Abstract
The global increases in obesity and nutrition-related noncommunicable diseases (NCDs) have created a need for major new food policy initiatives. A major concern has been the large impact of ultra-processed food and drink products on weight gain and the risk of several NCDs. These foods, generally high in energy and added sugar, sodium and unhealthy fats, and poor in fiber, protein, and micronutrients, are viewed as a major health concern while also adversely impacting the environment (both carbon emission and water scarcity concerns). Although this may be true in other countries, in SA there is a tendency to add a load of micronutrients to UPF. Food control refers to this as “fake foods.” While over 45 countries and smaller subregional or urban entities have created taxes on ultra-processed beverages such as sugar-sweetened beverages (SSBs), only a few have adopted taxes on snacks and other ultra-processed foods, and none have added major subsidies for truly healthy fresh or minimally processed food for the poor. A second major focus has been on developing impactful front of the package labeling. A smaller number of countries have selected the most impactful warning labels and linked them with other policies to create a mutually reinforcing set of policies. A few have developed meaningful school feeding policies. We present in depth results from key countries involved in all these actions as well as comprehensive marketing controls. We then end with our recommendations for the future. This area is quite young; progress to date is substantial but much more is left to learn.
Introduction
In the last decades, in all low- and middle-income countries (LMICs) across the globe we saw significant increases in overweight/obesity and nutrition-related noncommunicable diseases (NCDs) including diabetes, hypertension, coronary heart disease, and 13 of the 15 most prevalent cancers.1–4 In most LMICs, these burdens are shifting from the affluent to the poor, and in many overweight/obesity is increasing even in rural areas.4, 5 Simultaneously in rural areas in South Asia and sub-Saharan Africa (SSA) countries are still struggling with stunting.4
During 1990–2010, LMICs primarily focused on reducing undernutrition and have focused less on obesity and related NCDs. Since the 2010s however, there has been a shift to focusing on reducing morbidity and mortality from NCDs through prevention and treatment, as recommended by WHO and outlined in SDG Target 3.4.6, 7 To achieve this goal, a number of LMICs, particularly countries in Latin America and South Africa, have led the way in instituting national policies, focusing both on cutting added sugar, sodium, and unhealthy fats as well as reducing consumption of ultra-processed foods (UPF), including sugar-sweetened beverages (SSB) and high-energy dense, nutrient-poor packaged foods, which have been strongly linked to weight gain as well as many prevalent NCDs. These policies include fiscal measures (primarily taxes); regulations to reduce or ban marketing of UPF, especially to children; front-of-the-package (FOP) warning labeling; setting limits on sodium or trans fats in processed food and regulations controlling access to and promotion of UPF in schools. National policies like these significantly modify the food environment in which people purchase and consume foods and affect millions of people simultaneously; thus, they are critical for preventing rapid increases in intake of unhealthy foods, and for preventing further increases in obesity and NCD prevalence throughout the population.
Segments of the corporate food industry have attempted to stop, delay, or weaken such policies globally. This wide-ranging interference extends to the following: (1) funding scientists to assert that regulations are not needed and do not work; (2) promoting ineffective corporate self-regulations; (3) directly fighting the proposed regulations; and (4) even tampering with health advocacy organizations using threats, spyware, and other actions as documented by scholars and journalists.
Below we first briefly present the concept of UPF, then we proceed to describe impactful policies that several countries have implemented and highlight a few cases.. We then summarize some industry activities, including a few implemented during the Covid-19 pandemic that raise concerns about the ways in which the food industry continues to undermine public actions to improve health.
Search Strategy
There was no search strategy for this paper. We selectively focus on studies/evaluations of national policies linked with the goal of reducing purchase or consumption of ultra-processed foods and sugar-sweetened beverages. Only for the next section were we systematic and we searched under three terms: nova classification, ultra-processed foods, and highly processed foods. We search in PubMed, Google Scholar, MedRxiv, BioRxiv, to systematically review all studies that were either RCT’s or longitudinal cohort studies. publications in Chinese or English that include data.
The mounting case against ultra-processed products
We define UPF as multi-ingredient, industrially formulated mixtures containing little if any intact foods, following the Nova classification.8 UPF are generally high in added sugar, added sodium, and/or added saturated or trans fats, and low in protein, fiber, and micronutrients.9 While UPF already account for more than 50% of total energy intake in countries like the US, Canada and the United Kingdom, food sales data indicate that these products are the most rapidly growing segment of the globe’s diet10–12. Studies from around the globe report that UPF can constitute as much as 25% of the diets of infants and preschoolers and are a major source of growth for global food companies.10, 12, 13 Moreover, large, carefully conducted cohort studies have consistently shown that increased UPF consumption has a significant impact on the risk of obesity, diabetes, hypertension, dyslipidemia, cardiovascular diseases, and all-cause mortality14,15
In the case of ultra-processed food intake and weight gain, the cohort study findings are supported by tightly controlled experimental data. In a large, well-designed random in-patient controlled trial, Hall and colleagues at the US National Institutes of Health used a crossover design so each person was his or her own control. They offered to normal-weight adults, for two weeks, diets with non-UPF and diets with most energy from UPF (near 80%). When fed the non-UPF diet participants lost 0·9 kilograms, but when fed the UPF diet they gained 0·9 kilograms.16 Participants were oriented to eat and drink as much or as little as they want of the meals provided and both offered meals that had the same amount of total energy, fiber, protein, carbohydrates, and fat. The researchers found that the same individuals consumed 500 kilocalories (kcal) more when they were in the UPF diet than when they were in the non-UPF diet. This suggests that the UPF diet was less satiating or through some other mechanism encouraged increased consumption, which is an area that needs further study.
Thus, one of the present challenges of food and nutrition policies, particularly for LMICs, relates to halting the increasing consumption of UPFs. In LMICs, this is especially pressing as they are new and growing markets particularly for multinational and transnational UPF companies. They are in effect representing a new kind of food colonialism that are controlling food markets in many countries.17–19 Countries have many routes to reduce harmful foods and policies focused on promoting them (e.g., using human rights for children to end manipulation of children with marketing). Here we focus on selected policies which are being promoted by various countries ranging from taxation to marketing controls to food subsidies, front-of-the-package (FOP) labeling and shifts in school foods and the school food environment. These policies have been effective in controlling harmful products such as tobacco and alcohol20–22.
