Abstract
Background:
The outcomes after high tibial osteotomy (HTO) with augmentation of intra-articular mesenchymal stem cell (MSCs) for medial tibiofemoral osteoarthritis remain controversial.
Purpose:
To pool existing studies to compare the outcomes of HTO with versus without intra-articular MSC augmentation when performed for medial tibiofemoral osteoarthritis.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
The systematic review was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Included were clinical studies that compared the outcomes of HTO with intra-articular MSC augmentation (MSC group) versus without (control group). Pre- and postoperative outcomes were compared between groups from measures including the Lysholm score, International Knee Documentation Committee (IKDC) score, Knee injury and Osteoarthritis Outcome Score, Hospital for Special Surgery Knee Rating Scale, Tegner score, visual analog scale for pain, arthroscopic and histological grading scales, femorotibial angle, weightbearing line, and posterior tibial slope.
Results:
We reviewed 4 studies with a total of 224 patients. The MSC group demonstrated significantly greater improvement versus controls in the pooled Lysholm score (weighted mean difference [WMD], 6.64; 95% CI, 0.90 to 12.39) and pooled IKDC score (WMD, 9.21; 95% CI, 4.06 to 14.36), which were within or close to the minimal clinically important difference. Radiological outcomes were similar in both groups, including the femorotibial angle (WMD, –0.01; 95% CI, –1.10 to 1.09), weightbearing line, and posterior tibial slope. The studies were homogeneous, and no publication bias was noted.
Conclusion:
Intra-articular MSC augmentation for HTO may modestly improve functional outcomes as compared with HTO alone. However, adequate data are lacking to make definitive conclusions regarding the effect of MSC augmentation on pain or arthroscopic and histologic grading.
Keywords: osteoarthritis, high tibial osteotomy, mesenchymal stem cell, systematic review, meta-analysis
Osteoarthritis (OA) is a common chronic joint pathology that has been estimated to affect as many as 350 million people worldwide, and it is the third leading cause of disability. 1,5 Patients often present with pain, limitation in daily activities, and reduced quality of life. However, the treatment of OA remains a challenge, and patients whose pain is not well-controlled with analgesia or anti-inflammatories often require surgeries in the form of either joint-preserving or joint-replacing surgeries. 12
High tibial osteotomy (HTO) is a common joint-preserving surgery performed in the treatment of OA. 8,14,26 It unloads the affected compartment and aims to relieve pain and slow the progression of unicompartmental knee OA to avoid or postpone knee arthroplasty in patients with unicompartmental OA. During the surgery, degenerative cartilage is often observed in the involved compartment, triggering the use of various surgical techniques to attempt to promote cartilage regeneration, with the hopes of delaying the progress of osteoarthritis.
Mesenchymal stem cell (MSC) augmentation is one form of increasingly popular regenerative medicine for OA, as reflected by the large number of clinical trials conducted. 2,4,9,10,15,18 –20,25 Despite this, the outcomes after HTO with augmentation of intra-articular MSCs remain controversial, with one meta-analysis suggesting that concurrent procedures performed during HTO are of little benefit, while another meta-analysis suggests some possible beneficial effects. 14,26 However, these meta-analyses focused on a variety of concurrent procedures including MSC augmentation, marrow-stimulation procedures, autologous chondrocyte implantation, platelet-rich plasma (PRP) augmentation, hyaluronic acid augmentation, and collagen augmentation. None of the meta-analyses have focused on the outcomes of HTO with or without intra-articular MSC augmentation; therefore, the effect of intra-articular MSC augmentation on HTO remains controversial.
The current systematic review and meta-analysis therefore aims to answer whether the addition of intra-articular MSC augmentation will improve the outcomes of HTO. All clinical studies that compared the outcomes of HTO without intra-articular MSC augmentation and the outcomes of HTO with intra-articular MSC augmentation were included.
Methods
Article Selection
The current systematic review was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. A search was conducted using PubMed, MEDLINE, Cumulative Index of Nursing and Allied Health Literature (CINAHL), and The Cochrane Library from inception through May 19, 2020. The keywords used were mesenchymal or multipotent or stem or stromal or progenitor and high tibial osteotomy. All clinical studies that compared the outcomes of HTO without intra-articular MSC augmentation (control group) with the outcomes of HTO with intra-articular MSC augmentation (MSC group) were included. Excluded were articles that did not include HTO or intra-articular MSC augmentation; those that did not compare between HTO with and without intra-articular MSC augmentation; those with no clinical outcomes; nonhuman studies; and review articles.
