Abstract
The feed additive ractopamine, a β-adrenergic agonist, has been approved for use in livestock for nearly 2 decades. Studies of its possible adverse effects in humans have concentrated exclusively on cardiovascular disease and cardiovascular functional disorders in the past. In this article, whether and how ractopamine may affect neurodegeneration, either to promote or to reduce the incidence of Alzheimer disease, will be discussed based on the recent controversial findings that β-adrenoreceptor activation not only can stimulate Alzheimer-pathogenic amyloid-β accumulation but also are able to enhance hippocampal neurogenesis and ameliorate mouse memory deficits in independent laboratory studies. Furthermore, environmental enrichment has been found to prevent impairment of memory-related hippocampal long-term potentiation and microglia-mediated neuroinflammation induced by amyloid-β. These beneficial effects are achieved mainly through enhanced β-adrenergic signaling and can be imitated by β agonist isoprotenerol. Finally, it has been demonstrated that the β-adrenergic agonist salbutamol could bind directly to tau protein and interfere with the tau filament formation seen in the prodromal phase of Alzheimer disease. These complex but interesting issues lead to contradictory speculations of possible effects of ractopamine residue in meat on Alzheimer disease. Hypotheses derived from this review surely deserve carefully designed laboratory investigations and clinical studies in the future.
Keywords: Alzheimer disease, Ractopamine, Amyloid-β, Tau protein, Neurogenesis, Neuroinflammation
Introduction
Alzheimer disease, the main cause of dementia, is the most prevalent and rapidly growing neurodegenerative disorder around the world, with incidence rates rising exponentially with age and increasing notably after 65 years [1]. The diagnosis of probable and possible Alzheimer disease chiefly depends on clinical symptoms and modern image studies such as magnetic resonance imaging and positron emission tomography, while a definite diagnosis usually needs autopsy-confirmed characteristic pathologic findings of amyloid neuritic plaques and neurofibrillary tangles [2, 3]. There is currently no curative or disease-modifying treatment for Alzheimer disease, although a number of acetylcholinesterase inhibitors and N-methyl-D-aspartate receptor antagonists could provide symptomatic improvement of cognition impairment [4]. Nonetheless, these now approved therapies are not able to change the rate of cognitive decline in a long-run aspect [5]. Preventative strategies thus seem to be an urgently important issue. Regarding risk factors for Alzheimer disease, in addition to genetic, vascular, lifestyle, physical, and metabolic ones, such as hypertension, diabetes, hypercholesterolemia, and smoking [6], is there any other agent worthy of concern? Herein, ractopamine, a β-adrenoreceptor agonist widely used as a feed additive in beef and pork production in the USA but prohibited in European Union and China [7], is the focus of interest.
Mechanism of Alzheimer Disease and Novel Therapies
Though the exact causes of Alzheimer disease are not certain and very complex, hypothesized mechanisms have been developed indicating that the gradually accumulated extracellular neuritic plaques composed of amyloid-β peptide (Aβ) interact with the intracellular neurofibrillary tangles formed by the tau protein and elicit neuroinflammation which finally leads to neurodegeneration [8]. Aβ aggregation derives from alterations of different Aβ species production from amyloidogenic amyloid-β protein precursor (AβPP) and their clearance, whereas the main pathogenic modification of tau is posttranslational hyperphosphorylation. Based on the recent understanding of the pathogenic roles that Aβ and tau play in the very beginning stage of Alzheimer disease's natural course, therapeutic modalities aimed at inhibition of Aβ and tau formation have been eagerly designed and tested [9]. Nevertheless, these candidate drugs will require successful clinical trials to prove their benefits and this will take time [10]. The biggest concern is the timing of treatment. Even if novel agents could inhibit Aβ and tau formation at once, the effects on dementia brains already suffering from long-term neurodegeneration would be doubtful.