In September 2021 in Tokyo there will be a UN Food Systems Summit.23 One key goal is to improve the dietary quality of the world’s diets. Unfortunately, it is still not clear that the organizers of this Summit and two action tracks related to healthy diets and sustainable consumption patterns will specifically address UPFs and the growing body of research which shows its large impact on our health.23 Not only do these foods adversely affect our health but they have a large deleterious effect on our carbon emissions and water supply.24–26
Policy options for meaningful national impact
Countries can employ one or many of the policies laid out below. It is important to note that no single policy is a panacea. Policies implemented in isolation can reduce to some extent some UPFs, particularly SSBs, but to drive large enough changes to change food systems and prevent NCDs, it will be important to follow a route like Chile [noted below] and create linked policies that are mutually reinforcing.27 It is important to note that the approaches discussed below have all been demonstrated as effective in controlling other harmful commodities, such as tobacco and alcohol; moreover these are most effective when involving a comprehensive set of linked strategies such as we note for Chile in this section, rather than single policies implemented in isolation.28, 29
Fiscal policy
Taxation has been a major policy used to discourage consumption of UPFs including SSBs and high-energy dense packaged foods.30 Countries have adopted a mixture of tax designs in terms of their base (ad valorem or percent of value vs specific), what the tax amount depends on (sugar density, volume, or base price), and the level of tax. Specific volume-based taxes with adjustments for inflation appear popular and have been shown to result in more complete pass-through of the tax onto prices. Specific sugar-based taxes have been introduced in the United Kingdom (UK) and South Africa. After conversion, rates of existing taxes vary from a small percentage tax up to a 50% tax on SSBs and 4–10% tax on packaged foods.
Mexico was the first to rigorously evaluate a volume based SSB tax. After several studies found that this tax significantly impacted consumption equivalent with its tax level, over 35 additional countries, regions within countries, and municipalities instituted an SSB tax.31, 32 At the same time Mexico also instituted an ad valorem tax on packaged foods considered nonessential. We highlight the evaluation of Mexico’s tax in box 1 and South Africa’s in box 2 as they represent two different approaches to creating SSB taxes.
Mexico Box (Box 1)
Mexican healthy food policies
We focus only on the SSB and nonessential food taxes; however, it is important to note Mexico introduced a strong FOP warning label policy in October 2020; evaluation is underway. The one peso per liter (volume-based specific excise) tax on SSBs and an 8% ad valorem nonessential food tax were implemented in 2014.
- SSB tax implemented since 1 Jan 2014.
- M. A. Colchero, S. W. Ng, and others have shown that the SSB tax were passed on to prices and that SSB purchases fell.31, 33–35 At one peso per liter, it was approximately a 10% volumetric tax, and purchases of taxed beverages fell by an average of 6%. Reductions from pretax trends were highest among lower socioeconomic status (SES) households, averaging a 9% decline over 2014 and showing a 17% decrease in December 2014. Untaxed beverage purchases increased 4%, mainly driven by an increase in bottled plain water purchases. Additionally, higher SSB purchasers who likely have poorer health outcomes, reduced their SSBs more.35
- Evaluations found that the implementation of tax had no impact on employment.36
- Due to their higher SSB reduction, the poor will reap the greatest health benefits from the taxes.
- Nonessential food tax
-
ii)Complex to implement, this tax generated thousands of queries about products. It was an 8% tax on all nonessential foods with energy densities ≥ 275 kcal/100 grams.
-
iii)Based on pretax trends in 2012–2013, the mean volume of purchases of taxed foods in 2014 declined by 25 grams/capita/month, or a 5·1% change beyond what would have been expected pretax, with no corresponding change in purchases of untaxed foods. Low SES households showed a greater response to the tax, purchasing on average of 10·2% fewer taxed foods than expected pretax. Middle and high SES households purchased 5·8% and 2·3% fewer taxed foods than expected, respectively.41,42
-
iv)High consumers were impacted much more than low consumers.43
-
ii)
South Africa Box (Box 2)
The South African Health Promotion Levy (SSB tax) implemented on 1 April 2018 was the first major tax based on grams of sugar.
This is a sugar-based tax at 0·021 rand per gram of sugar, approximately 10% of the per liter price. Prices of taxable beverages increased over the first year of the tax, while nontaxable beverage prices did not changed meaningfully.44
Urban household purchases of taxable beverages post implementation fell by 29%, and sugar content from these purchases fell by 51%. Importantly, lower SES urban households reduced their SSB volumes and grams of sugar from SSBs by 32% and 57%, respectively.45
Young (18–39 years old) adults surveyed in a Western Cape township about intakes of taxable beverages self-reported a 37% reduction in volume and a 31% reduction in sugar.46 A longitudinal survey of adolescents and adults in Soweto, Johannesburg, found that intake fell by two times/week among medium SSB consumers and seven times/week in high SSB consumers between baseline and 12 months, and the reductions were maintained 24 months post-implementation of the tax.47
Public data on employment in the sugar and beverage industries showed no statistically significant change in employment and followed pre-implementation trends despite expectations that scapegoated the levy.48–50
Lessons learned from studies on Mexico and South Africa’s SSB taxes include:
At an equivalent tax level, a sugar-based SSB tax reduces sugar consumption more than a volume-based tax, while a volume-based SSB tax provides more revenue because it does not stimulate as much reformulation.51
Taxation is progressive from a health perspective. In South Africa and Mexico, the poor are likely to have a higher burden of overweight/obesity, untreated and undiagnosed nutrition related NCDs. The poor are shown to be more likely to reduce their purchases in response to the tax, and thus stand to gain more health benefits by prevention.37–40
Implementing an UPF tax is ideally facilitated when combined with front-of-pack warning labels on selected foods. In Mexico, without such a warning label regulation, enormous complexities and loopholes existed in systematically implementing their packaged food tax based on energy density. For example, not taxing most ice-cream due to lower energy density resulting from the amount of air in the product.
