Supplemental digital content is available in the text.
SIGNIFICANCE
Head-mounted low vision devices have become a viable alternative to enhance residual vision. This study supports the use of a head-mounted display to improve aspects of functional vision and quality of life. Much is still unknown regarding the required frequency, duration, or potential effectiveness of this telerehabilitation training protocol or what characteristics best identify optimal users.
PURPOSE
A randomized study explored the effect of telerehabilitation on quality of life and functional vision in individuals with low vision using a head-mounted display.
METHODS
We recruited 57 participants (age, 21 to 82 years; mean, 54.5 years) among new prospective eSight Eyewear users, randomized 1:1 into two parallel groups; the experimental group received the telerehabilitation training provided by a low vision therapist, whereas the control group received the self-training standard offered by the device manufacturer and without involvement of a low vision therapist. The primary outcome measures were the impact of telerehabilitation on validated measures of assistive technology–related quality of life: the Psychosocial Impact of Assistive Devices Scale and the Quebec User Evaluation of Satisfaction with Assistive Technology scale. Exploratory outcomes were the assessment of self-reported functional vision using the Veterans Affairs Low Vision Visual Functioning Questionnaire-48 and cybersickness associated with head-mounted display use with the Simulator Sickness Questionnaire.
RESULTS
Assistive technology–related quality of life was improved when measured by the satisfaction scale but not the psychosocial scale within the first 3 months, independently of training type. Overall, functional vision improvement was observed within the first 2 weeks of device use and maintained during the 6-month study, independently of group type. Cybersickness outcomes were similar between training groups and did not change significantly for 6 months.
CONCLUSIONS
eSight Eyewear, either with telerehabilitation or with the manufacturer self-training comparison, improved functional vision and increased users' quality of life within the initial 3 months of device training and practice.

Visual impairment (blindness and low vision) is globally prevalent across the life span and affects at least 2.2 billion people.1 An individual with low vision is defined as a person experiencing difficulty with accomplishing visuals tasks, even with optimal standard refraction, and having the potential to enhance his/her ability to perform these tasks using compensatory visual strategies, low vision assistive devices, and environmental modifications.2 Low vision rehabilitation is the primary intervention for individuals with reduced visual function and can improve independence, functional visual abilities, and quality of life by maximizing the individual's remaining visual abilities.3 Among the most common forms of intervention in low vision rehabilitation is the provision of, and training in, the use of low vision aids, including optical and electronic magnification devices4 that are commonly recommended and provided in face-to-face rehabilitation sessions.
In recent decades, wearable head-mounted displays have undergone major technological evolution (i.e., rapid miniaturization of the camera, image processing, and display electronics) and have become a viable alternative to enhance residual vision in individuals with vision impairment.5,6 Among the new generation of head-mounted displays, eSight Eyewear (eSight Corporation, Toronto, Ontario, Canada), a semi-immersive system (e.g., virtual reality), was designed to improve on previous device features, such as magnification, offering auto focus, contrast enhancement at all distances, hands-free use, and approximately 30° of field of view through digital image processing. In 2018, a multicenter prospective trial demonstrated improvement in visual ability including activities of daily living and reading in 51 novice eSight Eyewear users, followed for 3 months and benefitting from a self-training program for 1 month (30 hours) provided by the device manufacturer.7 The benefits of practice and training with head-mounted displays have not been extensively studied, although the importance of training in their use has previously been demonstrated as important, specifically for distant and intermediate vision, compared with traditional low vision aids.8
Despite the functional and evidence-based benefits of magnifying low vision aid use,9 a scoping review documented highly variable rates of device nonuse.10 If an assistive device fails to improve functional vision, or if quality of life is not improved or even declines, the device tends to be abandoned. A cross-sectional study documented that, of 109 eSight Eyewear users, 17.4% (n = 19) did not use their device in the past 3 months,11 reporting multiple reasons. Importantly, device users who perceived a more positive effect of the device on their quality of life were consistently more likely to continue using eSight Eyewear. Day et al.12(p34) stated that “an assistive device should promote good quality of life for the user to the extent to which it makes the user feel competent, confident, and inclined (or motivated) to exploit life's possibilities.” In addition, the presence of headaches while using the device was determined as a consistent predictor of eSight Eyewear nonuse.11 More generally, cybersickness can be described as a range of symptoms including disorientation, vertigo, headaches, and eyestrain induced by virtual reality13 and could be considered as an important usability issue, potentially influencing the adoption of such technology.14 Enhanced image motion, sometimes exaggerated through magnification, increases the risk of cybersickness and other symptoms of visual discomfort15 because the camera included in a head-mounted low vision enhancement system moves with the users' head movements. Insufficient training, duration, and frequency have also been identified as important predictors of magnifying low vision aid nonuse.10 The most common approach for delivering low vision rehabilitation in-office may be a barrier in the process of acquiring and incorporating magnifying low vision aids, given the need for transportation to and from the session.16 This is particularly a challenge given the paucity of specialty services and the limited access to care in rural areas of geographically dispersed countries.17
Telerehabilitation has become a viable alternative for delivering rehabilitation services, allowing individuals to remain at home while receiving services through Internet-based communication technology.18 However, a Cochrane systematic review reported very few applications and no published outcomes in the context of low vision.19 The visually impaired population, however, tends to use more and more mobile mainstream devices with built-in video systems (e.g., smartphone and tablet), suggesting that they could be used to deliver telerehabilitation services.20,21 Considering the absence of previous randomized controlled studies in the context of low vision telerehabilitation and to help guide evidence-based practice recommendations, the present study was conducted with the primary objective of determining whether administering several low vision rehabilitation training sessions using an Internet-based video platform can improve users' quality of life. One of the instruments used in this study measured three quality-of-life domains related to the use of assistive technology, specifically competence, adaptability, and self-esteem. In the context of head-mounted displays, device factors (e.g., interpupillary distance)22 and general ergonomics (e.g., heavy and inappropriate fitting headsets) are responsible for physical discomfort and can also contribute to cybersickness symptoms that can weaken the visual experience.23 Awareness of these factors and individualized attention commonly offered by vision rehabilitation services is essential to increase the adoption of the technology. Thus, secondary objectives were to determine if a personalized telerehabilitation intervention plan could improve self-reported functional vision and/or reduce symptoms of cybersickness.
METHODS
Study Design
The protocol of this prospective randomized intervention feasibility study has previously been published in more details.24 The study complied with the Declaration of Helsinki and was approved by the institutional review board of the Centre de recherche interdisciplinaire en réadaptation du Montréal métropolitain (CRIR no. 1286-1217).
Initial Contact
Directly after renting or buying an eSight device, potential participants were informed by an employee of eSight Corporation of the opportunity to participate in this research project. A letter introducing the study was sent by e-mail at the time of device delivery, and a paper version was included in the parcel, providing the contact information of the research team to the users, so they could express their interest in participation. In addition, the device manufacturer sent the users' telephone contact to the research team to optimize recruitment.
