Abstract
Introduction
Medical societies have heavily prioritized preventive care, as evidenced by numerous best practice guidelines supporting counseling patients on lifestyle factors. This report examines preventive counseling by healthcare providers in a rural healthcare system. We utilized electronic medical records to determine whether patient characteristics and chronic conditions were predictors of preventive counseling, and what the average time-interval was before a patient received this counseling.
Methods
Medical records from a cohort of 395 subjects participating in the 1999 Bassett Health Census Survey were reviewed for documented counseling with respect to smoking cessation, weight management, physical activity, and health condition-related diets (anti-hypertensive and diabetic diets).
Results
Our analyses revealed extensive delays in counseling for smoking cessation among smokers (median time to counseling = 4.2 years), for weight management among the obese (median time = 4.8 years), and for physical activity for all subjects (median time = 10.9 years). For those with diabetes, a median time of 7.5 years passed before being counseled on a diabetic diet. Hypertensive diet counseling did not occur for more than 50% of hypertensives.
Conclusion
In this population, we did not find documentation of lifestyle counseling that was in compliance with current guidelines for any of the lifestyle factors. The measurement of actual delay times provides further support for the position that preventive efforts of health care providers need to be improved.
Keywords: lifestyle counseling, time-to-event analysis, chronic disease prevention, preventive healthcare, physicians
Introduction
The adverse health effects of obesity, smoking, hypertension, and diabetes in America are well documented. These effects involve not only the individual’s health, but also society in general when one considers the increased health costs and lost productivity.1-4 Therefore, it is a major priority in this country to address these health issues, as demonstrated by Healthy People 2020. 5
Approximately 38% of the population is obese (defined as a body mass index (BMI) ≥ 30 kg/m2), 4 17% are smokers, 2 29% are hypertensive, 3 and 9% are diabetic. 1 Many more people are at risk for these diseases as well; 31% have pre-hypertension, 3 over 35% are classified as pre-diabetic, 1 and about a third are overweight (defined as a body mass index (BMI) of 25-29.9 kg/m2). 4
Obesity is the second leading cause of preventable death in America. It was estimated that in 1999 almost 300 000 people died from obesity related causes. 6 According to the CDC, the US spends 147 billion dollars annually on direct medical care costs related to obesity and between 3.4 billion and 6.4 billion indirectly for increased work absenteeism and lost productivity. 4 Research has shown that when healthcare practitioners recommend that patients lose weight, they are more likely to lose weight and keep the weight off than patients who do not receive this recommendation. 7 Although, surprisingly, practitioners are less likely to recommend weight loss than expected. Most studies show that practitioners counsel obese patients on weight loss less than half the time,8-11 and 1 study puts that number as low as 15%. 12
According to CDC estimates, 40 million Americans currently smoke. Consequently, smoking is the leading cause of preventable death in America, killing 480 000 people every year. While the percentage of smokers has declined from 21% in 2005 to 17% in 2014, 2 healthcare practitioners could still do more to improve the results.12,13
Almost one third of Americans have hypertension, and only about half of them have their hypertension under control. In 2013, 360 000 Americans had high blood pressure as a primary or contributing cause of death, with many of these deaths preventable through lifestyle modifications and medical treatments. 3 Lower blood pressure is associated with many health benefits, including decreased risk of stroke and heart disease. 14 Involvement from one’s doctor and other healthcare professionals plays a key role in a patient’s ability to lower his/her blood pressure. 3 However, studies suggest that physicians aren’t doing a good job in their treatment of hypertension.14,15
Almost a quarter million deaths a year list diabetes as the main or contributing factor. Over 90% of diabetics have type 2 diabetes mellitus, which can be prevented through exercise and diet. 1 Again, many studies are critical of healthcare practitioners’ treatment of diabetes and many practitioners find treating diabetes to be more difficult than the treatment of hypertension, angina, hyperlipidemia and arthritis. 16
There is also a synergy to these issues; obesity and smoking increase one’s risk of diabetes and hypertension.16-18 This means that a failure in the treatment of obesity or smoking is a failure in the treatment for diabetes and hypertension.
This report examines the documentation of preventive efforts of healthcare providers in a rural healthcare system. The study had 2 goals: First, to determine whether obesity, hypertension, diabetes, smoking, and gender were predictors of preventive counseling. Second, to see how long the average patient had to wait before they received preventive counseling for a documented condition.