The articles were selected in 2 stages. First, the abstracts of the articles that had been identified were downloaded and assessed based on the inclusion and exclusion criteria outlined in this article. Second, the full text of the shortlisted list was then searched for additional relevant studies. The process was repeated once independently. The selection process for the systematic review is shown in Figure 1.
Figure 1.
Selection process for systematic review. HTO, high tibial osteotomy; MSC, mesenchymal stem cell.
Quality Assessment of Studies
The studies included were examined for study design. The revised Methodological Index for Non-Randomized Studies (MINORS) tool was used to determine the methodological quality of the studies. 21 The items are scored 0 if not reported, 1 if reported but inadequate, or 2 if reported and adequate. The global ideal score is 24. This was evaluated independently by 2 authors (S.H.S.T. and Y.T.K.), and any disagreements between the 2 authors were discussed or appealed to a third author (J.H.H.) .
Data Abstraction
Data for each study were retrieved individually. These included the study design and outcomes between the control and MSC groups. Details noted regarding the study design included the sample size, patient age and sex, the comparison groups within the study, and the duration of follow-up of the studies. We included all clinical outcome measures in which both pre- and postoperative data were reported. Attempts were made to contact authors of the paper when certain details of the studies were not reported.
Data Analysis
The random-effects model was used to analyze the pooled estimates of differences between the study groups. Comparisons were made between the change in the postoperative compared to the preoperative outcomes in the MSC versus control groups. Pooling was performed when the outcomes were reported in 2 or more studies. The random-effects model assumed that the studies represented a random sample, with each study having its own underlying effect size. Under this model, it was assumed that there was a mean population effect size about which the study-specific effect varied. As the random-effects model properly accounted for the interstudy heterogeneity, such as differences in study design, it provided a more conservative evaluation of the significance of the association than one based on fixed effects. 3 The pooled weighted mean difference (WMD) and relative risk for the studies were then reported with their 95% CI and provided as forest plots.
Tests of heterogeneity were conducted for pooled studies. This was performed with the Q statistic that was distributed as a chi-square variate under the assumption of homogeneity of effect sizes. The extent of between-study heterogeneity was assessed with the I2 statistic. 6,7 Funnel plots of the sample sizes were also plotted against the standard error of each study in outcomes reported in 2 or more studies. Additionally, the Egger statistical tests were performed for outcomes reported in 3 or more studies to evaluate the possibility of publication bias. 23
All statistical evaluations were made using Stata Version 12 (Stata) assuming a 2-tailed test at a 5% CI. P < .05 was considered statistically significant. Qualitative data analysis was performed when the original data precluded quantitative data analysis.
Results
A total of 4 studies 11,13,22,24 were reviewed. They included a total of 224 patients, with 111 patients in the MSC group and 113 patients in the control group. There were 143 women and 81 men. The mean age of the patients was 56.2 years, and the mean follow-up was 29.6 months.
Patients in the control group had either HTO alone or HTO with PRP augmentation. Patients in the MSC group had the aforementioned procedures with additional intra-articular MSC augmentation; the only difference between the control and MSC groups was the presence or absence of MSC augmentation in the respective studies. The characteristics, patient details, and comparison groups of the included studies are provided in Table 1.
TABLE 1.
Characteristics of Patients and Studies a
| Author (year) | LOE | Sample Size (knees) | Female: Male Patients, n | Mean Age, y | Follow-up, mo | Control Group | MSC Group |
|---|---|---|---|---|---|---|---|
| Kim (2018) 11 | 3 | 100 | 68:32 | 58.8 | 38 | HTO alone | HTO + MSC |
| Koh (2014) 13 | 2 | 44 | 33:11 | 53.3 | 24.4 | HTO + PRP | HTO + PRP + MSC |
| Wakitani (2002) 22 | 2 | 24 | 15:9 | 63 | 16 | HTO alone | HTO + MSC |
| Wong (2013) 24 | 2 | 56 | 27:29 | 51 b | 24.7 | HTO alone | HTO + MSC |
a HTO, high tibial osteotomy; LOE, level of evidence; MSC, mesenchymal stem cells; PRP, platelet-rich plasma.
b Median reported instead of mean.