Validation of Eligibility Criteria and Recruitment
Once a potential participant had expressed interest in the study, the research team verified inclusion criteria and explained the objectives and the schedule of the study and finally obtained informed written consent via a scanned, photographed, or mailed consent form. We enrolled novice users of eSight Eyewear aged 18+ years with self-reported low vision who had a tablet, desktop, or laptop computer with Internet access and recently bought (<1 month) or were renting eSight Eyewear. Exclusion criteria are detailed in the published protocol.24 Participants were randomized (1:1 ratio) to receive 30 hours of either personalized low vision training through telerehabilitation, or the self-training standard provided by eSight using the eSkills User Guide.25 This guide was available both in PDF and paper versions and written in large print and was completely self-administered at home by the participants. It spans 1 hour per day for 1 month (30 hours) to be performed self-guided at home and is divided into 4 consecutive weeks of exercises. The self-training focused on the technical aspects of using the eSight device and provided instructions about the settings for distance vision and reading as well as viewing techniques with other media (i.e., digital tablets, TV). The personalized training consisted of six 1-hour online training sessions within the first 2 weeks (6 hours), 12 additional hours of homework in parallel during the same 2 weeks, and an additional 12 hours of homework in the following 2 weeks. Telerehabilitation focused on the functional aspects of using eSight. In addition to distance vision and reading exercises, participants were trained on specific writing (i.e., crosswords, drawing, or painting) and other eye-hand coordination tasks, according to each person's needs (i.e., playing cards, sewing). Eye movement control and, if needed, eccentric fixation were trained using exercises extracted from standard/well-established clinical low vision guides (the McGill Low Vision Manual26 and the VisExc-INLB eccentric fixation program27). Participants in the telerehabilitation group trained themselves at home using the eSkills learning and training guide and additional personalized exercises extracted from the two cited low vision guides. In both groups, participants had optional access to standard support for technical issues available through eSight Corporation staff. Both interventions are described in the detailed protocol publication, and a summary is available in the parallel study.28 Fig. 1 summarizes the design of the study.
FIGURE 1.
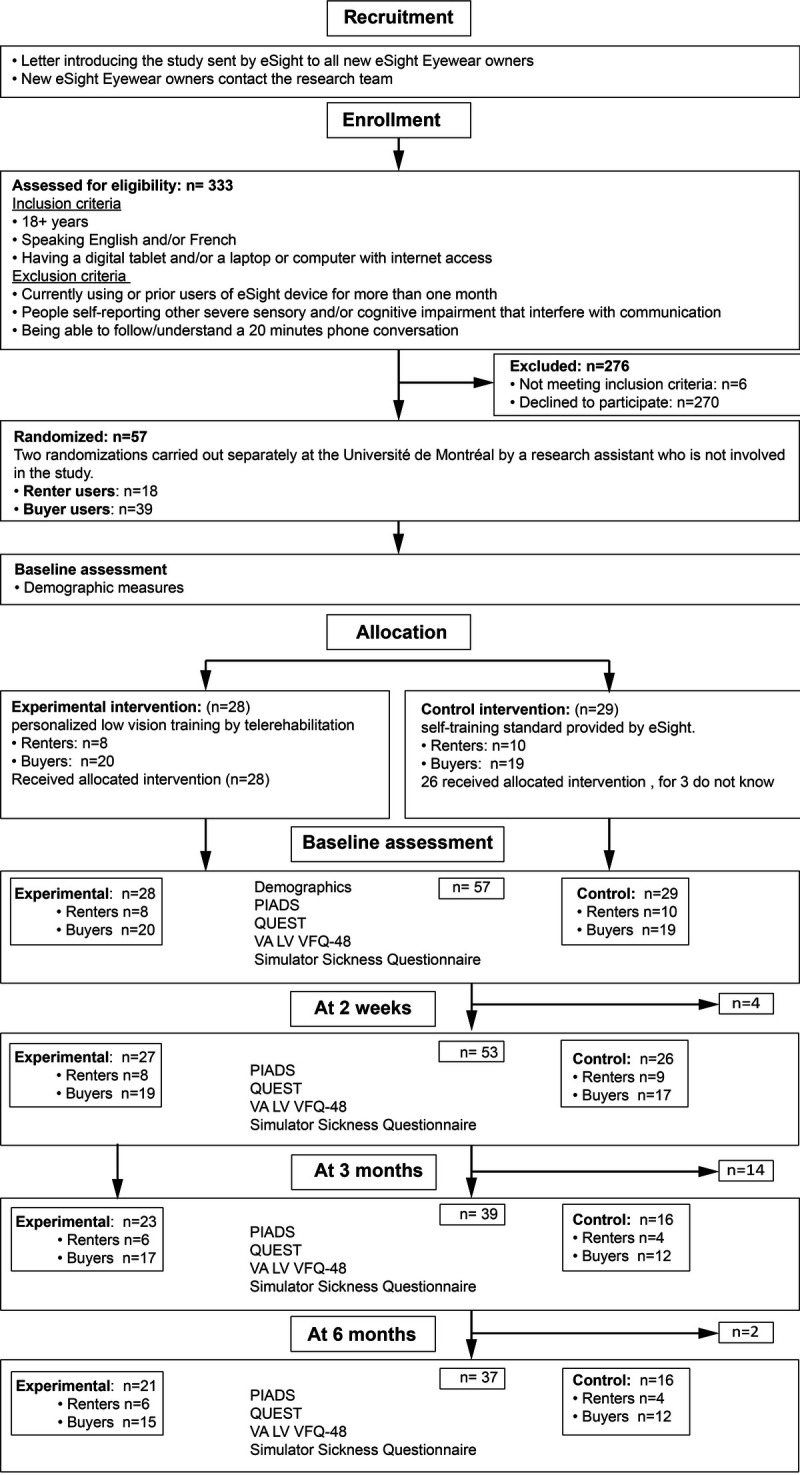
Chart showing participant flow that summarizes the design of the study with each following aspects: recruitment, enrollment, allocation with intervention types, evaluation timeline, and primary and secondary outcomes.
Sample Size
A previous multicenter prospective study7 exploring the short- and medium-term effects of eSight Eyewear reported various effect sizes that cover the secondary outcome measures proposed in the present protocol, ranging from ω2 = 0.04 to 0.83. Choosing a conservative average effect size of ω2 = 0.23 to calculate the sample of the present study (mixed-design ANOVA), power analysis using G*Power (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany) indicated that, with a desired power of 0.95 and α level of 0.05, the necessary sample size is n = 60, with n = 30 in each arm, a sample size commonly used in feasibility studies.
Telerehabilitation Equipment
In the case of personalized training by telerehabilitation, participants received distance training sessions delivered to their home via video conferencing, with the study's low vision therapist located at the School of Optometry of the Université de Montréal. Each participant was able to interact in real time using a secure and password-protected connection, with the low vision therapist using the REACTS telehealth platform, accessible for all through their computer or digital tablet at specific appointments (https://www.iitreacts.com).