Methods
Study Setting
This study was conducted in rural, central New York in Otsego, Schoharie, Chenango, Montgomery, Herkimer, Delaware, and Madison counties. 19 The study counties are more than 90% rural with only 2 municipalities of greater than 10 000 inhabitants.20,21 These counties are served by an integrated health care system (Bassett Healthcare) that includes an academic medical center and more than 2 dozen primary care clinics. This region has been noted to have high prevalence of cardiovascular disease and relevant risk factors, including obesity. 22 The median income of the 7-county region was $39 157 at the time of the 1999 Bassett Health Census and roughly 36% of the population had an educational attainment of high school or less. 23
1999 Bassett Health Census
The 1999 Bassett Health Census consisted of a survey that assessed chronic disease, obesity, and positive and negative health behaviors. All permanent residents (residing ≥6 months of the year) of Otsego County were mailed survey forms in the summer of 1999, along with a sample of 5000 permanent residences in each of the 6 surrounding counties (30 000 total). A month after the forms were mailed, a follow-up letter was sent encouraging people that did not complete the form to do so. Lastly, random samples of 200 subjects from each county who did not respond to either the initial mailing or the follow-up letter were offered a financial incentive to complete the questionnaire either by mail or telephone. 24 These methods resulted in a weighted combined response rate of 75.1%. Comparisons of survey responders and non-responders revealed no meaningful differences with regard to median household income, number of household members, or age of the head of household. 24
This survey data was combined with electronic medical records from the Bassett Healthcare Network for 405 census participants who received their care there. These 405 subjects were selected at random from all subjects who had at least 1 year of follow-up documented in the medical record. Data were abstracted for only those visits occurring after age 18; 10 subjects with no data after age 18 were excluded from analysis.
Abstraction of Data from the Electronic Medical Record
The electronic medical record (EMR) at Bassett Healthcare is divided into many individual systems. These include EPIC-Unity, GE-IDX, McKesson HPF Web, Meditech, and Bassett Electronic Medical Record Star Panel. Initially the subjects were identified using GE-IDX. However, to complete the data set and assess all of the endpoints, it was necessary to abstract data manually from the other 4 systems. This involved tracking each patient’s follow-up visits from 2003 to 2016. For each visit, we recorded height, weight, blood pressure, pulse, and smoking status. Furthermore, we documented whether the practitioner mentioned smoking cessation counseling, weight loss counseling, physical activity recommendations, an anti-hypertensive diet, a diabetic diet, or performed a foot exam. Appointments were limited to primary care, cardiology, podiatry, vascular, neurology, pulmonary, endocrinology, obstetrics and gynecology, and emergency room visits. A great deal of the information relating to the patients’ counseling had to be abstracted from the free text of the provider’s note. Weekly meetings were held with the research project team to validate the data abstraction process and discuss any records where a consensus was required to complete the abstraction.
Definition of Counseling
Patients whose records contained written documentation to lessen or quit smoking habits were considered to have been given smoking cessation counseling. Similarly, records with written documentation relating to the patients’ weight (gain, lose, or maintain) were considered to contain counseling on weight management. Written documentation to change activity regimens was taken as proof of activity recommendations. A patient recommended for a DASH diet or low sodium diet due to hypertension was considered to have been recommended for an antihypertensive diet. Similarly, patients who were told to go on an American Diabetes Association diet, count their carbohydrates, or cut back on simple sugars, were considered to have been counseled for a diabetic diet. Lastly, a foot exam was considered to have been done if any part of the bare foot was examined.
Assigning Baseline Values
To establish baseline obesity, we obtained weight and height from the self-reported information on the health census and calculated BMI using the formula BMI = weight (kg)/height (m2). To estimate measured BMI from self-reported values, linear regression equations were used to apply correction factors to self-reported height and weight. 25 Patients having a BMI of 30 kg/m2 or greater were defined as obese. Similarly, smoking status and gender were taken from the self-reported health census. Diabetic status could have been indicated in 1 of 3 ways: (1) A response of “yes” to the health census question, “Have you ever been told by a physician that you have diabetes,” (2) Their GE-IDX visit closest to the date of completion of the health census (if within 1 year) had an ICD-9 indicating diabetes (code 250.xx), or (3) Any other abstracted information (also within 1 year of the census), such as the practitioners note taken from the EMR indicated diabetes. The same strategy was used to determine baseline hypertension. Baseline age was taken at the time of the 1999 Health Census. All procedures performed in this study were in accordance with the ethical standards of the Mary Imogene Bassett Hospital Institutional Review Board.
