Abstract
Purpose
The present study aimed to assess the influence of personality traits on the variability of sensitivity to pain in two distinct groups of healthy subjects with low versus high sensitivity to pain (LSP vs HSP, respectively).
Methods
Healthy subjects (n=156) were allocated to two groups according to their tolerability to cold stimulation (cold pressor test, CPT, 1°C). Group LSP (n=76) reached the cut-off time of 180±0 sec, and a size matched group of HSP (n=80) tolerated the CPT for an average of 10.5±3.4 sec only. Subjects from both groups completed the self-reported pain sensitivity questionnaire (PSQ), the Pain Catastrophizing Scale (PCS), and the Neuroticism Extraversion Openness - Five Factor Inventory (NEO-FFI).
Results
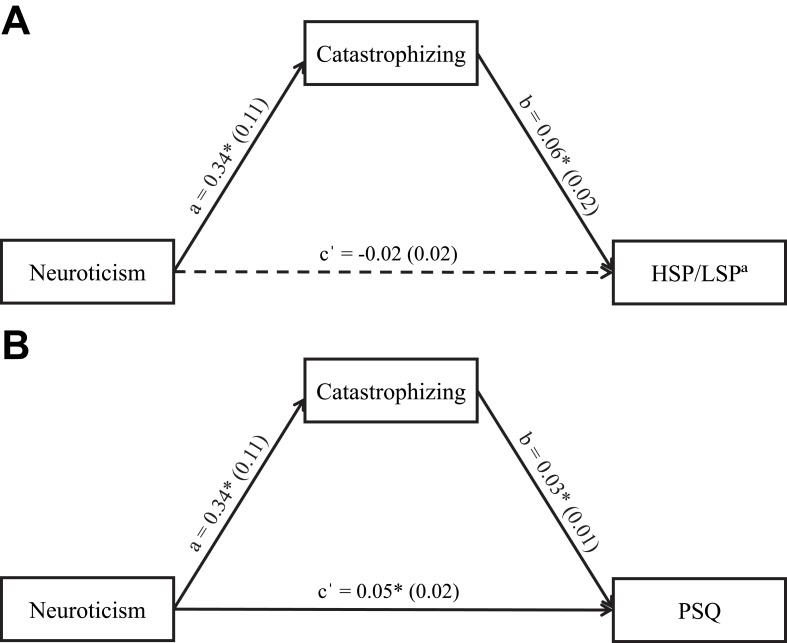
In comparison to the LSP group, HSP individuals had higher scores of PSQ (p<0.001), catastrophizing (p=0.001), and extraversion (p=0.01). By adjusting for age and gender, mediation analyses revealed that catastrophizing mediated the relationship between neuroticism and pain sensitivity, both in the allocation of subjects to a certain group of sensitivity to pain (LSP or HSP, B=0.02 95% CI: 0.006–0.040) and in the PSQ score (B=0.01 95% CI: 0.001–0.023).
Conclusion
These results, which were demonstrated by two different prisms (CPT and PSQ), point to the potential of the five-factor inventory and pain catastrophizing scale as tools for identifying specific personality traits associated with a high sensitivity to pain.
Keywords: personality traits, sensitivity to pain, FFM, pain catastrophizing, PSQ
Introduction
Experimental models of evoked pain by quantitative sensory testing (QST) and self-report pain questionnaires (eg, Pain Sensitivity Questionnaire, PSQ) are commonly used to explore and demonstrate inter-individual differences in pain perception in healthy subjects and in clinical settings.1,2 Although it is widely recognized that inter-individual differences exist, studies have yielded conflicting evidence regarding the contribution of personality traits and cognitive-affective factors to these variations.3–5
Using experimental pain models, numerous studies on healthy subjects showed relationships between sensitivity to pain and the personality traits of neuroticism,6–10 extraversion,11–13 and pain catastrophizing.14–17 For example, individuals with high scores of neuroticism exhibited a short pain tolerance,9 a high pain intensity10 and high scores on self-reported sensitivity to pain questionnaires;6,8 subjects with high scores of extraversion demonstrated a long pain tolerance12 and high pain thresholds;13 and finally, participants with high scores of catastrophizing reported a high pain intensity16,18 and short pain tolerance.17
Neuroticism is considered as a higher-order broad personality domain which has been shown to have associations with some pain-related cognitive and behavioral lower-order traits, such as pain catastrophizing.15,19–21 Pain catastrophizing has been associated with sensitivity to pain in healthy pain-free individuals exposed to various experimental evoked-pain paradigms, as well as in patients with chronic pain conditions,16,22–24 and has appeared as a solid predictor of pain.15,16,24 Furthermore, both neuroticism and catastrophizing have been shown to have mediation relationships to pain related responses (eg, pain vigilance, pain anxiety) rather than to have responses to actual painful stimuli.25–28
In an attempt to investigate the role of personality in the variability of pain perception, several studies adopted the Five-Factor Model (FFM) theory of personality.29 According to this theory, a variety of behaviors and a comprehensive set of traits can be attributed and generalized into five broad domains of characters: Neuroticism, Extraversion, Openness to Experience, Agreeableness, and Conscientiousness. Although the FFM has been used to study associations between personality and pain both in clinical26,30–32 and experimental pain settings,7,10,27,33,34 the findings have been inconsistent, leaving these associations open for further research.
