Abstract
To describe the audio-vestibular disorders related to the newly SARS-CoV-2 infection, including the possible ototoxicity side-effects related to the use of drugs included in the SARS-CoV-2 treatment protocols. A systematic review was performed according to the PRISMA protocol. The Medline and Embase databases were searched from March 1, 2020 to April 9, 2021. Initially the search yielded 400 manuscripts, which were reduced to 15, upon the application of inclusion criteria. Sensorineural hearing loss (SNHL) is the most frequent audio-vestibular symptom described, occurring alone or in association with tinnitus and vertigo. The etiopathogenesis of the inner ear disorders related to COVID-19 infection is still poorly understood. The number of reports of COVID-19 infections associated to audio-vestibular disorders is increasing; even if the quality of the studies available is often insufficient, audio-vestibular disorders should be considered as possible manifestations to be included among the symptoms of this infection.
Keywords: COVID-19, hearing loss, inner ear, ototoxicity, SARS-CoV-2, tinnitus, vertigo
Introduction
Since the spread of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection, several authors have tried to outline a comprehensive clinical description of the disease, including its possible audiological manifestations. 1
The relevance of olfactory and gustatory dysfunction, alone or in association with other symptoms, supports the hypothesis of the SARS-CoV-2 neurotropic and neuroinvasive properties, as observed in other coronaviridae infections.2,3 Also, neurological manifestations have been reported as possible complications of up to 30% of patients affected by COVID-19. 4 Among the nervous structures, the inner ear can be a possible target of the virus, and the induced damage can manifest as sensorineural hearing loss (SNHL), tinnitus and/or vertigo. However, the scientific literature focused on this topic is still in its early stages.
Aim of this systematic review is to describe the audio-vestibular disorders related to the newly SARS-CoV-2 infection, including the possible ototoxicity side-effects related to the use of drugs administrated in the SARS-CoV-2 treatment protocols.
Methods
A systematic review was performed following PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) protocol, of English-language studies focused on the audio-vestibular manifestations (including SNHL, tinnitus and vertigo) of the newly COVID-19 infection via the online database Medline and Embase.
The structure of the search strategy was adapted to suit both databases. The keywords and Mesh terms ‘COVID-19’, ‘Hearing Loss’, ‘Vertigo’, ‘Tinnitus’, ‘inner ear’, ‘hearing impairment’ and ‘ototoxicity’ were used to select the studies of interest.
Case reports and case series were included.
The last literature search was done on 9th April 2021.
The search keywords yielded a total number of 400 papers. These were filtered by the following inclusion/exclusion criteria:
Inclusion:
- Direct temporal correlation between the new-onset of SNHL, vertigo and/or tinnitus and COVID-19 infection.
- Established SARS-CoV-2 infection by Polymerase Chain Reaction (PCR), detection of specific antibodies by serology testing or chest CT scan suggestive of COVID-19 or reported admission to the hospital for COVID-19.
Exclusion:
- Not established SARS-CoV-2 infection.
- Studies containing duplicated data from other published work.
- Studies reporting cases of conductive hearing loss.
- No direct temporal correlation between audio-vestibular symptoms and COVID-19.
- Studies published in languages other than English.