Measurement of Time to Counseling
Follow-up time to each counseling outcome was measured from the date of the first abstracted EMR visit to the date of notation of the counseling. Uncounseled subjects were right-censored for each outcome at the time of the last abstracted visit.
Statistical Analyses
Univariate proportional hazards regression models were used to test the relationship of each of the 6 baseline covariates (age, obesity, hypertension, diabetes, smoking status, and gender) to time to each of the counseling outcomes. Following this, multivariable survival models were created for time to counseling for (1) anti-hypertensive diet, (2) weight management, (3) diabetic diet, (4) foot exam, (5) activity recommendations, and (6) smoking cessation. These models contained any baseline covariate that was significant (P < .05) in the univariate analyses. Attempts were made to try to model the multiplicative effects of having more than one of the comorbidities. However, due to the large possible number of combinations of comorbidities versus the sample size, these analyses were not possible. Instead, the presence or absence of the other comorbidities were included in the models as a means of adjusting for any condition that was predictive of the counseling outcome(s).
Stratified Kaplan-Meier (KM) survival curves were created for various strata of the 6 baseline variables. These included smoker versus non-smoker and time to smoking cessation, obese versus non obese and time to weight management, diabetic versus non-diabetic and time to both foot exam and diabetic diet counseling, hypertensive versus non-hypertensive, and time to an anti-hypertensive diet. Finally a KM curve for time to activity recommendations was created for the combined sample without stratification. Median survival time to each outcome was also recorded.
There were instances where the GE-IDX data for a patient indicated that a visit had occurred where the data from the EMR system that contained the counseling outcomes were not available. In order to estimate the effect of this missing data on time to the counseling outcomes a sensitivity analysis was performed. Specifically, median time to counseling for each outcome was estimated for subjects with less than 10% missing data, less than 33% missing data, and less than 50% missing data.
All statistical analyses were performed using SAS 9.3 (Cary, NC).
Results
Of the 395 eligible patients (321 for the obesity variable as the frequency missing was 74), 94 (29.3%) were obese, 133 (33.67%) were hypertensive, 45 (11.4%) were diabetic, 60 (18.6%) were smokers and 183 (46.3%) were male. At baseline, 147/395 subjects (37.2%) did not have documented obesity, hypertension, or diabetes. The ages of the subjects at the time of their first recorded visit ranged from 18.1 to 94.9 years old, with a mean age of 53.3 years.
For obese patients, 59.6% (56/94) were counseled at least once on weight management over the course of follow-up versus only 22% (49/227) of non-obese patients. Median time to counseling for obese patients was 4.8 years (Figure 1).
Figure 1.
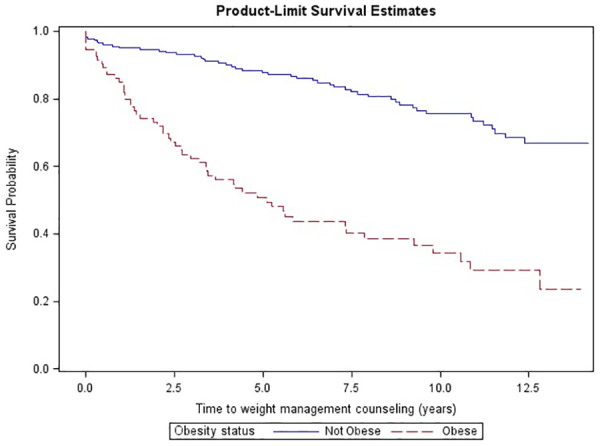
Kaplan-Meier survival curve for time to weight management counseling among obese (BMI ≥ 30 kg/m2) and non-obese (BMI < 30 kg/m2) subjects in the 1999 Bassett Health Census.
Non-obese patients did not reach median time throughout more than 14 years of follow-up. Obesity, hypertension, and diabetes were all significantly predictive of earlier weight management counseling at the univariate level; however, only obesity was retained as an independent predictor in the multivariable model (Table 1).
Table 1.