Outcomes
Primary Outcomes
The primary focus of this study was the effect of telerehabilitation on eSight users' quality of life and encompassed two standardized measures: the Psychosocial Impact of Assistive Devices Scale,29 a 26-item questionnaire composed of three subscales (competence, adaptability, and self-esteem), and the Quebec User Evaluation of Satisfaction with Assistive Technology30 scale, a 12-item outcome measure that assesses user satisfaction with device and services, both of which are reliable and validated in English and French. In addition, we administered open- and closed-ended questions specifically developed for this study.24 For example, participants were asked to what extent (entirely, half, more than the half, not at all) they considered that they had completed their training (eSkills manual for control group and online training sessions as well as the eSkills manual and VisExc program for the experimental group).
Secondary Outcomes
We assessed the effect of personalized telerehabilitation on functional visual ability using the Veterans Affairs Low Vision Visual Functioning Questionnaire-48.31 The four functional domains of this questionnaire are reading (reading newspaper, print on television, or street signs), visual information (recognizing faces, finding an item on a crowded shelf), visual motor (activities of daily living such as pouring a liquid into a cup, preparing a meal, or self-grooming), and mobility (use of public transport, navigating stairs, and getting around in unfamiliar places). Scores were converted into logit units using the algorithm developed by Stelmack and Massof32 for use in clinical settings and small samples.
We measured cybersickness, given its potential link to head-mounted display use, with the Simulator Sickness Questionnaire.33 It is a widely applied measurement tool in research studying cybersickness and a standard for accessing virtual reality–related sickness. It assesses 16 symptoms grouped into three categories, namely, nausea that refers to motion sickness condition (i.e., increased salivation, sweating), disorientation related to simulator sickness (i.e., vertigo blurred vision), and oculomotor issues that refer to cybersickness (i.e., fatigue, headache, eyestrain). All questionnaires were administered at baseline by the low vision therapist and self-administered online through a URL link at 2 weeks, 3 months, and 6 months after randomization. Questionnaires were administered to participants orally (by telephone) at baseline by the low vision therapist. They were instructed to answer as if they were using their habitual visual assistive devices other than their eSight unit. Please note that all participants reported to already be using at least one assistive device for reading or magnification at baseline. For follow-up assessments, the questionnaires were self-administered, available via a URL link, and included written instructions for participants to answer as if they were using their eSight unit.
Statistical Methods
Statistical analyses were conducted using JASP version 0.9 (University of Amsterdam, Amsterdam, the Netherlands) and JAMOVI version 1.0.5 (Sydney, Australia) software. The analysis plan consisted of three steps. For step 1, descriptive measures, including participants' demographic and clinical characteristics, were summarized as means and standard deviations, and medians and interquartile ranges and by counts and percentages as appropriate. For steps 2 and 3, given the repeated-measures component of the study and to accommodate potentially missing data, the analyses were conducted using a mixed-effects model and post hoc tests using Bonferroni correction (P < .05). Linear mixed-effects models with repeated-measures design quantified the dependent variables, Psychosocial Impact of Assistive Devices Scale, Quebec User Evaluation of Satisfaction with Assistive Technology, Veterans Affairs Low Vision Visual Functioning Questionnaire-48, and Simulator Sickness Questionnaire scores, as a function of the two categorical predictors: group (i.e., personalized telerehabilitation training/control), consumer type (i.e., renter/buyer), as well as their group-by-time/group-by-consumer type/time-by-consumer type interactions, according to a 2 × 2 × 4 factorial design approach (Fig. 1). We constructed four separate linear mixed-effects models that analyzed each of the dependent variables scores as a function of their predictors.
RESULTS
Baseline Characteristics
Recruitment took place from June 2018 to June 2019. A total of 333 eSight users were assessed for eligibility and approached by eSight Corporation. We recruited 57 participants, their mean (standard deviation) age was 54.5 (16.7) years (range, 21 to 82 years), median age was 59.0 years, and 58% were male. Participant characteristics at randomization are presented in the parallel study28 and show comparable descriptive characteristics, albeit with more men in the control group and more retired participants in the control-renters subgroup. Descriptive statistics of the outcome measures for all dependent variables across the four time points are displayed in Appendix Table A1, available at http://links.lww.com/OPX/A494. Participants' compliance with the training in the control group did not differ from the experimental group (χ23 = 2.58, P = .46) when measured at 3 months.
Primary Outcomes
Assistive Technology–related Quality-of-life Measures
Our first linear mixed-effects model revealed a main effect of time on the Psychosocial Impact of Assistive Devices Scale score in both the experimental and control groups (F3,129 = 2.83, P = .04, η2 = 0.05). However, subsequent pairwise comparisons between the different time points (baseline, 2 weeks, 3 and 6 months) did not reveal any specific effects, given that the overall effect size was too small to render any conservative comparisons statistically significant (Fig. 2). However, the comparison approached significance as a statistical trend for this improvement from baseline to 3 months (P = .10), when collapsing both groups. A main effect of consumer type was observed (F1,58 = 5.04, P = .03, η2 = 0.08), indicating that Assistive Devices Scale mean scores from buyers were significantly higher than those of renters. The mean Psychosocial Impact of Assistive Devices Scale score of the participants in the control group was not statistically significantly different (F1,58 = 0.35, P = .56) from the experimental group. Regarding the Psychosocial Impact of Assistive Devices questionnaire subscales, three supplemental models were conducted and revealed main effects of consumer type for the competency (F1,55 = 6.35, P = .02, η2 = 0.10) and the adaptability subscales (F1,57 = 6.64, P = .01, η2 = 0.11), indicating that the buyers' mean was significantly higher than that of renters. No subscales improved statistically significantly over time (all, P > .05), and no trends were observed.
FIGURE 2.
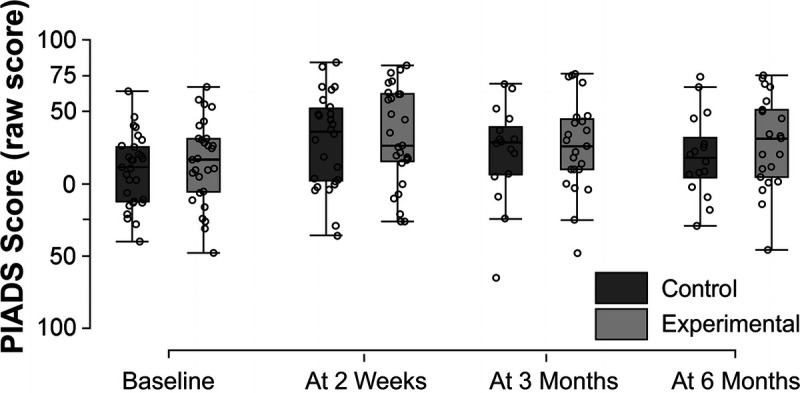
Results of the Psychosocial Impact of Assistive Devices Scale (PIADS) at baseline, 2 weeks, and 3 and 6 months after randomization. The result patterns were similar in the three subscales of this questionnaire. Therefore, the results for the self-esteem, or the competency, or the adaptability domains are not presented here. The score statistically significantly improved over time across participants in both study groups. However, subsequent pairwise comparisons did not reveal any specific effects. None of the subscales improved statistically significantly over time (all, P > .05).