The majority of the patients (200 of 224) had opening-wedge HTO fixed with a long fixed angle locking plate, while the remaining 24 patients included in the study by Wakitani et al 22 had dome osteotomy fixed with Steinmann pins, Charnley clamps, and 2 staplers. Prior to the HTO, all patients in both the MSC and control groups included in the studies by Kim et al 11 and Koh et al 13 also had arthroscopic evaluation of the medial, lateral, and patellofemoral compartments of the knee with synovectomy, debridement, excision of degenerative meniscal tears, removal of articular cartilage fragments, chondral flaps, or osteophytes. Moreover, all patients in both the MSC and control groups included in the study by Wong et al 24 additionally had arthroscopic evaluation of the compartments and microfracture. All patients in the study by Wakitani et al underwent either open abrasion arthroplasty or microfracture.
Uncultured adipose-derived MSCs were used for the 144 patients included in the studies by Kim et al 11 and Koh et al, 13 while cultured bone marrow-derived MSCs were used for the 80 patients included in the studies by Wakitani et al 22 and Wong et al. 24 These were injected into the patients’ knees under arthroscopic guidance during the surgical procedure for patients included in the studies by Kim et al and Koh et al and via intra-articular injections 3 weeks after the HTO for the patients included in the study by Wong et al. The patients included in the study by Wakitani et al had open MSC transplantation using a gel-cell composite directly onto the eburnated bone after abrasion during the surgical procedure.
Quality Assessment of Studies
The included studies were examined for the methodological quality using the revised MINORS tool. 21 The mean MINORS score was 23.25 out of 24. Table 2 shows the results of the quality assessment.
TABLE 2.
Assessment of Study Quality According to MINORS Score a
| Author (year) | Assessment Item b | Overall Score | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||
| Kim (2018) 11 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 23/24 |
| Koh (2014) 13 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 23/24 |
| Wakitani (2002) 22 | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 23/24 |
| Wong (2013) 24 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 24/24 |
a MINORS, Methodological Index for Non-Randomized Studies.
b Key to assessment items: 1 = stated aim of the study; 2 = inclusion of consecutive patients; 3 = prospective collection of data; 4 = endpoint appropriate to the study aim; 5 = unbiased evaluation of endpoints; 6 = follow-up period appropriate to the major endpoint; 7 = loss to follow-up not exceeding 5%; 8 = control group having the gold standard intervention; 9 = contemporary groups; 10 = baseline equivalence of groups; 11 = prospective calculation of the sample size; 12 = statistical analyses adapted to the study design.
Study Outcomes
Outcome measures with both pre- and postoperative data included the Lysholm score, International Knee Documentation Committee (IKDC) score, Knee injury and Osteoarthritis Outcome Score (KOOS), Hospital for Special Surgery (HSS) Knee Rating Scale, Tegner score, visual analog scale (VAS) for pain, arthroscopic and histological grading scales, femorotibial angle, weightbearing line, and posterior tibial slope. Table 3 illustrates the outcomes reported in each study.
TABLE 3.
Outcome Measures Reported in the Included Studies a
| Author (year) | Lysholm | IKDC | KOOS | HSS Knee Rating Scale | Tegner Score | VAS Pain | Arthroscopic and Histological Grading Scale | Femorotibial Angle | Weightbearing Line | Posterior Tibial Slope |
|---|---|---|---|---|---|---|---|---|---|---|
| Kim (2018) 11 | X | X | — | — | — | — | — | X | — | X |
| Koh (2014) 13 | X | — | X | — | — | X | — | X | X | — |
| Wakitani (2002) 22 | — | — | — | X | — | — | X | — | — | — |
| Wong (2013) 24 | X | X | — | — | X | — | — | — | — | — |
a Dash indicates that the outcome measure was not reported. HSS, Hospital for Special Surgery; IKDC, International Knee Documentation Committee; KOOS, Knee injury and Osteoarthritis Outcome Score; VAS, visual analog scale.
Lysholm Score
Three studies reported the change in pre- to postoperative Lysholm scores for both the MSC and the control groups. 11,13,24 All studies reported a greater increase in Lysholm score in the MSC group compared with the control groups. The pooled WMD comparing the MSC group with the control groups was 6.64 (95% CI, 0.90-12.39) (Figure 2), 26 which is more than the minimal clinically important difference (MCID) of 4.2 for the Lysholm score. 16 The studies were homogeneous (P = .585) (Figure 2), and there was no publication bias (P = .467) (Figure 3).
