ABSTRACT
Objective
The aim of this study was to establish the mobility, satisfaction, and quality of life (QoL) among prosthesis users with dysvascular/diabetic amputation at both acute and long-term phases of prosthetic rehabilitation.
Methods
This is a multisite, cross-sectional outcomes analysis. A total of 341 individuals met the inclusion/exclusion criteria. Individuals were grouped into acute phases (0–3 months [n = 24], 4–6 months [n = 72]) and chronic phases (24–36 months [n = 91], 37–48 months [n = 53], 49–60 months [n = 47], and 60–84 months [n = 54]) after amputation. Mobility was measured with the Prosthetic Limb Users Survey of Mobility (PLUS-M), whereas QoL and satisfaction (Sat) were reported using 10-point scales adapted from the Prosthesis Evaluation Questionnaire–Well-Being (PEQ-WB). Composite PEQ-WB scores were also compared.
Results
The average mobility, QoL, and Sat among prosthesis users was, respectively, 44.8 ± 10.6, 7.6 ± 2.2, and 7.6 ± 2.2. There were no observed differences in mobility (F5,330 = 1.52, P = 0.18), QoL (F5,333 = 0.78, P = 0.57), or PEQ-WB (F5,335 = 1.618, P = 0.155) between any groups. For Sat, there was a group difference (F5,334 = 2.44, P = 0.03) as individuals appear to experience an initial increase in Sat with receipt of a prosthesis (0–3 months) compared with 25 to 36 months (P = 0.005), 49 to 60 months (P = 0.008), and 61 to 84 months (P = 0.009).
Conclusions
Those individuals with amputation secondary to dysvascular disease and diabetes who continue to participate in prosthetic rehabilitation appear to experience levels of mobility, Sat, and QoL 7 years after amputation comparable to that reported in the first 6 months postamputation. There may be a modest increase in Sat with receipt of an initial prosthesis, potentially due to an increased optimism for one's situation. Notably, the mobility levels observed in the dysvascular population through a range of long-term postamputation periods remain within a single standard deviation of the population mean for individuals with a lower-limb amputation using a prosthesis for mobility.
KEY INDEXING TERMS: amputation, quality of life, prostheses, outcomes, mobility, PLUS-M
Irrespective of the cause, amputation brings a dramatic change in the life situation of an individual in almost all aspects of daily living and functioning.1 Although major lower-limb amputation may result from traumatic injury or acute disease processes such as cancer or septic infection, the most common cause in the United States is vascular disease typically with associated diabetes.2–4
Recent articles on the long-term prognosis of those individuals who undergo major lower-limb amputation due to vascular disease and diabetes have emphasized mortality rates. A recent meta-analysis observed aggregated mortality rates of 47.9%, 61.3%, 70.6%, and 62.6% at 1-, 2-, 3-, and 5-year follow-up, respectively.5 A separate systematic review among the same target population reported comparable 5-year mortality rates of 52% to 80%.6 In addition, postamputation surgical revisions, including revisions to more proximal amputations, are frequently indicated.7 Finally, return to ambulation rates are equally concerning with reports varying between 23% and 55% approximately 1 year postamputation.7–11 Yet, clinical experience of prosthetists supports the premise that many individuals with amputations of dysvascular etiology continue to ambulate successfully with a prosthesis for many years, an observation subjectively echoed in the vascular literature.8
Long-term mobility levels among individuals with amputation due to vascular disease have generally been reported in a binary fashion, distinguishing only between those who sustain or lose their ability to walk.8–13 The relative mobility levels of those individuals with dysvascular amputation who sustain their prosthetic rehabilitation over an extended period have not been characterized. Importantly, the term prosthetic rehabilitation refers to the process of restoring loss of function due to amputation through the primary means of a limb prosthesis. The individuals that continue to use a prosthesis throughout their lives will continue to require visits to a rehabilitation professional (i.e., prosthetist) for as long as they choose to utilize a prosthesis. As such, it is appropriate to state that continued prosthesis users are effectively sustaining their prosthetic rehabilitation. The frequency of such visits, however, will depend on the activity level of the individual.
Patients with peripheral vascular disease have been associated with a known reduction in quality of life (QoL).14–17 Similarly, individuals with major limb amputation have reported reduced QoL compared with both the general population and controls.1 As might be expected, individuals who experience major limb amputation due to dysvascular reasons report a poorer QoL than those with amputations associated with trauma or tumor.18 Although prosthetic ambulation has recently been identified as a key factor favorably influencing QoL after dysvascular amputation,1,19 the QoL levels of initial and long-term prosthesis users after dysvascular amputation who engage in and sustain their prosthetic rehabilitation have not been specifically reported.