Our second model revealed that the Quebec User Evaluation of Satisfaction with Assistive Technology scores improved over time in both the experimental and control groups (F3,131 = 3.14, P = .03, η2 = 0.05). Pairwise comparisons between the different time points indicated that the mean pre-intervention was significantly lower than that at 3 months after intervention (t135 = 2.80, P = .04, d = 0.61; Fig. 3). None of the other pairwise contrasts or the main effects of group or consumer type were significant (all, P > .05), and no trends were observed. Fifty-seven percent of the participants (30/53) were satisfied with the ease of use of their eSight device (a specific item on the Quebec User Evaluation of Satisfaction with Assistive Technology). There were no differences in our assistive technology–related quality-of-life measures based on age or sex (P > .05).
FIGURE 3.
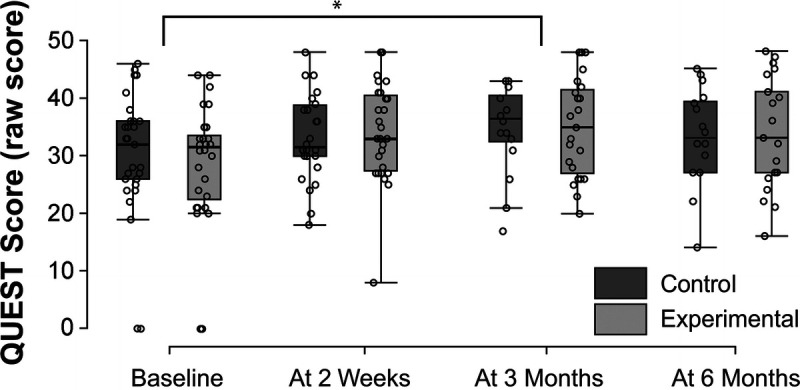
Results of the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST) at baseline, 2 weeks, and 3 and 6 months after randomization. The scores statistically significantly improved over time in both study groups. The mean (standard deviation) baseline score was 29.46 (10.80), which improved to 34.85 (8.19) after 3 months of device use and training. Scores did not demonstrate a significant change after 3 months (all, P > .05). *P < .05.
Secondary Outcomes
Visual Functioning
Using the Veterans Affairs Low Vision Visual Functioning Questionnaire-48, we constructed five separate linear mixed-effects models to examine the overall visual ability score, as well as its subscales using the same analysis pattern as in the previous analyses. The overall model revealed that visual ability improved over time in both the experimental and control groups (F3,124 = 32.54, P < .001, η2 = 0.37). Subsequent pairwise comparisons between the different time points indicated that the mean from pre-intervention (baseline) was significantly lower than that from 2 weeks (t120 = 8.03, P < .001), 3 months (t126 = 7.47, P < .001), and 6 months after intervention (t126 = 7.61, P < .001; Fig. 4). No other pairwise contrast was significant. A main effect of consumer type was observed (F1,58 = 4.82, P = .03, η2 = 0.08), indicating that the mean from the participants who bought the eSight device was significantly higher than that from the participants who rent it. Our subsequent models revealed that all the subscales (i.e., reading, visual mobility, visual information, and visual motor) improved over time in both the experimental and control groups (reading: F3,124 = 26.58, P < .001, η2 = 0.33; visual information: F3,124 = 31.93, P < .001, η2 = 0.37; visual motor: F3,124 = 22.26, P < .001, η2 = 0.29; and visual mobility: F3,121 = 8.35, P < .001, η2 = 0.13, respectively). Pairwise comparisons indicated that the mean from pre-intervention was significantly lower than that from 2 weeks, 3 months, and 6 months after intervention for reading, visual information, visual motor, and visual mobility (Table 1). No other pairwise contrasts were significant (all, P > .05). A main effect of consumer type was observed for the visual mobility–related model only (F1,56 = 10.11, P = .002, η2 = 0.16), indicating that the mean score from the buyers was significantly higher than that of renters. Overall, in each of the five models tested, scores of the participants of the experimental group were not statistically significantly different from the control group. Participants who remained in the study did not report better success in the two quality-of-life or functional vision measures compared with those who withdrew from the study (t51 = 1.75, P = .09; d = 0.52, U = 358, P = .23, rank biserial correlation = 0.21; and t51 = 1.15, P = .26, d = 0.34, respectively). There were no differences in visual functioning measures based on age or sex (P > .05).
FIGURE 4.
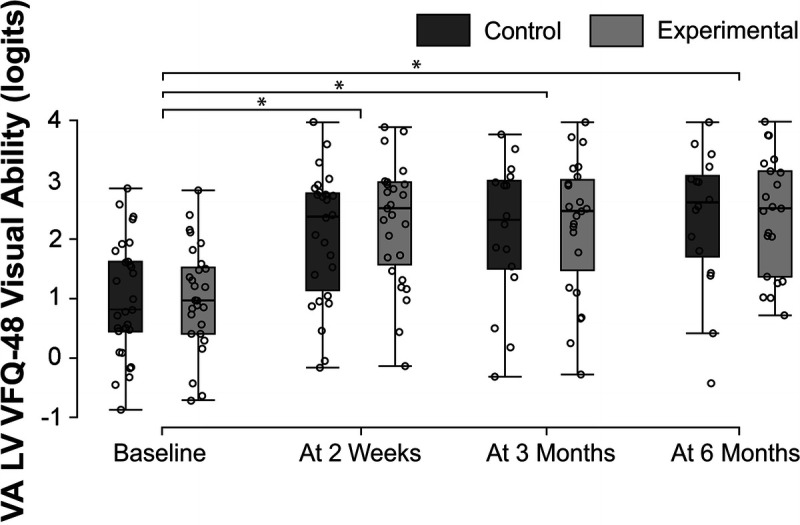
Results of the Veterans Affairs Low Vision Visual Functioning Questionnaire-48 (VA LV VFQ-48) at baseline, 2 weeks, and 3 and 6 months after randomization. Results for the reading, or the visual information, or the visual motor, or the mobility domains are not presented here because the patterns were similar in four subscales of the questionnaire. Visual ability statistically significantly improved over time in both study groups. The mean (standard deviation [SD]) baseline visual ability score was 0.99 (0.93) logit units, which improved to 2.19 (1.07) logits, 2.35 (1.05) logits, and 2.38 (1.07) logits after 2 weeks and 3 and 6 months of device use and training, respectively. *P < .05.
TABLE 1.
