Abstract
This study assesses the quality of care for preterm, low birth weight (LBW), and sick newborns across the public health care system levels in 3 regions of Ethiopia. Qualitative data based on the WHO framework to assess provision and experience of care was collected using in-depth interviews and focus group discussions with women who recently delivered preterm, LBW, and sick newborns, as well as health care providers and health extension workers, and facility administrators associated with study health facilities. This qualitative approach revealed perspectives of patients, health care providers and facility administrators to assess what is actually happening in facilities. Clinical guidelines for the care of preterm, LBW, and sick newborns were not available in many facilities, and even when available, often not followed. Most providers reported little or no communication with parents following hospital discharge. Human resource challenges (shortage of skilled staff, motivation and willingness, lack of supervision, and poor leadership) inhibited quality of care. Participants reported widespread shortages of equipment and supplies, medication, physical space, water, electricity, and infrastructure. Economic insecurity was a critical factor affecting parents’ experience. Acceptance by users was impacted by the perceived benefits and cost. Users reported they were less likely to accept interventions if they perceived that there would be financial costs they couldn’t afford. The quality of care for preterm, LBW, and sick newborns in Ethiopia as reported by recently delivered women, health care providers and facility administrators is compromised. Improving quality of care requires attention to process of care, experience of care, and health system capacity, structure, and resources.
Keywords: Quality of Care, Newborn, Infant, Premature, Preterm Birth, Low Birth Weight, Sick Newborn, Qualitative Research, Ethiopia
Background
The period from birth to 28 days is the most vulnerable for child survival. Globally, 2.4 million newborns died in 2019, comprising 47% of under-5 mortality. 1 Causes included preterm complications, intrapartum-related events, sepsis, meningitis, congenital problems, and other causes. 2 Almost 80% of newborn deaths occurred in sub-Saharan Africa and Southern Asia. 3 Ethiopia’s estimated neonatal mortality is 29 deaths per 1000 live births. 4 An estimated 10% of all newborns were preterm, and 20% were low birth weight (LBW). 4 With evidence-based, cost-effective care during and after delivery, most newborns born at 32 to 37 weeks gestation can survive even without neonatal intensive care.5,6 In lower- and middle-income countries, neonatal intensive care units vary in infrastructure and quality of care, affecting newborn survival.7,8 Skilled newborn care using evidence-based practices respectfully in a supportive environment can end preventable maternal and newborn morbidity and mortality. 9
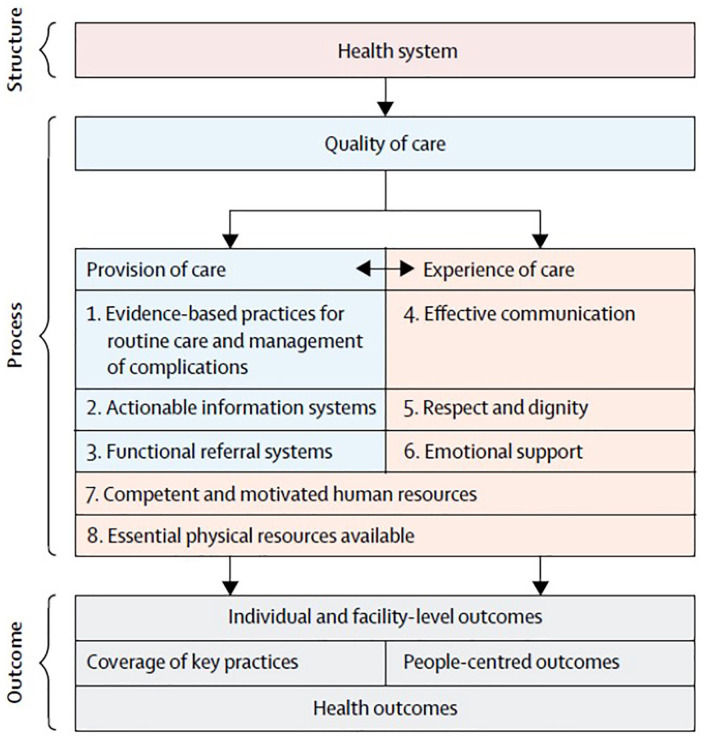
High-quality care, integral to the right to health, equity, and the preservation of dignity for women, newborns, and children, requires appropriate use of effective clinical and non-clinical interventions, strengthened health infrastructure, optimum skills, and positive provider attitude. 9 Quality of care includes: availability of equipment, supplies, guidelines, and protocols; knowledge, skills, training, experiences, and motivation of health workers; supportive supervision; and client satisfaction with the care provided. The WHO quality standards are organized into 3 domains: provision of care, experience of care, and cross-cutting (Table 1).10,11
Table 1.
Summary of WHO quality of care standards.
| Domain | Quality standard | Description of quality standard |
|---|---|---|
| Provision of care | Evidence-based practices | Every woman and newborn receive routine, evidence-based care and management of complications during labor, childbirth, and the early postnatal period, according to WHO guidelines. |
| Actionable information systems | The health information system enables use of data to ensure early, appropriate action to improve the care of every woman and newborn. | |
| Functional referral systems | Every woman and newborn with condition(s) that cannot be dealt with effectively with the available resources is appropriately referred. | |
| Experience of care | Effective communication | Communication with women and their families is effective and responds to their needs and preferences. |
| Respect and preservation of dignity | Women and newborns receive care with respect and preservation of their dignity. Respectful care preserves women’s dignity, privacy, confidentiality, and freedom from mistreatment—physical/sexual/verbal abuse, discrimination, neglect, detainment, extortion, or denial of services—at any time and in any facility. | |
| Emotional support of families | Every woman and her family are provided with emotional support that is sensitive to their needs and strengthens the woman’s and family’s capability. | |
| Cross-cutting | Competent and motivated human resources | For every woman and newborn, competent, motivated staff are consistently available to provide routine care and manage complications. |
| Essential physical resources | The health facility has an appropriate physical environment, with adequate water, sanitation and energy supplies, medicines, supplies, and equipment for routine maternal and newborn care and management of complications. |
Abbreviation: WHO, World Health Organization.
Ethiopia’s Federal Ministry of Health (FMOH) has introduced hospital guidelines to improve the quality of government hospitals that began in 2006 with the Ethiopian Hospital Management Initiative. 12 The most recent Ethiopian Hospital Services Transformation Guidelines released in 2016 build on and expand previous guidelines to include maternal, neonatal, and child health services, 12 but the quality of newborn health care has not maintained pace with health service expansion.
Most of the quality measures assessed by existing quantitative tools relate to input measures and availability of physical resources, and leave important gaps in measuring experience of care.13,14 Previous research from low-income countries has been focused on assessments of health system readiness to deliver newborn care, but assessments of the quality of newborn care are incomplete in scope.15-17 The goal of this narrative research study was to describe quality of care for preterm, LBW, and sick newborns using qualitative methods, across the public health care system levels in 3 regions in Ethiopia.