To further explore the complex relationships between personality and pain perception, the present study focused on two extreme groups of healthy subjects with low vs high sensitivity to pain. The study aims were to: (1) determine if the subjects in these groups differed in their personality traits; and (2) examine further relationships between personality traits and sensitivity to pain.
Materials and Methods
Subjects
The study protocol was conducted in accordance with the Declaration of Helsinki and was approved by the local ethics committee of the University of Haifa (no. 165/16). Inclusion criteria included: 1) Healthy males and females over the age of 18; 2) Free from chronic pain of any type; 3) No medication use (except for oral contraceptives); and 4) Able to understand the purpose and instructions of the study. Subjects suffering from any painful conditions, those using medications or recreational drugs, or pregnant women were excluded from the study. Eligibility to participate in the study was based on self-completed questionnaires.
Instruments and Measurements
Pain Sensitivity-Related Measurements
Cold Pressor Test (CPT)
The CPT was administered using Heto CBN 8–30 Lab equipment, Allerod, Denmark; a temperature-controlled water bath with a maximum temperature variance of ± 0.5°C which is continuously stirred by a pump. In this study we used the CPT for defining two extreme groups by time to hand withdrawal (tolerance). Subjects were asked to place their dominant hand in the CPT bath at 1°C and to maintain their hand in the cold water for as long as possible. The latency to intolerability (spontaneous hand removal) was defined as pain tolerance (sec). For safety reasons, a cut-off time of 180 s was set.
Self-Reported Pain Sensitivity: Pain Sensitivity Questionnaire (PSQ)
The PSQ is a valid and reliable self-reported questionnaire based on pain magnitude scores of imagined painful daily life situations in different somatosensory sub-modalities.2 The PSQ total score has shown a modest correlation with experimental thermal pain threshold, tolerance, and intensity.2,8,35 The PSQ contains 17 items: fourteen items relate to situations that are usually considered to be painful for most persons covering a variety of different pain qualities, while three items (items 5, 9, 13) describe normally non-painful situations. Pain magnitude is rated on a 0–10 scale with one anchor at 0, representing ‘no pain at all’, and the other anchor at 10, representing the ‘worst pain one can imagine’. A mean score is used for calculating the total PSQ scale. Bar-Shalita et al36 validated the PSQ to Hebrew.
Personality Questionnaires
Pain Catastrophizing Scale (PCS)
Catastrophizing was assessed by the Pain Catastrophizing Scale (PCS) developed by Sullivan et al24 using the validated Hebrew version.37 The instrument includes 13 items representing the three components of pain catastrophizing: rumination, magnification and helplessness. Items are rated on a Likert scale ranging from 0 = not at all to 4 = all the time.
The Neuroticism Extraversion Openness - Five Factor Inventory (NEO-FFI)
Personality was assessed using the Hebrew version of the NEO-Five Factor Inventory (NEO-FFI) questionnaire based on the ‘Big Five’ theory of personality.38 There are 60 statements in this self-rating questionnaire, 12 for each of the big five factors: Neuroticism, Extraversion, Agreeableness, Openness, Conscientiousness. For each item, participants rate their agreement or disagreement on a five-point Likert type scale ranging from “completely disagree” to “fully agree”. Scores are based on a sum for each of the five personality dimensions.
Study Design
The subjects were enrolled through advertisements distributed on a campus bulletin board at the University of Haifa. After meeting the inclusion criteria, subjects were invited to participate in the study. All eligible subjects received a full explanation on the purpose of the study and signed the informed consent form. Subjects were allocated to low or high sensitivity to pain groups according to their individual cold pain tolerance evoked by CPT.
Subjects who could hold their hand in the CPT up to the cut-off time of 180 s were a priori defined as having low sensitivity to pain (LSP) and a size-matched group of subjects who displayed the shortest tolerance to the CPT were classified as having high sensitivity to pain (HSP). Since this study focused on extreme groups of sensitivity to pain only, all other participants were considered to have ‘in-between’ pain sensitivity and were released from the study. Subsequently, subjects from both high and low sensitivity to pain groups were asked to complete the three questionnaires.
This manuscript presents some findings of a broader study aimed at identifying factors that contribute to the variability in pain perception in two extreme groups of healthy subjects. A previous intermittent analysis revealed findings related to the role of the endogenous pain inhibition systems in determining sensitivity to pain in these groups.39 The only similarity between both manuscripts relates to the approach by which the two groups were distinguished from each other in their sensitivity to pain. The method of classifying the two distinct groups according to cold pain tolerance is based on our previous observations39,40 and on several other reports.41–44 Accordingly, healthy subjects typically demonstrate a large variability in enduring the CPT. Within this variability, a group of approximately 20% of the tested cohort can tolerate the CPT up to the cut-off time point (often 180 sec), whereas an opposing group (of a more or less similar ratio of individuals) withdraw their hand within the first few seconds. Therefore, distinguishing between individuals with high vs low sensitivity to pain can be based on cold pain tolerance.
