Abstract
Background
After the global epidemic of coronavirus disease 2019 (COVID-19), lifestyle changes to curb the spread of COVID-19 (e.g., wearing a mask, hand washing, and social distancing) have also affected the outbreak of other infectious diseases. However, few studies have been conducted on whether the incidence of gastrointestinal infections has changed over the past year with COVID-19. In this study, we examined how the incidence of gastrointestinal infections has changed since COVID-19 outbreak through open data.
Methods
We summarized the data on the several viruses and bacteria that cause gastrointestinal infections from the open data of the Korea Disease Control and Prevention Agency for 3 years from March 2018 to February 2021 (from Spring 2018 to Winter 2020). Moreover, we confirmed three most common legal gastrointestinal infectious pathogens from March 2016.
Results
From March 2020, when the COVID-19 epidemic was in full swing and social distancing and personal hygiene management were heavily emphasized, the incidence of infection from each virus was drastically decreased. The reduction rates compared to the averages of the last 2 years were as follows: total viruses 31.9%, norovirus 40.2%, group A rotavirus 31.8%, enteric adenovirus 13.4%, astrovirus 7.0%, and sapovirus 12.2%. Among bacterial pathogens, the infection rates of Campylobacter and Clostridium perfringens did not decrease but rather increased in some periods when compared to the average of the last two years. The incidence of nontyphoidal Salmonella, Staphylococcus aureus, or enteropathogenic Escherichia coli somewhat decreased but not significantly compared to the previous two years.
Conclusion
The incidence of infection from gastrointestinal viruses, which are mainly caused by the fecal-to-oral route and require direct contact among people, was significantly reduced, whereas the incidence of bacterial pathogens, which have food-mediated transmission as the main cause of infection, did not decrease significantly.
Keywords: COVID-19, Enteritis, Colitis, Viral Infection, Bacterial Infection, Incidence Rate
Graphical Abstract

INTRODUCTION
The year 2020 will be remembered as the time when the global epidemic of coronavirus disease 2019 (COVID-19) tremendously impacted everyone's lives. In South Korea, COVID-19 cases emerged in the early stages of the epidemic before the infection spread globally. People coped with this situation collectively by refraining from going out and gathering with others.1 In addition, personal hygiene guidelines, such as wearing a mask and hand washing, were strictly observed all year round. These lifestyle changes to curb the spread of COVID-19 also affected the outbreak of other infectious diseases.2,3 For example, unlike previous years, enterovirus-related diseases were seldom reported in the summer of 2020. In addition, the incidence of influenza virus, respiratory syncytial virus, and mycoplasma infections, which are prevalent in every winter, also decreased in 2020.4,5,6
However, such reductions are not common to all infectious diseases. The outbreak of enterohemorrhagic Escherichia coli (EHEC), which can cause hemolytic uremic syndrome in children, was actually a social issue in June 2020 in Korea.7 Gastrointestinal infections have been one of the most common life-threatening etiologies in pediatric patients for centuries.8 Nevertheless, few studies have been conducted on whether and how the incidence rate has changed before and after COVID-19. Therefore we examine this and try to explain the reasons behind the identified changes using open data released by the Korea Disease Control and Prevention Agency (KDCA).
METHODS
Data extraction of infectious causes
The KDCA has been making available open data on various infectious diseases or strains on its website (Infectious Disease Portal) since 2001.9 The portal provides yearly and monthly data on legal infectious diseases, including infectious gastrointestinal diseases, such as cholera, typhoid fever, shigellosis, and EHEC. These data are collected from 192 hospitals participating in sample surveillance through the National Infectious Disease Surveillance System. These KDCA data can be used without copyright issues unless used for personal benefit.
The cause of gastrointestinal infection was identified using information published in KDCA. From these data, we extracted data for 3 years from March 2018 to February 2021 (from Spring 2018 to Winter 2020). Gastrointestinal pathogens are categorized into bacteria, viruses, and protozoa.10 We excluded the data on protozoa that caused fewer than 10 cases per year. Five enteric viruses—group A rotavirus, norovirus, sapovirus, astrovirus, and enteric adenovirus—that cause gastrointestinal infections were identified. Among the 11 bacterial pathogens of investigation, we finally selected data on the five most common strains of Campylobacter, Clostridium perfringens, nontyphoidal Salmonella, Staphylococcus aureus, and enteropathogenic E. coli (EPEC), excluding pathogens with few occurrences. In addition, among data on legal infectious diseases, we excluded cholera, of which fewer than 10 cases were reported per year. Therefore, data on the remaining three diseases (typhoid fever, shigellosis, and EHEC) from March 2016 to February 2021 were selected for study.
