Supplemental digital content is available in the text.
ABSTRACT
SIGNIFICANCE
A recent trend in low vision rehabilitation has been the use of portable head-mounted displays to enhance residual vision. Our study confirms the feasibility of telerehabilitation and informs the development of evidence-based recommendations to improve telerehabilitation interventions to reduce device abandonment.
PURPOSE
To develop evidence-based recommendations for telerehabilitation, we conducted a feasibility study in preparation for a future randomized trial on the use of head-mounted displays.
METHODS
We recruited novice eSight Eyewear users, randomized 1:1: the experimental group received telerehabilitation by a low vision therapist using video conferencing; the control group completed at home self-training provided by the device manufacturer. The primary feasibility outcomes were whether the recruitment goal of 60 participants (30/group) was attainable within 1 year and how participants judged the accessibility and acceptability of the telerehabilitation. An exploratory outcome was the impact of telerehabilitation on eSight Eyewear use behavior.
RESULTS
Among 333 eSight users, 57 participants were enrolled, of which 35% withdrew from the study, whereas the remainder completed the 6-month follow-up. The withdrawal rate was higher in the control group but did not differ significantly from the experimental group. High accessibility (93% of participants accessed the platform) and global acceptability (100% overall satisfaction) were reported among those who completed the telerehabilitation protocol. The therapist had no difficulty judging the participants' reading performances qualitatively while participants used their device to read their eSkills and VisExc guides. Most participants improved their daily activities, based on qualitative reports of the attained goals. Seventy-nine percent of individuals declined to participate, whereas 16% of participants decided not to use eSight Eyewear anymore.
CONCLUSIONS
The data demonstrated the feasibility of a randomized controlled telerehabilitation study for people with low vision using a head-mounted display. Positive feedback from the participants and the therapist suggests the potential value of this modality for low vision services.

Worldwide, around 314 million people have a visual impairment.1 This is a public health concern that is likely to expand as the population of older adults increases. Visual impairment is globally prevalent across the lifespan and includes blindness and low vision. Low vision is defined as a partial visual impairment that is not correctable with glasses, contact lenses, or surgical interventions and interferes with normal everyday functioning.2 Low vision rehabilitation is the primary intervention for individuals with reduced visual function to improve independence in activities of daily living and quality of life by enhancing their remaining sight.3 The most common form of intervention in low vision rehabilitation is the provision of, and training in, the use of visual aids, such as optical and electronic magnification devices, including handheld magnifiers and close-circuit televisions.4
A recent development in low vision rehabilitation has been toward the use of wearable head-mounted displays that are immersive systems (e.g., virtual reality) providing hands-free magnification and contrast enhancements at all distances, using optoelectronics and real-time video technology.5 One of the first head-mounted displays, the Low Vision Enhancement System, demonstrated positive vision outcomes, improving visual acuity and contrast sensitivity.6,7 Benefitting from major technological evolution, head-mounted display performance has been compared with traditional optical visual aids and demonstrated positive outcomes.8 Continuing this trend, a new head-mounted display, eSight Eyewear (eSight Corp., Toronto, Ontario, Canada), was designed to improve on previous devices by not only providing adjustable magnification, autofocus, contrast enhancement, hands-free use, and portability but also offering the user approximately 30° of field of view through digital image processing.9 A multicenter prospective trial demonstrated improvement in visual ability including activities of daily living and reading in 51 novice users followed up for 3 months.9
Despite the functional and evidence-based benefits of magnifying low vision aid use,10 rates of device nonuse are highly variable.11 A cross-sectional study revealed that of 109 eSight Eyewear users, 17.4% (n = 19) did not use their device in the past 3 months.12 The reasons for nonuse had been identified as multifactorial, involving the device, the user, the environment, and the intervention. The costs associated with the device as well as the low vision examination and low motivation of the patient to undergo a low vision examination13 were identified as important barriers.11
In addition, limited access to transportation to receive training with a device11,14 and insufficient training duration and frequency were also reported as predictors of low vision aid abandonment.11 This is particularly a challenge given the paucity of specialty low vision clinics, thereby considerably affecting the access to care in rural areas of geographically dispersed countries, such as the United States and Canada.15,16
In recent years, telerehabilitation has become a viable alternative for delivering rehabilitation services, allowing individuals to remain at home while interacting with a rehabilitation professional via the Internet.17 A systematic review of telerehabilitation across disabilities revealed that most of the interventions were successful,18 thereby contributing to evidence-based practice recommendations toward its implementation. In the context of low vision, a Cochrane systematic review documented very few applications and no published outcomes.19 Since then, a pilot study confirmed the feasibility and acceptability of training to optimize the use of handheld magnifiers in 10 individuals via telerehabilitation.20
Given the absence of randomized controlled studies and to help guide evidence-based practice recommendations for this modality, the present feasibility study was conducted. The primary objective was to determine whether telerehabilitation with participants with low vision using their eSight Eyewear would be feasible. Specifically, we asked whether 1 year would be sufficient to recruit the required number of participants, what proportion of participants would be lost to follow-up, and whether participants would judge the intervention as accessible and acceptable. Our secondary objective was to determine if personalized intervention through telerehabilitation would be able to reduce discontinuance of head-mounted display use.
METHODS
Study Design
Following the CONSORT guidelines,21 this parallel two-arm randomized feasibility study consisted of training individuals with low vision in the use of eSight Eyewear when engaging in activities of daily living. The participants were enrolled through the School of Optometry of the Université de Montréal, Montreal, Quebec, Canada. The protocol has previously been published in detail,22 was approved by the institutional review board of the Centre de recherche interdisciplinaire en réadaptation du Montréal métropolitain (CRIR No. 1286-1217), and complied with the ethical standards for research with human participants defined by the Declaration of Helsinki.
Sample Size and Participant Eligibility Criteria
Through eSight Corporation, we recruited novice users aged 18+ years who had a tablet, desktop, or laptop computer with Internet access and recently bought (<1 month) or were renting eSight Eyewear. The eligible rental period offered by the device manufacturer was 2 weeks. At the end of the rental period, renters had the possibility to either purchase (keep their current device) or return their device to the manufacturer. Detailed exclusion criteria are available in the detailed protocol publication.22 Fig. 1 summarizes the design of the study with each aspect described hereinafter.
FIGURE 1.
