Abstract
Objective:
Women who have experienced childhood maltreatment are at increased risk for experiencing mental health problems. When these occur during pregnancy, they are associated with birth complications and worse developmental outcomes for children. Emotion dysregulation (ED) may be an important, and potentially modifiable, mechanism that links women’s maltreatment experiences with their mental health. However, there is limited information about the emotion regulation skills of pregnant women to guide treatment. The current study examines the unique effects of childhood threat (physical, sexual, and emotional abuse and exposure to violence) and deprivation (physical and emotional neglect and separation from primary caregivers) experiences on pregnant women’s ED, posttraumatic stress and negative emotional symptoms, and social support.
Method:
243 women were recruited from an urban prenatal care clinic, the majority of whom identified as Latinx (80%) and low-income (90%). The mean age of the women was 27 years (SD = 5.5).
Results:
Structural Equation Modeling revealed significant indirect pathways from childhood threat experiences to posttraumatic stress and negative emotional symptoms via women’s ED. In contrast, childhood deprivation experiences were associated with inattention to one’s emotions and low perceived social support.
Conclusions:
These results underscore the importance of identifying women during pregnancy who may be at risk for ED or emotional inattentiveness due to childhood maltreatment experiences and providing prevention and intervention efforts aimed at enhancing their emotional awareness and regulation.
Keywords: childhood maltreatment, emotion dysregulation, pregnancy, mental health
INTRODUCTION
Mental health problems are one of the most common pregnancy complications, with as many as 1 in 3 pregnant women experiencing at least one psychiatric diagnosis in the past year (Cook et al., 2010; Uguz et al., 2019; Vesga-López et al., 2008), and comorbidity is common (Le Strat et al., 2011). Psychiatric disorders during pregnancy are associated with increased risk for preterm birth, low birthweight, and other pregnancy and birth complications (Gold & Marcus, 2008; Lopez et al., 2019) as well as with children’s adverse developmental outcomes (Monk et al., 2019; Stein et al., 2014). When mental health problems persist into motherhood, the risk for the intergenerational transmission of psychopathology to the next generation of children is well-documented (Goodman et al., 2011; Leen-Feldner et al., 2013).
Women who have experienced abuse, violence exposure, and/or neglect in childhood may be at particularly high risk for the development of psychopathology (Edwards et al., 2003; Scott et al., 2012) and problems with social relationships (Davis et al., 2001; Ducharme et al., 1997), including during pregnancy (Seng et al., 2009). Therefore, understanding the mechanisms by which maltreatment incurs risk for mental health problems among pregnant women can inform prevention and intervention efforts for this vulnerable population. One such mechanism is emotion dysregulation, which has been identified as a mediating pathway linking adverse childhood experiences with a transdiagnostic array of child, adolescent, and adult mental health problems (Cloitre et al., 2019; Heleniak et al., 2016; McLaughlin et al., 2020). Yet there is limited information about the emotion regulation skills of pregnant women to guide interventions (Li et al., 2020; Lin et al., 2019).
Emotion regulation is conceptualized here as an individual’s ability to control the timing, duration, and intensity with which one’s emotions are experienced and expressed in a manner which facilitates the attainment of one’s behavioral goals and allows for optimal engagement with one’s environment (Dvir et al., 2014; Mende-Siedlecki et al., 2012; Thompson, 1994). It is comprised of a multidimensional set of skills and strategies that involves the conscious and unconscious interplay of behavioral, psychological, cognitive, and neurobiological systems (Dvir et al., 2014; Gratz & Roemer, 2004; Mende-Siedlecki et al., 2012). When these skills and strategies instead act to impede the attainment of one’s goals, emotion dysregulation results (Thompson, 2019).
The current study aims to garner a better understanding of the associations among childhood maltreatment experiences, emotion dysregulation, and mental health outcomes of a low-income sample of pregnant women at high risk for childhood maltreatment experiences and mental health disorders. Targeting the emotion regulation skills of pregnant women potentially provides a critical opportunity to reduce adverse mental health outcomes for women, improve pregnancy outcomes, and interrupt the intergenerational transmission of psychopathology. Further, because racial/ethnic minority women are at higher risk for mental health difficulties related to pregnancy (Howell et al., 2005), the current study investigates these associations among a sample of primarily Latinx women participating in a larger study examining prenatal stress and trauma-related epigenetic effects.
Mental health and emotion dysregulation in pregnancy
Estimates of past year psychiatric diagnoses in pregnant women range from 18–31%, with higher rates found among low-income women (Cook et al., 2010; Uguz et al., 2019; Vesga-López et al., 2008) and Latinx women (Kuo et al., 2004; Lara et al., 2008). Major depressive disorder, PTSD, and anxiety disorders are the most prevalent diagnoses (when nicotine dependence is excluded). Despite the fact that the vast majority of pregnant women in the United States have contact with a healthcare provider during their pregnancy (Osterman & Martin, 2018), pregnant women are less likely than non-pregnant women to receive mental health treatment (Vesga-López et al., 2008), with women in economically disadvantaged populations (Farr et al., 2010) and of minority racial/ethnic backgrounds (Lara-Cinisomo et al., 2018) having even lower odds of receiving treatment. This suggests that although screening for depression and anxiety during pregnancy has greatly increased over the past decade (Rhodes & Segre, 2013), identification of mental health problems and access to mental health care remains a significant concern.
Identification of problems with emotion regulation during pregnancy might help to identify a broad subset of women at risk for current and/or subsequent mental health problems during parenthood. Emotion dysregulation is a transdiagnostic feature of numerous mental health disorders (Kring, 2008). It has also been found in longitudinal studies to precede the onset or worsening of symptoms, suggesting that it may also be a risk factor for subsequent psychiatric diagnoses (Aldao et al., 2010; Althoff et al., 2010; Crowell et al., 2015). Indeed, in one of the few studies to examine emotion dysregulation in pregnant women, Lin et al (2019) found support for emotion dysregulation as an indicator of risk for psychopathology during pregnancy, with moderate associations between emotion dysregulation and depressive, anxious, borderline, and self-injurious symptoms.
Childhood maltreatment, emotion regulation, and maternal mental health.
Although much of the extant child maltreatment literature examines either single subtypes of maltreatment or cumulative profiles of polyvictimization, there is emerging evidence that these approaches may obscure the unique effects of different types of maltreatment experiences. McLaughlin and her colleagues have proposed a dimensional model that suggests that childhood threat (involving harm and/or threat of harm) and deprivation (involving the absence or removal of expected physical, cognitive or social inputs from the environment) experiences have unique consequences on the development of emotional, cognitive, and neurobiological mechanisms and are differentially associated with psychopathology (McLaughlin, 2016; McLaughlin & Sheridan, 2016; McLaughlin et al., 2014). Recent studies of children and adolescents associate threat experiences with alterations in the ways in which emotions and social information are processed (Lambert et al., 2017; Machlin et al., 2019; McLaughlin et al., 2020). In contrast, deprivation experiences have been associated with impaired executive function skills and deficits in language learning (Lambert et al., 2017; Machlin et al., 2019; McLaughlin, 2016; Miller et al., 2018; Wolf & Suntheimer, 2019).
Given these potentially disparate pathways, it is likely that threat and deprivation experiences will likewise have different associations with emotion regulation. The research linking threat experiences to emotional processing suggest that these experiences may have direct associations with emotion regulation, and that women’s threat experiences and mental health outcomes may be linked indirectly via emotion regulation (Berzenski, 2019; Milojevich et al., 2019; Weiss et al., 2013). Indeed, Milojevich and colleagues (2019) examined the use of adaptive and maladaptive emotion regulation strategies among a high-risk sample of adolescents, finding that experiences of threat, but not deprivation, were associated with greater use of avoidant regulation strategies. These strategies, in turn, predicted depressive and posttraumatic stress symptoms. In contrast, deprivation experiences are not expected to be associated directly with deficits in emotion regulation skills; rather, they may be linked directly to mental health outcomes via executive functioning or cognitive deficits (e.g., Infurna et al., 2016; Nikulina et al., 2011; Widom et al., 2007).