Methods
Study design
As part of a multi-site qualitative study, we conducted qualitative interviews and focus groups from December 2017 to February 2018 in Addis Ababa, Amhara, and Oromia regions of Ethiopia. All participants’ demographic data were collected via questionnaire. Qualitative data were collected from individuals in the government health care system as follows: (1) health facility-based obstetric/newborn care providers including health extension workers (HEWs) (hereafter “providers”): focus group discussions (FGDs) and in-depth interviews (IDIs); (2) public health care system administrators (hereafter “administrators”): key informant interviews (KIIs); and (3) recently delivered women; mothers of preterm, LBW and sick newborns (hereafter RDW): IDIs.
We utilized O’brien’s Standards for Reporting Qualitative Research as a guide for our work and our reporting. 18 Verbal informed consent was provided by all participants prior to their enrollment. Participants were allowed to terminate the interviews at any time and informed that non-participation would not result in any penalties.
Ethiopia’s FMOH partnered with the USAID-funded Every Preemie—SCALE project/Global Alliance to Prevent Prematurity and Stillbirth (GAPPS) and St. Paul’s Hospital Millennium Medical College in Addis Ababa to study current services and programs across all tiers of the public health care system. The research team was comprised of medical doctors, public health professionals, an anthropologist, and local data collectors. Data collectors were experienced conducting interviews and FGDs and were supervised by master degree level study administrators. They were trained in qualitative data collection and use of all study tools prior to starting their work. Data collectors were not previously known to interviewees.
Study sites
Ethiopia is the second most populated African country, with a 2018 population estimate of 107 million. 19 Our selection of regional sites represented semi-pastoral agrarian, settled agrarian, and urban communities of Ethiopia. Table 2 shows regional characteristics.
Table 2.
Characteristics of study regions. a
| Characteristics | National | Addis Ababa | Amhara | Oromia |
|---|---|---|---|---|
| Demographic indicators | ||||
| Proportion urban population, % b | 16.2 | 100.0 | 12.3 | 12.4 |
| Total fertility rate, No. of children per woman | 4.6 | 1.8 | 3.7 | 5.4 |
| Proportion of women who are literate, % | 42.0 | 87.8 | 44.9 | 37.3 |
| Proportion of women who own/use bank account, % | 15.1 | 53.6 | 20.9 | 8.4 |
| Proportion of women who own/use a mobile phone, % | 27.3 | 87.0 | 21.2 | 23.3 |
| Proportion of men who are engaged in agriculture, % | 71 | 1 | 62 | 41 |
| Mortality rates | ||||
| Under-5 mortality, No. per 1000 live births | 67 | 39 | 85 | 79 |
| Infant mortality, No. per 1000 live births | 48 | 28 | 67 | 60 |
| Neonatal mortality, No. per 1000 live births) | 29 | 18 | 47 | 37 |
| Maternal and child health services indicators | ||||
| Physician to population ratio c | 1:36 158 | 1:3056 | 1:58 567 | 1:76 075 |
| Proportion of pregnant women who received antenatal care from a skilled provider, % | 28.0 | 96.8 | 67.1 | 50.7 |
| Proportion of deliveries in health facility, % | 26.0 | 96.6 | 27.1 | 18.8 |
| Proportion of women with a postnatal checkup in first 2 days after birth, % | 17.0 | 55.4 | 21.9 | 11.8 |
| Proportion of children (ages 12-23 mo) who received all basic vaccinations by 12 mo, % | 22.0 | 81.6 | 39.9 | 24.3 |
Working with the Ethiopian Federal Ministry of Health, we considered other ongoing research, health infrastructure, size of population, civil security, and federal priorities when choosing 65 facilities in settings that were broadly representative of local contexts (Table 3).
Table 3.
Number of study sites and number of participants completing interviews or focus group discussions.
| Addis Ababa, No. | Amhara, No. | Oromia, No. | Total, No. | |
|---|---|---|---|---|
| Study sites | ||||
| Health post | 0 | 13 | 14 | 27 |
| Health center | 21 | 8 | 3 | 32 |
| Primary hospital | 0 | 1 | 1 | 2 |
| Secondary hospital | 1 | N/A | 1 | 2 |
| Tertiary hospital | 2 | N/A | N/A | 2 |
| Study instrument completed | ||||
| In-depth interview, Recently delivered women | 18 | 4 | 0 a | 22 |
| In-depth interview, Health extension workers | 4 | 8 | 9 | 21 |
| Focus group discussion, Providers | 10 | 9 | 4 | 23 |
| Key informant interview, Facility administrators | 12 | 14 | 11 | 37 |
Abbreviation: N/A, non-applicable.
Recently delivered women in Oromia could not be included in the study due to geography and limited study resources.
Recruitment and sampling
We used purposive sampling for recruitment. A sample of staff and clients participated at each tier of the public health care system from health facilities, including health post (HP), health center (HC), and primary, general, and specialized hospitals in each region. Participant eligibility criteria varied by study tool for a total of 103 participants.
IDIs
All eligible RDW at secondary and tertiary hospitals in Addis Ababa and at HPs, HCs and primary hospitals in Amhara were recruited. Eligibility criteria: (1) Delivered small (ie, preterm, LBW, intrauterine growth restriction, or small for gestational age births) or sick newborn within any tier study facility in the government health system; (2) resided in the study catchment areas; (3) spoke Amharic, English, or Oromiffa; and (4) If <18 years of age, obtained parental or guardian consent. RDW were identified from delivery and discharge registers at tertiary, secondary, and primary hospitals and from health centers and health posts. RDW were interviewed at their home or facility depending on the convenience of the RDW. A total of 22 RDW completed the IDI (Table 2).
IDIs were also conducted with 21 HEWs using the provider FGD instrument in Amharic (Table 2). Eligibility criteria: (1) currently working in a study facility with 6 months experience; and (2) currently providing maternal/newborn care.
KIIs
A subset of HPs and HCs, and all public primary, secondary and tertiary hospitals (Addis Ababa, Amhara, Oromia) were included. All clinical, nursing, and administrative leads at the study health facilities involved in pregnancy, labor, and delivery/obstetrics and gynecological, postnatal, and newborn care services at the facility were recruited. A total of 37 participated in Amharic or Oromiffa (Table 2).
FGDs
All eligible clinical, nursing, midwifery staff (at HCs and hospitals), and HEWs (at HPs) were recruited. Eligibility criteria: (1) currently working in a study facility with 6 months experience; and (2) currently providing maternal/newborn care. A total of 96 participated in 23 FGDs (Table 2).
Interview data were reviewed from all 3 study regions weekly during data collection by 2 study investigators until data saturation was reached (indicated by thematic repetition within subsamples).