Statistical Analysis
The sample size was calculated by G* Power analysis to include 150 subjects ie, 75 subjects for each group (power (1-β) = 0.8; α ≤0.05; effect size f2(v)=0.06). A multivariate analysis of covariance (MANCOVA) was used to examine the effect of the groups (HSP/LSP) on the 6 personality traits and PSQ, including age and gender as covariates. The assumptions for the use of MANCOVA were tested. Pearson’s correlations were applied to examine associations between the traits. Finally, mediation analyses were performed to explore indirect effects between personality traits and pain sensitivity. Specifically, two mediation models, in which pain catastrophizing was used as a mediator, were conducted to determine if pain catastrophizing mediates between neuroticism and sensitivity to pain group allocation (Model 1), and PSQ score (Model 2). The mediation analyses yield results for a direct effect (c’) of the independent variable (IV; neuroticism) on the dependent variable (DV; sensitivity to pain group allocation (HSP/LSP) [dichotomous DV, 0=LSP: 1=HSP] or PSQ score); an indirect effect (a*b) of the IV on the DV through the mediator (pain catastrophizing); and a total effect (c) which comprises the direct and indirect effects. Path a denotes the effect of the IV on the mediator, whereas path b is the effect of the mediator on the DV. Percentile confidence intervals (CIs) were estimated for the indirect effects based on 5000 bootstrap samples of the data. The indirect effect was significant (p < 0.05) if its 95% confidence interval does not encompass zero.
Data were analyzed using IBM SPSS statistics version 25 and PROCESS SPSS macro which is an observed variable ordinary least squares (OLS) and logistic regression path analysis modeling tool for SPSS.45 Results were considered significant at the 0.05 probability level. Values are presented as means ± standard deviation (SD).
Results
Subjects
Three hundred and eighty-seven healthy subjects (268F/119M) met the inclusion criteria and underwent the CPT. Of these, 156 subjects (97F/59M) ranging in age from 18 to 54 years old (mean ± SD, 25.2±5.4 years), were identified as being LSP or HSP according to their tolerance time. Seventy-six subjects (20% of the entire study sample) were identified as LSP (36F/40M, mean tolerance = 180±0 sec), and a ‘size matched’ group of 80 subjects were identified as HSP (61F/ 19M, tolerance ≤20 sec, mean tolerance = 10.5±3.4 sec). Comparing the HSP/LSP groups for age and gender yielded significant results. Specifically, compared to the LSP group, HSP were younger (24.4±3.4 vs 26.2±6.8 years, p = 0.045) and had a higher proportion of females (76% vs 47%, χ2(1) = 13.82, p < 0.001).
Differences in Personality Traits Between the Groups
Table 1 depicts the differences in personality trait scores between the two groups. Significant differences between the groups were found in catastrophizing and extraversion. Specifically, the HSP group reported significantly higher scores than the LSP group in these traits (p=0.001 and p=0.01, respectively). The groups showed a significant main effect in the MANCOVA model (F (71,46) = 8.12, p ≤ 0.001).
Table 1.
Scores of Personality Traits in HSP and LSP Groups
| Trait | LSP (n = 76) | HSP (n = 80) | F | P-value |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||
| PCS | 22.4±10.5 | 29.1±10.7 | 10.87 | 0.001 |
| Neuroticism | 36.3±8.2 | 36.4±7.1 | 0.00 | 0.95 |
| Extraversion | 40.1±6.4 | 42.6±5.4 | 6.32 | 0.01 |
| Openness to experience | 41.5±5.4 | 41.1±5.8 | 0.22 | 0.63 |
| Agreeableness | 43.7±5.4 | 44.8±5.3 | 1.44 | 0.23 |
| Conscientiousness | 44.7±8.5 | 45.6±6.7 | 0.51 | 0.47 |
Notes: Bold, significant difference between LSP and HSP.
Abbreviations: HSP, High Sensitivity to Pain; LSP, Low Sensitivity to Pain; PCS, Pain Catastrophizing Scale.
The univariate results revealed a significant difference in PSQ scores between groups (F (1, 152) = 40.12, p < 0.001), indicating that HSP had a higher mean score than the LSP group (6.21±0.16 vs 4.72±0.16, respectively).
Correlations
Neuroticism was positively correlated with catastrophizing (r = 0.32, p < 0.001) and PSQ total scores (r = 0.33, p < 0.001). No correlations were found between catastrophizing and the other personality traits. The associations between neuroticism and pain catastrophizing formed the basis for exploring the underlying relationship between these factors and sensitivity to pain.