The UPF industry is flexible in the beverages and foods they can sell. Evaluations in Mexico and South Africa found that the taxes did not change employment in the food and beverage sectors.36
FOP warning labels
A significant literature examines FOP labels.48, 52 The rationale for preferring FOP warning labels, used successfully for decades in tobacco regulations, has been also discussed and reviewed by others.52 In short, warning labels help consumers identify SSBs and UPFs, and discourage them from consumption. Chile successfully introduced an octagonal warning label that has had a strong impact and has led many other countries to adopt the labels. To date Israel, Mexico, and Peru have implemented warning label laws, Brazil and Uruguay have passed similar laws and are in the implementation phase, and several countries such as Argentina, Colombia, Costa Rica are discussing similar approaches. In the Chile case we highlight detailed studies of the impacts of that country’s law on SSBs, food reformulations, attitudes toward food, and a potential shift in child food norms;53–55 evaluations also show that the implementation of the FOP label did not impact employment or wages.56 Argentina’s proposal is more all-encompassing as shown in Appendix Table 1. See the Chile details of the evaluation in Box 3.
Chile Box (Box 3)
Chile’s mutually reinforcing policies
Chile introduced a set of linked policies. Building off a nutrient profile model to identify food and drinks high in selected nutrients, it introduced a FOP warning label and linked school bans and marketing controls on the same products over a 4-year period in which the regulation became increasingly stricter. Further, the country is currently considering adding a tax on products with warning labels. Figure 1 lays out these policies.
Figure 1.
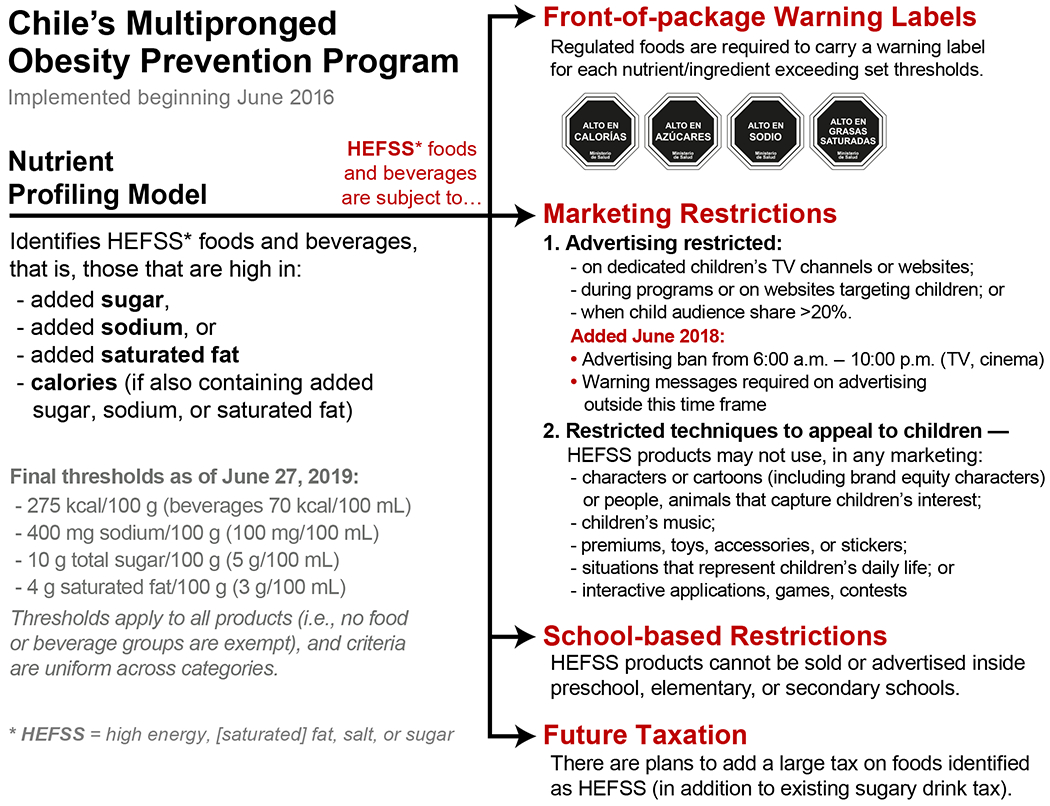
Chile’s Multipronged Obesity Prevention Program
-
1
Chile developed a coordinated comprehensive set of policies to significantly reduce UPF consumption and a nutrient profile model to unite all policies.57, 58 Planners first created the model to delineate products with excessive nutrient content, or were high in added sugar, added saturated fat, or added sodium and whether any of those was added to a food also high in energy density;59 limits became increasingly stringent over 3 phases.
-
2
Research found that the octagonal FOP warning label was impactful, and it was required on all “high-in” foods and beverages with sophisticated size and location requirements.58 Figure 2 presents pictures of foods before and after the FOPL regulation went into effect. Also, notice the cartoon character removal.
-
3
Focus groups with low- and middle-income mothers suggest that after initial implementation of the law profound changes in attitudes toward food purchases driven both by the knowledge mothers gained from these labels and by children telling their mothers not to purchase products with warning labels.55, 59 In conjunction with other Chilean health regulations, including a sugary drink tax and restrictions on junk food marketing to children, Chile’s FOP warning label policy has been associated with a roughly 24% drop in sugary drink purchases in the year following initial implementation.53
-
4
An evaluation comparing the nutritional profiles of products before and after the first year of Chile’s FOP law and other regulations found significant reductions in the proportion of products required to carry warning labels, suggesting that companies reformulated products to improve their health profiles and avoid the FOP warning label requirement.54
-
5
Econometric analyses have shown that the implementation of the policies did not impact labor market outcomes such as employment and wages of sectors likely affected by the regulation.56
Figure 2.
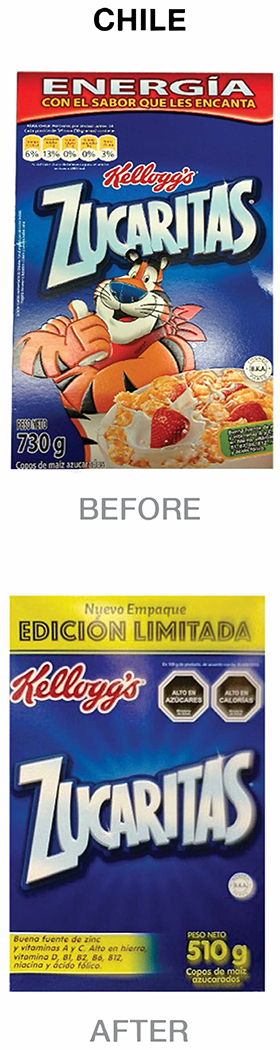
Pictures of Foods before and after the institution of the Chilean set of laws and regulations
Marketing: Chile’s food marketing policies are worth special consideration as the most comprehensive of any country to date.60 The law also prohibits MARKETING those products to children under 14 years of age or marketing with themes or promotional strategies that appeal to children regardless of audience, media, or location. The prohibited marketing approaches include fun or fantasy themes, cartoon characters, animation, children’s music, child actors, situations representing children’s daily lives, free gifts or toys, contests, interactive games, or apps to attract children’s attention; the ban was later expanded to include any type of marketing from 6am to 10pm of high-in products.