γ-Secretase and β-Adrenoreceptor
The amyloidogenic Aβ is generated from the transmembrane AβPP through successive cleavage by β- and γ-secretases while AβPP processed by α-secretase results in nonamyloidogenic products. Dyshomeostasis of Aβ leads to synaptotoxic soluble oligomers capable of phosphorylating tau and insoluble fibrils which aggregate into plaques [11]. The γ-secretase is a complex composed of 4 subunits, i.e., presenilin, nicastrin, anterior pharynx-defective 1, and presenilin enhancer 2 [12]. Mutations of AβPP and presenilin genes are found to be closely associated with familial Alzheimer disease, highlighting the key role of γ-secretase in the pathogenesis of Alzheimer disease [13]. Further disclosing of the underlying causes of Alzheimer disease, research on regulation of γ-secretase by environmental factors has revealed that activation of β-adrenoreceptor can enhance γ-secretase activity in cell culture, and treatment with β-adrenoreceptor agonist increased cerebral amyloid plaques in a mouse model, suggesting that abnormal β-adrenoreceptor activation by stress might contribute to Aβ accumulation in Alzheimer disease [14].
Hypothesis: Ractopamine and Amyloid-β
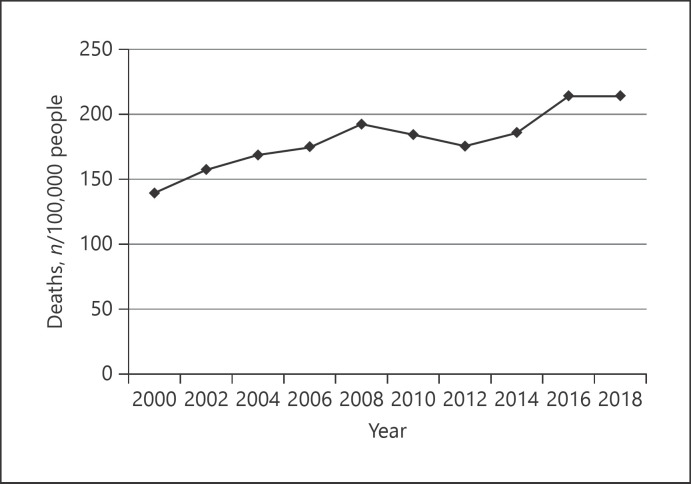
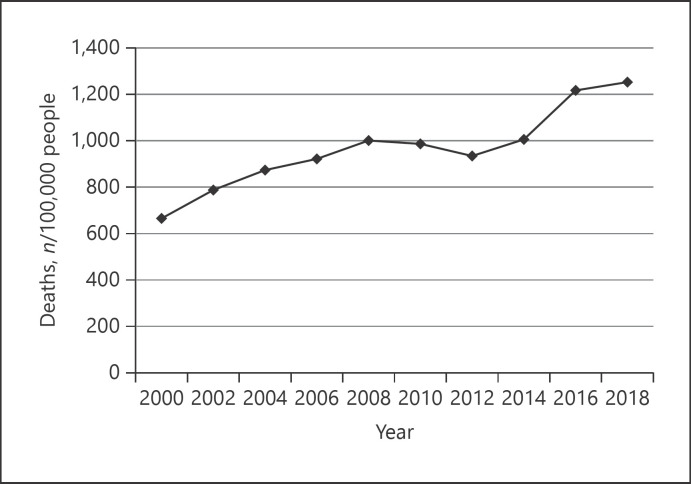
The global population is still growing, especially in Asia, creating a need for food production. It is therefore not strange to see livestock producers in the USA, Canada, Brazil, and Mexico using the β-adrenoreceptor agonist ractopamine to increase the growth rate and percentage of leanness of their finishing cattle and swine [15]. Although ractopamine has been approved for use under the no-observed-adverse-effect level for nearly 20 years, as a β-adrenoreceptor activator its chronic potential influence on Aβ accumulation and thus the incidence of Alzheimer disease deserve careful investigation. Figures 1 and 2 were created based on annual Alzheimer's death rates by age and year in the USA from 2000 to 2018 [16]. As we can see, in both age groups (i.e., 75–84 years and 85 years or older) there seems to be a progressive elevation trend across the time period. This trend is coincidentally compatible with the hypothesis that consumption of meat containing ractopamine might stimulate Aβ production and aggregation in the brain, silently resulting in Alzheimer disease.