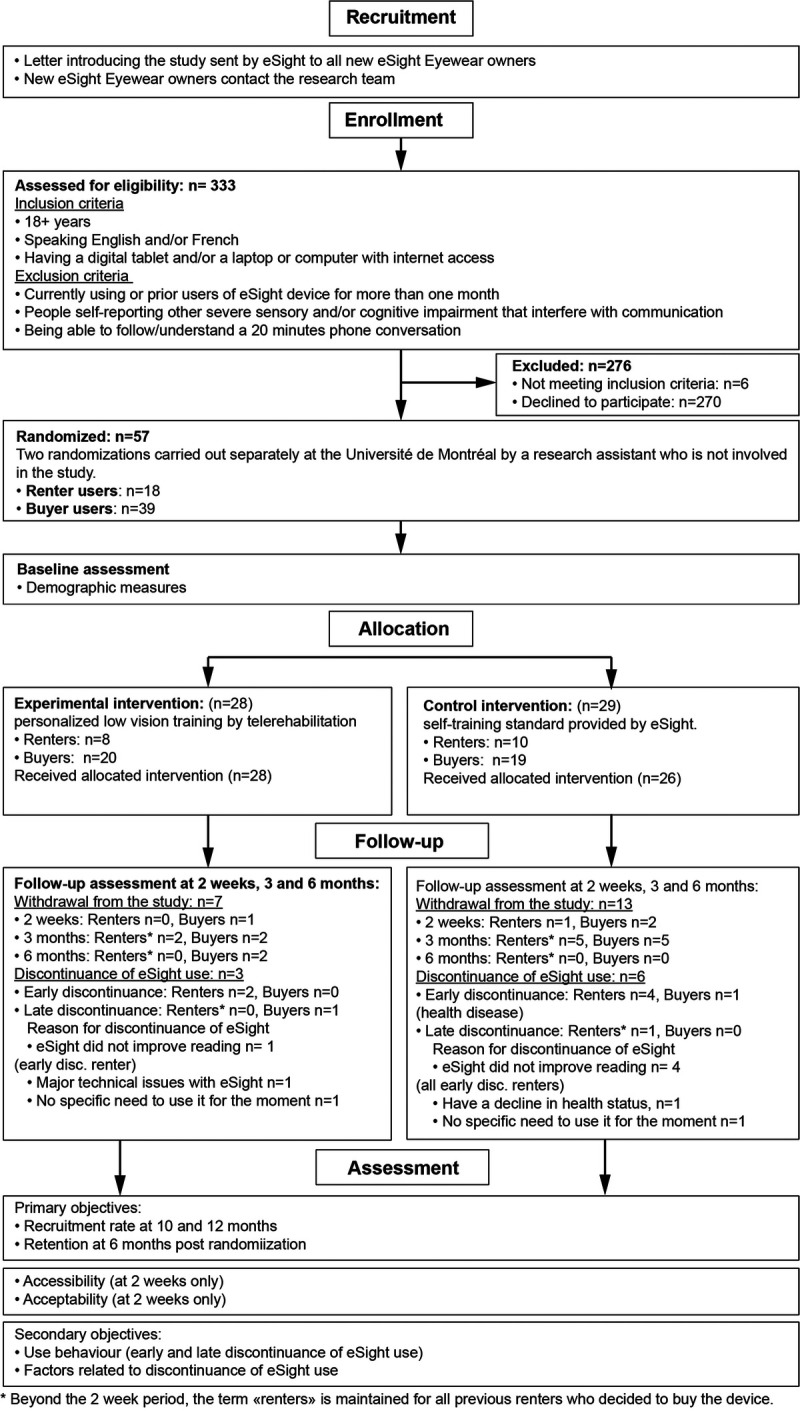
Chart showing participant flow. Design of the study with each of the following aspects: recruitment, enrollment, allocation with intervention types, evaluation timeline, and primary and secondary outcomes.
Interventions
Participants were randomized (1:1 ratio) into the control and experimental groups to each receive 30 hours of training for 1 month. The detailed interventions are described in the protocol publication.22 Briefly, the control group received a self-training standard provided by eSight, including the eSkills learning and training guide,23 which is provided when purchasing the device. This guide is a self-administered program that spans 1 hour per day for 1 month (30 hours) to be performed self-guided at home and is divided into 4 consecutive weeks of exercises. The experimental group received personalized training through telerehabilitation provided by a low vision therapist using the eSkills learning and training guide23 and digitized exercises extracted from the VisExc eccentric fixation program24 (partially adapted from the McGill Low Vision Manual25). The personalized training consisted of six 1-hour online training sessions within the first 2 weeks (6 hours), 12 additional hours of homework in parallel during the same 2 weeks, and an additional 12 hours of homework in the following 2 weeks. At the end of their respective training, the participants continued to use the device in their environment until the end of the study 5 months later (and beyond).
Outcomes
Primary Outcomes
The primary outcome was the feasibility of telerehabilitation: (1) enrollment target (signed consent) within 12 months, (2) retention of participants until 6 months after randomization, (3) accessibility of telerehabilitation training, and (4) acceptability of telerehabilitation training.
Our enrollment target was 60 participants with 30 individuals in each group (a sample size comparable to other feasibility studies in low vision rehabilitation26) for 12 months, with a success criterion of n = 60 (100%). Given the proposed recruitment period, this sample size allowed for the evaluation of any possible limitations with enrollment and retention more robustly and provided rich data on accessibility and acceptability of telerehabilitation training. We recorded the number of eligible individuals declining to participate and why and captured whether any participants withdrew from the study and why. Retention was monitored by follow-up evaluations and through questionnaires including individual questions specifically developed for the study to measure the number of participants who withdrew from the study. Accessibility of the training by telerehabilitation was determined from the report of any problems related to Internet connectivity, access to the Reacts telehealth platform (https://www.iitreacts.com), use of the hardware, and audio/visual quality. We used the secured React telehealth platform in its simplest basic form of Skype/FaceTime-like session to make navigation as easy as possible for both the clinician and participants. At the time of the study, the eSight device did not allow the clinician to also visualize what the participants are seeing through their display. Regarding acceptability, participants of the experimental group completed a satisfaction survey with a research assistant, whereby they were asked to rate the experience of telerehabilitation for comfort, efficiency, effectiveness, likelihood for future use, and overall satisfaction rated on a 4-point Likert scale (strongly agree, somewhat agree, somewhat disagree, and strongly disagree). The low vision therapist was asked to use a rating scale (no difficulty, little difficulty, moderate difficulty, and impossible) to indicate the difficulty with using the videoconference portal to clinically and qualitatively estimate the participants' working distance (i.e., distance participants are from their intended viewing object such as reading material) and lighting environment while using their eSight device and to quantify their reading fluency (i.e., speed, accuracy) using shared reading materials, as well as her impressions of the effect of both the eSkills guide and/or the VisExc program on participants (estimate of goals reached for each participant ranged from completely to not at all). The low vision therapist and participants shared common work materials composed of exercises that they could easily refer to: the eSkills learning and training guide23 and digitized exercises extracted from the VisExc eccentric fixation program24 (partially adapted from the McGill Low Vision Manual25), as detailed in the published protocol.22 Overall, common exercises of the eSkills were performed by both the control and the experimental groups. However, the VisExc program was performed by the experimental group exclusively. Participants who received telerehabilitation received assistance from the low vision therapist by telephone if needed. In addition, we noted who received assistance from a friend or family member during some of the training sessions.
Secondary Outcomes
We assessed the effect of telerehabilitation on eSight device use behavior (discontinuance rate) at two different times. Early discontinuance was defined as when a participant stopped using the device during the first 2 weeks of the study (either a renter who decided not to buy the device at the end of the rental period or a buyer who decided not to use it anymore). We defined late discontinuance as when a participant reported complete nonuse of the device in the previous 3 months, a period commonly used in previous research.27 The tasks were recorded using 94 open and closed questions adopted from and including the items of the Psychosocial Impact of Assistive Devices Scale28 and the Quebec User Evaluation of Satisfaction with Assistive Technology29 (see additional analyses of these measures in our parallel study30) and questions specifically developed for this study about a device user's characteristics and changes in use.22 The questionnaires were administered at baseline by the low vision therapist and self-administered through a URL link at 2 weeks and 3 and 6 months after randomization.