Veterans Affairs Low Vision Visual Functioning Questionnaire-48 subscales statistical analyses pairwise comparisons
| Mean difference (logits) |
95% confidence interval | df | t | P | Cohen d value | |
|---|---|---|---|---|---|---|
| Reading subscale | ||||||
| T0–T2 weeks | −2.2 | −6.26 to 1.87 | 119 | 7.659 | <.001 | 1.24 |
| T0–T3 months | 1.02 | −5.33 to 7.38 | 126 | 6.513 | <.001 | 1.14 |
| T0–T6 months | −2.17 | −5.72 to 1.38 | 127 | 6.365 | <.001 | 1.35 |
| Visual information subscale | ||||||
| T0–T2 weeks | −1.29 | −3.58 to 1.01 | 120 | 7.962 | <.001 | 1.16 |
| T0–T3 months | −1.30 | −3.63 to 1.02 | 126 | 6.987 | <.001 | 1.26 |
| T0–T6 months | −1.41 | −3.85 to 1.04 | 126 | 7.854 | <.001 | 1.46 |
| Visual motor subscale | ||||||
| T0–T2 weeks | −1.03 | −3.14 to 1.09 | 120 | 6.610 | <.001 | 1.03 |
| T0–T3 months | −1.17 | −3.25 to 0.91 | 125 | 6.464 | <.001 | 1.09 |
| T0–T6 months | −1.11 | −3.65 to 1.44 | 125 | 6.059 | <.001 | 1.04 |
| Visual mobility subscale | ||||||
| T0–T2 weeks | −0.66 | −2.80 to 1.49 | 118 | 4.395 | <.001 | 0.58 |
| T0–T3 months | −0.88 | −2.97 to 1.22 | 124 | 4.395 | <.001 | 0.86 |
| T0–T6 months | −0.73 | −3.04 to 1.57 | 124 | 2.889 | .03 | 0.67 |
Pairwise comparisons indicated that the mean from pre-intervention (T0) was significantly lower than that from 2 weeks, 3 months, and 6 months after intervention for reading, visual information, visual motor, and visual mobility subscales. The results are combined from all participants in both study groups.
Cybersickness
We constructed a linear mixed-effects model that followed the same structure as the previous models. No significant differences emerged (all, P > .05), indicating that scores were stable over the 6-month period, and training type did not affect cybersickness scores. When analyzing the different subscores of the questionnaire after 2 weeks of device use, to the question evaluating how much the symptom is affecting the user and considering the oculomotor-related symptoms subscore, 29% responded none, 43% slight, 23% moderate, and 5% severe. Regarding the nausea-related symptoms subscale, 89% responded none, 8% slight, 3% moderate, and 0% severe. Finally, regarding the disorientation-related symptoms subscale, 75% responded none, 17% slight, 7% moderate, and 1% severe.
DISCUSSION
We carried out a randomized study of telerehabilitation for persons with low vision using a head-mounted display to assess the effect of this rehabilitation modality on quality of life, self-reported functional vision, and cybersickness. We observed that the Psychosocial Impact of Assistive Devices Scale and scores on the Quebec User Evaluation of Satisfaction with Assistive Technology questionnaire increased for all participants (in both the experimental and control groups) between baseline and 3 months of device use, indicating that assistive technology–related quality of life improved independently of the type of training during the early months of use. We detected improvement in early (within the first 2 weeks) functional vision outcomes using the Veterans Affairs Low Vision Visual Functioning Questionnaire-48 in all participants, regardless of group types. Either the training is indeed sufficient, which explains why a plateau is reached within the first 2 weeks for functional capacities or after 3 months for quality-of-life measures, or the training is not sufficient and needs more sessions to exceed this plateau. Because the effects of training and practice are difficult to dissociate, it is also possible that the improvement is only related to the use of the eSight device and not to training. It is important to mention that the findings for the training are relevant for this group of participants who may or may not be representative of all individuals who obtain an eSight device. Indeed, there was a high proportion of eligible individuals who declined to participate (79%) likely because of a lack of interest in the study. They may have different training needs from those who were studied. We did not observe changes in patient-reported cybersickness outcomes in either group.
Assistive Technology–related Quality-of-life Outcomes
The data indicate that assistive technology–related quality of life did not improve within the first 2 weeks. This may be because this construct is related to more global changes, which may take longer to manifest. Different psychosocial factors have been related to each other in the two complementary questionnaires that were used and that focused on the assistive technology experience. They are included within the construct of quality of life and constitute at least a portion of this complex construct. The quality-of-life improvement across time measured in eSight users, as reflected in improved Psychosocial Impact of Assistive Devices Scale scores (i.e., perceiving a higher positive impact of the device on their quality of life) and Quebec User Evaluation of Satisfaction with Assistive Technology scores (i.e., reporting higher satisfaction with the device), could explain the relatively low rate of eSight discontinuance. Indeed, this rate was reported as being 16% in a publication focusing on the feasibility aspect of this study28 compared with the 23% measured in eSight users during the 3-month study period7 and the 30% discontinuance rate of assistive technology use traditionally observed in the literature.34 These results align with predictors of head-mounted device use documented in a cross-sectional study, whereby device owners who reported higher scores in these two assistive technology–related quality-of-life questionnaires were consistently more likely to continue using eSight Eyewear.11 Contrary to the Psychosocial Impact of Assistive Devices Scale scores, different reasons may explain why we only found a main effect but no differences on subsequent pairwise comparisons among the different time points for the Quebec User Evaluation of Satisfaction with Assistive Technology scores. One plausible hypothesis is that the latter questionnaire focuses specifically on the user satisfaction with the device and involves practical/immediate changes (i.e., weight, size, efficiency, delivery services), whereas the former involves more global changes (i.e., self-esteem, competency, adaptability) that may take longer to manifest. The context of our small sample size may also make it more difficult to find effects among the different time points. Insofar as all participants were already using at least one assistive device for reading or magnification at baseline, it is also likely that quality-of-life scores at baseline were already high and did not allow the eSight device to significantly improve the scores. In addition, it is worth highlighting that the Quebec User Evaluation of Satisfaction with Assistive Technology score improvement at 3 months was not maintained at 6 months. After extended use of the device and potential exposure to new activities, it is likely that the eSight device was unable to meet or no longer met certain needs. After several months, it is also probable that social desirability35 was less pronounced and that participants provided more realistic/honest responses. We did not observe a difference between the two training approaches, suggesting that the technical training offered by the company has the same effect on these quality-of-life measures as individualized training provided by a low vision therapist through telerehabilitation. It is possible that no training would also have an increase in assistive technology–related quality-of-life scores just by virtue of using the eSight unit only and should be considered in future studies.
Very few studies have explored human and quality-of-life factors in relation to head-mounted display use. One study emphasized that head-mounted display users perceived ease of usability (especially of device controls and screen) as equally important as visual improvement (Jeganathan VSE, et al. IOVS 2019;60:ARVO E-Abstract 4036). In this study, semistructured usability interviews documented that, among three head-mounted display types, 50% of participants showed an overall preference for the eSight device (vs. NuEyes [NuEyes Technologies Inc., Newport Beach, CA] or Epson [Epson America, Inc., Los Alamitos, CA]). This finding supports the subjectively reported success of this device by their users and aligns with the ease of use reported by the majority of our participants. It should be highlighted that insofar as a sizable proportion (43%) of participants are less satisfied with ease of use of the eSight device, the research and development department of the company should focus future efforts on optimizing usability.