-
6
Research shows that the percentage of ads for foods high in energy, saturated fat, sugar, or sodium decreased from 41·9% before the regulation to 14·8% after the regulation’s implementation, resulting in a 44% decrease in exposure to “high-in” foods advertisement in children and a 58·0% declined for adolescents during the first year of the law implementation.61
Mexico also implemented the FOPL and baseline data for an evaluation are being organized. By the end of 2022 it will also remove characters and in addition claims on packages with warning labels. Figure 3 presents foods from Mexico where the warning labels are larger.
Figure 3.

Pictures of Foods from Mexico before and after institution of the Front-of-the package warning label law
Marketing bans on UPF.
Over decades, we have learned that industry self-regulation does not work.62, 63 Box 3 presented results from the important Chilean government introduced marketing bans, first on children-focused marketing and subsequently a complete ban on all marketing of warning labeled food from 6am to 10pm. Following Chile (see Chile box), 67–69 the UK introduced a proposal to limit marketing of foods excessively high in fat, salt and sugar on November 12, 2020.64–66 They do not have as of this time a FOPL warning label that would facilitate such a ban.
School Food Policies
School feeding is an important vehicle to address inequities in diet and may be the only way to give a healthy meal to children from poor families. In addition, the school environment plays an important role in shaping children’s perspective on life and the food marketing and school food program are key parts of that.
Several countries have banned all UPF marketing in schools. Brazil’s efforts have been exemplary (see Boxes 3 and 4) However, efforts in schools still lack rigorous evaluations.
Along with banning marketing, many countries have banned SSBs from school meals and vending. Fewer have banned all UPF, which remains an important goal. Chile has banned all foods with warning labels from schools as well as their promotion or free distribution (see Figure 1).
Another effort to improve school food is to increase the proportion of real food available. Many countries focus on nutrient content of the meals offered which allows caterers to provide often ultra-processed food as long as minimal nutrient requirements are met. Brazil’s national school food program requires that 30% of the food come from local farmers and includes clear nutritional requirements. As we discuss in the Brazil box, a second phase with new guidelines will begin in 2023.
Brazil Box (Box 4)
Brazil’s guidelines
Brazil was one of the first countries with its school ban and now its push to follow the unique Brazilian dietary guidelines to systematically address all aspects of school feeding and the school environment.
Brazil’s school program feeds children in over 150,000 schools and serves over 80% of the country’s school-aged children. The Programa Nacional de Alimentação Escolar (PNAE) includes a 2009 law that requires that > 30% of food procured for schools must come from local family farmers. This is the first national school food program in the world with a mandatory farm-to-school component to increase healthy food in schools and support local farmers. In 2013 Brazil strengthened the law with regulations requiring a minimum of three servings of fruits and vegetables per week, prohibition of sugary drinks, and maximum values for added sugar, fat, saturated fat, trans fat, and sodium in processed foods.
In 2023 new regulations will bring the PNAE procurement guidelines closer to the Dietary Guidelines for the Brazilian Population.67 The regulations state that a minimum 75% of school meal funds must be spent on unprocessed or minimally processed foods, a maximum of 20% on processed foods (preferably not UPF), and up to 5% on culinary ingredients, such as salt, oil, and sugar.
Several Latin American, SSA, and Asian countries have copied this law. The program’s impact on both farmers and schoolchildren is currently under evaluation.
4). Media campaigns
Very few countries institute meaningful media campaigns to explain new laws and regulations. Usually, most knowledge comes from the media without government involvement. In Mexico a multisectoral working group (GISAMAC), in which the ministries of Health, Economics, Environment, Education and other government agencies participate has developed a Media campaign to explain the warning labels, other healthy eating recommendations.68 South Africa and Chile also have media campaigns following major regulatory actions by the Ministries of Health.
Neutralizing and minimizing industry influences on and interference in health policy making
Most countries critically need a consortium to systematically study, call out and neutralize industry interference with health policy making. In theory, decision making around health policy should be up to consumers and the government. However, the food and beverage sector routinely attempt to stop mandatory regulation,69 including through corporate responsibility pledges.70 Compared to most governmental policies, industry pledges are narrower in scope, use weak nutrition criteria, are poorly implemented, and enforced, and inconsistent across companies and jurisdictions.62, 71–74
Industry often interferes with research by creating front groups, funding academics or research institutes to challenge the research behind regulations or to proclaim that regulations are unneeded.75 Industry-funded studies usually claim that SSBs and other products that public health advocates wish to regulate have no health impact."76–79
In the last year, many industry players in LMICs tried to position UPF as essential products. During the Covid-19 pandemic the industry has donated UPF and drinks and infant formula to vulnerable populations, including schoolchildren and low-income people, contributing to worsening health conditions like obesity, diabetes, and cardiovascular disease.80–82 Infant formula is governed by global marketing bans, and its promotion is unethical.82
We cannot cite even one example of the industry playing a positive role in advancing impactful regulations to reduce consumption of the unhealthiest UPF.
Colleagues in Mexico initiated a unique initiative to offset industry interference in public health policy. The Nutricia Code was created as an alliance between health institutions, universities, government sectors and civil society in Mexico to increase awareness of the negative influence that commercial interests from food industry have on NCD prevention policies.83
The Future
We are still early in our understanding of the best practices for changing the food environment to reduce consumption of UPF and promoting heathier eating. We need more objective evaluations not funded by the industry. Critically, evaluation research must focus on actual purchases and consumption. We can also learn from qualitative research into what might change eating norms, to ensure that the healthy choice is the easy choice which is our long-term goal.
Our goal is ultimately to promote healthier eating; however, it is clear with the large and fairly rapid increases in sales and consumption of UPFs, we must first reduce their consumption and change the global and country food environments. Then we can focus on promoting healthy eating by both fiscal policy and encouraging healthy whole foods. A number of countries have logos focusing on only health foods such as the Keyhole in Scandinavia and Israel’s very selective green label.84–86 Given the rapid growth in UPFs globally, reducing UPFs must be the first priority before addressing the healthy eating goals personified by the Brazilian and Israeli dietary guidelines.