Rehabilitation of the patient with a lower-limb amputation has traditionally focused on mobility.20–24 However, more recent work has noted the impact of mobility on QoL for the patient with lower-limb amputation.24–29 The largest of these studies recently reported a strong relationship between mobility and QoL in a study of 509 lower-limb prosthesis users.29 That study was inclusive of all causes of amputation but included over 200 individuals with dysvascular etiology.
Importantly, the majority of those studies looking into QoL among individuals with vascular amputations have not focused on the impact of the prosthesis.20,21,26,30 For example, Pell et al.26 used the Nottingham Health Profile to assess QoL, which allows for use of a wheelchair in its mobility assessment and, thus, did not discriminate between wheelchair and prosthesis use. The construct of mobility is clouded for individuals with a lower-limb amputation when responses and data from prosthesis users and wheelchair-only users are combined. The designing and fitting of a custom prosthesis and the physical therapy involved with prosthetic rehabilitation is more complicated than providing a wheelchair. For persons with lower-limb loss due to diabetes or vascular disease, wheelchairs are not typically custom-designed. Given the added effort and expense for providing a prosthesis, it would be valuable to understand long-term changes in mobility and QoL with sustained prosthesis use for patients with a lower-limb amputation.
Thus, the purpose of this study was to begin to characterize the mobility, QoL, and Sat observed in both acute and long-term prosthesis users with lower-limb amputations of dysvascular etiology. It was hypothesized that such outcomes would not differ significantly among lower-limb prosthesis users who have initially been fit and those who have maintained long-term use of a prosthesis after a lower-limb amputation due to vascular or diabetic cause. The PEQ-WB composite score comprising QoL and Sat was secondarily analyzed as it has been validated for use in individuals with lower-limb amputation.
METHODS
STUDY DESIGN
In this study, a multisite review of an outcomes database was performed. Outcomes were previously collected as part of routine standard of care for patients seen at private prosthetic care facilities from April 2016 through November 2017. Outcomes are then further compiled into various databases. This analysis focused on the diabetic/vascular disease database for existing prosthesis users. Patients without any Sat or QoL scores on record were excluded. Patients were divided into groups based on time since amputation, and a retrospective cross-sectional analysis was performed. This retrospective database review was approved by the Western Investigational Review Board (protocol #20170059).
PARTICIPANTS
The inclusion criteria were as follows: 1) unilateral amputation, 2) age 18 years and older, 3) amputation etiology identified as vascular disease/diabetes, 4) time since amputation reported and matched with the specific time groupings used for analysis, 5) able to read and write English or Spanish, and 6) had previously received a prosthesis. Individuals were excluded if they had partial foot amputation, bilateral amputations, or the time since amputation did not fall within the noted periods. Individuals were also excluded if they did not have any element of the Prosthesis Evaluation Questionnaire–Well-Being (PEQ-WB) subsection recorded. There were no inclusion criteria based on specific prosthesis types.
PROCEDURE
As part of the routine standard of care, patients' Sat and QoL were assessed using the PEQ-WB. The PEQ-WB is administered only at specific time points within the patients' episodes of care including evaluations when patient presents for a new prosthesis or replacement of a major component (i.e., socket, knee, foot) and at certain follow-up appointments. The PEQ-WB is a subsection of the longer Prosthesis Evaluation Questionnaire (PEQ). The PEQ as well as its various subsections, including the PEQ-WB, have been validated for use in patients with limb loss.31 The PEQ-WB is designed to assess patient well-being through a combination of questions that ask about patient general Sat with regards to amputation and the patient's QoL over the prior 4 weeks. It was originally published as a continuous visual analog scale. However, for purposes of easier administration, clinics have adopted the modified 10-point ordinal scale version of the PEQ-WB (scale 1–10).29 Previous work has utilized ordinal scale adaptations of the PEQ and shown results consistent with the original visual analog scale.32
In addition to the PEQ-WB, patients with a prosthesis were administered the Prosthetic Limb Users Survey of Mobility (PLUS-M). The PLUS-M is a patient report outcomes instrument developed and validated to specifically assess functional mobility of the lower-limb prosthesis user.33–35 The 12-item PLUS-M comprises 12 different questions about various functional mobility tasks. Individuals respond regarding their difficulty in completing the task varying from “unable to do” to “without any difficulty.” A T-score is generated based on responses, whereby 50 corresponds to the average lower-limb prosthesis users' mobility and ±10 points corresponds to ±1 standard deviation for the population.
Notably, other patient report outcomes instruments were available to assess QoL, Sat, and mobility. In this case, the data were collected as part of the routine standard of care. In the clinical setting, it is critical to balance the additional time needed to complete the outcomes with the risk of impeding clinical workflow. The PEQ-WB and PLUS-M both have short times for administering and scoring the instruments. Subsequently, the use of these instruments resulted in marginal disruption to the clinic workflow and afforded the opportunity for clinicians to score and know their patient's status to aid in their care.