Mediation Analyses
While controlling for age and gender as covariates, Model 1 showed that the path (a) from neuroticism to pain catastrophizing was significant, as was the path (b) from pain catastrophizing to HSP/LSP allocation. The direct effect (c′) between neuroticism and sensitivity to pain group allocation was non-significant (B = −0.02, SE = 0.02, p = 0.46). Bootstrapping for the indirect effect (a*b) between neuroticism and group allocation yielded significant results (B = 0.02, SE = 0.01, 95% CI: 0.006–0.040) (Table 2, Figure 1A). The Nagelkerke’s R-squared for predicting group allocation was 21%.
Table 2.
Mediation Analyses
| Path | Effect (B) | SE | BootLLCI | BootULCI | P-value |
|---|---|---|---|---|---|
| Model 1 | |||||
| Direct effect (c′) | −0.02 | 0.02 | −0.067 | 0.030 | 0.46 |
| a | 0.34 | 0.11 | 0.117 | 0.567 | 0.003 |
| b | 0.06 | 0.02 | 0.022 | 0.092 | 0.001 |
| Indirect effect (a*b) | 0.02 | 0.01 | 0.006 | 0.040 | - |
| Total effect (c) | - | - | - | - | - |
| Model 2 | |||||
| Direct effect (c′) | 0.05 | 0.02 | 0.012 | 0.080 | 0.008 |
| a | 0.34 | 0.11 | 0.118 | 0.567 | 0.003 |
| b | 0.03 | 0.01 | 0.007 | 0.053 | 0.01 |
| Indirect effect (a*b) | 0.01 | 0.01 | 0.001 | 0.023 | - |
| Total effect (c) | 0.06 | 0.02 | 0.023 | 0.090 | 0.001 |
Notes: aThe path between the independent variable and the mediator; bThe path between the mediator and the dependent variable; cThe total effect of the independent variable on the dependent variable.
Abbreviations: Effect (B), unstandardized coefficient; SE, standard error; LLCI, lower limit confidence interval; ULCI, upper limit confidence interval.
Figure 1.
Mediation analyses. Catastrophizing as a mediator of neuroticism in: 1(A) the subgroup of sensitivity to pain (HSP/LSP) allocation, and 1(B) PSQ score. a = the path between the independent variable and the mediator; b = the path between the mediator and the dependent variable; c′ = the direct effect of the independent variable on the dependent variable. Values are unstandardized regression coefficients. In parentheses: standard errors. Solid lines: significant paths; dashed line: non-significant path. Asterisks indicate significant associations between two specific arms. *p<0.05.
Abbreviations: HSP, High Sensitivity to Pain; LSP, Low Sensitivity to Pain; a0, LSP; 1, HSP; PSQ, Pain Sensitivity Questionnaire.
Model 2 showed that the path from neuroticism to pain catastrophizing (a) and the path from pain catastrophizing to PSQ (b) were significant. The significant total effect (c) between neuroticism and PSQ was significant in the direct model (B = 0.06, SE = 0.02, p = 0.001) (Table 2, Figure 1B). Bootstrapping yielded significant results for the indirect effect (a*b) (B = 0.01, SE = 0.01, 95% CI: 0.001–0.023). The R-squared for predicting PSQ was 18%.
Discussion
The present study extends the previous work on the relationship between sensitivity to pain and personality traits, by testing two extreme groups of healthy individuals presenting low versus high sensitivity to pain. The two main findings of the study are first, that high scores of extraversion and catastrophizing characterize the high sensitivity to pain group; and second, that catastrophizing mediated the association between neuroticism and sensitivity to pain. The latter was shown by the allocation of subjects to each sensitivity to pain group based on their cold pain tolerance (CPT) and on their scores on the self-report pain sensitivity questionnaire (PSQ).
The finding regarding higher extraversion scores among the HSP group is not surprising since extraversion is characterized by a focused interest on external objects; a tendency to be talkative and outgoing; and a high expression of emotions.46 Moreover, extraverts are characterized by being more attracted to positive stimulation47,48 and therefore may not notice threats from the environment and so subsequently express a high negative affect when meeting such a threat. Hence, in the context of pain perception, we expected that individuals with high levels of extraversion would amplify their pain responses and, in the setting of the present study in which tolerance to cold pain determined sensitivity to pain, would be unable to endure painful stimuli for a long time. In other words, in the setting of the present study, it is not surprising that the HSP group, who were found to be more extravert, withdrew their hand from the cold bath after a short time, trying to immediately avoid a situation perceived as threatening. Furthermore, imaging studies in healthy subjects have demonstrated that extraversion is associated with increased activity in brain regions which are also known to be related to the nociceptive system (eg, the anterior cingulate gyrus, prefrontal cortex, middle temporal gyrus, and the amygdala).49,50 Congruently, clinical studies have found that extraverted individuals are more likely to complain about discomfort and pain,51 tend to suffer more from chronic pain,52 and require more analgesic treatment.53 However, these results are equivocal: Eysenck’s early biological theory of personality (1960) suggested that extraverts are less sensitive to pain due to low levels of cortical arousal, as shown by their higher thresholds and tolerances to pain.54 It was claimed that these individuals were aroused by over stimulating activities and experiences. Later on, this theory was found to be inconclusive and dependent on the situation in which arousal was measured.55 Additionally, contradictory to our finding, laboratory-induced pain studies have demonstrated higher pain thresholds and tolerances5,12 and lowered sensitivities to cold pain10 in extraverted individuals. These inconsistencies can possibly be explained by using different inventories for assessing extraversion [eg, Eysenck’s EPI,56 NEO-FFI38] or by basing findings on specific domains of extraversion in a given inventory.10
