Abstract
Introduction
The response to the COVID-19 pandemic became increasingly politicized in the U.S., and the political affiliation of state leaders may contribute to policies affecting the spread of the disease. This study examines the differences in COVID-19 infection, death, and testing by governor party affiliation across the 50 U.S. states and the District of Columbia.
Methods
A longitudinal analysis was conducted in December 2020 examining COVID-19 incidence, death, testing, and test positivity rates from March 15, 2020 through December 15, 2020. A Bayesian negative binomial model was fit to estimate the daily risk ratios and posterior intervals comparing rates by gubernatorial party affiliation. The analyses adjusted for state population density, rurality, Census region, age, race, ethnicity, poverty, number of physicians, obesity, cardiovascular disease, asthma, smoking, and presidential voting in 2020.
Results
From March 2020 to early June 2020, Republican-led states had lower COVID-19 incidence rates than Democratic-led states. On June 3, 2020, the association reversed, and Republican-led states had a higher incidence (risk ratio=1.10, 95% posterior interval=1.01, 1.18). This trend persisted through early December 2020. For death rates, Republican-led states had lower rates early in the pandemic but higher rates from July 4, 2020 (risk ratio=1.18, 95% posterior interval=1.02, 1.31) through mid-December 2020. Republican-led states had higher test positivity rates starting on May 30, 2020 (risk ratio=1.70, 95% posterior interval=1.66, 1.73) and lower testing rates by September 30, 2020 (risk ratio=0.95, 95% posterior interval=0.90, 0.98).
Conclusions
Gubernatorial party affiliation may drive policy decisions that impact COVID-19 infections and deaths across the U.S. Future policy decisions should be guided by public health considerations rather than by political ideology.
INTRODUCTION
Coronavirus disease 2019 (COVID-19) has resulted in a global public health crisis. As of December 15, 2020, there have been >16 million confirmed COVID-19 cases and 300,000 deaths in the U.S.1 In response to the pandemic, the governors of all the 50 states declared states of emergency. Shortly thereafter, states began enacting policies to help stop the spread of the virus. However, these policies vary and are guided in part by decisions from state governors.
Through state constitutions and laws, governors have the authority to take action in public health emergencies. In early 2020, nearly all state governors issued stay-at-home executive orders that advised or required residents to shelter in place.2 However, recent studies found that Republican governors were slower to adopt stay-at-home orders, if they did so at all.3 , 4 Moreover, another study found that Democratic governors had longer durations of stay-at-home orders.5 Furthermore, researchers identified governor Democratic political party affiliation as the most important predictor of state mandates to wear face masks (C Adolph, PhD, unpublished data, September 2020).
Although recent studies have examined individual state policies, such as mandates to socially distance, wear masks, and close schools and parks (C Adolph, PhD, unpublished data, September 2020 and P Matzinger, PhD, unpublished data, September 2020),3 , 4 , 6 multiple policies may act together to impact the spread of COVID-19. In addition, the pandemic response has become increasingly politicized.6, 7, 8 As such, the political affiliation of state leaders and specifically governors might best capture the omnibus impact of state policies. Therefore, the purpose of this study is to quantify the differences in incidence, death, testing, and test positivity rates over time, stratified by governors’ political affiliation among the 50 states and the District of Columbia.
METHODS
A longitudinal analysis examined COVID-19 incident cases, death rates, polymerase chain reaction testing, and test positivity from March 15, 2020 (March 24, 2020 for testing and test positivity) through December 15, 2020 for the 50 states and the District of Columbia. On the basis of previous studies (C Adolph, PhD, unpublished data, September 2020),3 , 4 , 6 it was hypothesized that states with Democratic governors would have higher incidence, death, and test positivity rates early in the pandemic owing to points of entry for the virus9 , 10 but that the trends would reverse in later months, reflecting policy differences that break along party lines. The IRBs at the Medical University of South Carolina and Johns Hopkins Bloomberg School of Public Health deemed this research exempt.
