Abstract
Background:
To introduce Lean approach principles in the management of patients undergoing intravitreal injections (IVIs) for wet age-related macular degeneration.
Methods:
Retrospective single-centre cohort study. Services location, IVIs scheduling, utilization of staff, data recording methods, ophthalmic examination and surgical procedures were analysed; a new Intravitreal Injection Centre (IVIC) was developed according to Lean principles. Mean number of daily IVIs performed, mean time between registration and discharge, mean turnover time in between patients, percentages of performed IVIs on the monthly scheduled IVIs and of patients rating their experience ⩾8/10 via standardized feedback questionnaires were retrospectively analysed.
Results:
The mean IVIs number per day increased from 20 ± 4.08 to 50 ± 7.07, and the mean time between registration and discharge of a patient decreased from 240 ± 14.14 to 60 ± 8.16 min (p = 0.00057 and p < 0.00001, respectively). Mean turnover time in between patients decreased from 10 ± 1.41 to 8 ± 2 min (p = 0.055). The percentage of monthly IVIs performed on the total of scheduled IVIs increased from 60% to 100%, and the percentage of satisfied patients who rated IVIC ⩾8/10 increased from 45% to 95% (p = 0.0177 and p < 0.00105, respectively).
Conclusion:
The IVIC improved the quality, efficiency, speed of the overall procedures and clinical capacity of the IVI service through a fast one-way route for patients, limiting time wasted and total distance travelled. This model facilitates the creation of a one-stop clinic through the just-in-time management principle and may be relevant to other ophthalmology services.
Keywords: age-related macular degeneration, anti-VEGF, intravitreal injection, Intravitreal Injection Centre, Lean methodology, patient care management
Introduction
Lean methodology, first introduced by Toyota to improve productivity,1,2 is a way of optimizing people, resources, effort and energy of an organization towards creating value for the customer. It is based on two guiding tenets, continuous improvement and respect for people and recently it has been applied in healthcare 3 and even in Ophthalmology.4,5 Lean approach involves creating more value for customers with fewer resources, minimizing waste. This goal is reached by applying Lean principles: identify the value, map the value stream, create the flow, establish a pull-based system and seek perfection. Various conceptual tools are available to support Lean organization, such as wastes identification (the 7 wastes of Ohno), materials mapping and information flow (Value Stream Mapping, VSM), and the analysis of routes of people inside a plant (Spaghetti Chart).1,6,7
Lean methodology has been previously utilized to design a new setting dedicated to the management of patients undergoing intravitreal injections (IVIs). 5 The intravitreal route has become an efficient approach for the delivery of anti-vascular endothelial growth factor (anti-VEGF) molecules at therapeutic levels in the vitreous cavity in order to limit systemic side effects.8,9 Monthly IVIs during the loading phase are necessary to obtain a functional result. Due to longer average life expectancy and improvements in diagnostic capabilities, a worldwide increase in incidence and prevalence of wet-age-related macular degeneration (w-AMD) has occurred, along with an increase in the demand for anti-VEGF injections. 10 Hospitals have often been unprepared to manage the increased demand, resulting in long waiting lists, high time consumption for each access, logistic difficulties in accommodating the average elderly patients and their caregivers. Consequences are undertreatments (due to inadequate capacity of the system and poor patients’ compliance) and lower visual outcomes compared with pre-existing clinical trials. 5
We introduced the Lean approach in our clinical practice to improve the management of patients undergoing IVIs for w-AMD at the Ophthalmology Department of Ospedali Riuniti Area Vesuviana. The aim of this study is to propose an innovative model to manage the IVI Service based on Lean methodology during the COVID-19 pandemic, in order to improve the quality of care in w-AMD patients.