The second finding of the current study relates to pain catastrophizing. Pain catastrophizing is a personality trait that may affect sensitivity to pain by increasing the sensory flow of pain signals and altering central excitability over time.24 It is conceptualized as a negative cognitive–affective response to anticipated or actual pain and has been associated with a number of important pain-related outcomes.23 In this study, a higher mean catastrophizing score was found in HSP compared to LSP individuals. This finding is in line with previous compelling evidence showing that catastrophizing is associated with sensitivity to pain in experimental evoked pain models,3 when using self-report pain questionnaires,2,6,8 and in relation to clinical pain intensity.16,23 This evidence suggests that pain catastrophizing is a stable response mode to painful experiences.57 Moreover, a recent study has demonstrated a cumulative impact of two distinct factors ie, PCS score and sensitivity to experimental pain (pressure pain threshold or PPT), on clinical outcomes in patients with chronic musculoskeletal pain. Namely, a subgroup with a combination of a high PCS score and a low PPT were most vulnerable in terms of pain rehabilitation outcomes (ie, this subgroup had the highest level of clinical pain intensity, disability, and self-reported physical interference).58 The present work extends the relationship between sensitivity to pain and catastrophizing by showing that catastrophizing has a role as a mediator trait between personality traits and pain sensitivity. Namely, catastrophizing was found to mediate between neuroticism and sensitivity to pain in two approaches for assessing pain sensitivity. Previous studies have found this mediation relationship using different pain-related behaviors (eg, avoidance, complaint, help-seeking, pain anxiety, vigilance to pain)25–28 rather than in responses to actual painful stimuli. In fact, only one recent study by Banozic et al57 showed that catastrophizing partially mediated the associations between neuroticism and pain among healthy individuals. A possible explanation for the role of pain catastrophizing in influencing sensitivity to pain is its negative-affective element that is associated with a heightened attentional bias to pain and to the inability to disengage from the noxious stimulus.23
Another interesting point concerning catastrophizing relates to the scores revealed in the present study. A slightly high mean catastrophizing score was found in the present study in comparison to the standard scores demonstrated in other pain-free human studies.22 This may be explained by the nature of our cohort that was based on subjects allocated to two extreme groups according to their sensitivity to pain, rather than a cohort comprising the whole spectrum of sensitivity to pain.
Our findings did not show differences between groups in the neuroticism trait. However, neuroticism was found to be associated with pain sensitivity through pain catastrophizing. It is well established that individuals characterized by high neuroticism report greater pain.7,9,10 This trait reflects a tendency to experience negative and distressing emotions that potentially may lead to engagement in a fearfulness ruminative style and feelings of helplessness.5 Therefore, individuals high in neuroticism could engage in a pattern of thinking that leads them to catastrophize or magnify the negative aspect of their situation. The association between neuroticism and catastrophizing are in line with several previous studies in healthy subjects,2,6,8,15 as well as in clinical settings.19,21 Our results therefore further support the notion that neuroticism may serve as a key personality trait that along with catastrophizing as a mediator, may relate to a higher sensitivity to pain.
Some limitations of the present study should be addressed. First, the HSP group includes an uneven number of men and women (24% men only). To overcome this potential bias, gender was added as a control variable in the statistical models. Second, age differences were found between the groups. As such, the mean age of the LSP was slightly older than the HSP (26 vs 24 years, respectively). Although statistically significant, we do not believe this two-year mean difference has any important impact. However, to avoid any potential bias, age was included as a control variable in all statistical models. Third, pain catastrophizing was the only mediator measured in the current study. Assessing other potential psychological mediators that may mediate between personality traits and sensitivity to pain could further elaborate these mediation relationships.
To conclude, the findings of the present study support the current literature regarding the role of personality traits in determining sensitivity to pain. The results, which were demonstrated through two different prisms, point to the potential of the five-factor inventory and the pain catastrophizing scale as tools to identify specific personality traits associated with experiencing a high sensitivity to pain. Further studies examining additional psychological risk factors, using other experimental pain models for defining groups of sensitivity to pain, and testing cohorts of patients with clinical pain rather than healthy individuals, may further strengthen our results and allow us to generalize our conclusions.
Funding Statement
The Israeli Pain Association (IPA) provided partial financial support for this study.
Disclosure
The authors state no conflicts of interest regarding this work.