Governor party affiliation was documented for each U.S. state; for the District of Columbia, mayoral affiliation was used. Daily incident cases and deaths were obtained from the COVID Tracking Project.11 Polymerase chain reaction testing and test positivity data came from the HHS.12 Potential confounders included state population density,13 Census region,13 state percentage of residents aged ≥65 years,13 percentage of Black residents,13 percentage of Hispanic residents,13 percentage below the federal poverty line,13 percentage living in rural areas,14 percentage with obesity,15 percentage with cardiovascular disease,16 percentage with asthma, percentage smoking,7 number of physicians per 100,000 residents,14 and percentage of individuals who voted Democratic (versus those who voted Republican) party in the 2020 presidential election.17
Bayesian negative binomial models were used to examine the incident case and death, testing, and test positivity rates. The models included penalized cubic B-splines for the fixed and random temporal effects. Models adjusted for the above covariates. Ridging priors were assigned to the fixed and random spline coefficients.18 Posterior computation was implemented using Gibbs sampling.16 , 19 Model details, including previous specification, computational diagnostics, and sensitivity analyses, are provided in the Appendix (available online).
Models were stratified by governors’ affiliation, and posterior mean daily rates were graphed with their 95% posterior intervals (PIs). Adjusted RRs and 95% PIs were calculated to compare states, with RRs >1.00 indicating higher rates among Republican-led states. Analyses were conducted using R, version 3.6.
RESULTS
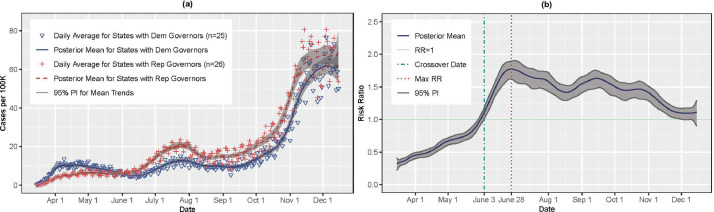
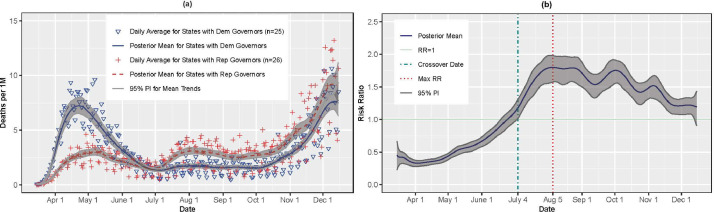
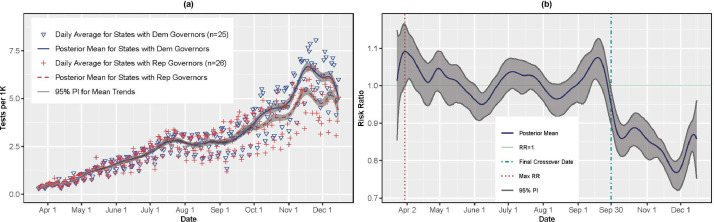
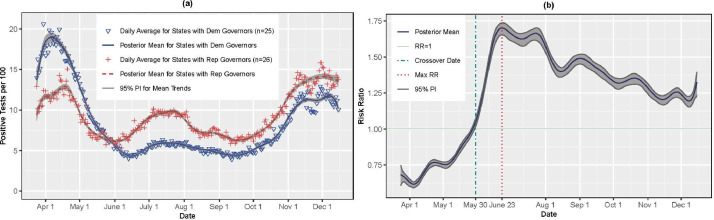
The sample comprised 26 Republican-led and 25 Democratic-led states. Figure 1A and B present the incidence trends (cases per 100,000) and adjusted RRs by gubernatorial affiliation. Republican-led states had fewer cases from March 2020 to early June 2020. However, on June 3, 2020, the association reversed (RR=1.10, 95% PI=1.01, 1.18), indicating that Republican-led states had on average 1.10 times more cases per 100,000 than Democratic-led states. The RRs increased steadily thereafter, achieving a maximum of 1.77 (95% PI=1.62, 1.90) on June 28, 2020 and remaining positive for the remainder of the study, although the PIs overlapped 1.00 starting on December 3, 2020. A similar pattern emerged for deaths (shown in Figure 2A and B). Republican-led states had lower death rates early in the pandemic, but the trend reversed on July 4, 2020 (RR=1.18, 95% PI=1.02, 1.31). The RRs increased through August 5, 2020 (RR=1.80, 95% PI=1.57, 1.98), and the PIs remained >1.00 until December 13, 2020 (RR=1.20, 95% PI=0.96, 1.39). Testing rates (Figure 3A and B) tracked similarly for Republican and Democratic states until September 30, 2020 (RR=0.95, 95% PI=0.90, 0.98). By November 27, 2020, the testing rate for Republican-led states was substantially lower than that for Democratic-led states (RR=0.77, 95% PI=0.72, 0.80). The test positivity rate (Figure 4A and B) was higher for Republican-led states starting on May 30, 2020 and was 1.70 (95% PI=1.65, 1.74) times higher on June 23, 2020.