In this review we do not address the large important input of civil society, namely key NGO consumer advocacy groups in Mexico, South Africa, and Brazil, which sought to advocate for these policies, lobby political champions, and strategically counteract or prevent industry pushback and interference. The sophisticated campaigns by these groups, usually linked with important researcher contributions took place over several years leading to final policies. And we cannot underestimate for Latin American countries and South Africa the important role of Bloomberg Philanthropies Food Policy Program in providing funding for many of these campaigns in the last decade.
A particular gap in the fiscal policy area is the lack of subsidies or incentives that promote purchases of healthier foods and encourage healthy eating. When combined with food taxes, subsidies and incentives have the potential to improve nutritional quality and health outcomes.87–89 We need to better understand what induces meaningful supply changes and how to enhance healthy purchases across store types. In addition, we need to work with the agricultural sector to reduce sugar production and promote alternate crops for sugar farmers. In LMICs, the presence of all forms of malnutrition (stunting, wasting, overweight and obesity) also means that policies must identify and target the shared drivers.
One important note is that we expect to see changes in the food supply, food purchases, and dietary intake. Only after a varying set of years changes in health, such as reductions in adiposity or incidence of type 2 diabetes, can be documented so we must take a long-term view of decades of monitoring to see meaningful changes.38, 40, 90, 91 This is especially important to understand, because we anticipate that the food industry will use a purported “lack of effect” as a key strategy in rejecting or removing these policies. They will call for immediate changes in child obesity and call out the policies as ineffective as changes will not be quickly seen.
This is a call for action. This article highlights a few countries with important documented policy with significant impacts across the globe to reduce obesity and key NCDs. Within a span of 10 years, there is already some good evidence of fiscal and FOP policies that can make projected future health changes as projected in Mexico that benefits the public, enhances equity, while not harming industry.38, 40, 90, 91 .Once the final implementation of Chile’s set of labeling and marketing laws is evaluated, we are sure comparable if not greater effects will be shown. The school food policies need much more careful evaluations before we can show a similar significant effect. Additional policies that are starting to be piloted should be also considered if they prove to be effective, equitable and appropriate for each setting. Because any one of these policies alone will not make enough of a difference, we also need to better understand cost-effectiveness of these actions (in isolation and together) under different contexts that can achieve the unifying goal of transforming foods systems for ensuring healthy diets for all.
As with the policies reviewed, we feel there is a strong need to focus on first reducing UPF consumption globally. Clearly this will benefit both those facing stunting and undernutrition as well as all the nutrition-related noncommunicable diseases(termed double duty actions).92 Also, we must consider the environmental aspects of the healthy food policies as seen in the Brazilian and Israeli dietary guidelines and thus consider triple duty actions to address our global syndemic of overweight/obesity, stunting and climate-environment-related sustainability.24, 67, 93 This requires industry to develop products that are less processed which will address many of our concerns for triple duty action benefiting those concerned with overweight-obesity and other NR-NCDs as well as stunting and other forms of undernutrition.
Above all else, we are calling for action. We want evidence-informed policy, but we also cannot afford to wait decades for the evidence to be complete. Given that evaluations to date have shown little to no economic harm, and that obesity and NCDs prevention is less costly and complex than obesity and NCDs treatment, the time to act is now.
Supplementary Material
Acknowledgements:
We thank Neena Prasad, Bloomberg Philanthropies for her leadership and Ms. Ariel Adams is thanked for administrative support for this paper.
Funding: All involved in this paper received funding from the Bloomberg Philanthropy for this work. Popkin, Ng, and Taillie received additional funding from the Laura and John Arnold Foundation, the Robert Wood Johnson Foundation, and the National Institutes of Health (NIH) (CPC P2C HD050924, P30 AG066615, NIH R01DK108148). Hofman received additional funding from the South African Medical Research Council (D1305910-03).
Footnotes
Conflicts of interest: None of the authors declare a conflict of interest.
REFERENCES
- 1.World Cancer Research Fund/American Institute for Cancer Research. Diet, nutrition, physical activity and cancer: a global perspective. London: World Cancer Research Fund International; 2018. [Google Scholar]
- 2.Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2020;396(10258):1204–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, et al. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020;396(10258):1223–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. The Lancet. 2020;395(10217):65–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bixby H, Bentham J, Zhou B, Di Cesare M, Paciorek CJ, Bennett JE, et al. Rising rural body-mass index is the main driver of the global obesity epidemic in adults. Nature. 2019;569(7755):260–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United Nations. Open Working Group proposal for Sustainable Development Goals. 2014. [Google Scholar]
- 7.Hawkes C, Popkin BM. Can the sustainable development goals reduce the burden of nutrition-related non-communicable diseases without truly addressing major food system reforms? BMC Medicine. 2015;13(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Monteiro CA, Cannon G, Moubarac JC, Levy RB, Louzada MLC, Jaime PC. The UN Decade of Nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutr. 2018;21(1):5–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Monteiro C, Cannon G, Lawrence M, Costa Louzada M, Pereira Machado P. Ultra-processed foods, diet quality, and health using the NOVA classification system. Rome: FAO; 2019. [Google Scholar]