Methods
As-was (previous): flow and setting
The study was carried out in agreement with the tenets of the Declaration of Helsinki. The study has been evaluated by the Institutional Review Boards of Ospedali Riuniti Area Vesuviana and deemed not to require ethics approval. Over 1500 patients with w-AMD are yearly undergoing IVIs at the Ophthalmology Department of Ospedali Riuniti Area Vesuviana; IVIs demand from the local population is growing. The limited availability of operating theatres (OTs) and of nursing staff/clerks to manage the access and registration procedures at the Medical Retina Unit (MRU) reduced the capacity of the Department. Patients had been divided into two different pathways: new patients and follow-up patients already under IVIs with pre-existing medical records. New patients were scheduled for a complete ophthalmologic examination and retinal imaging session. Once registered, the patients accessed the MRU to perform eye examination and were consented for IVI after a detailed description of the procedure by a Consultant Ophthalmologist assisted by an Ophthalmic-trained nurse. Routine blood tests, cardiologic (electrocardiogram) and anaesthesiologic pre-assessment for risk stratification were performed at a different Hospital floor. This phase was reported to be particularly discomfortable and distressing for elderly visually impaired patients, who needed to queue together with more urgent patients from the general A&E, and time-consuming for Hospital staff involved, as Consultant Anaesthetists were often busy at the Intensive Treatment Unit with critically unwell patients. Finally, if no further pre-operative tests were required, patients would return to MRU where a date for their IVI was given. Follow-up patients were scheduled by the Ophthalmic Lead nurse for their next IVI date within the established time frames. On the IVI date, an Ophthalmologist assessed the suitability of the eye to receive IVI and the patients’ general conditions. If suitable, patients were divided into groups of three to be accompanied to the pre-OT room, where they were prepared and dressed to receive their IVI. The lack of suitable spaces caused inconvenience and delays in the procedures. Once the IVI was completed, a brief 5-min observation was held at the pre-OT room, medical records were updated with all procedures performed for each patient. Finally, medical records were returned to the ward, where patients were discharged. All data were recorded on medical records that followed patients along their Hospital journey. An anonymous five-question patients’ feedback questionnaire was filled out at each discharge as an indicator of the patient’s perceived outcome (Table 1).
Table 1.
Anonymous five-question patients’ feedback questionnaire filled out at each discharge as indicator of the patient’s perceived outcome.
| Patients’ anonymous feedback questionnaire | |||
|---|---|---|---|
| As-was (mean ± SD) | IVIC (mean ± SD) | p | |
| Reply rate (%) | 55% | 92% | |
| 1. Invitation letter | 7.27 ± 2.52 (1–10) | 9.11 ± 0.42 (1–10) | 0.00006 |
| 2. Waiting time | 5.89 ± 1.97 (1–10) | 8.05 ± 1.23 (1–10) | <0.00001 |
| 3. Procedure | 7.21 ± 1.93 (1–10) | 8.89 ± 0.56 (1–10) | 0.00001 |
| 4. Post-operative instructions | 6.57 ± 0.79 (1–10) | 9.06 ± 0.45 (1–10) | <0.00001 |
| 5. Discharge | 5.47 ± 1.97 (1–10) | 8.69 ± 0.84 (1–10) | <0.00001 |
| Overall grade | 6.48 ± 0.71 (1–10) | 8.76 ± 0.38 (1–10) | <0.00001 |
| Satisfied patients who rated their experience ⩾8/10 (%) | 45% | 95% | 0.00105 (chi-square test) |
IVIC, Intravitreal Injection Centre; SD, standard deviation.
Data are given as mean ± standard deviation (SD) and range (1–10) in patients who received intravitreal injections at the previous Medical Retina Unit and at the Intravitreal Injection Centre (IVIC). Patient satisfaction was recorded by five-question questionnaire having each variable graded from 1 to 10. One-tailed Student’s t-test was used to compare the statistically significant differences in continuous variables, whereas chi-square test was used to compare statistically significant differences in categorical variables among all subgroups, p < 0.05 was considered statistically significant.
IVIs were performed at the available elective OT twice a week at the end of elective cataract, glaucoma or vitreoretinal surgery. An IVI session would typically include 15 patients in average and would start at 11:00 a.m. However, starting time was highly variable depending on completion of previous elective cases. The average time spent in the Hospital by each patient was highly variable depending on prompt availability of theatre nursing staff, who were not exclusively dedicated to IVIs.
Lean approach
The daily difficulties and the scarce resources available pushed us to introduce the Lean approach in our clinical practice of IVIs for w-AMD patients. The Lean is a management approach created for the manufacturing industry and then also applied in healthcare sector worldwide, 3 including Italy.5,11 The goal is to improve the quality of healthcare offered by minimizing wastes. 12 As a result, any waste (transportation, inventory, motion, waiting, over-production, defects and skills) at the Eye Department of ‘Ospedali Riuniti Area Vesuviana’ (Naples, Italy) is identified and minimized. Some of the key tools of the Lean approach are also introduced, as follows:
The VSM to define the process (measure it and identify any improvement in the use of resources and in the organization of the flow of patients and information);
The Spaghetti Charts to map the physical flows of patients and materials in the Eye Clinic.
