., Zangrillo A. Introducing the video call to facilitate the communication between health care providers and families of patients in the intensive care unit during COVID-19 pandemia. Intensive Crit. Care Nurs. 2020:60. doi: 10.1016/j.iccn.2020.102893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neuraz A., Guérin C., Payet C., et al. Patient mortality is associated with staff resources and workload in the ICU: a multicenter observational study. Crit. Care Med. 2015;4398(1587):1594. doi: 10.1097/CCM.0000000000001015. [DOI] [PubMed] [Google Scholar]
- NVIC. Checklist zorgbeleidsplan IC-afdelingen in nederland. 2017.
- Padilha K.G., de Sousa R.M., Queijo A.F., Mendes A.M., Reis Miranda D. Nursing activities score in the intensive care unit: analysis of the related factors. Intensive Crit. Care Nurs. 2008;24(3):197–204. doi: 10.1016/j.iccn.2007.09.004. [DOI] [PubMed] [Google Scholar]
- Padilha K.G., Stafseth S., Solms D., Hoogendoom M., Monge F., Gomaa O.H., Giakoumidakis K., Giannakopoulou M., Gallani M.C., Cudak E., Nogueira Lde S., Santoro C., Sousa R.C., Barbosa R.L., Miranda Ddos R. Nursing activities score: an updated guideline for its application in the intensive care unit. REV ESC ENFERMAGEM USP. 2015;49(Spec No):131–137. doi: 10.1590/S0080-623420150000700019. [DOI] [PubMed] [Google Scholar]
- Prokop M., Everdingen W., Vellinga T., Ufford J., Stöger L., Beenen L., et al. CO-RADS – A categorical CT assessment scheme for patients with suspected COVID-19: definition and evaluation. Radiology. 2020;296(2) doi: 10.1148/radiol.2020201473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuedahl M., Vold S., Klepstadt P., Stafseth S.K. Interrater reliability of nursing activity score among intensive care unit health professionals. Rev.Esc.Enferm.USP. 2015;49(117):122. doi: 10.1590/S0080-623420150000700017. [DOI] [PubMed] [Google Scholar]
- V&VN. Grote mentale gevolgen voor ic verpleegkundigen na eerste coronapiek. https://www.venvn.nl/afdelingen/intensive-care/nieuws/grote-mentale-gevolgen-voor-ic-verpleegkundigen-na-eerste-coronapiek/. Updated 2020.
- Van De Klundert N., Holman R., Dongelmans D., De Keizer N. Data resource profile: the dutch national intensive care evaluation (NICE) registry of admissions to adult intensive care units. Int J Epidemiol. 2015;44(6):1850. doi: 10.1093/ije/dyv291. [DOI] [PubMed] [Google Scholar]
- West E., Barron D., Harrison D., Rafferty A., Rowan K., Sanderson C. Nurse staffing, medical staffing and mortality in intensive care: an observational study. Int J Nurs Stud. 2014;51(5):781–794. doi: 10.1016/j.ijnurstu.2014.02.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.