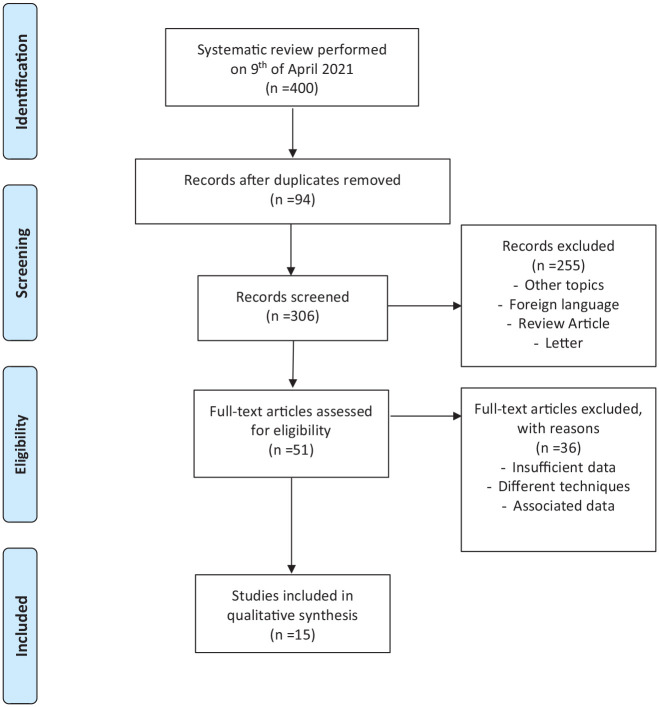
Of the 400 papers initially selected, only 15 passed the selection criteria. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) diagram of the selection process, is illustrated in Figure 1.
Figure 1.
Flow chart of study inclusion process.
Results
The database search identified 15 case reports or case series (level of evidence 4) for a total of 20 patients with established SARS-CoV-2 infection.5–19 All patients reported a new-onset of audio-vestibular symptoms. The mean patient age was 42.4 ± 35.1 years, while the male to female ratio was 7:13.
The documented time-interval, between the SARS-CoV-2 infection and the onset of audio-vestibular symptoms, was maximally a 6-week period. 17
Major findings such as: first author, country of the study, patient’s characteristics, type of audio-vestibular manifestations, investigations, treatments and outcomes are summarized in Table 1.
Table 1.
Summary of the results of the papers included in the review.
| Authors | Country | N# Patient |
Age | Sex | Symptoms | Major findings/Investigations/Treatments/Outcomes | |
|---|---|---|---|---|---|---|---|
| 1 | Sriwijitalai and Wiwanitkit 5 | Thailand | 1 | Old (ND) | F | SNHL | • Coincidental SNHL and COVID-19 infection (first world report). |
| 2 | Malayala et al. 6 | USA (patients from different Countries) |
4 | 23 29 63 71 |
F F F F |
Vertigo Vertigo Vertigo Vertigo + tinnitus |
• Diagnosis: covid induced neuritis (Ny not described). PCR +. MRI negative; treated with prednisone; resolved. • Ny not described. Normal blood tests, Brain CT and MRI normal, IV steroid; long lasting symptoms; PCR +; treated with oral hydroxychloroquine and azithromycin after discovered SARS-CoV-2 positive. • Twitching of left face, skin rash and Herpes labialis, anosmia, dysgeusia, Raynaud phenomenon, spontaneous Ny to the Right. Diagnosis: Post-viral vestibular neuritis. Treated with prednisone. • Loss of Balance and episodes of vertigo lasting up to 20 min; Ny not described. PCR +. |
| 3 | Kilic et al. 7 | Turkey | 1 | 29 | M | SNHL | • Audiogram: confirmed unilateral SNHL. PCR+. Absence of risk factors. Patient treated with oral hydroxychloroquine 200 mg twice daily for 5 days. Outcome: Complete recovery from SNHL. |
| 4 | Degen C. et al. 8 | USA | 1 | 60 | M | Bilateral SNHL + tinnitus | • Audiogram: complete deafness on the right and profound SHL on the left side. PCR+. MRI: inflammatory process with pronounced contrast enhancement in the right cochlea and a partially decreased fluid signal in the basal turn of the right cochlea plus meningeal contrast enhancement in the base of the right temporal lobe. Hypothesis: virus-triggered inflammation of the meninges with subsequent spread to the cochlea. The left ear was treated with three intratympanic steroid injections. Patient treated for COVID-19 pneumonia with azithromycin and furosemide. Urgent Cochlear implant (CI) insertion was performed under local anaesthesia. |
| 5 | Abdel Rhman and Abdel Wahid 9 | Egypt | 1 | 53 | M | SNHL + tinnitus | • Audiogram: severe unilateral SNHL. PCR+. Blood tests: elevated C-reactive protein; full autoimmune screen negative; MRI scan negative. Treatment: Intra-tympanic injection of steroids; Outcome: improvement of hearing level. |
| 6 | Lang et al. 10 | Ireland | 1 | 30 | F | SNHL | • Audiogram: high frequency unilateral SNHL; MRI normal. PCR for SARS-CoV-2 positive. Therapy: oral steroids. Outcome: No improvement reported. |