- 10.Monteiro CA, Moubarac JC, Cannon G, Ng SW, Popkin B. Ultra-processed products are becoming dominant in the global food system. Obes Rev. 2013;14 Suppl 2:21–8. [DOI] [PubMed] [Google Scholar]
- 11.Wu Y, Wang L, Zhu J, Gao L, Wang Y. Growing fast food consumption and obesity in Asia: Challenges and implications. Social Science & Medicine. 2021;269:113601. [DOI] [PubMed] [Google Scholar]
- 12.Baker P, Machado P, Santos T, Sievert K, Backholer K, Hadjikakou M, et al. Ultra-processed foods and the nutrition transition: Global, regional and national trends, food systems transformations and political economy drivers. Obes Rev. 2020;21(12):e13126. [DOI] [PubMed] [Google Scholar]
- 13.Pries AM, Rehman AM, Filteau S, Sharma N, Upadhyay A, Ferguson EL. Unhealthy Snack Food and Beverage Consumption Is Associated with Lower Dietary Adequacy and Length-for-Age z-Scores among 12-23-Month-Olds in Kathmandu Valley, Nepal. J Nutr. 2019;149(10):1843–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pagliai G, Dinu M, Madarena MP, Bonaccio M, Iacoviello L, Sofi F. Consumption of ultra-processed foods and health status: a systematic review and meta-analysis. Br J Nutr. 2021;125(3):308–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lawrence MA, Baker PI. Ultra-processed food and adverse health outcomes. BMJ. 2019;365:12289. [DOI] [PubMed] [Google Scholar]
- 16.Hall KD, Ayuketah A, Brychta R, Cai H, Cassimatis T, Chen KY, et al. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell Metab. 2019;30(1):67–77.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Friedmann H From Colonialism to Green Capitalism: Social Movements and Emergence of Food Regimes. In: Frederick HB, Philip M, editors. New Directions in the Sociology of Global Development. Research in Rural Sociology and Development. 11: Emerald Group Publishing Limited; 2005. p. 227–64. [Google Scholar]
- 18.Dreher N Food from Nowhere: Complicating Cultural Food Colonialism to Understand Matcha as Superfood. Gradfoodstudies. 2018;5(1). [Google Scholar]
- 19.Dietler M Culinary encounters: food, identity, and colonialism. In: Twiss K, editor. In The Archaeology of Food and Identity. Carbondale: Center for Archaeological Investigations Press, Southern Illinois Univ; 2007. p. 218–42. [Google Scholar]
- 20.Warner KE. Tobacco Policy in the United States: Lessons for the Obesity Epidemic. In: Mechanic D, Rogut LB, Colby DC, Knickman JR, editors. Policy Challenges in Modern Health Care. New Brunswick, NJ: Rutgers University Press; 2005. p. 99–114. [Google Scholar]
- 21.Chaloupka FJ, Powell LM, Warner KE. The Use of Excise Taxes to Reduce Tobacco, Alcohol, and Sugary Beverage Consumption. Annual Review of Public Health. 2019. [DOI] [PubMed] [Google Scholar]
- 22.Moodie R, Stuckler D, Monteiro C, Sheron N, Neal B, Thamarangsi T, et al. Profits and pandemics: prevention of harmful effects of tobacco, alcohol, and ultra-processed food and drink industries. Lancet. 2013;381(9867):670–9. [DOI] [PubMed] [Google Scholar]
- 23.United Nations. The 2021 Food Systems Summit New York City New York City: United Nations; 2021. [Available from: https://www.un.org/en/food-systems-summit. [Google Scholar]
- 24.Fardet A, Rock E. Ultra-processed foods and food system sustainability: What are the links? Sustainability. 2020;12(15):6280. [Google Scholar]
- 25.Hoekstra AY, Chapagain AK. Water footprints of nations: Water use by people as a function of their consumption pattern. Water Resources Management. 2007;21(1):35–48. [Google Scholar]
- 26.Constantino-Toto R, Montero D. Water Footprint of Bottled Drinks and Food Security. Water, Food and Welfare Briefs in Environment, Security, Development and Peace. New York: Springer; 2016. p. 229–39. [Google Scholar]
- 27.The World Bank. Obesity: Health and Economic Consequences of an Impending Global Challenge. Shekar M, Popkin B, editors. Washington DC: The World Bank; 2020. January 27, 2020. [Google Scholar]
- 28.Knai C, Petticrew M, Capewell S, Cassidy R, Collin J, Cummins S, et al. The case for developing a cohesive systems approach to research across unhealthy commodity industries. BMJ Glob Health. 2021;6(2):e003543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Warner KE. Tobacco policy in the United States: Lessons for the obesity epidemic. Policy Challenges in Modern Health Care. 2005:99–114. [Google Scholar]
- 30.The World Bank. Taxes on Sugar-Sweetened Beverages : Summary of International Evidence and Experiences. Washington DC; 2020. [Google Scholar]
- 31.Colchero MA, Popkin BM, Rivera JA, Ng SW. Beverage purchases from stores in Mexico under the excise tax on sugar sweetened beverages: observational study. BMJ. 2016;352:h6704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Colchero MA, Rivera-Dommarco J, Popkin BM, Ng SW. In Mexico, evidence of sustained consumer response two years after implementing a sugar-sweetened beverage tax. Health Affairs. 2017;36(3):564–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Colchero MA, Zavala JA, Batis C, Shamah-Levy T, Rivera-Dommarco JA. Changes in prices of taxed sugar-sweetened beverages and nonessential energy dense food in rural and semi-rural areas in Mexico. Salud Publica Mex. 2017;59(2):137–46. [DOI] [PubMed] [Google Scholar]
- 34.Colchero MA, Salgado JC, Unar-Munguia M, Molina M, Ng S, Rivera-Dommarco JA. Changes in prices after an excise tax to sweetened sugar beverages was implemented in Mexico: evidence from urban areas. PLoS ONE. 2015;10(12):e0144408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ng SW, Rivera JA, Popkin BM, Colchero MA. Did high sugar-sweetened beverage purchasers respond differently to the excise tax on sugar-sweetened beverages in Mexico? Public Health Nutr. 2018:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guerrero-López CM, Molina M, Colchero MA. Employment changes associated with the introduction of taxes on sugar-sweetened beverages and nonessential energy-dense food in Mexico. Prev Med. 2017;105s:S43–s9. [DOI] [PubMed] [Google Scholar]
- 37.Basto-Abreu A, Braverman-Bronstein A, Camacho-García-Formentí D, Zepeda-Tello R, Popkin BM, Rivera-Dommarco J, et al. Expected changes in obesity after reformulation to reduce added sugars in beverages: A modeling study. PLOS Medicine. 2018;15(10):e1002664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Torres-Álvarez R, Barrán-Zubaran R, Canto-Osorio F, Sánchez-Romero LM, Camacho-García-Formentí D, Popkin BM, et al. Body weight impact of the sugar-sweetened beverages tax in Mexican children: A modeling study. Pediatric Obesity. 2020;15(8):e12636. [DOI] [PubMed] [Google Scholar]