ANALYSIS
After the initial identification of participants that met inclusion/exclusion criteria, individuals were grouped according to time since amputation into both initial and long-term cohorts. The former was subdivided into those individuals 0 to 3 months and 4 to 6 months postamputation, whereas the latter was subdivided into those 24 to 36, 37 to 48, 49 to 60, and 61 to 84 months postamputation. Group means for QoL and Sat scores from the PEQ-WB as well as PEQ-WB composite scores were determined. Similarly, PLUS-M T-scores were used to determine group means for mobility. Group differences were compared using separate general linear univariate models with alpha equal to 0.05. When significant differences were noted, Fisher's LSD post hoc tests were used to determine between group differences.
RESULTS
There were initially 1,231 patient outcomes reviewed for analysis. This ultimately resulted in 341 patients included for final analysis (Table 1, Figure 1). Distribution of amputation levels was generally consistent across groups, with transfemoral amputations accounting for 18% of the total population analyzed (Table 1). However, individuals with transfemoral amputation were underrepresented in those individuals receiving their first prosthesis within the first 3 months after amputation (4%).
Table 1.
Group demographics
| Group | Age (yrs) | Height (cm) | Mass (kg) | Prosthesis Wear Time (hrs/d) | Amputation Level | Time Postamputation (mo) |
|---|---|---|---|---|---|---|
| 0–3 | 57.7 ± 10.3 | 178.4 ± 10.0 | 92.2 ± 25.9 | 6.6 ± 4.5 | 1 TF; 23 TT | 2.6 ± 0.6 |
| 4–6 | 61.9 ± 10.1 | 175.5 ± 10.8 | 90.0 ± 25.5 | 6.6 ± 4.3 | 15 TF; 1 KD; 56 TT | 4.9 ± 0.8 |
| 25–36 | 61.0 ± 11.7 | 172.1 ± 10.5 | 88.1 ± 22.8 | 9.9 ± 5.2 | 19 TF; 1 KD; 71 TT | 30.2 ± 3.2 |
| 37–48 | 64.0 ± 11.6 | 174.2 ± 10.8 | 94.0 ± 25.1 | 11.0 ± 4.4 | 6 TF; 47 TT | 42.5 ± 3.5 |
| 49–60 | 59.2 ± 10.7 | 176.3 ± 11.1 | 95.1 ± 28.7 | 10.2 ± 5.2 | 8 TF; 39 TT | 53.8 ± 3.2 |
| 61–84 | 61.1 ± 13.8 | 173.3 ± 10.4 | 85.3 ± 18.9 | 11.3 ± 4.6 | 10 TF; 44 TT | 71.3 ± 7.4 |
Mean ± S.D. TF indicates transfemoral; KD, knee disarticulation; TT, transtibial.
Figure 1.
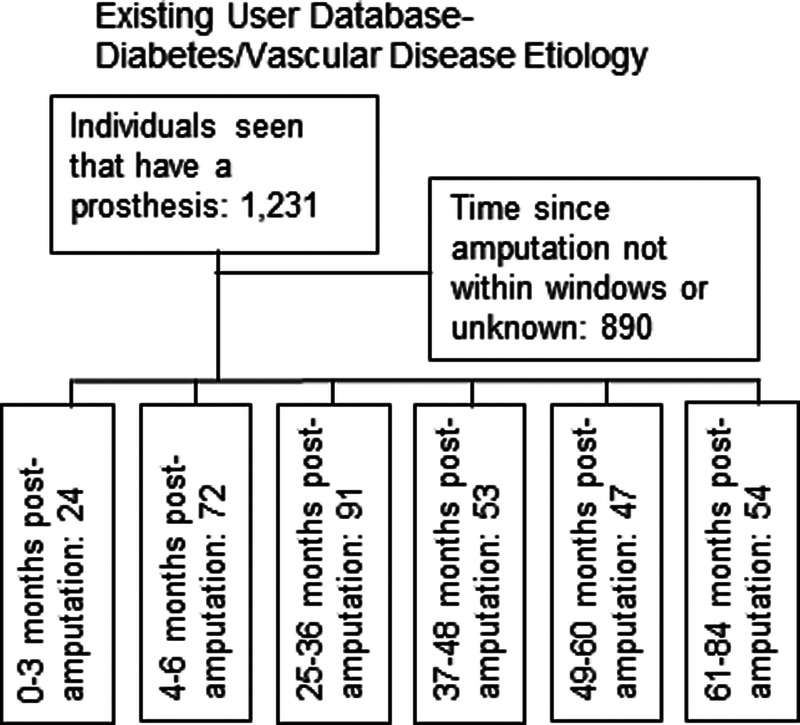
Inclusion process for individuals. There were initially 1,231 patients in the outcomes database. After application of inclusion/exclusion criteria, there were 341 individuals with lower-limb amputation included for analysis.