Current study
The current study extends previous research examining differential trajectories of threat (physical, sexual, and emotional abuse and exposure to violence) and deprivation (physical and emotional neglect and separation from primary caregivers) experiences. To date, most of the studies exploring threat and deprivation pathways, as described above, have been conducted with adolescents and young adults. Given the aforementioned risks associated with mental health problems during pregnancy, we extend these findings by examining the unique associations of childhood threat and deprivation experiences on problems with emotion regulation among a highly stressed, low SES, ethnic minority sample of adult women in their third trimester of pregnancy. We further examine the role of emotion dysregulation in the association between childhood maltreatment and three indicators of mental health in pregnant women: PTSD symptoms, negative emotionality, and social support. Because lack of social support is associated with postpartum depression, posttraumatic stress symptoms, and poor pregnancy outcomes, and increased social support has been found to be protective against these adverse outcomes, it is included here as an important mental health indicator (Elsenbruch et al., 2006; Morikawa et al., 2015; Sumner et al., 2012). We hypothesized that there would be unique direct associations between childhood threat and deprivation experiences and women’s increased risk for mental health problems during pregnancy. Because of the emerging evidence associating threat (but not deprivation) experiences with emotional processing, we also hypothesized that there would be an indirect path from threat experiences to increased adult mental health problems via problems with emotion regulation.
METHOD
Participants
A low SES sample of pregnant women (n = 254) was recruited from an urban prenatal care clinic as part of a larger longitudinal study examining prenatal and epigenetic effects on the stress response system of newborns (Grasso et al., 2019). Eleven women did not provide information on emotion regulation or childhood trauma experiences and were removed, resulting in final study sample of 243. The 11 women with incomplete data did not differ from the remaining participants on age, race/ethnicity, poverty status, or education.
The women in the final study sample ranged in age from 18 to 42 years (M = 27.04, SD = 5.46) and identified primarily as Latinx and did not identify a racial group (n = 121, 49.8%), followed by those who identified as Latinx and White (n = 58, 23.9%), Black and non-Latinx (n = 31, 12.8%), Black and Latinx (n = 15, 6.2%), White and non-Latinx (n = 13, 5.3%), and Other (n = 5, 2.1%). Ninety percent of the women reported that they received Medicaid assistance and/or had an annual household income of less than $20,000. Approximately half of the sample was single and not in a committed relationship (53.3%). About half reported current employment (52.5%) and one quarter of the participants had not earned a high school diploma or a GED (24.5%); 36.5% had a high school degree or GED, 33.6% had some college or a vocational, trade school, or associate’s degree, and 5.3% had a bachelor’s or graduate degree. Childhood maltreatment experiences were reported extensively among the participants. Mean scores for each of the threat and deprivation subscales are provided in Table 1.
Table 1:
Correlations, Means, and Standard Deviations
| Age | Childhood Threat | Childhood Deprivation | Emotion Dysregulation | Mental Health | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | ||||||
| 1 | Maternal Age | ─ | .04 | −.03 | .10 | .09 | .02 | −.02 | −.01 | .03 | −.01 | −.05 | −.09 | −.09 | −.02 | −.02 | −.05 | .07 | ||||
| 2 | Physical abuse | ─ | .71*** | .55*** | .37*** | .41*** | .36*** | .23*** | .21** | .29*** | .27*** | .02 | .32*** | .23*** | .26*** | .37*** | −.13 | |||||
| 3 | Emotional abuse | ─ | .54*** | .44*** | .49*** | .51*** | .29*** | .35*** | .33*** | .36*** | .02 | .44*** | .33*** | .35*** | .50*** | −.26*** | ||||||
| 4 | Sexual abuse | ─ | .28*** | .25*** | .21** | .27*** | .28*** | .24*** | .20** | −.05 | .21** | .13* | .20** | .32*** | −.08 | |||||||
| 5 | Witness violence | ─ | .24*** | .18** | .21** | .25*** | .26*** | .21** | −.08 | .26*** | .20** | .24*** | .31*** | −.02 | ||||||||
| 6 | Physical neglect | ─ | .69*** | .28***. | .20** | .16* | .29*** | .28*** | .26*** | .31*** | .12 | .25*** | −.38*** | |||||||||
| 7 | Emotional neglect | ─ | .18** | .22** | .20** | .34*** | .35*** | .27*** | .37*** | .09 | .21** | −.47*** | ||||||||||
| 8 | Separation | ─ | .12 | .12 | .14* | −.01 | .14* | .17** | .26*** | .21** | −.18** | |||||||||||
| 9 | Non-acceptance | ─ | .55*** | .57*** | −.01 | .71*** | .46*** | .46*** | .67*** | −.09 | ||||||||||||
| 10 | Goals | ─ | .58*** | .11 | .75*** | .44*** | .43*** | .66*** | −.20** | |||||||||||||
| 11 | Impulsivity | ─ | .30*** | .73*** | .47*** | .37*** | .62*** | −.23*** | ||||||||||||||
| 12 | Awareness | ─ | .24*** | .49*** | −.02 | .11 | −.22** | |||||||||||||||
| 13 | Strategies | ─ | .55*** | .47*** | .81*** | −.26** | ||||||||||||||||
| 14 | Clarity | ─ | .34*** | .52*** | −.29*** | |||||||||||||||||
| 15 | PTSS | ─ | .55*** | −.13* | ||||||||||||||||||
| 16 | Neg. emotionality | ─ | −.19** | |||||||||||||||||||
| 17 | Social support | ─ | ||||||||||||||||||||
| Mean/% | 27.0 | 6.73 | 8.49 | 7.38 | 16 % | 7.63 | 10.74 | 16 % | 10.42 | 10.72 | 10.29 | 14.84 | 13.79 | 8.73 | 17.83 | 0.00 | 62.87 | |||||
| SD | 5.46 | 3.26 | 4.93 | 4.96 | ─ | 3.13 | 5.74 | ─ | 4.95 | 4.82 | 4.34 | 5.78 | 5.92 | 3.44 | 15.80 | 0.95 | 19.30 | |||||
Note:
p < .05,
p < .01,
p < .001
Procedures
The current study is a secondary analysis of data from a larger study examining prenatal stress and trauma-related epigenetic effects in pregnant women and their newborn infants. The study was approved by the institutional review boards of UConn Health, Hartford Hospital, and Connecticut Children’s Medical Center. Pregnant women in their third trimester of pregnancy were invited to participate during prenatal care visits at an urban women’s health clinic. Women were eligible if they were English speaking, having a singleton pregnancy, and planned to deliver at Hartford Hospital. Informed consent was obtained by research staff. Following informed consent, during a prenatal appointment at the women’s health clinic, women completed a battery of self-report measures on a computer tablet equipped with REDCap survey software. A research assistant facilitated data collection and was available to address any questions or concerns. A licensed clinical psychologist provided on-call support in the event that any of the women requested to speak with a mental health professional; however, this was never requested nor was it necessary. Clinic social work staff were also available if onsite support were needed. Participants were compensated for their involvement in the study.
Measures
Childhood threat and deprivation experiences.
Childhood abuse and neglect experiences were evaluated based on the women’s responses on the Childhood Trauma Questionnaire (CTQ; Bernstein & Fink, 1998). The CTQ is a widely-used 28-item self-report inventory assessing five types of trauma experienced as a child and/or teenager: emotional, physical and sexual abuse, and emotional and physical neglect (e.g., “People in my family hit me so hard that it left me with bruises or marks.”). Each of these scales has 5 items that are rated on a 5-point scale according to their frequency (1 = never true to 5 = very often true) and summed to yield a total score for each type of trauma, ranging from 5 to 25, with higher scores indicating greater severity. The CTQ has been demonstrated to have acceptable convergent validity, test-retest reliability, and internal consistency in both clinical and community samples (Scher et al., 2001). The 5 subscales used in the current study demonstrated acceptable internal consistency in the current sample (Cronbach’s α from .88 - .93 for all subscales except physical neglect, α = .57). Witnessing Violence and Separation from Caregivers were each assessed with an item (‘Did you ever see or hear adults in your home beat each other up or throw things at each other?’ and ‘Were you separated from a parent or someone you depended on for love or safety for an extended period of time?’, respectively) from the trauma inventory child exposure portion of the Structured Trauma-Related Experiences and Symptom Screener for Adults (STRESS-A; Grasso et al., 2019).
Emotion dysregulation.