Figure 2.
Forest plot comparing the Lysholm scores for high tibial osteotomy with and without MSC augmentation. Mean differences to the right of the line of null effect (vertical black line) favor the MSC group. Results that do not cross the line of null effect represent statistically significant differences. MSC, mesenchymal stem cell; WMD, weighted mean difference.
Figure 3.

Funnel plot comparing Lysholm scores with the SEs of the studies. Each dot represents a study while the dashed lines indicate the region within which 95% of the studies are expected to lie in the absence of bias and heterogeneity.
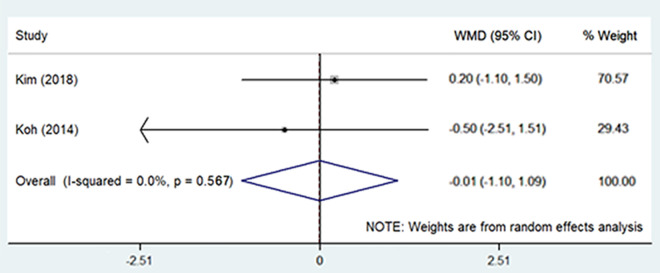
IKDC Score
Two studies reported the change in IKDC score postoperatively compared with preoperatively in both the MSC and the control groups. 11,24 Both studies reported a significant increase in IKDC score in the MSC group compared with the control groups. The pooled WMD comparing the MSC group with the control groups was 9.21 (95% CI, 4.06-14.36) (Figure 4), which is close to the MCID of 9.8 for the IKDC score. 17 The studies were homogeneous (P = .698) (Figure 4), and there was no publication bias (Figure 5).
Figure 4.
Forest plot comparing the International Knee Documentation Committee scores for HTO with MSC augmentation with HTO alone. Mean differences to the right of the line of null effect (vertical black line) favor the MSC group. Results that do not cross the line of null effect represent statistically significant differences. HTO, high tibial osteotomy; MSC, mesenchymal stem cell; WMD, weighted mean difference.
Figure 5.
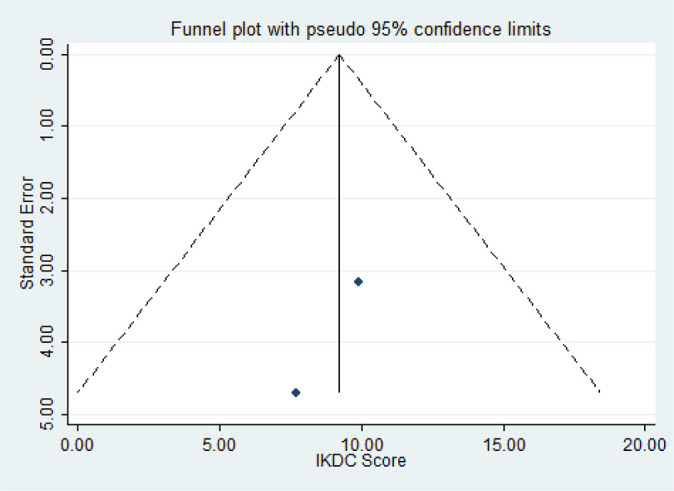
Funnel plot comparing IKDC scores with the SE of the studies. Each dot represents a study, while the dashed lines indicate the region within which 95% of the studies are expected to lie in the absence of bias and heterogeneity. IKDC, International Knee Documentation Committee.
KOOS
The KOOS score was reported in only 1 study: Koh et al. 13 In that study, patients in the MSC group showed a trend toward greater improvements in all the KOOS subscales compared with the control group. Statistically significant differences were also noted in the KOOS Pain and Symptoms subscales when comparing the improvement in the MSC group and the control group.
HSS Knee Rating Scale
Only 1 study, by Wakitani et al, 22 reported the pre- and postoperative HSS Knee Rating Scale score for both the MSC and control groups. While no statistically significant difference was found between the groups, the improvement was greater in the MSC group (65.0 ± 6.7 improved to 81.3 ± 8.6) compared with the control group (66.3 ± 10.5 improved to 79.2 ± 8.7).