We identified the differences in incidence rate of each pathogen before and after COVID-19 by comparing to the mean values of the season for the past 2 years and 2020 through the χ2 analysis in the R program (ver. 3.6.3. https://www.r-project.org).
Ethics statement
This study was conducted with approval from the institutional review board (IRB) of Chung-Ang University Hospital (IRB no.:2012-028-19346), and informed consent was waived due to the retrospective nature of the study.
RESULTS
Changes in number of viral pathogens that cause gastrointestinal infections after COVID-19
From March 2018 to February 2021, the incidence of five gastrointestinal infection-related viruses that were subject to sample monitoring was investigated (Fig. 1). In this period, the average number of occurrence was the highest for norovirus with 4,468 cases (4,986, 6,174, and 2,244 cases, respectively), followed by group A rotavirus with 2,499 cases (3,564, 2,903, and 1,029 cases, respectively). These were followed by enteric adenovirus (1,311, 563, and 126 cases, respectively), astrovirus (776, 912, and 59 cases, respectively) and sapovirus (293, 511, and 49 cases, respectively).
Fig. 1. Incidence of viruses that cause gastrointestinal infections after coronavirus disease 2019 pandemic; confirmed in open data from the Korea Disease Control and Prevention Agency.
From March 2020, when the COVID-19 epidemic was peaking and social distancing and personal hygiene management were heavily emphasized, the incidence of each viral infection drastically decreased, with the reduction rates compared to the averages of the last 2 years being as follows: (total viruses: 31.9%, norovirus: 40.2%, group A rotavirus: 31.8%, enteric adenovirus: 13.4%, astrovirus: 7.0%, and sapovirus: 12.2%). Seasonal values also decreased significantly for each virus: P < 0.001 except astrovirus (P = 0.04).
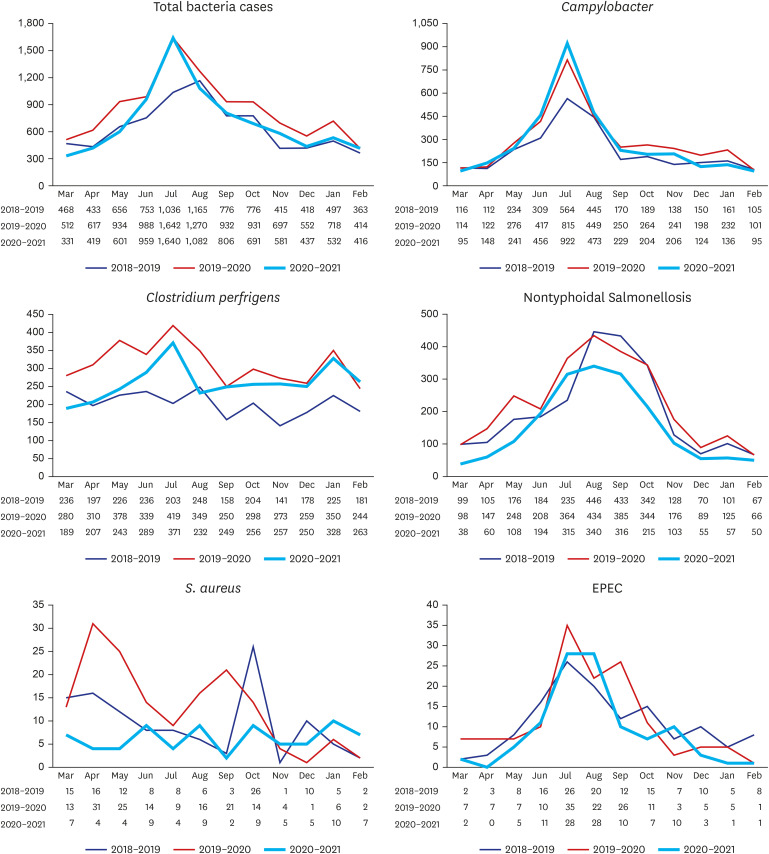
Changes in number of bacterial pathogens that cause gastrointestinal infections after COVID-19
The incidence of gastrointestinal infection-related bacteria that are subject to sample monitoring was also investigated from March 2018 to February 2021 (Fig. 2). Campylobacter infection was the most common during this period, followed by C. perfringens and nontyphoidal Salmonella infections. Next, about 100 cases of S. aureus and EPEC occurred each year. The incidence of these bacteria did not decrease in 2020 compared to what it was in the last 2 years. Rather, Campylobacter, C. perfringens, and nontyphoidal Salmonella infections, which accounted for more than 100 cases a month, increased in some periods (P < 0.001, P < 0.001, and P < 0.001, respectively). From March 2020 to February 2021, the incidence of Campylobacter and C. perfringens increased by 107.9% and 101.4%, respectively, compared to the average of last 2 years. In addition, the incidence of nontyphoidal Salmonella decreased by 73.0% compared to the 2-year average. The incidence of S. aureus was evenly distributed every month in 2020 and decreased by 56.0% compared to the 2-year average; however, it increased in some months. The incidence of EPEC also decreased by 78.2% compared to the 2-year average but increased in some periods.