| 7 | Koumpa and Forde 11 | UK | 1 | 45 | M | SNHL + tinnitus | • Audiogram: high frequency severe unilateral SNHL. Blood test: slightly elevated C-reactive protein; full autoimmune screen negative; ACE, C3 and C4 in normal range. MRI scan negative. Treatment: combined corticosteroid therapy (oral and intratympanic). Outcome: partial improvement. |
| 8 | Lamounier et al. 12 | Brazil | 1 | 67 | F | SNHL + tinnitus | • Patient admitted to hospital for COVID-19 pneumonia for which he was treated with remdesivir, intravenous steroids and plasma exchange. Chronic use of hydroxychloroquine to treat rheumatoid arthritis, without previous audio-vestibular problems. Audiogram: severe unilateral SNHL. MRI: isolated microhaemorrhagic lesions, but changes in the internal auditory canal were not reported. Treatment: combined corticosteroid therapy (oral and intratympanic). |
| 9 | Karimi-Galougahi M. et al. 13 | Iran | 3 | 22 40 23 |
M F F |
SNHL SNHL + tinnitus SNHL + tinnitus + vertigo |
• For all three patients the audiogram confirmed unilateral SNHL; in addition, one complained of associated tinnitus and another of tinnitus and vertigo. PCR+. Absence of previous relevant medical history. No additional details provided. |
| 10 | Takahashi et al. 14 | Japan | 1 | 65 | M | SNHL | • Coincidental unilateral SNHL 7 days before discovering to be COVID-19 positive; patient deteriorated rapidly and died. |
| 11 | Chirakkal et al. 15 | Qatar | 1 | 35 | F | SNHL + tinnitus | • Audiogram: mild low-frequency unilateral SNHL. OAEs absent for low frequencies in left ear suggesting outer hair cell damage. PCR+. MRI normal. |
| 12 | Chern et al. 16 | USA | 1 | 18 | F | Bilateral SNHL + tinnitus + vertigo | • Audiogram: bilateral SNHL. Bilateral aural fullness, vertigo, nausea and vomiting, anosmia and dysgeusia. Serology testing performed 10 weeks after symptoms onset revealed IgG COVID-19 antibodies. MRI: bilateral intra-labyrinthic haemorrhage. Treated with oral and intra-tympanic injections of steroids. |
| 13 | Aasfara et al. 17 | Morocco | 1 | 36 | F | SNHL + tinnitus + vertigo | • Pregnant women at 37 weeks of gestation. Previous SARS-CoV-2 infection 6 weeks before the onset of audio-vestibular symptoms. Blood serology: SARS-CoV-2 IgG positive antibody. Spontaneous III grade Ny -> left; Tinnitus and fullness. Audiogram: severe right SNHL. Videonystagmography: right vestibular areflexia on caloric examination. Diagnosis: right vestibulocochlear neuritis. Other symptoms: Bilateral facial weakness and paraesthesia MRI: negative. Lumbar puncture: raised protein levels. Peripheral muscles EMG: demyelinating pattern of Guillain Barré Syndrome. Therapy: Intravenous immunoglobulins and intravenous steroids. Outcome: recovery of the right facial palsy and the sensorineural hearing loss and vertigo. Spontaneous delivery at 40 weeks of gestation. |
| 14 | Mat et al. 18 | Belgium | 1 | 13 | F | Vertigo | • Right spontaneous grade III Ny. PCR+. vHIT: diagnosis of left superior vestibular neuritis. MRI negative. |
| 15 | Perret et al. 19 | France | 1 | 84 | M | SNHL + tinnitus + vertigo | • Vertigo and unbalance with left peripheral Ny, associated with sudden right SNHL (not further details provided). PCR +. MRI: right cochlea and semicircular canals hyperintense on FLAIR and on diffusion-weighted images, suggestive of acute inflammatory process of the right labyrinthitis. |
SNHL: sensorineural hearing loss; ND: not described; MRI: magnetic resonance imaging; Ny: nystagmus; PCR+: polymerase chain reaction positive for SARS-CoV-2; CT: computed tomography; OAEs: otoacoustic emissions; EMG: electromyography; vHIT: video head impulse test.