A new IVI Centre was created (IVIC) with the aim of achieving a fast and one-way route, limiting any loss of time and space, and improving the management of the centre’s capacity.
As-is (new): flow and setting
The IVIC was created in a large centralized Outpatient area of the ‘Ospedali Riuniti Area Vesuviana’ with a one-way path dedicated to the management of IVIs. The new centre is located on the ground floor with dedicated access, easy access ramp and ambulance access. The complete elimination of architectural barriers (stairs/corridors/waiting rooms/lifts) facilitates access to IVIC also for disabled patients on wheelchairs or sight-impaired.
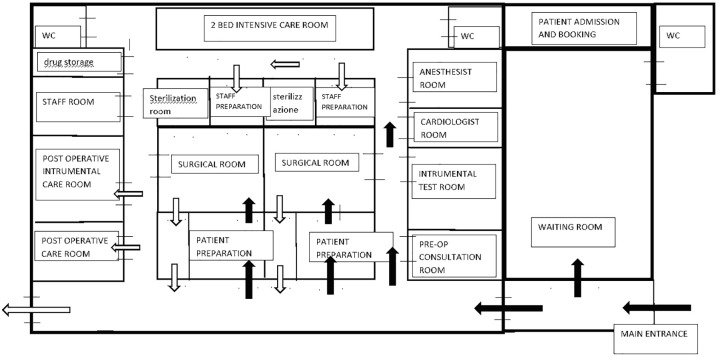
The IVIC runs Monday to Friday from 8:00 to 14:00, performing an average of 50 IVIs on 50 different patients per session, with an option to extend the treatment also in the afternoon. Upon arrival, the patient will be registered at the Reception of the IVIC. Administrative registration will be facilitated by the IT platform in communication with the general practitioner (GP) in charge of the patient. All demographic data will be quickly verified, since they have been previously transferred to IVIC Reception by the GP’s IT software. The receptionist facilitates a prompt access to the IVIC also through the use of WhatsApp© technology reminder text messages. A maximum of three patients are scheduled during each 15-min slot. After registration, patients start the unidirectional path attending a series of dedicated rooms in sequence: clinical examination room, Retinal Imaging room, phlebotomist room, Cardiologist and Anaesthetist assessment room, OT and discharge room (DR) (Figure 1). The OT is equipped with video-monitors that support the surgeon displaying all next patient’s clinical data and video recording the entire procedure. Three additional separate small service rooms are in communication with the OT: the scrubbing room, a room with computerized controlled drugs cabinet and a drugs-storage refrigerator, and a room used for collection of used contaminated medical equipment. The planning involves a one-way flow of sterile supplies into the OT, with dirty/contaminated materials and waste exiting the OT through a separate exit. Air conditioning and ventilation systems with laminar flows are regularly monitored by an electronic system. IVIC staff is trained and dedicated exclusively to IVIs and consist of three orthoptists who carry out the clinical and instrumental pre-IVI evaluation of patients; an auxiliary nurse who dresses patients with surgical disposable scrubs; a scrub nurse and a Consultant Ophthalmologist who performs IVIs, and two extra scrub nurses assisting in the OT. A dedicated Consultant Anaesthetist monitors the OT flow from the monitor in his room and is ready to intervene if needed, and in the meanwhile carries out his outpatient activities pre-assessing new patients. Each patient is guided by an orthoptist from reception to the OT under the supervision of the Consultant Ophthalmologist, who can also book further diagnostic pre-IVI tests through the dedicated IT software. Best-corrected visual acuity (BCVA) is measured using ETDRS charts and autorefractometry. Each patient undergoes bilateral macular optical coherence tomography (OCT) and if necessary OCT angiography (OCT-A). Clinical examination of the anterior segment is performed in order to identify any risk factors (RFs) before IVI. In case of RFs for post-IVI exogenous endophthalmitis such as conjunctivitis, blepharitis or dacryocystitis, the IVI is rescheduled on a different date and the patient is booked onto a clinic appointment with topical treatment. A dilated fundus examination is always performed to evaluate the peripheral retina status and detect possible optic media opacification (cataract, posterior capsular opacification, vitreous haemorrhage). At the end of the pre-IVI clinical examination, patients wear disposable surgical scrubs and mask, disposable theatre cap and shoe covers, undergo the IVI in the OT as per protocol, and enter the DR, where their next follow-up visits are scheduled.