Participants’ emotion dysregulation was measured with the Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004), a 36-item self-report scale that assesses 6 facets of emotion dysregulation: Non-acceptance (6 items; negative response to one’s negative emotions), Goals (5 items; difficulty engaging in desired, goal-directed behavior when experiencing negative emotions), Impulse (6 items; ability to inhibit undesired behaviors when experiencing negative emotions), Awareness (6 items; inattention to one’s emotional response), Strategies (8 items; belief that there is little one can do to control their emotional response), and Clarity (5 items; lack of knowledge of emotions one is experiencing). Items are rated on a 5-point scale (almost never, sometimes, about half the time, most of the time, and almost always), and were summed to create each subscale score, with higher scores indicating greater difficulty with emotion regulation. The 6 subscales were used in the current study and demonstrated adequate internal consistency (Cronbach’s α from .76 to .86 for all subscales except Clarity, α = 68). The DERS has demonstrated good reliability and validity among racially and ethnically diverse populations (Bjureberg et al., 2016).
Previous investigations have indicated that the Awareness subscale may not measure the same underlying construct as the other five DERS subscales. In numerous studies, it has demonstrated only modest associations with the other DERS subscales (Hallion et al., 2018) and failed to correlate with mental health symptoms and/or differentiate between groups of individuals in the same pattern as the other subscales (Bardeen & Fergus, 2014; Hallion et al., 2018; Osborne et al., 2017). Rather, noticing one’s emotions may be discrete from responding to one’s emotions (Hallion et al., 2018). Several researchers recommend using a revised DERS total score that excludes Awareness items (Bardeen & Fergus, 2014; Hallion et al., 2018; Osborne et al., 2017). In the current study, therefore, we first tested the factor structure of the emotion dysregulation variable before proceeding with the structural model.
Posttraumatic stress symptoms.
Posttraumatic stress symptoms (PTSS) were evaluated utilizing the symptom report of the Structured Trauma-Related Experiences and Symptom Screener for Adults (STRESS-A; Grasso et al., 2019). Participants rated the frequency of symptoms experienced over the past week on a 4-point rating scale (none, 1 day, 2–3 days, most days). A total symptom severity score was used (Cronbach’s α = .95). The STRESS-A has demonstrated reliability, validity and clinical utility (Grasso et al., 2019).
Negative emotionality.
Negative emotional symptoms were assessed with the Depression, Anxiety, Stress Scales (DASS-42; Lovibond & Lovibond, 1995), a self-report measure that has been well-validated in clinical (Brown et al., 1997) and non-clinical populations (Crawford & Henry, 2003), consisting of three 14-item subscales: depression (Cronbach’s α = .95), anxiety (Cronbach’s α = .90), and stress (Cronbach’s α = .94). Participants rated their negative emotional state during the past week on a 4-point scale (did not apply, applied to me to some degree, applied to me to a considerable degree, applied to me much); items are summed to create each subscale score. In the current sample, because correlations among the subscales were high (rs from .84 to .86), the 3 subscales were z-score converted and averaged to create a composite score reflecting negative emotional state, following guidelines of the measure developers (www2.psy.unsw.edu.au).
Social Support.
Perceived social support scores were derived from the women’s responses to the Multidimensional Scale of Perceived Social Support (MSPSS; Zimet et al., 1988), a 12-item self-report measure of the perceived adequacy of one’s support from friends, family members, and significant others with demonstrated validity in a wide range of samples, including among pregnant women (Zimet et al., 1990). Items are rated on a 7-point scale (from very strongly agree to very strongly disagree); reliability in the current sample was excellent (Cronbach’s α = 96).
Analytic Plan
All analyses were conducted using SPSS version 25 and Mplus version 8. Descriptive statistics were calculated for all study variables and preliminary analyses examined inter-relationships among study variables and the following potential demographic covariates: participants’ age, poverty status, race/ethnicity, and education.
Given the extant literature’s mixed support for the 6-subscale model of the DERS, we first conducted confirmatory factor analyses of 5- and 6-subscale models of emotion dysregulation. Next, measurement models testing the hypothesized latent variables of deprivation and threat experiences and the DERS total score were evaluated using Confirmatory Factor Analysis (CFA). Structural equation modeling (SEM) was then used to examine the hypothesized associations among the childhood maltreatment, emotion dysregulation, and mental health outcomes. To address non-normality in the outcome variables and two categorical indicators of the deprivation and threat latent variables, weighted least square mean and variance adjusted (WLSMV) estimation was used in the SEM models (Brown, 2006). Indirect effects in the final model were evaluated using 95% bias-corrected confidence intervals generated by 2,500 bootstrap samples. Current research indicates that commonly accepted cut-off values for model fit statistics that have been established using maximum likelihood estimation (e.g., those established by Hu and Bentler (1999)), may not be appropriate for use with ordered categorical data. Therefore, no a priori fit statistics are suggested here (Xia & Yang, 2019).
Results
Descriptive Statistics
Table 1 presents Pearson correlations among the study variables and the continuous demographic characteristics. The childhood maltreatment variables demonstrated primarily low to moderate intercorrelations, with the exception of the associations among physical and emotional abuse (r = .71) and physical and emotional neglect (r = .69). Most of the DERS subscales were moderately to highly intercorrelated, with the notable exception of the Awareness scale which was not associated with Non-Acceptance or Goals. Similarly, while most of the DERS subscales correlated with the child maltreatment variables, the Awareness scale was associated only with the Neglect variables. Together, these seemingly different patterns of association lend support to the analytical plan to investigate the 5- and 6-subscale models of the emotion dysregulation latent construct in this sample. Associations among child maltreatment, emotion dysregulation, and the mental health outcome variables were in the expected directions (positive for PTSS and negative emotionality; negative for social support).
Kruskal-Wallis H tests were used to examine associations between the non-normally distributed mental health outcome variables (PTSS, Negative Emotionality, and Social Support) and the categorical education and race/ethnicity variables. Mann-Whitney U tests were used to examine associations with the dichotomous poverty status variable. There were no statistically significant associations among the education, race/ethnicity or poverty status variables and the mental health outcome variables. Similarly, mental health outcome variables were not correlated with maternal age (see Table 1). Therefore, the demographic variables were not included as covariates in the models.
Structural Equation Models
Confirmatory Factor Analysis of the DERS.
The first step of our analyses was to examine the fit of a single factor model using either 5- or 6-subscales of the DERS by running separate models with and without the Awareness subscale. Fit for the single factor model using all 6 subscales (Strategies, Goals, Impulse, Non-Acceptance, Clarity and Awareness) was poor [χ2(9) = 99.964, p < .001; RMSEA = .20 [.17, .24]; CFI = .88; SRMR = .08]. In contrast, the single factor model using 5 subscales (excluding Awareness) exhibited good fit [χ2(5) = 2.626, p < .757; RMSEA = 0 [0, .06]; CFI = 1.0; SRMR = .01]. Therefore, the 5-subscale Emotion Dysregulation latent variable was used in the remaining models, and the Awareness subscale score was retained as an independent exogenous variable.
Measurement.
The measurement portion of the SEM was conducted using CFA to test the latent constructs Deprivation, Threat, and Emotion Dysregulation. Deprivation included three indicators: the emotional and physical neglect subscales of the CTQ and the separation item from the STRESS-A. Because emotional and physical neglect are conceptually related, more than half of the items assessing these subscales are grouped together on the CTQ, and they are the only subscales on the CTQ to utilize reverse-scoring, the error of these two indicators were correlated in the measurement and structural models. Threat included four indicators: the physical, sexual, and emotional abuse subscales of the CTQ and the witnessed violence item from the STRESS-A. The five-subscale model of the DERS described above was used to measure Emotion Dysregulation. The measurement model demonstrated adequate fit [χ2(86) = 218.166 p < .001; RMSEA = .08 [.07, .09]; CFI = .84; SRMR = .06], validating the factor structure. Therefore, the latent factors were retained for the remaining analyses. Correlations among the structural variables are presented in Table 2.
Table 2:
Correlations among the latent and endogenous variables in the SEM structural model.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||
|---|---|---|---|---|---|---|---|---|
| 1 | Threat | ─ | .767 | .502 | −.009 | .390 | .537 | −.212 |
| 2 | Deprivation | ─ | .485 | .381 | .221 | .372 | −.615 | |
| 3 | Emotion Dysregulation | ─ | .282 | .535 | .854 | −.277 | ||
| 4 | Awareness | ─ | −.023 | .107 | −.221 | |||
| 5 | PTSS | ─ | .551 | −.131 | ||||
| 6 | Negative Emotion | ─ | −.191 | |||||
| 7 | Social Support | ─ |
Structure.