Functional Vision Outcomes
Unlike the quality-of-life measures that improved after 3 months (intermediate effects) of practice and training with the device, eSight usage and training yielded immediate (within the first 2 weeks) improvements (large effect) in self-reported functional vision as reflected in the overall visual ability score and all its subscores (i.e., reading, visual information, mobility, visual motor) and continued to improve during the first 3 months. These results align with a previous multicenter study,7 whereby eSight introduction yielded immediate improvements in visual ability measured with the Melbourne Low Vision Activities of Daily Living Index.36 Mirroring our results, functional vision performance did not change further after the 3-month follow-up period.7 In this study, overall, participants' Veterans Affairs Low Vision Visual Functioning Questionnaire-48 scores (administered at baseline and after 3 months of use) indicated significant improvement (intermediate effect) in their visual abilities with device use and training. This improvement was largely driven by the reading subscale (large effect), followed by changes in the visual information items (large effect). However, contrary to our present findings, there was no significant change among the mobility items. This may be explained by the device design differences between the two studies, with eSight 3 being less immersive than eSight 2. Improvement in mobility may be attributed to change in the perception of the environment observed through the head-mounted display. Insights into how computer-assisted sight enabled individuals with visual impairment to see the environment in ways previously unavailable was recently explored.37 Interestingly, the steps described by eSight users to build a mental model of their physical environment are similar to the strategy used by a game designer creating a virtual environment. Some participants self-reported the experience of seeing better than family or friends in their environment with normal sight, for example, being able to see small details at a great distance using the eSight device, blurring the borders between assistive and augmentative technology. Replicating previous findings,8 a new generation of head-mounted displays being used in augmented reality improved the ability to perform timed daily living tasks at all viewing distances (Kammer R, et al. IOVS 2019;91:ARVO E-Abstract 989). Previous research on head-mounted low vision aids has reported that device usage and/or training is important for reading.38 This was especially the case when aiming to improve complex functional vision tasks38; similarly, our participants self-reported improvement in their reading skills over time. Interestingly, eSight buyers exhibited higher scores of quality of life related to assistive technology and functional vision. One hypothesis that may explain these findings is of a psychological nature, whereby cognitive dissonance39 may explain that the money spent to purchase a device can induce a change in judgment and motivate buyers to use their device more than people who have rented it.
Cybersickness and Visual Discomfort Symptoms
The cybersickness score was stable over the 6-month period and was independent of training type. Most users reported having only slightly oculomotor-related symptoms (cybersickness condition), whereas only few were severely affected. In parallel, a low device use discontinuance rate was reported with these participants. Insofar as oculomotor-related symptoms (headache) associated with head-mounted display use have been identified as a predictor of use discontinuance,11 these findings are congruent. The large majority of users did not experience nausea-related symptoms (referring to motion sickness condition) and/or disorientation-related indications (reflecting simulator sickness condition), and few of them reported having felt such symptoms severely.40 Among those who withdrew from the study or discontinued eSight usage, none had reported any of these symptoms as being the cause. Of the 74 participants who joined a previous multicenter trial, 17 discontinued their usage during the 3-month study period. Among them, only one exhibited nausea,7 one of the most extreme and unpleasant symptoms. However, the presence of general discomfort or eyestrain was not associated with use discontinuance11; however, it is possible that the presence (and type and severity) of cybersickness and related symptoms is underestimated because it was not systematically investigated then.
Although cybersickness and visual discomfort were more extensively and accurately investigated in the present study, few participants were severely affected. This may be explained by the fact that head-mounted displays, such as eSight, do not use a complete immersive virtual environment made of a synthetic image but a semi-immersive environment with a real image and an unoccluded peripheral visual field. Other potential reasons may include the duration of the exposure to the virtual environment and the likely sensory adaptation; for instance, one study documented that the experience of cybersickness mainly occurred within the first 10 minutes of exposure to the virtual environment.14 A systematic review documented that children have the greatest susceptibility to cybersickness, and this rapidly decreases from adolescence to adulthood.41 Given the older population recruited in the context of our study, this could explain why our participants were less susceptible to exhibit notable experience of cybersickness. Device factors, such as lag,13 calibration of interpupillary distance, and general ergonomics, such as heavy and inappropriate fitting headsets,23 can also contribute to cybersickness symptoms. Awareness of these factors is essential to increase the adoption of the technology and the continued improvement of the virtual technology.
Different potential reasons may explain why we did not find differences on our outcome measures between the two interventions. It is possible that the selected measures did not allow for the differentiation of the effects of telerehabilitation compared with self-training. Exploration of most common measures, such as standardized reading speed tools, reading speed (meaningfully improved in handheld magnifier users receiving telerehabilitation42), or evaluation of functional vision with more practical functional vision assessments (e.g., the Melbourne Low Vision ADL Index36 test) may have been more sensitive to reveal a difference between the two interventions. Eccentric fixation training was only provided in the context of telerehabilitation, and as suggested by the low vision therapist, it is likely that six sessions for 2 weeks were insufficient, especially for participants who needed eccentric fixation training, to detect difference between the two interventions. Because the low vision therapist focused on relatively simple activities of daily living (e.g., spot reading), it would be meaningful to follow up participants beyond 6 months to explore if telerehabilitation has a long-term and transferable effect on more complex activities (e.g., gardening, playing an instrument, or a specific sport) compared with self-training. Another potential reason that could explain the lack of differences in outcomes between the intervention groups may be related to the characteristics of the participants. They were potentially tech-savvy, mostly younger to middle-aged adults who may be able to independently master using the eSight technology without needing much training or professional assistance. Although we chose to focus on a new form of visual aid that is increasingly used by the low vision population, we anticipate that it could be feasible to provide telerehabilitation to optimize the use of more common low vision aids (e.g., handheld magnifiers and closed-circuit televisions). This modality has already been applied to users of magnifiers in small samples where the authors indicated the need to conduct a larger-scale randomized study (Bittner AK, et al. IOVS 2019;60:ARVO E-Abstract 4030).42
Limitations
The study participants were not representative of the general low vision population, and the study findings may not be generalizable to all future eSight users. Indeed, the study population had greater access to technology (all owned a computer, had access to the Internet, and were already accustomed to using other visual assistive devices) than did most people with low vision who are older adults, possibly leading them to be more willing to try technology used for telerehabilitation and/or video conferencing. However, this limitation will probably be less contextual over the next decades with upcoming generations. Even if it was not the case for low vision individuals who are the recipients of an eSight device, it is important to highlight that the requirement to have a computer or tablet may have excluded those with demographic disparities related to age, sex, or socioeconomic status or people who are not accustomed to using technology. Self-selection bias needs to be considered, as we enrolled participants who spontaneously decided to rent or purchase eSight Eyewear. In addition, a very large proportion of those who were eligible for the study had declined to participate (79%); there may be inherent differences among those who choose to participate versus those who did not, which could affect the study findings and conclusions about the two interventions. A limitation of the current study that may impact outcomes is that the two randomized groups were not balanced in terms of duration and level of visual impairment. A methodological limitation concerns the difference in the administration methods for the questionnaires at baseline versus follow-ups. The potential influence of the low vision therapist at baseline toward participants' answer (e.g., social desirability, whereby participants want to please the therapist and may report more positively) versus self-administration at follow-ups (e.g., they may be more comfortable reporting their actual experience and perceptions) may have induced a bias in the outcomes. Another potential limitation that relates to the online survey nature of data collection is the lack of objective visual function measures (i.e., visual acuity or contrast sensitivity) that could contribute to a more holistic description of our participants. However, allowing for enrollment and participation across both rural and urban environments, our approach made it possible to reach a wide range of individuals with visual impairment using eSight Eyewear. Isolating the effect of providing the device from the intervention modality would only be possible by adding a third group to the implemental design that receives a device with a delayed intervention; however, future studies would need to first overcome the ethical and commercial implications of such an approach. Despite high accessibility and acceptability of the telerehabilitation,28 challenges may have been underestimated in the protocol. Telerehabilitation may challenge personal privacy and confidentiality,43 as video conferencing makes the participants' personal space visible to the clinician and may be perceived as an intrusion into their home.44 Although specific attention had been taken to ensure privacy (user empowerment, controlling when and how the session is initiated and terminated), it was unknown if privacy was an issue because it was not assessed during the study. Future studies will need to address this limitation. Finally, we did not assess the cognitive status of our participants; however, the low vision therapist systematically judged whether participants had sufficient cognition to complete protocol procedures using her clinical judgment and excluded them if comprehension and/or communication was challenged. Insofar as most people with low vision are older adults, it would be relevant for future studies to use a cognitive screening measure. We did not observe differences in our outcomes based on age or sex; however, future studies will need to focus on older adults who acquire eSight Eyewear to explore if they need more support via telerehabilitation with a therapist, as compared with younger low vision participants.