- 39.Barrientos-Gutierrez T, Zepeda-Tello R, Rodrigues ER, Colchero-Aragonés A, Rojas-Martínez R, Lazcano-Ponce E, et al. Expected population weight and diabetes impact of the 1-peso-per-litre tax to sugar sweetened beverages in Mexico. PLOS ONE. 2017;12(5):e0176336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Sánchez-Romero LM, Penko J, Coxson PG, Fernández A, Mason A, Moran AE, et al. Projected Impact of Mexico’s Sugar-Sweetened Beverage Tax Policy on Diabetes and Cardiovascular Disease: A Modeling Study. PLoS Med. 2016;13(11):e1002158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Batis C, Rivera JA, Popkin BM, Taillie LS. First-Year Evaluation of Mexico’s Tax on Nonessential Energy-Dense Foods: An Observational Study. PLoS Med. 2016;13(7):e1002057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hernández-F M, Batis C, Rivera JA, Colchero MA. Reduction in purchases of energy-dense nutrient-poor foods in Mexico associated with the introduction of a tax in 2014. Preventive Medicine. 2019;118:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Taillie LS, Rivera JA, Popkin BM, Batis C. Do high vs. low purchasers respond differently to a nonessential energy-dense food tax? Two-year evaluation of Mexico’s 8% nonessential food tax. Prev Med. 2017;105s:S37–s42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stacey N, Mudara C, Ng SW, van Walbeek C, Hofman K, Edoka I. Sugar-based beverage taxes and beverage prices: Evidence from South Africa’s Health Promotion Levy. Social Science & Medicine. 2019;238:112465. [DOI] [PubMed] [Google Scholar]
- 45.Stacey N, Edoka I, Hofman K, Swart R, Popkin BM, Ng SW. Changes in Beverage Purchases Following the Announcement and Implementation of South Africa’s Health Promotion Levy: An Observational Study. Lancet Planetary Health. 2021. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Essman M, Taillie L, Ng S, Popkin B, Jenkings T, R S. Changes in taxed and untaxed beverage intake by South African young adults after a national sugar-sweetened beverage tax: a before-and-after study. PLoS Med. 2021. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wrottesley SV, Stacey N, Mukoma G, Hofman KJ, Norris SA. Assessing sugar-sweetened beverage intakes, added sugar intakes and BMI before and after the implementation of a sugar-sweetened beverage tax in South Africa. Public Health Nutr. 2020:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mandle J, Tugendhaft A, Michalow J, Hofman K. Nutrition labelling: a review of research on consumer and industry response in the global South. Glob Health Action. 2015;8:25912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.BFAP. BFAP BASELINE AGRICULTURAL OUTLOOK 2019 - 2028. Pretoria: Bureau for Food and Agricultural Policy (BFAP); 2019. [Google Scholar]
- 50.Priceless SA. Policy Brief: The Health Promotion Levy and the South African Labor Market 2019. Johannesburg, South Africa: Priceless SA; 2019. [Google Scholar]
- 51.Allcott H, Lockwood BB, Taubinsky D. Should We Tax Sugar-Sweetened Beverages? An Overview of Theory and Evidence. Journal of Economic Perspectives. 2019;33(3):202–27. [Google Scholar]
- 52.Taillie LS, Hall MG, Popkin BM, Ng SW, Murukutla N. Experimental Studies of Front-of-Package Nutrient Warning Labels on Sugar-Sweetened Beverages and Ultra-Processed Foods: A Scoping Review. Nutrients. 2020;12(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Taillie LS, Reyes M, Colchero MA, Popkin B, Corvalán C. An evaluation of Chile’s Law of Food Labeling and Advertising on sugar-sweetened beverage purchases from 2015 to 2017: A before-and-after study. PLOS Medicine. 2020;17(2):e1003015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Reyes M, Smith Taillie L, Popkin B, Kanter R, Vandevijvere S, Corvalán C. Changes in the amount of nutrient of packaged foods and beverages after the initial implementation of the Chilean Law of Food Labelling and Advertising: A nonexperimental prospective study. PLoS medicine. 2020;17(7):e1003220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Correa T, Fierro C, Reyes M, Dillman Carpentier FR, Taillie LS, Corvalan C. Responses to the Chilean law of food labeling and advertising: exploring knowledge, perceptions and behaviors of mothers of young children. International Journal of Behavioral Nutrition and Physical Activity. 2019;16(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Paraje G WJM, Colchero A, Popkin B M,. Employment and Real Wage Changes associated with the warning label regulations in Chile. Food Policy. 2021. [Google Scholar]
- 57.Corvalán C, Reyes M, Garmendia ML, Uauy R. Structural responses to the obesity and non-communicable diseases epidemic: the Chilean Law of Food Labeling and Advertising. Obes Rev. 2013;14 Suppl 2:79–87. [DOI] [PubMed] [Google Scholar]
- 58.Reyes M, Garmendia ML, Olivares S, Aqueveque C, Zacarías I, Corvalán C. Development of the Chilean front-of-package food warning label. BMC Public Health. 2019;19(1):906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Corvalán C, Reyes M, Garmendia ML, Uauy R. Structural responses to the obesity and non-communicable diseases epidemic: Update on the Chilean law of food labelling and advertising. Obes Rev. 2019;20(3):367–74. [DOI] [PubMed] [Google Scholar]
- 60.Taillie LS, Busey E, Stoltze FM, Dillman Carpentier FR. Governmental policies to reduce unhealthy food marketing to children. Nutr Rev. 2019;77(11):787–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Correa T, Reyes M, Taillie LS, Corvalán C, Dillman Carpentier FR. Food Advertising on Television Before and After a National Unhealthy Food Marketing Regulation in Chile, 2016-2017. American journal of public health. 2020;110(7):1054–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Galbraith-Emami S, Lobstein T. The impact of initiatives to limit the advertising of food and beverage products to children: a systematic review. Obes Rev. 2013;14(12):960–74. [DOI] [PubMed] [Google Scholar]
- 63.Chambers SA, Freeman R, Anderson AS, MacGillivray S. Reducing the volume, exposure and negative impacts of advertising for foods high in fat, sugar and salt to children: A systematic review of the evidence from statutory and self-regulatory actions and educational measures. Prev Med. 2015;75:32–43. [DOI] [PubMed] [Google Scholar]