COVID-19 and audio-vestibular symptoms
Sensorineural hearing loss
Sensorineural hearing loss (SNHL) was the most frequent audio-vestibular symptom described in 15 out of the 20 patients: it was described as isolated SNHL in five cases, associated to tinnitus in seven cases and to tinnitus/vertigo in three subjects (see Table 1).
The first postulated correlation between SNHL and COVID-19 dates back to April 2020, but the association appeared coincidental, and the patient details were not provided (Sriwijitalai and Wiwanitkit). 5 Since then, various anecdotal cases of unilateral or bilateral SNHL, alone or in association to tinnitus or vertigo, have been described.
In a few reports, hearing loss has been only supposed and not documented, while some authors theorized a direct correlation to COVID-19 based on a temporal association, a plausible pathophysiology and the absence of relevant medical history or other risk factors rather than the viral infection.13,20
Overall, the available studies evidenced that the audiological examination (i.e. audiometric testing) was challenging, due to the sanitation requirements all the equipment and the clinical environment after each evaluation. Pure tone audiometry was performed in 10 subjects with a new onset of SNHL. Two papers (Degen et al., 8 Chern et al. 16 ) report data from a binaural SNHL. In both cases, the cerebral MRI found evidence of inner ear damage, a bilateral intra-labyrinthine haemorrhage and a bilateral cochlear inflammation, respectively. One patient, not responsive to steroid therapy, underwent a cochlear implant under local anaesthesia, due to the presence of cochlear fibrosis evidenced by MRI (Degen et al. 8 ).
Another issue, since the early stages of the pandemic, is the treatment of the audio-vestibular disorders, and in particular the treatment of SNHL. Even if steroids are usually administrated in subjects affected by SNHL of a newly onset, their use in the early stages of viral infections should be considered carefully, because of the risk of causing a delayed viral clearance and a consequent deterioration of the general health status due to the infection. 21 Therefore, aiming the avoidance of adverse systemic effects, the intratympanic injection is the ideal route of administration, due to the minimal systemic but higher perilymphatic absorption. 22
Vertigo
Descriptions of vestibular deficit associated to COVID-19 infection have been documented, but a comprehensive vestibular examination is rarely available. Malayala et al. 6 reported on six cases of vestibular deficit from different parts of the world, but coexistent SARS-CoV-2 infection was confirmed in four over six subjects. Unfortunately, the evidence of nystagmus in these series was described in only two cases, challenging any hypothesis about the correlation of specific vestibular disorder (i.e. neuritis, benign paroxysmal positional vertigo or Ménière disease) and the viral infection.
A complete vestibular evaluation is difficult to achieve in COVID-19 patients, as protective equipment and careful disinfection of all surfaces is required. In addition, the chance of triggering vomiting during the examination increases the risk of contagion. As a result, only one report described a comprehensive vestibular assessment, including a vHIT (video Head Impulse Test) evaluation (Mat et al. 18 ).