CONCLUSIONS
This is the only randomized study we are aware of that explores the impact of telerehabilitation on quality of life and self-reported functional vision in individuals with low vision using assistive technology. Independent of the training type, head-mounted display users' visual abilities and quality of life increased over time, after 2 weeks and 3 months of device use, respectively. The study findings fail to demonstrate a difference between conducting telerehabilitation and self-training where quality-of-life outcomes are concerned. Future studies should specifically focus on further exploring whether it is more resource- and time-efficient to allow head-mounted display users to self-train using the device manufacturer's instructions rather than involve a professional rehabilitation therapist. Insofar as the current study findings may not be generalizable to all future eSight users, it will be important to determine whether participant characteristics are predictive of training success when learning to use eSight or other virtual reality/augmented devices for vision augmentation. Our participants did not extensively report cybersickness; it remained stable over the 6-month period and was independent of training type and did not emerge as a widespread usability issue. Given the increasing use of such technologies in low vision rehabilitation and the limited literature available on the link between cybersickness and head-mounted displays for low vision, further exploration of its mechanisms and associated factors is essential to improve methods to reduce cybersickness. To the extent that the use of such technologies involves a physical and psychological transformation, the systematic evaluation of the psychosocial factors and potential cybersickness should be included during the acquisition of head-mounted displays to optimize their adoption.
Supplementary Material
Footnotes
Supplemental Digital Content: Appendix Table A1, available at http://links.lww.com/OPX/A494, displays descriptive statistics of the outcome measures for all dependent variables across the four time points. Dispersion measures are represented using the mean, median, and interquartile range for all the variables.
Funding/Support: Mitacs (IT08595 Grant; to M-CL) and Fonds de Recherche du Québec—Santé (Junior 2 chercheur boursier Career Award No. 281454; to WW).
Conflict of Interest Disclosure: None of the authors have reported a financial conflict of interest. The sponsor facilitated subject recruitment; however, the sponsor was not involved in study design, analyses, and interpretation. The authors were responsible for the preparation of this article and the decision to submit this article for publication. Each of the authors had access to the study data and takes full responsibility for his/her presentation in this article.
Author Contributions and Acknowledgments: Conceptualization: M-CL, WW; Data Curation: M-CL; Formal Analysis: M-CL, WW; Funding Acquisition: M-CL; Investigation: M-CL; Methodology: M-CL, WW; Project Administration: M-CL; Resources: WW; Software: M-CL; Supervision: WW; Validation: WW; Writing – Original Draft: M-CL; Writing – Review & Editing: M-CL, WW.
The authors thank Dr. Aaron Johnson for his advices for conducting mixed-effects model analyses, Josée Duquette for her permission to use the VisExc-INLB eccentric fixation program, and Nancy Primeau for her support for the formatting of bibliographic references.
Supplemental Digital Content: Direct URL links are provided within the text.
REFERENCES
- 1.World Health Organization . Blindness and Vision Impairment; 2019. Available at: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment. Accessed October 16, 2019.
- 2.Corn A, Lusk KE. Perspectives on Low Vision. In: Corn A, Koenig A, eds. Foundations of Low Vision: Clinical and Functional Perspectives. 2nd ed. New York, NY: AFB Press; 2010:3–25. [Google Scholar]
- 3.Markowitz SN. Principles of Modern Low Vision Rehabilitation. Can J Ophthalmol 2006;41:289–312. [DOI] [PubMed] [Google Scholar]
- 4.Trauzettel-Klosinski S. Rehabilitation for Visual Disorders. J Neuroophthalmol 2010;30:73–84. [DOI] [PubMed] [Google Scholar]
- 5.Hwang AD, Peli E. An Augmented-reality Edge Enhancement Application for Google Glass. Optom Vis Sci 2014;91:1021–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Luo G, Woods RL, Peli E. Collision Judgment when Using an Augmented-vision Head-mounted Display Device. Invest Ophthalmol Vis Sci 2009;50:4509–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wittich W Lorenzini MC Markowitz SN, et al. The Effect of a Head-mounted Low Vision Device on Visual Function. Optom Vis Sci 2018;95:774–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Culham LE, Chabra A, Rubin GS. Clinical Performance of Electronic, Head-mounted, Low-vision Devices. Ophthalmic Physiol Opt 2004;24:281–90. [DOI] [PubMed] [Google Scholar]
- 9.Stelmack JA Tang XC Wei Y, et al. Outcomes of the Veterans Affairs Low Vision Intervention Trial II (LOVIT II): A Randomized Clinical Trial. JAMA Ophthalmol 2017;135:96–104. [DOI] [PubMed] [Google Scholar]
- 10.Lorenzini MC, Wittich W. Factors Related to the Use of Magnifying Low Vision Aids: A Scoping Review. Disabil Rehabil 2020;42:3525–37. [DOI] [PubMed] [Google Scholar]
- 11.Lorenzini MC, Hamalainen AM, Wittich W. Factors Related to the Use of a Head-mounted Display for Individuals with Low Vision [published online December 28, 2019]. Disabil Rehabil 2019. doi: 10.1080/09638288.2019.1704892. [DOI] [PubMed] [Google Scholar]
- 12.Day H, Jutai J, Campbell KA. Development of a Scale to Measure the Psychosocial Impact of Assistive Devices: Lessons Learned and the Road Ahead. Disabil Rehabil 2002;24:31–7. [DOI] [PubMed] [Google Scholar]
- 13.LaViola JJ., Jr.A Discussion of Cybersickness in Virtual Environments. SIGCHI Bull 2000;32:47–56. [Google Scholar]
- 14.Cobb SV Nichols S Ramsey A, et al. Virtual Reality–induced Symptoms and Effects (VRISE). Presence Teleop Virt Environ 1999;8:169–86. [Google Scholar]