Unadjusted and adjusted hazard ratios for time to counseling on weight management, physical activity, a diabetic diet, and smoking cessation among n = 395 participants of the 1999 Bassett Health Census.
| Time to counseling for. . . | Predictor | Unadjusted hazard ratio (95% CI) | P * | Adjusted hazard ratio (95% CI) | P * |
|---|---|---|---|---|---|
| Weight management | Obesity | 4.14 (2.81-6.10) | <.001 | 3.83 (2.52-5.84) | <.001 |
| Hypertension | 1.63 (1.13-2.35) | .001 | 1.04 (0.68-1.57) | .87 | |
| Diabetes | 2.58 (1.63-4.07) | <.001 | 1.29 (0.77-2.17) | .33 | |
| Physical activity | Obesity | 1.70 (1.20-2.42) | .003 | 1.52 (1.05-2.22) | .03 |
| Diabetes | 2.08 (1.34-3.21) | .001 | 1.61 (1.00-3.44) | .05 | |
| Anti-hypertensive diet | Hypertension | 2.91 (1.70-4.98) | <.001 | 2.54 (1.37-4.71) | .003 |
| Obesity | 1.89 (1.08-3.33) | .03 | 1.52 (0.85-2.72) | .16 | |
| Age | 1.02 (1.00-1.04) | .02 | 1.01 (0.99-1.03) | .67 | |
| Diabetic diet | Obesity | 6.18 (3.21-11.89) | .02 | 3.55 (1.76-7.16) | <.001 |
| Diabetes | 10.83 (5.90-19.91) | <.001 | 4.73 (2.39-9.34) | <.001 | |
| Hypertensive | 4.60 (2.45-8.64) | <.001 | 2.19 (1.06-4.53) | .03 | |
| Age | 1.02 (1.00-1.04) | .0163 | 1.0 (0.97-1.02) | .72 | |
| Smoking cessation | Smoker | 45.38 (17.79-115.79) | <.001 | 43.05 (16.78-110.43) | <.001 |
| Hypertension | 0.44 (0.22-0.92) | .03 | 0.70 (0.33-1.47) | .34 |
P for likelihood ratio chi square test, proportional hazards regression models.
Among obese patients, 53.2% (50/94) received physical activity recommendations versus 37.0% (84/227) of non-obese patients. As shown in Table 1, the only significant predictors of this outcome were obesity and diabetes. The Kaplan-Meier analysis among all subjects showed that only 39% were given activity recommendations (regardless of weight status), and 10.9 years passed before half of them received that advice.
Hypertension, obesity, and age were significant univariate predictors of time to counseling for an anti-hypertensive diet, with hypertension the only independent predictor in the adjusted model. Such counseling was more common among those with hypertension versus those without, 21.8% (29/133) to 9.5% (25/262). Median survival time, both for those with or without hypertension, was not reached over the course of the 14-year follow-up period.
Median time to counseling for an anti-diabetic diet among diabetic patients was 7.5 years. Over the entire course of follow-up, a diabetic diet was recommended to 42.2% (19/45) of diabetics as opposed to only 6.9% (24/350) of non-diabetics (HR = 10.83, P < .001). Additionally, 30.9% (29/94) of subjects with obesity as opposed to 5.73% (13/227) of those without obesity were told to go on a diabetic diet (HR = 6.18, P = .02). These 2 predictors remained significant in the multivariable equation to predict time to counseling, as did hypertension (Table 1).
Median time to smoking cessation counseling for smokers was 4.2 years (Figure 2).
Figure 2.
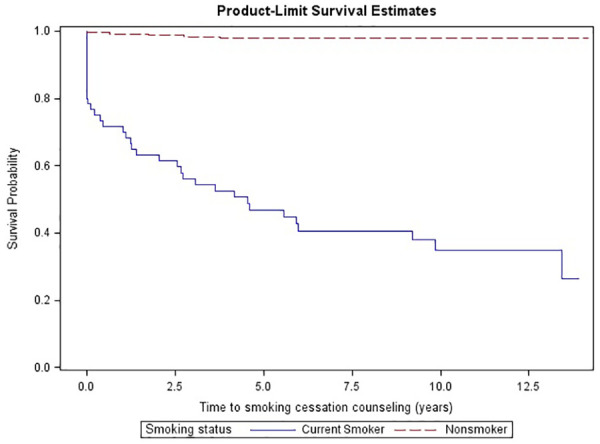
Kaplan-Meier survival curve for time to smoking cessation counseling among smokers and non-smoking subjects in the 1999 Bassett Health Census.