Tegner Score
Tegner score was reported by only 1 study: Wong et al. 24 Statistically significant greater improvement of the Tegner score was noted in the MSC group compared with the control group, with an added improvement of 0.64 (95% CI, 0.10-1.19) for Tegner scores after adjustment for age, baseline scores, and time of evaluation. 24
VAS for Pain
The VAS for pain was reported pre- and postoperatively only in 1 study: Koh et al. 13 Both the groups showed improvement postoperatively compared with preoperatively, but the MSC group had statistically significant greater improvement in the VAS for pain as compared with the control group (10.2 ± 5.7 vs 16.2 ± 4.6).
Arthroscopic and Histological Grading Scale
Only 1 study reported the change in pre- to postoperative histological grading of the cartilage. 22 Wakitani et al 22 performed pre- and postoperative arthroscopy of the knees and reported a statistically significant greater improvement in the arthroscopic and histological grading scale for the MSC group compared with the control group. The remaining 3 studies also assessed the status of the repaired cartilage and reported significantly better repair in the MSC group compared with the control group, though the change from preoperative to postoperative status was not reported. 11,13,24 Kim et al 11 and Koh et al 13 assessed the repaired cartilage via second-look arthroscopy, while Wong et al 24 assessed the repaired cartilage using magnetic resonance imaging (MRI).
Femorotibial Angle
Two studies reported the pre and postoperative femorotibial angle in both the MSC and control groups. 11,13 No statistically significant difference was noted in the improvement of the femorotibial angle when the 2 groups were compared. The pooled WMD comparing the MSC group with the control groups was –0.01 (95% CI, –1.10 to 1.09) (Figure 6). The mean femorotibial angle achieved for Koh et al 13 was valgus 8.7° ± 2.3° for the MSC group and valgus 9.8° ± 2.4° in the control group, while the mean femorotibial angle achieved for Kim et al was valgus 8.9° ± 2.6° for the MSC group and valgus 8.8° ± 2.9° for the control group. The studies were homogeneous (P = .567) (Figure 6), and there was no publication bias (Figure 7).
Figure 6.
Forest plot comparing the femorotibial angles for HTO with MSC augmentation with HTO alone. Mean differences to the right of the line of null effect (vertical black line) favor the MSC group. Results that do not cross the line of null effect represent statistically significant differences. HTO, high tibial osteotomy; MSC, mesenchymal stem cell; WMD, weighted mean difference.
Figure 7.
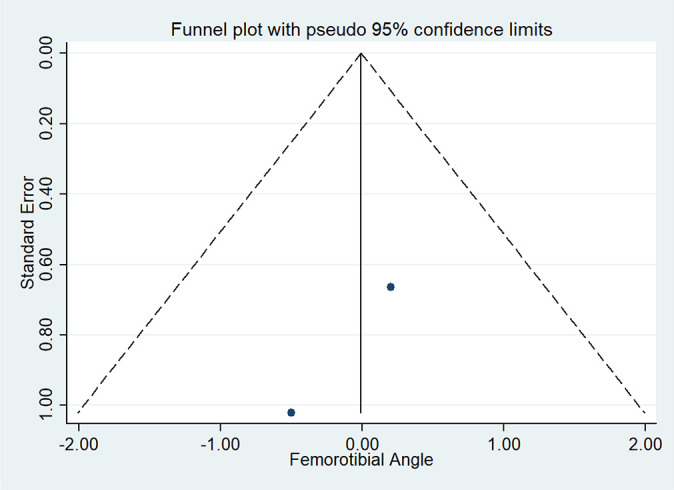
Funnel plot comparing the femorotibial angles with the SE of the studies. Each dot represents a study while the dashed lines indicate the region within which 95% of the studies are expected to lie in the absence of bias and heterogeneity.
Weightbearing Line
The position of the weightbearing line was reported by Koh et al. 13 No statistically significant difference was noted between the MSC (61.1% ± 3.4%) and the control groups (60.3% ± 3.0%) with regard to the weightbearing line.
Posterior Tibial Slope
The posterior tibial slope was reported by Kim et al. 11 Both the MSC and control groups showed similar posterior tibial slope when compared, with no statistically significant difference between the 2 groups (10.4° ± 2.7° vs 10.3° ± 2.5°).
Discussion
The principal finding of this systematic review and meta-analysis was that intra-articular MSC augmentation for HTO was able to produce small but significant improvements in functional outcomes compared with HTO alone. Results from single observations also suggest that there may be some improvement in pain scores and histologic outcomes.