- 64.Sweney M UK to ban all online junk food advertising to tackle obesity 2020. Available from: https://www.theguardian.com/media/2020/nov/10/uk-to-ban-all-online-junk-food-advertising-to-tackle-obesity. [Google Scholar]
- 65.Ofcom. Television Advertising of Food and Drink Products to Children London 2006. [Available from: https://www.ofcom.org.uk/consultations-and-statements/category-2/foodads_new. [Google Scholar]
- 66.Silva A, Higgins LM, Hussein M. An Evaluation of the Effect of Child-Directed Television Food Advertising Regulation in the United Kingdom. Canadian Journal of Agricultural Economics/Revue canadienne d’agroeconomie. 2015;63(4):583–600. [Google Scholar]
- 67.Ministry of Health Brazil. Dietary Guidelines for the Brazilian Population, 2nd edition. Brasilia: Ministry of Health Brazil; 2014. [Google Scholar]
- 68.Carrera VS. Gisamac presenta acciones a favor de la alimentación mexicana. In: Development UoFaCotSoAaR, editor. Mexico: 2020. p. 8:52. [Google Scholar]
- 69.Sharma LL, Teret SP, Brownell KD. The food industry and self-regulation: standards to promote success and to avoid public health failures. Am J Public Health. 2010;100(2):240–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gunningham N, Rees J. Industry Self-Regulation: An Institutional Perspective. Law & Policy. 1997;19(4):363–414. [Google Scholar]
- 71.Kunkel DL, Castonguay JS, Filer CR. Evaluating Industry Self-Regulation of Food Marketing to Children. Am J Prev Med. 2015;49(2):181–7. [DOI] [PubMed] [Google Scholar]
- 72.Ronit K, Jensen JD. Obesity and industry self-regulation of food and beverage marketing: a literature review. Eur J Clin Nutr. 2014;68(7):753–9. [DOI] [PubMed] [Google Scholar]
- 73.Kelly B, Vandevijvere S, Ng S, Adams J, Allemandi L, Bahena-Espina L, et al. Global benchmarking of children’s exposure to television advertising of unhealthy foods and beverages across 22 countries. Obesity Reviews. 2019;20(S2):116–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lacy-Nichols J, Scrinis G, Carey R. The politics of voluntary self-regulation: insights from the development and promotion of the Australian Beverages Council’s Commitment. Public Health Nutr. 2020;23(3):564–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nestle M Unsavory truth: how food companies skew the science of what we eat. New York: Basic Books; 2018. [Google Scholar]
- 76.Lesser LI, Ebbeling CB, Goozner M, Wypij D, Ludwig DS. Relationship between funding source and conclusion among nutrition-related scientific articles. PLoS Med. 2007;4(1):e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ojeda E, Torres C, Carriedo Á, Mialon M, Parekh N, Orozco E. The influence of the sugar-sweetened beverage industry on public policies in Mexico. Int J Public Health. 2020;65(7):1037–44. [DOI] [PubMed] [Google Scholar]
- 78.Mialon M, Crosbie E, Sacks G. Mapping of food industry strategies to influence public health policy, research and practice in South Africa. Int J Public Health. 2020;65(7):1027–36. [DOI] [PubMed] [Google Scholar]
- 79.Mialon M, Corvalan C, Cediel G, Scagliusi FB, Reyes M. Food industry political practices in Chile: “the economy has always been the main concern”. Globalization and Health. 2020;16(1):107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Global Health Advocacy Incubator. Facing Two Pandemics: How Big Food Undermined Public Health in the Era of COVID-19. Washington DC: Global Health Advocacy Incubator; 2020. November 17, 2020. [Google Scholar]
- 81.Our commitment to society during the COVID-19 contingency [press release]. Vevey, Switzerland: Nestle, February 12, 2020. 2020. [Google Scholar]
- 82.van Tulleken C, Wright C, Brown A, McCoy D, Costello A. Marketing of breastmilk substitutes during the COVID-19 pandemic. The Lancet. 2020;396(10259):e58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Barquera S, Balderas N, Rodríguez E, Kaufer-Horwitz M, Perichart O, Rivera-Dommarco JA. Nutricia Code: nutrition and conflict of interest in academia. Salud Publica Mex. 2020;62(3):313–8. [DOI] [PubMed] [Google Scholar]
- 84.Endevelt R, Grotto I, Sheffer R, Goldsmith R, Golan M, Mendlovic J, et al. Policy and Practice - Regulatory measures to improve the built nutrition environment for prevention of obesity and related morbidity in Israel. World Health Organization; 2017. December 2017. [Google Scholar]
- 85.Gillon-Keren M, Kaufman-Shriqui V, Goldsmith R, Safra C, Shai I, Fayman G, et al. Development of Criteria for a Positive Front-of-Package Food Labeling: The Israeli Case. Nutrients. 2020;12(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Mørk T, Tsalis G, Grunert K. Campaigning for a healthier diet: Evaluating the case of the Nordic “Keyhole” label 2014T: Trine Mørk. European Journal of Public Health. 2015;25(suppl_3). [Google Scholar]
- 87.Peñalvo JL, Cudhea F, Micha R, Rehm CD, Afshin A, Whitsel L, et al. The potential impact of food taxes and subsidies on cardiovascular disease and diabetes burden and disparities in the United States. BMC Med. 2017;15(1):208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Valizadeh P, Ng SW. Would A National Sugar-Sweetened Beverage Tax in the United States Be Well Targeted? American Journal of Agricultural Economics. n/a(n/a). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Cobiac LJ, Tam K, Veerman L, Blakely T. Taxes and Subsidies for Improving Diet and Population Health in Australia: A Cost-Effectiveness Modelling Study. PLOS Medicine. 2017;14(2):e1002232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Basto-Abreu A, Torres-Alvarez R, Reyes-Sánchez F, González-Morales R, Canto-Osorio F, Colchero MA, et al. Predicting obesity reduction after implementing warning labels in Mexico: A modeling study. PLOS Medicine. 2020;17(7):e1003221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Capewell S, O’Flaherty M. Rapid mortality falls after risk-factor changes in populations. Lancet. 2011;378(9793):752–3. [DOI] [PubMed] [Google Scholar]
- 92.Hawkes C, Ruel MT, Salm L, Sinclair B, Branca F. Double-duty actions: seizing programme and policy opportunities to address malnutrition in all its forms. The Lancet. 2020;395(10218):142–55. [DOI] [PubMed] [Google Scholar]
- 93.Swinburn BA, Kraak VI, Allender S, Atkins VJ, Baker PI, Bogard JR, et al. The Global Syndemic of Obesity, Undernutrition, and Climate Change: The Lancet Commission report. The Lancet. 2019;393(10173):791–846. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