Figure 1.
(A) COVID-19 incidence rates per 100K individuals by governor affiliation; (B) adjusted RRs and 95% PIs. RRs >1 indicate higher rates for Rep governors. 100K, 100,000; Apr, April; Aug, August; Dec, December; Dem, Democratic; Max, maximum; Nov, November; Oct, October; PI, posterior interval; Rep, Republican; Sep, September.
Figure 2.
(A) COVID-19 death rates per 1M individuals by governor affiliation; (B) adjusted RRs and PIs. RRs >1 indicate higher rates for Rep governors. 1M, 1 million; Apr, April; Aug, August; Dec, December; Dem, Democratic; Max, maximum; Nov, November; Oct, October; PI, posterior interval; Rep, Republican; Sep, September.
Figure 3.
(A) PCR testing rates per 1K individuals by governor affiliation; (B) adjusted RRs and PIs. RRs >1 indicate higher rates for Rep governors. 1K, 1,000; Apr, April; Aug, August; Dec, December; Dem, Democratic; Max, maximum; Nov, November; Oct, October; PCR, polymerase chain reaction; PI, posterior interval; Rep, Republican; Sep, September.
Figure 4.
(A) PCR test positivity rates per 100 tests by governor affiliation; (B) adjusted RRs and PIs. RRs >1 indicate higher rates for Rep governors. Apr, April; Aug, August; Dec, December; Dem, Democratic; Max, maximum; Nov, November; Oct, October; PCR, polymerase chain reaction; PI, posterior interval; Rep, Republican; Sep, September.
DISCUSSION
In this longitudinal analysis, Republican-led states had fewer per capita COVID-19 cases, deaths, and positive tests early in the pandemic, but these trends reversed in early May 2020 (positive tests), June 2020 (cases), and July 2020 (deaths). Testing rates were similar until September 2020, when Republican states fell behind Democratic states. The early trends could be explained by the high COVID-19 cases and deaths among Democratic-led states that were home to the initial ports of entry for the virus in early 2020.9 , 10 However, the subsequent reversal in trends, particularly with respect to testing, may reflect policy differences that could have facilitated the spread of the virus (C Adolph, PhD, unpublished data, September 2020 and P Matzinger, PhD, unpublished data, September 2020).3 , 4 , 6 , 7
Adolph et al.3 found that Republican governors were slower to adopt both stay-at-home orders and mandates to wear face masks. Other studies have shown that Democratic governors were more likely to issue stay-at-home orders with longer durations.4 , 5 Moreover, decisions by Republican governors in spring 2020 to retract policies, such as the lifting of stay-at-home orders on April 28, 2020 in Georgia,20 may have contributed to increased cases and deaths. Democratic states also had lower test positivity rates from May 30, 2020 through December 15, 2020, suggesting more rigorous containment strategies in response to the pandemic. Thus, governors’ political affiliation might function as an upstream progenitor of multifaceted policies that in unison impact the spread of the virus. Although there were exceptions in states such as Maryland and Massachusetts, Republican governors were generally less likely to enact policies aligned with public health social distancing recommendations.3
Limitations
This is the first study to quantify the differences over time on the basis of governor party affiliation. However, there are limitations. This was a population-level rather than individual-level analysis. Although analyses were adjusted for potential confounders (e.g., rurality), the findings could reflect the virus's spread from urban to rural areas.9 , 10 In addition, as with any observational study, causality cannot be inferred. Finally, governors are not the only authoritative actor in a state; governors in states such as Wisconsin may have been limited by Republican-controlled legislatures. Future research could explore the associations between party affiliation of state or local legislatures, particularly when these differ from those of the governors.