Statistically significant greater improvement was noted in the MSC group compared with the control group for most of the functional, pain, and histological outcomes that were analyzed. These included the pooled Lysholm score and IKDC score, which were within or close to the MCID, as well as the KOOS, Tegner score, VAS for pain, and arthroscopic and histological grading scale identified in the individual studies. The only clinical outcome that did not show statistically significant improvement in the MSC group compared to the control group was the HSS Knee Rating Scale, but even so, greater improvements were noted in the MSC group compared with the control groups. 22 The radiological outcomes, including the femorotibial angle, weightbearing line, and posterior tibial slope, were similar between the 2 groups, suggesting that correction attained from the HTO itself is similar between the 2 groups, and the additional improvement in the MSC group compared with the control group was due to the MSC augmentation in the MSC group. 11,13
This finding that the pooled functional, pain, and histological outcomes were superior in the MSC group compared with the control group was novel to the current meta-analysis. While 2 previous meta-analyses have been performed on the topic, both meta-analyses concluded that while concomitant procedures could improve the histological and arthroscopic outcomes, there was no significant difference in the outcomes in terms of pain and radiological outcomes. 14,26 Discrepancies were noted when comparing the 2 meta-analyses for other outcomes, including clinical outcomes and MRI. While Lee et al 14 reported no significant difference in clinical outcomes when concomitant procedures were performed, Yao et al 26 performed subgroup analysis and noted that the use of MSCs as opposed to other concomitant procedures could possibly improve the clinical outcomes in general. Neither meta-analyses, however, specifically focused on pooling the outcomes with or without MSC augmentation for HTO.
The discrepancies between the 2 meta-analyses, the discrepancy between the outcomes of the meta-analyses and the individual studies on MSCs augmentation for HTO, and the lack of a specific meta-analysis focusing on the outcomes of HTO with or without intra-articular MSC augmentation prompted the current systematic review and meta-analysis. 11,13,14,22,24,26 Interestingly, the pooling of studies that compared the outcomes of HTO with or without intra-articular MSC augmentation alone then pointed out in a novel manner that while concomitant procedures for HTO in general were not able to improve the functional outcomes and pain compared with HTO alone, augmentation with MSCs was able to improve the functional outcomes and pain compared with HTO alone. The pooled differences between HTO with MSC augmentation and HTO alone were within or close to the established minimal clinically important difference for cartilage procedures, including an MCID of 4.2 for Lysholm score compared with 6.64 identified in the review as well as an MCID of 9.8 for IKDC score compared with 9.21 identified in the review. 16,17 Additionally, MSC augmentation for HTO was also identified to be able to improve the arthroscopic and histological outcomes, with Wakitani et al 22 demonstrating greater improvement in the MSC group compared with HTO alone.
The improvement in outcomes after HTO with MSC augmentation versus HTO alone had been postulated to secondary to better cartilage regeneration with MSC augmentation. This was because the primary pathogenesis of knee osteoarthritis involved both biomechanical and biochemical changes in the cartilage of the knee joint. Therefore, while HTO corrected the weightbearing axis, thus providing the ideal mechanical environment for halting degenerative changes in the articular cartilage, the overall long-term success of HTO remained debatable if cartilage regeneration of medial osteoarthritic cartilage changes could not be achieved. MSC augmentation then allowed for cartilage regeneration as evidenced by prior publications secondary to its ability to differentiate into chondrocytes and its favorable paracrine secretion of bioactive materials.
The current review exhibited several strengths. First, the current review represented the first systematic review and meta-analysis to have compared the outcomes of HTO with and without MSC augmentation. The specific focus of the meta-analysis then allowed for novel findings. Second, focusing on only 1 concomitant procedure compared with all concomitant procedures allowed for pooling of a homogeneous group of studies that compared MSC augmentation with no MSC augmentation. The fact that all studies were homogeneous, all the outcomes identified showed greater improvement in the MSC group compared with the control group, and no publication bias was noted between the studies then further lent confidence to the conclusions drawn from the current systematic review and meta-analysis. Third, the systematic review and meta-analysis separately pooled together the individual outcome scores reported, instead of pooling all the clinical outcome scores together, thereby allowing for each of the outcome scores to be analyzed individually. The influence of MSC augmentation on the outcomes of HTO can also be better interpreted through the unweighted mean differences identified. Finally, the review presented all outcomes that were reported both pre- and postoperatively in all the studies, allowing for the presentation of an unbiased review of the topic.
