Abstract
IgG4 (immunoglobulin G4)-related systemic disease is an autoimmune process affecting multiple organ systems. This inflammatory process can present as but not limited to pancreatitis, cholangitis, or unspecified kidney disease. In this case, our patient developed IgG4-related kidney disease while already on a prolonged steroid course for IgG4-related pancreatitis. The patient ultimately had renal recovery after starting a higher dose of prednisone, but also developed steroid-related complications. This case further highlights the relationship between IgG4 diseases now termed IgG4-related systemic disease. This case brings to light the need for further investigative research into ideal steroid dosing, as well as steroid-sparing agents for IgG4-related systemic disease.
Keywords: nephrology, gastroenterology, IgG4, IgG4-related systemic disease
Introduction
IgG4 (immunoglobulin G4)-related systemic disease is a recently discovered autoimmune disease that affects several organ systems. 1 While the disease typically responds well to steroids, the ideal dose remains unclear.2-5 Given its relatively recent discovery in 2003, the literature on IgG4-related systemic disease is limited. 6 While it frequently responds to steroids, the appropriate regimens and doses have yet to be determined. 5 The following report describes a novel case of IgG4-related kidney disease that developed while the patient was already on steroids for autoimmune IgG4 pancreatitis.
Case Presentation
A 57-year-old male with a medical history significant for well-controlled diabetes mellitus type 2 without retinopathy, autoimmune IgG4 pancreatitis, and benign prostate hyperplasia presented to nephrology clinic for worsening creatinine.
Two years prior to the kidney biopsy, the patient was admitted for acute pancreatitis (AP). Investigation for common causes of AP was negative. IgG4 levels were elevated more than 1000, with peak level of 1270. Pancreatic biopsy was performed in October 2018, and immunostaining revealed increased IgG4 plasma cells.
Family history was significant for unspecified autoimmune diseases, end-stage renal disease, and unspecified kidney disease.
The patient’s last episode of AP was in 2018. At that point, he was initiated on a prolonged steroid course of prednisone 40 mg daily starting in August 2018, which was gradually tapered off by September 2020.
While creatinine was normal (0.8) in May 2019 (Figure 1), it was noted to progressively worsen over the course of steroids, reaching 2.08 by November 2020 (Figure 2). Urinalysis revealed no red blood cells, blood, white blood cells, eosinophils, or protein. Urine protein/creatinine ratio initially was 0.1 mg/g in May 2019, and remained minimal at 0.3 mg/g by November 2020. No nephrotoxic medications were given during this rise of creatinine besides steroids, and the patient denied any use of nonsteroidal anti-inflammatory drugs for his pancreatitis pain.
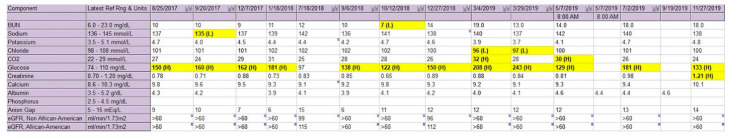
Figure 1.
Trending baseline creatinine from August 25, 2017, until November 27, 2019.
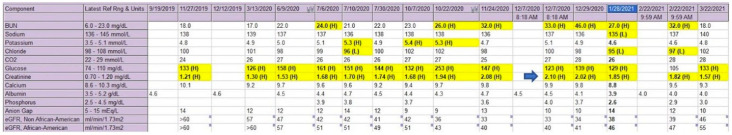
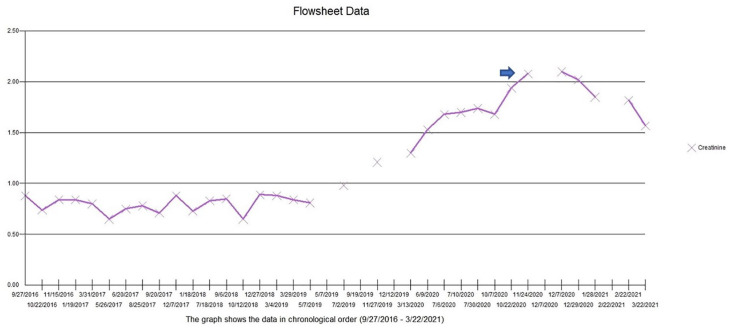
Figure 2.