MOBILITY
When comparing mobility, there were no differences between groups (F5,330 = 1.519, P = 0.183). The average individual group values for mobility ranged from 42.6 ± 1.4 (4–6 months) to 45.3 ± 2.4 (0–3 months) (Figure 2).
Figure 2.
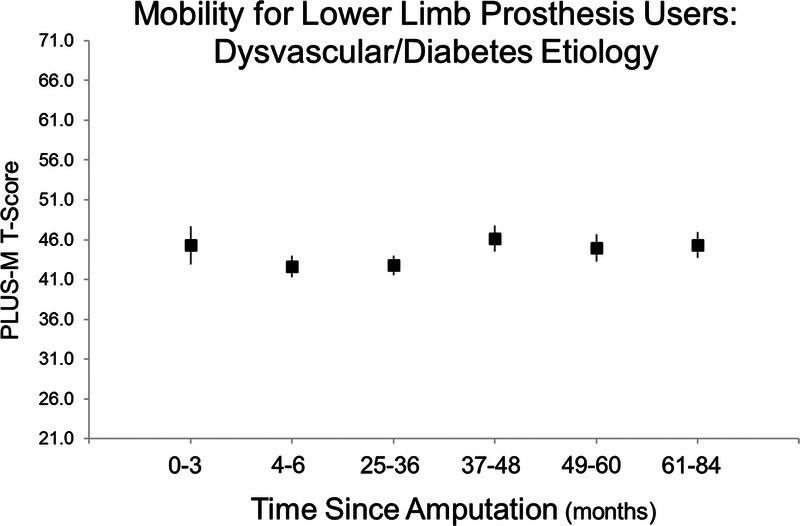
Mobility was analyzed across groups. There were no significant differences across groups, indicating similar mobility for patients that were 6 to 7 years postamputation as those in their first-year postamputation. Mean ± S.E.
QUALITY OF LIFE
There were no significant group differences for QoL (F5,330 = 0.777, P = 0.567). Among acute users of lower-limb prostheses, the highest QoL values were observed among those individuals 0 to 3 months postamputation (mean = 8.0 ± 0.36). Among long-term users of lower-limb prostheses, the highest QoL values were observed among those individuals 61 to 84 months postamputation (mean = 7.7 ± 0.22). These values remained generally constant across all groups of legacy prosthesis users. No significant differences were observed in QoL values for any of the acute or chronic cohorts (Figure 3).v
Figure 3.
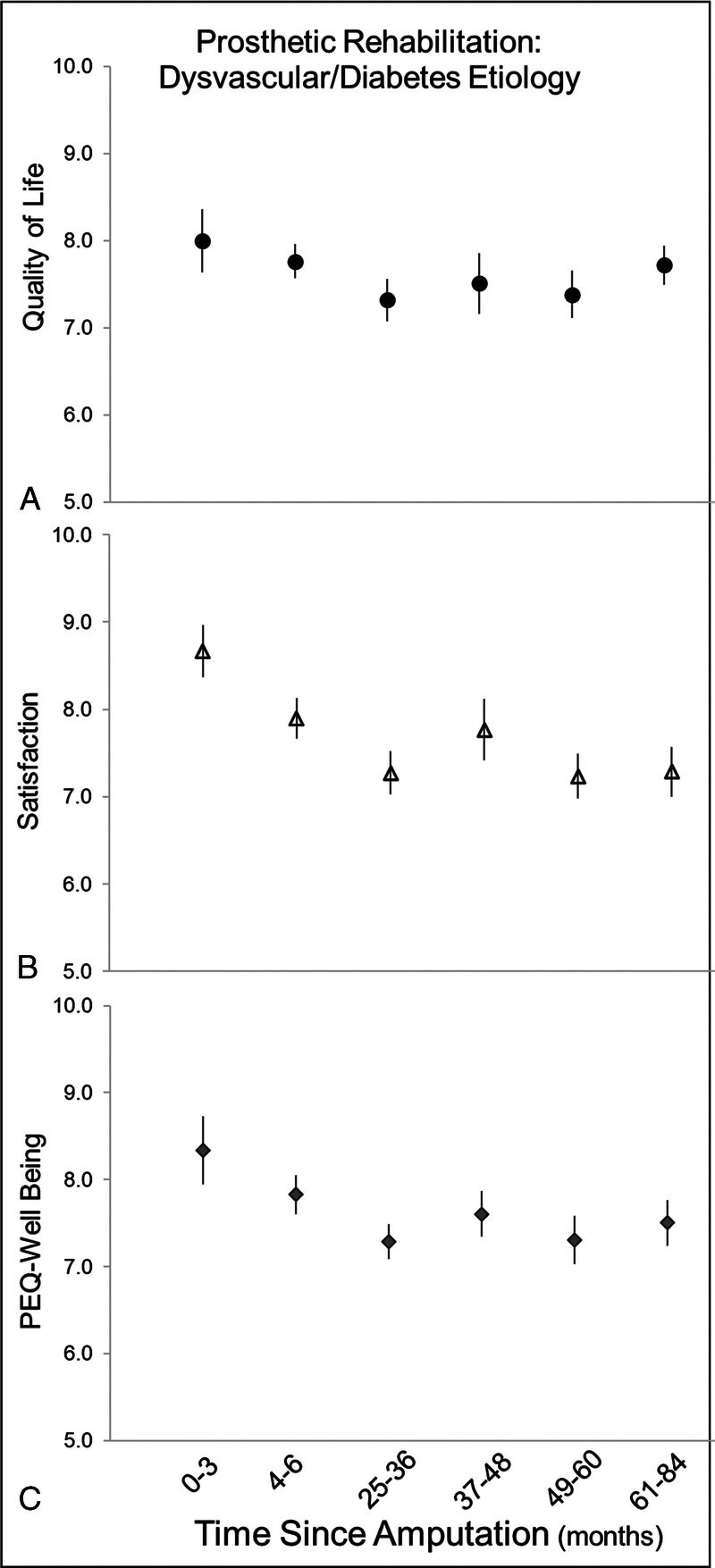
Quality of life, satisfaction, and well-being scores were analyzed across groups at different time points postamputation. Only satisfaction had any differences, with early satisfaction (0–3 months) levels postamputation being inflated, which subsequently led to similar trends in Prosthesis Evaluation Questionnaire–Well-Being (PEQ-WB) composite score, but this was not significant. Mean ± S.E.
SATISFACTION
There was a significant group difference for Sat (F5,334 = 2.443, P = 0.034). The highest mean Sat values were observed among those 0 to 3 months postamputation (8.7 ± 0.30). This value was observed to be significantly higher than Sat values observed in cohorts 25 to 36 months (P = 0.005), 49 to 60 months (P = 0.008), and 61 to 84 months (P = 0.009) postamputation (Figure 3).
WELL-BEING (PEQ-WB COMPOSITE SCORE)
There were no significant group differences for PEQ-WB (F5,335 = 1.618, P = 0.155). Among acute users of lower-limb prostheses, the highest PEQ-WB values were observed among those individuals 0 to 3 months postamputation (mean = 8.3 ± 0.39). Among long-term users of lower-limb prostheses, the highest PEQ-WB values were observed among those individuals 37 to 48 months postamputation (mean = 7.6 ± 0.26). These values remained generally constant across all groups of legacy prosthesis users. No significant differences were observed in PEQ-WB values for any of the acute or chronic cohorts (Figure 3).