Fig. 1.
Annual Alzheimer death rates (per 100,000 people) by year in the age group 75–84 years in the USA. Data are from the Alzheimer's Association [16].
Fig. 2.
Annual Alzheimer death rates (per 100,000 people) by year in the age group 85 years or older in the USA. Data are from the Alzheimer's Association [16].
Enhancement of Neurogenesis
Nonetheless, the role of β-adrenoreceptor in the pathogenesis of Alzheimer disease is still quite controversial. Contrary to what has been mentioned above, activation of the β2-adrenoreceptor by the β2-adrenergic agonist clenbuterol in transgenic mice carrying chimeric mouse/human AβPP and mutant human presenilin 1, an Alzheimer disease animal model, significantly stimulated hippocampal neurogenesis and reversed memory deficits [17]. Another selective β2-adrenergic agonist, i.e., salmeterol, when chronically administrated in mice, exerts a prosurvival effect of neuroblasts and beneficially modulates hippocampal neuroplasticity [18]. Accordingly, ractopamine residue in meat probably would improve symptoms of dementia in Alzheimer disease rather than worsen them. However, the net results of a speculated increased Aβ accumulation and presumed enhanced neurogenesis clearly require more intelligent laboratory work and long-term clinical observation in order for a definite conclusion to be reached.
Environmental Enrichment against Amyloid-β
Furthermore, impairment of memory-related hippocampal long-term potentiation by Aβ was found to be protected by an enriched environment for rodents through activation of the β2-adrenergic receptor and the cAMP/PKA signaling pathway [19, 20]. Environmental enrichment by adding novel objects and running wheels to mouse cages constitutes a behavior paradigm that models cognitive activity of humans. Researchers of these studies disclosed that the β1/2 agonist isoproterenol prevented the inhibition of Aβ on long-term potentiation while nonselective β antagonist decreased the beneficial effects of environmental enrichment. In addition to long-term potentiation, microglia-mediated neuroinflammation, a key factor in the progression of Alzheimer disease, could also be blocked by environmental enrichment through enhanced β-adrenergic signaling [21, 22]. All of these results lead to speculation that ractopamine, a β1/2 agonist, might play an ameliorating role in the development of Alzheimer disease.
Inhibition of Tau Aggregation
Besides Aβ, neurofibrillary tangle from tau filaments is considered to be another therapeutic target in Alzheimer's disease due to its pathogenic roles. A variety of modalities have been developed to inhibit tau expression, disturb tau aggregation, stabilize microtubules, and remove tau with immunotherapy, but their satisfactory efficacy and safety have yet to be proven clinically [23]. Interestingly, the β-adrenergic agonist salbutamol was recently found to be capable of inhibiting tau aggregation in an experiment adopting high-throughput synchrotron radiation circular dichroism and conventional circular dichroism spectroscopy. Surprisingly, the mechanism of tau inhibition by salbutamol is not through β-adrenoreceptor activation but rather an interfering effect by direct binding of salbutamol to prefilament tau [24]. It is thus hard to deduce whether ractopamine also has a molecular docking action similar to that of salbutamol because different molecules have different conformations and hydrogen bonding orientations.
Discussion and Conclusion
In the past, the safety concern of ractopamine as a feed additive has mainly focused on its risk of carcinogenesis, genotoxicity, and cardiovascular disorders, with almost no attention being paid to chronic neurologic influence [25]. It is hoped that this review will help to arouse interest in this aspect, especially the occurrence of Alzheimer disease. Although there is much controversy surrounding the real impact of ractopamine on neurodegeneration, thanks to the progress of nuclear medicine imaging techniques, early amyloid accumulation and neuroinflammation induced by Aβ or tau can now be detected by position emission tomography, facilitating the diagnosis of Alzheimer disease in its prodromal phase [26, 27]. In countries where people consume meat containing ractopamine, close follow-up and monitoring with such modern imaging devices is highly recommended in order to investigate and survey the possible influence of ractopamine on the central nervous system to see whether it is a friend or foe.