The blue arrow denotes creatinine when prednisone 1 mg/kg therapy was initiated on December 7, 2020.
Of note, the patient underwent a right submandibular mass biopsy 4 years prior to kidney biopsy, which demonstrated florid follicular lymphoid hyperplasia, lymphoplasmacytic infiltration, and stromal fibrosis. The immunostaining ratio of IgG versus IgG4 was only 1:1, which, per the pathology report, did not support IgG4 disease.
In the setting of progressively worsening creatinine, kidney biopsy was planned for November 2020 with the expectation that it would differentiate steroid-induced acute interstitial nephritis from IgG4-related kidney disease. Kidney biopsy demonstrated chronic active tubulointerstitial nephritis on light microscopy, and immunofluorescence staining confirmed positive IgG4 staining (Figures 3-6).
Figure 3.
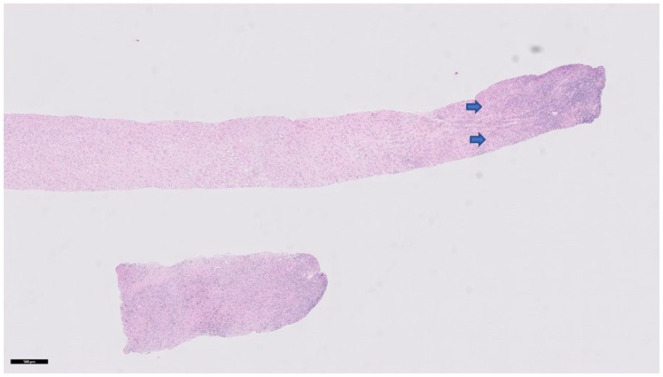
Light microscopy of H&E (hematoxylin and eosin)-stained renal parenchymal biopsy at 40× magnification demonstrating a well-demarcated border between a region of dense inflammation (right) and uninvolved parenchyma (left). This demarcation is a typical finding in IgG4-related kidney disease. Arrow points to border.
Figure 4.
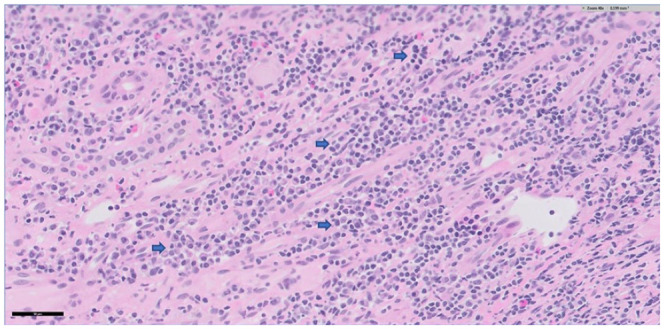
Light microscopy of H&E (hematoxylin and eosin)-stained renal parenchymal biopsy at 100× magnification demonstrating (blue arrows) dense mononuclear tubulointerstitial infiltration. This finding is known to be seen in IgG4-related kidney disease.
Figure 5.
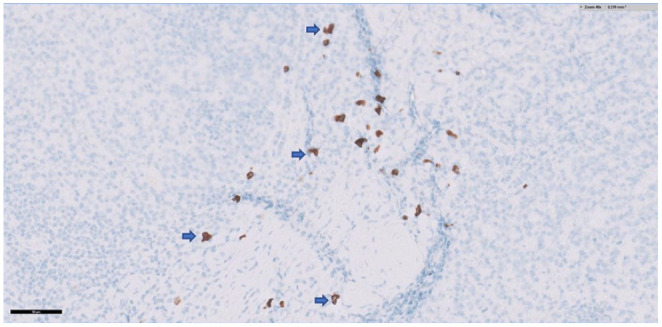
Renal parenchymal biopsy at 100× magnification demonstrating positive IgG4 immunohistochemical staining (blue arrows), confirming IgG4-related disease.