Figure 1.
Plan of the new Intravitreal Injection Centre layout.
Patients’ carers and family members can wait in a smart comfortable environment with WIFI access, and an electronic wrist-band is provided to patients, so that they can be located at the IVIC by their carers at any time.
At the discharge, an informative confidential email about examinations and procedures performed, visual prognosis, and about additional patient’s needs is sent out to patient’s GP. Personalized electronic medical records (EMRs) with demographics, clinical history, clinical and retinal imaging exams, follow-up visits and scheduled procedures facilitate the patients’ management and implement clinical governance. All EMR data are collected in a personalized patient’s electronic folder, in order to promptly retrieve EMR when required, and in an electronic database, which allows data analysis and can be accessed by all Consultants Specialists involved and by patient’s GP. At the end of the IVI, the IVIC electronic register and the paper OT register are also updated. Entry and exit time from IVIC are recorded and compared with the scheduled time for IVI for each patient over 1-month period, in order to estimate the waiting time and the procedure time at the IVIC.
Follow-up visits are documented in the patients’ electronic folders, which guarantee compliance with the therapeutic plan, personalization or postponement of the following visit in case of unforeseen events. Safety is implemented by the combination of all procedures performed to the patient with a quick response (QR) code for each phase of the process, drug, tests, reports, prescriptions and discharge. An anonymous five-question patients’ feedback questionnaire is filled out at each discharge as an indicator of the patient’s perceived outcome (Table 1).
Statistical analysis
Data were analysed using Microsoft Excel 1997-2003. Descriptive statistics were calculated for all variables of interest. Mean and standard deviation (SD) values were calculated for continuous variables, while percentages were calculated for categorical variables. One-tailed Student’s t-test was used to compare the statistically significant differences in continuous variables, whereas chi-square test was used to compare statistically significant differences in categorical variables among all subgroups, p < 0.05 was considered statistically significant. In order to evaluate effectiveness and efficiency of the IVIC, the following outcome measures were considered:
Mean time between registration and discharge.
Mean turnover time in between patients at the OT.
Percentage of satisfied patients who rated their experience ⩾8/10 via standardized feedback anonymous questionnaires.
Mean number of patients treated in a 6-h shift.
Percentage of performed IVIs on the monthly scheduled IVIs.
Results
The differences between MRU and IVIC are summarized in Tables 1 and 2. The total route measured 315 m in the as-was layout compared with 72 m in the new layout (77% reduction), the difference was statistically significant (p < 0.00001, one-tailed Student’s t-test). In the previous setting, patients used stairs or elevators twice, while in the new IVIC patients do not use stairs or elevators as all rooms are on the same floor.
Table 2.
Comparison between the previous Medical Retina Unit and the new Intravitreal Injection Centre setting.
| Outcome measure | Medical Retina Unit | Intravitreal Injection Centre | Statistic test and p value |
|---|---|---|---|
| Total distance of flow (m) | 315 m | 72 m | p < 0.00001 (one-tailed Student’s t-test) |
| Elevator or stairs (times) | 2 | 0 | |
| Sessions days per week | 2 | 5 | |
| IVIs slots per session | 15 ± 2 | 72 ± 2.94 | p < 0.00001 (one-tailed Student’s t-test) |
| Mean time ± standard deviation (SD) between registration and discharge | 240 ± 14.14 min | 60 ± 8.16 min | p < 0.00001 (one-tailed Student’s t-test) |
| Mean number of patients treated in a 6-h shift ± SD | 20 ± 4.08 | 50 ± 7.07 | p = 0.00057 (one-tailed Student’s t-test) |
| Mean turnover time ± SD in between patients at the OT | 10 ± 1.41 min | 8 ± 2 min | p = 0.055 (one-tailed Student’s t-test) |
| Booking options | Booking through Sole Booking Centre | Direct booking from GP | |
| Percentage of performed IVIs on the monthly scheduled IVIs | 60% | 100% | p = 0.0177 (chi-square test) |
| Number of critical incidents or near-misses reported | 1 | 0 | |
| Percentage of satisfied patients rating IVIC ⩾8/10 points | 45% | 95% | p = 0.00105 (chi-square test) |
| Examination | BCVA anterior segment and dilated fundoscopy examination | BCVA anterior segment and dilated fundoscopy examination, macular OCT and OCT-A, tonometry | |
| Medical records | Paper | Paper + electronic medical records stored in personalized patients’ folders |
BCVA, best-corrected visual acuity; GP, general practitioner; IVIC, Intravitreal Injection Centre; OCT, optical coherence tomography; OCT-A, OCT angiography; OT, operating theatres; SD, standard deviation.