CONCLUSIONS
These findings suggest that governor political party affiliation may differentially impact COVID-19 incidence and death rates. Attitudes toward the pandemic were highly polarized in 2020.6, 7, 8 , 21, 22, 23 Future state policy actions should be guided by public health considerations rather than by political expedience24 and should be supported by a coordinated federal response within the new presidential administration.
ACKNOWLEDGMENTS
The content of this article does not represent the views of the Department of Veterans Affairs or the U.S. government. This article represents the views of the authors and not those of the Department of Veterans Affairs or Health Services Research and Development. The funder had no influence on the study design, implementation, or findings.
BN is a part-time employee of the Department of Veterans Affairs. NTM was supported by the National Heart, Lung, and Blood Institute of NIH under Award Number K01HL141589 (Principal Investigator: NTM).
Author contributions are as follows: BN had full access to all data in the study and took responsibility for the integrity of the data and the accuracy of the data analysis. BN, NTM, JLP, and SEBN contributed to the concept and design of the study. BN and FM contributed to the acquisition, analysis, and interpretation of the data. BN and SEBN drafted the manuscript, and NTM, JLP, and FM provided critical revisions.
A preprint of this manuscript is posted on MedRχiv at www.medrxiv.org/content/10.1101/2020.10.08.20209619v1.
No financial disclosures were reported by the authors of this paper.
Footnotes
Supplemental materials associated with this article can be found in the online version at https://doi.org/10.1016/j.amepre.2021.01.034.
Appendix. SUPPLEMENTAL MATERIAL
REFERENCES
- 1.COVID data tracker: United States laboratory testing. Centers for Disease Control and Prevention. https://www.cdc.gov/covid-data-tracker/index.html#testing. Updated March 23, 2021. Accessed December 15, 2020.
- 2.Gostin LO, Wiley LF. Governmental public health powers during the COVID-19 pandemic: stay-at-home orders, business closures, and travel restrictions. JAMA. 2020;323(21):2137–2138. doi: 10.1001/jama.2020.5460. [DOI] [PubMed] [Google Scholar]
- 3.Adolph C, Amano K, Bang-Jensen B, Fullman N, Wilkerson J. Pandemic politics: timing state-level social distancing responses to COVID-19. J Health Polit Policy Law. Online September 16, 2020 doi: 10.1215/03616878-8802162. In Press. [DOI] [PubMed] [Google Scholar]
- 4.Baccini L, Brodeur A. Explaining governors’ response to the COVID-19 pandemic in the United States. Am Polit Res. 2021;49(2):215–220. doi: 10.1177/1532673X20973453. [DOI] [Google Scholar]
- 5.Kosnik LR, Bellas A. Drivers of COVID-19 stay at home orders: epidemiologic, economic, or political concerns? Econ Disaster Clim Chang. 2020;4(3):503–514. doi: 10.1007/s41885-020-00073-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Grossman G, Kim S, Rexer JM, Thirumurthy H. Political partisanship influences behavioral responses to governors’ recommendations for COVID-19 prevention in the United States. Proc Natl Acad Sci U S A. 2020;117(39):24144–24153. doi: 10.1073/pnas.2007835117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Christensen SR, Pilling EB, Eyring JB, Dickerson G, Sloan CD, Magnusson BM. Political and personal reactions to COVID-19 during initial weeks of social distancing in the United States. PLoS One. 2020;15(9) doi: 10.1371/journal.pone.0239693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jiang J, Chen E, Lerman K, Ferrara E. Political polarization drives online conversations about COVID-19 in the United States. Hum Behav Emerg Technol. Online June 18, 2020 doi: 10.1002/hbe2.202/v2/response1. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paul R, Arif AA, Adeyemi O, Ghosh S, Han D. Progression of COVID-19 from urban to rural areas in the United States: a spatiotemporal analysis of prevalence rates. J Rural Health. 2020;36(4):591–601. doi: 10.1111/jrh.12486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Y, Liu Y, Struthers J, Lian M. Spatiotemporal characteristics of COVID-19 epidemic in the United States. Clin Infect Dis. 2021;72(4):643–651. doi: 10.1093/cid/ciaa934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The data. The COVID Tracking Project, The Atlantic Monthly Group. https://covidtracking.com/data. Updated Updated March 7, 2021. Accessed December 16, 2020.