Statistical Analyses
Statistical analyses were conducted using JASP version 0.9 software (Eric-Jan Wagenmakers, University of Amsterdam, Amsterdam, Netherlands).31 In step 1, descriptive statistics were used to present the sample and responses on all outcome measures. In step 2, enrollment was analyzed using the 1-year period of recruitment reporting the number of participants assessed for eligibility and the number of participants who were excluded (number of participants declining to participate and number of participants not meeting the inclusion criteria). Retention in both the experimental and the control groups was analyzed at 2 weeks, as well as 3 and 6 months, using the number of participants remaining in the study. If participants wished to withdraw after they had been allocated to an intervention group, we gave them the opportunity to explain their reasoning, should they be interested in sharing these reasons. Variables assessing accessibility of telerehabilitation training (numbers and types of issues with Internet connectivity, access to the videoconference platform, use of the hardware, and audio/visual quality) were presented as frequency counts. Acceptability was measured using ordinal data from a satisfaction survey and descriptive statistics. In step 3, early and late discontinuance rates were analyzed using descriptive statistics. We decided to analyze data from the renters and the buyers separately and also to differentiate early and late device discontinuance because of the eSight buyer/renter policy.
RESULTS
Recruitment
Recruitment took place from June 2018 to June 2019. The participant flow is shown in Fig. 1. A total of 333 eSight users were assessed for eligibility and approached by eSight Corporation. Then, the study team contacted all of the 333 eSight users by telephone to confirm eligibility and whether they accepted or declined to participate in the study. The recruitment efforts occurred gradually over time. Of these, 270 declined to participate, and 6 did not meet the inclusion criteria (1 did not speak English and or French, 2 were younger than 18 years, 2 had poor general health, 1 had cognitive issues interfering with communication).
Baseline Characteristics
The mean (standard deviation) age of the participants was 54.5 (16.7) years (range, 21 to 82 years; see Table 1 for group-specific details). Participant characteristics at randomization are summarized in Tables 1 and 2 and show comparable demographic and descriptive variables in both groups, albeit with retired participants' preponderance in the control-renter subgroup (Table 1) and a male majority in the control group. Participants completing the trial had a range of ocular pathologies, with optic nerve dystrophies and central degenerations being the most common (Table 3). The 20 individuals who withdrew from the study (lost during the follow-up period) did not differ statistically on any of the demographic measures from those who completed the follow-up period (Table 4). The nine individuals who reported not using their eSight Eyewear anymore (both early and late discontinuance) did not differ statistically on any of the demographic measures (statistically comparable, given the frequency distribution of the data) from those with complete data, with the exception of their distribution across their country of residence: more Canadians reported to not use their device anymore after the initial assessment (five from Canada vs. four from the United States), whereas the user pool contained more Americans (41 from the United States vs. 7 from Canada; χ21 [n = 57] = 7.66, P < .01; Table 5).
TABLE 1.
Participant characteristics
| Control buyers (n = 19) | Control renters (n = 10) | Experimental buyers (n = 20) | Experimental renters (n = 8) | |
|---|---|---|---|---|
| Age (y), mean (SD) | 55.5 (11.7) | 61.4 (12.9) | 50.3 (21.0) | 54.1 (18.9) |
| Male/female, n (%) | 12 (63)/7 (37) | 7 (70)/3 (30) | 10 (50)/10 (50) | 4 (50)/4 (50) |
| Country, n (%) | ||||
| United States | 17 (89) | 6 (60) | 17 (85) | 5 (63) |
| Canada | 2 (11) | 4 (40) | 3 (15) | 3 (37) |
| Living situation, n (%) | ||||
| Student/employed | 8 (42)* | 1 (10) | 4 (20) | 3 (37) |
| Unemployed | 7 (37) | 2 (20) | 7 (35) | 1 (13) |
| Retired | 4 (21) | 7 (70) | 9 (45) | 4 (50) |
| Living arrangement, n (%) | ||||
| Alone | 4 (21) | 3 (30) | 3 (15) | 2 (25) |
| Not alone | 15 (79) | 7 (70) | 17 (85) | 6 (75) |
| Level of study, n (%) | ||||
| Secondary | 7 (37) | 3 (30) | 11 (55) | 1 (13) |
| Post-secondary | 12 (63) | 7 (70) | 9 (45) | 7 (87) |
| Visual field deficit, n (%) | ||||
| Peripheral | 5 (26) | 2 (20) | 8 (40) | 2 (25) |
| Central | 7 (37) | 4 (40) | 4 (20) | 4 (50) |
| Both | 4 (21) | 3 (30) | 3 (15) | 1 (12) |
| None | 3 (16) | 1 (10) | 5 (25) | 1 (13) |
| Ocular disease, n (%) | ||||
| Central | 8 (42) | 5 (50) | 7 (35) | 3 (37) |
| Peripheral | 2 (11) | 3 (30) | 1 (5) | 2 (25) |
| General | 9 (47) | 2 (20) | 12 (60) | 3 (38) |
| Eye disease onset, n (%) | ||||
| Birth | 6 (32) | 3 (30) | 7 (35) | 2 (25) |
| >10 y | 6 (31) | 4 (40) | 6 (30) | 5 (62) |
| <6 mo to 10 y | 7 (37) | 3 (30) | 7 (35) | 1 (13) |
| Other sensory impairment, n (%) | ||||
| No | 15 (79) | 8 (80) | 17 (85) | 6 (75) |
| Yes | 4 (21) | 2 (20) | 3 (15) | 2 (25) |
| Cognitive impairment, n (%) | ||||
| No | 19 (100) | 10 (100) | 20 (100) | 8 (100) |
| Physical impairment, n (%) | ||||
| No | 16 (84) | 8 (80) | 16 (80) | 7 (87) |
| Yes | 3 (16) | 2 (20) | 4 (20) | 1 (13) |
| Health condition, n (%) | ||||
| Poor to good | 11 (58) | 6 (60) | 12 (60) | 4 (50) |
| Very good | 5 (26) | 2 (20) | 7 (35) | 2 (25) |
| Excellent | 3 (16) | 2 (20) | 1 (5) | 2 (25) |
*χ2 Test with P < .05. SD = standard deviation.
TABLE 2.