Over 1 quarter (38.3% or 23/60) of patients who smoked had no documentation of smoking cessation counseling at any time. In addition to smoking (HR = 45.38, P < .001), time to smoking cessation counseling was inversely related to hypertension (HR = 0.44, P = .03) at the univariate level (Table 1). However, hypertension was no longer a significant predictor after controlling for smoking status.
The only predictors of a foot exam were diabetes (HR = 1.53, P = .01) and age (HR = 1.01, P = .01) with the median time to exam just over 1 month for diabetics.
Sensitivity Analyses
Table 2 shows the effect of missing data (visits for which electronic data were unavailable) on estimated median time to counseling. It is noteworthy that the effect of missing data on median survival time, even when as high as 50%, is typically less than 1 year. The main exception to this was for smoking cessation counseling. Overall, these data indicate that the results are relatively insensitive to missing visits in the electronic medical record.
Table 2.
Effect of missing data on median time to counseling among n = 395 participants of the 1999 Bassett Health Census.
| Median time to counseling (in years) for | N | All records | ≤50% missing data | ≤33% missing data | ≤10% missing data |
|---|---|---|---|---|---|
| Weight management (for obese subjects) | 94 | 4.8 | 5.1 | 5.6 | 5.6 |
| Physical activity recommendations (for all subjects) | 395 | 10.9 | 11.5 | 11.8 | 13.3 |
| Diabetic diet (for diabetic subjects) | 45 | 7.5 | 8.3 | 8.3 | 8.3 |
| Hypertensive diet* (for hypertensive subjects) | 133 | 9.4 | 9.4 | 9.4 | 8.8 |
| Foot exam (for diabetic subjects) | 45 | 0.1 | 0.1 | 0.1 | 0.1 |
| Smoking cessation (for smokers) | 60 | 4.2 | 4.2 | 4.2 | 4.2 |
Mean value given as sample did not reach 50% counseled.
Discussion
To our knowledge, there has been no research that has looked at the duration of time before an obese, hypertensive, diabetic, or smoking patient was counseled to treatment. Our time-to-counseling data are consistent with many previous studies of the prevalence of subjects who have been counseled, confirming that these patients are not receiving the counseling that they need. Further, even among patients who are receiving the counseling, it is not being delivered in a timely manner.
Previous research has shown that healthcare practitioners can have a substantial impact on starting patients on the right path towards a healthy lifestyle when they deliver lifestyle counseling. In 1 study, overweight and obese patients that discussed weight loss with their physician were more than twice as likely to lose 10% of their body weight than those who didn’t discuss it. 7 Another study reported that patients who recalled being counseled felt more prepared to lose weight than those who did not recall receiving such counseling. 26 However, that study found that only 5% of patients recalled being counseled on weight loss. This result, in conjunction with our finding that nearly 5 years passed before half of obese patients were counseled, and over 15 years before all obese patients had been counseled, indicates an alarming degree of missed opportunity. Similar delays were observed for 2 of obesity’s primary co-morbidities; hypertension and diabetes.
As has been shown for weight loss counseling, when a practitioner counsels a patient about smoking cessation they are more likely to quit. 27 However, the prevalence of a physician’s counseling on smoking cessation, 21% on any given visit in 1 study, 28 has also been shown to be inadequate. We found that the average smoker waited more than 4 years before they received counseling. This also underscores the inadequacy of counseling in this area.