Conflict of Interest Statement
The author has no conflict of interests to report.
Funding Sources
This research received no external funding.
Author Contributions
F.S.F. alone conceptualized the idea, collected the literature, and wrote this review.
References
- 1.Mayeux R, Stern Y. Epidemiology of Alzheimer disease. Cold Spring Harb Perspect Med. 2012 Aug;2((8)):a006239. doi: 10.1101/cshperspect.a006239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Castellani RJ, Rolston RK, Smith MA. Alzheimer disease. Dis Mon. 2010 Sep;56((9)):484–546. doi: 10.1016/j.disamonth.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reitz C, Brayne C, Mayeux R. Epidemiology of Alzheimer disease. Nat Rev Neurol. 2011 Mar;7((3)):137–52. doi: 10.1038/nrneurol.2011.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Joe E, Ringman JM. Cognitive symptoms of Alzheimer's disease: clinical management and prevention. BMJ. 2019 Dec;367:l6217. doi: 10.1136/bmj.l6217. [DOI] [PubMed] [Google Scholar]
- 5.Weller J, Budson A. Current understanding of Alzheimer's disease diagnosis and treatment. F1000Res. 2018;7:F1000. doi: 10.12688/f1000research.14506.1. Faculty Rev-1161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patterson C, Feightner JW, Garcia A, Hsiung GY, MacKnight C, Sadovnick AD, Diagnosis and treatment of dementia: 1. Risk assessment and primary prevention of Alzheimer disease. CMAJ. 2008 Feb;178((5)):548–56. doi: 10.1503/cmaj.070796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Centner TJ, Alvey JC, Stelzleni AM. Beta agonists in livestock feed: status, health concerns, and international trade. J Anim Sci. 2014 Sep;92((9)):4234–40. doi: 10.2527/jas.2014-7932. [DOI] [PubMed] [Google Scholar]
- 8.Sala Frigerio C, De Strooper B. Alzheimer's Disease Mechanisms and Emerging Roads to Novel Therapeutics. Annu Rev Neurosci. 2016 Jul;39((1)):57–79. doi: 10.1146/annurev-neuro-070815-014015. [DOI] [PubMed] [Google Scholar]
- 9.Suzuki K, Iwata A, Iwatsubo T. The past, present, and future of disease-modifying therapies for Alzheimer's disease. Proc Jpn Acad, Ser B, Phys Biol Sci. 2017;93((10)):757–71. doi: 10.2183/pjab.93.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hung SY, Fu WM. Drug candidates in clinical trials for Alzheimer's disease. J Biomed Sci. 2017 Jul;24((1)):47. doi: 10.1186/s12929-017-0355-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pinheiro L, Faustino C. Therapeutic Strategies Targeting Amyloid-β in Alzheimer's Disease. Curr Alzheimer Res. 2019;16((5)):418–52. doi: 10.2174/1567205016666190321163438. [DOI] [PubMed] [Google Scholar]
- 12.Wolfe MS. Unraveling the complexity of γ-secretase. Semin Cell Dev Biol. 2020 Sep;105:3–11. doi: 10.1016/j.semcdb.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Scheltens P, Blennow K, Breteler MM, de Strooper B, Frisoni GB, Salloway S, et al. Alzheimer's disease. Lancet. 2016 Jul;388((10043)):505–17. doi: 10.1016/S0140-6736(15)01124-1. [DOI] [PubMed] [Google Scholar]
- 14.Ni Y, Zhao X, Bao G, Zou L, Teng L, Wang Z, et al. Activation of beta2-adrenergic receptor stimulates gamma-secretase activity and accelerates amyloid plaque formation. Nat Med. 2006 Dec;12((12)):1390–6. doi: 10.1038/nm1485. [DOI] [PubMed] [Google Scholar]