Data tools
We designed a short demographic questionnaire to collect data on age, parity, marital status, education and profession. Semi-structured qualitative IDI, KII, and FGD guides were developed using a multi-step process to assess standards in the World Health Organization (WHO) quality maternal and newborn care framework 10 that conceptualizes quality maternal and newborn care by identifying 8 domains: (1) Evidence-based practices, (2) Actionable information systems, (3) Functional referral systems, (4) Effective communications, (5) Respect and preservation of dignity, (6) Emotional support, (7) Competent motivated human resources, and (8) Essential physical resources available (see Figure 1). Our 3 tools were initially designed and questions created based on the WHO framework, then pre-tested with RDW, providers, and administrators by trained data collectors. The tools were then adjusted for clarity and functionality 22 to gather data to inform how and why the system needed improvements based on the WHO framework and from the perspectives of 3 actors integral to the process: mothers, providers, and administrators. With respect to protocols and guidelines, we asked providers and administrators about the existence and use of protocols/guidelines and requested they show the materials for verification.
Figure 1.
World Health Organization (WHO) framework for the quality of maternal and newborn health.
Reproduced from Standards for Improving Quality of Maternal and Newborn Care in Health Facilities. 10
Data management
Recording, transcribing, and translation
Demographic questionnaires were administered orally immediately preceding each IDI/KII and on paper for FGDs, recorded on a tablet or log sheet, then uploaded into Excel software for simple descriptive analyses. Qualitative IDIs, KIIs, and FGDs were recorded digitally then transcribed and translated. Recordings were transcribed into the local written language by experienced transcriptionists and were subsequently translated into English by professional translators. A third team member spot-checked for accuracy. During recruitment and data collection, participants were assigned identification numbers which were subsequently linked to data. No names were attached to recordings or transcripts. No personal identifying information is associated with any quotes in this or any other publications from the project. We include quote identifiers as follows: source (IDI, KII, FGD), facility level (HP = health post, HC = health center, HOSP = hospital), and interviewee (RDW = recently delivered woman, HCP = health care provider, FA = facility administrator).
Analysis
Demographic questionnaire responses were analyzed using Excel. Qualitative data were analyzed in NVivo 23 Version 12 using thematic analysis with an iteratively developed codebook derived from study goals, tools, data, and the conceptual framework. Each transcript was coded by 1 member of a multiple coder team of study investigators (medical doctors, public health professionals, and an anthropologist) with periodic reconciliation (every fifth transcript) during which 2 coders coded the same transcript to check for coding consistency between coders and accuracy/usability of the codebook. Each code report was synthesized by 1 team member using a systematic approach in which annotated comments were summarized into a table of theme domains and subdomains with associated quotes. These tables were then interpreted, using the WHO framework as a guide. Triangulation between IDI, KII, and FGD further enhanced validity.
Informed consent and ethical approval
Individual participants were informed that participation was voluntary and there were no benefits nor consequences to participating. No financial incentives were provided to participants. Data collectors provided aural or written consent forms to RDW per their literacy level; all participants signed consent forms in their preferred language. All participating offices and institutions submitted letters of support. The Institutional Review Boards of the St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia (IRB No. PM23/111), and Project Concern International (IRB No. 25) approved this study.
Results
Description of sample
All RDWs were from Addis Ababa, Amhara Region, and Oromia Region. The largest proportion of RDWs were from Addis Ababa, 20 to 29 years, primiparous, and married. The number of facility administrators who participated in the KIIs were proportionate across the 3 regions, 66.7% were 20 to 29 years old, and 40.5% were head nurses. For providers participating in the FGDs and IDIs, 61.5% of providers were from Addis Ababa, 81.3% were 20 to 29, 74.0% were from HCs, 60.0% had 2 to 5 years of experience, 92.0% had diplomas or bachelor degrees, and 4.2% were medical doctors.
Qualitative findings
Facilities did not meet WHO standards of care, primarily in provision of care (evidence-based practices, actionable information systems, functional referral system, competent and motivated human resources, and essential physical resources). In other areas primarily in experience of care, meeting standards varied by facility or staff member (effective communication, respectful care, emotional support) (Table 4).
Table 4.
Themes and sub-themes from thematic analysis of responses.
| Themes and sub-themes |
|---|
| Provision of care themes |
| Evidence-based practices |
| Low availability of, and adherence to, protocols and guidelines |
| Actionable information systems |
| Medical records absent for outpatient children; confidentiality not protected |
| Routine care not adequately documented |
| Functional referral system |
| Referrals necessary for sophisticated care beyond initial facility capacities |
| Poor referral communication |
| Referrals complicated by transportation deficits |
| Experience of care themes |
| Effective communication between provider and patient |
| Some patients satisfied with provider guidance, for example, breastfeeding, danger signs |
| Variability in degree to which providers were transparent and supportive to patients |
| Permission and informed consent not consistent |
| Respectful care and preservation of dignity |
| Focus on parent-newborn unity and parent involvement not consistent across facilities |
| No consistent policy/practice on parent-newborn unity |
| Respect for family members varied by facility and staff member; impacted by high patient load |
| Emotional support of families |
| Staff support provided to emotional RDW varied by facility and by individual staff |
| Cross-cutting themes |
| Competent and motivated human resources |
| Shortages of trained staff and specialists |
| Under-incentivized and overworked staff |
| Variable staff supervision |
| Essential physical resources |
| Deficits in equipment/supplies, medication, space, water, electricity, infrastructure at all facility levels |
| Emergent theme affecting experience of care |
| Financial insecurity |
| Parents’ perception of cost for transport, services, medication resulted in delays or refusals |
Provision of care
Evidence-based practices
Availability and use of protocols and guidelines
Most participants noted that relevant protocols and guidelines were not available despite providing care for preterm, LBW, and sick newborns. Specifically, kangaroo mother care (KMC), LBW, and neonatal care protocols were missing, particularly at HCs.
Even with available guidelines, lack of space, equipment, supplies, trained professionals, and high patient load limited adherence. As one participant described: “Based on the guideline, one baby should stay in one incubator, but due to a shortage of materials we put even three preterm babies in one incubator. We put up to six babies for phototherapy” (KII-HOSP-FA). Guideline recommendations and the reality of practicing medicine in an under-resourced setting did not align. For example: “The guideline says women should stay in the health facility for 24 hours after giving birth, but it is difficult to implement this because there are not enough beds” (KII-HC-FA).
Despite these challenges, some providers reported using guidelines (including for basic emergency obstetric and newborn care and Integrated Management of Childhood Illness [IMNCI]), but content was limited regarding the special care of preterm, LBW, and sick newborns. Physicians appeared to be primary users of guidelines, and especially for asphyxia, resuscitation, referral procedures, NICU care, jaundice, and diarrhea.
Actionable information systems
Medical record handling and confidentiality
Medical records need to be available for prompt, good-quality medical care, but according to participants, priority was not given to outpatient children; the absence of medical records could result in medical order and prescription errors: “If the file is lost, how can you treat him? How can you know what medication he has taken?” (FGD-HC-HCP). This failure was attributed to no coordination between staff. Providers said records were accessible to personnel from other units or departments within the facility, and not on a strictly “need to know” policy.