Participant characteristics and their relationship with group type
| Control group (n = 29) | Experimental group (n = 28) | P | Buyers (n = 39) | Renters (n = 18) | P | |
|---|---|---|---|---|---|---|
| Age (y), mean (SD) | 57.6 (12.3) | 51.4 (20.1) | .34* | 52.9 (17.1) | 58.2 (15.80) | .30* |
| Male/female, n (%) | 19 (66)/10 (34) | 14 (50)/14 (50) | .24 | 22 (56)/17 (44) | 11 (61)/7 (39) | .56 |
| Country, n (%) | .67 | .15 | ||||
| United States | 23 (79) | 22 (79) | 34 (87) | 11 (61) | ||
| Canada | 6 (21) | 6 (21) | 5 (13) | 7 (39) | ||
| User type, n (%) | .63 | |||||
| Renter | 10 (34) | 8 (29) | ||||
| Buyer | 19 (66) | 20 (71) | ||||
| Living situation, n (%) | .80 | NV | ||||
| Student/employed | 9 (31) | 7 (25) | 12 (31) | 4 (22) | ||
| Unemployed | 9 (31) | 8 (29) | 14 (36) | 3 (17) | ||
| Retired | 11 (38) | 13 (46) | 13 (33) | 11 (61) | ||
| Living arrangement, n (%) | .56 | .40 | ||||
| Alone | 7 (24) | 5 (18) | 7 (18) | 5 (28) | ||
| Not alone | 22 (76) | 23 (82) | 32 (82) | 13 (72) | ||
| Level of study, n (%) | .52 | .08 | ||||
| Secondary | 10 (34) | 12 (43) | 18 (46) | 4 (22) | ||
| Post-secondary | 19 (66) | 16 (57) | 21 (54) | 14 (78) | ||
| Visual field deficit, n (%) | .53 | .53 | ||||
| Peripheral | 7 (24) | 10 (36) | 13 (33) | 4 (22) | ||
| Central | 11 (38) | 8 (29) | 11 (28) | 8 (45) | ||
| Both | 7 (24) | 4 (14) | 7 (18) | 4 (22) | ||
| None | 4 (14) | 6 (21) | 8 (21) | 2 (11) | ||
| Ocular disease, n (%) | .48 | .06 | ||||
| Central | 13 (45) | 10 (36) | 15 (38) | 8 (44) | ||
| Peripheral | 4 (14) | 3 (11) | 3 (7) | 5 (28) | ||
| General | 11 (38) | 15 (53) | 21 (54) | 5 (28) | ||
| Eye disease onset, n (%) | .88 | .35 | ||||
| Birth | 9 (31) | 9 (32) | 13 (33) | 5 (28) | ||
| >10 y | 10 (34) | 11 (39) | 12 (31) | 9 (50) | ||
| <6 mo to 10 y | 10 (35) | 8 (29) | 14 (36) | 4 (22) | ||
| Other sensory impairment, n (%) | .79 | .70 | ||||
| No | 23 (79) | 23 (82) | 32 (82) | 14 (78) | ||
| Yes | 6 (21) | 5 (18) | 7 (18) | 4 (22) | ||
| Cognitive impairment, n (%) | NV | NV | ||||
| No | 29 (100) | 28 (100) | 39 (100) | 18 (100) | ||
| Physical impairment, n (%) | .95 | NV | ||||
| No | 24 (83) | 23 (82) | 32 (82) | 15 (83) | ||
| Yes | 5 (17) | 5 (18) | 7 (18) | 3 (17) | ||
| Health condition, n (%) | .68 | NV | ||||
| Poor to good | 17 (58) | 16 (57) | 23 (59) | 10 (56) | ||
| Very good | 7 (24) | 9 (32) | 12 (31) | 4 (22) | ||
| Excellent | 5 (17) | 3 (11) | 4 (10) | 4 (22) |
P value calculated with χ2 test. *P value calculated with Mann-Whitney tests. NV = “no value” when statistical comparisons were not possible given the frequency distribution of the data; SD = standard deviation.
TABLE 3.
Causes of vision impairment
| Cause of sight impairment, n (%) | Control group (n = 29) |
Experimental group (n = 28) |
|---|---|---|
| Optic nerve disease | 8 | 10 |
| AMD | 6 | 6 |
| Retinopathy of prematurity | 3 | 2 |
| Retinitis pigmentosa | 3 | 1 |
| Diabetic retinopathy | 0 | 2 |
| Stargardt disease | 1 | 1 |
| Congenital nystagmus | 1 | 1 |
| Retinal detachment | 1 | 1 |
| Keratoconus | 1 | 0 |
| Central retinal vein occlusion | 1 | 0 |
| Central serous retinopathy | 1 | 0 |
| Malign myopia | 1 | 0 |
| Stroke | 1 | 0 |
| Optic atrophy with cerebral visual impairment | 0 | 2 |
| Congenital cataract | 0 | 1 |
| Peter syndrome | 0 | 1 |
| Erdheim-Chester disease | 1 | 0 |
TABLE 4.
Participants characteristics and their relationship with study withdraw
| Variables | No withdraw group (n = 37) | Withdraw group (n = 20) | P |
|---|---|---|---|
| Age (y), mean (SD) | 54.0 (17.9) | 55.5 (14.7) | .97* |
| Male/female, n (%) | 22 (59)/15 (41) | 11 (55)/9 (45) | .75 |
| Country, n (%) | .59 | ||
| United States | 30 (81) | 15 (75) | |
| Canada | 7 (19) | 5 (25) | |
| Group type, n (%) | .12 | ||
| Control | 16 (43) | 13 (65) | |
| Experimental | 21 (57) | 7 (35) | |
| Customer type, n (%) | .32 | ||
| Renter | 10 (27) | 8 (40) | |
| Buyer | 27 (73) | 12 (60) | |
| Living situation, n (%) | .40 | ||
| Student/employed | 12 (33) | 4 (20) | |
| Unemployed | 9 (24) | 8 (40) | |
| Retired | 16 (43) | 8 (40) | |
| Living arrangement, n (%) | .22 | ||
| Alone | 6 (16) | 6 (30) | |
| Not alone | 31 (84) | 14 (70) | |
| Level of study, n (%) | .68 | ||
| Secondary | 15 (41) | 7 (35) | |
| Post-secondary | 22 (59) | 13 (65) | |
| Visual field deficit, n (%) | .87 | ||
| Peripheral | 11 (30) | 6 (30) | |
| Central | 13 (35) | 6 (30) | |
| Both | 6 (16) | 5 (25) | |
| None | 7 (19) | 3 (15) | |
| Ocular disease, n (%) | .35 | ||
| Central | 14 (38) | 9 (45) | |
| Peripheral | 7 (19) | 1 (5) | |
| General | 16 (43) | 10 (50) | |
| Eye disease onset, n (%) | .93 | ||
| Birth | 12 (32) | 6 (30) | |
| >10 y | 14 (38) | 7 (35) | |
| <6 mo to 10 y | 11 (30) | 7 (35) | |
| Other sensory impairment, n (%) | NV | ||
| No | 30 (81) | 16 (80) | |
| Yes | 7 (19) | 4 (20) | |
| Cognitive impairment, n (%) | NV | ||
| No | 37 (100) | 20 (100) | |
| Physical impairment, n (%) | NV | ||
| No | 31 (84) | 16 (80) | |
| Yes | 6 (16) | 4 (20) | |
| Health condition, n (%) | .69 | ||
| Poor to good | 20 (54) | 13 (65) | |
| Very good | 11 (30) | 5 (25) | |
| Excellent | 6 (16) | 2 (10) |
P value calculated with χ2 test. *P value calculated with Student t test. n = number of participants; NV = “no value” when statistical comparisons were not possible given the frequency distribution of the data; SD = standard deviation.
TABLE 5.
