The complex immunological mechanisms of vaccines bring about an inevitable risk of immune-mediated adverse reactions. Of special interest in this time of epidemic is the safety of COVID-19 vaccines and, in particular, the emerging evidence that the ChAdOx1 nCoV-19 adenoviral vector vaccine from AstraZeneca can cause vaccine-induced immune thrombotic thrombocytopenia (VITT). We present the case of a patient who developed an acute paracentral scotoma after having received this vaccine.
A 27-year-old female was referred for ophthalmology evaluation because of visual disturbances in her left eye. Her past medical history was unremarkable. Her only medication was an oral contraceptive (combined desogestrel and ethinylestradiol). As she worked in a hospital, she had been prioritised for COVID-19 vaccination and had recently received the first dose of the AstraZeneca vaccine. The same day she developed flu-like symptoms. These resolved 2 days later. However, a left paracentral scotoma appeared at this point.
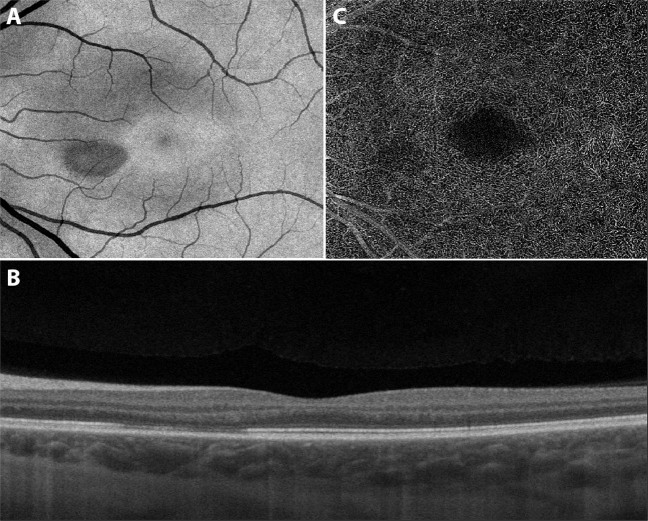
On clinical examination the best-corrected visual acuity was 20/20 in both eyes. Threshold perimetry of the left eye showed a modest paracentral scotoma in the upper temporal quadrant. The intraocular pressure was normal in both eyes, and there were no signs of intraocular inflammation. Fundoscopy of the left eye revealed a delicate teardrop-shaped macular lesion nasally to the fovea (Fig. 1), which was visualised better on swept source optical coherence tomography (SS-OCT) en face images (Fig. 2A). Cross-sectional SS-OCT of the lesion demonstrated slight hyperreflectivity of the outer nuclear and plexiform layers and disruption of the ellipsoid zone (Fig. 2B). SS-OCT angiography indicated subtle dropout in the deep capillary plexus corresponding to the lesion (Fig. 2C). There was no evidence of VITT; laboratory work-up showed a normal complete blood count, negative C-reactive protein and absence of antibodies to platelet factor 4-polyanion complexes.
Fig. 1. Fundus photography of the left macula.

The image displays a delicate teardrop-shaped lesion nasally to the fovea.
Fig. 2. Swept source optical coherence tomography of the left macula.
A The en face image displays a teardrop-shaped macular lesion nasally to the fovea. B The cross-sectional image displays slight hyperreflectivity of the outer nuclear and plexiform layers and disruption of the ellipsoid zone corresponding to the lesion. C The angiogram indicates subtle dropout in the deep capillary plexus corresponding to the lesion.
The signs and symptoms of our patient were consistent with acute macular neuroretinopathy (AMN). The exact pathophysiology of AMN is unknown, but several risk factors have been identified; the most common associations are non-specific flu-like illness or fever and use of oral contraceptives [1]. The present case further expands the spectrum of possible associations. To the best of our knowledge, AMN following COVID-19 vaccination has not been previously published, and a coincidental finding cannot be ruled out. However, there are case reports of AMN in the course of COVID-19 infection [2–4]. An association between AMN and both COVID-19 infection and vaccination raises the question as to whether a common immune-mediated pathway can trigger this peculiar macular disease.
Acknowledgements
The authors wish to thank Dr Ingvild Hausberg Sørvoll for performing the antibody analysis.
Author contributions
All authors took part in the clinical work-up. ADB and ØKJ wrote the draft paper. All authors provided critical feedback and contributed to the final version of the paper.
Competing interests
MCM has been a member of a Bayer, Novartis and Allergan advisory board and has received lecture fees from Bayer and Roche. ØKJ has been member of a Bayer, Allergan and Roche advisory board and has received lecture fees from Bayer and Allergan. ADB, MES and KUS have nothing to disclose.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bhavsar KV, Lin S, Rahimy E, Joseph A, Freund KB, Sarraf D, et al. Acute macular neuroretinopathy: a comprehensive review of the literature. Surv Ophthalmol. 2016;61:538–65. doi: 10.1016/j.survophthal.2016.03.003. [DOI] [PubMed] [Google Scholar]
- 2.Virgo J, Mohamed M. Paracentral acute middle maculopathy and acute macular neuroretinopathy following SARS-CoV-2 infection. Eye. 2020;34:2352–3. doi: 10.1038/s41433-020-1069-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gascon P, Briantais A, Bertrand E, Ramtohul P, Comet A, Beylerian M, et al. Covid-19-associated retinopathy: a case report. Ocul Immunol Inflamm. 2020;28:1293–7. doi: 10.1080/09273948.2020.1825751. [DOI] [PubMed] [Google Scholar]
- 4.Zamani G, Ataei Azimi S, Aminizadeh A, Shams Abadi E, Kamandi M, Mortazi H, et al. Acute macular neuroretinopathy in a patient with acute myeloid leukemia and deceased by COVID-19: a case report. J Ophthalmic Inflamm Infect. 2021;10:39. doi: 10.1186/s12348-020-00231-1. [DOI] [PMC free article] [PubMed] [Google Scholar]