DISCUSSION
To the extent that prosthetic mobility among survivors of major dysvascular amputations has been reported, it has largely been done in a binary fashion between those that either do or do not utilize a prosthesis,8–13 with occasional attempts to further classify mobility as either indoor or outdoor.7 This effort represents the first attempt to further characterize the mobility of this population. The mean PLUS-M T-score observed in this population, 44.5, is consistent with mobility at the 30th percentile of all lower-limb prosthesis users36 and within 1 standard deviation of the average mobility reported by all lower-limb prosthesis users. Coupled with mean daily prosthesis wear times of 10 to 11 hrs, these scores suggest regular meaningful daily ambulation within this targeted cohort. This observation stands in contrast to the common perception that individuals with dysvascular amputation can be expected to display a fairly quick decline in mobility.
QoL and the related construct of Sat have been measured among prosthesis users using a broad range of outcomes measures, making it difficult to compare QoL across clinical trials and publications.1,19 However, systematic review has generally characterized QoL among individuals with acquired amputations as “poor.”1,19 In contrast, the current analysis, in which QoL was assessed using a 10-point Likert scale where 10 suggests the “Best Life Possible,” observed a mean QoL value of 7.6. Similarly, using a 10-point Likert scale to assess Sat, in which a score of 10 suggests “Extremely Satisfied,” patients identified a mean Sat value of 7.6. Interestingly, the initial reported QoL and Sat is the highest after amputation. This may be reflective of the common anecdotal feelings from patients that have undergone numerous limb salvage procedures that they wish the decision to amputate would have been sooner, and hence amputation and receipt of a prosthesis has come with new optimism for their current state. As a result, it may be worth rethinking much of the literature that denotes “poor” QoL; recognizing this may be a limitation of heterogeneity of samples blending individuals with a prosthesis and those without.