The direct and indirect paths between Deprivation and Threat; Awareness and emotion dysregulation; and PTSS, negative emotionality, and social support were next estimated. Because there were no statistically significant associations between demographic variables and the mediator or outcome variables, they were not included in the model. The first model included all paths between childhood maltreatment, emotion dysregulation, and mental health outcomes [χ2(86) = 218.46, p < .001; RMSEA = .08 [.07, .09]; CFI = .84; SRMR = .06] Although model fit for this full conceptual model was adequate, a second trimmed model was run in which non-statistically significant paths were deleted. Fit for the final model was also adequate: χ2(92) = 241.522, p < 001; RMSEA = .08 [.07, .09]; CFI = .82; SRMR = .07.
The final model is represented in Figure 1, with parameter estimates, standard errors, and confidence intervals presented in Table 3. Childhood deprivation experiences had a large direct effect on Awareness (β = .70, SE = .20, p = .001) such that women who reported more deprivation experiences also reported more inattention to their emotional responses (after controlling for threat experiences). Results also demonstrated a moderate direct effect of deprivation on social support (β = −.50, SE = .06, p <.001), such that women who reported more deprivation experiences in childhood perceived themselves as having less social support (after controlling for the other predictors of social support). There was no effect of childhood deprivation experiences on Emotion Dysregulation, PTSS, or Negative Emotionality. Childhood threat experiences had a moderate direct effect on Emotion Dysregulation (β = .57, SE = .08, p <.001) and Awareness (β = −.51, SE = .20, p = .011). This suggests that women who reported more threat experiences in childhood also reported greater problems regulating their emotions and less inattention to their emotional responses (after controlling for their deprivation experiences). Childhood threat experiences also had an indirect effect via Emotion Dysregulation on PTSS (β = .31, 95% CI = [.20, .42]) and Negative Emotionality (β = .46, 95% CI = [.31, .62]).
Figure 1:
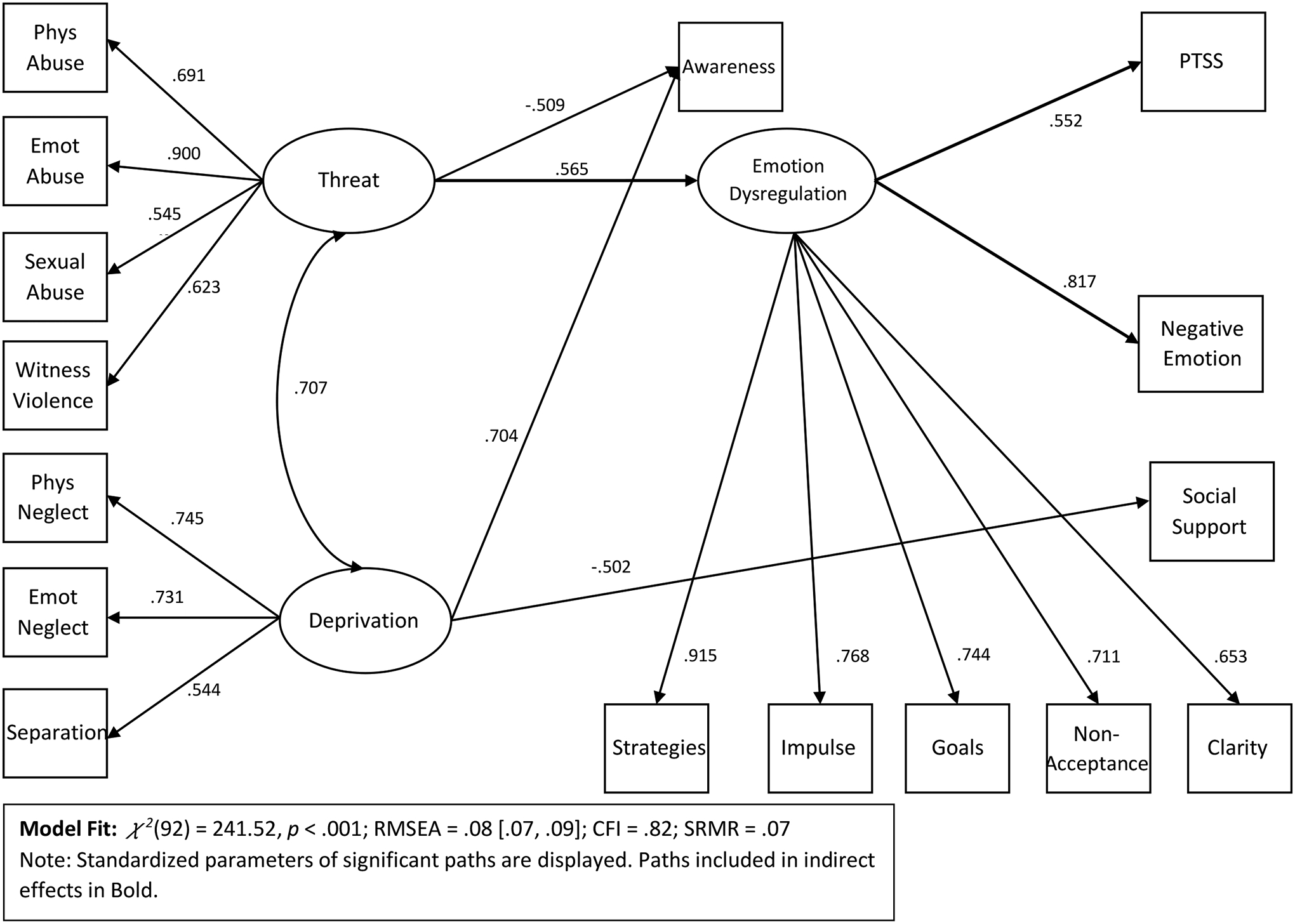
Final SEM model
Table 3:
Parameter estimates, standard errors, significance levels, and confidence intervals for model in Figure 1
| Unstandardized | SE | Standardized | SE | p | ||
|---|---|---|---|---|---|---|
| Direct Effects | ||||||
| Threat → ED | .88 | .21 | .57 | .08 | <.001 | |
| Threat → Aware | −1.30 | .60 | −.51 | .20 | .011 | |
| Deprivation → SS | −4.10 | .82 | −.50 | .06 | <.001 | |
| Deprivation → Aware | 1.74 | .61 | .70 | .20 | .001 | |
| ED → PTSS | 2.52 | .35 | .55 | .06 | <.001 | |
| ED → NE | .22 | .03 | .82 | .06 | <.001 | |
| Indirect Effects | 95% CI | |||||
| Threat → ED → PTSS | 2.23 | .51 | .31 | .06 | <.001 | [.20, .42] |
| Threat → ED → NE | .20 | .05 | .46 | .08 | <.001 | [.31, .62] |
Note: ED = Emotion Dysregulation; NE = Negative Emotionality; PTSS = posttraumatic stress symptoms; SS = Social Support; reported p-values are for the standardized estimates.
Discussion
In the current study, strong associations between childhood threat experiences and emotion dysregulation, as well as between emotion dysregulation and women’s mental health, emerged among this urban, low-income sample of primarily Latinx pregnant women. Although few previous studies have examined emotion dysregulation within this population, the current findings suggest that this may be an important target of intervention for women during pregnancy.
Following the dimensional approach of McLaughlin and Sheridan (2016), we examined childhood threat and deprivation experiences separately in our analyses. The extant literature provides extensive evidence that the experience of childhood maltreatment can interfere significantly with the development of adaptive emotion regulation skills, with ensuing problems of emotion dysregulation continuing into adulthood (Cloitre et al., 2019; Dvir et al., 2014; Kim & Cicchetti, 2010; Messman-Moore & Bhuptani, 2017). Yet studies utilizing this dimensional approach provide more consistent evidence for the influence of threat rather than deprivation experiences on emotional regulation processes (Busso et al., 2017; McLaughlin et al., 2019; Miller et al., 2018). Consistent with this previous research, and as hypothesized, childhood threat experiences in the current sample were associated with adult emotion dysregulation, but childhood deprivation experiences were not.
Emotion dysregulation, in turn, was associated with mental health symptoms. As expected, greater problems with emotion regulation were associated with more PTSS and negative emotionality symptoms, and the indirect effects from childhood threat through emotion dysregulation to these symptoms were significant. These findings are consistent with numerous other studies that have identified emotion dysregulation as a mediator of the association between childhood maltreatment and posttraumatic stress, depressive, and anxious symptoms in similar cross-sectional analyses (e.g. Klumparendt et al., 2019; Poole et al., 2017; Stevens et al., 2013). Although these other studies primarily use broad indices of childhood trauma that include both elements of threat and deprivation, the current study suggests that these effects may be specific to childhood threat. Interestingly, direct effects from threat experiences to symptoms did not emerge, suggesting these pathways may be fully mediated by problems of emotion dysregulation although the contemporaneous assessment of emotion dysregulation and mental health symptoms in the current study could not be used to confirm this explanatory mechanism.