Routine care documented
Teams used guideline checklists, cards, and the facility health information system for documenting care and auditing mortality data, but handover of patients and referrals often relied solely on verbal transmission of information. Reasons included lack of coordination and fragmentation across different units in the documentation process, no standard referral forms at HP, and a lack of process for recording detailed information.
Functional referral systems
Recognized need for referral
An effective referral system was seen by respondents across the sample as critical for successful care of preterm, LBW, and sick newborns for 3 primary reasons:
Newborns required sophisticated hospital care: HEWs direct parents to take newborns directly from home to hospital for care and medication when the newborn was perceived as needing secondary or tertiary care.
Inadequate medical care at HC: HC staff advised KMC/skin-to-skin contact and placement under radiant heater (if available), then referred to the hospital.
Nonexistent medical care at HP: HPs lack even the most rudimentary equipment, space, and supplies for care of fragile newborns: “We only have one scale to check the weight of the newborns. The lack of [equipment in] these facilities is a big obstacle in implementing the regulations” (KII-HP-FA).
Participants clearly stated that HEWs worked most closely with the community at the grassroots level, serving as the primary referral link to higher-level facilities: “HEWs make home visits to women who gave birth in their community, and use this visit to identify sick newborns. Then they link the cases to the health center. If there were low birth weight cases or any birth defect, they would be referred directly to [a specialty] hospital” (FGD-HC-HCP).
Post-discharge follow-up care of mothers and newborns should function via the HEW program; however, most providers noted that there was little or no hospital feedback communication with HEWs about discharge. Participants reported that HCs provided feedback to HEWs in person, by phone, or at catchment HC meetings, although hospitals failed to do so.
Transportation problems in referral system
The referral system was plagued by transportation problems (lack of vehicles, expenses, traffic jams), resulting in serious delays and poor outcomes for preterm, LBW, and sick newborns. In one particularly harrowing example, a respondent reported that a RDW unable to access transportation arrived at the hospital with her dead baby 2 days after her referral was initiated.
In Addis Ababa, government-supported, no-cost ambulances were reported to be readily available and HCs were near hospitals; transportation and ambulance problems were minimal. Problems were reported from the majority of health facilities outside of Addis Ababa: a shortage or complete absence of no-cost ambulances in remote districts, delays, equipment/oxygen/medication shortages in ambulances, provider absences in ambulances. Ambulances were often understood to be only for RDW and not for newborns even if originally or administratively intended for both.
Ambulance orders were expected to come through hospital liaison officers or district health offices, not through providers or HC level officers. As a result, drivers failed to respond when providers called them directly. Other delays occurred when recipient hospital personnel denied referral requests (in contradiction to guidelines); as one facility administrator explained, “When we refer children there is one tradition practiced that the baby will not be referred if all investigations are not done. The baby may wait until some investigation is done” (KII-HOSP-FA). Delays resulted in unintended home delivery and also in newborn death.
Experience of care
Effective communication between providers and parents
Participants reported that providers communicated to RDW and their families regarding breastfeeding, temperature regulation, newborn condition, danger signs, and referral decisions.
RDW’s satisfaction varied as exemplified by 2 excerpts: “After he was admitted here they told me he will be all right and will get a good follow-up. They also told me not to worry about the care given here and it would be dangerous for him if I take him away to home. They are the ones who advised and helped me to cope” (IDI-RDW); and “My baby was admitted for 10 days without informing me why, so I am not happy with this too. I am very sad” (IDI-RDW).
Facility administrators reported that both informed consent and parental permission were consistently obtained before provision of newborn care, except in the case of some minor procedures and medications. Across the sample, providers and administrators agreed that informed consent was necessary, and parents were informed prior to procedures. But several RDW reported their newborns were treated without their informed consent because providers did not respect mothers’ choices. When RDW were not informed by providers, parental involvement in newborn care became limited.
Respectful care and preservation of dignity
Parent-newborn unity and parent involvement
Barriers to parent-newborn unity during inpatient care appeared to vary between providers and health facilities. Depending on facility, RDW or both parents or larger families could access preterm, LBW, and sick newborns. Access might be restricted due to: space restrictions, few/no parent beds, infection risk, or no policy promoting unity. Social factors could also impact parental participation in newborn care including: parents’ inability to pay for transportation and housing to accompany newborn to hospital, household domestic responsibilities, beliefs that unbaptized small newborns may be destined to die and are not yet full members of a family, and maternal health condition.
Participants noted a lack of policy on parent-newborn unity, and variation in practices between facilities. With the exception of fathers providing skin-to-skin contact, generally, fathers’ access to preterm, LBW, and sick newborns was restricted depending on the infant’s condition, number of visitors and time of visit. When the infant was in critical condition or the RDW was absent, fathers may have had more access. RDW access was universally prioritized over fathers or other family caregivers: “No one other than the mother is allowed to enter [the NICU]; even logically it is not good to allow other persons to enter because they cannot do anything. The service is provided by providers and the mother should follow her baby in nearby place” (FGD-HOSP-HCP).
Respect to family members caring for newborns
Some RDW felt respected and relieved during facility treatment, whereas others felt strongly that they were disrespected and even refused care. Patients at hospitals and HCs reported experiencing disrespect from doctors, nurses, or medical records room workers (who refused to provide information). While some providers attributed disrespect to a lack of supervision, others reported that providers became aggressive or loud for the “comfort of the baby” or because caregivers had created problems.
Facility staff perceptions reflected a nuanced recognition of the challenging environment where newborns received care. Administrators recognized that some aggressive providers responded with a “poor approach” when parents asked for something. This was thought to occur especially at HCs and hospitals with a high patient load.
Emotional support of families
According to RDW, parents experienced severe crises requiring emotional support, including: fear-induced crying, inability to control emotions, worry prior to treatment, extended stay in health facility, stress and loneliness, concern about newborn’s outcome, and hopelessness from hearing poor outcome. Administrators, too, recognized that parents were emotional due to referral and awareness of their newborn’s compromised health status.
Recognizing the necessity of emotional support, advice, information, and assistance, some RDW and providers reported that staff supported mothers, while others said providers failed to inform parents about newborns’ condition or provide emotional support. As one RDW described, “After delivery they didn’t tell me what happened to my baby for two days. He [the provider] didn’t even respond when I asked him” (IDI-RDW).
Cross-cutting themes affecting provision and experience of care
Competent and motivated human resources
Preterm, LBW, and sick newborns’ vulnerability for morbidity or death require adequate staffing, but limits to human resources inhibited quality of care. One provider captured this well: “Each baby needs continuous care; it is not like adults that you can give care at some time interval. So there should be constant providers and the number of providers need to be increased; one provider is needed for one baby if they are critically sick; if possible one nurse should assign for one baby” (FGD-HOSP-HCP).