Figure 6.
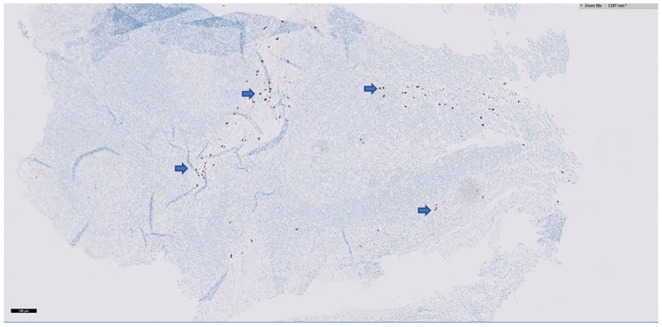
Renal parenchymal biopsy at 40× magnification demonstrating positive IgG4 immunohistochemical staining (blue arrows), confirming IgG4-related disease.
Because the kidney biopsy confirmed the presence of IgG4-related kidney disease that developed during steroid treatment, he was restarted on steroids at a higher dose than previously prescribed. Prednisone 1 mg/kg was initiated in December 2020 (Figure 7), with immediate improvement in renal function as evidenced by downtrending creatinine following initiation of high-dose steroids to 1.85 mg/kg even just a few weeks later. He continues to have renal recovery as of March 2021.
Figure 7.
Additional graph depicting the rise in creatinine on July 2, 2019, as well as when steroids were initiated on December 7, 2020 (blue arrow).
Discussion
IgG4-related systemic disease has only recently been described in the literature, first mentioned in 2003. 7 Patients have been observed to demonstrate a constellation of manifestations including autoimmune pancreatitis, kidney disease, and sclerosing cholangitis. 6 The mechanism behind the development of IgG4-related systemic disease remains unclear: whether elevated IgG4 levels are the cause as opposed to simply a result of the disease has yet to be definitively determined, 8 although immune complex formation has been proposed as a potential mechanism, perhaps by complement fixation via the lectin pathway or via the classical pathway. 5
The most common manifestation of IgG4-related kidney disease is tubulointerstitial disease, as seen in our patient. Membranous glomerulonephropathy is less frequently seen and was considered less likely in our patient even prior to biopsy given the low urine protein-creatinine ratio.8,9 Typical biopsy findings in IgG4-related tubulointerstitial disease include dense infiltration of IgG4-positive mononuclear cells, well-demarcated borders between involved and uninvolved regions, and storiform fibrosis,8,9 all of which were seen in our patient.
Concomitant pancreatitis and IgG4-related kidney disease has been reported: a retrospective study from Sweden evaluating 71 patients with autoimmune pancreatitis type 1 found that 27.4% of those patients also had concomitant IgG4-related kidney disease with a male predominance. 10
While there are currently no randomized controlled trials investigating the management and treatment of IgG4-related systemic disease, review of the current literature supports the use of glucocorticoids.2-5 Data suggest a favorable response to steroids, as demonstrated in our patient.2-5 Unlike in other kidney diseases, the presence of extensive fibrosis on biopsy surprisingly does not portend resistance to steroids. 11 While several potential contenders to steroid treatment have been identified (including rituximab, mycophenolate mofetil, azathioprine, and bortezomib), evidence on the utility of these agents is limited to preliminary data based on a few case reports.2-5 Identification of a steroid-sparing agent is crucial given the detrimental effects that high-dose steroids can have on the kidneys. In our patient, high-dose steroids raised his A1C from 7.2 to 11.5 within 2 months, unfortunately increasing his risk for diabetic-related kidney disease. Patients like ours would benefit tremendously from steroid-sparing agents, highlighting the need for additional investigative research into treatment strategies.