Furthermore, this disparity may originate in part between the range of measures used to report QoL and Sat in disparate publications; the role of sustained utilization of a prosthesis may contribute to the uncharacteristically high QoL and Sat values observed in our review. In their systematic review of major lower-limb amputations across all etiologies, Sinha et al.1 identified limitations in physical functioning as a meaningful factor negatively affecting QoL for individuals with amputation in general and, in particular, those with amputation due to vascular disease. Similarly, in their systematic review of QoL after amputation for peripheral arterial occlusive disease, Davie-Smith et al.19 identified walking with a prosthesis as the most notable factor that influenced QoL. It was suggested that even small amounts of walking resulted in improved QoL compared with complete nonambulation, and in addition to the immediate benefits of physical fitness, further benefits may derive from the positive influences encountered with associated social interactions.19
In a similar manner, Norvell et al.24 reported upon the relationships between mobility and Sat in a cohort of 87 subjects undergoing major lower-limb amputation due to complications of peripheral vascular disease and diabetes. Tracking their subjects' premorbid mobility and 12-month postamputation mobility using the Locomotor Capabilities Index (LCI), the authors defined “mobility success” as those individuals who ultimately returned to their premorbid mobility levels. Sat was assessed using the Satisfaction With Life Scale (SWLS). Authors reported that the 28 subjects who obtained “mobility success” at their 12-month follow-up reported a satisfaction with life rate 28% higher than those who did not, and that satisfaction with life was significantly associated with the LCI score observed at 12-month follow-up.24
Although proximal amputation levels have been identified as predictive of both decreased mobility and QoL,7–10,19 it should be noted that subjects with transfemoral amputations accounted for just under 20% of the current study's sample of individuals who have sustained prosthetic rehabilitation 2 to 7 years after amputation. Further work is needed to confirm that successful prosthetic rehabilitation is not limited to distal amputation levels.
There are limitations to this analysis that should be considered. First, there is sampling bias associated with a convenience sample of patients presenting for follow-up care at a prosthetic clinic. Those patients that may have abandoned their prosthesis or died prior to the targeted time window of 2 to 7 years postamputation were not included. However, the intent of the current analysis was not to track the longitudinal outcomes of individuals within this population but to provide a cross-sectional analysis of the mobility, QoL, and Sat reported by those individuals who are able to sustain their prosthetic rehabilitation and compare these values against those observed during the acute phase of prosthetic rehabilitation. In addition, the decision was made to omit a small number of individuals that did not complete QoL and Sat, which may have created bias if such individuals were either those that were quite low on the scale or those that were very high on the scale. This percentage of individuals (~1%), however, was considered small enough that the impact to the analysis would be minimal.
The results underline the value of sustained utilization of a prosthesis. Not only do individuals with a prosthesis continue to experience elevated QoL and Sat values, but their use of a prosthesis and continued mobility may contribute to their ability to continue to thrive in light of the elevated mortality rates observed in this population.5,37–39 Chopra et al.9 reported a 15% lower 1-year survival rate among nonambulatory patients after major lower-limb amputations, and Stern et al.5 concluded that nonambulatory status was associated with a greater than 2-fold increased mortality rate after lower-limb amputation.
Our results suggest sustained mobility, QoL, and Sat as long as 6 to 7 years after amputation is possible among those individuals who maintain prosthetic rehabilitation after dysvascular amputation. Similar results were found for the PEQ-WB composite score. These findings highlight the value of continued prosthetic rehabilitation into the postamputation care plan.
CONCLUSIONS
The results from the current study demonstrate high levels of QoL, satisfaction, and sustained mobility for those that remained actively engaged in prosthetic rehabilitation as far out as 7 years postamputation due to vascular disease/diabetes. Although patients experience an initial spike in satisfaction within the first 3 months, this satisfaction declines within 4 to 6 months and is then fairly consistent. Most surprising is the understanding that, among those individuals with amputation that did remain engaged in prosthetic rehabilitation, mobility levels in those as far as 7 years postamputation were still within 1 standard deviation of the overall lower-limb prosthesis users' average mobility. Future efforts are needed to understand within the larger aggregate of diabetic/dysvascular prosthesis users if certain care plans (i.e., prosthetic design and management, prosthetic education, physical therapy treatment, etc.) lend themselves to higher levels of QoL, satisfaction, and mobility.
Footnotes
Disclosure: The authors declare no conflict of interest.
Funding/Support: Support for this work was partially provided by a Small Grant Award (EB-043016) from the American Orthotics and Prosthetics Association.