Over the past 2 decades, several national and international medical associations were calling for increases in counseling for unhealthy lifestyle habits. In 2013 the American Heart Association, the American College of Cardiology and The Obesity Society made recommendations that all patients with BMIs over 25 be advised to lose weight and all patients with BMIs under 25 be recommended to avoid weight gain. 29 In 1998 the Centre for Health Economics at the University of York also recommended healthcare professionals advise smokers to quit at every visit. 30 It was also recommended by the World Health Organization and the International Society of Hypertension that all hypertensive patients watch their weight, increase exercise, and change to a healthier diet. 31 The same recommendations were made by the American Diabetes Association. 32
Clearly, there is no shortage of guidelines with respect to healthcare practitioner counseling for healthy lifestyles. However, it is possible that provision of such guidelines, without accompanying recommendations and training for how to deliver this counseling, is inadequate to change practitioner behavior. Among the barriers to counseling that physicians have reported is their lack of confidence in their patient’s willingness to follow such advice. 26 In the same study, lack of weight loss resources and insufficient time were also mentioned. General practitioners have also stated certain types of counseling, such as smoking cessation, could hinder their relationship with their patients. 33
Until these barriers to counseling, (time, training, and resources) are addressed, it seems unlikely that practitioners’ counseling for healthy lifestyles will increase in prevalence and timeliness. The reluctance of insurance companies to provide financial incentives or reimbursements for such counseling is also a major impediment. For example, although the Affordable Care Act has recommended state-level insurance coverage for nutritional counseling for obesity, only 16 states have enacted the coverage (New York is not one of them). 34 With regard to smoking cessation counseling, Medicare does have a reimbursement mechanism, but it requires that the practitioner document the time spent counseling (in minutes) and apply the proper procedure codes. Most private insurers do not provide any such reimbursement for smoking cessation counseling. 35 There appears to be a great need for the institutes that provide these recommendations and guidelines to also champion the removal of these barriers.
The main limitation in our study was access to patient data. This limitation came in several forms. As discussed, some visits could not be abstracted from the EMR and so our assessment of the time to counseling could have been overestimated. The sensitivity analysis that was performed with various levels of missing data suggests that this did not have major impact on the conclusions. A second limitation was that we only had the ability to record what was written in the EMR. It is plausible that healthcare practitioners could have recommended counseling and not documented it.
In this population, unacceptable delays were found in preventive care counseling for smoking cessation, weight management, physical activity, and prevention and management of both hypertension and diabetes. The measurement of these actual delay times provides further support for the position that preventive efforts of health care providers need to be improved.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Melissa Brower Scribani  https://orcid.org/0000-0002-2397-3337
https://orcid.org/0000-0002-2397-3337
References
- 1. American Diabetes Association. Statistics about diabetes. 2017. Accessed August 15, 2018. http://www.diabetes.org/diabetes-basics/statistics/
- 2. Centers for Disease Control and Prevention. Current cigarette smoking among adults in the United States. 2017. Accessed August 15, 2018. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/
- 3. Centers for Disease Control and Prevention. High blood pressure facts. 2017. Accessed August 15, 2018. https://www.cdc.gov/bloodpressure/facts.htm
- 4. Centers for Disease Control and Prevention. National Center for Health Statistics: obesity and overweight. 2017. Accessed February 13, 2018. https://www.cdc.gov/nchs/fastats/obesity-overweight.htm
- 5. Office of Disease Prevention and Health Promotion. Healthy people 2020. 2017. Accessed June 26, 2017. https://www.healthypeople.gov/2020/About-Healthy-People
- 6. Allison DB, Fontaine KR, Manson JE, Stevens J, VanItallie TB. Annual deaths attributable to obesity in the United States. JAMA. 1999;282:1530-1538. [DOI] [PubMed] [Google Scholar]
- 7. Pool AC, Kraschnewski JL, Cover LA, Lehman EB, Stuckey HL, Hwang KO, et al. The impact of physician weight discussion on weight loss in US adults. Obes Res Clin Pract. 2014;8(2):e131-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Galuska DA, Will JC, Serdula MK, Ford ES. Are health care professionals advising obese patients to lose weight? JAMA. 1999;282:1576-1578. [DOI] [PubMed] [Google Scholar]