Fig. 2. Incidence of bacteria that cause gastrointestinal infections after coronavirus disease 2019 pandemic; confirmed in open data from the Korea Disease Control and Prevention Agency.
EPEC = enteropathogenic Escherichia coli.
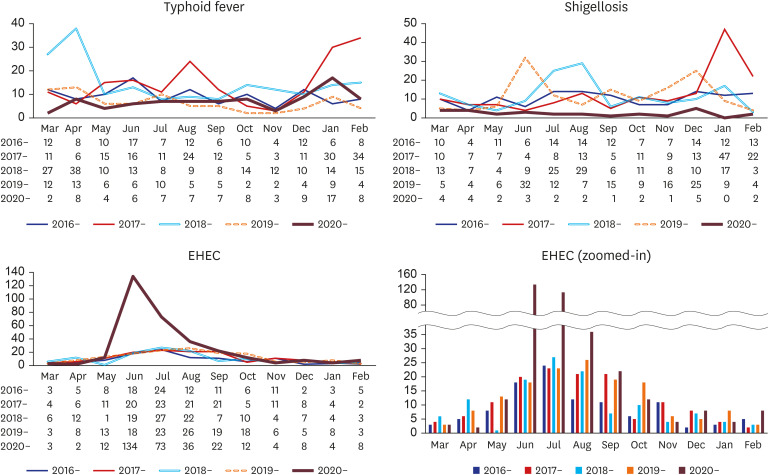
Changes in number of legal infectious diseases related to gastrointestinal infections after COVID-19
The incidence of typhoid fever, shigellosis, and EHEC from March 2016 to February 2021 is shown in Fig. 3. In the case of typhoid fever, the mean number of cases per year from March 2016 to February 2020 was 136.5; however, during the COVID-19 pandemic from March 2020 to February 2021, it reduced by 37.0% to 86 cases. However, it did not decrease evenly every month, and there was also a period when the number of occurrences in a month increased compared to the previous one. In the case of shigellosis, an average of 141.5 cases occurred annually from March 2016 to February 2020, and the incidence decreased by 80.2% to 28 from March 2020 to February 2021. The incidence decreased evenly over all seasons. Conversely, the incidence of EHEC heavily increased from an average of 129 cases per year from March 2016 to February 2020 to 318 cases from March 2020 to February 2021 due to a large outbreak of EHEC from June to August 2020. Except for the 3 months of the outbreak, the number of occurrence did not increase or decrease significantly compared to before.
Fig. 3. Incidence of legal infectious diseases that cause gastrointestinal infections after coronavirus disease 2019 pandemic; confirmed in open data from the Korea Disease Control and Prevention Agency.
EHEC = enterohemorrhagic Escherichia coli.