The number of weekly IVIs sessions increased from 2 to 5 (increase by 150%), the mean number of slots available per session increased from 15 ± 2 to 72 ± 2.94 and the difference was statistically significant (p < 0.00001, one-tailed Student’s t-test).
The mean IVI number per daily operating list increased from 20 ± 4.08 to 50 ± 7.07, the mean time between registration and discharge of a patient decreased from 240 ± 14.14 to 60 ± 8.16 min and both differences were statistically significant (p = 0.00057 and p < 0.00001, respectively, one-tailed Student’s t-test). The mean turnover time in between patients at the OT decreased from 10 ± 1.41 to 8 ± 2 min, and the difference was not statistically significant (p = 0.055, one-tailed Student’s t-test).
The percentage of monthly IVIs performed on the total of scheduled IVIs increased from 60% to 100%, the percentage of satisfied patients who rated their overall experience at the IVIC ⩾8/10 points raised from 45% to 95% (Table 1) and both differences were statistically significant (p = 0.0177 and p < 0.00105 respectively, chi-square test).
The pre-IVI examination shows a substantial change: in the as-was layout, BCVAs measurement, anterior segment and dilated fundoscopy examination were performed. In the as-is layout, in addition to the previous exams, macular OCT, OCT-A and tonometry are performed at each visit.
According to our Hospital’s policies, the paper medical record remains mandatory, at the IVIC in addition to it, an EMR is also completed and used to collect all data (demographics and clinical data) in an electronic database.
Discussion
The management of w-AMD patients is a significant financial and social commitment for the Italian National Health System. W-AMD can present at the age of 50 onwards, and its incidence increases with increasing age. About 2% of the Italian population is affected, that is, more than 1 million people, with an incidence of about 63,000 new cases of AMD every year. 13 The IVI of anti-VEGF drugs is an effective treatment, especially for w-AMD and diabetic macular oedema (DMO), two major causes of blindness globally. 8 Worldwide healthcare services fail to provide the appropriate rate of IVIs because of two main reasons. First, inadequate clinical capacity limits the patient’s access: medical retinal services and OTs are overcrowded, waiting lists for follow-up appointments or IVIs are long, and times and distances from hospital admission to discharge are excessive. Second, various factors influence patient compliance, 14 among these, clinic and operating conditions, mobility issues or lack of caregivers. Moreover, the low letter gain due to under-treatment generates, on the patients’ perspective, doubts as to the benefit of the treatment, to which they therefore tend not to adhere adequately. The aims of healthcare in elderly patients with multiple chronic comorbidities are to improve their functional status, minimizing symptoms, preventing disability and improving quality of life. For this purpose, we reshaped care pathways and propose a new model to manage the IVIs treatment, based on Lean methodology. This management approach has already been tested in cataract surgery, 15 laser posterior capsulotomy treatment protocols 16 and in IVIs for w-AMD, DMO and retinal vein occlusion. 5 The main goals of our IVIC are to ensure adequate level of healthcare to the changing needs of patients with sustainable costs for the National Health System, to create Smart intelligent environments to favour safety and personalization of healthcare pathways (particularly when the treatments are aimed to fragile not self-sufficient patients), and to promote close collaboration of all healthcare professionals involved with a view on e-Health software that guarantee a continuity of clinical care until the patient is discharged. A fundamental prerequisite is the training and redefining nursing staff technical skills in order to enhance their competences.