References
- 1.Nielsen CS, Staud R, Price DD. Individual differences in pain sensitivity: measurement, causation, and consequences. J Pain. 2009;10:231–237. doi: 10.1016/j.jpain.2008.09.010 [DOI] [PubMed] [Google Scholar]
- 2.Ruscheweyh R, Marziniak M, Stumpenhorst F, Reinholz J, Knecht S. Pain sensitivity can be assessed by self-rating: development and validation of the Pain Sensitivity questionnaire. Pain. 2009;146:65–74. doi: 10.1016/j.pain.2009.06.020 [DOI] [PubMed] [Google Scholar]
- 3.Hansen MS, Horjales-Araujo E, Dahl JB. Associations between psychological variables and pain in experimental pain models. A Systematic Review Acta Anaesthesiol Scand. 2015;59:1094–1102. doi: 10.1111/aas.12555 [DOI] [PubMed] [Google Scholar]
- 4.Naylor B, Boag S, Gustin SM. New evidence for a pain personality? A critical review of the last 120 years of pain and personality. Scand J Pain. 2017;17:58–67. doi: 10.1016/j.sjpain.2017.07.011 [DOI] [PubMed] [Google Scholar]
- 5.Wade JB, Price DD. Nonpathological factors in chronic pain: implications for assessment and treatment. In: Gatchel RJ, Weisberg JN, editors. Personal Charact Patients With Pain. Washington DC: American Psychological Association; 2000:89–107. doi: 10.1037/10376-004 [DOI] [Google Scholar]
- 6.Bar-Shalita T, Cermak SA. Multi-sensory responsiveness and personality traits predict daily pain sensitivity. Front Integr Neurosci. 2020;13. doi: 10.3389/fnint.2019.00077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Paine P, Kishor J, Worthen SF, Gregory LJ, Aziz Q. Exploring relationships for visceral and somatic pain with autonomic control and personality. Pain. 2009;144:236–244. doi: 10.1016/j.pain.2009.02.022 [DOI] [PubMed] [Google Scholar]
- 8.Quan X, Fong DYT, Leung AYM, Liao Q, Ruscheweyh R, Chau PH. Validation of the mandarin chinese version of the pain sensitivity questionnaire. Pain Pract. 2018;18:180–193. doi: 10.1111/papr.12587 [DOI] [PubMed] [Google Scholar]
- 9.Shiomi K. Relations of pain threshold and pain tolerance in cold water with scores on maudsley personality inventory and manifest anxiety scale. Percept Mot Skills. 1978;47:1155–1158. doi: 10.2466/pms.1978.47.3f.1155 [DOI] [PubMed] [Google Scholar]
- 10.Vassend O, Røysamb E, Nielsen CS. Five-factor personality traits and pain sensitivity: a twin study. Pain. 2013;154:722–728. doi: 10.1016/j.pain.2013.01.010 [DOI] [PubMed] [Google Scholar]
- 11.Barnes GE. Extraversion and pain. Br J Soc Clin Psychol. 1975;14:303–308. doi: 10.1111/j.2044-8260.1975.tb00182.x [DOI] [PubMed] [Google Scholar]
- 12.Ferracuti S, De Carolis A. Relationships among eysenck’s extraversion, rorschach’s erlebnistypus, and tolerance of experimental tonic pain (cold water pressor test). Percept Mot Skills. 2005;100:237–248. doi: 10.2466/PMS.100.1.237-248 [DOI] [PubMed] [Google Scholar]
- 13.Phillips JM, Gatchel RJ. Extraversion–introversion and chronic pain. In: Gatchel RJ, Weisberg JN, editors. Personal Charact Patients With Pain. Washington DC: American Psychological Association; 2000:181–202. doi: 10.1037/10376-008 [DOI] [Google Scholar]
- 14.Kristiansen FL, Olesen AE, Brock C, et al. The role of pain catastrophizing in experimental pain perception. Pain Pract. 2014;14:E136. doi: 10.1111/papr.12150 [DOI] [PubMed] [Google Scholar]
- 15.Lee JE, Watson D, Frey Law LA. Lower-order pain-related constructs are more predictive of cold pressor pain ratings than higher-order personality traits. J Pain. 2010;11:681–691. doi: 10.1016/j.jpain.2009.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Leung L. Pain catastrophizing: an updated review. Indian J Psychol Med. 2012;34:204–217. doi: 10.4103/0253-7176.106012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Patanwala AE, Norwood C, Steiner H, et al. Psychological and genetic predictors of pain tolerance. Clin Transl Sci. 2019;12:189–195. doi: 10.1111/cts.12605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goodin BR, Fillingim RB, Machala S, et al. Subjective sleep quality and ethnicity are interactively related to standard and situation-specific measures of pain catastrophizing. Pain Med. 2011;12:913–922. doi: 10.1111/j.1526-4637.2011.01138.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kadimpati S, Zale EL, Hooten MW, Ditre JW, Warner DO. Associations between neuroticism and depression in relation to catastrophizing and pain-related anxiety in chronic pain patients. PLoS One. 2015;10:e0126351. doi: 10.1371/journal.pone.0129871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muris P, Meesters C, Van Den Hout A, Wessels S, Franken I, Rassin E. Personality and temperament correlates of pain catastrophizing in young adolescents. Child Psychiatry Hum Dev. 2007;38:171–181. doi: 10.1007/s10578-007-0054-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wong WS, Lam HMJ, Chen PP, et al. The fear-avoidance model of chronic pain: assessing the role of neuroticism and negative affect in pain catastrophizing using structural equation modeling. Int J Behav Med. 2015;22:118–131. doi: 10.1007/s12529-014-9413-7 [DOI] [PubMed] [Google Scholar]