- 15.Peli E. Visual Perceptual, and Optometric Issues with Head-mounted Displays (HMD). Playa del Rey, CA: Society for Information Display; 1996. Available at: https://pelilab.partners.org/papers/Visual%20and%20optometric%20issues%20with%20head-mounted%20displays.pdf. Accessed April 13, 2021. [Google Scholar]
- 16.Hooper P Jutai JW Strong G, et al. Age-related Macular Degeneration and Low-vision Rehabilitation: A Systematic Review. Can J Ophthalmol 2008;43:180–7. [DOI] [PubMed] [Google Scholar]
- 17.Gold D, Zuvela B, Hodge WG. Perspectives on Low Vision Service in Canada: A Pilot Study. Can J Ophthalmol 2006;41:348–54. [DOI] [PubMed] [Google Scholar]
- 18.Brennan DM Tindall L Theodoros D, et al. A Blueprint for Telerehabilitation Guidelines—October 2010. Telemed J E Health 2011;17:662–5. [DOI] [PubMed] [Google Scholar]
- 19.Bittner AK Yoshinaga PD Wykstra SL, et al. Telerehabilitation for People with Low Vision. Cochrane Database Syst Rev 2020;2:CD011019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Crossland MD, Silva RS, Macedo AF. Smartphone, Tablet Computer and E-reader Use by People with Vision Impairment. Ophthalmic Physiol Opt 2014;34:552–7. [DOI] [PubMed] [Google Scholar]
- 21.Martiniello N Eisenbarth W Lehane C, et al. Exploring the Use of Smartphones and Tablets among People with Visual Impairments: Are Mainstream Devices Replacing the Use of Traditional Visual Aids? Assist Technol 2019;1–12. [DOI] [PubMed] [Google Scholar]
- 22.Kolasinski EM. Simulator Sickness in Virtual Environments. United States Army Research Institute for Behavioral and Social Sciences; 1995. Available at: https://apps.dtic.mil/dtic/tr/fulltext/u2/a295861.pdf. Accessed April 13, 2021.
- 23.McCauley ME, Sharkey TJ. Cybersickness: Perception of Self-motion in Virtual Environments. Presence Teleop Virt Environ 1992;1:311–8. [Google Scholar]
- 24.Lorenzini MC, Wittich W. Measuring Changes in Device Use of a Head-mounted Low Vision Aid After Personalised Telerehabilitation: Protocol for a Feasibility Study. BMJ Open 2019;9:e030149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.eSight Corporation . Eskills User Guide & Proficiency Program. Toronto, Ontario, Canada: The Corporation; 2015. [Google Scholar]
- 26.Overbury O, Conrod EB. McGill Low Vision Manual. Montreal, Quebec, Canada: Betacom Group; 1997. [Google Scholar]
- 27.Duquette J, Lapointe N, Loiselle J. Visexc-Inlb: Method of Evaluation and Training in Eccentric Vision of the Nazareth and Louis-Braille Institute: User Manual. Longueuil, Quebec, Canada: Institut Nazareth et Louis-Braille; 2013. [Google Scholar]
- 28.Lorenzini MC, Wittich W. Personalized Telerehabilitation for a Head-mounted Low Vision Aid: A Randomized Feasibility Study. Optom Vis Sci 2021;98:570–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Day H, Jutai J. Measuring the Psychosocial Impact of Assistive Devices: The PIADS. Can J Rehabil 1996;9:159–68. [Google Scholar]
- 30.Demers L, Weiss-Lambrou R, Ska B. Development of the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST). Assist Technol 1996;8:3–13. [DOI] [PubMed] [Google Scholar]
- 31.Stelmack JA Szlyk JP Stelmack TR, et al. Psychometric Properties of the Veterans Affairs Low-vision Visual Functioning Questionnaire. Invest Ophthalmol Vis Sci 2004;45:3919–28. [DOI] [PubMed] [Google Scholar]
- 32.Stelmack JA, Massof RW. Using the VA LV VFQ-48 and LV VFQ-20 in Low Vision Rehabilitation. Optom Vis Sci 2007;84:705–9. [DOI] [PubMed] [Google Scholar]
- 33.Kennedy RS Lane NE Berbaum KS, et al. Simulator Sickness Questionnaire: An Enhanced Method for Quantifying Simulator Sickness. Int J Aviat Psychol 1993;3:203–20. [Google Scholar]
- 34.Scherer MJ Sax C Vanbiervliet A, et al. Predictors of Assistive Technology Use: The Importance of Personal and Psychosocial Factors. Disabil Rehabil 2005;27:1321–31. [DOI] [PubMed] [Google Scholar]
- 35.Fisher RJ, Katz JE. Social-desirability Bias and the Validity of Self-reported Values. Psychol Market 1999;17:105–20. [Google Scholar]
- 36.Haymes SA, Johnston AW, Heyes AD. The Development of the Melbourne Low-vision ADL Index: A Measure of Vision Disability. Invest Ophthalmol Vis Sci 2001;42:1215–25. [PubMed] [Google Scholar]
- 37.Zolyomi A, Shukla A, Snyder JL. Technology-mediated Sight: A Case Study of Early Adopters of a Low Vision Assistive Technology. In: ASSETS '17 Proceedings of the 19th International ACM SIGACCESS Conference on Computers and Accessibility 2017. Available at: 10.1145/3132525.3132552. Accessed April 13, 2021. [DOI]
- 38.Kinateder M Gualtieri J Dunn MJ, et al. Using an Augmented Reality Device as a Distance-based Vision Aid—Promise and Limitations. Optom Vis Sci 2018;95:727–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Festinger L. Cognitive Dissonance. Sci Am 1962;207:93–102. [DOI] [PubMed] [Google Scholar]
- 40.Deemer AD Swenor BK Fujiwara K, et al. Preliminary Evaluation of Two Digital Image Processing Strategies for Head-mounted Magnification for Low Vision Patients. Transl Vis Sci Technol 2019;8:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kolasinski EM. Simulator Sickness in Virtual Environments: Technical Report 1027; 1995. Available at: https://apps.dtic.mil/dtic/tr/fulltext/u2/a295861.pdf. Accessed October 12, 2019.
- 42.Bittner AK Yoshinaga P Bowers A, et al. Feasibility of Telerehabilitation for Low Vision: Satisfaction Ratings by Providers and Patients. Optom Vis Sci 2018;95:865–72. [DOI] [PubMed] [Google Scholar]
- 43.Gelinas-Bronsard D Mortenson WB Ahmed S, et al. Co-construction of an Internet-based Intervention for Older Assistive Technology Users and Their Family Caregivers: Stakeholders' Perceptions. Disabil Rehabil Assist Technol 2019;14:602–11. [DOI] [PubMed] [Google Scholar]
- 44.Burns RB Crislip D Daviou P, et al. Using Telerehabilitation to Support Assistive Technology. Assist Technol 1998;10:126–33. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