A newly onset vertigo should be always investigated carefully, especially when a peripheral vestibular deficit is not certain. Differential diagnosis from acute cerebrovascular events is mandatory; in particular, it is necessary to exclude acute thrombosis of the intracranial arteries (vertebral artery and PICA (posterior inferior cerebellar artery)) as already reported in a patient affected by COVID-19, and manifesting vertigo and nystagmus. 23
Tinnitus
Tinnitus was described as a concomitant symptom in 11 over 20 subjects, while isolated presentations were not reported. The specific features of tinnitus were not reported in all studies; only one evaluated the matching frequency and intensity, revealing the tinnitus perception at 10 dB of 4 kHz; the impact on life quality and definitive resolution were not routinely registered. 15
A survey on 185 patients with positive PCR nasopharyngeal swabs reported that tinnitus started after COVID-19 diagnosis in 23.2% of cases. 24 Emotional factors, anxiety, poor sleep quality experienced during the course of the disease can play a relevant role in developing or enhancing this symptom, which appears to be more bothersome for those quarantined. 25
Ototoxicity of COVID-19 treatments
Patients affected by COVID-19 often receive medication with potential ototoxic effects. 26
The administration of hydroxychloroquine especially is a discussion topic, because of its wide off-label use in the early times of the pandemic. The subset of neural, retinal and audio-vestibular adverse manifestations caused by quinine and derivatives, including hydroxychloroquine, are well known since the 18th century with the name of ‘cinchonism’.27,28 Nowadays the major Health Surveillance Agencies, because of the lack of evidence about potential benefit and the well-known side effects, restricted its prescription as a part of approved clinical trials under close monitoring. 29
Azithromycin, a macrolide antibiotic with known anti-inflammatory properties, was proposed in multiple treatment protocols for COVID-19. In vitro and in vivo ototoxic effects of this class of antibiotics, including azithromycin, have been reported. 30 A recent meta-analysis and literature review underlined that the frequency of SNHL due to exposure to macrolide antibiotics is higher compared to that of other antibiotics or placebo, even at standard oral doses.31,32
The drug combination lopinavir–ritonavir (antiviral protease inhibitor) is listed among current treatments against SARS-CoV-2. Few reports described anecdotal cases of hearing loss associated with their use, postulating possible mitochondrial toxicity as a potential etiologic mechanism. 33
Another antiviral agent, ribavirin, is known to cause severe SNHL if prescribed alongside interferon, even if the data about ototoxic effects of ribavirin alone are scarce. 34
Specific references on the history of exposure to ototoxic drugs were reported in 4 over 20 patients and these cases are included in this review.7,10,14,24 All patients received hydroxychloroquine alone or in association to other established potential ototoxic drugs, such as azithromycin or furosemide; a clear correlation between their symptoms and the adverse effects of these medications was not established. 38
Discussion
The uncontrolled recent growth of literature, among the SARS-CoV2 infection, raised the problem of how to establish a relationship between the virus and the inner ear damage. 35
An accurate anamnesis, including previous audiological events, is crucial to guide the clinician in the identification of the etiopathogenesis. Previous history of noise exposure, head trauma, autoimmune diseases, exposure to ototoxic drugs, Ménière disease, anatomical alterations of the ear and other predisposing factors should be always ruled out before postulating a link to SARS-CoV-2. In addition, Magnetic Resonance Imaging (MRI) is required to exclude retro-cochlear pathology.
The damage of the audio-vestibular system during a SARS-CoV2 infection could be related to a direct impairment of inner ear structures or to a virus-mediated immune response. Blood vessels, lymphatics and nerves and in some cases the meninges (as proposed by Degen et al. 8 ), have been proposed as entry routes for the virus. 8
The hypothesis of a possible direct damage to the cochlear hair cell has been supported by studies reporting a reduced amplitude of transient otoacoustic emissions (TEOAEs) in infected adults and even in newborn patients exposed to SARS-CoV-2 intrauterinely.36,37
Some Authors have advocated a potential inflammatory involvement of inner ear vessels or of the stria vascularis (eventually causing vasculitis or endothelitis), since its highly vulnerability to hypoxic damage. 38 In fact, brain microhaemorrhages have been reported to be another peculiar sign of COVID-19 infection. 39 In effect, bilateral intralabyrinthine haemorrhage has been documented in a case of bilateral SNHL and vertigo in a patient with a history of SARS-CoV-2 and in a patient with unilateral SNHL and diffuse cerebral microhaemorrhages (Lamounier et al. 12 and Chern et al. 16 ).