Conclusion
Patients presenting with one form of IgG4 disease may be predisposed to developing other IgG4 disease manifestations. Increased awareness of this diagnosis will allow clinicians to screen patients appropriately and anticipate possible complications. Given the risks and complications associated with steroid treatment, particularly at high doses, further research into steroid-sparing agents is vital to provide clinicians with the tools necessary to optimize the medical management of this disease process.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent: Verbal informed consent was obtained from the patient for their anonymized information to be published in this article.
ORCID iDs: Jonathan Vincent M. Reyes  https://orcid.org/0000-0002-2572-6436
https://orcid.org/0000-0002-2572-6436
Dawn Maldonado  https://orcid.org/0000-0003-2136-8720
https://orcid.org/0000-0003-2136-8720
References
- 1. Bledsoe JR, Della-Torre E, Rovati L, Deshpande V. IgG4-related disease: review of the histopathologic features, differential diagnosis, and therapeutic approach. APMIS. 2018;126:459-476. doi: 10.1111/apm.12845 [DOI] [PubMed] [Google Scholar]
- 2. Khosroshahi A, Bloch DB, Despande V, Stone JH. Rituximab therapy leads to rapid decline of serum IgG4 levels and prompt clinical improvement in IgG4-related systemic disease. Arthritis Rheum. 2010;62:1755-1762. [DOI] [PubMed] [Google Scholar]
- 3. Khosroshahi A, Carruthers MN, Deshpande V, Unizomy S, Bloch DB, Stone JH. Rituximab for the treatment of IgG4-related disease: lessons from 10 consecutive patients. Medicine (Baltimore). 2012;91:57-66. doi: 10.1097/MD.0b013e3182431ef6 [DOI] [PubMed] [Google Scholar]
- 4. Khan ML, Colby TV, Viggiano RW, Fonseca R. Treatment with bortezomib of a patient having hyper IgG4 disease. Clin Lymphoma Myeloma Leuk. 2010;10:217-219. doi: 10.3816/CLML.2010.n.034 [DOI] [PubMed] [Google Scholar]
- 5. Fernández-Codina A, Pinilla B, Pinal-Fernández I, et al. ; Spanish Registry of IgG4 Related Disease (REERIGG4) Investigators; Autoimmune Diseases Group (GEAS); Spanish Internal Medicine Society (SEMI). Treatment and outcomes in patients with IgG4-related disease using the IgG4 responder index. Joint Bone Spine. 2018;85:721-726. doi: 10.1016/j.jbspin.2018.01.014 [DOI] [PubMed] [Google Scholar]
- 6. Brar JSS, Gupta S, Mohideen SMH, Liauw L, Lath N. The pancreatic and extrapancreatic manifestations of IgG4-related disease. Diagn Interv Radiol. 2018;24:83-88. doi: 10.5152/dir.2018.17319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maritati F, Peyronel F, Vaglio A. IgG4-related disease: a clinical perspective. Rheumatology (Oxford). 2020;59(suppl 3): iii123-iii131. doi: 10.1093/rheumatology/kez667 [DOI] [PubMed] [Google Scholar]
- 8. Raissian Y, Nasr SH, Larsen CP, et al. Diagnosis of IgG4-related tubulointerstitial nephritis. J Am Soc Nephrol. 2011;22:1343-1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kamisawa T, Zen Y, Pillai S, Stone JH. IgG4-related disease. Lancet. 2015;385:1460-1471. [DOI] [PubMed] [Google Scholar]
- 10. Vujasinovic M, Mucelli RP, Valente R, Verbeke CS, Haas SL, Lohr JM. Kidney involvement in patients with type 1 autoimmune pancreatitis. J Clin Med. 2019;8:258. doi: 10.3390/jcm8020258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Khosroshahi A, Stone JH. Treatment approaches to IgG4-related systemic disease. Curr Opin Rheumatol. 2011;23:67-71. [DOI] [PubMed] [Google Scholar]