Contributor Information
Shane R. Wurdeman, Email: shanewurdeman@gmail.com.
Phillip M. Stevens, Email: pstevens@hanger.com.
James H. Campbell, Email: jhcampbell@hanger.com.
REFERENCES
- 1.Sinha R, Van Den Heuvel WJ. A systematic literature review of quality of life in lower limb amputees. Disabil Rehabil 2011;33(11):883–899. [DOI] [PubMed] [Google Scholar]
- 2.Ziegler-Graham K MacKenzie EJ Ephraim PL, et al. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil 2008;89(3):422–429. [DOI] [PubMed] [Google Scholar]
- 3.Ephraim PL Dillingham TR Sector M, et al. Epidemiology of limb loss and congenital limb deficiency: a review of the literature. Arch Phys Med Rehabil 2003;84(5):747–761. [DOI] [PubMed] [Google Scholar]
- 4.Dillingham TR, Pezzin LE, MacKenzie EJ. Limb amputation and limb deficiency: epidemiology and recent trends in the United States. South Med J 2002;95(8):875–883. [DOI] [PubMed] [Google Scholar]
- 5.Stern JR Wong CK Yerovinkina M, et al. A meta-analysis of long-term mortality and associated risk factors following lower extremity amputation. Ann Vasc Surg 2017;42:322–327. [DOI] [PubMed] [Google Scholar]
- 6.Thorud JC, Seidel JL. A closer look at mortality after lower extremity amputation. Podiatry Today 2018;31(4):12–16. [Google Scholar]
- 7.Nehler MR Coll JR Hiatt WR, et al. Functional outcome in a contemporary series of major lower extremity amputations. J Vasc Surg 2003;38(1):7–14. [DOI] [PubMed] [Google Scholar]
- 8.Taylor SM Kalbaugh CA Blackhurst DW, et al. Preoperative clinical factors predict postoperative functional outcomes after major lower limb amputation: an analysis of 553 consecutive patients. J Vasc Surg 2005;42(2):227–235. [DOI] [PubMed] [Google Scholar]
- 9.Chopra A Azarbal AF Jung E, et al. Ambulation and functional outcome after major lower extremity amputation. J Vasc Surg 2018;67(5):1521–1529. [DOI] [PubMed] [Google Scholar]
- 10.Toursarkissian B Shireman PK Harrison A, et al. Major lower-extremity amputation: contemporary experience in a single veterans affairs institution. Am Surg 2002;68(7):606–610. [PubMed] [Google Scholar]
- 11.Remes L Isoaho R Vahlberg T, et al. Predictors for institutionalization and prosthetic ambulation after major lower extremity amputation during an eight-year follow-up. Aging Clin Exp Res 2009;21(2):129–135. [DOI] [PubMed] [Google Scholar]
- 12.Stone PA, Flaherty SK, Hayes JD, AbuRahma AF. Lower extremity amputation: a contemporary series. W V Med J 2007;103(5):14–18. [PubMed] [Google Scholar]
- 13.Cruz CP Eidt JF Capps C, et al. Major lower extremity amputations at a veterans affairs hospital. Am J Surg 2003;186(5):449–454. [DOI] [PubMed] [Google Scholar]
- 14.Liles DR, Kallen MA, Petersen LA, Bush RL. Quality of life and peripheral arterial disease. J Surg Res 2006;136(2):294–301. [DOI] [PubMed] [Google Scholar]
- 15.Regensteiner JG Hiatt WR Coll JR, et al. The impact of peripheral arterial disease on health-related quality of life in the peripheral arterial disease awareness, risk, and treatment: new resources for survival (PARTNERS) program. Vasc Med 2008;13(1):15–24. [DOI] [PubMed] [Google Scholar]
- 16.Nehler MR McDermott MM Treat-Jacobson D, et al. Functional outcomes and quality of life in peripheral arterial disease: current status. Vasc Med 2003;8(2):115–126. [DOI] [PubMed] [Google Scholar]
- 17.Myers SA Johanning JM Stergiou N, et al. Claudication distances and the walking impairment questionnaire best describe the ambulatory limitations in patients with symptomatic peripheral arterial disease. J Vasc Surg 2008;47(3):550–555. [DOI] [PubMed] [Google Scholar]
- 18.Pernot HF, Winnubst GM, Cluitmans JJ, De Witte LP. Amputees in Limburg: incidence, morbidity and mortality, prosthetic supply, care utilisation and functional level after one year. Prosthet Orthot Int 2000;24(2):90–96. [DOI] [PubMed] [Google Scholar]
- 19.Davie-Smith F Coulter E Kennon B, et al. Factors influencing quality of life following lower limb amputation for peripheral arterial occlusive disease: a systematic review of the literature. Prosthet Orthot Int 2017;41(6):537–547. [DOI] [PubMed] [Google Scholar]