Deprivation experiences, on the other hand, were strongly associated with deficits in women’s ability to pay attention to and acknowledge their own emotional state, as measured by the DERS Awareness subscale. This finding is consistent with existing research linking childhood neglect with alexithymia (Aust et al., 2013; Brown et al., 2018) and poor emotional understanding (Edwards et al., 2005). Children’s experience of emotions and emotion regulation are socialized during interactions with their parents through direct modeling of emotional expression, labeling of emotional experiences, and supportive and appropriate responding to children’s emotional displays (Eisenberg et al., 1998). However, when children reside in environments characterized by the types of deprivation assessed in the current study (neglect and separation), parents are likely to be unreliable or unavailable to meet children’s needs, and have been found to engage in less emotion talk and provide less support of children’s negative emotions (Edwards et al., 2005; Milot et al., 2010). As a result, children may not have the opportunity to develop emotional literacy and awareness, or, given repeated unrecognized, invalidated, or mismatched responses to their emotions, may learn to ignore or numb their emotional experience.
In contrast, childhood threat experiences were predictive of less inattention to one’s emotions. Children who are exposed to violence are likely to pay close attention to the emotional climate in which they reside, developing a heightened, survival-oriented capacity to anticipate, detect and respond to real or perceived threats (Briggs-Gowan et al., 2015; Pollak, 2008). It is possible that for some victims of abuse and violence exposure, this sensitivity to threat may also incorporate a heightened attunement to their own stress reactivity cues and/or negative emotions. Along these lines, a small body of literature has identified an association between childhood trauma and emotional rumination (Kim et al., 2017; Raes & Hermans, 2008). Other investigations have found that emotional awareness can moderate the impact of abuse on psychopathology and revictimization (Westbrook & Berenbaum, 2017; Zamir & Lavee, 2015), suggesting that emotional awareness may have a complex association with threat experiences warranting further investigation.
In the current study, deprivation experiences were not associated with self-reported PTSS or negative emotionality symptoms. Although some associations between neglect (Schalinski et al., 2016) and separation (Briggs-Gowan et al., 2019) and symptoms of psychopathology have been previously documented, the current findings are consistent with McLaughlin’s dimensional model (McLaughlin, 2016). According to this framework, it would be expected that the association between deprivation and psychopathology is mediated by an indirect process not assessed in the current study, such as impaired executive functioning or cognitive deficits. Further, the identified association of deprivation with lack of emotional awareness suggests that women in the current sample who have experienced separation and neglect have difficulty accurately assessing their emotional symptoms and therefore the self-reported symptom questionnaires utilized here may not accurately capture their emotional experience. Given this association with emotional awareness, future studies with survivors of deprivation experiences would benefit from the use of a structured interview to assess participants’ symptoms.
Consistent with extensive research among victims of child maltreatment (e.g., Sperry & Widom, 2013), deprivation experiences were strongly associated with women’s reports of a lack of social support. This finding is also in line with the dimensional model’s suggestion that deprivation is associated with blunted reward processing (Novick et al., 2018), which in turn is associated with multiple forms of psychopathology (Zald & Treadway, 2017). While much of the human and animal research in this area examines the processing of material rewards (e.g. food or money), common neural substrates – in particular, the striatum – are involved in the evaluation of both material and social rewards (e.g. smiles, praise; Bhanji & Delgado, 2014), suggesting that deprivation may likewise be associated with a reduced valuation of and/or motivation to seek out social rewards that could interfere with the attainment of social interactions and thus, social support. This association with blunted reward processing, however, has not been found consistently among survivors of childhood threat experiences.
The association between deprivation experiences and reduced social support may be particularly salient for pregnant women, as social support is associated with pregnant women’s emotional and physical outcomes. Women who perceive themselves to have low social support are more likely to develop depressive symptoms and report a lower quality of life during pregnancy and are at greater risk of pregnancy complications and postpartum depression (Elsenbruch et al., 2006; Feldman et al., 2000; Hahn-Holbrook et al., 2013). Further the presence of social support has been found to buffer against the effect of psychological distress on cortisol secretion among pregnant women (Giesbrecht et al., 2013).
A few limitations of the current study should be noted, the most significant of which is the reliance on self-report for all of the measures. In particular, retrospective reports of childhood maltreatment may be influenced by current circumstances and psychological state (White et al., 2007). In the absence of prospective studies, future research might utilize child protection records or other corroborating evidence. Similarly, self-reported mental health symptoms might have been influenced by participants’ emotion regulation styles and emotional awareness, as noted earlier, and would benefit from the assessment of symptoms by diagnostic interview. Our investigation did not account for the timing of threat and deprivation experiences in childhood. Given variations in the sensitive periods of social, emotional, and cognitive development and the neurobiological systems that support them, it is possible that the timing of children’s exposure to threat and deprivation experiences may affect their influence on the development of emotion regulation (McLaughlin et al., 2019). Finally, because the current study consists of a largely Latinx and low-income sample of women, the findings may not generalize to other populations of pregnant women and warrant further investigation. Nevertheless, the study’s focus on this otherwise under-studied population of women is also one of its strengths.
Conclusions
Mental health problems in pregnancy are common and pose significant risks to the health and well-being of mothers and their children, especially for women with a history of child maltreatment experiences. Difficulty with emotion regulation is not only a common element of many psychological disorders, it also may be an indicator of emerging psychopathology. The current study suggests that for pregnant women with childhood threat experiences, emotion dysregulation may be a critical pathway by which those experiences influence poor mental health outcomes. For women with deprivation experiences, inattention to their emotional experiences and lack of social support may be significant concerns. Thus, identifying women during pregnancy who may be at risk for emotion dysregulation or emotional inattentiveness due to their childhood maltreatment experiences and providing targeted prevention and intervention efforts aimed at enhancing their emotional awareness and regulation has the potential to reduce adverse mental health outcomes for women, improve pregnancy outcomes, and interrupt the intergenerational transmission of psychopathology.
Clinical Impact Statement.
This study builds upon existing evidence in support of emotion dysregulation as a mechanism linking childhood maltreatment experiences with symptoms of psychopathology by examining these associations within a low-income sample of primarily Latinx pregnant women. The findings indicate that this mechanism may be specific to threat-related maltreatment, suggesting that pregnant women who experienced childhood threat may benefit from interventions focused on enhancing their emotion regulation skills. In contrast, pregnant women who experienced childhood deprivation may benefit from interventions focused on increasing their emotional attunement and bolstering social support.
Author Note
Pilot funding for the study was provided by the Connecticut Institute for Clinical and Translational Science and the Patterson Trust Fellowship Program (PI Grasso). Later stage funding was provided by the National Institute of Child Health and Development (NICHD) (R21HD090379-01A1, PI Grasso) and the Brain and Behavior Research Foundation (PI Grasso). Additional in-kind staff effort was provided by the UConn School of Medicine, Department of Psychiatry and the Connecticut Children’s Injury Prevention Center. Support for the writing of this manuscript was provided by NICHD (K23HD094824, PI Greene). None of the funding sources were involved in the study design; collection, analysis and interpretation of data; in the writing of the report; nor in the decision to submit the article for publication. The authors declare that they have no conflict of interest.