A cerebral MRI was performed in 10 of the 20 patients with audio-vestibular disorders. The neuroimaging revealed a clear inflammatory process of the inner ear in two of them, in one case bilateral, supporting the hypothesis of a direct cochlear and labyrinth damage (Degen et al. 8 and Perret et al., 19 ).
Other proposed etiopathogenetic mechanisms have been related to (i) the presence of a persistent inflammatory status with the production of proinflammatory cytokines that may hamper the inner ear functions 36 ; and (ii) to the concomitant onset of an autoimmune response, such as granulomatosis with polyangiitis. 40
Drawbacks. This review considered among other data individual reports and case series (level of evidence 4), therefore it is susceptible to information bias, which might represent a limitation of the study.
Furthermore, in some of the reported cases the absence of audiological examination prior to the onset of the acute hearing loss, is another possible drawback since it is not possible to compare pre and post hearing threshold levels. This aspect has been discussed by other Authors41,42,43,44; in some of the reported cases, it is not clear if the symptoms represent the worsening of a pre-existing disease triggered by SARS-CoV-2, or a clinical manifestation entirely related to the virus, or a coincidental event.
Conclusion
Still little is known among the possible inner ear involvement of the newly COVID-19 infection and in particular among the possible pathophysiology of the associated inner ear disorders. At present, there is only a very limited amount of literature focusing on this topic and mainly case reports; however, SNHL, tinnitus and vertigo should be considered as possible manifestations to be included between the symptoms of this infection.
Furthermore, due to the potential ototoxicity related to the use of some medications in the treatment of the COVID-19 infection, it is necessary to strictly monitor the use of these drugs because induced hearing loss, vertigo and/or tinnitus can be irreversible.45,46
Finally, in our opinion, due to several factors such as: (i) the often-precarious conditions of patients affected, and (ii) the highly infectivity and the rapid spread of the virus, Otoacoustic Emissions (OAEs) protocols could provide information about the cochlear function in a simple, fast, non- invasive and feasible way. 47 Since no subject-cooperation is required, OAEs may represent a first line ‘audiological’ tool, for assessing patients affected by COVID-19 and complaining auditory symptoms, directly at home or in COVID-19 wards.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Andrea Ciorba  https://orcid.org/0000-0003-3455-2295
https://orcid.org/0000-0003-3455-2295
References
- 1. Hsia W. Emerging new coronavirus infection in Wuhan, China: situation in early 2020. Case Study Case Rep 2020; 10: 8–9. [Google Scholar]
- 2. Luís ME, Hipólito-Fernandes D, Mota C, et al. A review of neuro-ophthalmological manifestations of human coronavirus infection. Eye Brain 2020; 12: 129–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hu J, Jolkkonen J, Zhao C. Neurotropism of SARS-CoV-2 and its neuropathological alterations: Similarities with other coronaviruses. Neurosci Biobehav Rev 2020; 119: 184–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ahmad I, Rathore FA. Neurological manifestations and complications of COVID-19: a literature review. J Clin Neurosci 2020; 77: 8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sriwijitalai W, Wiwanitkit V. Hearing loss and COVID-19: a note. Am J Otolaryngol 2020; 41: 102473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Malayala SV, Mohan G, Vasireddy D, et al. A case series of vestibular symptoms in positive or suspected COVID-19 patients. Infez Med 2021; 29(1): 117–122. [PubMed] [Google Scholar]