Demographic variables and their relationship with eSight device use
| Variables | eSight users (n = 48) | Discontinuance of eSight use (n = 9) | P |
|---|---|---|---|
| Age (y), mean (SD) | 53.4 (17.0) | 60.8 (14.4) | .28* |
| Male/female, n (%) | 26 (54)/22 (46) | 7 (78)/2 (22) | .19 |
| Country, n (%) | <.01 | ||
| United States | 41 (85) | 4 (44) | |
| Canada | 7 (15) | 5 (56) | |
| Group type | .30 | ||
| Control | 23 (48) | 6 (67) | |
| Experimental | 25 (52) | 3 (33) | |
| User type, n (%) | NV | ||
| Renter | 11 (23) | 7 (78) | |
| Buyer | 37 (77) | 2 (22) | |
| Withdraw the study | NV | ||
| No | 35 (73) | 2 (22) | |
| Yes | 13 (27) | 7 (78) | |
| Living situation, n (%) | NV | ||
| Student/employed | 15 (31) | 1 (11) | |
| Unemployed | 15 (31) | 2 (22) | |
| Retired | 18 (38) | 6 (67) | |
| Living arrangement, n (%) | .33 | ||
| Alone | 9 (19) | 3 (33) | |
| Not alone | 39 (81) | 6 (67) | |
| Level of study, n (%) | NV | ||
| Secondary | 19 (40) | 3 (33) | |
| Post-secondary | 29 (60) | 6 (67) | |
| Visual field deficit, n (%) | NV | ||
| Peripheral | 15 (31) | 2 (22) | |
| Central | 13 (27) | 6 (67) | |
| Both | 10 (21) | 1 (11) | |
| None | 10 (21) | 0 (0) | |
| Ocular disease, n (%) | NV | ||
| Central | 18 (37) | 5 (56) | |
| Peripheral | 7 (15) | 1 (11) | |
| General | 23 (48) | 3 (33) | |
| Eye disease onset, n (%) | NV | ||
| Birth | 18 (38) | 0 (0) | |
| >10 y | 15 (31) | 6 (67) | |
| <6 mo to 10 y | 15 (31) | 3 (33) | |
| Other sensory impairment, n (%) | NV | ||
| No | 39 (81) | 7 (78) | |
| Yes | 9 (19) | 2 (22) | |
| Cognitive impairment, n (%) | |||
| No | 48 (100) | 9 (100) | |
| Physical impairment, n (%) | NV | ||
| No | 39 (81) | 8 (89) | |
| Yes | 9 (19) | 1 (11) | |
| Health condition, n (%) | .61 | ||
| Poor to good | 29 (60) | 4 (44) | |
| Very good | 13 (27) | 3 (33) | |
| Excellent | 6 (13) | 2 (22) |
P value calculated with χ2 test. *P value calculated with Student t test. n = number of participants; NV = “no value” when statistical comparisons were not possible given the frequency distribution of the data; SD = standard deviation.
Table 1 displays descriptive comparisons between buyers and renters belonging to the control group, and between buyers and renters belonging to the experimental group. Statistical comparisons were calculated when the frequency distribution of the data allowed it. Participant characteristics at randomization show comparable demographic and descriptive variables across groups, albeit with a retired participant's preponderance in the control-renter subgroup.
Table 2 displays descriptive comparisons between the control and experimental groups and between the buyer and renter groups. Participant characteristics at randomization show comparable demographic and descriptive variables across groups, albeit with a male majority in the control group.
Table 4 displays descriptive comparisons (number of participants and percentage are provided in the table) between participants who remained in the study and those who withdrew from the study. Statistical comparisons were calculated when the frequency distribution of the data allowed it. Participant characteristics show comparable demographic and descriptive variables in groups.
Table 5 displays descriptive comparisons (number of participants and percentage are provided in the table) between participants who maintained their eSight use and those who discontinued their use. Statistical comparisons were calculated when the frequency distribution of the data allowed it. Participant characteristics show comparable demographic and descriptive variables in groups, albeit with a statistically significant majority of participants who resided in the United States in the group that maintained eSight use.
Primary Outcomes
Recruitment Target
We enrolled 32 participants (>50%) within 6 months and 57 participants (95%) within 12 months, with the target number of 60 participants being nearly reached (the last participant was enrolled on June 15, 2019). There were no adverse events requiring exclusion of participants.
Retention Rates
The retention rates were 93% (n = 53) at 2 weeks, 68% (n = 39) at 3 months, and 65% (n = 37) at 6 months. Of the 18 renters, 5 returned their device after the 2-week loan. The main reason was because they were not able to be proficient in reading with their device. For the participants who bought eSight (initial and new buyers, n = 52), the retention rates at 3 months were 75% and 71% at 6 months. Of the 20 participants who did not complete assessments within 6 months, 7 belonged to the experimental and 13 to the control group. The withdrawal did not differ significantly from the experimental group (χ21 [n = 57] = 2.46, P = .12). In the experimental group, one participant decided not to buy the device, two had difficulty accessing the Reacts telehealth portal and lacked support from their family/friends for usage of the platform (one of them had a technical device failure), and four withdrew from the study without giving any reason. In the control group, four participants decided not to buy the device, one participant had a decline in his health status, and eight withdrew without giving any reason. The 20 individuals who withdrew from the study did not differ statistically on any of the available variables displayed in Table 4, which included demographic (i.e., age, sex, country, living situation, living arrangement, and level of study) and ocular and general health conditions (i.e., ocular disease, eye disease onset, visual field deficit, and health condition). Twenty-six of 28 participants in the experimental group completed the six telerehabilitation sessions; the 2 remaining participants completed only the first two sessions.
Accessibility of Telerehabilitation
All of the participants in the experimental group had their own desktop computer to access the telehealth platform application with the help of the low vision therapist. None of them used their tablet or smartphone for the study. Either the camera was already incorporated into the computer, or participants added their own webcam and centered it in front of their face. Therefore, participants had both hands free during the entire session. Four (14%) of these 28 participants received assistance from a friend or family member during some of the training sessions and completed all six sessions. Two participants (7%) withdrew from the study (did not complete all six sessions) because they were not able to access the platform independently, of which one decided not to use the device anymore. There were no major issues with the audio component of the sessions; however, three participants had a weak signal connection that resulted in inconsistent and jerky audio when joining the platform, requiring them to intermittently use their telephone until the issue was solved. For six participants, the video did not automatically connect when they joined the session for the first time. Audio and/or video issues never jeopardized participants' training and were not a cause for withdrawing from the study.
Acceptability of Telerehabilitation Training
Participants' Ratings of Telerehabilitation Training
The 5-minute satisfaction survey was completed by 23 of 28 participants in the experimental group after the 2-week training in a separate session. All of the five participants who did not respond withdrew from the study. The respondents agreed that they were comfortable with receiving telerehabilitation training, of which 83% strongly agreed with this statement. The majority of the participants (overall 66%) strongly or mostly agreed that the training was as efficient (16/23), was as effective (16/23), and allowed them to better accomplish their goals (17/23) compared with other previous in-person rehabilitation services. Finally, most of the participants (20/23) strongly agreed that they would be interested in using telerehabilitation again if their visual needs change in the future. All agreed that they were satisfied overall with receiving telerehabilitation training, with 65% strongly agreeing with this statement (see Appendix, available at http://links.lww.com/OPX/A493, for detailed individual ratings).