Our study shows that there is a significant increase of the mean number of slots for IVIs, of patients treated and in the percentage of IVIs performed monthly, as reported in previous studies.5,16 The time spent by each patient in Hospital for IVI has been significantly reduced with the new current settings (p = 0.00057). Three appointments are scheduled every 15 min, as there are only three main stops (admission, BCVA examination, macular OCT or OCT-A). Crowding in the waiting room is prevented by a continuous patient turnover. We consider this result particularly remarkable now during COVID-19 pandemic, where Ophthalmologists are at high risk due to their proximity and short working distance at the time of slit-lamp examination, 17 and when contact time between healthcare professionals and patients’ needs to be reduced. 18 On average, around 50 patients per day undergo IVI without over-crowding the IVIC and OT, which allows personnel to be redeployed for other OTs, and 72 slots for IVI are available for each daily session. These results are in line with a previous study, which also has shown an increase of the weekly number of slots for IVIs available and of weekly IVIs sessions. 5 The IVIC optimizes time usage, resources and costs, increasing visual outcomes and reducing the waiting list for IVIs. Also, although not formally assessed with feedback questionnaires, an increased qualification and satisfaction in healthcare professionals working at the IVIC has been perceived. The availability of diagnostic tools, surgical instruments and administrative logistic support in the same Centre within a few metres from each other ensures a faster and more reliable flow of information. The continuous monitoring of the second eye is very useful for the purpose of early detection of w-AMD, and this is critical in order to improve visual outcomes. 19 Moreover, with the new generations of OCTs, the time needed for scan acquisition is significantly shorter.20,21 Although it has not been recommended by clinical trials, OCT (and OCT-A, in the presence of suspicious areas) should be performed upon each access, even within the fixed regimen, without wasting time. As a result and similarly to a previous study, our IVIC also implements the just-in-time management principle: patients just diagnosed with w-AMD with clinical indication for IVI therapy are able to undergo their first IVI on the same day (one-stop clinic). 5 A more standardized intervention process seems to optimize the IVI care pathway. Van Calster and colleagues 22 have shown that the use of the same protocol for all patients admitted for IVI causes a reduction in the waiting time. Moreover, the introduction of digital medical records in ophthalmology23–25 can produce benefits from both economic and management perspectives, 26 protect patients’ confidential data and increase patients’ safety as adverse reaction to IVIs can be more easily identified, implementing the Clinical Governance principles. Finally, the ‘big data’ collected in a database will improve the knowledge of retinal diseases, ameliorating the treatments.27,28
Our study also shows that the percentage of satisfied patients rating IVIC ⩾8/10 points at the standardized feedback questionnaire was significantly higher when compared with MRU (p = 0.00105). To the best of our knowledge, this result has not been reported so far with a Lean methodology approach applied to IVIs, but only for patients undergoing laser posterior capsulotomy treatment protocols. 16 In fact, in the analysis of the patients’ standardized feedback questionnaires, a significant comfort perceived by elderly patients at the IVIC emerged. Patient satisfaction is increased by less crowded rooms, minimum time wasted, shorter distance travelled at the IVIC, familiarity with the same highly qualified staff, the appointment-calendar containing all IVIs and the follow-up visits scheduled over the following weeks or months (depending on the treatment regimen), and the functional and anatomic examinations performed during each access. This explains the good compliance of our patients, as demonstrated by the results of the patient recall, unlike previous series reporting high rates of patient-associated non-adherence to IVI regimens, defines as unintended gaps >56 days between treatments/follow-ups. 29
This study has some limitations: the retrospective design, which may cause ascertainment bias, and the single-centre setting. Nevertheless, a strength of this report include the analysis of patients’ standardized feedback questionnaires which helped in gathering information about the satisfaction of patients and caregivers, as opposed to previous literature. 5 However, this study reinforces the concept of ‘patient center care’, on which the entire IVIC staff was trained.
Conclusion
The response to the varying health needs of the population must be planned and remodelled in line with the emerging epidemiological framework and must adhere to specific requirements of appropriateness, effectiveness, efficiency and safety. An adequate balance between healthcare and wise use of financial resources cannot ignore, in addition to the financial resources invested, the identification, creation and implementation of an efficient and appropriate sustainable re-organizational model. 30 Despite pre-existing limitations in personnel and resources, our IVIC will improve the quality of healthcare offered by the IVI service of ‘Ospedali Riuniti Area Vesuviana’ with its one-way fast route and accelerated overall procedure. We hope that this new setting could be tested also in different Hospitals and services, such as in a Vitreoretinal service for the management of patients with vitreoretinal interface syndrome, for whom a standardized surgical technique is available and has already shown significant post-operative visual improvements. 31 We believe that the introduction of Lean methodology in this field could facilitate patients for surgery and optimize human resources and surgical timings. We also hope that relevant data could be collected in order to obtain more epidemiological and clinical information about its effectiveness in different ophthalmology fields.