References
- Aldao A, Nolen-Hoeksema S, & Schweizer S (2010). Emotion-regulation strategies across psychopathology: A meta-analytic review. Clinical Psychology Review, 30(2), 217–237. 10.1016/j.cpr.2009.11.004 [DOI] [PubMed] [Google Scholar]
- Althoff RR, Verhulst FC, Rettew DC, Hudziak JJ, & van der Ende J (2010). Adult outcomes of childhood dysregulation: A 14-year follow-up study. Journal of the American Academy of Child & Adolescent Psychiatry, 49(11), 1105–1116. 10.1016/j.jaac.2010.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aust S, Härtwig EA, Heuser I, & Bajbouj M (2013). The role of early emotional neglect in alexithymia. Psychological Trauma: Theory, Research, Practice, and Policy, 5(3), 225–232. 10.1037/a0027314 [DOI] [Google Scholar]
- Bardeen JR, & Fergus TA (2014). An examination of the incremental contribution of emotion regulation difficulties to health anxiety beyond specific emotion regulation strategies. Journal of Anxiety Disorders, 28(4), 394–401. 10.1016/j.janxdis.2014.03.002 [DOI] [PubMed] [Google Scholar]
- Bernstein DP, & Fink L (1998). Childhood Trauma Questionnaire: A retrospective self-report manual. The Psychological Corporation. [Google Scholar]
- Berzenski SR (2019). Distinct emotion regulation skills explain psychopathology and problems in social relationships following childhood emotional abuse and neglect. Development & Psychopathology, 31(2), 483–496. 10.1017/s0954579418000020 [DOI] [PubMed] [Google Scholar]
- Bhanji JP, & Delgado MR (2014). The social brain and reward: social information processing in the human striatum. WIREs Cognitive Science, 5(1), 61–73. 10.1002/wcs.1266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjureberg J, Ljótsson B, Tull MT, Hedman E, Sahlin H, Lundh L-G, Bjärehed J, DiLillo D, Messman-Moore T, Gumpert CH, & Gratz KL (2016). Development and Validation of a Brief Version of the Difficulties in Emotion Regulation Scale: The DERS-16. Journal of Psychopathology and Behavioral Assessment, 38(2), 284–296. 10.1007/s10862-015-9514-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Greene C, Ford J, Clark R, McCarthy KJ, & Carter AS (2019). Adverse impact of multiple separations or loss of primary caregivers on young children. European Journal of Psychotraumatology, 10(1), 1646965–1646965. 10.1080/20008198.2019.1646965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Pollak SD, Grasso D, Voss J, Mian ND, Zobel E, McCarthy KJ, Wakschlag LS, & Pine DS (2015). Attention bias and anxiety in young children exposed to family violence. Journal of child psychology and psychiatry, and allied disciplines, 56(11), 1194–1201. 10.1111/jcpp.12397 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown S, Fite PJ, Stone K, Richey A, & Bortolato M (2018). Associations between emotional abuse and neglect and dimensions of alexithymia: The moderating role of sex. Psychological Trauma: Theory, Research, Practice, and Policy, 10(3), 300–308. 10.1037/tra0000279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA (2006). Confirmatory Factor Analysis for Applied Research. The Guilford Press. [Google Scholar]
- Brown TA, Chorpita BF, Korotitsch W, & Barlow DH (1997). Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behav Res Ther, 35(1), 79–89. 10.1016/s0005-7967(96)00068-x [DOI] [PubMed] [Google Scholar]
- Busso DS, McLaughlin KA, & Sheridan MA (2017). Dimensions of Adversity, Physiological Reactivity, and Externalizing Psychopathology in Adolescence: Deprivation and Threat. Psychosom Med, 79(2), 162–171. 10.1097/psy.0000000000000369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cloitre M, Khan C, Mackintosh MA, Garvert DW, Henn-Haase CM, Falvey EC, & Saito J (2019). Emotion regulation mediates the relationship between ACES and physical and mental health. Psychological Trauma: Theory, Research, Practice, and Policy. 10.1037/tra0000374 [DOI] [PubMed] [Google Scholar]
- Cook CAL, Flick LH, Homan SM, Campbell C, McSweeney M, & Gallagher ME (2010). Psychiatric Disorders and Treatment in Low-Income Pregnant Women. Journal of Women’s Health, 19(7), 1251–1262. 10.1089/jwh.2009.1854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crawford JR, & Henry JD (2003). The Depression Anxiety Stress Scales (DASS): normative data and latent structure in a large non-clinical sample. Br J Clin Psychol, 42(Pt 2), 111–131. 10.1348/014466503321903544 [DOI] [PubMed] [Google Scholar]
- Crowell SE, Puzia ME, & Yaptangco M (2015). The ontogeny of chronic distress: emotion dysregulation across the life span and its implications for psychological and physical health. Current Opinion in Psychology, 3, 91–99. 10.1016/j.copsyc.2015.03.023 [DOI] [Google Scholar]
- Davis JL, Petretic-Jackson PA, & Ting L (2001). Intimacy dysfunction and trauma symptomatology: Long-term correlates of different types of child abuse. Journal of Traumatic Stress, 14(1), 63–79. 10.1023/a:1007835531614 [DOI] [Google Scholar]
- Ducharme J, Koverola C, & Battle P (1997). Intimacy Development:The Influence of Abuse and Gender. Journal of Interpersonal Violence, 12(4), 590–599. 10.1177/088626097012004007 [DOI] [Google Scholar]
- Dvir Y, Ford JD, Hill M, & Frazier JA (2014). Childhood maltreatment, emotional dysregulation, and psychiatric comorbidities. [Review]. Harvard Review of Psychiatry, 22(3), 149–161. 10.1097/HRP.0000000000000014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards A, Shipman K, & Brown A (2005). The Socialization of Emotional Understanding: A Comparison of Neglectful and Nonneglectful Mothers and Their Children. Child Maltreatment, 10(3), 293–304. 10.1177/1077559505278452 [DOI] [PubMed] [Google Scholar]
- Edwards V, Holden GW, Felitti VJ, & Anda RF (2003). Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the Adverse Childhood Experiences Study. American journal of Psychiatry, 160(8), 1453–1460. [DOI] [PubMed] [Google Scholar]
- Eisenberg N, Cumberland A, & Spinrad TL (1998). Parental Socialization of Emotion. Psychological Inquiry, 9(4), 241–273. 10.1207/s15327965pli0904_1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsenbruch S, Benson S, Rücke M, Rose M, Dudenhausen J, Pincus-Knackstedt MK, Klapp BF, & Arck PC (2006). Social support during pregnancy: effects on maternal depressive symptoms, smoking and pregnancy outcome. Human Reproduction, 22(3), 869–877. 10.1093/humrep/del432 [DOI] [PubMed] [Google Scholar]
- Farr SL, Bitsko RH, Hayes DK, & Dietz PM (2010). Mental health and access to services among US women of reproductive age. American Journal of Obstetrics & Gynecology, 203(6), 542.e541–542.e549. 10.1016/j.ajog.2010.07.007 [DOI] [PubMed] [Google Scholar]
- Feldman PJ, Dunkel-Schetter C, Sandman CA, & Wadhwa PD (2000). Maternal Social Support Predicts Birth Weight and Fetal Growth in Human Pregnancy. Psychosomatic Medicine, 62(5), 715–725. https://journals.lww.com/psychosomaticmedicine/Fulltext/2000/09000/Maternal_Social_Support_Predicts_Birth_Weight_and.16.aspx [DOI] [PubMed] [Google Scholar]
- Giesbrecht GF, Poole JC, Letourneau N, Campbell T, & Kaplan BJ (2013). The buffering effect of social support on hypothalamic-pituitary-adrenal axis function during pregnancy. Psychosom Med, 75(9), 856–862. 10.1097/psy.0000000000000004 [DOI] [PubMed] [Google Scholar]
- Gold KJ, & Marcus SM (2008). Effect of maternal mental illness on pregnancy outcomes. Expert Review of Obstetrics & Gynecology, 3(3), 391–401. 10.1586/17474108.3.3.391 [DOI] [Google Scholar]
- Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, & Heyward D (2011). Maternal depression and child psychopathology: A meta-analytic review [Meta-Analysis]. Clinical Child and Family Psychology Review, 14(1), 1–27. 10.1007/s10567-010-0080-1 [DOI] [PubMed] [Google Scholar]
- Grasso DJ, Ford JD, & Greene CA (2019). Preliminary psychometrics of the Structured Trauma-Related Experiences and Symptoms Screener for Adults (STRESS-A) in an urban prenatal healthcare clinic. Psychological Trauma: Theory, Research, Practice, and Policy, 11(8), 927–935. 10.1037/tra0000476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL, & Roemer L (2004). Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 26(1), 41–54. [Google Scholar]