- 20.Francis W, Renton CJ. Mobility after major limb amputation for arterial occlusive disease. Prosthet Orthot Int 1987;11:85–89. [DOI] [PubMed] [Google Scholar]
- 21.Finch DR, MacDougal M, Tibbs DJ, Morris PJ. Amputation for vascular disease: the experience of a peripheral vascular unit. Br J Surg 1980;67:233–237. [DOI] [PubMed] [Google Scholar]
- 22.Barnes RW, Shanik GD, Slaymaker EE. An index of healing in below-knee amputation: leg blood pressure by doppler ultrasound. Surgery 1976;79:13–20. [PubMed] [Google Scholar]
- 23.Jamieson MG, Ruckley CV. Amputation for peripheral vascular disease in a general surgical unit. J R Coll Surg Edinb 1983;28:46–50. [PubMed] [Google Scholar]
- 24.Norvell DC Turner AP Williams RM, et al. Defining successful mobility after lower extremity amputation for complications of peripheral vascular disease and diabetes. J Vasc Surg 2011;54(2):412–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Suckow BD Goodney PP Nolan BW, et al. Domains that determine quality of life in vascular amputees. Ann Vasc Surg 2015;29(4):722–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pell JP, Donnan PT, Fowkes FG, Ruckley CV. Quality of life following lower limb amputation for peripheral arterial disease. Eur J Vasc Surg 1993;7(4):448–451. [DOI] [PubMed] [Google Scholar]
- 27.Asano M, Rushton P, Miller WC, Deathe BA. Predictors of quality of life among individuals who have a lower limb amputation. Prosthet Orthot Int 2008;32(2):231–243. [DOI] [PubMed] [Google Scholar]
- 28.Davies B, Datta D. Mobility outcome following unilateral lower limb amputation. Prosthet Orthot Int 2003;27(3):186–190. [DOI] [PubMed] [Google Scholar]
- 29.Wurdeman SR, Stevens PM, Campbell JH. Mobility analysis of AmpuTees (MAAT 1): quality of life and satisfaction are strongly related to mobility for patients with a lower limb prosthesis. Prosthet Orthot Int 2018;42(5):498–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zidarov D, Swaine B, Gauthier-Gagnon C. Quality of life of persons with lower-limb amputation during rehabilitation and at 3-month follow-up. Arch Phys Med Rehabil 2009;90(4):634–645. [DOI] [PubMed] [Google Scholar]
- 31.Legro MW Reiber GD Smith DG, et al. Prosthesis Evaluation Questionnaire for persons with lower limb amputations: assessing prosthesis-related quality of life. Arch Phys Med Rehabil 1998;79(8):931–938. [DOI] [PubMed] [Google Scholar]
- 32.Franchignoni F Giordano A Ferriero G, et al. Measuring mobility in people with lower limb amputation: Rasch analysis of the mobility section of the Prosthesis Evaluation Questionnaire. J Rehabil Med 2007;39(2):138–144. [DOI] [PubMed] [Google Scholar]
- 33.Hafner BJ Gaunaurd IA Morgan SJ, et al. Construct validity of the prosthetic limb users survey of mobility (PLUS-M) in adults with lower limb amputation. Arch Phys Med Rehabil 2017;98(2):277–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hafner BJ, Morgan SJ, Askew RL, Salem R. Psychometric evaluation of self-report outcome measures for prosthetic applications. J Rehabil Res Dev 2016;53(6):797–812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hafner BJ, Morgan SJ, Abrahamson DC, Amtmann D. Characterizing mobility from the prosthetic limb user's perspective: use of focus groups to guide development of the prosthetic limb users survey of mobility. Prosthet Orthot Int 2016;40(5):582–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.UWCORR . Prosthetic limb user survey. Prosthetic limb users survey web site. Available at: www.plus-m.org. Updated 2013. Accessed December 2016.
- 37.Aulivola B Hile CN Hamdan AD, et al. Major lower extremity amputation: outcome of a modern series. Arch Surg 2004;139(4):395–399. [DOI] [PubMed] [Google Scholar]
- 38.Feinglass J Pearce WH Martin GJ, et al. Postoperative and late survival outcomes after major amputation: findings from the department of veterans affairs national surgical quality improvement program. Surgery 2001;130(1):21–29. [DOI] [PubMed] [Google Scholar]
- 39.Brown BJ, Attinger CE. The below-knee amputation: to amputate or palliate? Adv Wound Care 2013;2(1):30–35. [DOI] [PMC free article] [PubMed] [Google Scholar]