The current review also faced several limitations. First, the level of evidence of the review is limited by the presence of adequately powered trials in the current literature. Indeed, while the studies included in this systematic review and meta-analysis were randomized controlled trials, prospective comparative studies, and cohort studies, the studies included were of level 2 and 3 evidence, and there is a lack of level 1 randomized controlled trials on the topic. The review then identified that the topic could benefit from further higher-powered trials to further confirm or refute the conclusions drawn.
Second, the inclusion of level 2 and 3 studies could have introduced confounding factors that were not controlled for in the original studies. However, all the studies included compared the baseline characteristics of the patients included in the study and reported that they were similar. Additionally, care was also taken to make sure that all studies included had MSC groups that were comparable with the control groups in all other ways apart from MSC supplementation, including the source, preparation, and delivery of MSCs, augmentation with PRP or hyaluronic acid, type of HTO performed, concomitant procedures performed (microfracture, abrasion arthroplasty, debridement), outcomes studied, and the duration of follow-up, therefore minimizing the risk of confounding bias.
Third, while the studies by Kim et al 11 and Koh et al 13 reported different study protocols, with the patients included in the study by Koh et al having PRP augmentation on top of MSC augmentation while the patients included in the study by Kim et al were reported to only have MSC augmentation, the study teams were similar across both papers; therefore, there could be a possible chance of overlap of patients within the 2 papers included. The decision, however, was made to still include both papers in the review as separate papers because of the different study protocols, patient population, and results reported.
Last, and most important, the limited evidence available precluded rigorous analysis and robust conclusions from being drawn from the available evidence. While some of the outcomes were studied in more than 1 study, many of the outcomes and improvements noted were reported in only individual studies. The homogeneity in results between the studies, despite the different outcome measures used, lent confidence to the conclusions drawn from the current systematic review and meta-analysis.
Conclusion
Intra-articular MSC augmentation for HTO may modestly improve functional outcomes compared with HTO alone. However, adequate data are lacking to make definitive conclusions regarding the effect of MSC augmentation on pain, arthroscopic, and histologic grading.
Footnotes
Final revision submitted October 1, 2020; accepted February 5, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Callahan LF, Ambrose KR, Albright AL, et al. Public health interventions for osteoarthritis---updates on the Osteoarthritis Action Alliance’s efforts to address the 2010 OA Public Health Agenda Recommendations. Clin Exp Rheumatol. 2019;37(5)(suppl 120):31–39. [PubMed] [Google Scholar]
- 2. Di Matteo B, Vandenbulcke F, Vitale ND, et al. Minimally manipulated mesenchymal stem cells for the treatment of knee osteoarthritis: a systematic review of clinical evidence. Stem Cells Int. 2019;2019:1735242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Fleiss JL. The statistical basis of meta-analysis. Stat Methods Med Res. 1993;2(2):121–145. [DOI] [PubMed] [Google Scholar]
- 4. Ha CW, Park YB, Kim SH, Lee HJ. Intra-articular mesenchymal stem cells in osteoarthritis of the knee: a systematic review of clinical outcomes and evidence of cartilage repair. Arthroscopy. 2019;35(1):277–288.e272. [DOI] [PubMed] [Google Scholar]
- 5. Hawker GA. Osteoarthritis is a serious disease. Clin Exp Rheumatol. 2019;37(5)(suppl 120):3-6. [PubMed] [Google Scholar]
- 6. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. [DOI] [PubMed] [Google Scholar]
- 8. Huang SC, Chen YF, Liu XD, Han YH, Li YQ. The efficacy and safety of opening-wedge high tibial osteotomy in treating unicompartmental knee osteoarthritis: protocol for a systematic review and meta-analysis. Medicine (Baltimore). 2019;98(12):e14927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Jevotovsky DS, Alfonso AR, Einhorn TA, Chiu ES. Osteoarthritis and stem cell therapy in humans: a systematic review. Osteoarthritis Cartilage. 2018;26(6):711–729. [DOI] [PubMed] [Google Scholar]