Low Vision Therapist's Ratings of Telerehabilitation Training
While participants used their device, the low vision therapist clinically and qualitatively judged the evaluation of the working distance and lighting environment as moderately difficult for all participants. No exact measurement of the working distance and reading posture was obtained, but they were estimated through the camera and corrected by providing instructions. Finding the minimum magnification with the best reading distance and posture, we adjusted the magnification level on the device. By asking the participants to use their computer camera to scan around the room and observe the presence of windows or lamps, the level of lighting was qualitatively estimated. Moreover, an optional light integrated in the eSight device, providing direct and constant illumination onto the reading material, was easy to manage by the low vision therapist and the participants. Finally, the low vision therapist clinically and qualitatively judged the evaluation of reading speed and reading accuracy through the shared reading material as not difficult for all participants. Even from nonstandardized text, it was possible to observe and identify reading problems including difficulties with long words, line breaks, or confusion of some letters.
Secondary Outcomes
eSight Eyewear Discontinuance
Early Discontinuance
Among the 57 participants, 7 (12%) reported discontinuing their eSight device use early: 5 renters decided not to buy the device because they did not experience reading improvement, and 2 buyers decided not to use the device anymore because of a decline in health and difficulty using the device. Three participants did not complete their questionnaire at 2 weeks and withdrew from the study without providing any reasons. For these participants, it was not possible to confirm if they discontinued their eSight use early. Considering their group membership, 71% (5/7) of the participants who discontinued their device use early belonged to the control group.
Late Discontinuance
Two participants reported nonuse of the device in the previous 3 months. They reported that they had not completely stopped using their device and that they simply had not needed it since their last use. At their 6-month evaluation, four participants reported nonuse between 1- and 3-month periods, and three of them reported that they completely stopped using their eSight device: two did not give a reason, and one reported a decline in health. At either time point, the number of participants who sustained their device use did not differ statistically between the two groups (Table 5).
The questions specifically developed for this study about device user's characteristics and changes in use identified that the activities for which eSight device was most used were as follows: reading and watching TV (see Appendix, available at http://links.lww.com/OPX/A493, for detailed individual goals), a finding that is consistent with other studies on head-mounted display systems.7,32 Those who reported nonuse of the device were those for which these activities were the least performed with the eSight. The activities for which the device was least used included cooking, shopping, and meetings.
DISCUSSION
The purpose of the present study was to conduct a feasibility study to assess the recruitment, retention, accessibility, and overall acceptability of telerehabilitation for people with low vision using a head-mounted display. Our results demonstrated that it was feasible to implement a randomized controlled study design, with individuals with visual impairment using eSight Eyewear receiving rehabilitation via a telehealth platform. Once enrolled, 35% of participants withdrew from the study. We observed high accessibility and acceptability of the telerehabilitation training sessions among those completing the protocol, and a low usage discontinuation of the head-mounted display (16% of all participants across the study). The participants' choice to continue using the device was independent of the training offered.
When we compared the current study with previous randomized trials of vision rehabilitation in terms of loss to follow-up or study withdrawal rates, we observed that our 35% is higher than the 8.5%,33 15%,34 and 24%35 reported in the literature. As opposed to our study that administered three successive follow-up assessments for 6 months, these cited studies implemented only one follow-up assessment at 3 months,33 4 months,34 or 12 months.35 If we considered the participants who bought eSight only, we obtained a withdrawal rate of 29% at 6 months that tends to align with the study by Bahrami et al.35 Although withdrawal from the study did not differ significantly from the experimental group, nearly twice as many participants withdrew from the control group. This difference may be explained by the lack of personalized guided instruction and accountability by a low vision therapist who provided the training in the telerehabilitation group. Future investigations including more participants will be useful to confirm the statistical relevance of this difference between the two interventions.
There were no major issues with the audio and video components of the telerehabilitation probably because participants used their own computer and did not experience such issues as reported in a previous pilot study.20 In addition, we used a secure and accredited telehealth platform that has been used by various telehealth projects by public health providers within the university health network of the research team. The high accessibility and acceptability reported by our participants suggest that telerehabilitation seems a promising modality for low rehabilitation services. The training delivered in our study was personalized, providing relevant insights into the participants' environment that were visually challenging to the low vision therapist. The telerehabilitation training was similar to services that would be given in-office, including the same confidence level and comfort in human interaction with participants, in particular for reading, writing, other eye-hand coordination tasks (e.g., sewing and drawing), and initial eccentric fixation training. The eccentric vision program was not offered in its entirety and not to all participants, only to those where the therapist identified a need. More than six sessions would be needed for the acquisition of a stable eccentric fixation according to the low vision therapist. Few participants needed direct assistance from a friend or family during the telerehabilitation sessions. Most were independent, and once connected and if they experienced technical challenges with the telehealth platform, it did not compromise training.
In light of an inconsistent training model for emerging head-mounted display technology, the present study compared a clinical-type intervention with a commercial self-training standard provided by the device manufacturer. A recent pilot study supported the potential value and feasibility of low vision telerehabilitation in 10 patients receiving a 1-hour unique training session at home to use their handheld magnifier, provided by an in-office clinician.20 Positive accessibility feedback was gathered from both participants and providers, and encouraging results were obtained regarding acceptability as well. An alternative telerehabilitation format is currently implemented by the Buffalo Veterans Affairs low vision service, in which participants travel to an equipped location in their vicinity to receive training from a remote low vision rehabilitation therapist.36 Considering the diversity of telerehabilitation types described, one of the next steps will be to compare our telerehabilitation training with a traditional in-office low vision service. Moreover, given these encouraging outcomes,20 it is likely feasible to provide telerehabilitation for other head-mounted displays or electronic low vision aids.
We included measures of device usage as secondary outcome measures; however, we did not find any significant difference in device use between the two intervention groups. This finding indicates that training provided by the device manufacturer is equally feasible as the proposed personalized telerehabilitation training. Insofar as low vision aid usage depends on training,37 this result is perhaps not surprising. In particular, a scoping review reported that intensive training was predictive of magnifying low vision aids use.11 Considering the sustained 30-hour training of the eSkills program, this may have produced the same effect on device use as the personalized telerehabilitation training. However, a cross-sectional study revealed that training was not a predicting factor of eSight device use.12 It is probable that follow-up assessments, required by the present longitudinal design, positively influenced participants' motivation regardless of their self-training compliance (Hawthorne effect).
Compared with the 30% discontinuance rate (also considered as a threshold for defining low and high rates of device abandonment38) of assistive technology use traditionally observed in the literature,39,40 the 16% (including early and late discontinuance) in the present study is considered low. It mirrors behavior use measured in an online survey, whereby 17% of the participants had discontinued their device use.12 This finding is also in line with the 17% abandonment rate reported in the context of patients receiving magnifiers via a novel low vision mobile clinic delivery model.27 We anticipated that this low discontinuation rate may be an underestimate, given the number of participants who withdrew from the study without providing any reasons, as well as a possible social desirability bias in the responses of the remaining participants. The cost involved in obtaining the device may also influence the motivation to maintain usage over the time. However, the logic that tends to associate people who withdraw from the study with those who discontinued their device use did not entirely apply here. The two participants who discontinued their device use late completed the entire 6-month follow-up. Moreover, five participants who completely stopped using their device (but did not meet our late discontinuance definition and were not categorized as nonusers) did not withdraw from the study.