- Hahn-Holbrook J, Dunkel Schetter C, Arora C, & Hobel CJ (2013). Placental Corticotropin-Releasing Hormone Mediates the Association Between Prenatal Social Support and Postpartum Depression. Clinical Psychological Science, 1(3), 253–265. 10.1177/2167702612470646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallion LS, Steinman SA, Tolin DF, & Diefenbach GJ (2018). Psychometric Properties of the Difficulties in Emotion Regulation Scale (DERS) and Its Short Forms in Adults With Emotional Disorders [Original Research]. Frontiers in Psychology, 9(539). 10.3389/fpsyg.2018.00539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heleniak C, Jenness JJ, Stoep AV, McCauley E, & McLaughlin KA (2016). Childood maltreatment exposure and disruptions in emotion regulation: A transdiagnostic pathway to adolesent internalizing and externalizing psychopathology. Cognitive Therapy and Research, 40, 394–415. 10.1007/s10608-015-9735-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howell EA, Mora PA, Horowitz CR, & Leventhal H (2005). Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstet Gynecol, 105(6), 1442–1450. 10.1097/01.Aog.0000164050.34126.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6, 1–55. [Google Scholar]
- Infurna MR, Reichl C, Parzer P, Schimmenti A, Bifulco A, & Kaess M (2016). Associations between depression and specific childhood experiences of abuse and neglect: A meta-analysis. J Affect Disord, 190, 47–55. 10.1016/j.jad.2015.09.006 [DOI] [PubMed] [Google Scholar]
- Kim J, & Cicchetti D (2010). Longitudinal pathways linking child maltreatment, emotion regulation, peer relations, and psychopathology. Journal of Child Psychology and Psychiatry, 51(6), 706–716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JS, Jin MJ, Jung W, Hahn SW, & Lee S-H (2017). Rumination as a Mediator between Childhood Trauma and Adulthood Depression/Anxiety in Non-clinical Participants [Original Research]. Frontiers in Psychology, 8(1597). 10.3389/fpsyg.2017.01597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klumparendt A, Nelson J, Barenbrügge J, & Ehring T (2019). Associations between childhood maltreatment and adult depression: a mediation analysis. BMC Psychiatry, 19(1), 36. 10.1186/s12888-019-2016-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kring AM (2008). Emotion Disturbances as Transdiagnostic Processes in Psychopathology. In Lewis M, Haviland-Jones JM, & Barrett LF (Eds.), Handbook of Emotions (3rd ed., pp. 691–708). Guildford Press. [Google Scholar]
- Kuo W-H, Wilson TE, Holman S, Fuentes-Afflick E, O’Sullivan MJ, & Minkoff H (2004). Depressive Symptoms in the Immediate Postpartum Period Among Hispanic Women in Three U.S. Cities [doi: 10.1023/BJOIH.0000045252.10412.fa]. [DOI] [PubMed]
- Lambert HK, King KM, Monahan KC, & McLaughlin KA (2017). Differential associations of threat and deprivation with emotion regulation and cognitive control in adolescence. Development & Psychopathology, 29(3), 929–940. 10.1017/S0954579416000584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara-Cinisomo S, Clark CT, & Wood J (2018). Increasing Diagnosis and Treatment of Perinatal Depression in Latinas and African American Women: Addressing Stigma Is Not Enough. Womens Health Issues, 28(3), 201–204. 10.1016/j.whi.2018.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lara MA, Le H-N, Letechipia G, & Hochhausen L (2008). Prenatal Depression in Latinas in the U.S. and Mexico. Maternal and Child Health Journal, 13(4), 567. 10.1007/s10995-008-0379-4 [DOI] [PubMed] [Google Scholar]
- Le Strat Y, Dubertret C, & Le Foll B (2011). Prevalence and correlates of major depressive episode in pregnant and postpartum women in the United States. J Affect Disord, 135(1), 128–138. 10.1016/j.jad.2011.07.004 [DOI] [PubMed] [Google Scholar]
- Leen-Feldner EW, Feldner MT, Knapp A, Bunaciu L, Blumenthal M, & Amstadter AB (2013). Offspring psychological and biological correlates of parental posttraumatic stress: Review of the literature and research agenda [Review]. Clinical Psychology Review, 33(8), 1106–1133. 10.1016/j.cpr.2013.09.001 [DOI] [PubMed] [Google Scholar]
- Li H, Bowen A, Bowen R, Balbuena L, Feng C, Bally J, & Muhajarine N (2020). Mood instability during pregnancy and postpartum: a systematic review. Archives of Women’s Mental Health, 23(1), 29–41. 10.1007/s00737-019-00956-6 [DOI] [PubMed] [Google Scholar]
- Lin B, Kaliush PR, Conradt E, Terrell S, Neff D, Allen AK, Smid MC, Monk C, & Crowell SE (2019). Intergenerational transmission of emotion dysregulation: Part I. Psychopathology, self-injury, and parasympathetic responsivity among pregnant women. Development & Psychopathology, 31(3), 817–831. 10.1017/S0954579419000336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez A, Becerra MB, & Becerra BJ (2019). Maternal Mental Illness Is Associated with Adverse Neonate Outcomes: An Analysis of Inpatient Data. International Journal of Environmental Research and Public Health, 16(21), 4135. https://www.mdpi.com/1660-4601/16/21/4135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy, 33(3), 335–343. 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- Machlin L, Miller AB, Snyder J, McLaughlin KA, & Sheridan MA (2019). Differential associations of deprivation and threat with cognitive control and fear conditioning in early childhood. Frontiers in Behavioral Neuroscience, 13, 80. 10.3389/fnbeh.2019.00080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA (2016). Future Directions in Childhood Adversity and Youth Psychopathology. Journal of Clinical Child & Adolescent Psychology, 45(3), 361–382. 10.1080/15374416.2015.1110823 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Colich NL, Rodman AM, & Weissman DG (2020). Mechanisms linking childhood trauma exposure and psychopathology: A transdiagnostic model of risk and resilience. BMC Med, 18(1), 96. 10.1186/s12916-020-01561-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, & Sheridan MA (2016). Beyond cumulative risk: A dimensional approach to childhood adversity. Current Directions in Psychological Science, 25(4), 239–245. 10.1177/0963721416655883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Sheridan MA, & Lambert HK (2014). Childhood adversity and neural development: Deprivation and threat as distinct dimensions of early experience. Neuroscience & Biobehavioral Reviews, 47, 578–591. 10.1016/j.neubiorev.2014.10.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Weissman D, & Bitrán D (2019). Childhood Adversity and Neural Development: A Systematic Review. Annual Review of Developmental Psychology, 1(1), 277–312. 10.1146/annurev-devpsych-121318-084950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mende-Siedlecki P, Kober H, & Ochsner KN (2012). Emotion regulation: Neural bases and beyond. In Decety J & Cacioppo JT (Eds.), Oxford Handbooks Online. Oxford University Press. 10.1093/oxfordhb/9780195342161.013.0018 [DOI] [Google Scholar]
- Messman-Moore TL, & Bhuptani PH (2017). A Review of the Long-Term Impact of Child Maltreatment on Posttraumatic Stress Disorder and Its Comorbidities: An Emotion Dysregulation Perspective. Clinical Psychology: Science and Practice, 24(2), 154–169. 10.1111/cpsp.12193 [DOI] [Google Scholar]
- Miller AB, Sheridan MA, Hanson JL, McLaughlin KA, Bates JE, Lansford JE, Pettit GS, & Dodge KA (2018). Dimensions of deprivation and threat, psychopathology, and potential mediators: A multi-year longitudinal analysis. Journal of Abnormal Psychology, 127(2), 160–170. 10.1037/abn0000331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milojevich HM, Norwalk KE, & Sheridan MA (2019). Deprivation and threat, emotion dysregulation, and psychopathology: Concurrent and longitudinal associations. Development & Psychopathology, 31(3), 847–857. 10.1017/S0954579419000294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milot T, St-Laurent D, Éthier LS, & Provost MA (2010). Trauma-Related Symptoms in Neglected Preschoolers and Affective Quality of Mother-Child Communication. Child Maltreatment, 15(4), 293–304. 10.1177/1077559510379153 [DOI] [PubMed] [Google Scholar]