- 7. Kilic O, Kalcioglu MT, Cag Y, et al. Could sudden sensorineural hearing loss be the sole manifestation of COVID-19? An investigation into SARS-COV-2 in the etiology of sudden sensorineural hearing loss. Int J Infect Dis 2020; 97: 208–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Degen C, Lenarz T, Willenborg K. Acute profound sensorineural hearing loss after COVID-19 pneumonia. Mayo Clin Proc 2020; 95: 1801–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Abdel Rhman S, Abdel Wahid A. COVID -19 and sudden sensorineural hearing loss, a case report. Otolaryngol Case Rep 2020; 16: 100198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lang B, Hintze J, Conlon B. Coronavirus disease 2019 and sudden sensorineural hearing loss. J Laryngol Otol. Epub ahead of print 1 October. DOI: 10.1017/S0022215120002145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Koumpa FS, Forde CT, Manjaly JG. Sudden irreversible hearing loss post COVID-19. BMJ Case Rep 2020; 13: e238419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lamounier P, Franco Gonçalves V, Ramos HVL, et al. A 67-year-old woman with sudden hearing loss associated with SARS-CoV-2 infection. Am J Case Rep 2020; 21: e927519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Karimi-Galougahi M, Naeini AS, Raad N, et al. Vertigo and hearing loss during the COVID-19 pandemic - is there an association? Acta Otorhinolaryngol Ital 2020; 40: 463–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Takahashi N, Abe R, Hattori N, et al. Clinical course of a critically ill patient with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). J Artif Organs 2020; 23: 397–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chirakkal P, Al Hail AN, Zada N, et al. COVID-19 and tinnitus. Ear Nose Throat J 2021; 100: 160S–162S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Chern A, Famuyide AO, Moonis G, et al. Bilateral sudden sensorineural hearing loss and intralabyrinthine hemorrhage in a patient with COVID-19. Otol Neurotol 2021; 42: e10–e14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Aasfara J, Hajjij A, Bensouda H, et al. A unique association of bifacial weakness, paresthesia and vestibulocochlear neuritis as post-COVID-19 manifestation in pregnant women: a case report. Pan Afr Med J 2021; 38: 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mat Q, Noël A, Loiselet L, et al. Vestibular neuritis as clinical presentation of COVID-19. Ear Nose Throat J. Epub ahead of print 11 February 2021. DOI: 10.1177/0145561321995021. [DOI] [PubMed] [Google Scholar]
- 19. Perret M, Bernard A, Rahmani A, et al. Acute labyrinthitis revealing COVID-19. Diagnostics (Basel) 2021; 11: 482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Jacob J, Flannery W, Mostert C. Novel ENT triad of anosmia, ageusia and hearing impairment in COVID-19. Intern Med J 2020; 50: 1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Recovery, Randomised Evaluation of COVID-19 Therapy, https://www.recoverytrial.net/results/dexamethasone-results (2020, accessed 23 April 2021)
- 22. Herman P, Vincent C, Parietti Winkler C, et al. Consensus statement. Corticosteroid therapy in ENT in the context of the COVID-19 pandemic. Eur Ann Otorhinolaryngol Head Neck Dis 2020; 137: 315–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sartoretti E, Sartoretti T, Imoberdorf R, et al. Long-segment arterial cerebral vessel thrombosis after mild COVID-19. BMJ Case Rep 2020; 13: e236571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Viola P, Ralli M, Pisani D, et al. Tinnitus and equilibrium disorders in COVID-19 patients: preliminary results. Eur Arch Otorhinolaryngol 2020; 23: 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Beukes EW, Baguley DM, Jacquemin L, et al. Changes in tinnitus experiences during the COVID-19 Pandemic. Front Public Health 2020; 8: 592878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ciorba A, Corazzi V, Skarżyński PH, et al. Don’t forget ototoxicity during the SARS-CoV-2 (Covid-19) pandemic! Int J Immunopathol Pharmacol 2020; 34: 2058738420941754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Bykowski A, Logan TD. Cinchonism. [Updated 2020 Dec 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021. Jan-. Available at: https://www.ncbi.nlm.nih.gov/books/NBK559319/ (accessed 23 April 2021) [Google Scholar]