- 22.Wheeler CHB, Williams ACDC, Morley SJ. Meta-analysis of the psychometric properties of the Pain Catastrophizing Scale and associations with participant characteristics. Pain. 2019;160:1946–1953. doi: 10.1097/j.pain.0000000000001494 [DOI] [PubMed] [Google Scholar]
- 23.Quartana PJ, Campbell CM, Edwards RR. Pain catastrophizing a critical review. Expert Rev Neurother. 2009;9:745–758. doi: 10.1586/ern.09.34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sullivan MJL, Thorn B, Haythornthwaite JA, et al. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain. 2001;17:52–64. doi: 10.1097/00002508-200103000-00008 [DOI] [PubMed] [Google Scholar]
- 25.Affleck G, Tennen H, Urrows S, Higgins P. Neuroticism and the pain-mood relation in rheumatoid arthritis: insights from a prospective daily study. J Consult Clin Psychol. 1992;60:119–126. doi: 10.1037/0022-006X.60.1.119 [DOI] [PubMed] [Google Scholar]
- 26.Martinez MP, Sánchez AI, Miró E, Medina A, Lami MJ. The relationship between the fear-avoidance model of pain and personality traits in fibromyalgia patients. J Clin Psychol Med Settings. 2011;18:380–391. doi: 10.1007/s10880-011-9263-2 [DOI] [PubMed] [Google Scholar]
- 27.Spada MM, Gay H, Nikčevic AV, Fernie BA, Caselli G. Meta-cognitive beliefs about worry and pain catastrophising as mediators between neuroticism and pain behaviour. Clin Psychol. 2016;20:138–146. doi: 10.1111/cp.12081 [DOI] [Google Scholar]
- 28.Goubert L, Crombez G, Van Damme S. The role of neuroticism, pain catastrophizing and pain-related fear in vigilance to pain: a structural equations approach. Pain. 2004;107:234–241. doi: 10.1016/j.pain.2003.11.005 [DOI] [PubMed] [Google Scholar]
- 29.McCrae RR, John OP. An introduction to the five‐factor model and its applications. J Pers. 1992;60:175–215. doi: 10.1111/j.1467-6494.1992.tb00970.x [DOI] [PubMed] [Google Scholar]
- 30.Bucourt E, Martaillé V, Mulleman D, et al. Comparison of the Big Five personality traits in fibromyalgia and other rheumatic diseases. Jt Bone Spine. 2017;84:203–207. doi: 10.1016/j.jbspin.2016.03.006 [DOI] [PubMed] [Google Scholar]
- 31.Koh CH, Othman Z. Neuroticism is associated with chronic severe pain among ex-opioid users on methadone maintenance therapy. Int Med J. 2019;26:15–18. doi: 10.5281/zenodo.2586234 [DOI] [Google Scholar]
- 32.Tanum L, Malt UF. Personality and physical symptoms in nonpsychiatric patients with functional gastrointestinal disorder. J Psychosom Res. 2001;50:139–146. doi: 10.1016/S0022-3999(00)00219-1 [DOI] [PubMed] [Google Scholar]
- 33.Boggero IA, Smart LM, Kniffin TC, Walker RL. Neuroticism and resting mean arterial pressure interact to predict pain tolerance in pain-free adults. Pers Individ Dif. 2014;69:140–143. doi: 10.1016/j.paid.2014.05.028 [DOI] [Google Scholar]
- 34.Croy I, Springborn M, Lötsch J, Johnston ANB, Hummel T. Agreeable smellers and sensitive Neurotics - Correlations among personality traits and sensory thresholds. PLoS One. 2011;6:e18701. doi: 10.1371/journal.pone.0018701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.McIntyre MH, Kless A, Hein P, Field M, Tung JY. Validity of the cold pressor test and pain sensitivity questionnaire via online self-administration. PLoS One. 2020;15:1–16. doi: 10.1371/journal.pone.0231697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bar-Shalita T, Deutsch L, Honigman L, Weissman-Fogel I. Ecological aspects of pain in sensory modulation disorder. Res Dev Disabil. 2015;45:157–167. doi: 10.1016/j.ridd.2015.07.028 [DOI] [PubMed] [Google Scholar]
- 37.Granot M, Ferber SG. The roles of pain catastrophizing and anxiety in the prediction of postoperative pain intensity: a prospective study. Clin J Pain. 2005;21:439–445. doi: 10.1097/01.ajp.0000135236.12705.2d [DOI] [PubMed] [Google Scholar]
- 38.Costa PT, McCrae RR. Revised NEO personality inventory (NEO-PI-R) and NEO five-factor inventory (NEO-FFI); 1992.