- Monk C, Lugo-Candelas C, & Trumpff C (2019). Prenatal Developmental Origins of Future Psychopathology: Mechanisms and Pathways. Annu Rev Clin Psychol, 15(1), 317–344. 10.1146/annurev-clinpsy-050718-095539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morikawa M, Okada T, Ando M, Aleksic B, Kunimoto S, Nakamura Y, Kubota C, Uno Y, Tamaji A, Hayakawa N, Furumura K, Shiino T, Morita T, Ishikawa N, Ohoka H, Usui H, Banno N, Murase S, Goto S, Kanai A, Masuda T, & Ozaki N (2015). Relationship between social support during pregnancy and postpartum depressive state: a prospective cohort study. Scientific Reports, 5(1), 10520. 10.1038/srep10520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikulina V, Widom CS, & Czaja S (2011). The role of childhood neglect and childhood poverty in predicting mental health, academic achievement and crime in adulthood. Am J Community Psychol, 48(3–4), 309–321. 10.1007/s10464-010-9385-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Novick AM, Levandowski ML, Laumann LE, Philip NS, Price LH, & Tyrka AR (2018). The effects of early life stress on reward processing. Journal of Psychiatric Research, 101, 80–103. 10.1016/j.jpsychires.2018.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborne TL, Michonski J, Sayrs J, Welch SS, & Anderson LK (2017). Factor Structure of the Difficulties in Emotion Regulation Scale (DERS) in Adult Outpatients Receiving Dialectical Behavior Therapy (DBT). Journal of Psychopathology and Behavioral Assessment, 39(2), 355–371. 10.1007/s10862-017-9586-x [DOI] [Google Scholar]
- Osterman MJK, & Martin JA (2018). Timing and adequacy of prenatal care in the United States, 2016 (National Vital Statistics Reports, Issue. N. C. f. H. Statistics. [PubMed]
- Pollak SD (2008). Mechanisms Linking Early Experience and the Emergence of Emotions: Illustrations From the Study of Maltreated Children. Current Directions in Psychological Science, 17(6), 370–375. 10.1111/j.1467-8721.2008.00608.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poole JC, Dobson KS, & Pusch D (2017). Anxiety among adults with a history of childhood adversity: Psychological resilience moderates the indirect effect of emotion dysregulation. J Affect Disord, 217, 144–152. 10.1016/j.jad.2017.03.047 [DOI] [PubMed] [Google Scholar]
- Raes F, & Hermans D (2008). On the mediating role of subtypes of rumination in the relationship between childhood emotional abuse and depressed mood: brooding versus reflection. Depression and Anxiety, 25(12), 1067–1070. 10.1002/da.20447 [DOI] [PubMed] [Google Scholar]
- Rhodes AM, & Segre LS (2013). Perinatal depression: a review of US legislation and law. Archives of Women’s Mental Health, 16(4), 259–270. 10.1007/s00737-013-0359-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schalinski I, Teicher MH, Nischk D, Hinderer E, Müller O, & Rockstroh B (2016). Type and timing of adverse childhood experiences differentially affect severity of PTSD, dissociative and depressive symptoms in adult inpatients. BMC Psychiatry, 16(1), 295. 10.1186/s12888-016-1004-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scher CD, Stein MB, Asmundson GJG, McCreary DR, & Forde DR (2001). The Childhood Trauma Questionnaire in a Community Sample: Psychometric Properties and Normative Data [journal article]. Journal of Traumatic Stress, 14(4), 843–857. 10.1023/a:1013058625719 [DOI] [PubMed] [Google Scholar]
- Scott KM, McLaughlin KA, Smith DA, & Ellis PM (2012). Childhood maltreatment and DSM-IV adult mental disorders: comparison of prospective and retrospective findings. Br J Psychiatry, 200(6), 469–475. 10.1192/bjp.bp.111.103267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Low LK, Sperlich M, Ronis DL, & Liberzon I (2009). Prevalence, trauma history, and risk for posttraumatic stress disorder among nulliparous women in maternity care. Obstet Gynecol, 114(4), 839–847. 10.1097/AOG.0b013e3181b8f8a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sperry DM, & Widom CS (2013). Child abuse and neglect, social support, and psychopathology in adulthood: A prospective investigation. Child Abuse & Neglect, 37(6), 415–425. 10.1016/j.chiabu.2013.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, Howard LM, & Pariante CM (2014). Effects of perinatal mental disorders on the fetus and child. The Lancet, 384(9956), 1800–1819. 10.1016/S0140-6736(14)61277-0 [DOI] [PubMed] [Google Scholar]
- Stevens NR, Gerhart J, Goldsmith RE, Heath NM, Chesney SA, & Hobfoll SE (2013). Emotion regulation difficulties, low social support, and interpersonal violence mediate the link between childhood abuse and posttraumatic stress symptoms. Behav Ther, 44(1), 152–161. 10.1016/j.beth.2012.09.003 [DOI] [PubMed] [Google Scholar]
- Sumner L, Wong L, Schetter C, Myers H, & Rodriguez M (2012). Predictors of Posttraumatic Stress Disorder Symptoms Among Low-Income Latinas During Pregnancy and Postpartum. Psychological Trauma: Theory, Research, Practice, and Policy, 4, 196–203. 10.1037/a0023538 [DOI] [Google Scholar]
- Thompson RA (1994). Emotion regulation: A theme in search of definition. Monographs of the Society for Research in Child Development, 59(2/3), 25–52. https://www.ncbi.nlm.nih.gov/pubmed/7984164 [PubMed] [Google Scholar]
- Thompson RA (2019). Emotion dysregulation: A theme in search of definition. Development & Psychopathology, 31(3), 805–815. 10.1017/S0954579419000282 [DOI] [PubMed] [Google Scholar]
- Uguz F, Yakut E, Aydogan S, Bayman MG, & Gezginc K (2019). Prevalence of mood and anxiety disorders during pregnancy: A case-control study with a large sample size. Psychiatry Res, 272, 316–318. 10.1016/j.psychres.2018.12.129 [DOI] [PubMed] [Google Scholar]
- Vesga-López O, Blanco C, Keyes K, Olfson M, Grant BF, & Hasin DS (2008). Psychiatric Disorders in Pregnant and Postpartum Women in the United States. Archives of General Psychiatry, 65(7), 805–815. 10.1001/archpsyc.65.7.805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss NH, Tull MT, Lavender J, & Gratz KL (2013). Role of emotion dysregulation in the relationship between childhood abuse and probable PTSD in a sample of substance abusers. Child Abuse & Neglect, 37(11), 944–954. 10.1016/j.chiabu.2013.03.014 [DOI] [PubMed] [Google Scholar]
- Westbrook J, & Berenbaum H (2017). Emotional Awareness Moderates the Relationship Between Childhood Abuse and Borderline Personality Disorder Symptom Factors. Journal of Clinical Psychology, 73(7), 910–921. 10.1002/jclp.22389 [DOI] [PubMed] [Google Scholar]
- White HR, Widom CS, & Chen PH (2007). Congruence between adolescents’ self-reports and their adult retrospective reports regarding parental discipline practices during their adolescence. Psychol Rep, 101(3 Pt 2), 1079–1094. 10.2466/pr0.101.4.1079-1094 [DOI] [PubMed] [Google Scholar]
- Widom CS, DuMont KA, & Czaja SJ (2007). A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up [Comparative Study [DOI] [PubMed] [Google Scholar]
- Research Support, N.I.H., Extramural.
- Research Support, U.S. Gov’t, Non-P.H.S.]. Archives of General Psychiatry, 64(1), 49–56. 10.1001/archpsyc.64.1.49 [DOI] [Google Scholar]
- Wolf S, & Suntheimer NM (2019). A dimensional risk approach to assessing early adversity in a national sample. Journal of Applied Developmental Psychology, 62, 270–281. 10.1016/j.appdev.2019.03.004 [DOI] [Google Scholar]
- Xia Y, & Yang Y (2019). RMSEA, CFI, and TLI in structural equation modeling with ordered categorical data: The story they tell depends on the estimation methods. Behavior Research Methods, 51(1), 409–428. 10.3758/s13428-018-1055-2 [DOI] [PubMed] [Google Scholar]
- Zald DH, & Treadway MT (2017). Reward Processing, Neuroeconomics, and Psychopathology. Annu Rev Clin Psychol, 13(1), 471–495. 10.1146/annurev-clinpsy-032816-044957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zamir O, & Lavee Y (2015). Emotional Awareness and Breaking the Cycle of Revictimization. Journal of Family Violence, 30(6), 675–684. 10.1007/s10896-015-9711-0 [DOI] [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, & Farley GK (1988). The Multidimensional Scale of Perceived Social Support. Journal of Personality Assessment, 52(1), 30–41. 10.1207/s15327752jpa5201_2 [DOI] [PubMed] [Google Scholar]
- Zimet GD, Powell SS, Farley GK, Werkman S, & Berkoff KA (1990). Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J Pers Assess, 55(3–4), 610–617. 10.1080/00223891.1990.9674095 [DOI] [PubMed] [Google Scholar]