Participants from most but not all health care facilities reported shortages of trained staff, neonatologists nationally, and night-duty staff, which resulted in understaffed units and overworked providers compounded by a lack of adequately skilled providers. Participants pointed out the need for trained neonatal nurses and physicians: “There should be at least one fully trained neonatal nurse in each facility; if we ensure this definitely we can minimize neonatal death. We have trained in neonatal resuscitation in three days but this is not enough to give quality service” (FGD-HC-HCP). Providers need practical training on medical equipment used to care for sick newborns.
Participants noted that lack of incentives and work overload decreased staff motivation, and in some settings administrators did not motivate staff. One RDW observed, “When your baby gets sick, you become surprised and go to get help, then they respond, ‘I am not on duty, wait for someone.’ How can someone say this while your baby is between life and death?” (IDI-RDW).
Supervision and leadership appeared to vary widely from facilities with no supportive supervision, for example, “All of us in NICU are not trained and there is no supervisor. I make best effort to care for the babies and he does his best too. . . .there is no one who says ‘Do this, don’t do that, follow the protocol’” (FGD-HC-HCP) to others where internal monitoring by immediate supervisors improved quality of care: “Our boss is a listener and problem solver; she is progressively working to improve the NICU in [areas of] material, infection prevention, and quality improvement” (FGD-HOSP-HCP).
Quality improvement was an ongoing focus in some facilities where leadership recognized the need for change. Participants reported ongoing efforts to improve data collection and management: “There are improvements regarding recordkeeping of maternal and newborn health. So we have now established a committee to improve documentation. . . . Currently we are working in this manner to improve the quality” (FGD-HOSP-HCP). The largest number of providers used consultation when they faced difficult cases and needed assistance.
Essential physical resources
Participants reported widespread barriers to vital resources including: medical equipment and supplies, medication, physical space, water and electricity, and infrastructure. While there were exceptions, the vast majority of responses catalogued deficits (Table 5).
Table 5.
Essential physical resource issues reported by study participants.
| Problems | Consequences |
|---|---|
| Medical equipment and supplies | |
| Shortage of medical oxygen. | Sharing of oxygen tube from one newborn to another. |
| “Because of [the] critical shortage of oxygen, sometimes they take the oxygen tube from one newborn [and give it to another who] needs critical intervention” (FGD-HOSP-HCP). | |
| Shortage of necessary equipment. | Employment of bioengineer to fabricate equipment or borrowing equipment from other hospitals. |
| No diapers or baby clothes. | Staff collect money from each other to purchase. |
| Shortage of lab materials and reagents. | Interruptions to critical medical services. |
| No equipment like glucometer, newborn intranasal prongs, only training. | Loss of life. “We have shortages of materials, like prong [of the] appropriate size for preterm [babies]. . . . Sometimes we don’t have glucometer for a baby [with] hypoglycemia” (KII-HOSP-FA). |
| Very common shortages of radiant warmers, beds, incubators, gloves, manual suction, X-ray, ultrasound, phototherapy machine. | Interruptions of service and care; loss of life. |
| Food available for RDW of KMC infants but not of NICU infants. | RDW must go hungry or provide own food. |
| Medication | |
| Lack of intravenous drugs for neonatal seizures. | Must use oral drugs, which delay response. |
| Frequent medication stockouts. | Regular follow-up required. |
| Shortage of first drugs for sick newborns prior to referral. | Must transport from health center and health post without administering drugs; RDW must purchase drugs. |
| Inadequate supply of vaccines. | Though vaccines are supposed to be free, providers successfully charge women; dearth of supply creates opportunity for corruption. |
| Expiration of medication. | “Currently we don’t have medication. All medicines, including amoxicillin, have expired. We urgently need them” (KII-HP-FA). |
| Physical space | |
| Lack of newborn beds. | Preterm, LBW, and sick newborns must share beds; infirmity or loss of life. |
| Hospital NICUs lack clean, separate space, and rooms. | Neonates must share space, risking infection; staff cannot provide proper care. |
| “What we see is that [the] room size is small, but they admit a high number of newborns. Because of this, all kinds of neonates are admitted in a single room” (FGD-HOSP-HCP). | |
| KMC rooms poorly equipped (no shower, limited food). | RDW cannot bathe or eat unless they leave the facility. |
| No beds or space for RDW with newborns in the NICU. | RDW sleep in chair or latrine or on the ground outside the hospital. “Parents are not allowed to sleep in this corridor, so they sleep on the ground. . . . Imagine how difficult to sleep on a ceramic floor after a day of labor” (KII-HOSP-FA). |
| Water and electricity | |
| Interruptions in water supply or complete absence of water. | Substandard hand washing, unsanitary latrines, absence of showers in facilities. Inadequate infection prevention and control practices. |
| Power interruptions or complete absence of power. | Inability to provide service, interruptions in water (due to lack of power for pump). |
| Some urban facilities have generators. | Provides some relief but does not forestall water interruptions. |
| Infrastructure | |
| Poor or inadequate roads, transportation, and phones, especially at the health center and health post levels. | Influences referral functionality, potential factor in choice of place of care. |
Abbreviations: FGD, focus group discussion; HOSP, hospital; HP, health post; KII, key informant interview; KMC, kangaroo mother care; LBW, low birth weight; NICU, neonatal intensive care unit; RDW, recently delivered women.
Additional emergent theme affecting experience of care
Implications of financial insecurity
In this setting, economic insecurity critically affected parents’ experience during care and care-seeking for preterm, LBW, and sick newborns. Many others reported that having to pay for newborn transport added to parents’ stress; “When the parents are told to take their preterm or low birth weight babies to the hospital they might not have money in hand. . . .They would say ‘I do not have money to pay for motor bike’ or ‘I would not get any benefit by going there’ and decide not to come” (FGD-HP-HCP). Furthermore, some parents believed care required payment and thus opted out. Providers reported that the longer the hospital stay, the bigger the financial consideration: “Depending on their income status, they think of the financial implications they may have from the day of admission to discharge and decide not to come to hospital” (FGD-HP-HCP).
Some parents made choices to delay or forgo care for preterm newborns that were perceived as unlikely to survive. According to providers, parents’ perceptions were based on lack of awareness of free services or the reality that shortages of supplies required them to pay for what would otherwise be free and medications could be expensive, especially in rural areas. Some parents refused providers’ orders to purchase drugs not available in the facility. In some cases, sympathetic providers pooled their own money to purchase newborn care supplies and donated blood for newborn treatment.
Recommendations to improve quality of health care for preterm, LBW, and sick babies
Recommendations of participants can be divided into 3 domains mentioned by all levels of providers:
Provide for the availability and dissemination of guidelines and protocols, adequate number of trained and motivated staff, and adequate medical materials and equipment. “If we have the guideline it will make every performance very easy. The second one is availability of trained [staff] because everything is nothing without trained personnel. Machines and technologies are also important to improve the quality” (KII-HC-FA).