- 39.Grouper H, Eisenberg E, Pud D. The relationship between sensitivity to pain and conditioned pain modulation in healthy people. Neurosci Lett. 2019;708:134333. doi: 10.1016/j.neulet.2019.134333 [DOI] [PubMed] [Google Scholar]
- 40.Pud D, Treister R, Eisenberg E. Sub-grouping healthy subjects’ sensitivity to pain and its relationship to personality traits: results of a cluster analysis. Appl Math. 2014;05:1705–1712. doi: 10.4236/am.2014.511163 [DOI] [Google Scholar]
- 41.Chen ACN, Dworkin SF, Haug J, Gehrig J. Human pain responsivity in a tonic pain model: psychological determinants. Pain. 1989;37:143–160. doi: 10.1016/0304-3959(89)90126-7 [DOI] [PubMed] [Google Scholar]
- 42.Cleeland CS, Nakamura Y, Howland EW, Morgan NR, Edwards KR, Backonja M. Effects of oral morphine on cold presser tolerance time and neuropsychological performance. Neuropsychopharmacology. 1996;15:252–262. doi: 10.1016/0893-133X(95)00205-R [DOI] [PubMed] [Google Scholar]
- 43.Geisser ME, Robinson ME, Pickren WE. Differences in cognitive coping strategies among pain-sensitive and pain-tolerant individuals on the cold-pressor test. Behav Ther. 1992;23:31–41. doi: 10.1016/S0005-7894(05)80306-5 [DOI] [Google Scholar]
- 44.Polianskis R, Graven-Nielsen T, Arendt-Nielsen L. Modality-specific facilitation and adaptation to painful tonic stimulation in humans. Eur J Pain. 2002;6:475–484. doi: 10.1016/S1090-3801(02)00058-7 [DOI] [PubMed] [Google Scholar]
- 45.Hays AF. Introduction to mediation, moderation, and conditional process analysis: a regession approach; 2018.
- 46.John OP, Naumann LP, Soto CJ. Paradigm shift to the integrative big five trait taxonomy: history, measurement, and conceptual issues. In: Johns O, Robins R, Previn L, editors. Handb Personal Theory Res. New York, NY: The Guilford Press; 2008:114–158. [Google Scholar]
- 47.Amin Z, Constable RT, Canli T. Attentional bias for valenced stimuli as a function of personality in the dot-probe task. J Res Pers. 2004;38:15–23. doi: 10.1016/j.jrp.2003.09.011 [DOI] [Google Scholar]
- 48.Derryberry D, Reed MA. Temperament and attention: orienting toward and away from positive and negative signals. J Pers Soc Psychol. 1994;66:1128–1139. doi: 10.1037/0022-3514.66.6.1128 [DOI] [PubMed] [Google Scholar]
- 49.Lei X, Yang T, Wu T. Functional neuroimaging of extraversion-introversion. Neurosci Bull. 2015;31:663–675. doi: 10.1007/s12264-015-1565-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ruffle JK, Farmer AD, Kano M, Giampietro V, Aziz Q, Coen SJ. The influence of extraversion on brain activity at baseline and during the experience and expectation of visceral pain. Pers Individ Dif. 2015;74:248–253. doi: 10.1016/j.paid.2014.10.024 [DOI] [Google Scholar]
- 51.Bond MR, Glynn JP, Thomas DG. The relation between pain and personality in patients receiving pentazocine (fortral) after surgery. J Psychosom Res. 1976;20:369–381. doi: 10.1016/0022-3999(76)90089-1 [DOI] [PubMed] [Google Scholar]
- 52.Burri A, Hilpert P, McNair P, Williams FM. Exploring symptoms of somatization in chronic widespread pain: latent class analysis and the role of personality. J Pain Res. 2017;10:1733–1740. doi: 10.2147/JPR.S139700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taenzer P, Melzack R, Jeans ME. Influence of psychological factors on postoperative pain, mood and analgesic requirements. Pain. 1986;24:331–342. doi: 10.1016/0304-3959(86)90119-3 [DOI] [PubMed] [Google Scholar]
- 54.Eysenck HJ. Biological dimensions of personality. Guilford Press; 1990. [Google Scholar]
- 55.Matthews G, Gilliland K. The personality theories of H. J. Eysenck and J. A. Gray: a comparative review. Pers Individ Dif. 2000;26:583–626. doi: 10.1016/s0191-8869(99)00166-x [DOI] [Google Scholar]
- 56.Eysenck HJ, Eysenck SBJ. Manual for the Eysenck personality questionnaire: (EPQ-R adult). Educ Ind Test Serv. 1994. [Google Scholar]
- 57.Banozic A, Miljkovic A, Bras M, et al. Neuroticism and pain catastrophizing aggravate response to pain in healthy adults: an experimental study. Korean J Pain. 2018;31:16–26. doi: 10.3344/kjp.2018.31.1.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Uddin Z, Woznowski-Vu A, Flegg D, Aternali A, Wideman TH. A cumulative impact of psychological and sensitization risk factors on pain-related outcomes. Pain Pract. 2020;1–13. doi: 10.1111/papr.12987 [DOI] [PubMed] [Google Scholar]