DISCUSSION
Since the COVID-19 pandemic, various studies have been published in the fields of medicine and healthcare. Thus far, most studies have been simple case reports or reports on topics directly related to COVID-19, such as vaccines, epidemiology, and prognosis according to the underlying disease. There has been little research related to the occurrence of gastrointestinal infection.11,12 This is the first study on the occurrence of gastrointestinal infections since COVID-19, and it is particularly meaningful in that it uses open data from South Korea, which is highly reliable. Because of the social distancing enforced due to COVID-19, we noted that there were few influenza viral infections (nearly none) during the usual epidemic period from February to April, and there were few enteroviral infections, which are common in May to July. Conversely, there was an unexpected outbreak of EHEC in June. It was clear that the outbreak of infectious diseases was somehow affected by nationwide social distancing. The incidence of some diseases decreased significantly, while that of others did not. This study was started to identify the association.
The open data of the KDCA showed that the incidence of viruses that cause gastrointestinal infections decreased dramatically in March 2020 (Fig. 1). In January and February 2020, the frequency of all viruses, including norovirus, was marginally higher than before, but after March, which is when the COVID-19 pandemic began in earnest, the incidence decreased significantly. This is closely related to the propagation path of the virus. Viruses are transmitted through the fecal-to-oral contamination route or by close contact between people. Consequently, hygiene management, such as hand washing or wearing a mask, can lead to a huge decrease.11,12,13 However, these gastrointestinal-related viruses did not show dramatic decrease like the respiratory-related viruses did, suggesting the presence of a food-borne infection route in the case of gastrointestinal-related viruses.13,14
Unlike viral pathogens, bacterial pathogens and legal infectious pathogens did not decrease significantly since the COVID-19 pandemic (Figs. 1, 2, and 3). However, it was difficult to identify statistical differences in the number of occurrence before and after the COVID-19. It's probably due to seasonal effects and sudden outbreaks, such as the EHEC outbreak in June 2020. But it was clear that a declining tendency of bacterial pathogens was not as pronounced as in viral pathogens. This is because the infection of these bacterial pathogens, such as Campylobacter, nontyphoidal Salmonella, C. perfringens, and S. aureus, is caused mainly through contaminated food or drinking water and not through direct person-to-person transmission as in viruses.7,15,16,17 This assumption is based on the increasing incidence during the summer. Restrictions on going outside may have contributed to the increase in the incidence of these food-mediated diseases. Gastrointestinal pathogens have a wide range of infection pathways, making it difficult to clearly identify these differences.
This study has several limitations. The data of the KDCA are from sample surveillance participating organizations at the hospital level or higher and not from all patients nationwide as in the Health Insurance Review and Assessment Service (HIRA). Outbreaks in specific regions can affect the numbers; therefore, they may not be representative of the overall trend. In addition, there were only 3 years of data from March 2018 to February 2021 because the participating organizations under investigation were changed in 2017. However, the legal infectious diseases were analyzed for 5 years because the data were from a nationwide sample. Conversely, HIRA data are based on disease codes, which can lead to missing or misdiagnosed actual pathogens, whereas the data from the KDCA have the advantage of being accurate. The possibility that patients did not visit the hospital or could not be treated due to the COVID-19 outbreak should also be considered. However, considering South Korea's low medical costs and easy access to medical institutions, such an impact is thought to have been minimal. KDCA also provides data on number of occurrence according to age. However, since this study was only trying to confirm the nationwide trend of gastrointestinal diseases after the pandemic, we did not investigate the data according to age. We are considering further studies that would take into account the incidence by age.
In conclusion, despite these limitations, we confirmed that there was a difference in the incidence of gastrointestinal pathogens depending on the route of infection transmission. After COVID-19, although most infectious diseases are thought to have decreased, interesting changes have been confirmed in gastrointestinal infectious diseases, which have various routes of transmission and are different from respiratory infectious diseases. The incidence of gastrointestinal viral infections, which are mainly caused by the fecal-to-oral route and require direct contact between people, was significantly reduced, whereas the incidence of bacterial pathogens, whose main cause of infection is food-mediated, did not decrease significantly.
ACKNOWLEDGMENTS
We thank EssayReview Language Editing Services for reviewing the manuscript and for their editorial assistance. The occurrence pattern of each pathogen was investigated using the open data of the Korea Disease Control and Prevention Agency (KDCA).
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualization: Chae SA, Yun SW.
- Data curation: Park JY, Kim SY, Lee NM.
- Formal analysis: Choi BS.
- Writing - original draft: Ahn SY, Yi DY.
- Writing - review & editing: Yi DY, Lim IS.