A limitation of the study design is that it is not possible in the experimental group to determine if the beneficial effects were from either or both the eSkills guide and/or the VisExc program. Compared with the 26%,35 28%,34 or 33%33 reported by previous randomized trials of vision rehabilitation, a rather large proportion of those who were eligible for the study had declined to participate (79%), perhaps because telerehabilitation is not desirable by new eSight users, and/or there may be inherent differences in terms of age, sex, or socioeconomic status among those who choose to participate versus those who did not. Although a lack of interest in the study was the reason reported by the individuals who did not participate, a major limitation of this current study is the lack of in-depth documentation to indicate the reasons why potential participants had declined to join the study; this deserves to be highlighted as an important area for future study. Self-selection bias is a limitation, insofar as we enrolled participants who spontaneously decided to use eSight Eyewear and were willing to participate in research and to try an Internet-based video conference platform. Future studies should consider providing the head-mounted display and Internet access, thereby avoiding the possibility of the purchase commitment to affect the outcomes. It is worth noticing that, among users who were contacted, nobody was excluded from this study because of a lack of Internet and/or computer/tablet access because all were already equipped. However, the participants were not representative of the general low vision population because they were already exposed to sophisticated technology, possibly leading them to be more willing to try technology used for telerehabilitation and/or videoconferencing. However, this limitation will probably be less contextual over the next decades with upcoming generations. Participants were experienced technology users, possibly leading them to be more willing to try the video conference platform and also making them less representative of the general low vision population. The two participants who withdrew from the study because they experienced difficulties using basic functions of their computer did not complete the training sessions and the satisfaction survey, and this may have induced a bias in the conclusion about acceptability. In terms of telerehabilitation acceptability, some questions of the satisfaction survey compare the telerehabilitation training for the eSight to previous in-person training for other visual assistive devices (e.g., handheld magnifiers or closed-circuit televisions or telescopes) in terms of being efficient, being effective, and accomplishing goals. However, those data may be difficult to interpret because the types of devices are different, and it is unknown if the ratings were influenced by the type of device (eSight vs. handheld magnifier) or the training modality (telerehabilitation video visit vs. in-office). In addition, it was not always possible to differentiate device discontinuance from other types of attrition, specifically with participants who withdrew from the study without explanation. However, through regular monitoring, we hope we were able to record most reasons for leaving the study. To further optimize a future trial, duration of use and the settings used by the participant should be monitored. Moreover, the absence of an effect of the offered training does not include the opinions of the 35% who withdrew from the study. Other potential limitations are the absence of an in-office evaluation with objective visual function measures, as well as the lack of assessment of the satisfaction for the control subjects, which could be added to future protocols. For example, a standardized near reading or acuity cards during the telerehabilitation session had already been successfully implemented.20 Finally, it was not possible to mask participants to the experimental intervention. This may have introduced social desirability bias, possibly influencing the usage of the head-mounted display and attrition. Randomized participant allocation, masking the researcher to group allocation, and the use of self-administered assessments minimized selection, detection, and experimenter bias.
CONCLUSIONS
The data demonstrated the feasibility of a randomized controlled study of telerehabilitation for people living with low vision and using a head-mounted display. Positive feedback from the participants and the low vision therapist suggests the potential value of this modality for low vision services. With the aging of the population, it is urgent to provide innovative care delivery strategies for low vision service to maintain and increase the standard of care and the quality of life for people with low vision. Low vision rehabilitation has the potential to overcome barriers associated with existing service delivery while maintaining personalized care and human interaction. Moreover, telerehabilitation has the potential to increase efficiency, reducing travel time and expenses for both the low vision therapist and the patients. This modality may increase the number of follow-up sessions to improve learning about device use and health-related outcomes. New reimbursement modes for telehealth services will need to be addressed and could open the door to future implementation of the services into current clinical practice.
Supplementary Material
Footnotes
Supplemental Digital Content: The Appendix, available at http://links.lww.com/OPX/A493, describes acceptability outcomes that include the goals of rehabilitation for each participant of the experimental group and the low vision therapist's ratings of the extent to which each goal was reached, as well as participants' ratings of telerehabilitation training. The activities for which the eSight device was most used were reading and watching TV. For 28 participants, the low vision therapist estimated that 17 completely and 7 partially reached their goals, but 4 did not complete their goals at all.
Funding/Support: Mitacs (IT08595 Grant; to M-CL) and Fonds de Recherche du Québec—Santé (Junior 2 chercheur boursier Career Award No. 281454; to WW).
Conflict of Interest Disclosure: None of the authors have reported a financial conflict of interest. The sponsor facilitated subject recruitment; however, the sponsor was not involved in study design, analyses, and interpretation. The authors were responsible for the preparation of this article and the decision to submit this article for publication. Each of the authors had access to the study data and takes full responsibility for his/her presentation in this article.
Author Contributions and Acknowledgments: Conceptualization: M-CL, WW; Data Curation: M-CL; Formal Analysis: M-CL, WW; Funding Acquisition: M-CL; Investigation: M-CL; Methodology: M-CL, WW; Project Administration: M-CL, WW; Resources: WW; Software: M-CL; Supervision: WW; Validation: WW; Writing – Original Draft: M-CL; Writing – Review & Editing: M-CL, WW.
The authors thank Josée Duquette for access to the VisExc-INLB eccentric fixation program and Nancy Primeau for her support for formatting of bibliographic references.
Supplemental Digital Content: Direct URL links are provided within the text.