Acknowledgments
Marco Verolino and Piergiacomo Grassi contributed equally to this paper and are both first authors.
Footnotes
Author contributions: M.V., P.G. and C.C. contributed to work design. G.S., G.D. and S.D.S. contributed to acquisition of data. M.V., P.G. and C.C. contributed to interpretation of the results. M.V., P.G. and C.C. contributed to revision of the manuscript. M.V., P.G. and C.C. contributed to approval of the final version.
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The authors received no financial support for the research, authorship and/or publication of this article.
Ethical issues: The study has been evaluated by the Institutional Review Boards of Ospedali Riuniti Area Vesuviana and deemed not to require ethics approval given its retrospective nature.
ORCID iD: Piergiacomo Grassi  https://orcid.org/0000-0001-8741-5919
https://orcid.org/0000-0001-8741-5919
Contributor Information
Marco Verolino, ASL Napoli 3 Sud, Ospedali Riuniti Area Vesuviana, Naples, Italy.
Piergiacomo Grassi, Clinical Fellow in Vitreoretinal Surgery, Department of Vitreoretinal Surgery, Moorfields Eye Hospital NHS Foundation Trust, 162 City Road, London EC1V 2PD, UK.
Gennaro Sosto, ASL Napoli 3 Sud, Ospedali Riuniti Area Vesuviana, Naples, Italy.
Gaetano D’Onofrio, ASL Napoli 3 Sud, Ospedali Riuniti Area Vesuviana, Naples, Italy.
Stefania De Simone, Institute for Research on Innovation and Services for Development (IRISS), National Research Council (CNR), Naples, Italy.
Ciro Costagliola, Full Professor in Ophthalmology, Department of Medicine and Health Science ‘V. Tiberio’, University of Molise, Campobasso, Italy.
References
- 1. Ohno T. Toyota production system: beyond largescale production. Portland, OR: Productivity Press, 1988. [Google Scholar]
- 2. Womack JP, Jones DT, Roos D. The machine that changed the world: the story of lean production-Toyota’s secret weapon in the global car wars that is now revolutionizing world industry. New York: Harper Perennial, 2007. [Google Scholar]
- 3. Fillingham D. Lean healthcare: improving the patient’s experience, vol. 26. Chichester: Kingsham Press, 2008. [Google Scholar]
- 4. Ciulla TA, Tatikonda MV, ElMaraghi YA, et al. Lean Six Sigma techniques to improve ophthalmology clinic efficiency. Retina 2018; 38: 1688–1698. [DOI] [PubMed] [Google Scholar]
- 5. Grassi MO, Furino C, Recchimurzo N, et al. Implementation of Lean healthcare methodology in designing an Intravitreal Injection Center: first Italian experience. Int Ophthalmol 2020; 40: 2607–2615. [DOI] [PubMed] [Google Scholar]
- 6. Womack JP, Jones DT. Lean thinking. New York: Simon & Schuster, 1996. [Google Scholar]
- 7. Burgess N, Radnor Z. Evaluating Lean in healthcare. Int J Health Care Qual Assur 2013; 26: 220–235. [DOI] [PubMed] [Google Scholar]
- 8. Spilsbury K, Garrett KL, Shen WY, et al. Overexpression of vascular endothelial growth factor (VEGF) in the retinal pigment epithelium leads to the development of choroidal neovascularization. Am J Pathol 2000; 157: 135–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Krzystolik MG, Afshari MA, Adamis AP, et al. Prevention of experimental choroidal neovascularization with intravitreal anti-vascular endothelial growth factor antibody fragment. Arch Ophthalmol 2002; 120: 338–346. [DOI] [PubMed] [Google Scholar]
- 10. Flaxman SR, Bourne RRA, Resnikoff S, et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and metaanalysis. Lancet Glob Health 2017; 5: e1221–e1234. [DOI] [PubMed] [Google Scholar]
- 11. Nicosia F. Sanita` lean. Migliorare il servizio ai pazienti, ridurre gli sprechi, innovare la gestione ospedaliera con il metodo Toyota. Milan: Guerini Next, 2017. (in Italian) [Google Scholar]
- 12. Toussaint JS, Berry LL. The promise of Lean in health care. Mayo Clin Proc 2013; 88: 74–82. [DOI] [PubMed] [Google Scholar]
- 13. Redazione, Osservatorio Malattie Rare (OMAR). Cos’è la degenerazione maculare? https://www.osservatoriomalattierare.it/38-descrizioni/sezioni/4046-cose-la-degenerazione-maculare (2013, accessed 13 May 2013).