- 9. Jackson JE, Doescher MP, Saver BG, Hart LG. Trends in professional advice to lose weight among obese adults, 1994 to 2000. J Gen Intern Med. 2005;20:814-818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. JAMA. 2001;286:1195-1200. [DOI] [PubMed] [Google Scholar]
- 11. Sciamanna CN, Tate DF, Lang W, Wing RR. Who reports receiving advice to lose weight? Results from a multistate survey. Arch Intern Med. 2000;160:2334-2339. [DOI] [PubMed] [Google Scholar]
- 12. Stafford RS, Farhat JH, Misra B, Schoenfeld DA. National patterns of physician activities related to obesity management. Arch Fam Med. 2000;9:631-638. [DOI] [PubMed] [Google Scholar]
- 13. Eckert T, Junker C. Motivation for smoking cessation: what role do doctors play? Swiss Med Wkly. 2001;131:521-526. [DOI] [PubMed] [Google Scholar]
- 14. Oliveria SA, Lapuerta P, McCarthy BD, L’Italien GJ, Berlowitz DR, Asch SM. Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162:413-420. [DOI] [PubMed] [Google Scholar]
- 15. Berlowitz DR, Ash AS, Hickey EC, et al. Inadequate management of blood pressure in a hypertensive population. N Engl J Med. 1998;339:1957-1963. [DOI] [PubMed] [Google Scholar]
- 16. Larme AC, Pugh JA. Attitudes of primary care providers toward diabetes: barriers to guideline implementation. Diabetes Care. 1998;21:1391-1396. [DOI] [PubMed] [Google Scholar]
- 17. Centers for Disease Control and Prevention. Smoking and diabetes. 2017. Accessed February 5, 2017. https://www.cdc.gov/tobacco/campaign/tips/diseases/diabetes.html
- 18. Re RN. Obesity-related hypertension. Ochsner J. 2009;9:133-136. [PMC free article] [PubMed] [Google Scholar]
- 19. Jenkins PL, Earle-Richardson G, Bell EM, May JJ, Green A. Chronic disease risk in central New York dairy farmers: results from a large health survey 1989-1999. Am J Ind Med. 2005;47:20-26. [DOI] [PubMed] [Google Scholar]
- 20. U.S. Census Bureau. 2010 census urban and rural classification and urban area criteria. 2012. Accessed December 21, 2018. https://www.census.gov/programs-surveys/geography/guidance/geo-areas/urban-rural/2010-urban-rural.html
- 21. Census Bureau. State and County QuickFacts. 2010. Accessed December 20, 2018. https://www.census.gov/quickfacts/fact/table/US/PST045218
- 22. Pearson TA, Lewis C. Rural epidemiology: insights from a rural population laboratory. Am J Epidemiol. 1998;148:949-957. [DOI] [PubMed] [Google Scholar]
- 23. U.S. Department of Agriculture Economic Research Service. 2000.Accessed April 30, 2021. https://data.ers.usda.gov/reports.aspx?ID=17829
- 24. Jenkins P, Scheim C, Wang JT, Reed R, Green A. Assessment of coverage rates and bias using double sampling methodology. J Clin Epidemiol. 2004;57:123-130. [DOI] [PubMed] [Google Scholar]
- 25. Scribani M, Shelton J, Chapel D, et al. Comparison of bias resulting from two methods of self-reporting height and weight: a validation study. JRSM Open. 2014;5(6):2042533313514048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Huang J, Yu H, Marin E, Brock S, Carden D, Davis T. Physicians’ weight loss counseling in two public hospital primary care clinics. Acad Med. 2004;79:156-161. [DOI] [PubMed] [Google Scholar]
- 27. West R, McNeill A, Raw M. Smoking cessation guidelines for health professionals: an update. Health Education Authority. Thorax. 2000;55:987-999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Thorndike AN, Rigotti NA, Stafford RS, Singer DE. National patterns in the treatment of smokers by physicians. JAMA. 1998;279:604-608. [DOI] [PubMed] [Google Scholar]
- 29. Shin M-S. Management of overweight and obesity: review of the “2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults”. Korean J Med. 2014;87:136. [Google Scholar]
- 30. Raw M, McNeill A, West R. Smoking cessation guidelines for health professionals. A guide to effective smoking cessation interventions for the health care system. Health Education Authority. Thorax. 1998;53: S1-S19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Whitworth JA. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003;21:1983-1992. [DOI] [PubMed] [Google Scholar]
- 32. American Diabetes Association. Standards of medical care in diabetes—2014. Diabetes Care. 2014;37:S14-S80. [DOI] [PubMed] [Google Scholar]
- 33. Coleman T, Murphy E, Cheater F. Factors influencing discussion of smoking between general practitioners and patients who smoke: a qualitative study. Br J Gen Pract. 2000;50:207-210. [PMC free article] [PubMed] [Google Scholar]
- 34. Cauchi R, Noble A. National conference of state legislatures: health reform and health mandates for obesity. 2015-2016. Accessed April 30, 2021. https://www.ncsl.org/research/health/aca-and-health-mandates-for-obesity.aspx
- 35. Theobald M, Jaen CR. An update on tobacco cessation reimbursement. Fam Pract Manag. 2006;13(5):75-78. [PubMed] [Google Scholar]