Prioritize services for care of preterm, LBW, and sick newborns in particular, by FMOH and regional health bureaus, health care administrators, and supervisors. According to some participants, MCH services are given attention, but services for RDW are prioritized over services for newborns; newborn deaths receive less attention than maternal deaths, except for data: “I have not seen newborn cases given attention by supervisors other than requesting data for reporting purposes” (FGD-HC-HCP).
Eliminate user fees for newborn care and postnatal care: “Newborn care should be free of charge; we heard this is the [official] rule but it is not yet implemented at health centers and hospitals, because we don’t have the guideline in written form” (KII-HC-FA).
Discussion
Previous research from low income countries is focused on quantitative assessments of health system readiness to deliver newborn care, but assessments of the quality of newborn care are incomplete in scope.7–9 The quality measures assessed by existing tools relate to input measures and availability of physical resources, and leave important gaps in measuring experience of care.24,25 While there is a broad choice of indicators for monitoring the quality of care, these indicators lack demonstrated validity and may not provide actionable information. They often refer to particular continuum phases and levels within the healthcare system. 26 The consensus is that measurement of performance is essential to support improvement and accountability. However, this has unleashed a multitude of uncoordinated and often duplicative measurement and reporting initiatives. 27 The Commission on High Quality Health Systems has raised more questions than it could answer with existing data. Some of the most pressing are how to comparably measure patient experience and outcomes across primary and secondary care platforms and over time, how to govern and manage systems that prize and reward excellence, and what it will cost to improve and sustain a high quality health system. 28
The WHO framework for quality, equity, and dignity provides a comprehensive scope of standards including appropriate provision and experience of care at each facility level. 10 In December 2020, WHO released standards that identify a set of process indicators for monitoring the quality of care for small and sick newborns at health facilities. 11 The advantage of process indicators is that they are more sensitive to differences in quality of care and they are direct measures of quality. 29 Existing widely-used monitoring tools for measuring quality rely on quantitative methods, dependent on hundreds of indicators, and assess only some of the WHO standards. Qualitative methods for the assessment of processes of care are a practical alternative to qualitative methods for the monitoring of the quality of care in facilities.
Using qualitative methods to collect and analyze data based on the WHO framework 10 we were able to assess provision and experience of care across levels of the Ethiopian primary health care system in 3 regions, and identify actionable interventions. Additionally, flexible qualitative methods allowed us to identify an emergent themes outside the content of the WHO framework: family financial insecurity. This approach revealed perspectives of patients, health care providers and facility administrators to assess what is actually happening in facilities. A better understanding of Ethiopia’s current public health care system as it relates to preterm, LBW, and sick newborns and their parents enables the identification of key intervention areas for this particularly vulnerable group.
Provision of care
Using qualitative methods, this study found that protocols and guidelines for the care of preterm, LBW, and sick newborns were not available in many of the study facilities, and even when available respondents reported they were often not followed. Barriers to parent-newborn unity during inpatient care persist. Most providers reported little or no communication with caregivers following hospital discharge. Human resource challenges such as shortage of skilled staff, motivation and willingness, lack of supervision, and poor leadership inhibited quality of care. In recent assessment of knowledge of providers in Ethiopia, providers scored substantially better on routine intrapartum and newborn care than on care for newborn and maternal complications. 30 The widespread need for competent providers of adequate number to achieve staffing norms to ensure quality newborn care in low- and middle-income countries has been highlighted by WHO and others.31,32 Providers ability to provide quality care is further limited by participants report of widespread shortages of equipment and supplies, medication, physical space, water, electricity, and infrastructure. Previous assessments of the referral system for preterm, LBW and sick newborns have called for a need for government investment in newborn referral systems and standardizing referral communications. 33 Perceptions of quality of provision of care seemed generally congruent across providers and patients.
Experience of care
According to our findings, RDW were prioritized over fathers or other family members in accessing newborns receiving care in facilities, but access was restricted due to space shortages, no parent beds, service disturbance, risk of infection, and no policy promoting unity. The right care needs to be offered at the right time, in the right place, and delivered in a manner that respects, protects, and promotes human rights. Family-centered care should be participatory and respectful; it should provide mothers and fathers with dignity at a time when they are most vulnerable. 34 Some RDW mentioned that staff recognized the importance of counseling and emotional support, providing information to parents to reduce worry. But others said that providers failed to inform parents about the condition of preterm, LBW, and sick newborns and did not provide emotional support. Qualitative case study research in South Africa confirms that positive communication between mothers and providers in neonatal units improves mothers’ parenting confidence and the mother-newborn bond. 35 All health care providers should understand that emotional support is an essential component of the experience of care. 34 Unlike with provision of care, the quality of experience of care showed more varied perceptions between providers and patients. For example, providers and administrators claimed that parents were informed prior to a child receiving a medical procedure but RDWs reported newborns were treated without informed consent. Similarly, while some RDW caring for newborns felt respected by providers, others felt disrespected and had been refused care. Reasons for such disrespect varied from blaming the caregiver parent to provider stress.
Emergent themes
Economic insecurity was a critical factor affecting parents’ experience and access to facility care. Fee structures (based on family ability to pay for newborn care) needed to be developed, tested and implemented to ensure that any charges are affordable to families. Since only 62% of mothers had received antenatal care during their pregnancy and nearly 3-quarters of deliveries occurred at home in 2016, 3 home visits by HEWs to identify preterm, LBW, and sick newborns should be encouraged,
Most preterm, LBW and sick newborns can survive and thrive if they have access to good-quality health care, including admission to a hospital or other health facility when necessary.7,36,37 Health care providers and systems need to monitor and ensure that all newborns receive high-quality, evidence-based, equitable, and respectful care that is safe, well organized, accessible, adequately resourced, efficient, timely, and people-centered.7,10
Limitations
Limitations to the study were as follows: (1) Study sites were located across 3 regions, but cannot be assumed to be representative of the whole country; (2) Participants may not be representative of all clinicians and patients; (3) In Oromia, the geography and isolation of RDW, combined with research resources, prohibited completion of RDW IDIs. Information obtained from interviews regarding guidelines was not verified by observation. We did not assess the actual content of protocols and guidelines; it was beyond the scope of the study and our available resources. These limitations were not likely to have affected the results because we utilized several approaches to ensure scientific rigor: triangulation of method (IDI, FG, KII) and of sample (providers, administrators, RDW; HP, HC, Hospital), employing trained data collectors and checking for data saturation or sufficiency.
Conclusions
Using qualitative methods to collect and analyze data we were able to assess quality of care across levels of the Ethiopian primary health care system in 3 regions, and identify actionable interventions. The quality of care for preterm, LBW, and sick newborns in Ethiopia is compromised, and perceived differently by mothers, health care providers and facility administrators. Improving quality of care requires attention to health system capacity, structure, and resources as well as the experience of care and the processes that deliver care.