- 14. Polat O, Inan S, Ozcan S, et al. Factors affecting compliance to intravitreal anti-vascular endothelial growth factor therapy in patients with age-related macular degeneration. Turk J Ophthalmol 2017; 47: 205–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Leivo T, Sarikkola AU, Uusitalo RJ, et al. Simultaneous bilateral cataract surgery: economic analysis; Helsinki simultaneous bilateral cataract surgery study report 2. J Cataract Refract Surg 2011; 37: 1003–1008. [DOI] [PubMed] [Google Scholar]
- 16. Lindholm JM, Laine I, Hippala H, et al. Improving eye care services with a lean approach. Acta Ophthalmol 2018; 96: 724–728. [DOI] [PubMed] [Google Scholar]
- 17. Gupta PC, Kumar MP, Ram J. COVID-19 pandemic from an ophthalmology point of view. Indian J Med Res 2020; 151: 411–418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Chandra A, Romano MR, Ting DS, et al. Implementing the new normal in ophthalmology care beyond COVID-19. Eur J Ophthalmol. Epub ahead of print 22 November 2020. DOI: 10.1177/1120672120975331. [DOI] [PubMed] [Google Scholar]
- 19. Zarranz-Ventura J, Liew G, Johnston RL, et al. The neovascular age-related macular degeneration database: report 2: incidence, management, and visual outcomes of second treated eyes. Ophthalmology 2014; 121: 1966–1975. [DOI] [PubMed] [Google Scholar]
- 20. Bosche F, Andresen J, Li D, et al. Spectralis OCT1 versus OCT2: time efficiency and image quality of retinal nerve fiber layer thickness and Bruch’s membrane opening analysis for glaucoma patients. J Curr Glaucoma Pract 2019; 13: 16–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Li XX, Wu W, Zhou H, et al. A quantitative comparison of five optical coherence tomography angiography systems in clinical performance. Int J Ophthalmol 2018; 11: 1784–1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Van Calster J, Willekens K, Seys D, et al. Standardized care by redesign of an intravitreal injection pathway. Eur J Ophthalmol 2019; 29: 92–99. [DOI] [PubMed] [Google Scholar]
- 23. Wakamiya S, Yamauchi K. Evaluation of electronic medical records for ophthalmology based on changes in staff work through introduction of electronization. Stud Health Technol Inform 2013; 192: 968. [PubMed] [Google Scholar]
- 24. Keenan TD, Johnston RL, Donachie PH, et al. United Kingdom National Ophthalmology Database Study: diabetic retinopathy; report 1: prevalence of centre-involving diabetic macular oedema and other grades of maculopathy and retinopathy in hospital eye services. Eye 2013; 27: 1397–1404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Writing Committee for the UK Age-Related Macular Degeneration EMR Users Group. The neovascular age-related macular degeneration database: multicenter study of 92 976 ranibizumab injections: report 1: visual acuity. Ophthalmology 2014; 121: 1092–1101. [DOI] [PubMed] [Google Scholar]
- 26. Wiggins RE, Jr, Fridl DC. Analysis of the financial return of electronic health records. Ophthalmology 2016; 123: 214–216.e212. [DOI] [PubMed] [Google Scholar]
- 27. Parke Ii DW, Lum F, Rich WL. The IRIS® registry: purpose and perspectives. Ophthalmologe 2017; 114: 1–6. [DOI] [PubMed] [Google Scholar]
- 28. Gillies MC, Walton R, Liong J, et al. Efficient capture of high-quality data on outcomes of treatment for macular diseases: the Fight Retinal Blindness! Project. Retina 2014; 34: 188–195. [DOI] [PubMed] [Google Scholar]
- 29. Ehlken C, Helms M, Bohringer D, et al. Association of treatment adherence with real-life VA outcomes in AMD, DME, and BRVO patients. Clin Ophthalmol 2017; 12: 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. De Simone S. Wellbeing at work: a survey on perception of health care workers. Riv Int Sci Soc 2015; 4: 395–412. [Google Scholar]
- 31. Romano MR, Cennamo G, Grassi P, et al. Changes in macular pigment optical density after membrane peeling. PLoS ONE 2018; 13: e0197034. [DOI] [PMC free article] [PubMed] [Google Scholar]