REFERENCES
- 1.Foster A, Gilbert C, Johnson G. Changing Patterns in Global Blindness: 1988–2008. Community Eye Health 2008;21:37–9. [PMC free article] [PubMed] [Google Scholar]
- 2.Corn A, Lusk KE. Perspectives on low vision. In: Corn A, Koenig A, eds. Foundations of Low Vision: Clinical and Functional Perspectives. 2nd ed. New York: AFB Press; 2010:3–25. [Google Scholar]
- 3.Binns AM Bunce C Dickinson C, et al. How Effective Is Low Vision Service Provision? A Systematic Review. Surv Ophthalmol 2012;57:34–65. [DOI] [PubMed] [Google Scholar]
- 4.Trauzettel-Klosinski S. Rehabilitation for Visual Disorders. J Neuroophthalmol 2010;30:73–84. [DOI] [PubMed] [Google Scholar]
- 5.Deemer AD Bradley CK Ross NC, et al. Low Vision Enhancement with Head-mounted Video Display Systems: Are We There Yet? Optom Vis Sci 2018;95:694–703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ortiz A Chung ST Legge GE, et al. Reading with a Head-mounted Video Magnifier. Optom Vis Sci 1999;76:755–63. [DOI] [PubMed] [Google Scholar]
- 7.Ballinger R Lalle P Maino J, et al. Veterans Affairs Multicenter Low Vision Enhancement System (LVES) Study: Clinical Results. Report 1: Effects of Manual-focus LVES on Visual Acuity and Contrast Sensitivity. Optometry 2000;71:764–74. [PubMed] [Google Scholar]
- 8.Lin CS Jan HA Lay YL, et al. Evaluating the Image Quality of Closed Circuit Television Magnification Systems versus a Head-mounted Display for People with Low Vision. Assist Technol 2014;26:202–8. [DOI] [PubMed] [Google Scholar]
- 9.Wittich W Lorenzini MC Markowitz SN, et al. The Effect of a Head-mounted Low Vision Device on Visual Function. Optom Vis Sci 2018;95:774–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Stelmack JA Tang XC Wei Y, et al. Outcomes of the Veterans Affairs Low Vision Intervention Trial II (LOVIT II): A Randomized Clinical Trial. JAMA Ophthalmol 2017;135:96–104. [DOI] [PubMed] [Google Scholar]
- 11.Lorenzini MC, Wittich W. Factors Related to the Use of Magnifying Low Vision Aids: A Scoping Review. Disabil Rehabil 2020;42:3525–37. [DOI] [PubMed] [Google Scholar]
- 12.Lorenzini MC, Hamalainen AM, Wittich W. Factors Related to the Use of a Head-mounted Display for Individuals with Low Vision [published online December 28, 2019]. Disabil Rehabil 2019. doi: 10.1080/09638288.2019.1704892. [DOI] [PubMed] [Google Scholar]
- 13.Malkin AG Ross NC Chan TL, et al. U.S. Optometrists' Reported Practices and Perceived Barriers for Low Vision Care for Mild Visual Loss. Optom Vis Sci 2020;97:45–51. [DOI] [PubMed] [Google Scholar]
- 14.Goldstein RB Dugan E Trachtenberg F, et al. The Impact of a Video Intervention on the Use of Low Vision Assistive Devices. Optom Vis Sci 2007;84:208–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lezzoni LI, Killeen MB, O'Day BL. Rural Residents with Disabilities Confront Substantial Barriers to Obtaining Primary Care. Health Serv Res 2006;41:1258–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gold D, Zuvela B, Hodge WG. Perspectives on Low Vision Service in Canada: A Pilot Study. Can J Ophthalmol 2006;41:348–54. [DOI] [PubMed] [Google Scholar]
- 17.Brennan DM Tindall L Theodoros D, et al. A Blueprint for Telerehabilitation Guidelines—October 2010. Telemed J E Health 2011;17:662–5. [DOI] [PubMed] [Google Scholar]
- 18.Hailey D Roine R Ohinmaa A, et al. Evidence of Benefit from Telerehabilitation in Routine Care: A Systematic Review. J Telemed Telecare 2011;17:281–7. [DOI] [PubMed] [Google Scholar]
- 19.Bittner AK Yoshinaga PD Wykstra SL, et al. Telerehabilitation for People with Low Vision. Cochrane Database Syst Rev 2020;2:CD011019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bittner AK Yoshinaga P Bowers A, et al. Feasibility of Telerehabilitation for Low Vision: Satisfaction Ratings by Providers and Patients. Optom Vis Sci 2018;95:865–72. [DOI] [PubMed] [Google Scholar]
- 21.Consolidated Standards of Reporting Trials (CONSORT) Group . Pilot and Feasibility Trials; 2018. Available at: http://www.consort-statement.org/extensions/overview/pilotandfeasibility. Accessed May 8, 2019.
- 22.Lorenzini MC, Wittich W. Measuring Changes in Device Use of a Head-mounted Low Vision Aid After Personalised Telerehabilitation: Protocol for a Feasibility Study. BMJ Open 2019;9:e030149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.eSight Corporation . Eskills User Guide & Proficiency Program. Toronto, Ontario, Canada: The Corporation; 2015. [Google Scholar]
- 24.Duquette J, Lapointe N, Loiselle J. Visexc-INLB: Method of Evaluation and Training in Eccentric Vision of the Nazareth and Louis-Braille Institute: User Manual. Longueuil, Quebec, Canada: Institut Nazareth et Louis-Braille; 2013. [Google Scholar]
- 25.Overbury O, Conrod EB. McGill Low Vision Manual. Montreal, Quebec, Canada: Betacom Group; 1997. [Google Scholar]
- 26.Gothwal VK Thomas R Crossland M, et al. Randomized Trial of Tablet Computers for Education and Learning in Children and Young People with Low Vision. Optom Vis Sci 2018;95:873–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gobeille MR Malkin AG Jamara R, et al. Utilization and Abandonment of Low Vision Devices Prescribed on a Mobile Clinic. Optom Vis Sci 2018;95:859–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Day H, Jutai J. Measuring the Psychosocial Impact of Assistive Devices: The PIADS. Can J Rehabil 1996;9:159–68. [Google Scholar]
- 29.Demers L, Weiss-Lambrou R, Ska B. Development of the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST). Assist Technol 1996;8:3–13. [DOI] [PubMed] [Google Scholar]
- 30.Lorenzini MC, Wittich W. Head-mounted Visual Assistive Technology–related Quality of Life Changes after Telerehabilitation. Optom Vis Sci 2021;98:582–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.JASP [Computer Program]. Version 0.9. Amsterdam, the Netherlands: University of Amsterdam; 2017. [Google Scholar]
- 32.Crossland MD Starke SD Imielski P, et al. Benefit of an Electronic Head-mounted Low Vision Aid. Ophthalmic Physiol Opt 2019;39:422–31. [DOI] [PubMed] [Google Scholar]
- 33.Smith HJ Dickinson CM Cacho I, et al. A Randomized Controlled Trial to Determine the Effectiveness of Prism Spectacles for Patients with Age-related Macular Degeneration. Arch Ophthalmol 2005;123:1042–50. [DOI] [PubMed] [Google Scholar]
- 34.Stelmack JA Tang XC Reda DJ, et al. Outcomes of the Veterans Affairs Low Vision Intervention Trial (LOVIT). Arch Ophthalmol 2008;126:608–17. [DOI] [PubMed] [Google Scholar]
- 35.Bahrami H, Melia M, Dagnelie G. Lutein Supplementation in Retinitis Pigmentosa: PC-based Vision Assessment in a Randomized Double-masked Placebo-controlled Clinical Trial [Nct00029289]. BMC Ophthalmol 2006;6:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ihrig C. Steps to Offering Low Vision Rehabilitation Services through Clinical Video Telehealth. J Vis Impair Blind 2016;110:441–7. [Google Scholar]
- 37.Copolillo A, Teitelman JL. Acquisition and Integration of Low Vision Assistive Devices: Understanding the Decision-making Process of Older Adults with Low Vision. Am J Occup Ther 2005;59:305–13. [DOI] [PubMed] [Google Scholar]
- 38.Scherer MJ. Outcomes of Assistive Technology Use on Quality of Life. Disabil Rehabil 1996;18:439–48. [DOI] [PubMed] [Google Scholar]
- 39.Scherer MJ Sax C Vanbiervliet A, et al. Predictors of Assistive Technology Use: The Importance of Personal and Psychosocial Factors. Disabil Rehabil 2005;27:1321–31. [DOI] [PubMed] [Google Scholar]
- 40.Verza R Carvalho ML Battaglia MA, et al. An Interdisciplinary Approach to Evaluating the Need for Assistive Technology Reduces Equipment Abandonment. Mult Scler 2006;12:88–93. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