References
- 1.Choi JY. COVID-19 in South Korea. Postgrad Med J. 2020;96(1137):399–402. doi: 10.1136/postgradmedj-2020-137738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ha KM. The principle of distance during COVID-19 outbreak in Korea. Int Microbiol. 2020;23(4):641–643. doi: 10.1007/s10123-020-00138-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lu N, Cheng KW, Qamar N, Huang KC, Johnson JA. Weathering COVID-19 storm: Successful control measures of five Asian countries. Am J Infect Control. 2020;48(7):851–852. doi: 10.1016/j.ajic.2020.04.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wee LE, Conceicao EP, Sim XY, Ko KK, Ling ML, Venkatachalam I. Reduction in healthcare-associated respiratory viral infections during a COVID-19 outbreak. Clin Microbiol Infect. 2020;26(11):1579–1581. doi: 10.1016/j.cmi.2020.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Itaya T, Furuse Y, Jindai K. Does COVID-19 infection impact on the trend of seasonal influenza infection? 11 countries and regions, from 2014 to 2020. Int J Infect Dis. 2020;97:78–80. doi: 10.1016/j.ijid.2020.05.088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Choi DH, Jung JY, Suh D, Choi JY, Lee SU, Choi YJ, et al. Impact of the COVID-19 outbreak on trends in emergency department utilization in children: a multicenter retrospective observational study in Seoul metropolitan area, Korea. J Korean Med Sci. 2021;36(5):e44. doi: 10.3346/jkms.2021.36.e44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim JS, Lee MS, Kim JH. Recent updates on outbreaks of Shiga toxin-producing Escherichia coli and its potential reservoirs. Front Cell Infect Microbiol. 2020;10:273. doi: 10.3389/fcimb.2020.00273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bryce J, Boschi-Pinto C, Shibuya K, Black RE WHO Child Health Epidemiology Reference Group. WHO estimates of the causes of death in children. Lancet. 2005;365(9465):1147–1152. doi: 10.1016/S0140-6736(05)71877-8. [DOI] [PubMed] [Google Scholar]
- 9.Korea Disease Control and Prevention Agency. Infectious disease portal. [Updated 2021]. http://www.kdca.go.kr/npt/biz/npp/portal/nppPblctDtaMain.do.
- 10.Ryoo E. Causes of acute gastroenteritis in Korean children between 2004 and 2019. Clin Exp Pediatr. 2021;64(6):260–268. doi: 10.3345/cep.2020.01256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karg MV, Alber B, Kuhn C, Bohlinger K, Englbrecht M, Dormann H. SARS-CoV-2, influenza and norovirus infection: a direct epidemiologic comparison. Med Klin Intensivmed Notf Med. doi: 10.1007/s00063-021-00783-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laszkowska M, Kim J, Faye AS, Joelson AM, Ingram M, Truong H, et al. Prevalence of Clostridioides difficile and other gastrointestinal pathogens in patients with COVID-19. Dig Dis Sci. doi: 10.1007/s10620-020-06760-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsuyama R, Miura F, Nishiura H. The transmissibility of noroviruses: Statistical modeling of outbreak events with known route of transmission in Japan. PLoS One. 2017;12(3):e0173996. doi: 10.1371/journal.pone.0173996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matsuyama R, Miura F, Tsuzuki S, Nishiura H. Household transmission of acute gastroenteritis during the winter season in Japan. J Int Med Res. 2018;46(7):2866–2874. doi: 10.1177/0300060518776451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wen SC, Best E, Nourse C. Non-typhoidal Salmonella infections in children: review of literature and recommendations for management. J Paediatr Child Health. 2017;53(10):936–941. doi: 10.1111/jpc.13585. [DOI] [PubMed] [Google Scholar]
- 16.Majowicz SE, Musto J, Scallan E, Angulo FJ, Kirk M, O'Brien SJ, et al. The global burden of nontyphoidal Salmonella gastroenteritis. Clin Infect Dis. 2010;50(6):882–889. doi: 10.1086/650733. [DOI] [PubMed] [Google Scholar]
- 17.Scallan E, Mahon BE, Hoekstra RM, Griffin PM. Estimates of illnesses, hospitalizations and deaths caused by major bacterial enteric pathogens in young children in the United States. Pediatr Infect Dis J. 2013;32(3):217–221. doi: 10.1097/INF.0b013e31827ca763. [DOI] [PubMed] [Google Scholar]