This study has gone beyond quantitative indicators by providing qualitative evidence for the need to address key process issues for the delivery of quality mother-newborn health care in Ethiopia. Substantial resources are already dedicated to providing infrastructure, equipment, and skilled human resources to care for preterm newborns in higher-level referral centers in Ethiopia. Further scale-up and development is needed but would require additional investment in infrastructure, equipment, and human resource capacity within these specialized care settings. Strengthening the quality of safe and effective interventions to address preterm birth, LBW, and severe illness remain a priority. An actionable national strategy with dedicated resources to provide high-quality and effective services is needed to improve outcomes.
Acknowledgments
The authors wish to acknowledge the regional health authorities of Oromia Region, Amhara Region, and Addis Ababa, and the mothers, health care providers, and facility administrators without whose cooperation this study would not have been possible. The Every Preemie—SCALE Ethiopia Implementation Research Collaboration Group includes: Hagos Gidey, Mekelle University, Mekelle, Ethiopia; Gillian Levine, Global Alliance to Prevent Prematurity and Stillbirth (GAPPS), Lynnwood, WA, USA; Judith Robb-McCord, Project Concern International, San Diego, CA, USA; Yared Tadesse, Ethiopia Federal Ministry of Health, Addis Ababa, Ethiopia; Abraham Tariku, Ethiopia Federal Ministry of Health, Addis Ababa, Ethiopia; Alemu Tesfahun, Defense University, College of Health Sciences, Ethiopia; Berhe Dessalegn Tuamay, College of Medicine and Health Sciences, Adigrat University, Ethiopia; Abubeker Kedir Usman, Madda Walabu University, Robe, Ethiopia; Abate Yeshidinber Weldetsadik, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia.
Footnotes
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was made possible by the generous support of the American people through the United States Agency for International Development (USAID), under the terms of the Cooperative Agreement AID-OAA-A-14-00049. The contents are the responsibility of the authors and do not necessarily reflect the views of USAID or the United States Government. Support was also provided by the Global Alliance to Prevent Prematurity and Stillbirth (GAPPS) to complete the manuscript and publication process.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf and declare funding support from USAID for the submitted work; authors have no other relationships or activities that could appear to have influenced the submitted work. The funders had no role in the study design, data collection, data analysis, data interpretation, or writing of the report. JL had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Author Contributions: JL conceived of the study. JL and WG were principal investigators. JL, AT, EK were responsible for study design, data collection, coordination. WG and JR assisted with study design. WG assisted with implementation. SJ, JL, KS, TH, AK, KK, EW participated in data analysis, synthesis, interpretation, writing. The Every Preemie—SCALE Ethiopia Implementation Research Collaboration Group members assisted with code book development and data synthesis. All authors read and approved the final manuscript. The authors alone are responsible for the views expressed in this article and they do not necessarily represent the views, decisions, or policies of the institutions with which they are affiliated. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Availability of Data and Materials: No additional data available. The qualitative data, individual stories and narratives have been collected in personal circumstances. Informants were assured that their contribution will remain confidential to the research project and will not be shared.
Ethical Approval and Consent to Participate: Ethics approval was obtained from the Institutional Review Boards of the St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia (IRB No. PM23/111), and Project Concern International (IRB No. 25). Letters of support were secured from all institutions and offices where data were collected. We obtained written consent from potentially eligible and interested participants in their preferred language and informed them that their participation would be voluntary and there would be no professional or personal consequences nor benefits of participation. Mothers were given the option to read or hear their consent form according to their literacy level. To avoid possible coercion, no financial incentives were provided.
ORCID iD: James A Litch  https://orcid.org/0000-0003-0570-0308
https://orcid.org/0000-0003-0570-0308
References
- 1. World Health Organization. Newborns: Improving Survival and Well-Being. Geneva: World Health Organization; 2020. Accessed September 10, 2020. https://www.who.int/news-room/fact-sheets/detail/newborns-reducing-mortality [Google Scholar]
- 2. World Health Organization. Global Health Observatory (GHO) Data 2017. Geneva: World Health Organization; 2017. Accessed 22 January 2020. https://www.who.int/data/gho/data/themes/topics/indicator-groups/indicator-group-details/GHO/causes-of-child-death [Google Scholar]
- 3. Every Preemie—SCALE (Scaling, Catalyzing, Advocating, Learning, and Evidence-Driven). Status of Preterm and Low Birth Weight Demographics, Risk Factors and Health System Responsiveness in USAID’s 24 MCH Priority Countries. Washington, DC: Every Preemie—SCALE; 2019. Accessed March 25, 2020. https://www.everypreemie.org/wp-content/uploads/2019/07/SummaryProfile_7.10.19.pdf [Google Scholar]
- 4. Central Statistical Agency, Federal Democratic Republic of Ethiopia; ICF. Ethiopia Demographic and Health Survey 2016: Key Indicators Report. Addis Ababa, Ethiopia: Central Statistical Agency and ICF; 2016. Accessed March 25, 2020. https://dhsprogram.com/pubs/pdf/FR328/FR328.pdf [Google Scholar]
- 5. Richardson DK, Gray JE, Gortmaker SL, Goldmann DA, Pursley DM, McCormick MC. Declining severity adjusted mortality: evidence of improving neonatal intensive care. Pediatrics. 1998;102:893-899. [DOI] [PubMed] [Google Scholar]
- 6. Doyle LW. Evaluation of neonatal intensive care for extremely-low-birth weight infants. Semin Fetal Neonatal Med. 2006;11:139-145. [DOI] [PubMed] [Google Scholar]
- 7. World Health Organization. WHO Recommendations on Interventions to Improve Preterm Birth Outcomes. Geneva: World Health Organization; 2015. Accessed March 25, 2020. http://apps.who.int/iris/bitstream/handle/10665/183037/9789241508988_eng.pdf?sequence=1 [PubMed] [Google Scholar]
- 8. World Health Organization. Survive and Thrive: Transforming Care for Every Small and Sick Newborn. Key Findings. Geneva: World Health Organization; 2018. Accessed March 25, 2020. https://apps.who.int/iris/bitstream/handle/10665/276655/WHO-FWC-MCA-18.11-eng.pdf?ua=1 [Google Scholar]
- 9. World Health Organization; United Nations Population Fund; United Nations Children’s Fund; Averting Maternal Death and Disability, Columbia University Mailman School of Public Health. Monitoring Emergency Obstetric Care: a Handbook. Geneva: World Health Organization; 2009. Accessed March 25, 2020. https://apps.who.int/iris/bitstream/handle/10665/44121/9789241547734_eng.pdf?sequence=1 [Google Scholar]