- 10. Kim SH, Djaja YP, Park YB, Park JG, Ko YB, Ha CW. Intra-articular injection of culture-expanded mesenchymal stem cells without adjuvant surgery in knee osteoarthritis: a systematic review and meta-analysis. Am J Sports Med. 2020;48(11):2839–2849. [DOI] [PubMed] [Google Scholar]
- 11. Kim YS, Koh YG. Comparative matched-pair analysis of open-wedge high tibial osteotomy with versus without an injection of adipose-derived mesenchymal stem cells for varus knee osteoarthritis: clinical and second-look arthroscopic results. Am J Sports Med. 2018;46(11):2669-2677. [DOI] [PubMed] [Google Scholar]
- 12. Kloppenburg M, Berenbaum F. Osteoarthritis year in review 2019: epidemiology and therapy. Osteoarthritis Cartilage. 2020;28(3):242–248. [DOI] [PubMed] [Google Scholar]
- 13. Koh YG, Kwon OR, Kim YS, Choi YJ. Comparative outcomes of open-wedge high tibial osteotomy with platelet-rich plasma alone or in combination with mesenchymal stem cell treatment: a prospective study. Arthroscopy. 2014;30(11):1453–1460. [DOI] [PubMed] [Google Scholar]
- 14. Lee OS, Ahn S, Ahn JH, Teo SH, Lee YS. Effectiveness of concurrent procedures during high tibial osteotomy for medial compartment osteoarthritis: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2018;138(2):227–236. [DOI] [PubMed] [Google Scholar]
- 15. Migliorini F, Rath B, Colarossi G, et al. Improved outcomes after mesenchymal stem cells injections for knee osteoarthritis: results at 12-months follow-up: a systematic review of the literature. Arch Orthop Trauma Surg. 2020;140(7):853–868. [DOI] [PubMed] [Google Scholar]
- 16. Ogura T, Ackermann J, Barbieri Mestriner A, Merkely G, Gomoll AH. Minimal clinically important differences and substantial clinical benefit in patient-reported outcome measures after autologous chondrocyte implantation. Cartilage. 2020;11(4):412–422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ogura T, Ackermann J, Mestriner AB, Merkely G, Gomoll AH. The minimal clinically important difference and substantial clinical benefit in the patient-reported outcome measures of patients undergoing osteochondral allograft transplantation in the knee. Cartilage. 2021;12(1):42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pas HI, Winters M, Haisma HJ, Koenis MJ, Tol JL, Moen MH. Stem cell injections in knee osteoarthritis: a systematic review of the literature. Br J Sports Med. 2017;51(15):1125–1133. [DOI] [PubMed] [Google Scholar]
- 19. Rodriguez-Merchan EC. Intra-articular injections of fat-derived mesenchymal stem cells in knee osteoarthritis: are they recommended? Hosp Pract (1995). 2018;46(4):172–174. [DOI] [PubMed] [Google Scholar]
- 20. Roffi A, Nakamura N, Sanchez M, Cucchiarini M, Filardo G. Injectable systems for intra-articular delivery of mesenchymal stromal cells for cartilage treatment: a systematic review of preclinical and clinical evidence. Int J Mol Sci. 2018;19(11):3322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 22. Wakitani S, Imoto K, Yamamoto T, Saito M, Murata N, Yoneda M. Human autologous culture expanded bone marrow mesenchymal cell transplantation for repair of cartilage defects in osteoarthritic knees. Osteoarthritis Cartilage. 2002;10(3):199–206. [DOI] [PubMed] [Google Scholar]
- 23. Whitehead A. Meta-Analysis of Controlled Clinical Trials. John Wiley; 2002. [Google Scholar]
- 24. Wong KL, Lee KB, Tai BC, Law P, Lee EH, Hui JH. Injectable cultured bone marrow-derived mesenchymal stem cells in varus knees with cartilage defects undergoing high tibial osteotomy: a prospective, randomized controlled clinical trial with 2 years’ follow-up. Arthroscopy. 2013;29(12):2020–2028. [DOI] [PubMed] [Google Scholar]
- 25. Xing D, Wang Q, Yang Z, et al. Mesenchymal stem cells injections for knee osteoarthritis: a systematic overview. Rheumatol Int. 2018;38(8):1399–1411. [DOI] [PubMed] [Google Scholar]
- 26. Yao RZ, Liu WQ, Sun LZ, Yu MD, Wang GL. Effectiveness of high tibial osteotomy with or without other procedures for medial compartment osteoarthritis of knee: an update meta-analysis. Published online January 17, 2020. J Knee Surg. doi: 10.1055/s-0039-1700978 [DOI] [PubMed] [Google Scholar]