- 12.COVID-19 diagnostic laboratory testing (PCR testing) time series. HealthData.gov. https://healthdata.gov/dataset/COVID-19-Diagnostic-Laboratory-Testing-PCR-Testing/j8mb-icvb. Updated March 24, 2021. Accessed December 16, 2020.
- 13.County population totals: 2010-2019. United States Census Bureau. https://www.census.gov/data/tables/time-series/demo/popest/2010s-counties-total.html. Updated June 22, 2020. Accessed September 1, 2020.
- 14.Rankings data & documentation. County Health Rankings & Roadmaps, Robert Wood Johnson Foundation.https://www.countyhealthrankings.org/explore-health-rankings/rankings-data-documentation. Updated March 24, 2021. Accessed August 8, 2020.
- 15.BRFSS prevalence & trends data. Centers for Disease Control and Prevention. https://www.cdc.gov/brfss/brfssprevalence/index.html. Updated September 13, 2017. Accessed February 15, 2021.
- 16.Dadaneh SZ, Zhou M, Qian X. Bayesian negative binomial regression for differential expression with confounding factors [published correction appears in Bioinformatics. 2019;35(13):2346] Bioinformatics. 2018;34(19):3349–3356. doi: 10.1093/bioinformatics/bty330. [DOI] [PubMed] [Google Scholar]
- 17.Wasserman D, Andrews S, Saenger L, Cohen L, Flinn A, Tatarsky. 2020 National popular vote tracker. The Cook Political Report. https://cookpolitical.com/2020-national-popular-vote-tracker. Updated March 24, 2021. Accessed December 16, 2020.
- 18.Kneib T, Konrath S, Fahrmeir L. High dimensional structured additive regression models: Bayesian regularization, smoothing and predictive performance. J R Stat Soc Ser C Appl Stat. 2011;60(1):51–70. doi: 10.1111/j.1467-9876.2010.00723.x. [DOI] [Google Scholar]
- 19.Pillow J, Scott J. In: Advances in Neural Information Processing Systems 25. Bartlett P, Pereira FCN, Burges CJC, Bottou L, Weinberger KQ, editors. MIT Press; Cambridge, MA: 2012. Fully Bayesian inference for neural models with negative-binomial spiking; pp. 1907–1915. [Google Scholar]
- 20.Each state's COVID-19 Reopening and reclosing plans and mask requirements. National Academy for State Health Policy. https://www.nashp.org/governors-prioritize-health-for-all/. Updated March 22, 2021. Accessed September 30, 2020.
- 21.Leventhal AM, Dai H, Barrington-Trimis JL, et al. Association of political party affiliation with physical distancing among young adults during the COVID-19 pandemic. JAMA Intern Med. 2021;181(3):399–403. doi: 10.1001/jamainternmed.2020.6898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Havey NF. Partisan public health: how does political ideology influence support for COVID-19 related misinformation? J Comput Soc Sci. 2020;3(2):319–342. doi: 10.1007/s42001-020-00089-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang VH, Pagán JA. Views on the need to implement restriction policies to be able to address COVID-19 in the United States. Prev Med. 2021;143 doi: 10.1016/j.ypmed.2020.106388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guest JL, Del Rio C, Sanchez T. The three steps needed to end the COVID-19 pandemic: bold public health leadership, rapid innovations, and courageous political will. JMIR Public Health Surveill. 2020;6(2):e19043. doi: 10.2196/19043. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.