- 15.Davis HE, Belk KE. Managing meat exports considering production technology challenges. Anim Front. 2018 Jun;8((3)):23–9. doi: 10.1093/af/vfy007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alzheimer's Association Alzheimer's disease facts and figures. Alzheimers Dement. 2020;2020((3)):391–460. [Google Scholar]
- 17.Chai GS, Wang YY, Yasheng A, Zhao P. Beta 2-adrenergic receptor activation enhances neurogenesis in Alzheimer's disease mice. Neural Regen Res. 2016 Oct;11((10)):1617–24. doi: 10.4103/1673-5374.193241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bortolotto V, Bondi H, Cuccurazzu B, Rinaldi M, Canonico PL, Grilli M. Salmeterol, a β2 Adrenergic Agonist, Promotes Adult Hippocampal Neurogenesis in a Region-Specific Manner. Front Pharmacol. 2019 Sep;10:1000. doi: 10.3389/fphar.2019.01000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang QW, Rowan MJ, Anwyl R. Inhibition of LTP by beta-amyloid is prevented by activation of beta2 adrenoceptors and stimulation of the cAMP/PKA signalling pathway. Neurobiol Aging. 2009 Oct;30((10)):1608–13. doi: 10.1016/j.neurobiolaging.2007.12.004. [DOI] [PubMed] [Google Scholar]
- 20.Li S, Jin M, Zhang D, Yang T, Koeglsperger T, Fu H, et al. Environmental novelty activates β2-adrenergic signaling to prevent the impairment of hippocampal LTP by Aβ oligomers. Neuron. 2013 Mar;77((5)):929–41. doi: 10.1016/j.neuron.2012.12.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu H, Gelyana E, Rajsombath M, Yang T, Li S, Selkoe D. Environmental Enrichment Potently Prevents Microglia-Mediated Neuroinflammation by Human Amyloid β-Protein Oligomers. J Neurosci. 2016 Aug;36((35)):9041–56. doi: 10.1523/JNEUROSCI.1023-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Xu H, Rajsombath MM, Weikop P, Selkoe DJ. Enriched environment enhances β-adrenergic signaling to prevent microglia inflammation by amyloid-β. EMBO Mol Med. 2018 Sep;10((9)):e8931. doi: 10.15252/emmm.201808931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Congdon EE, Sigurdsson EM. Tau-targeting therapies for Alzheimer disease. Nat Rev Neurol. 2018 Jul;14((7)):399–415. doi: 10.1038/s41582-018-0013-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Townsend DJ, Mala B, Hughes E, Hussain R, Siligardi G, Fullwood NJ, et al. Circular Dichroism Spectroscopy Identifies the β-Adrenoceptor Agonist Salbutamol As a Direct Inhibitor of Tau Filament Formation in Vitro. ACS Chem Neurosci. 2020 Jul;11((14)):2104–16. doi: 10.1021/acschemneuro.0c00154. [DOI] [PubMed] [Google Scholar]
- 25.Zaitseva NV, Shur PZ, Atiskova NG, Kiryanov DA, Kamaltdinov MR. Health risk assessment of exposure to ractopamine through consumption of meat products. Int J Adv Res (Indore). 2014;2((9)):538–45. [Google Scholar]
- 26.Filippi L, Chiaravalloti A, Bagni O, Schillaci O. 18F-labeled radiopharmaceuticals for the molecular neuroimaging of amyloid plaques in Alzheimer's disease. Am J Nucl Med Mol Imaging. 2018 Aug;8((4)):268–81. [PMC free article] [PubMed] [Google Scholar]
- 27.Zimmer ER, Leuzy A, Benedet AL, Breitner J, Gauthier S, Rosa-Neto P. Tracking neuroinflammation in Alzheimer's disease: the role of positron emission tomography imaging. J Neuroinflammation. 2014 Jul;11((1)):120. doi: 10.1186/1742-2094-11-120. [DOI] [PMC free article] [PubMed] [Google Scholar]