- 10. World Health Organization. Standards for Improving Quality of Maternal and Newborn Care in Health Facilities. Geneva: World Health Organization; 2016. Accessed June 5, 2020. https://apps.who.int/iris/bitstream/handle/10665/249155/9789241511216-eng.pdf [Google Scholar]
- 11. World Health Organization. Standards for Improving the Quality of Care for Small and Sick Newborns in Health Facilities. World Health Organization; 2020. Accessed December 22, 2020. https://www.who.int/publications/i/item/9789240010765 [Google Scholar]
- 12. Federal Democratic Republic of Ethiopia Ministry of Health, Ethiopian Hospital Management Initiative. Ethiopian Hospital Services Transformation Guidelines, Volume 1, September 2016. Accessed June 1, 2020. http://repository.iifphc.org/bitstream/handle/123456789/219/Ethiopian%20Hospital%20Services%20Transformation%20Guideline%20Volume%201.pdf?sequence=1&isAllowed=y
- 13. Canavan ME, Brault MA, Tatek D, et al. Maternal and neonatal health services in Ethiopia: measuring and improving quality. Bull World Health Organ. 2017;95:473-477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Brizuela V, Leslie H, Sharma J, Langer A, Tunçalp Ö. Measuring quality of care for all women and newborns: how do we know if we are doing it right? A review of facility assessment tools. Lancet Glob Health. 2019;7:e624-e632. [DOI] [PubMed] [Google Scholar]
- 15. Usman AK, Wolka E, Tadesse Y, et al. ; Every Preemie-SCALE Ethiopia Implementation Research Collaboration Group. Health system readiness to support facilities for care of preterm, low birth weight, and sick newborns in Ethiopia: a qualitative assessment. BMC Health Serv Res. 2019;19:860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Moxon SG, Lawn JE, Dickson KE, et al. Inpatient care of small and sick newborns: a multi-country analysis of health system bottlenecks and potential solutions. BMC Pregnancy Childbirth. 2015;15:S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dickson KE, Simen-Kapeu A, Kinney MV, et al. ; for The Lancet Every Newborn Study Group. Every Newborn: health-systems bottlenecks and strategies to accelerate scale-up in countries. Lancet. 2014;384:438-454. [DOI] [PubMed] [Google Scholar]
- 18. O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89:1245-1251. [DOI] [PubMed] [Google Scholar]
- 19. Population Division, Department of Economic and Social Affairs, United Nations. World Population Prospects: The 2017 Revision. Key Findings and Advance Tables. New York, NY: United Nations; 2017. Accessed March 25, 2020. https://esa.un.org/unpd/wpp/publications/files/wpp2017_keyfindings.pdf [Google Scholar]
- 20. Central Statistical Authority. Population and Housing Census of Ethiopia Administrative Report. Addis Ababa, Ethiopia: Central Statistical Authority; 2012. Accessed June 1, 2020. https://unstats.un.org/unsd/censuskb20/KnowledgebaseArticle10701.aspx [Google Scholar]
- 21. Federal Democratic Republic of Ethiopia Ministry of Health (FMOH). National Human Resources for Health Strategic Plan for Ethiopia 2016-2025. Addis Ababa, Ethiopia: FMOH; 2016. Accessed March 25, 2020. https://pdf.usaid.gov/pdf_docs/PA00TWMW.pdf [Google Scholar]
- 22. Tolley EE, Ulin PR, Mack N, Robinson ET, Succop SM. Qualitative Methods in Public Health: a Field Guide for Applied Research. San Francisco, CA: Jossey-Bass; 2016. [Google Scholar]
- 23. NVivo qualitative data analysis software [computer program]. Version 12; QSR International Pty Ltd.; 2018. [Google Scholar]
- 24. Kawaza K, Kinshella MW, Hiwa T, et al. Assessing quality of newborn care at district facilities in Malawi. BMC Health Serv Res. 2020;20:227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Manu A, Arifeen S, Williams J, et al. Assessment of facility readiness for implementing the WHO/UNICEF standards for improving quality of maternal and newborn care in health facilities - experiences from UNICEF’s implementation in three countries of South Asia and sub-Saharan Africa. BMC Health Serv Res. 2018;18:531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Saturno-Hernández PJ, Martínez-Nicolás I, Moreno-Zegbe E, et al. Indicators for monitoring maternal and neonatal quality care: a systematic review. BMC Pregnancy Childbirth. 2019;19:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Blumenthal D, McGinnis JM. Measuring vital signs: an IOM report on core metrics for health and health care progress. JAMA. 2015;313:1901-1902. [DOI] [PubMed] [Google Scholar]
- 28. Kruk ME, Pate M. The Lancet Global Health Commission on High Quality Health Systems 1 year on: progress on a global imperative. Lancet Glob Health. 2020;8(1):e30-e32. [DOI] [PubMed] [Google Scholar]
- 29. Mandt J. Process versus outcome indicators in the assessment of quality of care. Int J Qual Health Care. 2001;13:475-480. [DOI] [PubMed] [Google Scholar]
- 30. Zemedu TG, Teshome A, Tadesse Y, et al. Healthcare workers’ clinical knowledge on maternal and newborn care in Ethiopia: findings from 2016 national EmONC assessment. BMC Health Serv Res. 2019;19:915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. World Health Organization. Roadmap on Human Resource Strategies to Improve Newborn Care in Health Facilities in Low and Middle-Income Countries. Geneva: World Health Organization; 2020. https://apps.who.int/iris/bitstream/handle/10665/336677/9789240015227eng.pdf?sequence=1&isAllowed=y [Google Scholar]
- 32. Bolan N, Cowgill K, Walker K, et al. Human resources for health-related challenges to ensuring quality newborn care in low- and middle-income countries: a scoping review. Glob Health Sci Prac. 2021;9:160-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Teklu AM, Litch JA, Wolka E, et al. ; Every Preemie-SCALE Ethiopia Implementation Research Collaboration Group. Referral systems for preterm, low birth weight and sick newborns in Ethiopia: a qualitative assessment. BMC Pediatr. 2020;20:409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Durairaj A, Litch JA, Robb-McCord J. Family participation in the care of the inpatient newborn. In Litch JA, Robb-McCord J, Kak L. (eds). Do No Harm Technical Brief Series. Washington DC: USAID; 2018. Accessed March 25, 2020. https://www.everypreemie.org/wp-content/uploads/2018/11/DNH_TechBrief_FamilyParticipation_11.17.18Final.pdf [Google Scholar]
- 35. Horwood C, Haskins L, Luthuli S, McKerrow N. Communication between mothers and health workers is important for quality of newborn care: a qualitative study in neonatal units in district hospitals in South Africa. BMC Pediatr. 2019;19:496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Federal Democratic Republic of Ethiopia Federal Ministry of Health (FMOH), Maternal and Child Health Directorate. National Strategy for Newborn and Child Survival in Ethiopia, 2015/16-2019/20. Addis Ababa, Ethiopia: FMOH; 2015:21-22. Accessed March 25, 2020. https://www.healthynewbornnetwork.org/hnn-content/uploads/nationalstrategy-for-newborn-and-child-survival-in-ethiopia-201516-201920.pdf [Google Scholar]
- 37. World Health Organization. Preterm Birth. Geneva: World Health Organization; 2019. Accessed July 6, 2020. http://www.who.int/mediacentre/factsheets/fs363/en/ [Google Scholar]