- 28. Saniasiaya J, Kulasegarah J. Auditory Cinchonism in COVID Era. Ear Nose Throat J 2020; 99: 597–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hydroxychloroquineinthe treatmentof adult patients with COVID-19. Available at: https://www.aifa.gov.it/documents/20142/1267737/Hydroxychloroquine_EN_22.12.2020.pdf/6f0c19ac-48cf-4200-6af4-b3fedbdbe440 (accessed 23 April 2021)
- 30. Pawlowski KS, Si E, Wright CG, et al. Ototoxicity of topical azithromycin solutions in the Guinea pig. Arch Otolaryngol Head Neck Surg 2010; 136: 481–7. [DOI] [PubMed] [Google Scholar]
- 31. Alsowaida YS, Almulhim AS, Oh M, et al. Sensorineural hearing loss with macrolide antibiotics exposure: a meta-analysis of the association. Int J Pharm Pract. Epub ahead of print 1 September 2020. DOI: 10.1111/ijpp.12670. [DOI] [PubMed] [Google Scholar]
- 32. Ikeda AK, Prince AA, Chen JX, et al. Macrolide-associated sensorineural hearing loss: a systematic review. Laryngoscope 2018; 128: 228–236. [DOI] [PubMed] [Google Scholar]
- 33. Williams B. Ototoxicity may be associated with protease inhibitor therapy. Clin Infect Dis 2001; 33: 2100–2. [DOI] [PubMed] [Google Scholar]
- 34. Little C, Cosetti MK. A narrative review of pharmacologic treatments for COVID-19: safety considerations and ototoxicity. Laryngoscope. 2021; DOI: 10.1002/lary.29424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Satar B. Criteria for establishing an association between Covid-19 and hearing loss. Am J Otolaryngol 2020; 41: 102658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Celik T, Simsek A, Koca CF, et al. Evaluation of cochlear functions in infants exposed to SARS-CoV-2 intrauterine. Am J Otolaryngol 2021; 42: 102982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mustafa MWM. Audiological profile of asymptomatic Covid-19 PCR-positive cases. Am J Otolaryngol 2020; 41: 102483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Iba T, Connors JM, Levy JH. The coagulopathy, endotheliopathy, and vasculitis of COVID-19. Inflamm Res 2020; 69: 1181–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Radmanesh A, Derman A, Lui YW, et al. COVID-19-associated Diffuse leukoencephalopathy and microhemorrhages. Radiology 2020; 297: E223–E227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Selvaraj V, Moustafa A, Dapaah-Afriyie K, et al. COVID-19-induced granulomatosis with polyangiitis. BMJ Case Rep 2021; 14: e242142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Almufarrij I, Munro KJ. One year on: an updated systematic review of SARS-CoV-2, COVID-19 and audio-vestibular symptoms. Int J Audiol. Epub ahead of print 22 March 2021. DOI: 10.1080/14992027.2021.1896793. [DOI] [PubMed] [Google Scholar]
- 42. Jafari Z, Kolb BE, Mohajerani MH. Hearing loss, tinnitus, and dizziness in COVID-19: a systematic review and meta-analysis. Can J Neurol Sci. Epub ahead of print 12 April 2021. DOI: 10.1017/cjn.2021.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Maharaj S, Bello Alvarez M, Mungul S, et al. Otologic dysfunction in patients with COVID-19: a systematic review. Laryngoscope Investig Otolaryngol 2020; 5: 1192–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Almufarrij I, Uus K, Munro KJ. Does coronavirus affect the audio-vestibular system? A rapid systematic review. Int J Audiol 2020; 59: 487–491. [DOI] [PubMed] [Google Scholar]
- 45. Konrad-Martin D, Poling GL, Garinis AC, et al. Applying U.S. national guidelines for ototoxicity monitoring in adult patients: perspectives on patient populations, service gaps, barriers and solutions. Int J Audiol 2018; 57: S3–S18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Prayuenyong P, Kasbekar AV, Baguley DM. Clinical implications of chloroquine and hydroxychloroquine ototoxicity for COVID-19 treatment: a mini-review. Front Public Health 2020; 8: 252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ciorba A, Skarżyński PH, Pelucchi S, et al. Ototoxicity prevention during the SARS-CoV-2 (COVID-19) emergency. J Glob Antimicrob Resist 2020; 23: 263–264. [DOI] [PMC free article] [PubMed] [Google Scholar]